Managing Sample Turbidity and Light Scattering in Drug Solutions: From Fundamental Principles to Regulatory Compliance
This article provides a comprehensive guide for researchers and drug development professionals on managing turbidity and light scattering in pharmaceutical solutions.
Managing Sample Turbidity and Light Scattering in Drug Solutions: From Fundamental Principles to Regulatory Compliance
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on managing turbidity and light scattering in pharmaceutical solutions. It covers the fundamental causes and implications of turbidity, explores advanced analytical techniques like Dynamic Light Scattering (DLS) and nephelometry, and offers practical troubleshooting strategies. The content also addresses critical validation requirements and regulatory considerations to ensure data integrity and compliance throughout the drug development lifecycle, from early discovery to final product release.
Understanding Turbidity and Light Scattering: Fundamental Principles and Impact on Drug Development
Turbidity is the cloudiness or haziness of a fluid caused by the presence of suspended particles that are invisible to the naked eye. These particles scatter and absorb light, preventing it from transmitting straight through the liquid. In pharmaceutical research, particularly in drug solution development, managing turbidity is critical as it directly impacts drug solubility, bioavailability, and safety [1] [2].
The underlying mechanism is light scattering. When a beam of light passes through a liquid sample, it interacts with suspended particles. The light is scattered in different directions, and the intensity and pattern of this scattered light provide information about the concentration, size, and sometimes the shape of the particles [3]. This phenomenon is described by several key techniques:
- Dynamic Light Scattering (DLS): Measures fluctuations in scattered light intensity to determine the size of nanoparticles (typically 5-500 nm) undergoing Brownian motion [3].
- Static Light Scattering (SLS): Measures the time-averaged intensity of scattered light at various angles to determine molecular weight and particle size over a broader range (0.1 µm to 100 µm) [3].
- Nephelometry: Specifically measures the intensity of light scattered at a specific angle (often 90 degrees) to determine particle concentration [2].
- Turbidimetry: Measures the intensity of light transmitted directly through a sample; higher particle concentration scatters more light, resulting in less transmitted light [4].
For drug development professionals, controlling turbidity is essential for ensuring drug product quality and efficacy, particularly for injectable and ophthalmic solutions where particulate matter can pose significant patient risks [5] [6].
Troubleshooting Guides & FAQs
Common Experimental Issues and Solutions
| Problem | Possible Causes | Troubleshooting Steps |
|---|---|---|
| Erratic/Unstable Readings [4] [7] | Sample precipitation/settling during measurement; Air bubbles in sample. | Use fresh samples; Control reaction times; Ensure gentle mixing (no vigorous shaking); Allow decantation time for bubbles to settle; Inspect sample for bubbles before measurement [4] [7]. |
| Abnormally High or Low Values [4] [7] | Dirty or scratched sample cuvettes; Incorrect calibration; Contaminated or expired standards. | Clean cuvettes with lint-free cloth; Replace damaged cuvettes; Recalibrate instrument before use; Check expiration dates of standards; Store standards properly to avoid contamination [4] [7]. |
| Negative Results [4] | Sample turbidity is below instrument's detection limit; Incorrect calibration range. | Verify instrument's lower detection limit; Re-calibrate using standards with concentrations appropriate for the expected sample range [4]. |
| Overloaded Samples [7] | Particle concentration exceeds instrument's measurement range; Incorrect sample dilution. | Dilute sample to fall within instrument's linear range; Follow manufacturer's dilution instructions precisely; Ensure thorough sample mixing for uniform particle dispersion [7]. |
| Calibration Problems [7] [8] | Contamination on optical surfaces; Insufficient instrument warm-up time. | Regularly clean lenses/cuvettes with manufacturer-recommended solution; Allow turbidity meter to warm up for the recommended time (e.g., 5 minutes) before use [7] [8]. |
Frequently Asked Questions
What is the difference between nephelometry and turbidimetry? Nephelometry measures the amount of light scattered by particles in a sample, typically at a 90-degree angle. It is often more sensitive for low particle concentrations. Turbidimetry, in contrast, measures the reduction in intensity of transmitted light (i.e., light that passes straight through the sample) due to scattering and absorption by particles [4] [2]. The choice depends on the sample's characteristics and the required sensitivity.
Why is kinetic solubility important in early drug discovery? Kinetic solubility refers to the concentration at which a compound precipitates out of solution in a short time frame. Testing this early in drug discovery helps identify compounds with poor solubility, which are high-risk candidates likely to fail in later development stages due to low bioavailability. High-throughput kinetic solubility screens using nephelometry can rapidly rank compounds, saving significant time and resources [2].
How do USP standards relate to turbidity and particulate matter? The United States Pharmacopeia (USP) sets strict limits on subvisible particulate matter in injectable and ophthalmic drug products to ensure patient safety. For example:
- USP <788> (Injections) limits particles to ≤6000 per container ≥10 µm and ≤600 per container ≥25 µm [5].
- USP <789> (Ophthalmic Solutions) has stricter, per-volume limits [5]. While not a compendial method, turbidity and light scattering techniques are vital orthogonal tools for monitoring and controlling these particulates during formulation and quality control [5].
What environmental factors can affect turbidity measurements? Ambient conditions can significantly impact results. Strong ambient light can interfere with the sensor's accuracy, and extreme temperature variations can affect instrument reliability and sample stability. Measurements should be performed away from direct sunlight and intense artificial lights, and instruments should be used within their specified temperature ranges [7].
Detailed Experimental Protocols
Protocol 1: Turbidimetric Measurement for Antigen Quantification
This protocol outlines a method for quantifying antigen concentration in a solution based on the formation of antigen-antibody complexes, which increase turbidity [4].
Sample Preparation
- Prepare a series of test tubes containing:
- Blank: Distilled water.
- Standard Curve: Serial dilutions of known antigen standards.
- Samples: Unknown samples to be tested.
- Add an equal volume of specific, particle-bound antibody reagent to each tube.
- Mix the contents of each tube thoroughly and incubate as required for complex formation [4].
Turbidimetry Measurement
- After incubation, analyze each mixture with a turbidimeter or a plate reader capable of measuring transmitted light.
- The level of transmitted light is inversely proportional to the amount of antigen in the solution. Higher antigen concentration leads to more complex formation, increasing turbidity and decreasing transmitted light [4].
Data Analysis
- Read the absorbance (optical density) of the standard samples.
- Plot a standard curve with antigen concentration on the x-axis and absorbance on the y-axis.
- Read the absorbance of the unknown sample tubes and use the standard curve to calculate their antigen concentrations [4].
Protocol 2: Two-Point Calibration of a Turbidity Sensor
Regular calibration is essential for accurate measurements. This is a generalized protocol based on industry practices [8].
Preparation
- Connect the turbidity sensor to the interface and allow it to warm up for at least five minutes.
- Enter the calibration mode in the data-collection software.
First Calibration Point (High Value)
- Gently invert the bottle containing the turbidity standard solution (e.g., 100 NTU) four times. Note: Do not shake, as this can introduce bubbles.
- Wipe the outside of the bottle with a clean, lint-free cloth.
- Place the bottle into the sensor, aligning any markings on the bottle with those inside the sensor chamber.
- Close the lid. Once the reading stabilizes, enter the known value of the standard (e.g., "100") and confirm/keep the value [8].
Second Calibration Point (Blank/Zero Value)
- Prepare a blank by rinsing and filling an empty sample bottle with distilled water to the fill line.
- Seal the bottle with the lid and wipe the outside clean.
- Place the blank bottle into the sensor, ensuring proper alignment.
- Close the lid. Once the reading stabilizes, enter "0" as the value and confirm/keep the value [8].
- The calibration is now complete. Subsequent sample measurements will be based on this calibration curve.
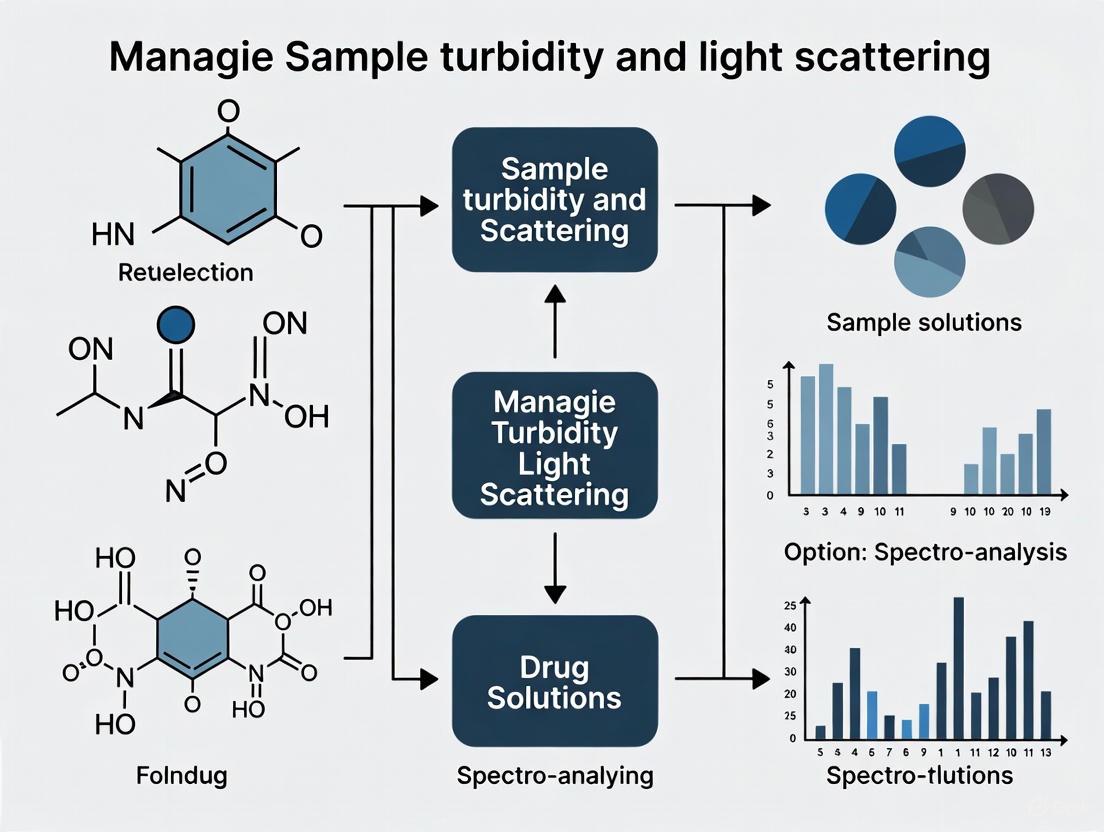
Visualizations and Workflows
Light Scattering Mechanisms
Light Scattering Measurement Principles
Turbidity Experiment Workflow
Experimental and Troubleshooting Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Function in Experiment |
|---|---|
| Turbidity Standards (e.g., Formazin) | Used to calibrate the turbidity meter, ensuring accurate and traceable measurements across different instruments and laboratories [8]. |
| Particle-Bound Antibodies | Essential for immunoturbidimetric assays. They bind to the target antigen in a sample, forming larger complexes that increase measurable turbidity [4]. |
| High-Purity Solvents & Buffers (e.g., McIlvaine buffer) | Provide a consistent and controlled chemical environment (pH, ionic strength) for solubility and particle analysis, minimizing interference from uncontrolled variables [1]. |
| Precipitation Inhibitors (e.g., specific polymers, cyclodextrins) | Excipients screened using turbidity methods to identify formulations that prevent drug precipitation, thereby maintaining supersaturation and enhancing bioavailability [1] [2]. |
| Lint-Free Wipes & Clean Cuvettes | Critical for preventing contamination from dust, fibers, or fingerprints, which are significant sources of error, especially in low-level turbidity measurements [4] [7]. |
| 1-Methyl-3-amino-4-cyanopyrazole | 1-Methyl-3-amino-4-cyanopyrazole, CAS:21230-50-2, MF:C5H6N4, MW:122.13 g/mol |
| 3,5-Dibromo-4-methoxybenzoic acid | 3,5-Dibromo-4-methoxybenzoic acid, CAS:4073-35-2, MF:C8H6Br2O3, MW:309.94 g/mol |
Turbidity, the cloudiness or haziness of a fluid caused by suspended particles, is a critical quality attribute in pharmaceutical solutions. It serves as a key indicator of product quality, safety, and stability. In drug development and manufacturing, unexpected turbidity can signal serious problems ranging from particulate contamination to chemical instability. This technical support guide addresses the common causes of turbidity—including algae, silt, clay, precipitated iron, and bacteria—within the broader context of managing sample turbidity and light scattering in pharmaceutical research.
Turbidity is quantified using Nephelometric Turbidity Units (NTU), which measure a solution's ability to scatter light [9] [10]. This light scattering occurs when suspended particles act as tiny mirrors that redirect incoming light in different directions [10]. For pharmaceutical applications, controlling turbidity is essential not only for product aesthetics but more importantly for ensuring efficacy, safety, and compliance with regulatory standards.
Fundamental Causes and Impact of Turbidity
Pharmaceutical solutions can become turbid due to various particulate contaminants, each with distinct origins and characteristics:
Bacteria and Microorganisms: Microbial growth introduces cells and cellular debris into solutions. Recent research demonstrates that bacterial activity can be detected through laser speckle imaging due to the light scattering properties of bacterial colonies [11] [12]. Certain bacteria can also cause precipitation of other dissolved components.
Inorganic Particles: Silt and clay particles may be introduced through water sources or as contaminants in raw materials. These particles typically range from 10 to 100 microns in diameter and can be identified by their mineral composition [10].
Precipitated Iron: Iron can precipitate out of solution, particularly when using iron-containing compounds like Fe(III)-EDTA or Fe(III)-citrate in formulations. Studies show that iron release rates differ between complexes, with Fe(III)-citrate releasing iron more readily than Fe(III)-EDTA, leading to potential precipitation and turbidity [13].
Algae and Organic Matter: While less common in controlled manufacturing, algal contamination can occur in water systems or from botanically-derived ingredients, introducing chlorophyll-containing cells and organic debris that scatter light [10].
Impact on Pharmaceutical Processes
Turbidity affects multiple aspects of pharmaceutical development and manufacturing:
Product Quality: Suspended particles may alter drug delivery characteristics, especially in injectable formulations where clarity is mandatory [9] [14].
Process Efficiency: High turbidity can clog filters, scale equipment, and reduce the efficiency of processing systems [9].
Analytical Interference: Turbidity interferes with light-based analytical methods, including spectrophotometry and dynamic light scattering, potentially leading to inaccurate particle size measurements [15] [14].
Troubleshooting Guides
Diagnostic Flowchart
The following diagram illustrates a systematic approach to diagnosing turbidity issues in pharmaceutical solutions:
Troubleshooting Common Scenarios
Scenario 1: Sudden Turbidity Increase Across Multiple Batches
- Problem: Multiple production batches show unexpected turbidity increases.
- Investigation Steps:
- Check water purification system performance and conductivity readings.
- Verify integrity of filters in manufacturing equipment.
- Review recent changes in raw material suppliers or specifications.
- Inspect cleaning and sterilization procedures for equipment.
- Potential Solutions:
- Replace water purification system filters and validate water quality.
- Implement additional filtration step (0.22 μm) before final packaging.
- Revise raw material acceptance criteria to include turbidity limits.
Scenario 2: Turbidity Development During Storage
- Problem: Solutions become turbid during stability studies.
- Investigation Steps:
- Conduct accelerated stability testing at different temperatures.
- Perform pH monitoring over time to detect shifts.
- Analyze particulate composition using microscopic and spectroscopic methods.
- Check container closure integrity for potential leaching.
- Potential Solutions:
- Adjust formulation pH to enhance stability.
- Add appropriate stabilizers to prevent precipitation.
- Modify packaging to prevent interaction with container.
Scenario 3: Interference with Analytical Measurements
- Problem: Turbidity interferes with Dynamic Light Scattering (DLS) measurements for nanoparticle characterization.
- Investigation Steps:
- Potential Solutions:
- Implement sample pre-filtration (0.22 μm) when appropriate.
- Use degassing procedures to remove air bubbles.
- Optimize DLS measurement parameters (duration, temperature, angle) [14].
Research Reagent Solutions for Turbidity Management
The following table summarizes key reagents and materials used in turbidity research and control:
Table: Essential Research Reagents for Turbidity Management
| Reagent/Material | Function in Turbidity Management | Application Context |
|---|---|---|
| 0.22 μm Filters | Removal of particulate contaminants | Sample preparation for DLS; solution clarification [14] |
| Citric Acid | Prevents iron precipitation through chelation | Stabilization of iron-containing formulations [16] [13] |
| EDTA | Metal chelation to prevent precipitation | Preservation of solution clarity in metal-sensitive formulations [13] |
| NaCl Solutions | Controls ionic strength in stability studies | Testing formulation robustness under different conditions [16] |
| Turbidity Standards | Instrument calibration | Ensuring measurement accuracy in quality control [7] [10] |
| Particle-bound Antibodies | Turbidimetric immunoassays | Quantification of specific analytes in solution [4] |
Experimental Protocols for Turbidity Analysis
Dynamic Light Scattering for Nanoparticle Characterization
Dynamic Light Scattering (DLS) is a laser-based method used to measure the size and distribution of particles in liquid samples by analyzing light scattered due to the Brownian motion of particles [15] [14].
Materials and Equipment:
- DLS instrument (e.g., Malvern Zetasizer)
- High-quality chemicals (ensure purity to avoid interference)
- 0.22 μm filters for sample preparation
- Clean, particle-free cuvettes
- Temperature-controlled sample chamber
Procedure:
- Sample Preparation:
Instrument Setup:
Measurement Parameters:
Data Analysis:
- Calculate Polydispersity Index (PDI): Values below 0.1 indicate monodisperse samples, while above 0.5 suggests aggregation [14].
- Report hydrodynamic diameter (Z-average) for monomodal distributions.
- For multimodal distributions, use appropriate algorithms (e.g., non-negative least squares analysis) [15].
Troubleshooting DLS Measurements:
- Unstable readings: Check for sample precipitation, settling, or air bubbles [4].
- High polydispersity: Consider additional filtration or sample purification.
- Irregular correlation functions: Verify sample concentration isn't too high, causing multiple scattering.
Turbidimetric Measurement of Particle Concentrations
Turbidimetry measures the intensity of transmitted light to determine the concentration of suspended substances [4].
Materials and Equipment:
- Turbidimeter or spectrophotometer
- Matched cuvettes
- Particle standards for calibration
- Lint-free cloth for cleaning cuvettes
Procedure:
- Instrument Calibration:
Sample Measurement:
Data Collection:
- Take multiple readings to ensure stability.
- Record values in NTU (Nephelometric Turbidity Units).
- Compare against calibration curve for quantitative analysis.
Advanced Technical FAQs
Q1: How does turbidity affect drug quality and efficacy? Turbidity directly impacts product quality and patient safety. Suspended particles can:
- Alter drug delivery characteristics and bioavailability [14]
- Cause physical instability in formulations
- Potentially harbor pathogens that are protected from disinfectants [9]
- Clog filters and delivery systems in administration devices [9]
Q2: What are the key differences between static and dynamic light scattering methods?
- Static Light Scattering analyzes time-averaged intensity of scattered light to determine molecular weight and radius of gyration [15].
- Dynamic Light Scattering analyzes intensity fluctuations caused by Brownian motion to determine hydrodynamic size and size distribution [15].
- DLS is generally faster and more sensitive to aggregation, while SLS provides more structural information [14].
Q3: How can we distinguish between biological and non-biological causes of turbidity?
- Microscopic Analysis: Direct visualization can identify cellular structures.
- Culture Methods: Biological particles will grow under appropriate conditions.
- Staining Techniques: Specific dyes can differentiate organic vs. inorganic particles.
- Spectroscopic Methods: FTIR and Raman spectroscopy identify chemical composition [12].
Q4: What preventive measures are most effective for controlling turbidity in pharmaceutical water systems?
- Regular monitoring and maintenance of water purification systems
- Proper design of distribution systems to prevent stagnation
- Effective sanitization procedures to control microbial growth
- Filtration using appropriate pore sizes (0.22 μm for bacterial removal)
- Validation of cleaning procedures for equipment and containers
Q5: How does particle composition affect light scattering measurements? Different particles scatter light differently based on:
- Refractive Index: Particles with higher refractive index differences from the medium scatter more light [15].
- Particle Size: Larger particles scatter more light at small angles, while smaller particles scatter more uniformly [10].
- Particle Shape: Non-spherical particles create asymmetric scattering patterns [15].
- Color/Pigmentation: Colored particles absorb specific wavelengths, affecting scattering measurements [10].
The following table summarizes key quantitative relationships in turbidity management:
Table: Turbidity Measurement Standards and Parameters
| Parameter | Acceptable Range | Critical Value | Measurement Context |
|---|---|---|---|
| Turbidity (NTU) | <1 NTU for purified water | >100 NTU impacts fish communities [10] | Pharmaceutical water quality [9] |
| Polydispersity Index (PDI) | 0.1-0.3 acceptable for pharmaceuticals [14] | >0.5 indicates significant aggregation [14] | DLS measurements of nanoparticle formulations [14] |
| Hydrodynamic Size | 10-100 nm ideal for bloodstream circulation [14] | >200 nm risk immune clearance [14] | Drug delivery system optimization [14] |
| Zeta Potential | ±30 mV for good electrostatic stability [16] | Near 0 mV indicates instability [16] | Colloidal stability assessment [16] |
| Iron Release Rate | 55 Mâ»Â¹dayâ»Â¹ (Fe(III)-EDTA, dark, 20°C) [13] | 11,330 Mâ»Â¹dayâ»Â¹ (Fe(III)-Cit, dark, 30°C) [13] | Tetracycline degradation studies [13] |
Light Scattering Principles Diagram
This technical support resource provides pharmaceutical researchers with comprehensive guidance for understanding, troubleshooting, and preventing turbidity issues in drug solutions. Proper management of turbidity and light scattering phenomena is essential for developing stable, effective, and safe pharmaceutical products.
The Critical Link Between Drug Solubility, Bioavailability, and Solution Clarity
Core Concepts: Understanding Turbidity, Solubility, and Bioavailability
What is the fundamental link between drug solubility, solution clarity, and bioavailability?
A drug's solubility is its ability to dissolve in a solvent, forming a clear solution. Solution clarity, often quantitatively measured as turbidity, indicates the presence of undissolved, suspended drug particles that scatter light [17]. Bioavailability is the proportion of the drug that enters circulation to exert its therapeutic effect. For a drug to be absorbed, it must first be in a dissolved state. Therefore, a cloudy, turbid solution signifies poor drug solubility, which is a primary rate-limiting step for absorption and directly leads to low bioavailability [18] [19].
Why is managing turbidity and light scattering critical in pre-formulation studies?
Managing turbidity is essential because it is a direct, measurable indicator of a drug's supersaturation and precipitation behavior [18]. During dissolution, a drug may temporarily achieve a supersaturated state (concentration higher than its equilibrium solubility) before precipitating. This precipitation, which causes a solution to become turbid, can be monitored in real-time using turbidimetry and light scattering techniques [20] [3]. Since maintaining supersaturation is key to enhancing absorption for poorly soluble drugs, these techniques are vital for screening polymers and formulations that inhibit precipitation and stabilize the drug in its dissolved state [18].
Troubleshooting Guides
Troubleshooting Guide 1: Addressing Poor Solubility and High Turbidity in Formulation
| Problem | Potential Root Cause | Recommended Solution | Key Performance Indicator (KPI) |
|---|---|---|---|
| Low Dissolution Rate & High Turbidity | High crystallinity of the Active Pharmaceutical Ingredient (API). | Implement a top-down approach like nanomilling to reduce particle size and increase surface area [19]. | Increase in dissolution rate; decrease in turbidity (NTU). |
| Poor Solubility in Biorelevant Media | Drug precipitation at different pH levels (e.g., in intestinal fluid). | Develop an amorphous solid dispersion (SD) using polymers like Soluplus or HPMCP to inhibit recrystallization [18]. | AUC (Area Under the Curve) in pharmacokinetic studies [18]. |
| Rapid Drug Precipitation | Inability to maintain supersaturation. | Use lipid-based systems (e.g., SEDDS/SMEDDS) to keep the drug solubilized in lipid droplets upon dilution [19]. | Duration of supersaturation (>2 hours) in pH-shift dissolution tests [18]. |
| Unstable Nanosuspension | Particle agglomeration over time. | Incorporate stabilizers (e.g., PVA, Parteck MXP) and consider a lipid coat for nanocrystals [18] [19]. | Particle size stability (DLS measurements) over shelf-life [3]. |
Troubleshooting Guide 2: Managing Turbidity Interference in Analytical Measurements
| Problem | Potential Root Cause | Recommended Solution | Key Performance Indicator (KPI) |
|---|---|---|---|
| Inaccurate Photometric Analysis | Light scattering by suspended particles mimics absorbance [17]. | Filter the sample using a 0.45 µm or 0.22 µm membrane, ensuring the analyte is not bound to particles [17]. | Recovery of >95% of the known analyte concentration. |
| High Background Signal | Sample turbidity interferes with the target analyte's signal. | Dilute the sample with a compatible solvent (e.g., deionized water) to reduce particle concentration [17]. | Linear response in calibration curve after dilution factor adjustment. |
| Variable Results | Particle size and distribution change over time. | Use instruments with automatic turbidity detection and correction (e.g., NANOCOLOR spectrophotometers) [17]. | Coefficient of variation (CV) of <5% in replicate measurements. |
| Difficulty in Endpoint Determination | Gradual precipitation causes continuous signal drift. | Apply dynamic light scattering (DLS) to monitor particle size changes in real-time, identifying the onset of aggregation [3]. | Clear identification of aggregation onset time. |
Frequently Asked Questions (FAQs)
FAQ 1: What is the difference between turbidimetry and nephelometry, and when should I use each?
- Turbidimetry measures the intensity of light transmitted through a sample at an angle of 0° to the incident beam. It is best for samples with moderate to high turbidity, where significant light is scattered [21] [20].
- Nephelometry measures the intensity of light scattered by the sample, typically at a 90° angle. It is more sensitive and is preferred for samples with low turbidity and small particle sizes [21] [17].
The choice depends on your sample's particle concentration and size. Nephelometry is more sensitive for dilute suspensions, while turbidimetry is more robust for concentrated ones [20].
FAQ 2: How can I quantitatively link solution turbidity to a drug's bioavailability?
Turbidity itself is an in-vitro measurement, but it correlates with bioavailability through the concept of supersaturation maintenance. You can establish a link as follows:
- Use a pH-shift dissolution test to simulate the gastrointestinal transition [18].
- Monitor turbidity (in NTU) and drug concentration simultaneously.
- Correlate the time-point of precipitation onset (sharp increase in turbidity) with the drop in dissolved drug concentration.
- In in-vivo studies, formulations that maintain a clear solution (low turbidity) for longer periods consistently show higher AUC (Area Under the Curve), indicating better bioavailability [18].
FAQ 3: Which polymers are most effective at reducing turbidity by preventing drug precipitation?
The effectiveness of a polymer depends on the drug's properties and the target absorption site. The table below summarizes high-performance polymers based on recent studies:
| Polymer | Primary Function | Key Application Context |
|---|---|---|
| Soluplus | Excellent solubilizer and crystallization inhibitor for amorphous solid dispersions [18] [19]. | Maintaining supersaturation of weakly basic drugs in intestinal fluids [19]. |
| HPMCP (HP-55) | pH-dependent polymer that dissolves in intestinal fluid and inhibits recrystallization [18]. | Targeted drug release in the intestine; protecting drugs from precipitation in gastric pH [18]. |
| PVA (Parteck MXP) | Provides good processability in Hot-Melt Extrusion (HME) and inhibits recrystallization in gastric environments [18]. | Enhancing solubility and stability of drugs in stomach fluid [18]. |
| EUDRAGIT FS 100 | Designed for colon-targeted delivery, also enhances drug solubility [19]. | Treating localized diseases of the colon while improving solubility [19]. |
FAQ 4: My formulation is a clear solution in the vial but becomes turbid upon dilution. What is happening and how can I prevent it?
This is a classic sign of solvent-mediated precipitation. The formulation is likely a co-solvent system or a lipid-based concentrate that is stable in its concentrated form. Upon dilution in aqueous media (like simulated gastric fluid), the solvent capacity drops, leading to rapid supersaturation and precipitation of the drug.
Solutions to prevent this:
- Reformulate using self-emulsifying systems (SEDDS/SMEDDS) that form a fine emulsion upon dilution, entrapping the drug in oil droplets [19].
- Incorporate precipitation inhibitors like polymers (e.g., HPMC, PVP) that interfere with the crystal nucleation and growth process [18].
Experimental Protocols & Data Presentation
Protocol 1: Formazin Turbidity Standard Preparation for Sensor Calibration
Principle: Formazin is a synthetic polymer suspension used as a primary standard for calibrating turbidimeters due to its reproducibility [21].
Materials:
- Hydrazine Sulfate (99% purity)
- Hexamethylenetetramine (99% purity)
- Distilled Water
- Volumetric Flasks (50 mL)
- Magnetic Stirrer
Methodology:
- Prepare a 4000 NTU Stock:
- Dissolve 1% w/v of hydrazine sulfate in 50 mL of distilled water.
- Dissolve 10% w/v of hexamethylenetetramine in 50 mL of distilled water.
- Mix both solutions in a single container and allow to stand for 48 hours at room temperature for complete polymerization and stabilization [21].
- Prepare Dilution Series:
- Perform serial dilutions of the 4000 NTU stock with distilled water to create a standard curve covering your expected turbidity range (e.g., 0.5 to 4000 NTU) [21].
- Calibration:
- Measure the transmitted or scattered light intensity for each standard.
- Plot the instrument response against the known NTU values to create a calibration curve.
Protocol 2: Assessing Drug Precipitation via pH-Shift Dissolution with Turbidity Measurement
Principle: This test simulates the transit of a drug from the stomach (acidic) to the intestine (neutral) and monitors the resulting precipitation via turbidity [18].
Materials:
- USP Apparatus II (Paddle)
- Dissolution tester with integrated turbidimeter or offline sampling capability
- Simulated Gastric Fluid (pH 1.2) without enzymes
- Simulated Intestinal Fluid (pH 6.8) without enzymes
- 0.45 µm Syringe Filters
Methodology:
- Gastric Phase: Place the formulation in 500 mL of Simulated Gastric Fluid at 37°C. Agitate at 50 rpm.
- Monitoring: At predetermined time points (e.g., 15, 30, 45, 60 min), withdraw samples.
- Filter a portion immediately and analyze for drug concentration via HPLC.
- Measure the turbidity (in NTU) of an unfiltered portion.
- pH-Shift Phase: After 2 hours, add a pre-warmed concentrated buffer solution to raise the medium pH to 6.8, simulating entry into the intestine.
- Intestinal Phase: Continue sampling and measuring both drug concentration and turbidity for the duration of the test (e.g., up to 6 hours).
- Data Analysis: Plot drug concentration and turbidity versus time. The point where turbidity spikes indicates precipitation, which should correspond with a drop in dissolved drug concentration.
Quantitative Data: Bioavailability Enhancement of Itraconazole Formulations
The following table summarizes pharmacokinetic data from a study on Itraconazole (ITZ), a poorly soluble drug, demonstrating how formulations that manage solubility and precipitation directly enhance bioavailability [18].
| Formulation | Description | AUC0–48h in Rats (mean ± SD) | Relative Bioavailability vs. Sporanox |
|---|---|---|---|
| Sporanox (Reference) | Marketed spray-dried formulation | 1073.9 ± 314.7 ng·h·mLâ»Â¹ | 1.0x |
| SD-1 Pellet | PVA-based, rapid release in gastric fluid [18] | 2969.7 ± 720.6 ng·h·mLâ»Â¹ | ~2.8x |
| SD-2 Pellet | HPMCP/Soluplus-based, release in intestinal fluid [18] | 7.50 ± 4.50 μg·h·mLâ»Â¹ (in dogs) | ~2.2x (vs. SD-1 in dogs) [18] |
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Soluplus | A polymer used in hot-melt extrusion to create amorphous solid dispersions, enhancing solubility and inhibiting crystallization [18] [19]. |
| HPMCP (HP-55) | A pH-dependent polymer that dissolves in the intestine, used to target drug release and inhibit precipitation in higher pH environments [18]. |
| Formazin Standard | The primary standard suspension for calibrating turbidimeters and nephelometers, ensuring accurate and reproducible turbidity measurements [21]. |
| Lipid Excipients (for SEDDS/SMEDDS) | A mixture of glycerides and surfactants that form fine oil-in-water emulsions upon gentle agitation, maintaining drug solubilization in the gut [19]. |
| Parteck MXP (PVA) | A polyvinyl alcohol polymer with excellent hot-melt extrusion processability, used to inhibit drug recrystallization in solid dispersions [18]. |
| EUDRAGIT Polymers | A family of polymers (e.g., FS 100) allowing for site-specific drug release in the GI tract, enhancing absorption where permeability is highest [19]. |
| 1-Bromopentadecane-D31 | 1-Bromopentadecane-D31, MF:C15H31Br, MW:322.50 g/mol |
| tert-Butyl (4-iodobutyl)carbamate | Tert-butyl 4-iodobutylcarbamate|CAS 262278-40-0 |
Visual Workflows and Diagrams
Diagram 1: Drug Solubility & Bioavailability Workflow
Diagram 2: Light Scattering & Turbidity Measurement
How Turbidity Shelters Pathogens and Affects Drug Safety Profiles
Turbidity, the cloudiness or haziness of a fluid caused by suspended particles, is a critical parameter in both water quality and pharmaceutical manufacturing. While often viewed as a simple aesthetic issue, elevated turbidity provides a protective shield for pathogenic microorganisms, compromising water disinfection and creating significant risks for drug safety and efficacy. In pharmaceutical research and development, unexpected turbidity in drug solutions can indicate physicochemical instability, microbial contamination, or particle aggregation that may alter drug performance. This technical support center provides targeted guidance for researchers and drug development professionals facing challenges related to sample turbidity and light scattering in their experimental workflows.
FAQs: Turbidity in Pharmaceutical Research
Q1: How does turbidity actually protect pathogens from disinfection methods? Turbidity protects pathogens through physical shielding. Suspended solid particles act as barriers that shield viruses and bacteria from disinfectants like chlorine [22]. Similarly, these suspended solids can protect microorganisms from ultraviolet (UV) sterilization by preventing the light from reaching and damaging the pathogens [22]. The higher the turbidity level, the greater the risk that pathogens may survive disinfection processes, potentially leading to gastrointestinal diseases, especially in immunocompromised individuals [22].
Q2: What level of turbidity in water is considered acceptable for pharmaceutical use? Regulatory standards for turbidity in water vary by region and application. The U.S. Environmental Protection Agency requires that public water systems using conventional or direct filtration methods must not have turbidity higher than 1.0 NTU at the plant outlet, with 95% of monthly samples not exceeding 0.3 NTU [22] [23]. The European turbidity standard is higher at 4 NTU [22]. For critical pharmaceutical applications, many utilities strive to achieve levels as low as 0.1 NTU to ensure water purity [22].
Q3: Can turbidity in drug solutions indicate product quality issues? Yes, turbidity in drug solutions can signal significant quality concerns. Microbial contamination of pharmaceuticals can lead to changes in their physicochemical characteristics, potentially altering active ingredient content or converting them to toxic products [24]. A study of nonsterile pharmaceuticals found that 50% of tested products were heavily contaminated with microorganisms including Klebsiella, Bacillus, and Candida species [24]. Such contamination not only poses infection risks but may also cause physicochemical deterioration that renders products unsafe.
Q4: What is the relationship between dynamic light scattering (DLS) measurements and turbidity? Dynamic light scattering and turbidity measurements both utilize light interaction with particles but provide different information. DLS analyzes intensity fluctuations from Brownian motion to determine hydrodynamic size of nanoparticles [25] [26], while turbidity measures light scattering and absorption to assess sample cloudiness [22]. For protein formulations and nanomedicines, an increase in turbidity often indicates aggregation that can be further characterized by DLS to determine the size distribution of the aggregates [25].
Q5: How does sample turbidity affect light scattering experiments in drug development? High turbidity can significantly complicate light scattering experiments used in drug development. In DLS, excessively turbid samples can cause multiple scattering effects where scattered light is re-scattered before detection, compromising size measurements [26]. This is particularly problematic when characterizing nanoparticle drug delivery systems where accurate size measurement (typically 10-1000 nm) is essential for predicting biodistribution and targeting efficiency [26].
Troubleshooting Guides
Guide 1: Addressing Turbidity in Water for Pharmaceutical Use
| Problem | Possible Causes | Recommended Solutions | Preventive Measures |
|---|---|---|---|
| Consistently high turbidity in source water | Surface water runoff, algal blooms, sediment disturbance | Implement pre-filtration (e.g., sand filters), adjust flocculation/coagulation processes | Regular monitoring of source water quality, watershed management |
| Turbidity spikes after filtration | Filter breakthrough, improper backwashing, membrane damage | Check filter integrity, optimize backwash cycles, replace damaged membranes | Continuous turbidity monitoring of individual filter effluents [23] |
| Variable turbidity affecting processes | Seasonal changes, storm events, upstream contamination | Use ratio turbidimeters for wide measurement range (0.1-10,000 NTU) [23] | Install multiple monitoring points (intake, pre-filtration, post-filtration) [23] |
Guide 2: Managing Turbidity in Drug Formulations and Analysis
| Problem | Impact on Research | Solution Approach | Technical Considerations |
|---|---|---|---|
| Unexpected turbidity in protein solutions | Indicates aggregation, may affect efficacy and safety | Characterize with DLS/SEC-MALS; optimize buffer conditions | For antibodies/ADCs, monitor aggregation via DLS and intrinsic fluorescence [27] |
| Turbidity interfering with analytical measurements | Compromised UV-Vis spectra, inaccurate concentration readings | Centrifugation or filtration; use alternative detection methods | For DLS, ensure sample turbidity doesn't cause multiple scattering [26] |
| Microbial contamination causing turbidity | Product spoilage, potential toxicity | Implement strict aseptic techniques; add preservatives | Study showed 50% contamination in nonsterile drugs; proper handling critical [24] |
Experimental Protocols and Data Presentation
Protocol 1: Turbidity Measurement and Pathogen Protection Assessment
Objective: Evaluate the relationship between turbidity levels and pathogen protection in pharmaceutical water systems.
Materials:
- Nephelometer or turbidimeter (calibrated with formazin standards)
- Sterile sample cuvettes
- Microfiber cloth for cleaning cuvettes
- Microbial cultures (e.g., Bacillus species)
- Chlorine-based disinfectant
- Culture media (nutrient agar, Sabouraud's dextrose agar)
Methodology:
- Calibrate turbidimeter using standard solutions per manufacturer instructions [28] [23]
- Prepare samples with varying turbidity levels (0.1, 1, 10, 100 NTU) using appropriate particles
- Inoculate samples with standardized microbial inoculum
- Apply disinfectant at specified concentrations and contact times
- Quantify surviving microorganisms using spread-plating on appropriate media [24]
- Correlate survival rates with initial turbidity levels
Table: Typical Turbidity Levels and Implications
| Turbidity Range (NTU) | Classification | Pathogen Protection Potential | Recommended Action |
|---|---|---|---|
| <0.1 | Excellent | Minimal | Suitable for critical pharmaceutical applications |
| 0.1-1.0 | Good | Low | Meets drinking water standards; acceptable for most uses |
| 1.0-10 | Moderate | Moderate | Requires filtration; investigate source |
| 10-100 | High | Significant | Unsuitable; implement treatment |
| >100 | Very High | Extensive | Reject source water; extensive treatment needed |
Protocol 2: Monitoring Drug Solution Stability via Light Scattering
Objective: Characterize nanoparticle aggregation and stability in drug formulations using dynamic light scattering.
Materials:
- Dynamic light scattering instrument (e.g., DynaPro series)
- Disposable or quartz cuvettes
- Buffer solutions for sample preparation
- Protein/nanoparticle drug formulation
- Centrifugal filters for sample clarification
Methodology:
- Sample Preparation: Clarify samples by centrifugation if necessary; adjust concentration to instrument specifications [26]
- Instrument Setup: Set temperature to 25°C (or desired condition); select appropriate measurement angle (90° or backscatter) [25]
- Data Acquisition: Perform measurements in triplicate; acquisition time typically 10-30 seconds per run [29]
- Size Analysis: Use autocorrelation function and Stokes-Einstein relationship to calculate hydrodynamic radius [26]
- Stability Assessment: Monitor changes in size distribution and polydispersity index over time or under stress conditions
Table: DLS Size Interpretation for Drug Nanoparticles
| Hydrodynamic Size Range | Polydispersity Index (PDI) | Interpretation | Formulation Implications |
|---|---|---|---|
| <10 nm | <0.1 | Monodisperse, likely monomers | Optimal for tissue penetration |
| 10-100 nm | 0.1-0.2 | Near-monodisperse | Ideal for drug delivery; avoids RES clearance [26] |
| 100-500 nm | 0.2-0.3 | Moderately polydisperse | May include some aggregates |
| >500 nm | >0.3 | Highly polydisperse, aggregated | Significant stability issues; requires reformulation |
Visualization: Turbidity and Pathogen Protection Mechanisms
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Materials for Turbidity and Light Scattering Research
| Item | Function | Application Notes |
|---|---|---|
| Formazin Standard | Primary turbidity calibration reference [23] | Provides consistent polymer size distribution; available at various NTU values |
| Nephelometer | Measures scattered light at 90° for low turbidity samples [22] [23] | Ideal for compliance monitoring; range typically 0-1000 NTU |
| Ratio Turbidimeter | Measures multiple angles for high turbidity samples [23] | Handles extreme ranges (0.1-10,000 NTU); uses transmitted and reflected light |
| Dynamic Light Scattering Instrument | Measures hydrodynamic size of nanoparticles [25] [26] | Essential for characterizing protein aggregates, liposomes, polymeric nanoparticles |
| Sterile Sample Cuvettes | Holds samples for turbidity and DLS measurements | Must be clean, scratch-free; fingerprints affect readings [28] |
| Microfiber Cloth | Cleans cuvette surfaces without scratching [28] | Critical for removing smudges that cause false high readings |
| Membrane Filters | Removes particles for sample clarification | Various pore sizes (0.22 μm for sterilization, 0.02 μm for nanoparticles) |
| Buffer Components (PBS, etc.) | Provides controlled ionic environment | Affects particle stability and aggregation; must be particle-free |
| 1,3-Dimethoxybenzene-D10 | 1,3-Dimethoxybenzene-D10, MF:C8H16O2, MW:154.27 g/mol | Chemical Reagent |
| 4E-Deacetylchromolaenide 4'-O-acetate | 4E-Deacetylchromolaenide 4'-O-acetate, MF:C22H28O7, MW:404.5 g/mol | Chemical Reagent |
Turbidity serves as both an indicator of water quality and a direct factor in compromising drug safety profiles by sheltering pathogens from disinfection methods. Through proper monitoring techniques, including nephelometry for turbidity assessment and dynamic light scattering for nanoparticle characterization, researchers can identify and mitigate risks associated with particulate contamination. The protocols and troubleshooting guides presented here provide practical approaches for maintaining sample integrity throughout pharmaceutical development processes, ultimately contributing to safer and more effective drug products.
In Dynamic Light Scattering (DLS), the path a photon takes before reaching the detector fundamentally determines the reliability of your size measurements. Single scattering occurs when a photon scatters off a single particle before being detected, providing direct information about that particle's Brownian motion. In contrast, multiple scattering happens when photons are scattered multiple times by different particles before reaching the detector, which randomizes the signal and compromises data accuracy [30] [31].
For researchers in drug development, managing this distinction is crucial when working with turbid samples like drug solutions and formulations. Multiple scattering becomes significant when sample turbidity increases, typically at high particle concentrations, leading to underestimated particle sizes and misleading conclusions about product stability and efficacy [30] [32].
Theoretical Foundations: Single vs. Multiple Scattering
The Ideal Case: Single Scattering
In a single scattering event, laser light interacts with a particle undergoing Brownian motion, scattering once, and then travels directly to the detector. The random motion of the particle causes Doppler broadening of the laser frequency, creating detectable intensity fluctuations over time [15].
These intensity fluctuations are analyzed via the autocorrelation function, which decays at a rate proportional to the particle's diffusion speed. The correlation function for a monodisperse sample in single scattering conditions follows a predictable exponential decay pattern [33] [34]:
g¹(q;τ) = exp(-Γτ)
where Γ is the decay rate, τ is the delay time, and q is the scattering vector. This relationship enables precise calculation of the hydrodynamic radius via the Stokes-Einstein equation [33] [34].
The Problem: Multiple Scattering
Multiple scattering occurs predominantly in turbid or concentrated samples where the mean free path of photons between particles is short. In this scenario, photons undergo a series of scattering events before detection, creating a composite signal that no longer accurately represents the motion of any single particle [30] [31].
Table 1: Key Differences Between Single and Multiple Scattering
| Characteristic | Single Scattering | Multiple Scattering |
|---|---|---|
| Photon Path | One scattering event before detection | Multiple scattering events before detection |
| Information Content | Direct relationship to particle diffusion | Randomized, indirect relationship to diffusion |
| Apparent Size | Accurate hydrodynamic radius | Artificially smaller sizes |
| Sample Concentration | Dilute, transparent samples | Concentrated, turbid samples |
| Correlation Function | High intercept, clear decay | Reduced intercept, faster decay |
| Polydispersity | Accurate representation | Artificially broadened |
The following diagram illustrates the fundamental differences in photon paths between single and multiple scattering scenarios:
Multiple scattering increases the randomness of the scattering signal, decreasing the correlation and making particles appear to move faster than they actually are. The net result is that DLS size measurements in the presence of multiple scattering are biased toward smaller sizes [30].
Troubleshooting Guide: Identifying Multiple Scattering
Key Symptoms of Multiple Scattering
Researchers should be alert to these telltale signs of multiple scattering in their DLS data:
Concentration-Dependent Sizing: Apparent particle size decreases systematically with increasing sample concentration [30] [32].
Reduced Correlation Function Intercept: The measured intercept (amplitude) of the correlation function decreases at higher concentrations [30].
Increased Apparent Polydispersity: The size distribution appears broader than expected, with the width increasing with concentration [30].
Unphysical Results: Size measurements that contradict other characterization methods or known sample properties [32].
Table 2: Quantitative Symptoms of Multiple Scattering in a 200 nm Polystyrene Standard
| Concentration | Apparent Size (nm) | Correlation Intercept | Polydispersity |
|---|---|---|---|
| Dilute | 200 | 0.95 | 0.02 |
| Moderate | 185 | 0.85 | 0.08 |
| High | 160 | 0.70 | 0.15 |
| Very High | 135 | 0.55 | 0.25 |
Data adapted from Malvern Panalytical technical documentation [30].
Experimental Protocols for Detection
Protocol 1: Concentration Series Test
- Prepare a series of dilutions from your stock sample
- Measure each concentration using the same DLS settings
- Plot apparent size and correlation function intercept against concentration
- Interpretation: A significant decrease in either parameter indicates multiple scattering becoming dominant [30]
Protocol 2: Path Length Dependence
- Use an instrument with variable measurement position capability
- Measure the same sample at different path lengths from the cuvette wall
- Compare the apparent sizes obtained
- Interpretation: Significant differences indicate multiple scattering effects [30]
Solutions and Mitigation Strategies
Sample Preparation Approaches
Optimal Dilution: The most straightforward approach is diluting the sample until the measured size becomes concentration-independent. This establishes the optimal concentration range for accurate DLS analysis [30] [32].
Sample Clarification: Remove dust and aggregates through centrifugation or filtration. For proteins, consider centrifugation at 10,000-15,000 × g for 10-30 minutes before measurement [33] [15].
Solvent Matching: For nanoparticle dispersions, ensure the dispersant has similar refractive index to the particles where possible, though this must be balanced with maintaining colloidal stability [35].
Instrumental Solutions
Backscatter Detection (NIBS): Non-Invasive Back Scatter technology measures at an angle of 173° and automatically positions the measurement point within the sample. This minimizes the path length that scattered light travels through the sample, reducing the probability of multiple scattering [30].
Cross-Correlation Techniques: 3D-dynamic light scattering methods use two beams and detectors to isolate singly scattered light by cross-correlation, effectively suppressing contributions from multiple scattering [33].
Low-Angle Measurements: For some samples, particularly those containing large aggregates, measurements at lower angles (as low as 15°) can provide better characterization, though these require specialized instrumentation [33] [32].
Table 3: Instrument Configuration Guide for Turbid Samples
| Sample Type | Recommended Angle | Optical Configuration | Rationale |
|---|---|---|---|
| Transparent, small particles | 90° | Side scattering | Maximizes signal for weakly scattering samples |
| Moderately concentrated | 173° | Backscatter (NIBS) | Reduces path length, minimizes multiple scattering |
| Highly concentrated, opaque | 173° with adjusted position | Backscatter with reduced path length | Further minimizes multiple scattering effects |
| Samples with large aggregates | 13-15° | Forward scattering | Enhances sensitivity to large particles |
Alternative Techniques for Highly Turbid Samples
When multiple scattering cannot be sufficiently suppressed in DLS, consider these alternative approaches:
Diffusing-Wave Spectroscopy (DWS): A specialized technique for strongly scattering media that explicitly accounts for multiple scattering, though it requires different theoretical analysis [33].
Nephelometry: Measures scattered light intensity at specific angles, useful for aggregation studies and solubility screening in drug development [36].
Asymmetrical Flow Field-Flow Fractionation (AF4): Separates particles by size before detection, allowing analysis of complex mixtures and overcoming some limitations of batch DLS [35].
FAQs: Addressing Common Researcher Concerns
Q1: My drug formulation is turbid due to high concentration. How can I obtain accurate DLS data? A: Implement a backscatter (NIBS) detection system if available, as it can measure much higher concentrations than conventional 90° systems. Alternatively, use the concentration series approach to identify the maximum concentration where sizing remains consistent, then report this diluted size with appropriate caveats [30].
Q2: How does multiple scattering lead to artificially small sizes? A: Multiple scattering increases the randomness of photon arrival times at the detector, making the intensity fluctuations appear faster. Since faster fluctuations are interpreted as faster diffusion (and thus smaller size), the apparent hydrodynamic radius is underestimated [30] [31].
Q3: Are single-angle DLS instruments suitable for characterizing nanoparticles for drug delivery? A: Single-angle instruments at large angles (90° or 173°) have limitations for precise size determination, particularly for non-spherical particles or complex mixtures. Their results should be interpreted with caution, and multiangle DLS is recommended for rigorous characterization, especially when correlating size with biological behavior [32].
Q4: What concentration range typically avoids multiple scattering issues? A: The optimal concentration depends on particle size and optical properties. As a general guideline, the sample should be sufficiently transparent that you can clearly read text through a standard cuvette filled with the sample. Empirically, perform a dilution series to identify where measured size becomes concentration-independent [30] [32].
Q5: How does serum protein binding affect DLS measurements of nanomedicines? A: Serum proteins form a "corona" around nanoparticles, increasing their apparent size and potentially causing aggregation. This represents a real physicochemical change rather than an artifact, but requires careful interpretation since the measured size now includes both the nanoparticle and its protein corona [32].
Essential Research Reagent Solutions
Table 4: Key Materials for Reliable DLS Analysis
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Size Standards | Verification of instrument performance and methodology | Use NIST-traceable nanosphere standards (e.g., 100 nm polystyrene) |
| Syringe Filters | Sample clarification | 0.02-0.45 μm pore size, compatible with sample solvent |
| Ultrapure Salts | Control ionic strength | For buffer preparation to maintain colloidal stability |
| Refractometer | Measure solvent refractive index | Critical for accurate size calculation via Stokes-Einstein equation |
| Quality Cuvettes | Sample containment | Optically clear, chemically clean, appropriate path length |
Understanding and managing multiple scattering effects is fundamental to obtaining accurate DLS data, particularly in pharmaceutical research where samples often include turbid drug formulations and complex biological media. By recognizing the symptoms of multiple scattering and implementing appropriate mitigation strategies—whether through sample preparation, instrumental configuration, or alternative techniques—researchers can ensure their size measurements reliably reflect true particle characteristics rather than optical artifacts.
The key principles are to validate your methodology with concentration series, utilize appropriate detection geometry for your sample type, and interpret DLS data with awareness of its limitations in complex, concentrated systems. With these approaches, DLS remains an invaluable tool for characterizing drug delivery systems and biopharmaceuticals across the development pipeline.
In drug development and research, managing sample turbidity is a critical parameter for ensuring product quality, safety, and efficacy. Turbidity, the cloudiness or haziness of a fluid caused by suspended particles, serves as a key indicator in various biopharmaceutical processes. It can signal the presence of unwanted particulates, inform on cell density in bioreactors, or affect the analysis of drug solutions themselves. This technical support guide focuses on the precise measurement of turbidity, specifically explaining the two predominant units—NTU and FNU—their appropriate applications, and troubleshooting common issues encountered by researchers and scientists. Understanding these concepts is fundamental for maintaining rigorous standards in pharmaceutical manufacturing and research, where the accurate quantification of suspended matter can directly impact product stability, sterility, and final release.
Understanding Turbidity Units: NTU vs. FNU
Turbidity is quantified using standardized units, with Nephelometric Turbidity Units (NTU) and Formazin Nephelometric Units (FNU) being the most prevalent in scientific and industrial applications. Both units are calibrated using the same primary standard, Formazin, and both measure the intensity of light scattered at a 90-degree angle from the incident beam, a method known as nephelometry [37] [38]. Despite these similarities, the crucial difference lies in the instrumentation and the underlying regulatory standards they comply with.
The table below provides a clear comparison of these two units:
Table: Key Differences Between NTU and FNU
| Feature | NTU (Nephelometric Turbidity Unit) | FNU (Formazin Nephelometric Unit) |
|---|---|---|
| Definition | Measures scattered light at a 90-degree angle | Measures scattered light at a 90-degree angle |
| Light Source | White light (visible spectrum, 400-600 nm) [37] | Infrared light (860 nm) [37] |
| Governing Standard | US EPA Method 180.1 [37] [38] | ISO 7027 (European standard) [37] [38] |
| Primary Application | Common in drinking water and wastewater treatment under US regulations; used in various industrial and research settings [38]. | Preferred in European markets and for applications requiring compliance with ISO standards; ideal for colored samples [37] [38]. |
| Key Advantage | Well-established protocol in the US. | Infrared light minimizes color interference, providing more reliable readings for colored samples [38]. |
For most practical purposes, 1 NTU is considered equivalent to 1 FNU on a Formazin standard scale [39]. However, it is critical to understand that measurements taken on the same sample with different light sources (white vs. infrared) may yield different values due to the varied interaction of light with particle size and color [37]. This distinction is vital for data comparison and regulatory reporting.
Other units you may encounter include:
- FTU (Formazin Turbidity Unit): A generic unit that does not specify the measurement method [38] [39].
- FAU (Formazin Attenuation Unit): Measures the reduction (attenuation) of transmitted light at 180 degrees and is not recognized by most regulatory agencies for compliance turbidity measurement [37] [38].
- JTU (Jackson Turbidity Units): An outdated, visual method that is no longer in common use [38].
Visualizing Turbidity Measurement Principles
The following diagram illustrates the core principles of nephelometric turbidity measurement and the key difference between NTU and FNU.
Troubleshooting Common Turbidity Meter Issues
Accurate turbidity measurement is sensitive to technique and instrument status. The following guide addresses common problems, their causes, and solutions relevant to a research environment.
Table: Turbidity Meter Troubleshooting Guide
| Problem | Possible Causes | Solutions & Preventive Actions |
|---|---|---|
| Inaccurate/ High or Low Values | 1. Contaminated optics: Dust, fingerprints, or dried residue on vial or lens [7] [4].2. Improper calibration: Out-of-date standards, incorrect procedure, or contaminated standards [7].3. Scratched or faulty cuvette: Scratches can scatter light [7] [4]. | • Clean optical surfaces and vials with lint-free cloth and recommended solution [7].• Follow manufacturer's calibration procedure precisely using fresh, certified standards [7] [40].• Inspect and replace damaged cuvettes [7]. |
| Unstable/ Erratic Readings | 1. Settling or sedimentation: Particles settling during measurement [41].2. Air bubbles (microscopic): Tiny bubbles scatter light [7] [41] [4].3. Insufficient warm-up time: Electronics or lamp not stable [7]. | • Ensure homogeneous sample mixing before measurement [7].• Allow sample to decant after mixing to let bubbles rise; handle gently to avoid introducing bubbles [7].• Use the meter's signal-averaging function (e.g., 5-10 measurements) [41].• Allow instrument to warm up for the recommended time [7]. |
| Negative Results | 1. Sample clearer than blank: Sample turbidity is at or below the instrument's blank reference [41].2. Incorrect blanking: Meter was accidentally blanked on a turbid standard [41]. | • Verify sample is expected to be more turbid than the blank.• Restore factory calibration settings and re-perform blanking with a true 0 NTU standard [41]. |
| Calibration Errors | 1. Standard out of tolerance: Reading deviates too far from expected value (e.g., >50%) [41].2. Using a zero sample to calibrate: Attempting to use the blank for calibration instead of only for setting the blank reference [41]. | • Use fresh, in-date calibration standards. Ensure standards match the instrument's requirements [7] [41].• Blank the meter with a 0 NTU standard, then calibrate with an appropriate non-zero standard (e.g., 1.0, 10 NTU) [41]. |
| Power/ Electronic Issues | 1. Low or faulty battery: Inconsistent power leads to unreliable operation [7] [41].2. Loose connections: Cables or battery not secure [7]. | • Use high-quality, brand-name alkaline batteries or operate with an AC adapter [41].• Check and secure all electrical connections [7]. |
Frequently Asked Questions (FAQs)
Q1: What is the correlation between turbidity (NTU/FNU) and suspended solids (mg/L)? While the relationship is empirical and sample-specific, a rough correlation exists: 1 mg/L of suspended solids is approximately equal to 3 NTU [38]. However, this factor can vary significantly depending on the size, shape, and refractive index of the particles, so site-specific calibration is recommended for precise work.
Q2: My turbidimeter displays an "Err 2" message. What does this mean? An "Err 2" typically indicates a calibration error where the reading of the standard solution deviates by more than the allowable range (often more than 50%) from its stated value [41]. This is usually caused by using expired or inappropriate standard solutions, or a problem with the initial blanking step. Check the standard's shelf life, reset the meter to factory calibration, and ensure proper blanking [41].
Q3: Why should I use an infrared (FNU) meter for my drug solution samples? Infrared light (as used in FNU meters per ISO 7027) is less susceptible to interference from the color of a sample [37] [38]. If your drug solutions have any intrinsic color, using an FNU-compliant instrument can provide more accurate turbidity readings by minimizing this color-induced error.
Q4: How often should I calibrate my turbidity meter? For research-grade accuracy, calibrate your meter before each use or at least at the beginning of each analytical session [4]. Always recalibrate if you change the measurement range, when using a new batch of standards, or if you suspect the results are inaccurate [7] [40].
Q5: Are there any safety concerns with turbidity calibration standards? Yes, the primary standard, Formazin, is traditionally made from hydrazine sulfate, a carcinogenic substance [42]. For safety, many commercial suppliers offer ready-made, stable Formazin solutions or safer, polymer-based surrogate standards that are certified to be equivalent. Always check the Material Safety Data Sheet (MSDS) and handle all standards with appropriate laboratory safety practices.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table lists key materials and reagents essential for performing accurate turbidity measurements in a research and development context.
Table: Essential Reagents and Materials for Turbidity Analysis
| Item | Function & Application |
|---|---|
| Formazin Standards | Primary reference material for calibrating turbidity meters across all scales (NTU, FNU, etc.) [38] [42]. Available in various concentrations (e.g., 0.1, 1, 10, 100, 1000 NTU). |
| Deionized/Distilled Water | Used for preparing blank (0.00 NTU) standards, diluting samples, and rinsing cuvettes to prevent contamination [4]. |
| Particle-Bound Antibodies | Critical reagent in immunoturbidimetric assays, where antigen-antibody complex formation increases turbidity for quantitative analysis of specific proteins or biomarkers [4]. |
| Reaction Buffer | Provides the optimal pH and ionic strength environment for consistent and reproducible reaction conditions, particularly in kinetic or biochemical turbidimetry [4]. |
| Antigen Standards | Used in immunoturbidimetry to create a standard curve for determining the concentration of an unknown antigen in a sample [4]. |
| Lint-Free Wipes | Essential for properly cleaning the external surfaces of sample cuvettes without introducing scratches or fibers that can scatter light and cause errors [7] [41]. |
| Certified Cuvettes | Specially designed vials that ensure consistent optical path length and clarity. Using scratched or non-certified cuvettes can lead to significant measurement inaccuracies [7]. |
| Disialyloctasaccharide | Disialyloctasaccharide, CAS:58902-60-6, MF:C76H125N5O57, MW:2020.8 g/mol |
| 6-Bromo-2-chloroquinolin-4-amine | 6-Bromo-2-chloroquinolin-4-amine, CAS:1256834-38-4, MF:C9H6BrClN2, MW:257.51 g/mol |
Analytical Techniques and Practical Applications: DLS, Nephelometry, and Sample Preparation
Why Turbidity Challenges DLS Measurements
In DLS, the fundamental theory assumes a single scattering event: a photon hits a particle, scatters once, and is detected [43]. Turbid samples, with their high concentration of particles or strongly scattering particles, violate this assumption. Here, photons are likely to be scattered multiple times before being detected—a phenomenon known as multiple scattering [43] [44].
Multiple scattering corrupts the core measurement because the detected fluctuation signal no longer corresponds to the true, fast Brownian motion of a single particle. Instead, it reflects a slower, composite motion, leading to the calculation of an apparently smaller particle size and unreliable data [44].
Methodologies for Reliable DLS in Turbid Samples
Several advanced methodologies have been developed to overcome the challenge of multiple scattering.
Technical Instrument Solutions
Modern DLS instruments incorporate hardware and optical configurations to physically minimize multiple scattering.
| Solution | Principle | Key Benefit |
|---|---|---|
| Backscattering Detection (173°-175°) [45] [43] | Detects scattered light at a near-180° angle, placing the scattering volume close to the cuvette wall. | Drastically reduces the photon path length in the sample, minimizing chances for multiple scattering. Ideal for concentrated/turbid samples [45]. |
| Adjustable Laser Focus Position [45] [43] | The instrument shifts the laser's focus point closer to the inner wall of the cuvette. | Further shortens the light path within the sample, enhancing the effectiveness of backscattering measurements [43]. |
| Automatic Angle & Position Selection [45] [43] | The instrument measures transmittance and other parameters to automatically select the optimal detection angle and focus position. | Removes user guesswork, ensuring the best possible configuration for a given sample's turbidity [43]. |
| Specialized Advanced Techniques [44] | Uses two independent laser beams detecting the same scattering volume and cross-correlates the signals. | Physically suppresses the contribution of multiple scattering to the correlation function, as these events are uncorrelated between the two beams [44]. |
Sample Preparation and Measurement Protocol
Proper sample handling is crucial for obtaining meaningful data from turbid samples.
- Sample Viscosity: Ensure the sample viscosity does not exceed 10 cP for reliable analysis [46].
- System Suitability: Use a monodisperse, standard reference material (e.g., 200 nm polystyrene latex spheres) at a comparable concentration to your sample to verify instrument performance under turbid conditions [44].
- Data Quality Verification: Before starting the actual measurement, use the instrument's live view to check the intensity trace and correlation function.
- The intensity trace should show regular fluctuations. Sharp spikes may indicate dust, while a steady ramp up or down can signal aggregation or sedimentation [45].
- The correlation function should be smooth with a single exponential decay. A non-linear baseline or "bumps" suggest the presence of large contaminants or aggregates [45].
The following workflow summarizes the key decision points for analyzing a turbid sample via DLS:
Researcher's Toolkit: Essential Reagents and Materials
The table below lists key materials required for DLS analysis of turbid samples.
| Item | Function | Specification Guidelines |
|---|---|---|
| Standard Cuvettes | Holds the liquid sample for measurement. | Standard square or cylindrical cells for clear to moderately turbid samples. |
| High-Concentration Cuvettes | Holds the liquid sample for measurement. | Specialized cells (e.g., ultra-thin flat cells) with reduced path lengths (e.g., 10 µm to 1 mm) to minimize multiple scattering [44]. |
| Size Reference Standards | Validates instrument performance and method accuracy under turbid conditions. | Monodisperse polystyrene latex spheres (e.g., 200 nm nominal diameter) [44]. |
| Filtration/Syringe Filters | Removes dust and large aggregates from solvents and samples. | Use appropriate pore sizes (e.g., 0.1 µm or 0.22 µm) before loading samples into cuvettes [47]. |
| Viscosity Standard | Verifies accurate viscosity input for the Stokes-Einstein equation. | Certified oil or solvent with known viscosity at the measurement temperature. |
| Methylcobalamin hydrate | Methylcobalamin hydrate, MF:C63H93CoN13O15P, MW:1362.4 g/mol | Chemical Reagent |
| 5-Methyl-2-thiouridine | 5-Methyl-2-thiouridine, CAS:32738-09-3, MF:C10H14N2O5S, MW:274.30 g/mol | Chemical Reagent |
Frequently Asked Questions (FAQs)
Q1: Can DLS be used for turbid samples at all? Yes, this is a common misconception. While standard DLS setups may struggle, modern instruments with backscattering detection (175°), adjustable laser focus, and automatic angle selection are specifically designed to provide reliable data for turbid samples [45] [43].
Q2: My DLS results for a turbid sample show a smaller size than expected. What is the likely cause? This is a classic signature of multiple scattering. When photons are scattered multiple times, the detected motion appears slower, and the correlation function decays faster, leading to an underestimation of the true particle size [44]. Switching to a backscattering geometry is the primary solution.
Q3: How does sample concentration affect my DLS measurement? Finding the right concentration is critical. Excessively high concentrations cause multiple scattering, distorting results [47]. Conversely, overly dilute samples may not scatter enough light, leading to a poor signal-to-noise ratio [45] [47]. The optimal concentration provides a strong signal without causing multiple scattering.
Q4: What are the key indicators of good data quality in a DLS measurement for a turbid sample? Monitor the correlation function: it should be smooth with a single exponential decay and a stable, linear baseline. Also, observe the intensity trace: it should show regular fluctuations without sharp spikes (dust) or steady ramping (sedimentation/aggregation) [45]. A high intercept value in the correlation function also indicates good signal quality [48].
Q5: Are there alternatives to standard DLS for highly turbid samples? Yes, advanced techniques exist. 3D Dynamic Light Scattering (3D-DLS) uses cross-correlation of two laser beams to suppress signals from multiple scattering physically [44]. Diffusing Wave Spectroscopy (DWS) leverages multiple scattering but requires a different theoretical model and is less sensitive to particle size distribution [44].
Dynamic Light Scattering (DLS) is a cornerstone technique for determining the size distribution of nanoparticles in suspension. For researchers in drug development, analyzing turbid or highly concentrated samples—common in lipid nanoparticle or protein formulation workflows—presents a significant challenge due to the phenomenon of multiple scattering, where photons are scattered by more than one particle before detection. This scrambles the signal and makes accurate size determination difficult. Utilizing a back-scattering detection angle, typically at 175°, provides an effective solution to this problem by minimizing the path length of the laser light within the sample, thereby substantially reducing multiple scattering events. This configuration is indispensable for obtaining reliable data from challenging, yet industrially relevant, biopharmaceutical samples.
Core Principles and Advantages of the 175° Angle
How Back-Scattering Minimizes Multiple Scattering
In a standard DLS setup, a laser is directed into a sample, and the scattered light is detected at a specific angle. The core principle of back-scattering detection lies in the strategic placement of the scattering volume. When the detector is positioned at 175°, the overlap between the incident laser beam and the detected scattered light occurs very close to the front wall of the cuvette. This configuration results in a very short path length for the laser light within the sample [45].
This short path is crucial because it drastically reduces the probability that a single photon will be scattered by multiple particles on its journey. In highly turbid samples, a longer path length (as encountered in a 90° side-scattering geometry) makes multiple scattering inevitable. By minimizing these events, back-scattering ensures that the detected fluctuations in light intensity are predominantly caused by Brownian motion of single particles, leading to a more accurate autocorrelation function and, consequently, a more reliable particle size distribution [45] [33]. For larger particles and those with a high refractive index contrast, this limits the technique to very low particle concentrations without a cross-correlation or back-scattering approach [33].
Operational Advantages for Drug Solution Research
The primary advantage of this configuration is the ability to analyze samples that would otherwise be inaccessible to conventional DLS. This directly enhances efficiency in drug development pipelines by minimizing the need for sample dilution, which can alter the state of the particles and provide unrepresentative results [49].
Key benefits include:
- Measurement of Concentrated Formulations: Enables direct sizing in liposomal, polymeric nanoparticle, and protein suspension formulations at their processing concentrations [49].
- Improved Data Quality: Provides a cleaner signal from turbid samples by suppressing the noise introduced by multiple scattering [45] [33].
- Monitoring of Process Streams: Facilitates inline monitoring during manufacturing, a key principle of Quality by Design (QbD), as the configuration is less affected by the high particle load of process streams [49].
The following diagram illustrates the optical path and the key advantage of the 175° back-scattering configuration.
Schematic of DLS Back-Scattering Detection at 175°
Technical Specifications and Configuration
Comparing DLS Detection Angles
Modern DLS instruments often provide multiple detection angles to accommodate samples with different properties. The choice between forward (e.g., 15°), side (90°), and back (175°) scattering depends on the sample's turbidity and particle size. The table below summarizes the optimal applications for each key angle.
Table 1: Comparison of DLS Detection Angles
| Detection Angle | Common Instrument Implementations | Optimal Sample Type | Key Advantage |
|---|---|---|---|
| Back-Scattering (175°) | Litesizer 500, ZetaStar, Mobius | Highly turbid, concentrated suspensions (e.g., liposomes, LNPs) | Minimizes multiple scattering; short laser path length [45] [25] [33] |
| Side-Scattering (90°) | DynaPro NanoStar | Weakly scattering, small particles (e.g., proteins), transparent samples | Provides a clean signal; less sensitive to dirt on cuvette walls [45] [33] |
| Forward-Scattering (15°) | Litesizer 500 | Samples with a few large particles or aggregates | Emphasizes large particles which scatter more light forward [45] [33] |
Key Research Reagent Solutions
Successful DLS analysis, especially with advanced configurations, relies on the use of appropriate consumables and reagents. The following table details essential items for your research toolkit.
Table 2: Essential Research Reagent Solutions for DLS
| Item | Function in DLS Experiment |
|---|---|
| Standardized Buffer Systems (e.g., PBS) | Provides a known viscosity and refractive index, which are critical input parameters for the Stokes-Einstein equation [25]. |
| Disposable or Quartz Cuvettes | Holds the sample. Disposable cuvettes prevent cross-contamination; quartz offers superior optical clarity for low-volume measurements [25]. |
| Inline Flow Cell | Enables continuous, inline monitoring of particle size during manufacturing processes, aligning with PAT for QbD [49]. |
| Solvent Library / Refractometer | A built-in solvent library (e.g., in DYNAMICS software) or a physical refractometer provides accurate solvent refractive index values, which are crucial for size calculation, especially for particles >100 nm [25] [33]. |
Troubleshooting Guide and FAQs
Q: My highly concentrated liposome sample still shows a noisy correlation function and unreliable size data, even at 175°. What should I check? A: First, verify that the instrument's laser attenuation is correctly set. For turbid samples, the laser light often needs to be attenuated to prevent the detector from being overwhelmed by scattered photons [45]. Second, ensure the sample is not sedimenting; a steady decrease in the intensity trace can indicate sedimentation, which invalidates the assumption of Brownian motion [45]. Finally, check the instrument's baseline and intercept of the correlation function; a non-linear baseline or low intercept can indicate poor signal-to-noise, potentially from dust contamination or an insufficiently concentrated sample [45].
Q: When should I use a 175° angle versus a 90° angle for my protein formulations? A: For clear, monodisperse protein solutions at low to moderate concentrations, the 90° side-scattering angle is often ideal as it provides a clean signal with high sensitivity to small particles [45] [33]. You should switch to the 175° back-scattering angle when the sample becomes turbid due to high protein concentration (>100 mg/mL), the presence of aggregates, or when formulating with excipients that increase sample opacity [49] [33]. Some advanced instruments can automatically select the best angle based on a continuous transmittance measurement [45] [33].
Q: Can I use the 175° back-scattering configuration for inline process monitoring? A: Yes. The 175° configuration is particularly well-suited for inline monitoring because it is robust against the high particle concentrations often found in process streams. For example, the NanoFlowSizer (NFS) systems utilize spatially resolved DLS and can perform real-time sizing in flow cells, successfully monitoring liposome formulations even at significant flow rates [49]. The short path length is key to handling these challenging conditions without dilution.
Q: The particle size I obtained from DLS at 175° is larger than what I see with electron microscopy. Is this an error? A: Not necessarily. This is a fundamental aspect of the DLS technique. DLS measures the hydrodynamic radius, which includes the core particle and any solvent layers, surfactants, or polymers attached to its surface that move with the particle in solution [45] [33]. Transmission electron microscopy (TEM), on the other hand, measures the core particle's physical dimensions and does not visualize bound solvent or soft layers due to poor contrast. Therefore, for a colloidal gold particle with a surfactant coating, DLS will rightly report a larger size than TEM [33].
Detailed Experimental Protocol for Sizing Liposomes at 175°
This protocol outlines the steps for characterizing the hydrodynamic diameter and polydispersity index (PDI) of a concentrated liposome formulation using back-scattering DLS.
Objective: To determine the size distribution of a turbid liposome suspension at its manufacturing concentration without dilution. Sample: Liposome suspension (e.g., 2.84 mg/mL lipid concentration in water) [49].
Procedure:
Sample Preparation:
- Centrifuge the liposome sample briefly (e.g., 5-10 minutes at a low g-force) to remove any large dust particles or air bubbles that could interfere with the scattering signal. Avoid aggressive centrifugation that may pellet the liposomes.
- Gently mix the sample to ensure homogeneity before loading.
Instrument Setup:
- Turn on the DLS instrument and laser, allowing sufficient time for stabilization (typically 15-30 minutes).
- On the instrument software, select the back-scattering detection angle (175°).
- Set the measurement temperature to 25°C (or as required by your protocol). Accurate temperature control is critical as it directly impacts solvent viscosity [15] [25].
- In the software parameters, input the dispersant properties: Viscosity (0.887 cP for water at 25°C) and Refractive Index (1.330 for water at 25°C). Use the instrument's solvent library if available [25].
Loading the Sample:
- Carefully transfer an appropriate volume of the liposome suspension (e.g., 50-100 µL, depending on the cuvette) into a clean, disposable cuvette or a flow cell.
- Seal the cuvette with a cap to prevent evaporation and avoid introducing air bubbles.
- Place the cuvette into the instrument's sample chamber and allow it to thermally equilibrate for 2-5 minutes.
Data Acquisition:
- Initiate the measurement. The instrument will automatically adjust the laser attenuator to achieve an optimal, processable scattered light intensity [45].
- Monitor the live intensity trace and autocorrelation function. For a good measurement, the intensity trace should show random fluctuations, and the correlation function should be smooth with a single exponential decay [45].
- Accumulate data for a duration sufficient to achieve a stable correlation function, typically 5-10 consecutive runs of 10 seconds each.
Data Analysis:
- The software will automatically fit the autocorrelation function using an algorithm (e.g., cumulant method) to extract the translational diffusion coefficient.
- Using the Stokes-Einstein equation, the software will calculate the Z-average hydrodynamic diameter (the intensity-weighted mean size) and the Polydispersity Index (PDI).
- Examine the intensity-weighted size distribution plot. A monodisperse sample will show a single, sharp peak.
- Record the Z-average diameter and PDI. A PDI value below 0.1 is generally indicative of a monodisperse sample, while a higher PDI suggests a broad distribution or multiple populations [45].
Troubleshooting Note: If the correlation function appears noisy or the baseline is unstable, ensure the sample is free of dust and check that the laser power is optimally attenuated. For formulations with very high polydispersity, more advanced analysis algorithms (e.g., non-negative least squares) may be required to resolve different particle populations.
Nephelometry as a High-Throughput Tool for Kinetic Solubility Screening
Key Experimental Protocol: High-Throughput Kinetic Turbidity Assay
This protocol enables the measurement of apparent amorphous solubility and the distinction between amorphous precipitation and crystallization for drug candidates [50].
Materials and Reagents
- Model Compounds: Small molecule drug candidates with at least 98% purity.
- Buffers: Standard aqueous buffers (e.g., phosphate-buffered saline); fasted state simulated intestinal fluid (FaSSIF-V2) can be used for biorelevant conditions [50].
- Polymer Excipients: Hydroxypropyl methylcellulose acetate succinate (HPMC-AS), poly(vinylpyrrolidone-co-vinyl acetate) (PVP-VA64) [50].
- Solvent: Dimethyl sulfoxide (DMSO) for compound stock solutions.
Equipment
- UV-Vis Plate Reader: Capable of kinetic readings, ideally with temperature control.
- Robotic Liquid Handler: For automated sample preparation in 96-well or 384-well plates.
- Microplates: Clear-bottomed, 96-well plates.
Step-by-Step Methodology
- Sample Preparation: A robotic liquid handler prepares a dilution series of the drug candidate in DMSO, which is then spiked into the aqueous buffer of choice. A typical final DMSO concentration should be ≤1% (v/v) to minimize cosolvent effects [50].
- Excipient Screening (Optional): Different polymer excipients at varying concentrations can be added to designated wells to screen for their impact on inhibiting crystallization.
- Kinetic Measurement: The plate is transferred to a UV-Vis plate reader, and turbidity is monitored kinetically at one or more wavelengths (e.g., 400-600 nm) over a defined period (e.g., 60-90 minutes) [50].
- Data Analysis: The time-course turbidity profiles are analyzed. The point where the signal deviates from the baseline is identified as the amorphous solubility. Different kinetic profiles (e.g., immediate precipitation vs. slow increase in turbidity) help distinguish between amorphous and crystalline precipitation [50].
Research Reagent Solutions
The following table details key reagents used in nephelometry and turbidity-based solubility assays.
| Reagent / Material | Function / Explanation |
|---|---|
| HPMC-AS (e.g., MF grade) | A polymer excipient used in amorphous solid dispersions to inhibit crystallization and maintain drug supersaturation [50]. |
| PVP-VA64 | A polymer excipient that helps stabilize supersaturated drug solutions and reduce the risk of crystalline precipitation [50]. |
| FaSSIF-V2 | Biorelevant medium that simulates the intestinal environment, providing physiologically relevant solubility and precipitation data [50]. |
| Diatomaceous Earth (DE) | A porous filter aid used in depth filtration to increase surface area and trap particles, improving clarification efficiency [51]. |
| Natural Coagulants (e.g., Moringa oleifera) | Used in water treatment to aggregate particles and reduce turbidity, demonstrating the principle of flocculation [52]. |
Data Presentation: Turbidity and Solubility Parameters
Table 1: Interpretation of Kinetic Turbidity Profiles
| Turbidity Profile | Phenomenon Indicated | Formulation Implication |
|---|---|---|
| Immediate, stable signal | Amorphous precipitation (Liquid-Liquid Phase Separation) | High risk of crystallization; requires stabilizing polymers [50]. |
| Signal slowly increasing over time | Crystalline precipitation | The compound has a strong tendency to form stable, low-energy crystals [50]. |
| No significant signal | Concentration below amorphous solubility | Lower risk of precipitation; may not require complex enabling formulations [50]. |
Table 2: Performance of Natural Coagulants in Turbidity Reduction (from Jar Tests)
| Natural Coagulant | Initial Turbidity (NTU) | Final Turbidity (NTU) | Turbidity Reduction (%) |
|---|---|---|---|
| Cicer arietinum | 100 | 3.9 | 96.1% [52] |
| Moringa oleifera | 100 | 5.9 | 94.1% [52] |
| Dolichos lablab | 100 | 11.1 | 88.9% [52] |
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our nephelometry results are inconsistent between replicate samples. What could be the cause? A1: Inconsistent results often stem from poor mixing or particle settling. Ensure your protocol includes standardized, controlled mixing steps (both rapid and slow) during sample preparation [52]. Verify that the plate reader is equipped with an orbital shaking function to keep particles in suspension during the kinetic reading.
Q2: How can I determine if the turbidity signal is from amorphous or crystalline material? A2: Analyze the kinetic profile. An immediate, stable jump in turbidity often indicates amorphous precipitation, while a signal that slowly increases over time suggests the growth of crystalline material [50]. For confirmation, this assay can be coupled with off-line techniques like polarized light microscopy (PLM) on selected samples to identify birefringent crystals.
Q3: We are getting high background signals even in our blank buffers. How can we troubleshoot this? A3: High background can be caused by contamination or particulate matter in buffers and labware.
- Solution 1: Filter all buffers and solutions using a 0.22 µm filter before use.
- Solution 2: Ensure that microplates and cuvettes are clean and dust-free. Use high-quality, particulate-free plates.
- Solution 3: Centrifuge stock solutions if precipitation is suspected.
Q4: What is the key difference between using nephelometry for qualitative screening versus quantitative measurement? A4: The high-throughput nephelometry protocol is designed for qualitative classification (e.g., sorting compounds as highly, moderately, or poorly soluble) to prioritize hits after an HTS campaign [53]. For quantitative solubility values, other methods like HPLC quantification after separation are required, as nephelometry does not directly measure concentration [53] [50].
Q5: How does the presence of polymer excipients affect the turbidity assay? A5: Polymer excipients can significantly impact the results. They may inhibit both amorphous and crystalline precipitation, leading to a higher measured "apparent" amorphous solubility and a lower turbidity signal [50]. This is a key feature of the assay, as it allows for direct screening of excipients that can improve formulation stability.
Experimental Workflow and Decision Pathways
Turbidity Assay Workflow
Frequently Asked Questions (FAQs)
1. What is the fundamental difference between these sample preparation methods?
The core difference lies in the level of sample clean-up prior to analysis.
- 'Dilute and Shoot' (D/S) is a minimalist approach where a sample is simply diluted with a suitable solvent and directly injected into an analytical instrument, like a Liquid Chromatography-Mass Spectrometry (LC-MS) system [54]. It is primarily used for protein-poor liquid samples such as urine or saliva [54].
- 'Grind, Extract, and Filter' represents more extensive sample preparation. It involves homogenizing solid or complex samples ('Grind'), separating analytes from the matrix using organic solvents or solid-phase sorbents ('Extract'), and removing particulate matter that could damage instrumentation ('Filter') [55] [56]. Techniques like Solid Phase Extraction (SPE) and Liquid-Liquid Extraction (LLE) fall under this category [54].
2. When should I choose the 'Dilute and Shoot' method?
'Dilute and Shoot' is ideal when:
- High-throughput and speed are critical, as it is quick and easy [54].
- Analyzing multi-class analytes simultaneously, as the non-selective dilution preserves all compounds in the sample [54].
- Working with relatively clean, protein-poor matrices like urine [54].
- Cost-saving is a priority, as it reduces solvent and consumable use [54].
3. What are the main drawbacks of 'Dilute and Shoot', and how can I mitigate them?
The main challenges and their solutions are summarized in the table below.
Table: Troubleshooting 'Dilute and Shoot' Challenges
| Challenge | Description | Mitigation Strategies |
|---|---|---|
| Matrix Effects (ME) [54] | Co-eluting matrix components alter the ionization efficiency of analytes in the LC-MS source, leading to signal suppression or enhancement and inaccurate results. | - Use a higher dilution factor to reduce matrix component concentration [54].- Optimize chromatographic separation to prevent co-elution [54].- Employ a filter plate (e.g., 0.2 µm) as a clean-up step to remove particulates [55]. |
| Suboptimal Detection Capability [54] | Dilution can lower analyte concentration, potentially pushing it below the method's limit of detection. | - Use a lower injection volume to reduce the amount of matrix introduced [54].- Apply sensitivity-focused instrumentation (e.g., tandem mass spectrometry) [57]. |
| Limited Applicability | Not suitable for solid samples, protein-rich samples (e.g., blood), or techniques like GC-MS that require volatile solvents [54]. | For these samples, a full 'Grind, Extract, and Filter' protocol is necessary. |
4. My sample is turbid. Why is this a problem, and how can 'Grind, Extract, and Filter' help?
Turbidity, often caused by light scattering from suspended particles or precipitates, is a critical issue in drug solution research [1].
- Problems: It can interfere with analytical techniques, particularly those relying on light transmission like UV-Vis spectroscopy, leading to inaccurate concentration readings [1]. In LC-MS, particulates can clog columns and instrumentation.
- Solution: A 'Grind, Extract, and Filter' approach directly addresses this. The filtration step (e.g., using a 0.2 µm filter) physically removes particulates causing turbidity, protecting your equipment and ensuring data integrity [55]. Furthermore, the extraction step selectively isolates the analyte from the turbid matrix.
5. Can you provide a direct comparison of these methods?
The following table outlines the key characteristics of each approach.
Table: Comparison of Sample Preparation Methods
| Feature | 'Dilute and Shoot' | 'Grind, Extract, and Filter' (e.g., SPE, LLE) |
|---|---|---|
| Sample Preparation Time | Short (quick and easy) [54] | Long (labor-intensive and time-consuming) [54] |
| Cost | Low (minimal consumables) [54] | High (solvents, extraction columns) [55] |
| Selectivity/Clean-up | Low (non-selective, all components are diluted) [54] | High (selective removal of matrix interferences) [54] |
| Matrix Effect in LC-MS | Typically higher [54] | Typically lower [54] [55] |
| Analyte Loss | Minimal to none [54] | Possible during transfer and extraction steps |
| Ideal Sample Type | Protein-poor liquids (urine, saliva) [54] | Complex matrices (blood, tissues, turbid solutions) [55] [56] |
| Quantitative Accuracy | Can be compromised by matrix effects; one study showed underestimation of oxycodone by up to 45% compared to SPE [55] | Generally higher due to reduced matrix effects [55] |
Troubleshooting Guides
Guide 1: Addressing Turbidity and Light Scattering in Drug Solutions
Turbidity indicates the formation of insoluble precipitates, a major concern for drug stability and bioavailability [1].
Problem: Drug precipitation in a solution, leading to high turbidity and light scattering. Goal: Identify formulations or excipients that act as precipitation inhibitors.
Experimental Protocol: A Microtiter Plate-Based Turbidity/Light Scattering Assay
This high-throughput method allows for the rank-ordering of excipients based on their ability to inhibit precipitation [1].
- Principle: Monitor the formation of precipitates (turbidity) in real-time by measuring light scattering or optical density.
- Materials:
- Research Reagent Solutions:
- Model Compound: A poorly soluble drug (e.g., Fenofibrate, Dipyridamole) [1].
- Precipitation Inhibitors: Various excipients (e.g., polymers like HPMC, PVP) [1].
- Dissolution Medium: Buffer solution, such as McIlvaine buffer at pH 6.8 [1].
- Solvent: A water-miscible organic solvent to create a drug stock solution (e.g., DMSO) [1].
- Equipment: Microtiter plate reader capable of measuring turbidity or light scattering, centrifuge [1].
- Research Reagent Solutions:
- Procedure:
- Preparation: Dissolve the drug in a suitable solvent to create a concentrated stock solution.
- Supersaturation: Inject a small volume of the drug stock into the dissolution medium in a microtiter plate well to induce a supersaturated state.
- Inhibition Testing: Perform this in wells containing different excipient solutions and a control well with no excipient.
- Measurement: Immediately place the plate in the reader and monitor the turbidity or light scattering signal over time.
- Centrifugation: After the experiment, centrifuge the plate (e.g., at 3500 rpm) to sediment precipitates for further analysis if needed [56].
- Data Analysis: Calculate a Precipitation Inhibition Parameter (PIP), such as the Area Under the Curve for the first 100 minutes (AUCâ‚₀₀). A higher AUCâ‚₀₀ indicates better inhibition of precipitation, as the solution remains clear for longer [1].
Experimental Workflow for Turbidity Assay
Guide 2: Optimizing a 'Dilute and Shoot' LC-MS Method for Urine
Problem: Matrix effects causing signal suppression/enhancement and poor reproducibility in a 'Dilute and Shoot' method.
Goal: Validate a robust, high-throughput 'Dilute and Shoot' method for multi-analyte screening.
Experimental Protocol: 'Dilute and Shoot' for Urine Toxicology [58]
- Materials:
- Procedure:
- Aliquot: Pipette 100 µL of urine sample into a vial.
- Dilute: Add 200 µL of a pre-mixed dilution solvent (e.g., Methanol:Acetonitrile, 3:1 v/v) and the internal standard solution [58].
- Mix: Vortex the mixture thoroughly.
- Clarify (Optional but Recommended): Centrifuge the sample to pellet any insoluble material [58].
- Shoot: Transfer the supernatant to an autosampler vial for LC-MS/MS injection.
- Optimization and Validation Steps:
- Dilution Factor: Test different dilution factors (e.g., 1:2, 1:5, 1:10) to find the optimal balance between minimizing matrix effects and maintaining sufficient sensitivity [54].
- Chromatography: Optimize the LC gradient and column (e.g., C18) to achieve the best possible separation of analytes from each other and from matrix components that elute at the void volume [54].
- Matrix Effect Test: Continuously post-infuse a standard analyte solution and inject a prepared sample. A dip or rise in the baseline at the analyte's retention time indicates ion suppression or enhancement [54].
'Dilute and Shoot' LC-MS Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
This table lists essential materials used in the sample preparation methods discussed.
Table: Essential Reagents and Materials for Sample Preparation
| Item | Function / Application | Example Use-Case |
|---|---|---|
| LC-MS Grade Solvents (Water, Methanol, Acetonitrile) [57] | High-purity solvents to minimize background noise and contamination in sensitive LC-MS analysis. | Diluent in 'Dilute and Shoot'; mobile phase in LC. |
| Solid Phase Extraction (SPE) Cartridges [54] | Selective capture and clean-up of analytes from complex samples, reducing matrix effects. | Extracting drugs from blood or plasma. |
| 0.2 µm Filter Plates or Syringe Filters [55] | Removal of particulate matter to prevent clogging of LC systems and reduce noise. | Final step in 'Grind, Extract, and Filter' or as a clean-up for 'Dilute and Shoot'. |
| Internal Standards (e.g., Deuterated Analogs) [57] | Account for variability in sample preparation and ionization efficiency in MS, improving accuracy. | Added to both 'Dilute and Shoot' and extraction methods before processing. |
| Microtiter Plates [1] | Enable high-throughput screening of multiple samples or conditions simultaneously. | Turbidity-based precipitation inhibition assays. |
| Enzymes (e.g., β-Glucuronidase) [54] | Hydrolyze conjugated drug metabolites (e.g., glucuronides) to measure total drug concentration. | Pre-treatment step for urine samples before 'Dilute and Shoot'. |
| Potassium ionophore III | Potassium ionophore III, CAS:99348-39-7, MF:C46H70N4O18, MW:967.1 g/mol | Chemical Reagent |
| Fluorescein diacetate 6-isothiocyanate | Fluorescein Diacetate 6-Isothiocyanate|6-FITC DA|CAS 890090-49-0 | Fluorescein diacetate 6-isothiocyanate is a cell-permeant viability and protein labeling probe. For Research Use Only. Not for human or veterinary use. |
In modern drug development, a significant hurdle facing scientists is the poor aqueous solubility of new Active Pharmaceutical Ingredients (APIs). It is estimated that 70% to 80% of pipeline drugs in development today are poorly soluble molecules, a figure that rises to over 70% when considering the broader drug development pipeline [59] [60]. This challenge is particularly acute in rapidly growing therapeutic areas like oncology, antivirals, and anti-inflammatories [60]. For researchers, the consequence of insufficient API solubility in a dosage form includes low drug loading, stability issues, and ultimately, lower bioavailability, which can compromise a drug's therapeutic potential [61].
Within the laboratory, poor solubility often manifests physically as sample turbidity. This cloudiness is a direct result of insoluble API particles scattering light, which can interfere with analytical measurements and is a key indicator of formulation instability [1] [62]. Effectively managing this turbidity and the underlying light scattering is not merely an analytical concern; it is central to developing a viable and effective drug product. This guide provides targeted, practical strategies for selecting diluents and excipients to overcome these challenges.
FAQs and Troubleshooting Guides
Frequently Asked Questions (FAQs)
Q1: Why is my drug solution cloudy, and why is this a problem? A cloudy or turbid solution indicates that undissolved API particles are suspended in the liquid. These particles scatter light, which is the root cause of the turbidity you observe [63]. This is a significant problem for several reasons:
- Bioavailability: Turbidity signals that the API is not fully dissolved, which can lead to poor and unpredictable absorption in the body [59] [64].
- Analytical Interference: Light scattering from particles can interfere with UV/VIS spectrophotometry and other optical analytical methods, leading to inaccurate concentration readings [1] [62].
- Stability Indicator: An increase in turbidity over time, especially for biotherapeutics, can indicate aggregation, precipitation, or other decomposition pathways, compromising drug stability [62].
Q2: What is the difference between a turbidimeter and a nephelometer, and which should I use? The choice depends on your sample's particle concentration and the required sensitivity [63].
- Nephelometers are dedicated instruments that measure the intensity of light scattered at a 90-degree angle by particles in the sample. They are highly sensitive and are the best choice for samples with low concentrations of small particles (< 1 µm), such as early-stage drug solubility screens or protein aggregates [1] [63] [62].
- Turbidimeters typically measure the reduction of transmitted light (attenuation or absorbance) caused by particles. They are a better fit for samples with a high concentration of scattering particles [63]. Many standard microplate readers can function as turbidimeters.
The table below summarizes the key differences:
Table 1: Comparison of Nephelometry and Turbidimetry
| Feature | Nephelometry | Turbidimetry |
|---|---|---|
| Measurement Principle | Intensity of scattered light (typically at 90°) | Reduction of transmitted light (attenuation) |
| Optimal Use Case | Low concentration of small particles | High concentration of particles |
| Sensitivity | High (approx. 30x more sensitive than turbidimetry) [63] | Moderate |
| Common Instrument | Dedicated nephelometer (e.g., NEPHELOstar Plus) [63] | UV/VIS spectrophotometer or microplate reader |
Q3: My API is not ionizable. Can salt formation still help? No, salt formation is only applicable to ionizable compounds (acids or bases) [60]. For the more than 50% of development compounds that are non-ionizable or form unstable salts, alternative strategies must be employed. These include lipid-based formulations, amorphous solid dispersions (ASDs), particle size reduction, and cyclodextrin complexation [61] [60].
Troubleshooting Common Experimental Issues
Problem: Inconsistent Turbidity Measurements in Colored Samples
- Symptoms: Turbidity values are artificially high and do not correlate with data from a reference nephelometer.
- Root Cause: Standard transmittance-based turbidity measurements (brightfield mode) cannot discriminate between light scattering from particles and light absorption from the sample's color [62].
- Solution:
- Use True Nephelometry: Employ an instrument with a detector set at a 90-degree angle to the light source, which specifically measures scattered light and is minimally affected by sample color [63] [62].
- Instrument Modification: If a brightfield system must be used, one proven solution is to modify the setup. As demonstrated in one study, adding a halogen lamp positioned at 90° from the camera axis enabled accurate nephelometric analysis of colored bovine serum albumin (BSA) solutions, bringing results in line with a standard nephelometer [62].
Problem: API Precipitation During Dilution or pH Shift
- Symptoms: A clear solution becomes turbid upon introduction to an aqueous environment (e.g., gastric fluid simulant) or upon dilution.
- Root Cause: The drug is in a supersaturated state, and the solution lacks adequate precipitation inhibitors to maintain this metastable state [1].
- Solution:
- Identify Precipitation Inhibitors: Screen excipients like polymers (e.g., HPMC, PVP) and surfactants that can act as precipitation inhibitors. They work by extending the duration of supersaturation, thereby improving the potential for absorption [1] [64].
- High-Throughput Screening: Utilize microplate plate-based laser scattering or turbidity methods for rapid rank-ordering of potential precipitation inhibitors. Parameters like AUC100 from laser scattering have shown an excellent correlation with classical concentration-based methods for identifying effective inhibitors like HPMC for drugs such as fenofibrate [1].
Problem: Poor Solubility in Both Aqueous and Organic Solvents
- Symptoms: An API, often referred to as a "brick dust" compound, has low solubility in water and common organic solvents (e.g., methanol, acetone), making formulation and processing (like spray drying) difficult [60].
- Root Cause: High crystal lattice energy and high melting point.
- Solution:
- Use Volatile Processing Aids: For ionizable "brick dust" compounds, use volatile acids (e.g., acetic acid for basic drugs) or bases (e.g., ammonia for acidic drugs) in the organic solvent. This ionizes the drug, dramatically increasing organic solubility (10- to 40-fold has been reported), and the aid is removed during subsequent processing like spray drying, regenerating the original API form [60].
- Apply Thermal Processes: For spray drying, use warm processes or a temperature-shift technology where a slurry is rapidly heated above the solvent's boiling point to dissolve the drug just before atomization. This can achieve an 8- to 14-fold increase in throughput [60].
Experimental Protocol: Screening Precipitation Inhibitors
This protocol outlines a method for using a microplate nephelometer to screen excipients for their ability to inhibit drug precipitation, a common cause of turbidity. The method is based on the high-throughput screening techniques described in the literature [1].
Objective: To rank-order the efficacy of various polymeric excipients as precipitation inhibitors for a poorly soluble model API (e.g., Fenofibrate or Dipyridamole).
Principle: A drug is dissolved in a water-miscible organic solvent to create a supersaturated solution when added to an aqueous buffer. The subsequent precipitation of the drug is monitored in real-time by measuring the increase in light scattering (nephelometry). Effective precipitation inhibitors slow down the rate and reduce the extent of precipitation, resulting in a lower scattered light signal [1].
Materials & Reagents:
- API: Poorly water-soluble model drug (e.g., Fenofibrate).
- Precipitation Inhibitors: A panel of polymers (e.g., HPMC, PVP, HPMCAS, Poloxamer).
- Solvent: Appropriate water-miscible solvent (e.g., DMSO).
- Buffer: McIlvaine buffer (pH 6.8) or another physiologically relevant buffer.
- Equipment: Laser-based microplate nephelometer (e.g., NEPHELOstar Plus) [1] [63].
- Labware: 96-well or 384-well microplates.
Procedure:
- Preparation of Incubation Plate: Dispense buffer solutions containing different excipients (at various concentrations) into the wells of a microplate. Include control wells with buffer alone.
- Generation of Supersaturation: Prepare a concentrated stock solution of the API in a suitable organic solvent. Use a liquid handler to rapidly inject a small volume of this stock solution into each well of the incubation plate, under continuous shaking, to instantaneously create a supersaturated solution.
- Nephelometric Measurement: Immediately place the plate in the nephelometer and start kinetic measurement. The instrument will periodically scan each well, measuring the intensity of scattered light over a defined period (e.g., 60-120 minutes).
- Data Analysis: Calculate a Precipitation Inhibition Parameter (PIP) for each well. The AUC100 (Area Under the scattering curve for the first 100 seconds) has been validated as a reliable PIP that correlates well with classical HPLC methods [1]. A higher AUC100 indicates less precipitation and a more effective inhibitor.
The workflow for this screening process is summarized in the following diagram:
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and their functions for working with poorly soluble APIs, particularly in the context of managing turbidity.
Table 2: Essential Research Reagents and Materials for Solubility and Turbidity Studies
| Reagent/Material | Function/Application | Examples & Notes |
|---|---|---|
| Polymeric Carriers (for ASDs) | Form amorphous solid dispersions to enhance apparent solubility and inhibit precipitation [59] [64]. | HPMC, HPMCAS, PVP, PVP-VA. Selection is API-dependent [64]. |
| Lipidic Excipients | Serve as the basis for lipid-based formulations like SEDDS, which solubilize lipophilic drugs before ingestion [59] [61]. | Triglycerides, mixed glycerides. Used in microemulsions and solid lipid nanoparticles [59]. |
| Surfactants | Enhance wettability, solubilization, and dissolution; can reduce in-vivo precipitation [1] [61]. | Poloxamers, various surfactants in SEDDS. Mechanisms are well-evaluated [61]. |
| Cyclodextrins | Form dynamic inclusion complexes to improve water-solubility and bioavailability of APIs [61]. | Substituted β-cyclodextrins are commonly used. They solubilize APIs as a function of their concentration [61]. |
| Volatile Processing Aids | Temporarily increase solubility of ionizable APIs in organic solvents for processing (e.g., spray drying) [60]. | Acetic acid (for basic APIs), Ammonia (for acidic APIs). Removed during drying [60]. |
| Microplate Nephelometer | High-throughput instrument for automated solubility and precipitation inhibition screening [1] [63]. | Measures scattered light at 90°. Key for detecting early precipitation and aggregation [63]. |
| Diethylumbelliferyl phosphate | 7-Hydroxy-4-methylcoumarin diethylphosphate|Substrate | 7-Hydroxy-4-methylcoumarin diethylphosphate is a fluorogenic OP-hydrolase substrate for enzymatic activity assays. For Research Use Only. Not for human use. |
| Methyl 3-O-feruloylquinate | Methyl 3-O-feruloylquinate, MF:C18H22O9, MW:382.4 g/mol | Chemical Reagent |
The Role of Static Light Scattering (SLS) and Multi-Wavelength Turbidimetry (MWT) in Comprehensive Analysis
Static Light Scattering (SLS) and Multi-Wavelength Turbidimetry (MWT) are powerful, non-invasive optical techniques essential for characterizing the dynamics and structure of nanoparticles and nanostructured networks in drug solution research. SLS analyzes the time-averaged angular distribution of scattered light to determine molecular weight, particle size, and morphological structure [3]. MWT measures the sample extinction coefficient across wavelengths (typically 300-1000 nm) to assess turbidity, which quantifies the loss of transmitted light intensity due to scattering [3]. For non-absorbing samples, this attenuation arises solely from scattering, making MWT an integrated scattering technique [3]. Together, these methods probe complementary length scales—from ~5-500 nm (Dynamic Light Scattering, DLS) to ~1-100 μm (Low Angle SLS)—providing a comprehensive approach for analyzing stationary, aggregating, polymerizing, or self-assembling samples critical to biopharmaceutical development [3].
Technical Fundamentals and Working Principles
Static Light Scattering (SLS) Fundamentals
SLS operates on the principle that when a laser beam impinges on an optically inhomogeneous sample, light is scattered due to local fluctuations in the dielectric constant [3]. The intensity of this scattered light is measured at one or more angles relative to the incident beam [65]. For small, dilute particles (relative to the light wavelength), the scattered light is isotropic (Rayleigh scattering), and its intensity is directly proportional to the molecular weight (M) of the particle, its concentration (C), the square of the refractive index of the buffer (n₀), and the square of the differential refractive index of the particle relative to concentration (dn/dc)² [65]. This relationship allows researchers to calculate absolute molecular weight without reference standards [66]. SLS can be performed in batch mode using a cuvette, providing the weight-average molecular weight of the entire sample, or coupled with separation techniques like GPC/SEC to determine molecular weight distributions across different populations in mixed samples [66].
Multi-Wavelength Turbidimetry (MWT) Fundamentals
MWT, while not strictly a scattering technique as it doesn't measure angular scattering, quantifies the overall power transmitted through a sample as a function of wavelength [3]. The measured extinction coefficient represents combined losses from both absorption and scattering. However, for non-absorbing samples or spectral regions without absorption, attenuation occurs exclusively through scattering, allowing MWT to serve as an integrated scattering measurement [3]. The technique employs formazin as a primary turbidity standard, with measurements expressed in Nephelometric Turbidity Units (NTU) [21]. Different light scattering regimes (Rayleigh, Mie, and geometric scattering) dominate depending on particle size and wavelength, which can be classified using a dimensionless calibration factor (γ = 2πNTU/λ) [21].
Complementary Nature of SLS and MWT
SLS and MWT provide complementary information for comprehensive sample characterization:
- SLS offers detailed structural information (molecular weight, size) through angular-dependent measurements [3] [66].
- MWT provides rapid stability assessment through turbidity profiling across wavelengths [3] [21].
- Together they bridge multiple length scales, enabling researchers to correlate structural changes with macroscopic solution behavior [3].
The diagram below illustrates how these techniques integrate within a comprehensive analysis workflow:
Key Research Reagent Solutions
Successful implementation of SLS and MWT methodologies requires specific reagent systems calibrated to appropriate standards. The table below details essential materials and their functions in light scattering and turbidimetry experiments:
| Reagent/Material | Function | Application Context |
|---|---|---|
| Formazin Standards | Synthetic polymer primary reference for turbidity calibration [21] | MWT instrument calibration across 0.5-4000 NTU range [21] |
| Hydrazine Sulfate | Reactant for formazin synthesis (99% purity) [21] | Production of 4000 NTU primary standard [21] |
| Hexamethylenetetramine | Reactant for formazin synthesis (99% purity) [21] | Production of 4000 NTU primary standard [21] |
| Mixed Bed Resin | Removes ammonium cyanate contaminants from urea solutions [67] | Sample preparation for electrophoresis and stability studies |
| Ammonium Chloride | Common ion effect to reduce cyanate formation in urea [67] | Maintaining protein stability in urea-containing buffers |
| Benzonase Nuclease | Degrades DNA/RNA without proteolytic activity [67] | Reduces viscosity in crude cell extracts for accurate light scattering |
Troubleshooting Guides
Common Experimental Artifacts and Remediation Strategies
Various artifacts can compromise light scattering and turbidity measurements. The table below identifies frequent issues and their solutions:
| Problem | Potential Cause | Solution | Prevention |
|---|---|---|---|
| Multiple bands in SDS-PAGE | Protease activity in sample buffer prior to heating [67] | Heat samples immediately after adding to buffer at 75°C for 5 min [67] | Design experiment: compare immediate vs. delayed heating [67] |
| Protein degradation | Asp-Pro bond cleavage at high temperatures [67] | Use lower heating temperature (75°C instead of 95-100°C) [67] | Limit heating time; several proteins stable for hours at 100°C [67] |
| Contaminating bands at 55-65 kDa | Keratin contamination from skin or dander [67] | Run sample buffer alone; remake if contaminated [67] | Aliquot and store lysis buffer at -80°C; use within 1-2 days [67] |
| Carbamylation (+43 Da mass) | Cyanate contamination in urea solutions [67] | Treat urea with mixed bed resin; add scavengers [67] | Use ammonium salts in buffer; minimize exposure time [67] |
| Inaccurate turbidity readings | Improper formazin calibration [21] | Recalibrate using fresh formazin standards across operational range [21] | Use standards immediately after preparation; verify calibration zones [21] |
| Poorly resolved bands | Insoluble material in sample [67] | Centrifuge at 17,000 x g for 2 min after heat treatment [67] | Add urea or nonionic detergent for problematic proteins [67] |
| High sample viscosity | Uns sheared nucleic acids in crude extracts [67] | Treat with Benzonase; vortex vigorously or sonicate [67] | Use recombinant endonuclease to degrade DNA/RNA [67] |
Sample Preparation Protocols
Proper Sample Preparation for Reliable SLS Analysis
- Protein Concentration Determination: Determine protein concentration using a standard assay before SLS analysis [67].
- Optimal Loading Parameters:
- SDS Ratio Maintenance: Maintain adequate SDS-to-protein ratio (recommended 3:1 mass ratio) to ensure complete denaturation [67].
- Special Additives for Problematic Proteins: For histones and membrane proteins that may not completely dissolve in SDS buffer alone, add 6-8 M urea or a nonionic detergent such as Triton X-100 [67].
- Insoluble Material Removal: Centrifuge samples at 17,000 x g for 2 minutes following heat treatment to remove insoluble material that causes streaking [67].
- Sample Storage: Store supernatants at 4°C overnight or frozen at -20°C for longer periods. Rewarm briefly at 37°C to redissolve SDS and recentrifuge before loading [67].
Formazin Turbidity Standard Preparation for MWT Calibration
- 4000 NTU Primary Standard:
- Dilution Series Preparation: Perform progressive dilutions of the 4000 NTU standard to generate a diverse set of calibration standards [21].
- Standard Usage: Use standards immediately after preparation to generate accurate calibration curves [21].
Frequently Asked Questions (FAQs)
Technique Selection and Application
Q1: What is the fundamental difference between Static Light Scattering (SLS) and Dynamic Light Scattering (DLS)? SLS measures the average intensity of scattered light to determine molecular weight and particle concentration [65], while DLS analyzes fluctuations in scattered light intensity over time to determine diffusion coefficients and hydrodynamic size [3] [65]. A helpful analogy: SLS tells you how loud the music is at a concert, while DLS tells you what song is being played [65].
Q2: When should I use SLS instead of DLS for protein characterization? SLS is ideal for detecting the onset of aggregation as it provides a direct measurement that increases immediately when molecular weight increases [65]. DLS is better for comparing sizes day-to-day or batch-to-batch and for measuring how particle size changes over long isothermal experiments [65].
Q3: What length scales can be probed using combined light scattering techniques? Combined techniques can probe broad length scales: DLS covers ~5-500 nm, Wide-Angle SLS covers ~0.1-5 μm, Low-Angle SLS covers ~1-100 μm, and MWT probes scales typical of WA-SLS [3].
Q4: Can SLS detect protein aggregation? Yes, SLS is highly sensitive to aggregation. When paired with a thermal ramp, it can detect the aggregation onset temperature (Tagg) as intensity increases, helping characterize formulation stability in response to heat stress [65].
Measurement and Calibration
Q5: What is the relationship between NTU, FNU, and other turbidity units? When calibrated with formazin suspensions, NTU (Nephelometric Turbidity Units), FNU (Formazin Nephelometric Units), and AU/FAU (Absorbance Units/Formazin Absorbance Units) exhibit 1:1 equivalence (1 NTU = 1 FNU = 1 AU = 1 FAU) [21].
Q6: How does Multi-Wavelength Turbidimetry extend beyond conventional turbidity measurements? MWT expands operational ranges beyond typical limitations (0.5-4000 NTU vs. conventional 0-1000 NTU) and across multiple wavelengths (500-1000 nm), while also identifying specific scattering mechanisms through a dimensionless calibration factor (γ = 2πNTU/λ) [21].
Q7: What are the key considerations for accurate SLS molecular weight determination? Accurate SLS requires knowledge of particle concentration (C), refractive index of buffer (n₀), and differential refractive index of the particle relative to concentration (dn/dc)² [65]. For batch measurements, the result represents the weight average molecular weight of the entire sample [66].
Problem Resolution
Q8: How can I prevent protein degradation during sample preparation? Heat samples immediately after adding to SDS buffer (at 75°C for 5 minutes rather than 95-100°C) to inactivate proteases and avoid Asp-Pro bond cleavage [67]. Even 1 pg of protease can cause major degradation if heating is delayed [67].
Q9: What causes high viscosity in samples, and how can it be reduced? High viscosity typically comes from unsheared nucleic acids in crude extracts [67]. Treatment with Benzonase Nuclease (which lacks proteolytic activity), vigorous vortexing of heated samples, or sonication can reduce viscosity [67].
Q10: How can I prevent carbamylation artifacts in urea-containing buffers? Carbamylation adds 43 Da per event and can be minimized by treating urea solutions with mixed bed resin, adding scavengers like ethylenediamine or glycylglycine, replacing some NaCl with ammonium chloride (25-50 mM), and minimizing protein exposure time to urea solutions [67].
Automated Transmittance Analysis and Adjustable Laser Focus
Frequently Asked Questions (FAQs)
What is the primary function of automated transmittance analysis in a DLS instrument? Automated transmittance analysis measures how much light passes through a sample. The instrument uses this measurement to automatically select the optimal scattering angle and laser focus position for the analysis, which is crucial for obtaining reliable data from turbid drug solutions without requiring manual, time-consuming optimization [43].
Why is an adjustable laser focus position critical for analyzing concentrated suspensions? In turbid samples, the laser light has a long path and can be scattered multiple times by different particles, a phenomenon called multiple scattering, which leads to measurement errors. By adjusting the laser focus position closer to the cuvette wall, the instrument shortens the light's path through the sample. This significantly reduces the probability of multiple scattering events, ensuring that the detected light provides an accurate representation of particle size and dynamics [43].
My research involves supersaturated drug solutions, which are often turbid. Can these techniques be applied? Yes, absolutely. The combination of automated transmittance analysis and adjustable laser focus is particularly well-suited for investigating drug precipitation from supersaturated solutions, a common scenario in bioavailability enhancement studies. Light scattering and turbidity methods are established tools for monitoring such dynamic processes in real-time [1] [3].
We study the formation of biologic nanofiber networks, which become highly turbid. Are these methods applicable? Yes, these techniques are powerful for characterizing polymerizing systems like nanofiber networks. Light scattering methods can probe a wide range of length scales, from nanometers to hundreds of micrometers, making them ideal for studying the structure and dynamics of fiber formation and gelation that occur during network assembly [3].
Troubleshooting Guide
The following table outlines common problems, their potential causes, and solutions related to managing sample turbidity.
| Problem | Possible Cause | Recommended Solution |
|---|---|---|
| Unreliable data or measurement failures with turbid samples. | Multiple scattering events due to high particle concentration or strong scatterers. | Utilize the instrument's automated transmittance analysis to determine and set the optimal laser focus position and scattering angle [43]. |
| Consistent overestimation of particle size in concentrated formulations. | Photons are scattered multiple times before detection, distorting the correlation function. | Employ a back-scattering (e.g., 175°) detection geometry and adjust the laser focus to minimize the photon path length in the sample [43]. |
| High noise or low signal-to-noise ratio in data from opaque suspensions. | Signal attenuation due to excessive scattering or absorption; suboptimal instrument settings. | Let the instrument automatically configure itself based on an initial transmittance measurement. Manual override should focus the laser near the inner cuvette wall [43]. |
| Inconsistent results between different runs of the same turbid sample. | Manual instrument setup leads to variations in scattering angle and focus position. | Standardize your protocol to always use the automated transmittance analysis feature for initial setup to ensure consistency and reproducibility [43]. |
Experimental Protocol: Monitoring Drug Precipitation Inhibition
This protocol utilizes a laser scattering microtiter plate-based method to identify excipients that effectively inhibit the precipitation of poorly soluble drug compounds from supersaturated solutions.
Background and Principle
During the development of drug formulations for poorly soluble compounds, maintaining a supersaturated state in the gastrointestinal tract is a common strategy to enhance oral bioavailability. This protocol screens for precipitation inhibitors (PIs) by monitoring the light scattering signal of a drug solution. When a drug precipitates, it forms particles that scatter light, causing a sharp increase in the scattering signal. Effective inhibitors delay or prevent this increase. This method has been validated against classical concentration-based methods and shows an excellent correlation, making it a reliable high-throughput "first screen" [1].
Materials and Reagents
| Research Reagent Solution | Function in the Experiment |
|---|---|
| Model Compound (e.g., Fenofibrate, Dipyridamole) | The poorly soluble active pharmaceutical ingredient (API) whose precipitation is being studied. |
| Precipitation Inhibitors (PIs) | Various excipients (e.g., polymers) tested for their ability to stabilize the supersaturated drug solution. |
| Supersaturated Drug Solution | The unstable solution of the drug compound, created at a concentration higher than its thermodynamic solubility. |
| McIlvaine Buffer (pH 6.8) | A biologically relevant dissolution medium that simulates the intestinal environment. |
| Microtiter Plate | A multi-well plate used for high-throughput testing of multiple excipient and control conditions simultaneously. |
| Plate Reader with Laser Scattering | An instrument capable of measuring the light scattering signal from each well of the plate over time. |
Step-by-Step Procedure
- Preparation of Incubation Plate: In a microtiter plate, prepare your test conditions. This typically includes:
- Test Wells: Supersaturated drug solution with different candidate precipitation inhibitors.
- Control Wells: Supersaturated drug solution without any inhibitor (negative control).
- Blank Wells: Buffer with inhibitor but no drug (to account for background scattering from the excipients) [1].
- Instrument Setup and Measurement:
- Place the microtiter plate into the plate reader.
- If available, leverage any automated features that assess sample turbidity to optimize detection parameters.
- Initiate the time-dependent measurement of the laser scattering signal (e.g., every 30-60 seconds for 60-120 minutes).
- Data Analysis:
- For each well, plot the light scattering intensity over time.
- Calculate the Area Under the Curve for the first 100 minutes (AUCâ‚₀₀), which has been shown to be a reliable Precipitation Inhibition Parameter (PIP) [1].
- Rank the performance of the various excipients based on their AUCâ‚₀₀ values. A higher AUCâ‚₀₀ indicates less precipitation and a more effective inhibitor.
Workflow Visualization
The logical workflow of the drug precipitation inhibition experiment is summarized in the following diagram:
Troubleshooting and Optimization Strategies: Overcoming Common Challenges in Turbid Samples
Troubleshooting Guides
Why is adjusting the laser focus position critical for analyzing turbid drug solutions?
In Dynamic Light Scattering (DLS), the theory assumes detected photons have been scattered only once. In turbid samples, like concentrated drug suspensions, the high particle density means photons are likely scattered multiple times before detection, a phenomenon called multiple scattering. This leads to incorrect correlation functions and artificially small calculated particle sizes, violating core DLS principles [43].
Adjusting the laser focus position mitigates this by controlling the photons' path length through the sample. The scattering volume is defined as the intersection of the laser and detector beams. By moving the focusing lens, this volume can be shifted within the sample cuvette [43] [45]. For turbid samples, positioning the focus close to the inner cuvette wall minimizes the distance light travels through the sample, drastically reducing the probability of multiple scattering events [43].
Figure 1: Troubleshooting workflow for multiple scattering issues in DLS.
How do I select the correct detection angle and path length for my sample?
Choosing the appropriate detection angle is crucial for managing turbidity. Modern DLS instruments often automatically select the optimal angle and focus position by assessing light transmittance, correlation function intercept, and detected light intensity prior to the main experiment [43].
Back-scattering (175°) is highly recommended for turbid samples. At this angle, the scattering volume is near the cuvette wall, creating a very short optical path length. This setup significantly reduces multiple scattering and is ideal for highly concentrated, turbid suspensions common in drug formulation development [43] [45].
Optical Path Length Reduction involves a physical adjustment of the sample cell. Placing the cuvette so the laser beam enters near its corner can reduce the effective path length to as little as 100 µm. This technique drastically decreases multiple scattering events while increasing single scattering events, enabling reliable DLS measurements even in opaque suspensions [68].
Table 1: DLS Detection Angle Selection Guide for Drug Solution Analysis
| Detection Angle | Best For Sample Type | Key Advantage | Path Length | Application in Drug Research |
|---|---|---|---|---|
| Back-Scattering (175°) | Highly concentrated, turbid suspensions [43] [45] | Minimizes path length, suppresses multiple scattering [43] | Very Short | Analyzing chemical slurries, drug formulations, opaque protein aggregates |
| Side-Scattering (90°) | Weakly scattering samples, small particles [45] | Clean signal, less sensitive to cuvette wall defects [45] | Medium | Measuring dilute proteins, nanomedicines, small molecule aggregates |
| Forward-Scattering (15°) | Monitoring aggregation, few large particles [45] | Emphasizes signal from larger particles [45] | Long | Detecting large aggregates or breakthrough in filtered samples |
Frequently Asked Questions (FAQs)
What are the signs of multiple scattering in my DLS data?
Several indicators in your raw data suggest significant multiple scattering:
- Artificially Small Calculated Size: The measured hydrodynamic diameter is consistently and unrealistically small for the known sample.
- Correlation Function Shape: The correlation function may exhibit a non-linear baseline or an abnormally fast decay [45].
- Intensity Trace: The intensity trace of the scattered light may show irregular fluctuations or a loss of defined signal [45].
My drug solution is colored. Does this affect multiple scattering strategies?
Yes, sample color adds complexity. Colored samples absorb light, which can reduce the overall scattering intensity. However, as long as the laser light is not completely absorbed, the sample can be measured. The core strategies—using back-scattering and reducing the optical path length—remain valid and are often even more critical to ensure a sufficient signal-to-noise ratio from the reduced scattering volume [69].
What is the role of sample concentration in multiple scattering?
Sample concentration is a primary factor. The Stokes-Einstein equation used in DLS applies to infinitely dilute solutions. As concentration increases, so does the probability of multiple scattering. For accurate DLS particle sizing, the sample must be clear to very slightly hazy. White or milky samples should be diluted until they are only slightly hazy. A simple dilution check is recommended: dilute the sample by 50%; if the measured size remains the same and the scattering intensity (count rate) halves, the original concentration was acceptable [69].
Are there advanced hardware solutions to suppress multiple scattering?
Yes, advanced techniques beyond standard angle and focus adjustments exist. Cross-correlation DLS is one such method. This technique uses two detectors aimed at the same scattering volume but with a slight angular offset. By cross-correlating their signals, contributions from multiple scattering (which are less correlated) can be mathematically suppressed, allowing the single scattering signal to be isolated [70]. This is particularly useful for extremely dense suspensions.
Experimental Protocol: Optimizing Laser Focus for Turbid Samples
This protocol provides a step-by-step methodology for analyzing a turbid drug suspension using laser focus adjustment and back-scattering detection.
Objective: To obtain a reliable particle size measurement from a turbid protein-based drug suspension by minimizing multiple scattering events.
Materials:
- DLS instrument with adjustable laser focus and back-scattering (175°) detection capability (e.g., Litesizer 500)
- High-quality, clean quartz cuvette (multiple polished windows)
- Sample of turbid drug suspension
- Appropriate dispersant (e.g., 10 mM KNO₃ in water for aqueous samples) [69]
- Pipettes and filters (if dilution is needed)
Table 2: Research Reagent Solutions for DLS of Turbid Samples
| Item | Function/Description | Technical Notes |
|---|---|---|
| Quartz Cuvette | Holds sample for analysis; multiple polished windows allow light access at various angles [71]. | Standard spectrophotometer cuvettes are not suitable. Ensure they are meticulously cleaned to remove dust [71]. |
| Ionic Solution (e.g., 10 mM KNO₃) | Aqueous dispersant that screens electrostatic interactions between charged particles [69]. | Prevents inflated size measurements in DI water. KNO₃ is preferred over NaCl as it is less aggressive and less likely to adsorb to particle surfaces [69]. |
| Formazin Standards | Synthetic polymer used as a primary reference material for turbidity calibration [21]. | Traceable to standards like NIST; used for validating instrument performance and establishing NTU-to-absorbance correlations [21] [72]. |
| Syringe Filters (0.1-0.2 µm) | Removes dust and large contaminants from dispersants and samples prior to measurement [69]. | Always rinse filters according to manufacturer's practice. Use a pore size ~3x larger than the largest particle to avoid altering the size distribution [69]. |
Procedure:
- Sample Preparation: If the sample is excessively turbid (milky or opaque), perform a preliminary dilution in the appropriate dispersant. The ideal concentration for DLS is a solution that is clear to slightly hazy [69]. Filter the dispersant through a 0.2 µm filter to remove dust.
- Instrument Initialization: Turn on the DLS instrument and allow the laser to stabilize. Set the temperature to the desired value (e.g., 25°C) and allow the sample chamber to equilibrate.
- Transmittance Analysis (if automated): Load the sample into a clean cuvette, ensuring no air bubbles are present. For instruments with automatic settings, initiate the pre-measurement analysis. The instrument will quickly assess light transmittance and other parameters to automatically select the best angle (likely 175°) and an initial laser focus position [43].
- Manual Focus Adjustment: If manual control is available or required, set the detector to back-scattering mode (175°). Begin by setting the laser focus to its position closest to the cuvette wall. This minimizes the path length through the sample [43].
- Data Quality Assessment: Run a short measurement and examine the correlation function and intensity trace.
- A good correlation function for a monomodal dispersion should be smooth with a single exponential decay [45].
- If the baseline is non-linear or the decay is too fast, multiple scattering may still be significant.
- Iterative Optimization: Slightly adjust the laser focus position away from the wall in small increments, repeating the measurement at each position. Monitor the measured particle size and the quality of the correlation function. The optimal position yields a stable, reproducible size and a high-quality correlation function.
- Final Measurement: Once the optimal focus position is identified, perform a longer measurement with an adequate number of runs to obtain a statistically robust result. Record the hydrodynamic diameter and polydispersity index (PDI).
Figure 2: Experimental workflow for optimizing DLS measurements of turbid samples.
Troubleshooting Guides
Guide 1: Addressing Low Throughput and Rapid Filter Fouling
Q: What are the primary causes of rapid filter fouling and low throughput in bioprocess clarification, and how can they be mitigated?
| Cause | Manifestation | Troubleshooting Action |
|---|---|---|
| High Cell Density & Debris [73] [51] | Increased turbidity, rapid pressure rise. | Implement a two-stage depth filtration (primary followed by secondary) or use functionalized, high-capacity depth filters [73] [51]. |
| High Level of Soluble Impurities [73] | Host Cell Proteins (HCP) and DNA foul downstream filters. | Use charged depth filters designed to adsorb impurities like nucleic acids [73]. |
| Incorrect Filter Pore Size [51] | Poor clarification or premature clogging. | Screen different depth filters with gradient pore sizes to find the optimal fit for your specific feed stream [51]. |
| Product Aggregation [73] | Low capacity on virus filters, especially for bispecific antibodies or lentivirus. | Optimize formulation buffers to reduce aggregation; pre-filter with a tighter pore size filter if applicable [73]. |
Experimental Protocol: Depth Filter Capacity Testing This methodology determines the maximum volume of a cell culture harvest that a specific depth filter can process before fouling [51].
- Filter Selection: Choose a range of depth filters with different pore sizes and media compositions (e.g., cellulose/silica with charged resins) [73] [51].
- Constant Flow Filtration: Set up the filtration system to operate at a constant flow rate. This method is known to provide more accurate capacity data than constant-pressure methods [51].
- Parameter Monitoring: Throughout the process, monitor the differential pressure across the filter and the turbidity of the output filtrate.
- Endpoint Determination: Continue filtration until a predefined endpoint is reached. This endpoint is typically either a maximum allowable pressure drop or a rise in output turbidity, as specified by the filter vendor [51].
- Capacity Calculation: The filter capacity is calculated as the total volume of harvest processed per unit area of the filter (e.g., in liters per square meter, L/m²). Compare the performance of different filters to select the one with the highest capacity and acceptable filtrate clarity (e.g., <15 NTU) [51].
Guide 2: Managing Sample Turbidity and Stability in Drug Formulations
Q: How can stability issues like sedimentation and high turbidity be controlled in pharmaceutical suspensions?
| Cause | Manifestation | Troubleshooting Action |
|---|---|---|
| Gravitational Settling [74] | Particles settle, forming a dense cake at the bottom. | Reduce particle size; induce flocculation to form loose, easy-to-redisperse structures; or increase the viscosity of the continuous phase [74]. |
| Insufficient Electrostatic Repulsion [74] | Particles aggregate and form compact sediments. | Modify the formulation's pH or use stabilizers to achieve a zeta potential more negative than -30 mV or more positive than +30 mV to ensure particle repulsion [74]. |
| Inadequate Redispersion [74] | Settled particles cannot be resuspended with mild shaking. | Promote controlled flocculation to create a weak, porous particle network that entraps liquid and prevents hard caking [74]. |
Experimental Protocol: Achieving Suspension Stability via Zeta Potential and Rheology This protocol uses particle size, zeta potential, and rheology measurements to optimize a stable suspension formulation [74].
- Particle Size Analysis: Use laser diffraction or dynamic light scattering (DLS) to determine the size distribution of the suspended drug particles [74].
- Zeta Potential Titration: Use an autotitrator to adjust the pH of the suspension while simultaneously measuring the zeta potential at each pH interval. Identify the pH region where the zeta potential is sufficiently high (e.g., beyond ±30 mV) for electrostatic stability [74].
- Rheological Profiling:
- Flow Curve: Measure the suspension's viscosity across a range of shear rates (from low to high) to understand its behavior at rest (low shear) and during shaking or pouring (high shear).
- Yield Stress Measurement: Perform a shear stress sweep test to determine if the formulation has a yield stress, a critical value that must be exceeded to initiate flow. A sufficient yield stress can prevent particle settling under gravity [74].
- Formulation Optimization: Correlate the zeta potential and rheology data with observed physical stability. For example, if a high zeta potential does not prevent settling, consider formulating to create a weak gel network with a measurable yield stress [74].
Guide 3: Troubleshooting Turbidity Measurement Inaccuracies
Q: What are common sources of error in turbidity measurements, and how can they be resolved?
| Cause | Manifestation | Troubleshooting Action |
|---|---|---|
| Optical Surface Contamination [7] | Erratic or consistently high readings. | Regularly clean the measurement cuvette and instrument's optical surfaces with a lint-free cloth and manufacturer-recommended cleaning solution [7]. |
| Air Bubbles in Sample [7] [4] | Unstable, fluctuating readings. | Allow the sample to rest after mixing to let bubbles rise; handle samples gently to avoid introducing air when pouring into the cuvette [7]. |
| Incorrect Calibration [7] | Systematic error in all measurements. | Follow the manufacturer's calibration procedure exactly, using fresh, uncontaminated standard solutions. Ensure the instrument has adequate warm-up time [7]. |
| Sample Overload [7] | Readings are off-scale or non-linear. | Dilute the sample so that its turbidity falls within the instrument's calibrated measurement range. Ensure thorough mixing before dilution and measurement [7]. |
| Instrument Limitations [4] | Negative results or readings below the blank. | The sample turbidity may be outside the instrument's detection limit. Use an instrument with a more suitable range and ensure the calibration range is appropriate [4]. |
Frequently Asked Questions (FAQs)
Q: How does flocculation improve the clarification process? A: Flocculation works by adding a cationic polymer to the harvest, which binds to cells and debris. Through van der Waals forces, these aggregates form larger, loose structures called flocs. These flocs settle more rapidly and can be more easily trapped by depth filters, significantly improving filter capacity and final filtrate clarity [51].
Q: What is the purpose of a "backwashing" filter, and where is it used? A: Backwashing is a cleaning process where flow is reversed through the filter media to flush out trapped contaminants. This regenerates the filter bed, extends its service life, and maintains consistent performance. It is commonly used in granular activated carbon (GAC) filters to remove accumulated organic matter and particulates, preventing channeling and pressure drop buildup [75].
Q: Why is my lentiviral vector showing low recovery after sterile filtration? A: Lentiviral vectors are large (~120 nm) and fragile, with a tendency to aggregate. Their size is close to the pore size of standard 0.22 µm sterilizing-grade filters, leading to retention and adsorption. Overcoming this may require using a more open pre-filter, adjusting the formulation buffer to minimize aggregation, or employing specialized, closed-system processing that can preclude the need for terminal sterile filtration [73].
Q: When should I use a depth filter versus a membrane filter? A: The choice depends on the application:
- Depth Filters are used for clarifying fluids with high particulate loads (e.g., cell culture harvest). They remove particles throughout their porous matrix, not just on the surface [73] [51].
- Membrane Filters are typically used for bioburden reduction, sterilizing-grade filtration, and virus removal. They act like a sieve, retaining particles larger than their absolute pore size primarily on the surface [73].
Q: How does activated carbon filtration work to reduce turbidity? A: Activated carbon is a highly porous material with a vast surface area that adsorbs (traps on its surface) organic molecules responsible for taste, odor, and color. In spirit beverages, it effectively removes fatty acid esters and other volatile compounds that cause haze (turbidity) when the alcohol content is reduced or the temperature is lowered [76]. It functions via physical adsorption and can also catalyze certain chemical reactions [76].
Experimental Workflows and Signaling Pathways
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials for Filtration and Clarification Experiments
| Item | Function | Application Example |
|---|---|---|
| Depth Filter Sheets (Cellulose/Silica) | Primary clarification; removes cells, debris, and soluble impurities via depth retention and charge interactions [73] [51]. | Clarifying high-density mammalian cell cultures [51]. |
| Sterilizing-Grade Membrane Filters (0.2 µm PES) | Bioburden reduction and sterile filtration; retains microorganisms via size exclusion [73]. | Sterilizing final drug product during fill/finish; filtering buffers and media [73]. |
| Flocculating Agent (Cationic Polymer) | Aggregates fine particles and cells into larger flocs, improving their removal by settling or filtration [51]. | Pre-treatment of challenging cell culture harvests to increase depth filter capacity and throughput [51]. |
| Diatomaceous Earth (DE) | A filter aid used as a body feed; pre-coats filters or is added to slurry to form a porous cake that prevents rapid fouling [51]. | Enhancing the capacity and clarity when filtering harvests with very high solids content [51]. |
| Granular Activated Carbon (GAC) | Removes organic contaminants, color, and odor-causing molecules via adsorption [76] [75]. | De-chlorination of water; reducing haze-forming compounds in spirits [76] [75]. |
| Turbidity Standard (Formazin) | A stable suspension used to calibrate turbidimeters, ensuring accurate and reproducible nephelometric turbidity unit (NTU) measurements [77]. | Calibrating turbidimeters before analyzing filtrate clarity in clarification studies [77] [51]. |
| 2-(1-hydroxypentyl)benzoic Acid | 2-(1-hydroxypentyl)benzoic Acid, MF:C12H16O3, MW:208.25 g/mol | Chemical Reagent |
This technical support center provides targeted guidance for researchers managing the challenges of sample turbidity and light scattering in drug solubilization studies. A primary cause of turbidity is the precipitation of poorly soluble drugs, which can interfere with analytical techniques and compromise data reliability. The following guides and FAQs address specific experimental issues related to enhancing solubility through the use of cyclodextrins and the control of parameters like pH and temperature.
FAQ & Troubleshooting Guides
FAQ 1: How do cyclodextrins enhance drug solubility and reduce sample turbidity?
Answer: Cyclodextrins (CDs) are cyclic oligosaccharides that improve the solubility of poorly water-soluble drugs, thereby reducing sample turbidity caused by drug precipitation [78] [79]. Their unique structure features a hydrophilic exterior and a hydrophobic internal cavity. This allows them to form inclusion complexes in which the hydrophobic drug molecule is encapsulated within the CD's cavity [78]. This process "hides" the drug from the aqueous environment, shifting the equilibrium from a turbid, heterogeneous suspension to a clear, homogeneous solution [78]. The primary mechanism for solubility enhancement is not chemical degradation but physical encapsulation via van der Waals forces [78].
FAQ 2: Why is my drug solution still turbid after adding cyclodextrins, and how can I troubleshoot this?
Answer: Persistent turbidity indicates that the inclusion complex may not have formed effectively. Please follow this troubleshooting guide.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Incorrect CD type | Review cavity size vs. drug molecule dimensions. | Select a CD with a cavity size appropriate for your drug (α-CD: small; β-CD: medium; γ-CD: large) [78] [79]. |
| Insufficient CD concentration | Perform phase-solubility studies to determine the stoichiometry. | Increase the molar ratio of CD to drug to ensure complete complexation [78]. |
| Unfavorable pH | Measure the solution pH versus drug's pKa. | Adjust pH to keep the drug in its neutral form, which has higher affinity for the CD's hydrophobic cavity. |
| Drug degradation/precipitation | Check for chemical instability of the drug under experimental conditions. | Use CDs that protect the drug from external factors (e.g., light, oxygen) to improve stability [78]. |
FAQ 3: How do I accurately analyze particle size in a turbid drug formulation?
Answer: A common misconception is that Dynamic Light Scattering (DLS) cannot analyze turbid samples. While multiple scattering events in concentrated samples can cause errors, modern DLS instruments have mitigation strategies [43] [3].
Recommended Protocol:
- Use Back-Scattering Detection: Configure your DLS instrument to detect scattered light at a 175° angle. This significantly reduces the path length of light through the sample, minimizing multiple scattering events [43].
- Adjust Laser Focus Position: Shift the scattering volume close to the cuvette wall to further shorten the light's path length [43].
- Employ Transmittance Analysis: Advanced instruments can automatically assess sample transmittance to select the optimal scattering angle and laser focus position for reliable data from turbid samples [43].
For highly turbid or aggregating systems, coupling DLS with Static Light Scattering (SLS) or Multi-Wavelength Turbidimetry (MWT) provides a more powerful approach for characterizing particles across different length scales [3].
FAQ 4: What is the difference between turbidimetry and nephelometry for solubility analysis?
Answer: Both methods assess sample cloudiness but based on different principles, making them suitable for different scenarios.
Turbidimetry measures the amount of light transmitted through the sample. The loss of intensity due to scattering is measured, similar to an absorbance read. This is often used for applications like monitoring bacterial growth (OD600) [80].
Nephelometry directly measures the intensity of light scattered by the particles in the sample. It is particularly well-suited for samples with small particle sizes, such as in kinetic solubility screens for drug compounds, and is generally more sensitive for these applications than turbidimetry [80].
The choice depends on your particle size and research goal: use turbidimetry for high particle concentrations and nephelometry for detecting small particles at low concentrations.
Experimental Protocols
Protocol 1: Phase-Solubility Study for Cyclodextrin Selection
Objective: To determine the ability of different cyclodextrins to enhance a drug's solubility and to establish the stoichiometry of the complex.
Materials:
- Drug compound
- Cyclodextrins (α-CD, β-CD, γ-CD, HP-β-CD, etc.)
- Buffer solutions (at relevant pH)
- Orbital shaker incubator
- Centrifuge
- HPLC system or UV-Vis spectrophotometer
- 0.22 μm syringe filters
Method:
- Preparation: Prepare an excess amount of the drug in multiple vials.
- Complexation: Add a fixed volume of aqueous CD solutions of increasing concentrations (e.g., 0-15 mM) to the drug vials.
- Equilibration: Seal the vials and agitate on an orbital shaker for 24-48 hours at a constant temperature (e.g., 25°C or 37°C) to reach equilibrium.
- Separation: Centrifuge the samples and filter the supernatant to remove any undissolved drug.
- Analysis: Quantify the dissolved drug concentration in the supernatant using a validated HPLC or UV-Vis method.
- Data Analysis: Plot the concentration of dissolved drug versus the concentration of CD. The slope of the phase-solubility diagram provides information on the complexation efficiency and stoichiometry.
Protocol 2: Kinetic Solubility Measurement via Nephelometry
Objective: To perform a high-throughput assessment of a drug's kinetic solubility in the presence of excipients.
Materials:
- Drug stock solution in DMSO
- Assay buffer (e.g., phosphate-buffered saline, pH 7.4)
- Microplate reader capable of nephelometry (e.g., NEPHELOstar Plus)
- 384-well microplates
- Liquid handling system
Method:
- Dilution: Dilute the drug stock solution in aqueous buffer across a range of concentrations in a 384-well plate. A typical final DMSO concentration should be ≤1%.
- Incubation: Allow the plate to incubate at room temperature for a predetermined time (e.g., 1 hour).
- Measurement: Place the plate in the nephelometer and measure the scattered light intensity for each well.
- Analysis: Plot the nephelometry signal (scattered light intensity) against the nominal drug concentration. The point where a significant increase in signal occurs indicates the kinetic solubility limit of the drug under those specific conditions.
The Scientist's Toolkit: Key Research Reagents & Materials
| Item | Function / Explanation |
|---|---|
| β-Cyclodextrin (β-CD) | The most commonly used native cyclodextrin for forming inclusion complexes with molecules of medium size [78]. |
| Hydroxypropyl-β-Cyclodextrin (HP-β-CD) | A modified CD with improved water solubility and a better safety profile for parenteral administration compared to native β-CD [78] [79]. |
| Sulfobutyl Ether-β-Cyclodextrin (SBE-β-CD) | A negatively charged, synthetically derived CD known for high aqueous solubility and its use in the formulation of drugs like amphotericin B [78]. |
| Randomly Methylated-β-Cyclodextrin (RAMEB) | A methylated derivative with enhanced hydrophobicity and superior capacity to solubilize highly insoluble drugs [79]. |
| Dynamic Light Scattering (DLS) Instrument | Used for determining the hydrodynamic diameter and size distribution of nanoparticles and inclusion complexes in solution [3]. |
| Nephelometer | A specialized instrument that directly measures scattered light, ideal for high-throughput kinetic solubility screens of small particles [80]. |
Experimental Workflow & Pathway Visualizations
CD Complex Formation
Troubleshooting Turbidity
Core Concepts: Solubility and Extraction
What is the primary challenge of low aqueous solubility in drug development?
Any drug to be absorbed must be present in an aqueous solution at the site of absorption. Low aqueous solubility is a major problem encountered with formulation development of new chemical entities, as it can lead to slow drug absorption, inadequate and variable bioavailability, and gastrointestinal mucosal toxicity. For orally administered drugs, solubility is a key rate-limiting parameter to achieve the desired concentration in systemic circulation for a pharmacological response. More than 40% of new chemical entities (NCEs) developed in the pharmaceutical industry are practically insoluble in water. [81]
How does solvent extraction work to isolate a solute?
Solvent extraction, or liquid-liquid extraction (LLE), is performed using two immiscible liquids to separate analytes from interferences by partitioning the sample between these two phases. Usually, one phase is aqueous (often the denser phase) and the second is an organic solvent (usually the lighter phase). More hydrophilic compounds prefer the polar aqueous phase, while more hydrophobic compounds will be found mainly in the organic solvent. The process relies on the equilibrium distribution of a compound between the two phases, quantified by its distribution constant (KD). [82]
K_D = C_o / C_aq
Where Co is the concentration of the analyte in the organic phase and Caq is its concentration in the aqueous phase. [83]
Troubleshooting Guides
Problem: Poor Solute Recovery in Single Extraction
| Possible Cause | Diagnostic Steps | Solution | Preventive Measures |
|---|---|---|---|
| Unfavorable Distribution Constant (KD) | Measure recovery at different pH values or with different solvents. | Perform multiple extractions with fresh solvent. | Select an organic solvent whose polarity matches the analyte. [82] |
| Incorrect pH for Ionizable Analytes | Check the pKa of the analyte and the pH of the aqueous phase. | For organic bases, buffer aqueous phase ≥1.5 pH units above its pKa to make it neutral. For organic acids, buffer ≥1.5 pH units below its pKa. [82] | Pre-plan the extraction pH based on the analyte's acid/base properties. |
| Solvent Miscibility Issues | Check for emulsion formation or a poorly defined interface. | Use a different, less miscible organic solvent (see Table 1). | Pre-saturate the aqueous solvent with the organic solvent to avoid volume changes. [82] |
Problem: Excessive Sample Turbidity Interfering with Analysis
| Possible Cause | Diagnostic Steps | Solution | Preventive Measures |
|---|---|---|---|
| High Concentration of Scattering Particles | Use turbidimetry or dynamic light scattering (DLS) to assess particle load. | For DLS analysis, use back-scattering detection (175°) and adjust the laser focus to minimize photon path length. [43] | Consider particle size reduction during sample prep to create a more stable suspension. [81] |
| Multiple Light Scattering Events | The sample appears cloudy/opaque; DLS correlation functions are poor. | Use instrument features that automatically determine the optimal scattering angle and laser focus position via transmittance analysis. [43] | For non-absorbing samples, use Multi-Wavelength Turbidimetry (MWT) to characterize structure via transmitted power. [3] |
| Presence of Interfering Matrix Components | The turbidity persists after attempted extraction. | Implement a two-step back-extraction to remove both acidic and neutral interferences. [82] | Use solid-phase extraction (SPE) with a multi-phase sorbent to clean up the sample before analysis. [84] |
Problem: Inefficient Removal of Matrix Interferences
| Possible Cause | Diagnostic Steps | Solution | Preventive Measures |
|---|---|---|---|
| Co-extraction of Interferences | Analyze both phases after extraction for target and impurity content. | Use a two-step back-extraction. First, extract the analyte into an organic phase to leave polar interferences in the aqueous phase. Then, back-extract with a fresh aqueous buffer to transfer the analyte back to the aqueous phase, leaving non-polar interferences in the organic phase. [82] | Plan a selective two-step extraction during method development. |
| Broad Spectrum of Interferences | The sample is complex (e.g., biological fluids, natural products). | Use a multi-phase SPE cleanup. For example, a combination of ENV+ and PHE sorbents has been shown to effectively retain a wide variety of nucleic acid adducts from urine. [84] | Select SPE sorbents based on the different chemical interactions needed to retain your target analytes. |
Detailed Experimental Protocols
Protocol 1: Standard Two-Step Acid/Base Back-Extraction for a Basic Analyte
Principle: This method separates a basic analyte from both acidic and neutral impurities by manipulating its ionization state across two extraction steps. [82]
Workflow:
Materials:
- Aqueous Sample: Contains the basic analyte (e.g., a primary amine).
- Organic Solvent: Dichloromethane or ethyl acetate (see Table 1 for selection).
- Basic Aqueous Buffer: (e.g., phosphate buffer pH 7-8, must be ≥1.5 pH units above the analyte's pKa).
- Acidic Aqueous Buffer: (e.g., phosphate buffer pH 2-3, must be ≤1.5 pH units below the analyte's pKa).
- Separatory Funnel or Centrifuge Tubes.
- pH Meter.
Step-by-Step Procedure:
- First Extraction (Remove Acidic Interferences): Transfer the aqueous sample containing the basic analyte to a separatory funnel. Adjust the pH to a value at least 1.5 units above the pKa of the basic analyte using the basic aqueous buffer. Add a volume of the selected organic solvent. Stopper the funnel and shake it vigorously with frequent venting. Allow the phases to separate completely. Drain the lower phase (whether it is aqueous or organic) and collect it. The basic analyte, now in its neutral form, should be in the organic phase, while ionized acidic compounds and other polar interferences remain in the aqueous phase, which is discarded.
- Back-Extraction (Remove Neutral Interferences): Transfer the organic phase (containing the basic analyte and neutral interferences) back into a clean separatory funnel. Add a fresh portion of the acidic aqueous buffer. Shake the funnel vigorously. The basic analyte will become protonated (ionized) and transfer into the acidic aqueous phase. Allow the phases to separate. Drain the phases. The purified, ionized basic analyte is now in the acidic aqueous phase, which is collected. The organic phase, containing the neutral interferences, is discarded.
- Analyte Recovery: The analyte can now be recovered from the aqueous phase, or the aqueous phase can be analyzed directly if compatible with the downstream analytical method (e.g., reversed-phase HPLC).
Protocol 2: Dispersive Liquid-Liquid Microextraction (DLLME) for Analyte Enrichment
Principle: This miniaturized extraction technique uses a three-component solvent system to rapidly form a cloud of fine organic solvent droplets within an aqueous sample, providing a very large surface area for rapid extraction and significant analyte concentration. [82]
Workflow:
Materials:
- Extraction Solvent: A water-immiscible solvent heavier than water (e.g., ~8 µL of tetrachloroethylene). [82]
- Disperser Solvent: A solvent miscible with both the extraction solvent and water (e.g., ~1 mL of acetone or methanol). [82]
- Aqueous Sample: Approximately 5 mL volume.
- Syringe: For rapid injection.
- Centrifuge Tubes.
- Centrifuge.
Step-by-Step Procedure:
- Injection: Place the aqueous sample (approx. 5 mL) into a centrifuge tube. Rapidly inject a mixture containing the disperser solvent (e.g., 1 mL acetone) and the extraction solvent (e.g., 8 µL tetrachloroethylene) into the aqueous sample using a syringe.
- Formation of Cloudy Solution: The rapid injection creates a "cloudy solution," which consists of very fine droplets of the extraction solvent dispersed throughout the aqueous phase. This provides an enormous surface area for extraction, making the process nearly instantaneous.
- Centrifugation: Centrifuge the tube for a few minutes. This causes the fine droplets of the dense extraction solvent to coalesce and form a sedimented droplet at the bottom of the tube.
- Sample Collection: The sedimented organic phase (now containing the concentrated analyte) is collected using a micro-syringe for subsequent analysis. Because the volume of the extraction solvent is very small, a high degree of analyte concentration is achieved.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function & Application in Extraction |
|---|---|
| Dichloromethane (DCM) | A common organic extraction solvent, denser than water. Useful for extracting medium-polarity compounds. [82] |
| Ethyl Acetate | A common organic extraction solvent, less dense than water. Good for a wide range of medium-polarity analytes. [82] |
| Hexane | A very non-polar solvent. Used for extracting non-polar compounds, often blended with more polar solvents to adjust polarity. [82] |
| ENV+ & PHE SPE Sorbents | A solid-phase extraction (SPE) sorbent combination shown to effectively retain a wide variety of nucleic acid adducts from urine, useful for cleaning complex samples. [84] |
| AllPrep Kit | A dual DNA/RNA co-extraction kit. Allows for the simultaneous extraction of both nucleic acids from a single sample, preserving limited sample material. [85] |
| Sodium Sulfate | A neutral salt used for "salting out." Adding it to the aqueous phase decreases the solubility of the analyte, driving it into the organic phase and improving recovery. [82] |
| Ion-Pair Reagents | Added to the organic phase to form a neutral, extractable complex with an ionized analyte, allowing its transfer into the organic phase. [82] |
| Tetrachloroethylene | A typical extraction solvent used in DLLME because it is heavier than water and has low solubility in it. [82] |
Frequently Asked Questions (FAQs)
Q1: How do I choose the best organic solvent for my extraction? The ideal organic solvent should have low solubility in water (<10%), high volatility for easy removal, be compatible with your detection method (e.g., not a strong UV absorber for HPLC-UV), and be of high purity. Most importantly, its polarity should match that of your target analyte to maximize KD. You can optimize by blending two solvents of different polarity (e.g., hexane and chloroform) and measuring KD at different blend ratios. [82]
Q2: My sample is very turbid after extraction. Will this affect my DLS analysis, and how can I mitigate it? Yes, turbidity can cause multiple scattering events in DLS, leading to measurement errors. To mitigate this, use a DLS instrument with back-scattering detection (at 175°) and adjust the laser focus position close to the cuvette wall to minimize the photon path length through the sample. Advanced instruments can automatically determine the best angle and focus position via transmittance analysis. [43]
Q3: When should I use a two-step back-extraction instead of a single extraction? A two-step back-extraction is highly recommended when you need to separate your analyte from multiple types of interferences (e.g., both acidic and neutral compounds). A single extraction can typically remove only one class of interference, while a two-step process provides a much higher degree of purification. [82]
Q4: What is the advantage of Dispersive Liquid-Liquid Microextraction (DLLME) over classical LLE? DLLME is much faster, uses microliter volumes of solvents (making it environmentally friendly and cost-effective), and achieves very high enrichment factors due to the extremely high phase ratio between the sample and the extraction solvent. The formation of fine droplets makes the extraction process very efficient. [82]
Q5: How can I handle very small distribution constants (KD)? If KD is very small, multiple extractions with fresh solvent are more efficient than a single extraction with a large volume. For extremely small KD values or large sample volumes, continuous liquid-liquid extraction, where fresh solvent is continuously recycled through the sample, or countercurrent distribution apparatus may be necessary. [82]
In drug development, the integrity of your sample preparation process is foundational to generating reliable and reproducible data. Two particularly prevalent challenges—incomplete API extraction and the moisture absorption by hygroscopic APIs—can directly compromise your results by altering solution composition, stability, and optical properties. This guide provides targeted troubleshooting advice to help you identify, resolve, and prevent these issues, ensuring the accuracy of your research within the critical context of managing sample turbidity and light scattering in drug solutions.
Troubleshooting Guides
FAQ: Incomplete API Extraction
Q: What are the common signs of incomplete API extraction during sample preparation?
Incomplete extraction can manifest as lower-than-expected yield, inconsistent results between replicates, and unexpected turbidity in the final solution, which interferes with subsequent light scattering analyses [86].
Q: How can I improve the extraction efficiency of my API?
To enhance extraction efficiency, ensure you are using the correct solvent and that the API is fully soluble in it. Verify the extraction time and temperature, as some compounds require prolonged mixing or specific thermal conditions. Techniques like sonication or using a homogenizer can also help break down the matrix and improve yield [86].
FAQ: Moisture Absorption by Hygroscopic APIs
Q: Why are hygroscopic APIs a problem in pharmaceutical development?
Hygroscopic APIs absorb moisture from the ambient air, which can lead to a range of issues including physical instability (clumping, reduced flowability), chemical degradation of the active ingredient, and an increased risk of microbial contamination. These changes can directly impact the drug's quality, stability, and efficacy [87].
Q: What are the visible signs that my hygroscopic API has absorbed too much moisture?
The most common signs are clumping or caking of the powder, which leads to poor flowability. You may also observe difficulties in achieving consistent dosing during capsule filling. In solution, absorbed moisture can sometimes contribute to increased turbidity [87].
Q: How can I prevent moisture absorption during storage and handling?
Prevention requires a multi-pronged approach:
- Environmental Control: Maintain low humidity in production and storage areas using dehumidifiers and climate control systems [87].
- Proper Packaging: Use packaging materials with high moisture-barrier properties, such as aluminum blister packs or foil pouches. Including desiccants like silica gel or calcium chloride in the packaging can actively maintain a dry environment [88] [87].
- Formulation Strategies: Where possible, select low-hygroscopicity excipients. Techniques like granulation or applying moisture-resistant coatings to the powder can also offer protection [87].
Q: How does moisture absorption relate to sample turbidity in my research?
When a hygroscopic powder clumps due to moisture, it may not dissolve completely during the preparation of a drug solution. These undissolved particles can scatter light, leading to increased turbidity. This turbidity can interfere with analytical techniques like Dynamic Light Scattering (DLS) or UV-Vis spectroscopy, leading to inaccurate particle size measurements or concentration readings [43] [77].
Data Presentation
Quantitative Data on Desiccant Performance
The table below compares common desiccants used to protect hygroscopic materials, based on data from real-world (field) conditions. Calcium chloride is particularly effective for controlling humidity in enclosed spaces like shipping containers [88].
| Desiccant Type | Moisture Absorption Capacity (at 90% RH, Field Conditions) | Key Characteristics |
|---|---|---|
| Calcium Chloride (94% purity) | Up to 250% of its own weight [88] | High capacity; cost-effective for controlling humidity in large spaces. |
| Silica Gel | Information not specified in search results | Commonly used in small packaging; can be regenerated. |
| Clay | Information not specified in search results | Lower absorption capacity; less effective than calcium chloride. |
Common Laboratory Errors and Consequences
This table summarizes frequent sample preparation errors and their potential impact on your research, emphasizing the link to turbidity and data integrity.
| Error Type | Consequence | Impact on Research & Turbidity |
|---|---|---|
| Inaccurate Measurement [86] | Incorrect concentration of solutions; flawed standard curves. | Leads to invalid results; particles from undissolved powder can cause light scattering [77]. |
| Cross-Contamination [86] | Introduction of foreign substances or analytes. | Compromises sample purity; foreign particles increase turbidity and interfere with analysis. |
| Improper Handling of Hygroscopic Materials [87] | Powder clumping, chemical degradation, altered flowability. | Undissolved clumps act as particulates, increasing turbidity and leading to unreliable DLS or HPLC data [89]. |
Experimental Protocols
Protocol 1: Testing the Hygroscopicity of an API
This methodology helps you evaluate your API's sensitivity to moisture and determine appropriate handling and storage conditions.
1. Objective: To determine the tendency of a given API to absorb moisture from the atmosphere under controlled humidity conditions.
2. Materials:
- API powder sample
- Analytical balance (high precision)
- Desiccator with a saturated salt solution to create a specific relative humidity (RH) environment
- Oven or vacuum oven for drying
- Aluminum weighing dishes
3. Procedure:
- Step 1: Dry the sample. Pre-dry a portion of the API in an oven or vacuum oven to establish a dry weight baseline.
- Step 2: Initial weighing. Accurately weigh the pre-dried powder (record as W_dry) in a pre-weighed dish.
- Step 3: Exposure. Place the sample in a desiccator maintained at a specific, elevated RH (e.g., 75% RH) and a constant temperature.
- Step 4: Monitor weight gain. Remove and weigh the sample at regular intervals until a constant weight is achieved (Equilibrium Moisture Content, EMC). Record the final weight as W_final [88].
- Step 5: Calculation. Calculate the percentage moisture uptake as:
[(W_final - W_dry) / W_dry] * 100.
Protocol 2: Assessing the Impact of Moisture on Solution Turbidity
This protocol assesses how moisture-induced degradation or clumping affects the clarity of your drug solution, which is critical for light-based analytical techniques.
1. Objective: To quantify the turbidity of an API solution prepared from a moisture-exposed sample versus a protected control.
2. Materials:
- Hygroscopic API sample (moisture-exposed and protected)
- Appropriate solvent
- UV-Vis spectrophotometer or dedicated turbidimeter
- Cuvettes
3. Procedure:
- Step 1: Sample preparation. Prepare solutions of the API at the same concentration from both the moisture-exposed powder and a control sample stored with desiccants.
- Step 2: Turbidity measurement. Using a spectrophotometer, measure the absorbance of the solutions at a wavelength where the API does not absorb (often in the near-infrared range, e.g., 600-700 nm). This absorbance is directly related to the turbidity caused by light scattering from suspended particles [77]. Alternatively, use a turbidimeter to measure in Nephelometric Turbidity Units (NTU).
- Step 3: Analysis. A significantly higher absorbance (or NTU value) in the solution made from the moisture-exposed sample indicates increased turbidity due to incomplete dissolution or the formation of degradation aggregates.
The Scientist's Toolkit
Key Research Reagent Solutions
This table lists essential materials for managing hygroscopic APIs and mitigating turbidity in your experiments.
| Item | Function/Benefit |
|---|---|
| Desiccants (e.g., Calcium Chloride, Silica Gel) | Absorb ambient moisture inside storage containers, protecting hygroscopic materials during storage and transport [88] [87]. |
| Moisture-Barrier Packaging (Aluminum Foil Pouches) | Provides a physical barrier against environmental humidity, maintaining the stability of sensitive APIs [87]. |
| Dehumidifier | Controls the relative humidity in larger storage and processing areas, creating a stable macro-environment [87]. |
| Anti-Caking Agents (e.g., Magnesium Stearate) | Improves the flowability of powders that tend to clump, aiding in accurate weighing and handling [87]. |
| UV-Vis Spectrophotometer | A key instrument for quantifying sample turbidity by measuring light absorption or scattering at non-analyte-absorbing wavelengths [77] [89]. |
In drug development research, managing sample turbidity and light scattering is paramount for obtaining accurate analytical results. Turbidity, often caused by suspended particles or incomplete dissolution, can severely interfere with spectroscopic methods and compromise data integrity. The choice of extraction and mixing method—sonication, shaking, or vortex mixing—directly influences particle size distribution, suspension homogeneity, and ultimately, solution clarity. This guide provides troubleshooting and methodological support for researchers navigating these critical sample preparation decisions to optimize drug solution properties.
Method Comparison & Selection Guide
The table below summarizes the core characteristics of each mixing method to guide your initial selection based on application needs.
| Parameter | Sonication | Orbital Shaking | Vortex Mixing |
|---|---|---|---|
| Principle of Operation | Uses high-frequency sound waves to create cavitation, generating intense local shear forces and turbulence [90] [91]. | Moves samples in a circular, orbital motion for gentle, uniform agitation over a platform [92] [93]. | Creates a rapid, localized swirling motion (vortex) via a motor-driven rotating cup head or platform [92] [93]. |
| Primary Mechanism | Acoustic cavitation (formation and collapse of bubbles) [90]. | Circular orbital motion for consistent mixing [93]. | Vigorous circulatory motion creating a whirlpool effect [92]. |
| Mixing Intensity | Very high; can disrupt cellular structures and protein aggregates [91]. | Low to moderate, gentle [93]. | High, intense, and localized [93]. |
| Typical Sample Volume | Wide range (mL to L), depends on horn/bath size. | Large volumes (flasks, bottles); suitable for bulk processing [92]. | Small volumes (test tubes, vials); typically under a few mL per tube [92] [93]. |
| Optimal Use Cases | Nanoemulsion formulation [94], particle size reduction [91], disrupting tough cells, enhancing drug release from microbubbles [90]. | Cell culture [93], long-term chemical reactions [93], solubility studies [92]. | Rapid homogenization of small volumes [93], resuspending pellets [93], mixing reagents before analysis [92]. |
| Impact on Turbidity | Can significantly reduce turbidity by breaking down large particles into nano-scale emulsions [94]. | Provides gentle mixing that can help suspend particles uniformly, but may not break up aggregates. | Excellent for quick, thorough homogenization to create a uniform suspension from a pellet. |
Workflow for Method Selection
The following diagram outlines a decision-making workflow to select the appropriate method based on your sample characteristics and research goals, particularly for managing turbidity in drug solutions.
Troubleshooting Guides
Sonication Troubleshooting
| Problem | Possible Root Cause | Solution |
|---|---|---|
| High Sample Turbidity Post-Sonication | Insufficient energy input; incorrect parameters. | Increase sonication amplitude/time. Ensure the probe is immersed correctly. For nanoemulsions, target parameters that yield droplets <200 nm for clarity [94]. |
| Overheating Sample | Prolonged sonication or high intensity without cooling. | Use short pulses (e.g., 10-30 sec on/off). Place sample tube in an ice bath during sonication. |
| Foaming or Loss of Material | Introduction of excess air from the sample being too close to the surface. | Immerse the probe deeper into the liquid, but not touching the bottom of the tube. |
| Low Drug Release Efficiency | Sub-optimal resonance frequency for cavitation of drug-loaded clusters [90]. | For clustered microbubbles, use "on-resonance" low-frequency US (e.g., ~100 kHz) to maximize payload release (up to 93% efficiency) [90]. |
Shaking Troubleshooting
| Problem | Possible Root Cause | Solution |
|---|---|---|
| Poor Solubility/ Persistent Turbidity | Insufficient mixing intensity to dissolve drug aggregates. | Increase shaking speed or switch to a more vigorous method (vortex or sonication) for initial dispersion. |
| Cell Viability Issues in Culture | Shaking speed too high, causing shear stress. | Reduce the shaking speed to a gentler range (e.g., 100-200 rpm for sensitive cells) [93]. |
| Condensation/Evaporation in Sealed Vessels | Temperature fluctuation in incubator shakers. | Ensure temperature is stable and vessels are properly sealed. Use non-heated shaking for room temperature protocols. |
| Inconsistent Results Across Platform | Load is uneven or exceeds weight capacity, affecting motion. | Balance the load on the platform and do not exceed the shaker's maximum weight capacity [92]. |
Vortex Mixing Troubleshooting
| Problem | Possible Root Cause | Solution |
|---|---|---|
| Sample Not Homogenized | Low speed setting or viscous sample. | Increase the speed. For very viscous samples, use a pulsed mode or consider sonication. |
| Liquid Splashing or Leaking | Excessive speed for the tube size and volume. | Reduce speed. Ensure the cap is secure. Avoid overfilling the tube. |
| Inefficient Mixing of Pellet | Pellet is too tight or not dislodged from tube bottom. | Gently tap the tube to dislodge the pellet before starting the vortex. Use a touch-sensitive mode for better control. |
| Cannot Process Multiple Samples | Using a single-tube vortex mixer with a rubber cup [92]. | Transfer to a multi-tube vortex mixer with a platform that can hold tube racks for higher throughput [92]. |
Frequently Asked Questions (FAQs)
Q1: Which method is most effective for reducing turbidity in a lipid-based drug solution? For fundamental reduction of turbidity, sonication is the most effective method. It uses cavitation to break down large lipid droplets into a nanoemulsion, significantly reducing particle size and scattering. For example, optimized sonication can produce avocado oil nanoemulsions with a droplet size of ~68 nm and low polydispersity, resulting in a clear and stable formulation [94].
Q2: Can vortex mixing be used for sample dissolution, not just homogenization? Yes, for readily soluble compounds in small volumes, vortex mixing is excellent for rapid dissolution. However, for compounds that tend to form aggregates or have poor solubility, the intense but localized shear may be insufficient. In such cases, sonication is the preferred method to break apart tough aggregates and promote complete dissolution.
Q3: How does the choice of method impact the stability of my drug solution? The method directly impacts physical stability. Sonication can create very stable nanoemulsions with minimal sedimentation or creaming [94]. Vortex mixing provides immediate homogeneity but may not prevent separation over time if particles are large. Orbital shaking is gentle and may not be sufficient to disrupt aggregates that lead to instability. Monitoring particle size and zeta potential (a measure of surface charge) is crucial for stability; sonication often yields a high zeta potential (e.g., > |50| mV), which promotes physical stability by preventing aggregation [94].
Q4: We are preparing samples for HPLC analysis and need to ensure they are perfectly clear. What is the best workflow? A recommended workflow is:
- Initial Dissolution: Dissolve the drug in the appropriate solvent.
- Primary Homogenization: Use vigorous vortex mixing for 30-60 seconds to ensure initial suspension.
- Clarity Enhancement: If the solution remains turbid, subject it to brief sonication (e.g., 1-2 minutes in a bath sonicator or 30 seconds with a probe at medium power) to disrupt sub-visible aggregates.
- Final Filtration: Pass the solution through a 0.22 µm or 0.45 µm membrane filter directly into an HPLC vial to remove any remaining particulate matter. This combined approach ensures a clear sample, protects your HPLC column, and provides accurate results.
Experimental Protocols
Detailed Protocol: Preparing a Stable Nanoemulsion via Sonication
This protocol is adapted from research on ultrasound-assisted nanoemulsions for drug delivery applications [94].
Objective: To formulate a stable oil-in-water nanoemulsion with minimal turbidity and droplet size below 200 nm.
Research Reagent Solutions & Key Materials:
| Reagent/Material | Function in the Experiment |
|---|---|
| Active Pharmaceutical Ingredient (API) or Oil (e.g., Avocado Oil [94]) | The core lipophilic compound or drug carrier to be emulsified. |
| Surfactants (e.g., PEG 40 Hydrogenated Castor Oil, Span 80 [94]) | Stabilize the oil-water interface, reduce surface tension, and prevent droplet coalescence. |
| Aqueous Phase (e.g., Deionized Water, Buffer) | The continuous phase of the emulsion. |
| Ultrasonic Processor (e.g., probe sonicator) | Provides high-intensity ultrasound energy to break down macroemulsions into nanoemulsions. |
Methodology:
- Formulate Pre-mix: Combine 8% (w/v) oil (e.g., avocado oil), 7.5% (w/v) PEG 40 hydrogenated castor oil, and 2.5% (w/v) Span 80 with your aqueous phase to 100% [94]. Use a magnetic stirrer or vortex mixer to create a coarse macroemulsion.
- Set Sonication Parameters: Set the ultrasonic processor to an amplitude of 80-90% of maximum power. Use a pulsed cycle (e.g., 30 seconds on, 10 seconds off) to manage heat generation.
- Sonication: Immerse the probe tip into the coarse emulsion. Sonicate for a total time of 5-10 minutes, keeping the sample in an ice bath to dissipate heat.
- Characterization:
- Droplet Size & PDI: Analyze the final nanoemulsion using dynamic light scattering (DLS). A successful formulation, like PS21, will have a small droplet size (~68 nm) and a low Polydispersity Index (PDI < 0.3) [94].
- Zeta Potential: Measure the surface charge. A high zeta potential (e.g., > |55| mV) indicates good electrostatic stability [94].
- Turbidity: Use a UV-Vis spectrophotometer to monitor absorbance at 600 nm; a decrease indicates reduced light scattering and turbidity [94].
Detailed Protocol: Combining Vortex and Sonication for Protein Modification
This protocol leverages the synergistic effects of two physical methods to modify protein structures, which can be useful for optimizing drug formulations involving protein-based APIs [91].
Objective: To synergistically modify the structure of a protein (e.g., Soy Protein Isolate) to improve its functional properties.
Methodology:
- Sample Preparation: Prepare a 15 mg/mL suspension of the protein in deionized water. Stir for 2 hours at room temperature to ensure hydration [91].
- Primary Sonication Treatment: Subject the hydrated solution to bath ultrasonication. Use a frequency of 40 kHz and a power of 220 W. Treat the sample for 30 minutes at 25 ± 2°C [91].
- Secondary Vortex Fluidic Device (VFD) Treatment: Immediately process the sonicated sample using a VFD (a high-shear vortex mixer) in continuous flow mode. Use a rotational speed of 8000 rpm, a flow rate of 0.3 mL/min, and a tube inclination angle of 45° [91].
- Characterization:
- Particle Size: Analyze via DLS. The combined US30VFD8000 treatment is expected to result in a particle size of ~760 nm, indicating modified aggregation [91].
- Structural Analysis: Use FTIR to quantify changes in secondary structure, such as a ~7.4% increase in β-sheet content [91].
- Thermal Stability: Use Differential Scanning Calorimetry (DSC) to measure changes in denaturation temperature [91].
Core Safety Principles and Definitions
What defines a High-Potency Active Pharmaceutical Ingredient (HPAPI)?
A compound is typically classified as highly potent if it meets one or more of the following criteria [95] [96]:
- An Occupational Exposure Limit (OEL) below 10 µg/m³ (eight-hour time-weighted average) [95].
- It produces a therapeutic effect at a very low dose, generally at or below 150 µg/kg of body weight or a daily dose of less than 1 mg [95].
- It exhibits high pharmacological selectivity and potency, meaning it can cause adverse effects like cancer, genetic mutations, or developmental defects at very low exposure levels [95].
Why is specialized handling required for HPAPIs?
The high biological activity of HPAPIs means that even minimal exposure through inhalation or skin contact can pose significant health risks to personnel. Therefore, the primary goal of handling procedures is to minimize occupational exposure and prevent cross-contamination with other products [95] [96].
Troubleshooting Guides for Common Handling Issues
FAQ: What is the first step in handling a new API when its potency is not fully characterized?
Until sufficient toxicological data is available, a new API should be treated as highly potent. It is safer to begin with conservative, stringent controls during early development and potentially relax them later if data confirms lower potency, rather than risking operator exposure [95].
FAQ: How do we determine the level of containment and personal protective equipment (PPE) needed for a specific HPAPI?
The required controls are determined by a risk assessment that considers both the hazard (the API's OEL) and the potential for exposure. Exposure is influenced by the physical form of the material (e.g., dry and dusty powders present a higher risk), the concentration of the API in the formulation, the handling volumes, and whether operations are open or contained [95].
Troubleshooting Guide: Contamination Control During Weighing
| Problem | Possible Root Cause | Recommended Solution |
|---|---|---|
| Visible powder residue on balance or workbench after weighing. | Inadequate cleaning between operations; failure of containment during transfer. | Use rigid isolators or gloveboxes for all weighing. Implement rigorous cleaning validation protocols with swab testing. Use closed transfer systems [95] [96]. |
| High background particle counts in room air samples. | Failure of room pressure cascades; inadequate HVAC filtration; poor gowning procedures. | Ensure facility uses 100% air renewal (no recirculation) and HEPA filtration. Maintain negative pressure in the weighing suite relative to corridors. Verify personnel are trained in proper gowning [95] [96]. |
| Consistent operator exposure readings during OEL monitoring. | PPE is inadequate for the potency band; isolator integrity is compromised. | Re-evaluate the HPAPI's OEL band. Upgrade to powered air-purifying respirators (PAPR). Perform integrity checks on isolators and gloveboxes [96]. |
Troubleshooting Guide: Sample Analysis and Turbidity Issues
| Problem | Possible Root Cause | Recommended Solution |
|---|---|---|
| Unable to measure particle size in a turbid HPAPI solution using standard Dynamic Light Scattering (DLS). | Multiple scattering or strong light absorption in the concentrated solution interferes with measurement. | Use a confocal DLS microscope designed for turbid samples, which eliminates multiple scattering effects. Alternatively, dilute the sample if compatible with the analysis, though this may not reflect the native state [97]. |
| Drug precipitation occurs during solubility or supersaturation studies, complicating data interpretation. | The supersaturated state is thermodynamically unstable and prone to precipitation. | Screen for precipitation inhibitors (e.g., certain polymers). Use high-throughput microtiter plate-based methods (laser scattering or turbidity) to quickly rank-order effective excipients that inhibit precipitation [1]. |
| Inconsistent turbidity readings in a time-dependent precipitation study. | Manual sampling and offline analysis introduce variability and prevent continuous monitoring. | Employ in-situ microtiter plate readers that continuously monitor light scattering or turbidity, allowing for real-time, high-throughput analysis without disruptive sample preparation [1]. |
Detailed Experimental Protocols
Protocol 1: Safe Weighing and Dispensing of HPAPIs Using the Double Barrier Principle
Principle: To ensure operator safety by maintaining at least two protective barriers between the operator and the HPAPI at all times [95].
Methodology:
- Facility and Equipment Preparation: Perform all operations within an isolator or glovebox (Barrier 1) located in an EU GMP Class C (or equivalent ISO 7) cleanroom. Ensure the room maintains a negative pressure cascade.
- Personal Protective Equipment (PPE): Don appropriate PPE before entering the area. This typically includes a coverall, gloves, and a Powered Air-Purifying Respirator (PAPR) (Barrier 2) [95] [96].
- Material Transfer: Introduce and remove materials from the isolator using sealed bags or closed containers through designated pass-through hatches.
- Weighing Procedure:
- Tare the receiving vessel inside the isolator.
- Carefully transfer the required amount of HPAPI from the primary container to the vessel.
- Seal the vessel securely before removing it from the isolator.
- Post-Operation: Clean all surfaces within the isolator and pass-throughs using validated cleaning agents. Treat all waste, including gloves and wipes, as hazardous and dispose of via incineration [95].
Protocol 2: Monitoring Drug Precipitation via a Light Scattering Microtiter Plate Assay
Principle: To high-throughput screen for excipients that inhibit the precipitation of a poorly soluble drug from a supersaturated solution by continuously monitoring the formation of precipitate particles [1].
Methodology:
- Reagent Preparation:
- Prepare a supersaturated solution of the model drug (e.g., fenofibrate or dipyridamole) in a suitable buffer (e.g., McIlvaine buffer, pH 6.8).
- Prepare aqueous solutions of various candidate precipitation inhibitors (excipients).
- Plate Setup:
- In a microtiter plate, mix the drug solution with the different excipient solutions.
- Include a control well containing only the drug solution without inhibitor.
- Measurement:
- Immediately place the plate in a plate reader capable of measuring laser light scattering or turbidity.
- Continuously monitor the signal (e.g., scattered light intensity or optical density) for a predetermined period (e.g., 60-90 minutes).
- Data Analysis:
- Calculate the area under the curve (AUC) for the scattered light signal over the measurement period (AUC100). A higher AUC100 indicates more precipitation, while a lower AUC100 indicates effective inhibition.
- Rank-order the efficacy of excipients based on their AUC100 values compared to the control [1].
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function / Explanation |
|---|---|
| Containment Isolator/Glovebox | A sealed, rigid enclosure with attached gloves, providing the primary physical barrier between the operator and the HPAPI during weighing and dispensing operations [95]. |
| Powered Air-Purifying Respirator (PAPR) | Personal protective equipment that provides a continuous flow of filtered air to the user, offering a high level of respiratory protection against airborne potent compounds [96]. |
| High-Efficiency Particulate Air (HEPA) Filter | A critical component of the facility's HVAC system that captures at least 99.97% of airborne particles, preventing the escape of HPAPI particles from the containment zone [96]. |
| Precipitation Inhibitors (e.g., Polymers like HPMC, PVP) | Excipients added to formulations to prolong the supersaturated state of a drug by inhibiting nucleation and crystal growth, thereby improving oral bioavailability [1]. |
| Confocal Dynamic Light Scattering (DLS) Microscope | An advanced instrument that uses a confocal optical system to measure the particle size distribution in turbid, concentrated solutions without requiring dilution, overcoming the limitations of conventional DLS [97]. |
| Laser Scattering Microtiter Plate Reader | A high-throughput instrument that enables continuous, in-situ monitoring of drug precipitation by detecting scattered light, facilitating rapid screening of formulation components [1]. |
| Occupational Exposure Limit (OEL) | The maximum allowable concentration of an HPAPI in the air for a defined time period, serving as the foundational metric for conducting risk assessments and designing containment strategies [95] [96]. |
Workflow and Process Diagrams
HPAPI Handling Safety Decision Workflow
High-Throughput Precipitation Inhibition Assay
Validation, Regulatory Compliance, and Technique Comparison for Robust Analytical Methods
Validating an analytical method for turbidity measurements is essential for ensuring the reliability, accuracy, and reproducibility of your data in pharmaceutical research. While the ICH Q2(R1) guideline does not explicitly mention turbidity measurements, its fundamental principles of accuracy, precision, and specificity provide a robust framework for validating these methods. Turbidity measurement is a physical technique that quantifies the cloudiness or haziness of a fluid caused by suspended particles, typically using nephelometers that measure scattered light at 90 degrees to the incident beam. In the context of drug development, managing sample turbidity is critical for formulations containing nanoparticles, proteins, or other colloidal systems where particle size and aggregation can significantly impact product quality, stability, and performance.
This technical support guide will help you navigate the validation process for turbidity methods, addressing common challenges and providing troubleshooting advice to ensure your methods meet regulatory standards.
Core Validation Parameters for Turbidity Measurements
Accuracy
Accuracy expresses the closeness of agreement between the measured turbidity value and the true value. For turbidity measurements, this is typically demonstrated through recovery studies using appropriate standard reference materials.
Experimental Protocol for Accuracy Determination:
- Prepare a dilution series of standardized turbidity standards (e.g., formazin or traceable commercial standards) across the intended range of your method.
- Measure each concentration in triplicate using your turbidimeter.
- Calculate the percent recovery for each measurement using the formula:
- Recovery (%) = (Measured Value / True Value) × 100
- The mean recovery should ideally be between 98% and 102%, demonstrating good accuracy.
Table: Example Accuracy Data for Turbidity Method Validation
| True Value (NTU) | Measured Value (NTU) | Recovery (%) | Acceptance Criteria |
|---|---|---|---|
| 1.0 | 0.98, 1.01, 0.99 | 99.3 ± 1.5 | 90-110% |
| 10.0 | 9.95, 10.10, 9.87 | 99.7 ± 1.2 | 95-105% |
| 100.0 | 98.5, 101.2, 99.8 | 99.8 ± 1.3 | 98-102% |
Precision
Precision refers to the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions. It is evaluated at repeatability (intra-assay) and intermediate precision (inter-day, inter-analyst) levels.
Experimental Protocol for Precision Determination:
- Repeatability: Prepare a homogeneous sample at three levels (low, mid, and high turbidity). Measure each sample six times in a single session.
- Intermediate Precision: Repeat the repeatability study on a different day, with a different analyst if possible, using a different lot of standard if applicable.
- Calculate the Relative Standard Deviation (RSD%) for each data set:
- RSD% = (Standard Deviation / Mean) × 100
- Acceptance criteria depend on the turbidity level but typically, an RSD of <5% for mid to high levels and <10% for low levels near the limit of quantitation is acceptable.
Table: Example Precision Data for Turbidity Method Validation
| Precision Level | Sample (NTU) | Mean (NTU) | Standard Deviation (NTU) | RSD% | Acceptance Criteria (RSD%) |
|---|---|---|---|---|---|
| Repeatability | Low (1.0) | 1.02 | 0.05 | 4.9 | < 10% |
| Repeatability | Mid (10.0) | 9.98 | 0.21 | 2.1 | < 5% |
| Intermediate Precision | Mid (10.0) | 10.05 | 0.29 | 2.9 | < 5% |
Specificity
Specificity is the ability to assess unequivocally the analyte (turbidity caused by the target particles) in the presence of components that may be expected to be present, such as impurities, degradants, or matrix components. For turbidity, this ensures that the measured signal is due to the particles of interest and not colored interferents or air bubbles.
Experimental Protocol for Specificity Determination:
- Measure the turbidity of your sample buffer or placebo formulation (without the active particles).
- Measure the turbidity of your final nanoparticle or drug formulation.
- The signal from the buffer/placebo should be negligible compared to the sample. A suitable acceptance criterion is that the blank signal is less than the Limit of Detection (LOD) for the method.
- To test for interference from color, measure a colored solution (e.g., with a dye) with and without particles. The difference in measured turbidity should be minimal if the instrument is properly calibrated and uses an infrared light source, which is less sensitive to color interference compared to white light [98].
The Scientist's Toolkit: Essential Materials for Turbidity Analysis
Table: Key Research Reagent Solutions and Materials
| Item | Function & Importance |
|---|---|
| Primary Turbidity Standards | Formazin or traceable polymer-based standards (e.g., from AMCO Clear or StablCal). Used for initial instrument calibration to establish the measurement scale [98]. |
| Secondary/Validation Standards | Pre-characterized, stable standards of known turbidity value. Used for daily verification of instrument calibration and accuracy checks during method validation [98]. |
| Silicone Oil | Used to mask minor scratches on glass sample vials. Scratches can scatter light, leading to falsely high readings. A few drops wiped on the vial exterior with a lint-free cloth eliminates this error [98]. |
| Lint-Free Wipes | Essential for cleaning sample vials without introducing fibers or scratches. Any dirt, dust, or fingerprints on the vial will scatter light and increase the measured turbidity [98]. |
| High-Purity Water & Filters | Water used for dilution or sample preparation must be particle-free (e.g., HPLC-grade water filtered through a 0.2 µm filter). Impurities contribute to background noise [14]. |
| Appropriate Sample Vials | High-quality, clear glass or optical plastic cuvettes/cells. Must be clean, unscratched, and dedicated to turbidity measurements to prevent contamination and signal artifacts. |
Troubleshooting Guides & FAQs
FAQ 1: Why is my turbidity reading higher than expected?
This is a common issue often related to sample preparation and handling.
- Cause: Contamination on the sample vial.
- Solution: Thoroughly clean the exterior of the vial with a lint-free cloth before measurement. Inspect for and replace any scratched or permanently stained vials [98].
- Cause: Presence of air microbubbles in the sample.
- Solution: Allow the sample to degas or use a brief, gentle centrifugation to remove bubbles before measurement.
- Cause: Inadequate calibration or drifting of the instrument.
- Solution: Regularly calibrate the turbidimeter using traceable standards and perform verification checks with a validation standard before measuring samples [98].
- Cause: Sample condensation on cold vials.
- Solution: Wipe down the sample vial thoroughly if condensation has formed, especially when measuring cold samples [98].
FAQ 2: How do I handle samples with color? My readings seem inaccurate.
Color can absorb light, leading to a lower scattering signal and an underestimation of turbidity.
- Solution: Use a turbidimeter with an infrared (IR) light source (ISO-compliant) instead of a white light source (EPA-compliant). Infrared light is less absorbed by sample color, providing more accurate results for colored solutions [98].
- Solution: If using a white light instrument is mandatory, the method should be validated to demonstrate that the color of the sample does not interfere with the accuracy of the turbidity measurement, as per the specificity requirement.
FAQ 3: My turbidity measurements are inconsistent. What could be wrong?
Poor precision often stems from instrumental or procedural inconsistencies.
- Cause: Inconsistent sample presentation (e.g., vial placement, vial rotation).
- Solution: Ensure the vial is placed in the same orientation in the sample chamber every time. Some instruments have markers for consistent positioning.
- Cause: Particle settling or aggregation during measurement.
- Solution: For samples that settle quickly, ensure a consistent mixing protocol prior to sampling and establish a strict time window for measurement after sample preparation.
- Cause: Instrument fluctuations or poor maintenance.
- Solution: Verify the instrument's stability by measuring a stable standard multiple times. Ensure the light source and detector are functioning correctly.
FAQ 4: How do I define the Limit of Detection (LOD) and Quantitation (LOQ) for a turbidity method?
While not always required for turbidity, LOD/LOQ can be useful for low-turbidity samples.
- LOD (Signal-to-Noise): Prepare a blank solution (particle-free buffer) and measure its signal. The LOD is the turbidity that yields a signal 3 times the standard deviation of the blank.
- LOQ (Signal-to-Noise): The LOQ is the turbidity that yields a signal 10 times the standard deviation of the blank. The LOQ should also be demonstrated to have acceptable precision (e.g., RSD < 10%) and accuracy [99].
Experimental Workflow for Validating a Turbidity Method
The following diagram illustrates the logical workflow for validating an analytical method for turbidity measurements, incorporating ICH Q2(R1) principles and key troubleshooting checks.
Ensuring Data Integrity and Regulatory Compliance in GxP Environments
Troubleshooting Guides
Guide 1: Troubleshooting Turbidity and Light Scattering Measurements
Problem: Inconsistent or Erratic Readings in Microtiter Plate-Based Assays
| Problem | Potential Cause | Solution |
|---|---|---|
| High data variability between replicates | Precipitate formation during sample handling or centrifugation [1] | Standardize and validate sample preparation steps; avoid manual centrifugation/filtration where possible [1]. |
| Discrepancy between light scattering and classical (HPLC/UV) data | Method not properly validated for your specific compound-excipient combination [1] | Correlate light scattering parameters (e.g., AUC100) with classical precipitation inhibition index (PIclassical) during method development [1]. |
| Poor signal-to-noise ratio | Instrument settings not optimized for compound or plate type [1] | Experimentally investigate and document instrumental settings (e.g., gain, threshold) for each new chemical entity [1]. |
| Suspected data integrity breach | Lack of immutable, system-generated audit trails for data changes [100] | Ensure audit trails are enabled, validated, and cannot be disabled for critical GxP data entries [100]. |
Guide 2: Addressing Common GxP Data Integrity Gaps
Problem: Audit Trail and Documentation Issues
| Problem | GxP Compliance Gap | Corrective Action |
|---|---|---|
| Shared user logins found on system | Violation of attributable principle (ALCOA+) [100] | Implement unique user IDs with role-based access controls; enforce via SOPs [100]. |
| No procedure for routine audit trail review | Failure to meet revised Annex 11 expectations [100] | Establish and train staff on an SOP for periodic audit trail review as part of data verification [100]. |
| Raw data files missing or not backed up | Violation of original and enduring principles [100] | Validate robust backup and data recovery procedures; ensure metadata is retained [100]. |
| Manual transcription errors in lab notebook | Violation of accurate and contemporaneous principles [101] | Automate data capture from instruments where possible; if manual entry is required, implement independent verification [101]. |
Frequently Asked Questions (FAQs)
Q1: Our drug formulation research uses a laser scattering microtiter plate method to screen precipitation inhibitors. Is this method acceptable under GxP, and how do we validate it?
A: Yes, it can be acceptable with proper validation. Research shows laser scattering microtiter plate-based methods can serve as a reliable "first screening line" when appropriately validated [1]. The validation should demonstrate that the method is fit for its intended purpose. This involves:
- Correlation with Classical Methods: You must correlate light scattering parameters with data from a classical method (e.g., HPLC quantification of dissolved drug). For instance, studies found that the area under the curve for light scattering (AUC100) showed an excellent correlation with the classical precipitation inhibition index [1].
- Defined Parameters: Establish and document predefined parameters (e.g., AUC100, OD max) that will be used for decision-making [1].
- Accuracy and Precision: Evaluate the method's accuracy, precision, and reliability to ensure it consistently produces reliable results [1].
Q2: What are the most critical data integrity principles we must follow in our laboratory's electronic notebook (ELN) and computerized systems?
A: The foundational principles are encapsulated by ALCOA+, which is mandatory under regulations like the revised EU Annex 11 [100]. All generated data must be:
- Attributable: Who created the data and when.
- Legible: Can the data be read?
- Contemporaneous: Was it recorded at the time of the activity?
- Original: Is this the first capture or a certified copy?
- Accurate: Does it reflect the actual observation?
The "+" adds further requirements:
- Complete: All data is present.
- Consistent: All elements are dated and sequenced properly.
- Enduring: Recorded for the lifetime of the product.
- Available: Can be accessed for review and inspection.
Q3: What is the difference between Computer System Validation (CSV) and Computer Software Assurance (CSA), and which should we use?
A: CSV is a traditional, often document-heavy approach to proving a system meets its requirements. In contrast, Computer Software Assurance (CSA) is a modern, risk-based approach that focuses on critical thinking and patient safety over exhaustive documentation [102].
- CSA is recommended for new systems and updates, especially with frequent software releases. It allows you to prioritize testing based on risk to product quality and patient safety, making the validation process more efficient and less burdensome while maintaining compliance [102].
Q4: We are setting up a new Dynamic Light Scattering (DLS) instrument for nanoparticle sizing. What are the key phases of the GxP validation process we must follow?
A: The GxP validation process for a new instrument or computerized system follows a structured lifecycle approach [102] [103]:
- Planning & Risk Assessment: Define the scope and perform a risk assessment (e.g., using FMEA).
- Requirements Specifications: Document what the system must do (User Requirements Specification (URS) and Functional Requirements Specification (FRS)).
- Design Qualification (DQ): Verify the supplier's design meets your requirements.
- Installation Qualification (IQ): Confirm the system is installed correctly in your environment.
- Operational Qualification (OQ): Verify that the system functions as intended across its expected operating ranges.
- Performance Qualification (PQ): Demonstrate the system performs consistently and reliably under actual operating conditions using your samples and methods.
Experimental Protocols & Data Presentation
Validating a Light Scattering Method for Precipitation Inhibition
This protocol is adapted from research evaluating light scattering as an alternative to classical methods for detecting excipient-mediated drug precipitation inhibition [1].
1. Detailed Methodology
- Reagents: Model poorly soluble compounds (e.g., Fenofibrate, Dipyridamole), various excipients (precipitation inhibitors), and suitable dissolution media (e.g., McIlvaine buffer at pH 6.8) [1].
- Instrumentation: A microtiter plate reader capable of measuring laser light scattering or turbidity (optical density).
- Preparation: An incubation plate and a reading plate are used. The drug is dissolved in an organic solvent and dispensed into the incubation plate. The solvent is then evaporated. The excipients (precipitation inhibitors) are dissolved in the dissolution medium and added to the reading plate [1].
- Supersaturation Generation: An aliquot from the reading plate is transferred to the incubation plate to dissolve the drug film, creating a supersaturated solution. This solution is then transferred back to the reading plate for measurement [1].
- Measurement: The laser scattering or turbidity (OD) is measured over time immediately after transferring the supersaturated solution. The classical method involves sampling at defined time points, followed by centrifugation, filtration, dilution, and quantification via HPLC [1].
2. Key Parameters for Validation
The table below summarizes quantitative parameters from the research that can be used to validate the light scattering method against the classical approach [1].
| Method | Key Parameter | Description | Correlation with Classical Method |
|---|---|---|---|
| Classical (HPLC/UV) | PIclassical | Precipitation Inhibition Index calculated from dissolved drug concentration over time. | Gold Standard |
| Laser Light Scattering | AUC100 | Area Under the Curve of the light scattering signal over 100 minutes. | Excellent correlation with PIclassical; chosen as most reliable [1]. |
| Turbidity (OD) | OD max | Maximum recorded Optical Density value. | Excellent correlation with PIclassical [1]. |
Research Reagent Solutions
The following table details key materials used in experiments for screening precipitation inhibitors using turbidity and light scattering techniques [1].
| Item | Function in the Experiment |
|---|---|
| Model Compounds (e.g., Fenofibrate) | Poorly soluble drugs used to test the efficacy of various precipitation inhibitors [1]. |
| Precipitation Inhibitors (Excipients) | Substances like polymers that help maintain a drug in a supersaturated state by inhibiting or slowing precipitation [1]. |
| McIlvaine Buffer (pH 6.8) | A biologically relevant dissolution medium used to simulate intestinal conditions for the supersaturation assay [1]. |
| Microtiter Plates | High-throughput platform for conducting multiple simultaneous assays with small volumes of reagents and compounds [1]. |
Workflow and Signaling Pathways
GxP Assay Validation Workflow
This workflow integrates the technical method development for a turbidity or light scattering assay with the mandatory GxP computer system validation process, ensuring data integrity from end-to-end.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for experiments involving light scattering techniques, along with their primary functions.
| Item | Function |
|---|---|
| Formazin Standards [104] [105] | Primary reference standard for instrument calibration, establishing a scale in Nephelometric Turbidity Units (NTU). |
| Antigen & Antibody Reagents [4] | Used in immunonephelometry and turbidimetry to form light-scattering immune complexes for quantification. |
| Particle-Free Distilled Water [4] [105] | Serves as a blank and for diluting samples and standards to prevent contamination from external particles. |
| Appropriate Buffer Solutions [106] [107] | Maintain sample pH and ionic strength, which is critical for stabilizing proteins and preventing unwanted aggregation. |
| High-Quality Microplates/Cuvettes [104] [7] | Sample containers with high optical quality; imperfections can scatter light and cause erroneous readings. |
Technical Comparison of Analytical Techniques
The table below summarizes the core principles, optimal application ranges, and key considerations for DLS, Nephelometry, and Turbidimetry to guide method selection.
| Feature | Dynamic Light Scattering (DLS) | Nephelometry | Turbidimetry |
|---|---|---|---|
| Measured Parameter | Fluctuations in scattered light intensity over time [107] | Intensity of scattered light (usually at 90°) [104] [108] | Intensity of transmitted light [104] [108] |
| Primary Output | Hydrodynamic size & size distribution; particle concentration [107] | Concentration of scattering particles [104] | Concentration of scattering particles [4] |
| Optimal Particle Size | 0.3 nm - 10 μm [107] | 0.1 - 1 μm [104] | Larger particles [104] |
| Optimal Concentration | Low to moderate (must avoid multiple scattering) [107] | Low concentrations [104] [108] | High concentrations [104] [108] |
| Key Advantages | Non-destructive, provides size data, rapid quantification [107] | High sensitivity for small particles at low concentrations [104] | Simple setup, robust for dense suspensions [104] |
| Common Applications in Drug Development | Viral particle quantification, protein aggregation studies, nanoparticle characterization [107] | Drug solubility screening, protein aggregation, immunonephelometry [104] [106] | Bacterial growth (cell density), high-concentration immunoassays [104] [4] |
Technique Selection Workflow
The following diagram outlines a logical workflow for selecting the most appropriate analytical technique based on your primary experimental question.
Troubleshooting Guides and FAQs
Frequently Asked Questions
What is the fundamental difference between nephelometry and turbidimetry? Nephelometry measures the intensity of light scattered by particles in a sample, typically at a 90-degree angle. In contrast, turbidimetry measures the reduction in intensity of light transmitted through the sample. Nephelometry is more sensitive for low concentrations of small particles, while turbidimetry is better suited for higher concentrations [104] [108].
My sample is highly opalescent. Which technique is most suitable for quantifying this in a high-concentration mAb formulation? For highly opalescent, concentrated samples like mAb formulations, microscale nephelometry is a promising technique. It can measure a wide dynamic range of nephelometric turbidity units (NTUs) with a very small sample volume (often <10 μL), making it ideal for screening during formulation development [109].
Can DLS be used to quantify viral particles instead of traditional plaque assays? Yes. DLS has been validated as a rapid, non-destructive method for quantifying viral particles. It directly counts viral particles in a solution within minutes, showing a strong correlation with traditional methods like plaque assays. A key advantage is that it does not rely on cell culture, but a limitation is that it cannot distinguish between infectious and non-infectious particles [107].
Troubleshooting Common Experimental Issues
Problem: Erratic or Unstable Readings
- Possible Cause 1: Air Bubbles in Sample. Even tiny air bubbles can scatter light and cause unstable readings [4] [7].
- Solution: After mixing, allow the sample to rest for sufficient decantation time to let bubbles escape. Handle samples gently to avoid introducing air [7].
- Possible Cause 2: Sample Sedimentation or Aggregation. Particles settling or aggregating during measurement will lead to drifting or erratic signals [4].
Problem: Detection Values are Too High or Too Low
- Possible Cause 1: Dirty or Scratched Cuvettes/Microplate Wells. Any imperfection on the optical surface will scatter light, leading to false high readings [104] [4].
- Solution: Clean cuvettes with lint-free cloth and use recommended cleaning solutions. Inspect for and replace any scratched consumables [7].
- Possible Cause 2: Incorrect or Lapsed Calibration. Calibration is critical for accuracy [4] [7].
Problem: Negative Results or Readings Below Blank
- Possible Cause: Sample Outside Detection Range. This can occur if the sample turbidity is near the instrument's detection limit or if the calibration range was selected improperly [4].
- Solution: Ensure the sample concentration is within the linear range of the instrument. If it's too low, concentrate the sample. If recalibrating, verify that the standard concentrations are appropriate for your samples [4].
Detailed Experimental Protocols
Protocol 1: Viral Particle Quantification Using Dynamic Light Scattering (DLS)
This protocol provides a rapid, non-destructive alternative to plaque assays for quantifying viral particles, useful for vaccine development and antiviral testing [107].
Workflow Overview:
Step-by-Step Procedure:
- Sample Preparation:
- Clarify the virus-containing supernatant by low-speed centrifugation to remove large cellular debris.
- Dilute the sample in an appropriate buffer to a concentration that falls within the instrument's optimal range. The ideal concentration should avoid multiple scattering events. The polydispersity index (PdI) should ideally be below 0.3 for reliable sizing [107].
- DLS Instrument Setup:
- Turn on the DLS instrument and laser, allowing a 5-10 minute warm-up period.
- Set the measurement temperature (e.g., 25°C).
- Select a scattering angle of 90° for optimal sensitivity to smaller particles like viruses [107].
- Data Acquisition:
- Load the diluted sample into a clean, high-quality cuvette, ensuring no air bubbles are present.
- Perform at least 3-5 measurement runs per sample to ensure reproducibility.
- Record the intensity trace and the correlation function for analysis [107].
- Data Analysis:
- Analyze the correlation function to determine the hydrodynamic radius (RH) of the particles using the Stokes-Einstein equation.
- Assess the quality of the measurement. A stable intensity trace and a high-quality fit of the correlation function are crucial for reliable data [107].
- Concentration Calculation:
- Correlate the scattering intensity (or the derived count rate) with viral concentration by creating a standard curve using a reference standard of known concentration (e.g., via plaque assay) [107].
Protocol 2: Assessing Protein Opalescence and Aggregation Using Microplate-Based Nephelometry
This protocol is optimized for high-throughput screening of protein solutions, such as monoclonal antibodies (mAbs), for opalescence and aggregation during formulation development [104] [109].
Workflow Overview:
Step-by-Step Procedure:
- Plate and Sample Preparation:
- Use 96- or 384-well microplates with high optical quality and clear, round (U)-bottom wells. Inspect plates for dust, scratches, or fingerprints [104].
- Prepare protein samples in the desired formulation buffers. Include a blank (buffer only) control.
- Pipette low-volume samples (e.g., <10 μL for microscale nephelometry) into the wells, avoiding bubble formation [109].
- Instrument Calibration:
- Power on the nephelometer (e.g., NEPHELOstar Plus) and allow it to warm up.
- Set the laser intensity and beam diameter according to the manufacturer's instructions to optimize sensitivity and minimize meniscus effects [104].
- Sample Measurement:
- Choose between endpoint measurement (a single read after a defined incubation) or kinetic measurement (multiple reads over time to monitor aggregation progress) [104].
- Load the microplate into the instrument and start the measurement cycle. The instrument will measure forward-angled scattered light [104].
- Data Collection:
- The instrument typically outputs data in Relative Nephelometric Units (RNU). The signal is generated when scattered light is reflected inside an Ulbricht sphere and detected [104].
- Data Interpretation:
- Compare RNU values across samples to rank relative opalescence or particle load.
- To convert RNU to standard Nephelometric Turbidity Units (NTU), use a calibration curve established with formazin standards, as described in the instrument's application notes [104].
Protocol 3: Quantifying Antigen Concentration via Turbidimetric Immunoassay
This protocol uses a turbidimeter or standard absorbance microplate reader to quantify antigen concentration by measuring the turbidity resulting from antigen-antibody complex formation [4].
Workflow Overview:
Step-by-Step Procedure:
- Prepare Reagents and Samples:
- Prepare a series of dilutions from an antigen standard of known concentration.
- Prepare the samples to be tested and a blank (distilled water).
- Have a specific antibody reagent ready [4].
- Mix Antigen and Antibody:
- Add an equal amount of the specific antibody reagent to tubes or wells containing the blank, standards, and unknown samples. Mix well.
- Incubate the mixture to allow the formation of insoluble antigen-antibody complexes, which increase the turbidity of the solution [4].
- Measure Transmitted Light:
- Plot a Standard Curve:
- Plot the OD values of the standard samples against their known concentrations.
- Generate a linear standard curve from this data [4].
- Determine Unknown Concentrations:
- Read the OD of each unknown sample tube and use the standard curve to calculate its antigen concentration [4].
This technical support center provides troubleshooting guides and FAQs to help researchers address specific issues related to sample preparation in the context of managing sample turbidity and light scattering in drug solutions research.
Troubleshooting Guide: Common Turbidity and Light Scattering Measurement Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| High background signal/noise | Multiple scattering in concentrated solutions [97], sample color interfering with transmittance-based detection [62], dust or particulate contamination [97] [86] | Dilute sample if possible; for concentrated polymer solutions, use a confocal dynamic light scattering (DLS) microscope to eliminate multiple scattering [97]. Use nephelometry (90-degree detection) instead of turbidimetry to avoid interference from colored samples [80] [62]. Filter samples and solvents to remove dust prior to measurement [97]. |
| Low initial amplitude in DLS correlation function | Weak scattering signal, often for common polymer solutions where reflected light intensity is much higher than scattered light [97] | Adjust the focal point of the confocal DLS microscope towards the interface between the cover glass and the sample to increase the amount of reflected light [97]. |
| Inconsistent or non-reproducible results | Sample preparation errors (miscalculations, contamination) [86], uncontrolled variations in method parameters (e.g., pH, temperature) [110] | Master accurate measurement skills and strict adherence to protocols [86]. Perform a robustness test to identify critical method parameters and define acceptable control limits for them [110]. |
| Reported particle size is twice the expected value (in DLS) | Partial heterodyne conditions where the initial amplitude of the time correlation function is set to less than 0.2 [97] | Note that the actual particle size is half the value obtained from the inverse Laplace transformation under these specific conditions [97]. |
| Difficulty measuring particle size in turbid samples | Multiple scattering effects or strong light absorption [97] | Avoid dilution by using a DLS microscope with a confocal optical system, which uses a pinhole to eliminate multiple scattering [97]. |
Frequently Asked Questions (FAQs)
General Sample Preparation and Validation
Q1: What is the difference between robustness and reproducibility in sample preparation? A1: Robustness (or ruggedness) is the capacity of an analytical procedure to remain unaffected by small, deliberate variations in method parameters (e.g., pH, temperature, mobile phase composition) and provides an indication of its reliability during normal usage [110]. Reproducibility, on the other hand, refers to the degree of agreement when the same sample is analyzed under a variety of normal conditions, such as different laboratories, analysts, or instruments [110].
Q2: Why is sample preparation so critical for data integrity? A2: Sample preparation errors are a significant source of irreproducibility in research [86]. A small inaccuracy at the beginning, such as a miscalculation or contamination, can transform into completely invalid results downstream, wasting costly reagents and research hours. Proper preparation creates the foundation for reliable and reproducible data [86].
Techniques and Measurements
Q3: When should I use nephelometry versus turbidimetry for turbidity measurement? A3:
- Nephelometry measures the intensity of light scattered by particles in the sample, typically at a 90-degree angle. It is best suited for samples with small particle sizes and is ideal for applications like kinetic solubility screens of drugs, as it is less affected by sample color [80] [62].
- Turbidimetry measures the reduction in transmitted light due to scattering and absorption by particles. It is commonly used for applications like monitoring bacterial growth (OD600) but can be inaccurate for colored samples, as it cannot distinguish between light loss from scattering and from absorption by the color [80] [62].
Q4: How can I measure particle size in a concentrated, turbid solution without diluting it? A4: Standard dynamic light scattering requires diluted samples. For concentrated solutions, a dynamic light scattering microscope can be used. This apparatus uses a confocal optical system with a pinhole to eliminate the multiple scattering effect that plagues standard DLS measurements of turbid samples, allowing for analysis in their native state without dilution [97].
Q5: What is a systematic approach to validating the robustness of my sample preparation method? A5: A robustness test can be broken down into key steps [110]:
- Select Factors and Levels: Choose critical method parameters (e.g., pH, temperature) and define small, realistic variations around their nominal values.
- Select an Experimental Design: Use a structured approach like a Plackett-Burman or fractional factorial design to efficiently test multiple factors simultaneously.
- Execute Experiments and Analyze Data: Perform the experiments per the design and statistically estimate the effect of each factor variation on your key responses (e.g., assay result, turbidity).
- Draw Conclusions: Identify which factors have a significant effect and define system suitability limits to control them, ensuring method reliability during transfer and routine use.
Experimental Protocols for Key Experiments
This protocol provides a framework for testing the robustness of an analytical method, such as one used to measure drug concentration or turbidity.
1. Selection of Factors and Levels:
- Identify key method parameters likely to affect the results (e.g., for HPLC: mobile phase pH, column temperature, flow rate).
- Define a "nominal" level and two extreme levels (high and low) for each factor. The extreme levels should represent the small variations expected during method transfer (e.g., nominal pH ± 0.1 units).
2. Selection of an Experimental Design:
- A two-level screening design, such as a Plackett-Burman design, is typically used.
- This design allows for the efficient examination of
ffactors in a minimal number of experiments (oftenf+1).
3. Selection of Responses:
- Choose relevant responses to monitor. These can include:
- Assay responses: e.g., content or recovery of the active compound.
- System Suitability Test (SST) responses: e.g., resolution between peaks in a chromatogram.
4. Execution of Experiments:
- Execute the experiments as defined by the design matrix.
- To account for potential "drift" in instrument response over time, it is recommended to run the experiments in a randomized order or in a special "anti-drift" sequence. Alternatively, include replicated measurements at the nominal conditions at regular intervals to correct for any observed drift.
5. Data Analysis:
- For each factor and each response, calculate the effect (
E), which is the difference between the average response when the factor is at its high level and the average response when it is at its low level [110]. - Analyze the effects graphically (e.g., using a normal probability plot) or statistically to identify which factors have a significant influence on the method.
This protocol allows for particle size distribution measurement in turbid samples where standard DLS fails.
1. Sample Preparation and Mounting:
- Prepare the polymer solution (e.g., temperature-responsive Poly(N-isopropylacrylamide)).
- Place 60 µL of the sample on a cavity slide.
- Cover with a circular cover glass, avoiding air bubbles.
- Remove excess solution and seal the edges with glue. Let it dry.
2. Instrument Optimization (Using a Standard):
- Place a slide with a standard suspension (e.g., 100-nm polystyrene latex beads) on the microscope stage.
- Adjust the objective lens to set the focal point within the sample suspension.
- Set a pinhole to achieve the confocal effect and maximize the light intensity at the detector.
- Measure the time correlation function of the scattered light intensity.
- Adjust the focal point to optimize the initial amplitude of the correlation function. For strong scatterers, it can be close to 1, but for common polymer solutions, a value below 0.2 is acceptable and simplifies analysis.
3. Sample Measurement:
- Place the prepared sample slide on the stage.
- Set the desired temperature (e.g., below and above the Lower Critical Solution Temperature).
- Measure the time correlation function of the scattered light intensity.
- If the initial amplitude is too large (e.g., >0.2), adjust the focal point to reduce it.
4. Data Analysis:
- Apply an inverse Laplace transformation (using software like CONTIN) to the obtained time correlation function to acquire the size distribution.
- Critical Note: If the initial amplitude was set to less than 0.2, the obtained hydrodynamic radius will be approximately twice the actual size and must be halved for the correct result [97].
Essential Research Reagent Solutions
| Item | Function/Explanation |
|---|---|
| NIPA (N-isopropylacrylamide) | A temperature-responsive monomer used to create model polymer solutions for studying phase transitions and turbidity changes related to the Lower Critical Solution Temperature (LCST) [97]. |
| Polystyrene Latex Beads | A standard suspension with a known, uniform particle size (e.g., 100 nm). Used for calibration and performance verification of dynamic light scattering instruments [97]. |
| Bovine Serum Albumin (BSA) | A model protein often used in analytical system development for biotherapeutics. Its slightly turbid and colored nature makes it ideal for testing and validating turbidity measurement methods [62]. |
| AMCO Clear Standards (SDVB) | Pre-calibrated styrene divinylbenzene turbidity standards (e.g., 0, 5, 10, 20, 40, 100 NTU). Used to calibrate both nephelometers and turbidimeters for accurate quantitative measurements [62]. |
| Precipitation Inhibitors | Excipients (e.g., various polymers) screened to prolong the supersaturated state of poorly soluble drugs, thereby inhibiting precipitation and potentially improving oral bioavailability [1]. |
Workflow and Relationship Diagrams
Diagram 1: Robustness Test Workflow
Diagram 2: Turbidity Measurement Decision
Diagram 3: Sample Prep Impact Chain
Clinical trials for pediatric populations face unique ethical and practical constraints. The most significant limitation is the limited blood volume of infants and young children, which restricts the number and volume of blood samples that can be collected for pharmacokinetic (PK) studies [111]. Furthermore, a lack of pediatric data for many drugs leads to unlicensed or off-label use, increasing the risk of adverse events and treatment failure [111]. This case study explores how a model-based approach to sampling optimization can maximize the information gained from PK studies while minimizing the burden on vulnerable pediatric patients.
Core Concepts and Key Terminology
What is Model-Based Sampling Optimization? It is a methodology that uses existing population PK models to design sparse sampling schemes. Instead of collecting numerous blood samples from each child, it identifies the few, most informative time points to estimate PK parameters with precision comparable to traditional, frequent sampling methods [111] [112].
The Role of Population PK (popPK) Modeling popPK is a crucial modeling approach that characterizes the PK properties of a drug and explains variability between subjects by evaluating the effects of covariates, such as body weight, age, and organ function [112]. In pediatric development, popPK models are used to predict adequate dosing regimens and to analyze sparse PK data collected from the study itself [112].
Connecting to Sample Turbidity and Light Scattering In the broader context of drug solution research, analytical methods are critical for quantifying drug concentration and understanding formulation properties. Techniques like Dynamic Light Scattering (DLS) and turbidimetry are used to characterize samples. However, turbid or cloudy samples can pose a challenge, as high particle concentrations can lead to multiple scattering events, where light is scattered more than once before detection, causing measurement inconsistencies or errors [43]. Managing this is essential for ensuring data quality in analytical assays supporting PK studies.
FAQs on Pediatric Sampling and Analytical Challenges
FAQ 1: Why can't we simply use adult dosing information for children? Children are not small adults. Physiological factors such as body size, organ maturation, and the development of enzyme systems significantly alter a drug's clearance and volume of distribution [112]. For example, in a pediatric model for cefepime, clearance was found to depend on body weight, postmenstrual age, and serum creatinine levels [111]. These factors must be formally studied to ensure safe and effective dosing.
FAQ 2: How many blood samples can typically be collected from a child? While the exact number depends on the child's age and health status, the goal is to minimize samples. This case study demonstrated that optimized sampling could reduce the number of samples to just two to four time points per patient, down from a full, traditional sampling schedule, without significantly losing precision in PK parameter estimation [111].
FAQ 3: Our drug solution is turbid. Will this affect our DLS-based particle size analysis? Turbidity can complicate DLS analysis due to multiple scattering. However, this can be mitigated by using back-scattering detection (at a 175° angle) and adjusting the laser focus position closer to the cuvette wall. This reduces the photon path length through the sample, making multiple scattering events less likely [43]. Advanced DLS instruments can automatically determine the optimal scattering angle and laser focus position by assessing light transmittance prior to the experiment [43].
FAQ 4: What is the difference between scatter and absorption measurements for turbidity? The choice depends on the turbidity level and particle size.
- Scatter Measurements (e.g., 11° or 90°): Ideal for low to medium turbidity values. The 11° forward scatter is highly sensitive to larger particles (0.5-5 μm), such as cells, while 90° side scatter is more sensitive to smaller particles (0.1-0.5 μm), like colloids [77].
- Absorption Measurements (0°): Better suited for medium to high turbidity levels. The absorption signal provides a linear response over a wide dynamic range where scatter signals may saturate [77]. Combining both approaches in one sensor can offer high sensitivity and a wide measurement range.
Troubleshooting Guide: Sampling and Analytical Methods
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Pediatric Study Design | Inability to estimate PK parameters with acceptable precision. | Sparse sampling at uninformative time points; insufficient number of patients. | Use model-based sampling optimization (e.g., Fisher information matrix) to identify the most informative sampling times [111]. Leverage clinical trial simulations to determine the required sample size [112]. |
| Pediatric Study Design | High inter-individual variability in drug exposure. | Failure to account for key covariates like body weight, age, or organ function in the dosing regimen. | Develop a population PK model that incorporates covariates (allometric scaling for weight, maturation functions for age) to explain variability and guide dose individualization [111] [112]. |
| Analytical Methods (DLS) | Poor quality correlation function or inconsistent particle size results. | Multiple scattering events in a turbid sample; inappropriate detector angle. | Switch to back-scattering geometry (175°); use an instrument with automatic positioning to minimize the light path length [43]. |
| Analytical Methods (Turbidity) | Signal saturation at medium turbidity levels. | Reliance solely on a scatter measurement (e.g., 11°). | Combine scatter with an absorption measurement (0°). The absorption signal remains linear at much higher turbidity values [77]. |
| Drug Formulation | Changes in formulation viscosity or stability during PK studies. | Inadequate control of critical process parameters (CPP) like mixing speed, time, and temperature [113]. | Implement a Quality-by-Design (QbD) approach to optimize and control CPPs, ensuring consistent drug product characteristics throughout the study [113]. |
Detailed Experimental Protocol: A Paradigm for Sampling Optimization
The following workflow, based on a published simulation study, outlines the steps for implementing model-based sampling optimization in pediatric drug development [111].
Workflow: Model-Based Sampling Optimization
Protocol Steps:
Drug and Model Selection:
Software and Optimization Setup:
- Use specialized software for population design evaluation, such as PFIM (Population Fisher Information Matrix), which integrates with the R statistical environment [111].
- Input the structural PK model, parameter estimates, and inter-individual variability from the identified popPK model.
- Define the target pediatric population covariates (e.g., body weight range, age groups).
Sampling Time Optimization:
- The software employs an algorithm (e.g., Fedorov-Wynn) to optimize over a discrete set of possible sampling times from the original, frequent-sampling design [111].
- The optimization criterion is based on maximizing the Fisher Information Matrix, which minimizes the expected uncertainty (standard errors) of the PK parameter estimates.
- The output is a reduced set of 2 to 4 optimal sampling times that are clinically feasible.
Clinical Trial Execution and Analysis:
- Conduct the pediatric clinical trial, collecting blood samples according to the optimized, sparse schedule.
- Analyze the collected sparse PK data using nonlinear mixed-effects modeling to obtain empirical Bayes estimates of the PK parameters for each individual.
- Evaluate the precision of the parameter estimates and the predicted drug efficacy (e.g., time above MIC for antibiotics) against the outcomes expected from full sampling.
Key Reagent and Material Solutions
| Item | Function in the Experiment | Specific Example / Note |
|---|---|---|
| Population PK Model | Serves as the prior knowledge base for simulating and optimizing the sparse sampling design. | A model for cefepime including covariates for weight, postmenstrual age, and serum creatinine [111]. |
| Software (PFIM) | A tool for calculating the Fisher Information Matrix to optimize the sampling design for a population PK model. | PFIM version 4.0, which uses the Fedorov-Wynn algorithm [111]. |
| DLS Instrument | For characterizing particle size in drug formulations, which can support PK study validation. | Instruments like the Litesizer 500, which facilitate analysis of turbid samples via transmittance analysis and adjustable focus points [43]. |
| Turbidity Sensor | To monitor and manage sample turbidity in drug solutions during analysis. | Sensors like the DTF16, which can perform both absorption and scatter (11°, 90°) measurements for a wide dynamic range [77]. |
Data Presentation and Analysis
Quantitative Outcomes of Sampling Optimization
The following table summarizes the results from a simulation study that applied this methodology to two antibiotics, cefepime (CFPM) and ciprofloxacin (CPFX) [111].
| Model Drug | Original Sampling | Optimized Sampling | Key PK Parameters | Precision of Estimates vs. Full Sampling |
|---|---|---|---|---|
| Cefepime (CFPM) | Full, frequent schedule | 2 - 4 time points | Clearance (CL), Volume of Distribution (VSS) | Generally comparable |
| Ciprofloxacin (CPFX) | Full, frequent schedule | 2 - 4 time points | Clearance (CL), Volume of Central Compartment (VC) | Generally comparable |
| Overall Conclusion | Traditional approach with high patient burden. | Model-based approach minimizing burden. | Efficacy predictions (e.g., Time > MIC) were also maintained. | Maximizes PK information with a minimum burden on infants and young children [111]. |
Turbidity Measurement Angles and Applications
Understanding light scattering techniques is vital for supporting analytical assays in drug development. The table below compares different turbidity measurement approaches [77].
| Measurement Principle | Detection Angle | Optimal Particle Size Range | Best For / Sensitivity |
|---|---|---|---|
| Scatter | 90° (Side) | 0.1 - 0.5 μm | Colloids; quality measurements in beer and drinking water. |
| Scatter | 11° (Forward) | 0.5 - 5 μm | Larger particles like cells; higher sensitivity for bigger particles. |
| Absorption | 0° | Mid to High Turbidity | Very high turbidity values; provides a linear response over a wide range. |
| Back-Scatter | 175° | High Turbidity | Extremely high turbidity values where other signals saturate. |
Visual Guide to Turbidity Management
The diagram below illustrates the decision process for selecting the appropriate analytical method based on sample turbidity and the property of interest.
Equipment Qualification and Cleaning Validation to Prevent Cross-Contamination
FAQs and Troubleshooting Guides
FAQ 1: Why is visual inspection alone insufficient for confirming equipment cleanliness, and how should it be properly implemented?
Visual inspection, while a required first criterion, should not be the sole method for confirming equipment cleanliness. The visual residue limit (VRL)—the lowest concentration of a residue detectable by the human eye—can vary significantly (from approximately 1 µg/cm² to over 10 µg/cm²) depending on the substance and inspection conditions [114]. If your calculated acceptable surface limit (ASL) is higher than your VRL, residues at the acceptable limit may be invisible to your staff.
- Troubleshooting Tip: If your analytical results consistently show residues below the ASL, yet your visual inspections find the equipment "visually clean," this is expected and confirms your method is working. The problem arises if the VRL is higher than the ASL, meaning dangerous residues could be present but undetectable by sight. In this case, you must supplement visual inspection with sensitive analytical techniques like swab sampling with HPLC or TOC analysis [114] [115].
- Solution: Implement a formal staff accreditation program for visual inspection. This involves training personnel and testing their ability to detect residues at or below the VRL on coupons made of representative materials (e.g., stainless steel, glass) under controlled lighting conditions that mimic the production environment [114].
FAQ 2: How do I select the worst-case Active Pharmaceutical Ingredient (API) for a cleaning validation study in a multi-product laboratory?
Adopt a risk-based, "worst-case" approach. The objective is to select an API that, if you can prove it is effectively removed, provides a high degree of confidence that other, less challenging APIs will also be cleaned effectively [116].
Consider these criteria for selection [116]:
- Solubility: APIs with low solubility in your cleaning agents (especially water) are typically harder to clean.
- Toxicity: Highly potent or toxic compounds require lower acceptance limits, making validation more demanding.
- Cleaning Difficulty: Historical data may show that certain APIs or finished products persistently contaminate equipment.
- A case study example: Oxcarbazepine was selected as a worst-case API due to its very low solubility in water (0.07 mg/mL), known cleaning challenges, and toxicity profile [116].
FAQ 3: My turbidity measurements for a colored protein solution are inconsistent. Could the sample's color be interfering with the measurement?
Yes, this is a common issue. Standard transmittance-based turbidity measurements (brightfield mode) cannot distinguish between light scattered by particles and light absorbed by the sample's color, leading to falsely high turbidity readings [62].
- Solution: Use a true nephelometric method. A nephelometer positions the detector at a 90-degree angle to the incident light beam, specifically measuring scattered light rather than a general loss of transmittance. Research has shown that for colored samples like Bovine Serum Albumin (BSA) solutions, modified nephelometric methods provide turbidity values that correlate well with a standard nephelometer, unlike brightfield methods [62].
- Alternative Approach: Light scattering microtiter plate-based methods can also be used as a high-throughput "first screening line" for detecting precipitation and have been validated against classical approaches [1].
Experimental Protocols and Data
Protocol 1: Swab Sampling for Residue Recovery
This protocol is used for sampling flat or irregular equipment surfaces to quantify residual contamination after cleaning [116].
- Swab Selection: Choose a swab material with high recovery for the target residue (e.g., polyester) [116].
- Swab Preparation: Pre-wet the swab with an appropriate solvent (e.g., acetonitrile or acetone for organic residues) that can dissolve the target API. Remove excess solvent [116].
- Sampling: Systematically wipe a defined surface area (e.g., 100 cm²) using both horizontal and vertical strokes. Use both sides of the swab to maximize residue recovery [116].
- Extraction: Place the swab head in a clean test tube containing a known volume of solvent. Allow it to extract for a defined period (e.g., 10 minutes) [116].
- Analysis: Quantify the residue concentration in the extract using a sensitive analytical technique such as HPLC or UPLC, and compare it to the predetermined acceptance limit [116] [115].
Protocol 2: Nephelometric Turbidity Measurement for Colored Biotherapeutic Formulations
This protocol ensures accurate turbidity measurement for colored drug solutions, which is critical for assessing stability and aggregation [62].
- Instrument Setup: Use a nephelometer or a visual inspection station modified for scattered light detection (SLD). The key is to have a light source positioned at 90 degrees from the detector axis [62].
- Calibration: Calibrate the instrument using standard turbidity standards (e.g., styrene divinylbenzene standards at 0, 5, 10, 20, 40, and 100 NTU) [62].
- Sample Preparation: Prepare the protein sample (e.g., BSA) in an appropriate buffer. Filter the stock solution using a 0.22 µm syringe filter to remove initial particulates. Confirm sample concentration via UV/VIS spectrophotometry [62].
- Measurement: For the modified SLD method, use a turbidity standard (e.g., 200 NTU) to normalize all luminance measurements. Measure the sample turbidity in SLD mode [62].
- Data Interpretation: Compare the results from the SLD mode to those from a standard nephelometer to validate the method. The SLD values should be closer to the true nephelometer values than those from brightfield mode [62].
Quantitative Data on Analytical Techniques
The table below summarizes key methods for detecting residues and their characteristics [115]:
Table 1: Common Analytical Techniques in Cleaning Validation
| Analytical Technique | Primary Function | Key Characteristics |
|---|---|---|
| Total Organic Carbon (TOC) Analysis | Measures organic carbon content | Excellent for detecting residual cleaning agents or organic contaminants; non-specific [115]. |
| Liquid Chromatography (HPLC/UPLC) | Detects and quantifies specific APIs/chemicals | Highly sensitive and specific for identifying and measuring particular residues [115]. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Detects trace metals and inorganic contaminants | Provides precise analysis for metal residues at very low levels [115]. |
Research Reagent Solutions and Materials
Table 2: Essential Materials for Cleaning Validation and Turbidity Studies
| Item | Function/Application |
|---|---|
| Polyester Swabs | Surface sampling for residual APIs during cleaning validation studies [116]. |
| Acetonitrile & Acetone | Solvents for dissolving and recovering poorly water-soluble APIs (e.g., Oxcarbazepine) from equipment surfaces [116]. |
| Phosphate-Free Alkaline Detergent | Used in manual cleaning processes to remove residues without introducing phosphates [116]. |
| Turbidity Standards (e.g., AMCO Clear) | Styrene divinylbenzene standards for calibrating nephelometers and turbidity measurement systems [62]. |
| Bovine Serum Albumin (BSA) | A model protein used for developing and validating analytical methods for biotherapeutic formulations [62]. |
Workflow and Pathway Diagrams
Cleaning Validation Lifecycle
Turbidity Method Selection
Establishing Scientifically Sound Acceptance Criteria for Solution Clarity
Turbidity, the cloudiness or haziness of a liquid caused by undissolved substances, is a critical quality attribute in drug development [117]. It is not a well-defined physical property like temperature, but is always expressed by reference to a defined standard [117]. For researchers and scientists, establishing acceptance criteria for solution clarity is essential for ensuring product quality, filtration process performance, and ultimately, drug safety and efficacy [117].
This guide provides troubleshooting and methodological support for managing sample turbidity and light scattering in pharmaceutical solutions.
Frequently Asked Questions (FAQs)
What is turbidity, and why is it a critical parameter in drug solution analysis?
Turbidity is the decrease in a liquid's transparency caused by undissolved substances [117]. It is an aggregate property of the solution caused by suspended particles, which can be organic, inorganic, or biological, and exist in suspended or colloidal form [118]. It is critical because it can:
- Serve as an indicator of unwanted precipitation or aggregation of active pharmaceutical ingredients (APIs) [117] [118].
- Affect the performance of filtration processes [117].
- Impact the accuracy of other analytical methods, such as photometric analysis, by scattering and absorbing light, potentially leading to measurement errors [17].
How do modern turbidity meters work, and what do the different measurement angles signify?
State-of-the-art turbidity meters no longer rely on subjective visual scales but accurately determine turbidity by measuring the scattering of light at multiple angles [117]. The evaluation of signals from different angles is crucial because light scattering depends on the size of the particles in the sample [117].
- Scattered light at 25° (Forward Scattering): Used to detect the presence of large particles [117].
- Scattered light at 90°: Used to detect the presence of small particles [117].
- Transmission at 0°: Used to compensate for the sample's color, ensuring the turbidity measurement is not skewed by the solution's inherent color [117]. Modern instruments often use the Ratio Method, which uses all these evaluated angles to calculate a turbidity value that is independent of particle size and sample color [117].
Measuring low-level turbidity requires meticulous technique. Common errors and their solutions include:
- Stray Light: Light detected by the sensor that was not scattered by the sample turbidity. This can come from electronic noise, internal optical reflections, or dirt, dust, fingerprints, and scratches on the sample tube [118]. It causes falsely high readings.
- Minimization: Use well-designed meters with blanking procedures, ensure sample tubes are impeccably clean and scratch-free, and wipe the outside of tubes with a lint-free cloth before measurement [118].
- Dissolved Gasses: Tiny invisible bubbles can cause positive interference [118].
- Minimization: Allow the sample to sit for several minutes in the tube to degas before measurement [118].
- Tube Geometry and Orientation: Slight variations in tube wall thickness or diameter, and inconsistent placement in the light chamber, can cause inconsistent results [118].
- Minimization: Use high-quality, matched sample tubes. Use tubes with indexing lines or an orientation device that ensures the tube is placed the same way every time [118].
- Contamination: Fingerprints, lint, or dried residues on tubes or caps [118].
- Minimization: Implement rigorous tube washing and handling procedures. Hold tubes only by the cap, and store clean, dry tubes with caps on [118].
My instrument occasionally gives a negative turbidity reading. What does this mean?
A negative result is theoretically impossible, but can occur in practice due to natural variations in measurements [118]. If a meter consistently gives a negative result, it indicates a potential problem with the operator's technique, the turbidity-free water used for blanking, or the instrument's calibration [118]. A meter that rounds negative values up to 0.00 NTU can hide this problem. Therefore, the ability to display negative values is a useful feature for troubleshooting low-level turbidity analysis [118].
How can turbidity interference in other photometric analyses be corrected?
Turbidity can interfere with colorimetric and spectrophotometric methods by scattering and absorbing light, leading to inaccurate analyte measurement [17]. Several approaches can reduce this impact:
- Filtration: Removing suspended particles using membrane or glass fiber filters [17]. Note: this may not be suitable if the analyte is bound to the particles.
- Dilution: Diluting the sample with pure water to lower turbidity, though this also reduces analyte concentration and may require result correction with a dilution factor [17].
- Automatic Correction: Many modern spectrophotometers, like the NANOCOLOR series, feature automatic turbidity detection (e.g., NTU Check) that warns users of high turbidity and can apply built-in correction factors [17].
Troubleshooting Guide
| Problem | Possible Cause | Recommended Action |
|---|---|---|
| High/Erratic Readings | Dirty or scratched sample tube | Clean tube with mild detergent, rinse with turbidity-free water, and air-dry. Discard scratched tubes [118]. |
| Fingerprints or smudges on tube | Wipe outside of tube with a clean, lint-free cloth before measurement. Handle tubes by the cap only [118]. | |
| Stray light interference | Ensure meter's blanking procedure is correctly performed. Keep the instrument's light chamber clean [118]. | |
| Dissolved gas bubbles (microbubbles) | Let the filled sample tube sit for several minutes to degas before taking a reading [118]. | |
| Low/Negative Readings | Incorrect calibration | Recalibrate the instrument using traceable standards. Verify calibration regularly [118]. |
| Problem with blank | Ensure the turbidity-free water used for blanking is truly free of particles [118]. | |
| Unstable Readings | Convection currents in sample | Ensure sample is at a quiescent state after mixing. Allow it to settle [118]. |
| Large particles passing through light beam | Use the instrument's signal-averaging function (if available) to obtain a stable, averaged reading [118]. | |
| Inconsistent Results Between Replicates | Inconsistent tube orientation | Use sample tubes with an orientation device or indexing line, and place them in the chamber the same way every time [118]. |
| Settling or inhomogeneity of sample | Invert the sample tube gently to re-suspend particles before measurement, then allow it to become quiescent [118]. |
Experimental Protocols for Turbidity Analysis
Protocol 1: Reliable Sample Preparation and Handling for Turbidity Measurement
Principle: To minimize pre-analytical errors and ensure that the measured turbidity accurately reflects the sample and is not an artifact of contamination or poor handling [118].
Materials:
- Turbidity-free water (e.g., filtered through a 0.1-0.2 µm filter)
- Mild laboratory detergent
- Lint-free, absorbent cloths
- High-quality, matched sample tubes (e.g., according to instrument manufacturer)
Methodology:
- Tube Cleaning: Wash tubes inside and out with a mild detergent. Rinse thoroughly (5-10 times) with turbidity-free water. Allow to air-dry in an inverted position. Store dry tubes with caps on [118].
- Sample Rinsing: Before measurement, rinse a clean tube 3-5 times with the sample solution [118].
- Sample Filling: Fill the tube with the sample and cap it immediately to prevent dust contamination [118].
- Degassing: Let the capped tube sit for several minutes to allow dissolved gasses to escape [118].
- Homogenization: Gently invert the tube to re-suspend any settled particles. Allow the sample to reach a quiescent state before measurement [118].
- External Wiping: Wipe the outside of the tube with a lint-free cloth until it is completely dry and free of smudges [118].
- Measurement: Place the tube in the instrument using a consistent orientation (using an indexing line or device). Take multiple readings to ensure stability [118].
Protocol 2: Establishing Method-Specific Acceptance Criteria
Principle: To define a scientifically sound and fit-for-purpose turbidity limit for a specific drug solution.
Materials:
- Validated and calibrated turbidity meter (nephelometer)
- Appropriate turbidity standards for calibration verification
- Representative samples of the drug solution (multiple batches)
Methodology:
- Method Definition: Document the complete measurement method, including instrument model, calibration frequency, sample temperature, and detailed sample preparation steps (as in Protocol 1) [117] [118].
- Baseline Characterization: Measure and record the turbidity of multiple batches of the drug solution that are known to have acceptable clarity based on other stability and quality tests.
- Data Analysis: Calculate the mean and standard deviation of the turbidity values from the acceptable batches.
- Limit Setting: Propose a preliminary acceptance criterion. A common approach is to set a limit based on the historical data, for example, the mean + 3 standard deviations, or based on a value that correlates with a known performance or stability failure.
- Robustness Testing: Challenge the set limit by testing samples with known marginal quality to ensure the criterion effectively discriminates between acceptable and unacceptable product.
- Documentation: Formally document the final acceptance criterion, the justification for the chosen limit (including the data from baseline characterization), and the full measurement procedure.
Workflow for Managing Sample Turbidity
The following diagram illustrates a systematic workflow for handling and analyzing samples with potential turbidity issues, integrating troubleshooting and corrective actions.
The Scientist's Toolkit: Essential Materials for Turbidity Management
| Item | Function & Importance |
|---|---|
| Turbidity Meter (Nephelometer) | The primary instrument for measuring turbidity. Modern meters measure scattered light at multiple angles (e.g., 25°, 90°, and 0°) to account for different particle sizes and sample color [117]. |
| High-Quality Sample Tubes | Matched sample tubes with consistent optical properties are essential. Scratches or imperfections on the tube can scatter light and cause erroneous readings [118]. |
| Turbidity-Free Water | Used for blanking the instrument, preparing dilutions, and rinsing glassware. Typically produced by filtration through a 0.1-0.2 µm filter to remove suspended particles [118]. |
| Traceable Turbidity Standards | Suspensions of known turbidity (e.g., in NTU or FNU) used for calibrating or verifying the calibration of the turbidimeter to ensure measurement accuracy [118]. |
| Membrane Filters & Syringes | Used for sample filtration to remove suspended particles that cause turbidity, either as a corrective action or to prepare turbidity-free water [17]. |
| Lint-Free Wipes | Used to dry and polish the outside of sample tubes before measurement to remove fingerprints and water spots, which are significant sources of stray light [118]. |
Conclusion
Effectively managing sample turbidity and light scattering is not merely a technical challenge but a critical component of successful drug development that impacts solubility, bioavailability, and ultimately, patient safety. By integrating foundational knowledge with advanced methodological approaches, robust troubleshooting protocols, and rigorous validation frameworks, researchers can transform turbidity from an obstacle into a source of valuable analytical data. The future of this field lies in the continued adoption of automated, model-based approaches and high-throughput techniques like laser nephelometry, which promise to enhance efficiency while maintaining regulatory compliance. As drug formulations grow more complex, mastering these principles will be essential for developing safe, effective, and high-quality pharmaceutical products.
References
- 1. Evaluation of the light scattering and the turbidity microtiter ... [https://www.sciencedirect.com/science/article/abs/pii/S0939641113003081]
- 2. Drug solubility: why testing early matters in drug discovery [https://www.bmglabtech.com/en/blog/drug-solubility-why-testing-early-matters-in-drug-discovery/]
- 3. Light Scattering and Turbidimetry Techniques for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9268389/]
- 4. Turbidimetry Protocol & Troubleshooting - Creative Biolabs [https://www.creativebiolabs.net/turbidimetry.htm]
- 5. An Overview of USP , , and Standards [https://www.fluidimaging.com/blog/usp-787-usp-788-usp-789-standards-injectables]
- 6. Inspection of Injectable Products for Visible Particulates [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/inspection-injectable-products-visible-particulates]
- 7. Troubleshooting Common Issues with Turbidity Meters [https://www.boquinstrument.com/a-news-troubleshooting-common-issues-with-turbidity-meters.html]
- 8. Turbidity Sensor Troubleshooting and FAQs [https://www.vernier.com/til/1388?srsltid=AfmBOoqLnRwc6WTQtdug-nbzadreoyPBYbqI6YVARyWJswFodsqGN0rv]
- 9. Understanding the turbidity of water: causes, measurement ... [https://www.aqualabo.fr/en/understanding-the-turbidity-of-water-causes-measurement-and-solutions/]
- 10. Water Clarity (Turbidity, Suspended Solids, and Color) [https://edis.ifas.ufl.edu/publication/SS526]
- 11. Light scattering-based screening method for rapid evaluating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297787/]
- 12. Rapid alignment-free bacteria identification via optical ... [https://www.nature.com/articles/s41598-024-71238-0]
- 13. Studies on the Efficiency of Iron Release from Fe(III)-EDTA ... [https://www.mdpi.com/1420-3049/27/23/8498]
- 14. Dynamic Light Scattering for Pharmaceutical Nanoparticles [https://allanchem.com/dynamic-light-scattering-for-pharmaceutical-nanoparticles/]
- 15. Dynamic light scattering: a practical guide and applications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5425802/]
- 16. Colloidal Stability of CA, SDS and PVA Coated Iron Oxide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9655895/]
- 17. Turbidity and its impact on photometric water analysis [https://www.news-medical.net/whitepaper/20250828/Turbidity-and-its-impact-on-photometric-water-analysis-with-advanced-auto-detection.aspx]
- 18. Improved Bioavailability of Poorly Water-Soluble Drug by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8707685/]
- 19. Improving Bioavailability & Solubility: A Top-Down Versus ... [https://drug-dev.com/special-feature-improving-bioavailability-solubility-a-top-down-versus-bottom-up-approach/]
- 20. Advancements in the exploration and application of ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993625002018]
- 21. Multi-Wavelength Calibration of a Low-Cost High-Range ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12612979/]
- 22. Turbidity [https://en.wikipedia.org/wiki/Turbidity]
- 23. Turbidity 101: What It Is, And Why It Is So Important [https://in.hach.com/turbidity-article-turbidity101?srsltid=AfmBOoqJp0rM0UDDsOV-WxfFlDasnG6Dz1H74J1WvBUCx03Q8e-csXI9]
- 24. Microbial contamination of nonsterile pharmaceuticals in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2952482/]
- 25. Dynamic Light Scattering (DLS) [https://www.wyatt.com/solutions/techniques/dynamic-light-scattering-nanoparticle-size.html]
- 26. Application of Light Scattering Techniques to Nanoparticle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6026678/]
- 27. “Negative†Impact: The Role of Payload Charge in ... [https://www.sciencedirect.com/science/article/pii/S0022354924001503]
- 28. Turbidity Sampling [https://www.wastormwatercenter.org/turbidity-sampling/]
- 29. Dynamic Light Scattering (DLS) [https://www.creative-proteomics.com/antibodydrug/dynamic-light-scattering-dls.html]
- 30. What is Multiple Scattering? [https://www.malvernpanalytical.com/en/learn/knowledge-center/faqs/160719faqmultiplescattering]
- 31. Dynamic Light Scattering - biophysics [https://physics.stackexchange.com/questions/29368/dynamic-light-scattering]
- 32. Pitfalls and novel applications of particle sizing by dynamic ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961216301648]
- 33. Dynamic light scattering [https://en.wikipedia.org/wiki/Dynamic_light_scattering]
- 34. Understanding Dynamic Light Scattering Theory - Waters [https://www.wyatt.com/library/theory/dynamic-light-scattering-theory.html]
- 35. LABTips: Mitigating Common Errors in Particle Analysis [https://www.labcompare.com/10-Featured-Articles/613687-Mitigating-Common-Errors-in-Particle-Analysis/]
- 36. Turbidity Measurements & Assays in Life Science [https://www.bmglabtech.com/en/blog/turbidity-measurements-in-life-science/]
- 37. Turbidity Meters: What is the difference between NTU and ... [https://www.instrumentchoice.com.au/blogs/news/turbidity-meters-what-is-the-difference-between-ntu-and-fnu?srsltid=AfmBOooyvSX8JnS53VzNteI_s4WaPboVwH4m3ehhRT9MqGsqlm72NDz2]
- 38. Understanding Turbidity Units: NTU, FNU, FTU, JTU, and ... [https://www.daruifuno.com/news/understanding-turbidity-units-ntu-fnu-ftu-jtu-and-fau-explained-323871.html]
- 39. Turbidity units - explained [https://www.kemtrak.com/the-difference-between-turbidity-units/]
- 40. FAQ on Turbidimeters Under the Category Environmental ... [https://gaotek.com/faq-turbidimeters/]
- 41. 2020e/2020i Turbidity Meter Troubleshooting Guide [https://lamotte.com/technical-tips/post/2020e-2020i-turbidity-meter-troubleshooting-guide]
- 42. Limitations of turbidity process probes and formazine as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5233748/]
- 43. DLS analysis of turbid samples [https://wiki.anton-paar.com/us-en/dls-analysis-of-turbid-samples/]
- 44. Dynamic light scattering in turbid colloidal dispersions [https://www.sciencedirect.com/science/article/abs/pii/S0021979706008095]
- 45. The principles of dynamic light scattering [https://wiki.anton-paar.com/us-en/the-principles-of-dynamic-light-scattering/]
- 46. Dynamic Light Scattering [https://particletechlabs.com/analytical-testing/dynamic-light-scattering/]
- 47. How to Minimize Errors in Dynamic Light Scattering ... [https://eureka.patsnap.com/report-how-to-minimize-errors-in-dynamic-light-scattering-measurements]
- 48. Dynamic Light Scattering (DLS) Particle Size Analysis [https://www.swabianinstruments.com/applications/dynamic-light-scattering/]
- 49. Real-Time Size Monitoring for Low Turbidity Formulations [https://www.news-medical.net/whitepaper/20241106/Continuous-inline-size-monitoring-of-low-turbidity-suspensions-under-flow-in-biopharmaceutical-processes.aspx]
- 50. High-throughput kinetic turbidity analysis for determination ... [https://www.sciencedirect.com/science/article/abs/pii/S037851732201050X]
- 51. Case Study: Depth-Filter Turbidity Recoveries - Single-Use ... [https://www.bioprocessintl.com/filtration/examining-single-use-harvest-clarification-options-a-case-study-comparing-depth-filter-turbidities-and-recoveries]
- 52. Reduction of Turbidity of Water Using Locally Available ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658559/]
- 53. High-throughput nephelometry methodology for qualitative determination of aqueous solubility of chemical libraries - PubMed [https://pubmed.ncbi.nlm.nih.gov/38492994/]
- 54. Dilute and shoot approach for toxicology testing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10749341/]
- 55. Why should I filter my samples instead of doing dilute-and- ... [https://www.biotage.com/blog/why-should-i-filter-my-samples-instead-of-doing-dilute-and-shoot]
- 56. Application of chemometrics for modeling and optimization ... [https://www.nature.com/articles/s41545-021-00113-6]
- 57. A 'Dilute and Shoot' Liquid Chromatography-Mass ... [https://www.mdpi.com/1660-4601/18/6/3068]
- 58. Development and validation of a 'dilute and shoot' LC-MS ... [https://pubmed.ncbi.nlm.nih.gov/40795634/]
- 59. 4 Strategies To Formulate Poorly Soluble APIs [https://www.drugdiscoveryonline.com/doc/strategies-to-formulate-poorly-soluble-apis-0001]
- 60. Solving Low Solubility Challenges to Optimize ... [https://drug-dev.com/bioavailability-enhancement-solving-low-solubility-challenges-to-optimize-drug-delivery-platforms/]
- 61. Formulation Development Strategies for Poorly Soluble ... [https://api.drreddys.com/article/effective-formulation-development-strategies-poorly-soluble-active-pharmaceutical]
- 62. Automated Nephelometric Turbidity Measurement of ... [https://www.labcompare.com/10-Featured-Articles/342759-Automated-Nephelometric-Turbidity-Measurement-of-Biotherapeutics-Formulationssample/]
- 63. Microplate Nephelometer - unique [https://www.bmglabtech.com/nephelometer/]
- 64. Bioavailability Enhancement Techniques for Poorly Aqueous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9495787/]
- 65. Static Light Scattering (SLS) [https://www.unchainedlabs.com/static-light-scattering/]
- 66. Static Light Scattering (SLS) - Absolute Molecular Weight ... [https://www.malvernpanalytical.com/en/products/technology/light-scattering/static-light-scattering]
- 67. Common artifacts and mistakes made in electrophoresis [https://pmc.ncbi.nlm.nih.gov/articles/PMC7295095/]
- 68. Optical Path Length Reduction [https://lsinstruments.ch/en/theory/dynamic-light-scattering-dls/optical-path-length-reduction]
- 69. Guide for Dynamic Light Scattering (DLS) sample preparation [https://www.brookhaveninstruments.com/guide-for-dls-sample-preparation/]
- 70. Improved Cross-Correlation Dynamic-Light-Scattering ... [https://www.techbriefs.com/component/content/article/29599-lew16781]
- 71. Tips on Dynamic Light Scattering Experiments [https://www.fireflysci.com/news/2015/6/1/tips-on-dynamic-light-scattering-experiments?srsltid=AfmBOop_Pr_zJSkflfk2Z61y9ySe44GmXBhDPVQA-sERkdTkt81Dr8pA]
- 72. Validation of a Next-Generation Single-Use Turbidity System [https://www.bioprocessintl.com/sponsored-content/validation-of-a-next-generation-single-use-turbidity-system]
- 73. Advances in Filtration Technology [https://www.biopharminternational.com/view/advances-in-filtration-technology]
- 74. Controlling the Stability of Medicinal Suspensions [https://www.americanpharmaceuticalreview.com/Featured-Articles/331619-Controlling-the-Stability-of-Medicinal-Suspensions/]
- 75. Fleck 2510 SXT Backwashing Granular Activated Carbon ... [https://flecksystems.com/products/fleck-2510-sxt-backwashing-granular-activated-carbon-filter]
- 76. Effect of filtration on elimination of turbidity and changes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6443810/]
- 77. Turbidity Guide: Measurements on light scattering ... [https://www.optek.com/en/turbidity-guide.asp]
- 78. Cyclodextrins: Enhancing Drug Delivery, Solubility and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11945013/]
- 79. Cyclodextrins: Advances in Chemistry, Toxicology, and ... [https://www.mdpi.com/1420-3049/29/22/5319]
- 80. Turbidity & Solubility [https://www.bmglabtech.com/en/turbidity-and-solubility/]
- 81. Drug Solubility: Importance and Enhancement Techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC3399483/]
- 82. Practical Aspects of Solvent Extraction [https://www.chromatographyonline.com/view/practical-aspects-solvent-extraction-1]
- 83. 4.5: Extraction Theory [https://chem.libretexts.org/Bookshelves/Organic_Chemistry/Organic_Chemistry_Lab_Techniques_(Nichols)/04%3A_Extraction/4.05%3A_Extraction_Theory]
- 84. Development of an Optimized Two-Step Solid-Phase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024844/]
- 85. The Power of Dual Extraction for Pre-Analytical Samples [https://cellcarta.com/science-hub/preanalytical-dual-extraction/]
- 86. Help for Your New Lab Techs: Avoiding Sample Prep ... [https://blog.omni-inc.com/blog/help-for-your-new-lab-techs-avoiding-sample-prep-mistakes]
- 87. Hygroscopic Problems Of Capsule Filled Powders [https://www.richpacking020.com/blog/hygroscopic-problems-of-capsule-filled-powders_b211]
- 88. Moisture protection for hygroscopic materials during transport [https://absortech.com/moisture-magazine/moisture-protection-for-hygroscopic-materials-during-transport/]
- 89. HPLC Troubleshooting: Precipitation of Buffers in Gradient ... [https://www.thermofisher.com/blog/analyteguru/hplc-troubleshooting-precipitation-of-buffers-in-gradient/]
- 90. Ultrasound-cavitation-enhanced drug delivery via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12013124/]
- 91. Effect of vortex fluidic device and its combined treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596217/]
- 92. Shakers or Mixers - What's best for my Lab? [https://www.biolabscientific.com/News/Shakers-or-Mixers--Whats-best-for-my-Lab/2023112001]
- 93. Comparison of Orbital Shaker vs. Vortex Mixer in ... [https://www.drawellanalytical.com/comparison-of-orbital-shaker-vs-vortex-mixer-in-laboratory-settings/]
- 94. Preparation and characterization of ultrasound-assisted ... [https://www.sciencedirect.com/science/article/pii/S2666154324000413]
- 95. Safety first: Considerations when formulating high potency ... [https://content.siegfried.ch/insights/safety-first-considerations-when-formulating-high-potency-compounds]
- 96. The rules on HPAPI containment in high potent ... [https://www.pharmaceutical-technology.com/sponsored/understanding-the-rules-on-hpapi-containment-in-high-potent-manufacturing/]
- 97. Measurement of Particle Size Distribution in Turbid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5409188/]
- 98. Why is my turbidity reading higher/lower than expected? [https://www.camlab.co.uk/blog/why-is-my-turbidity-reading-higher-lower-than-expected]
- 99. Key ICH Method Validation Parameters to Know [https://altabrisagroup.com/ich-method-validation-parameters/]
- 100. Enhancing Data Integrity Under EMA's Revised Annex 11 [https://www.rephine.com/resources/blog/enhancing-data-integrity-under-emas-revised-annex-11-audit-trail-alcoa-controls/]
- 101. GxP Compliance: A Comprehensive Guide to 2025 [https://www.compliancequest.com/what-is-gxp-compliance-with-fda-regulations/]
- 102. GxP Validation Process: What It Is And How to Implement It [https://www.sware.com/blog/gxp-validation-process]
- 103. GxP Validation: Overview and Best Practice Guide [https://www.leapwork.com/blog/how-to-secure-gxp-compliance-in-pharma-with-test-automation]
- 104. What is Nephelometry: Meaning & Examples [https://www.bmglabtech.com/en/nephelometry/]
- 105. Turbidity Sensor Troubleshooting and FAQs [https://www.vernier.com/til/1388?srsltid=AfmBOorpeuPxr25FPe1CTMd4oAGpPp753l9kwLfYr4UqVVALkc-Vhshl]
- 106. Nephelometry / Turbidity Analysis [https://www.coriolis-pharma.com/our-services/nephelometry-turbidity/]
- 107. Development and validation of a dynamic light scattering ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0324298]
- 108. How does nephelometry differ from turbidimetry? - Pearson [https://www.pearson.com/channels/microbiology/asset/20f341af/how-does-nephelometry-differ-from-turbidimetry]
- 109. Measuring the Opalescence of mAb Solutions with ... [https://www.wyatt.com/library/webinars/measuring-the-opalescence-of-mab-solutions-with-microscale-nephelometry.html]
- 110. Robustness Tests [https://www.chromatographyonline.com/view/robustness-tests]
- 111. Modelâ€based approach to sampling optimization in studies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8301546/]
- 112. Modeling and Simulation in Pediatric Drug Development [https://www.allucent.com/resources/blog/leveraging-modeling-and-simulation-pediatric-drug-development]
- 113. A Troubleshooting Guide for Topical Drug Manufacturing [https://www.pharmtech.com/view/troubleshooting-guide-topical-drug-manufacturing]
- 114. Visual inspection, accreditation of staff in “visually clean†[https://www.a3p.org/en/cleaning-validation-equipment/]
- 115. Understanding Cleaning Validation in Pharmaceutical ... [https://csanalytical.com/understanding-cleaning-validation-in-pharmaceutical-manufacturing/]
- 116. Cleaning validation in pharmaceutical quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229404/]
- 117. analysis | Anton Paar Wiki Turbidity [https://wiki.anton-paar.com/ae-en/turbidity-analysis/]
- 118. – Clarifying Low Level Measurements Turbidity [https://lamotte.com/technical-tips/post/turbidity-%E2%80%93-clarifying-low-level-measurements]