Optimizing Cryopreservation Protocols for Flow Cytometry: A Guide to Preserving Cell Viability and Data Integrity
This article provides a comprehensive guide for researchers and drug development professionals on cryopreserving cells for flow cytometry analysis.
Optimizing Cryopreservation Protocols for Flow Cytometry: A Guide to Preserving Cell Viability and Data Integrity
Abstract
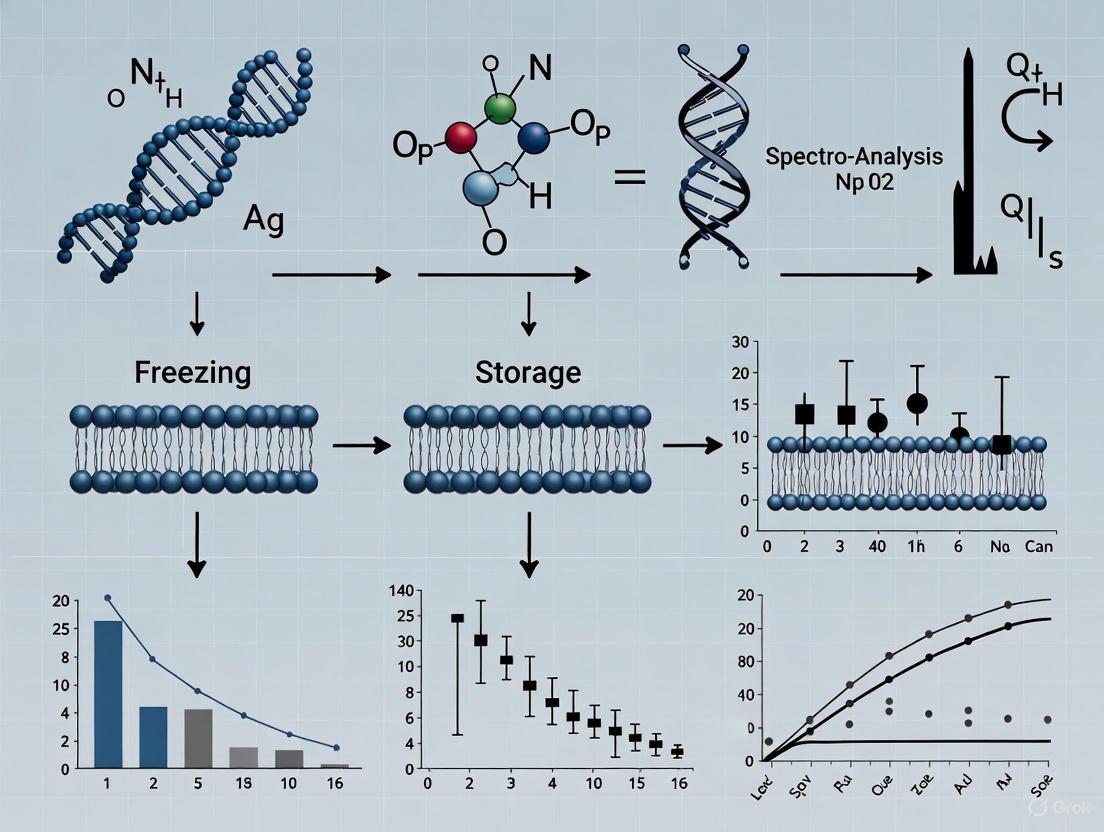
This article provides a comprehensive guide for researchers and drug development professionals on cryopreserving cells for flow cytometry analysis. It covers the foundational impact of freezing on cell viability and marker expression, details step-by-step protocols for PBMCs and other sample types, and offers troubleshooting for common issues like low viability and phenotypic shifts. Furthermore, it validates long-term storage stability and compares manual gating with emerging automated analysis methods, synthesizing current evidence to ensure reliable and reproducible immunophenotyping results from cryopreserved samples.
The Science of Cryopreservation: How Freezing Impacts Flow Cytometry Results
Cryopreservation of peripheral blood mononuclear cells (PBMCs) serves as a critical tool for standardizing immunophenotyping in multi-center flow cytometry studies. This application note details the fundamental principles, validated protocols, and key considerations for implementing cryopreservation workflows that maintain cell viability, recovery, and phenotypic integrity. By enabling batch analysis of samples collected across multiple sites and timepoints, cryopreservation significantly reduces inter-laboratory variability introduced by differing instrumental settings, operators, and analytical timelines. The procedures outlined herein provide researchers and drug development professionals with standardized methodologies to enhance data reproducibility and reliability in both clinical and research settings.
Cryopreservation has emerged as an indispensable methodology in flow cytometry-based research, particularly for multi-center clinical trials and large-scale cohort studies. The process involves preserving biological samples at cryogenic temperatures, effectively halting all biological activity while maintaining structural integrity for extended periods [1]. For immunophenotyping studies, cryopreservation of PBMCs enables simultaneous batch analysis of samples collected over time or across different geographical locations, thereby minimizing technical variability caused by day-to-day instrumental fluctuations or operator differences [2] [3].
The fundamental advantage of cryopreservation in multi-center flow cytometry studies lies in its capacity for standardization. When samples from various collection sites are processed and analyzed in a single, centralized laboratory using standardized protocols, inter-laboratory variability is substantially reduced [2] [4]. This approach is especially valuable in vaccine research, clinical trials for immunological conditions, and large-scale biobanking initiatives where comparable and reliable results between different institutions are paramount [3]. Furthermore, cryopreservation facilitates retrospective studies and allows multiple research centers to utilize identical sample sets, optimizing the use of limited biological resources [2].
Fundamental Principles of Cryopreservation
Successful cryopreservation relies on understanding and controlling several key physical and biological processes to minimize cellular damage during freezing and thawing.
Mechanisms of Cellular Damage
During cryopreservation, cells face two primary damage mechanisms:
- Intracellular Ice Crystal Formation: Rapid cooling leads to the formation of intracellular ice crystals, which can cause mechanical damage to cellular structures and membranes [3].
- Solution Effects and Osmotic Damage: As water freezes, solutes become concentrated in the remaining liquid, creating hypertonic conditions that draw water out of cells, leading to osmotic stress and potential membrane damage [3].
The two-factor hypothesis established by Mazur et al. describes the optimal freezing rate for successful cryopreservation, balancing these competing damage mechanisms [3].
Cryoprotective Agents
Cryoprotective agents (CPAs) are essential components of cryopreservation media that protect cells during freezing. The most commonly used CPA is dimethyl sulfoxide (DMSO), typically employed at concentrations of 10% in freezing media [2] [5]. DMSO functions by penetrating cells and reducing ice crystal formation, while extracellular CPAs like fetal calf serum (FCS) provide additional protection [2]. The composition of cryopreservation media varies but typically includes a base medium (such as RPMI-1640), 40-50% FCS, and 10% DMSO [2] [6].
Temperature Considerations
For long-term storage, samples should be maintained at temperatures below the glass transition temperature of -130°C to avoid biochemical reactions and recrystallization processes [3]. Storage in liquid nitrogen (-196°C) or its vapor phase (below -135°C) effectively preserves cellular integrity [3] [1]. Temperature stability during storage is critical, as repeated temperature fluctuations during storage, sorting, and removal can significantly impact cell viability, recovery, and functionality [3].
Effects of Cryopreservation on Flow Cytometric Analysis
Cell Viability and Recovery
The quality of cryopreserved samples is fundamentally assessed through viability and recovery rates. Studies demonstrate that optimized protocols can maintain high viability, though both parameters tend to decrease with increasing numbers of freeze-thaw cycles and suboptimal storage conditions [3] [6].
Table 1: Impact of Storage Conditions on PBMC Viability and Recovery
| Parameter | 50 Temperature Cycles | 100 Temperature Cycles | 400 Temperature Cycles |
|---|---|---|---|
| Viability | Significant decrease [3] | Progressive decrease [3] | Marked decrease [3] |
| Recovery | Significant decrease [3] | Progressive decrease [3] | Marked decrease [3] |
| T-cell Functionality | Significant effect [3] | Progressive decrease [3] | Marked impairment [3] |
Temperature cycles refer to fluctuations between -130°C and -60°C during storage.
Immunophenotyping Consistency
Recent evidence indicates that flow cytometric immunophenotyping shows minimal differences between freshly isolated and cryopreserved PBMCs for most lymphocyte populations [2].
Table 2: Comparison of Immune Cell Populations Between Fresh and Cryopreserved PBMCs
| Cell Population | Fresh vs. Cryopreserved PBMCs | Whole Blood vs. Cryopreserved PBMCs |
|---|---|---|
| CD4+ T-cells | No major differences [2] | Higher percentages in whole blood [2] |
| T-regulatory cells | No differences [2] | Higher proportions in whole blood [2] |
| CD8+ T-cells | No differences in naive, memory subsets [2] | Higher percentages in whole blood [2] |
| CD56+ NK cells | No differences [2] | Lower percentages in whole blood [2] |
| CD19+ B-cells | No differences [2] | Higher percentages in whole blood [2] |
| Monocyte subsets | No differences in classical/nonclassical [2] | Not reported |
Functional Assays and Transcriptomic Profiles
The effects of cryopreservation on functional assays require careful consideration. While immunophenotyping remains relatively stable, some functional responses may be affected. Studies indicate that cryopreservation can inhibit antigen-induced IL-2 secretion and PHA-induced IL-10 secretion, while augmenting spontaneous TNF-α secretion and PHA-induced IL-2 responses [4]. For transcriptomic analyses, optimized procedures demonstrate minimal effects on PBMC viability, population composition, and transcriptomic profiles after 6 or 12 months of storage, though scRNA-seq cell capture efficiency may decline by approximately 32% after 12 months [1].
Standardized Protocols for Multi-Center Studies
PBMC Isolation and Cryopreservation
Materials:
- Sodium-heparin or EDTA blood collection tubes
- Lymphocyte Separation Medium (e.g., Ficoll-Histopaque)
- Cryopreservation medium: 50% base medium (e.g., RPMI-1640), 40% FCS, 10% DMSO
- Controlled-rate freezer or isopropanol freezing containers
- Cryogenic vials
Procedure:
- Collect peripheral blood in sodium-heparin or EDTA tubes and process within 2-8 hours of collection.
- Isolate PBMCs using density gradient centrifugation with Ficoll-Histopaque:
- Centrifuge well-mixed blood samples for 20 minutes at 1500× g at room temperature.
- Collect the PBMC layer and wash twice in phosphate-buffered saline supplemented with 2% FCS.
- Resuspend the final cell pellet in 1 mL of appropriate medium.
- Prepare cells for cryopreservation:
- Adjust cell concentration to 5-10 × 10^6 cells/mL in cryopreservation medium.
- Add cold cryopreservation medium dropwise to cell suspensions under continuous mixing.
- Aliquot 1 mL of cell suspension into cryotubes.
- Freeze cells using a controlled cooling rate:
- Use a controlled-rate freezer or freezing container (e.g., "Mr. Frosty") precooled to +4°C.
- Freeze at a controlled cooling rate of -1°C/min from +4°C to -80°C.
- Transfer cryopreserved samples to long-term storage:
Thawing and Recovery
Materials:
- 37°C water bath
- Pre-warmed complete medium: RPMI-1640 with 10% FCS and supplements
- Centrifuge
Procedure:
- Rapidly thaw cryopreserved vials in a 37°C water bath with gentle agitation until a small ice crystal remains.
- Transfer cell suspension to a tube containing 10 mL of pre-warmed complete medium.
- Centrifuge at 400-500 × g for 5-10 minutes at room temperature.
- Discard supernatant and gently resuspend cell pellet in fresh complete medium.
- Allow cells to rest for 60 minutes at room temperature before proceeding with flow cytometry staining or functional assays [2] [1].
Cryopreservation Workflow for Flow Cytometry
Essential Research Reagents and Materials
Table 3: Essential Reagents for Cryopreservation and Flow Cytometry
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Density Gradient Medium (Ficoll) | Isolation of PBMCs from whole blood | Separates mononuclear cells from granulocytes and erythrocytes [2] |
| Dimethyl Sulfoxide (DMSO) | Cryoprotective agent | Prevents intracellular ice crystal formation; typically used at 10% concentration [2] [5] |
| Fetal Calf Serum (FCS) | Extracellular cryoprotectant | Provides additional protection during freezing; typically 40-50% in cryomedium [2] |
| Controlled-Rate Freezer | Controlled freezing | Ensures optimal cooling rate of -1°C/min; alternatives include isopropanol containers [3] [7] |
| Cryogenic Vials | Sample storage | Designed for low-temperature storage; ensure proper sealing [2] |
| Liquid Nitrogen Storage System | Long-term sample preservation | Maintains temperatures below -135°C; vapor phase minimizes contamination risk [3] [1] |
| Flow Cytometry Antibody Panels | Cell population identification | Validate antibodies post-cryopreservation; some epitopes may be affected [2] [6] |
Advanced Considerations for Standardization
Temperature Management During Storage
Temperature stability during storage is crucial for maintaining sample quality. Studies demonstrate that repeated temperature fluctuations during storage significantly impact PBMC viability, recovery, and T-cell functionality [3]. Exposure to as few as 50 temperature cycles (between -130°C and -60°C) can cause significant detrimental effects, with all parameters progressively decreasing as cycle numbers increase [3]. These findings highlight the importance of maintaining consistent storage temperatures and minimizing unnecessary handling of cryopreserved samples.
Analysis Methodologies
Advances in flow cytometry data analysis methodologies offer improved standardization for cryopreserved samples. Traditional manual gating approaches are susceptible to subjective bias, particularly with complex multicolor panels [6]. Automated algorithmic analysis methods, such as UMAP and FlowSOM, provide enhanced reproducibility and objectivity in analyzing cryopreserved samples [6]. These computational approaches can better identify spatial relationships between cell populations and reduce analyst-derived variability, which is especially valuable in multi-center studies [8] [6].
Standardization Benefits in Multi-Center Studies
Cryopreservation represents a robust methodology for standardizing multi-center flow cytometry studies when implemented using optimized, standardized protocols. When properly executed, cryopreservation maintains the integrity of most immune cell populations for immunophenotyping analyses while enabling the batch processing essential for reducing technical variability across sites. Successful implementation requires careful attention to each step of the process—from sample collection and controlled-rate freezing to stable storage conditions and standardized thawing procedures. As flow cytometry technologies continue to advance, incorporating automated analysis methods and maintaining rigorous quality control throughout the cryopreservation workflow will further enhance data reproducibility and reliability in multi-center research initiatives.
For researchers, scientists, and drug development professionals working with cellular samples, cryopreservation represents a fundamental enabling technology for flow cytometry studies, biobanking, and cell-based therapies. The process allows for the long-term storage of cells and tissues by suspending cellular metabolism at cryogenic temperatures (typically -80°C to -196°C) [9]. While essential for preserving cellular material for future analysis, the cryopreservation process introduces two primary, interconnected challenges that can significantly compromise sample viability and functionality: ice crystallization and osmotic stress [10] [11]. Understanding these mechanisms is crucial for developing optimized protocols that maintain cell integrity, viability, and phenotypic stability—attributes paramount for reliable flow cytometry data and downstream applications.
This application note examines the fundamental cryoinjury mechanisms and provides detailed, practical methodologies to mitigate these challenges within the context of cryopreserving samples for flow cytometry analysis. By implementing these evidence-based protocols, researchers can significantly enhance the quality and reproducibility of their cryopreserved samples.
Fundamental Mechanisms of Cryoinjury
Ice Crystallization and Its Consequences
Ice crystallization presents a multifactorial threat to cellular integrity during both freezing and thawing processes. The formation of ice crystals can be extracellular, intracellular, or occur during the dangerous phase of recrystallization upon warming [10] [11].
- Extracellular Ice Formation: As the temperature drops below 0°C, ice crystals initially form in the extracellular solution. This formation excludes solutes, leading to a progressive increase in the solute concentration of the remaining unfrozen fluid. Cells become trapped in the narrowing liquid-filled channels between growing ice crystals, subjecting them to mechanical shear forces and deformation that can disrupt membrane integrity [10] [11].
- Intracellular Ice Formation: With rapid cooling rates, intracellular water does not have sufficient time to exit the cell. Consequently, it freezes internally, forming ice crystals that can mechanically damage organelles, the cytoskeleton, and other critical cellular structures. This intracellular ice formation is typically lethal to cells [11].
- Recrystallization: During the thawing process, particularly when warming rates are suboptimal, small ice crystals undergo recrystallization. This phenomenon involves the growth of larger, more damaging ice crystals at the expense of smaller ones as the system seeks to minimize its surface energy. Recrystallization can cause significant mechanical damage during the critical phase when cells are emerging from their preserved state [10] [12].
Table 1: Types of Ice-Related Cryoinjury and Their Effects on Cells
| Type of Ice Formation | Phase of Occurrence | Primary Consequence | Resulting Cellular Damage |
|---|---|---|---|
| Extracellular Ice | Cooling | Mechanical stress & solute concentration | Membrane deformation, osmotic injury, protein denaturation [10] [11] |
| Intracellular Ice | Rapid Cooling | Mechanical disruption of internal structures | Organelle damage, cytoskeleton disruption, lethal cell injury [11] |
| Recrystallization | Warming/Thawing | Growth of larger ice crystals | Mechanical damage to partially thawed cells, reduced viability [10] [12] |
Osmotic Stress and Solution Effects
Osmotic stress, also referred to as "solution effects" injury, is intrinsically linked to ice formation. As extracellular water freezes, solutes (salts, metabolites) become concentrated in the diminishing volume of unfrozen solution [10] [13]. This creates a severe hypertonic environment outside the cell.
In response to this elevated external osmolarity, water rapidly moves out of the cell down its osmotic gradient, leading to profound cellular dehydration and shrinkage. A cell can lose up to 90% of its water content during conventional slow freezing [11]. This dehydration has several detrimental effects:
- Membrane Stress: The massive loss of volume places considerable mechanical stress on the plasma membrane, potentially leading to lysis or irreversible damage.
- Protein Denaturation: The high intracellular solute concentration can disrupt the hydration shells of proteins and other macromolecules, leading to their denaturation and functional impairment [11].
- pH Changes: The concentration of buffering components can lead to drastic shifts in pH, further disrupting cellular biochemistry.
The relationship between cooling rate and these two injury mechanisms is described by the "two-factor hypothesis" of cryoinjury, as illustrated below [10].
Quantitative Impact on Cell Viability and Function
The detrimental effects of ice crystallization and osmotic stress are not merely theoretical; they manifest as quantifiable losses in cell yield, viability, and functionality—key concerns for any flow cytometry-based assay.
- Viability and Recovery: Studies on peripheral blood mononuclear cells (PBMCs) have shown that while recovery and viability can remain stable after long-term cryopreservation, the numbers of certain innate immune cells (e.g., monocytes and B cells) can be significantly reduced compared to freshly isolated samples [14]. The freeze-thaw process itself can lead to a slight decrease in both cell number and viability, with these effects becoming more pronounced with increased cryopreservation time and repeated freeze-thaw cycles [6].
- Functional Impairment: Perhaps more critical than simple viability is the preservation of cellular function. Research on porcine PBMCs demonstrated that cryopreservation can significantly impair antigen-specific responses. For instance, the frequency of IFN-γ-secreting cells in response to a specific viral antigen was notably decreased in frozen cells compared to their fresh counterparts. Similarly, proliferation assays, particularly for memory T-cell subsets, showed significantly reduced responses after thawing [15]. This indicates that effector and memory cell functions may be more susceptible to cryopreservation damage than those of naïve cells.
- Phenotypic Alterations: Flow cytometric analysis has revealed that cryopreservation can dynamically alter the proportions of certain T-cell subsets, including activated T, naïve T, and central memory T cells, even if the broad proportions of major subtypes (e.g., CD4+ and CD8+) remain stable [14]. This underscores the importance of standardizing cryopreservation protocols to minimize pre-analytical variables in immunophenotyping studies.
Table 2: Documented Impacts of Cryopreservation on Various Cell Parameters
| Cell Parameter | Impact of Cryopreservation | Experimental Evidence |
|---|---|---|
| Overall Viability | Slight decrease post-thaw; declines with time/cycles [6] | Trypan blue exclusion; >89% viability possible with optimized media [15] |
| Monocyte & B Cell Counts | Significant reduction post-thaw [14] | Flow cytometry of PBMCs from healthy donors |
| T Cell Subset Proportions | Dynamic changes in naïve, memory, activated subsets [14] | Multi-parameter flow cytometry with longitudinal tracking |
| Antigen-Specific Response | Significant impairment, especially in memory cells [15] | IFN-γ ELISPOT and proliferation assays post-thaw |
| Proliferative Capacity | Reduced response to specific mitogens (e.g., Con A) [15] | CFSE-based proliferation assays |
Essential Protocols for Mitigating Cryoinjury
Standard Protocol for PBMC Cryopreservation
This protocol is optimized for the preservation of human Peripheral Blood Mononuclear Cells (PBMCs) to maintain high viability and functionality for flow cytometry and immunological assays [9] [16].
Principles: The protocol utilizes slow, controlled-rate cooling to minimize intracellular ice formation and a cryoprotectant solution containing DMSO to mitigate osmotic stress and solution effects.
Materials:
- Supplies: Ficoll-Paque PLUS or equivalent density gradient medium; Phosphate-buffered saline (PBS); Fetal Bovine Serum (FBS); Dimethyl Sulfoxide (DMSO); Cryogenic vials (externally threaded); 50 mL conical centrifuge tubes.
- Equipment: Refrigerated centrifuge with swinging bucket rotor; Biosafety Cabinet (Class II); Controlled-rate freezing device (e.g., isopropanol freezer like "Mr. Frosty" or a programmable freezer); -80°C freezer; Liquid nitrogen storage tank.
Procedure:
- Isolate PBMCs: Isolate PBMCs from whole blood using standard density gradient centrifugation with Ficoll-Paque [14] [16].
- Wash and Count: Wash the isolated PBMCs twice in PBS. Perform a cell count and viability assessment using trypan blue exclusion. Adjust cell concentration to 10-20 x 10ⶠcells/mL in a cold culture medium (e.g., RPMI-1640 with 10% FBS) [16].
- Prepare Cryopreservation Medium: Prepare a cryoprotectant solution of 90% FBS and 10% DMSO. Keep this solution cold (4°C) to reduce DMSO toxicity [15] [16]. Commercially available, serum-free alternatives like CryoStor CS10 are highly recommended for greater consistency and reduced variability [9] [15].
- Combine Cell Suspension with Cryoprotectant: Gently add an equal volume of the cold cryopreservation medium to the cell suspension dropwise, while gently swirling the tube. This gradual addition prevents osmotic shock. The final concentration will be 5-10 x 10ⶠcells/mL in a solution containing 95% FBS / 5% DMSO or the commercial cryomedium [16].
- Aliquot and Begin Freezing: Quickly aliquot 1 mL of the cell suspension into each pre-chilled cryogenic vial. Place the vials immediately into a controlled-rate freezing device and transfer them to a -80°C freezer for 18-24 hours. The controlled-rate device ensures an optimal cooling rate of approximately -1°C per minute [9] [12].
- Long-Term Storage: After 24 hours, promptly transfer the cryovials to a liquid nitrogen storage system (-135°C to -196°C) for long-term preservation. Avoid storage at -80°C for extended periods, as viability degrades over time at this temperature [9].
Optimized Thawing Protocol for Functional Assays
Rapid and careful thawing is critical to minimize the damaging effects of ice recrystallization.
Procedure:
- Rapid Thawing: Remove the cryovial from liquid nitrogen and immediately place it in a 37°C water bath with gentle agitation. Thawing should be rapid, typically requiring 1-2 minutes. Ensure the vial's cap remains above the water level to maintain sterility [14] [9].
- Dilution and Washing: Immediately upon thawing, wipe the vial with 70% ethanol. Transfer the cell suspension dropwise into a 15 mL tube containing 10 mL of pre-warmed complete culture medium. This large-volume dilution gradually reduces the concentration of DMSO, preventing osmotic shock as the cryoprotectant diffuses out of the cell [14].
- Centrifuge and Resuspend: Centrifuge the cell suspension at 300-400 x g for 10 minutes. Carefully decant the supernatant containing the DMSO and resuspend the cell pellet in fresh, pre-warmed culture medium [16].
- Post-Thaw Rest (Critical Step): For functional assays, it is highly recommended to resuspend the washed cells in complete medium and incubate them for 4-8 hours (or overnight) in a standard cell culture incubator (37°C, 5% CO₂) before proceeding with stimulation or staining. This "resting" period allows cells to recover from osmotic stress, repair membrane damage, and restore metabolic homeostasis, leading to more reliable functionality in downstream assays [14].
The complete workflow, from isolation to final application, is summarized below.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Cryopreservation
| Reagent/Material | Function & Rationale | Application Notes |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Permeating Cryoprotectant Agent (CPA). Penetrates the cell, reduces ice crystal formation by hydrogen bonding with water, and depresses the freezing point [13] [11]. | Standard final concentration: 5-10%. Can be toxic; use pre-chilled and limit exposure time at room temperature [11] [9]. |
| CryoStor CS10 | A commercially available, serum-free, GMP-manufactured cryopreservation medium. Contains 10% DMSO in an optimized, defined solution [9] [15]. | Provides high, reproducible post-thaw viability and function. Reduces lot-to-lot variability and safety concerns associated with FBS [9]. |
| Fetal Bovine Serum (FBS) | Non-permeating agent and base for homemade freezing media. Provides extracellular cryoprotection and helps stabilize cell membranes [16]. | Subject to variability; heat-inactivation is recommended. Use at 90% concentration in homemade DMSO mixtures [16]. |
| Controlled-Rate Freezer (e.g., Mr. Frosty) | Device to ensure an optimal, consistent cooling rate of -1°C/minute, which is critical for balancing intracellular ice formation and osmotic stress [9] [12]. | Essential for protocol standardization. Isopropanol-based containers provide a simple and reliable method for achieving this rate in a -80°C freezer [9]. |
| Programmable Freezer | Advanced equipment that provides precise control over cooling rates and can initiate "ice nucleation" at a specific temperature, improving consistency for large or sensitive samples. | Used in advanced therapeutic and GMP settings for high-value samples like cell therapy products [17]. |
| Trehalose | Non-permeating disaccharide sugar. Acts as a natural osmoprotectant; can stabilize membranes and proteins in a dehydrated state by forming a glassy matrix [13]. | Investigated for delivery into cells to provide intracellular protection without the toxicity of permeating CPAs [10] [13]. |
| Leteprinim Potassium | Leteprinim Potassium, CAS:192564-13-9, MF:C15H12KN5O4, MW:365.38 g/mol | Chemical Reagent |
| Xanthoanthrafil | Xanthoanthrafil | High-Purity Research Compound | Xanthoanthrafil for research applications. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Ice crystallization and osmotic stress represent the principal physical-chemical challenges in cellular cryopreservation, directly impacting the viability, recovery, and most importantly, the functionality of samples critical for flow cytometry and drug development research. A deep understanding of these mechanisms—extracellular/intracellular ice formation, recrystallization, and solute-induced damage—is fundamental to developing effective preservation strategies.
By adhering to the detailed protocols outlined in this application note, particularly the use of optimized cryoprotectants, a controlled slow cooling rate of -1°C/minute, and a rapid thaw followed by a post-thaw rest period, researchers can significantly mitigate these sources of cryoinjury. Standardizing these practices across experiments and laboratories ensures the generation of high-quality, reliable, and reproducible data from cryopreserved samples, thereby upholding the integrity of research and development pipelines in biomedicine.
Cryopreservation represents a critical step in the workflow of translational research and clinical applications of cellular therapies. While it enables long-term storage and logistical flexibility, the process of freezing and thawing cells can induce significant changes in their immunophenotype, potentially altering the outcomes of flow cytometry analyses and the perceived biological characteristics of cell-based products. This application note systematically examines the effects of cryopreservation on key immunophenotypic markers—focusing on the classical mesenchymal stromal cell (MSC) marker CD105 and the immunomodulatory marker CD274 (PD-L1)—across different cell types. We present consolidated quantitative data, detailed experimental protocols for assessing marker stability, and essential reagent solutions to support robust pre- and post-thaw cell characterization within the broader context of optimizing cryopreservation protocols for flow cytometry samples.
The following tables synthesize findings from recent studies on how cryopreservation impacts the expression and detection of critical surface markers.
Table 1: Effects of Cryopreservation on Classical and Non-Classical MSC Markers
| Cell Type | Marker | Post-Thaw Change | Key Findings | Reference |
|---|---|---|---|---|
| Umbilical Cord MSCs (UCX) | CD105, CD90, CD73 | No significant change | Phenotype maintained after cryopreservation and thawing; high viability recovery. | [18] |
| Adipose-Derived MSCs (ASCs) | CD274 (PD-L1), CD146 | Emergence of stable lineages | CD274+ and CD274+CD146+ subpopulations become dominant after passage 4, suggesting selective survival or adaptation. | [19] |
| Adipose-Derived MSCs (ASCs) | CD274 (PD-L1) | Variable expression | Identified as a non-classical marker showing variability among donors and culture conditions. | [20] |
Table 2: Effects of Cryopreservation on Immune Cell Markers in PBMCs and Murine Splenocytes
| Cell Type | Marker / Population | Post-Thaw Change | Key Findings | Reference |
|---|---|---|---|---|
| Mouse Splenocytes (T-cells) | CD3, CD4, CD8 | Minor change (short-term) | No significant change in subpopulation proportions after 2 weeks of cryopreservation. | [6] |
| Mouse Splenocytes (T-cells) | CD3, CD4, CD8 | Significant change (long-term) | Significant alterations with increased cryopreservation time and freeze-thaw cycles. | [6] |
| Human PBMCs | Transcriptome Profile | Minimal perturbation | No substantial transcriptome changes after 6 or 12 months; key stress genes showed <2-fold change. | [1] |
Detailed Experimental Protocols
To ensure the reliability and reproducibility of surface marker analysis following cryopreservation, adherence to standardized protocols is paramount. The following sections detail critical procedures for cell thawing, staining, and data analysis.
Protocol: Thawing and Recovery of Cryopreserved PBMCs
This protocol is adapted from the HANC/IMPAACT PBMC Thawing SOP and recent research to maximize viability and preserve immunophenotype [1] [21].
Key Materials:
- Pre-warmed RP10 Medium: RPMI-1640 supplemented with 10% heat-inactivated Fetal Bovine Serum (FBS), 10 mM HEPES, and 0.1 mg/mL Gentamycin.
- Water bath (37°C)
- Centrifuge
Procedure:
- Rapid Thawing: Remove the cryovial from liquid nitrogen storage and immediately place it in a 37°C water bath. Gently agitate until only a small ice crystal remains.
- Dilution: Gently transfer the cell suspension to a 15 mL conical tube containing 10 mL of pre-warmed RP10 medium. Pipette gently 2-3 times to mix.
- Centrifugation: Centrifuge the cell suspension at 500 x g for 5 minutes at room temperature.
- Supernatant Removal: Carefully decant the supernatant. Gently tap the tube to break up the cell pellet.
- Washing: Resuspend the cells in 10 mL of pre-warmed RP10 medium. Repeat the centrifugation step (500 x g, 5 minutes).
- Resuspension and Counting: Resuspend the cell pellet in an appropriate volume of culture medium or staining buffer. Count cells and assess viability using trypan blue exclusion or a similar method.
Protocol: Multicolor Flow Cytometry for Dim Epitopes
The accurate detection of dimly expressed markers like CD274 requires careful panel design and instrument setup [19].
Key Materials:
- Fluorescence-conjugated antibodies (see Section 5 for reagents)
- Fixable Viability Stain
- Flow cytometer with multiple lasers (e.g., MoFlo Astrios EQ)
- Brilliant Stain Buffer (to mitigate fluorochrome polymer formation)
Procedure:
- Panel Design: Sort antibodies into panels based on brightness. Resolve bright markers (e.g., CD73, CD90) and dim markers (e.g., CD34, CD274, CD146) into separate panels to minimize spectral overlap and spillover.
- Instrument Setup: Fine-tune fluidics and photomultiplier tube (PMT) voltage using unstained cells and rainbow calibration particles. Set voltages to ensure dim signals are above electronic noise but within the linear range.
- Staining:
- Viability Staining: Stain cells with Fixable Viability Stain for 15 minutes at room temperature, protected from light.
- Surface Staining: Incubate cells with titrated antibody cocktails diluted in Brilliant Stain Buffer for 30 minutes at 4°C.
- Acquisition and Analysis: Resuspend stained cells in staining buffer and acquire data immediately. Use fluorescence-minus-one (FMO) controls to set accurate gating boundaries for dim markers.
Protocol: Automated Algorithmic Analysis of Flow Cytometry Data
Traditional manual gating can introduce subjective bias. Automated analysis improves objectivity, especially for complex post-thaw data [6].
Software:
- FlowJo (v10.8.1 or higher) with plugins for UMAP and FlowSOM.
Procedure:
- Data Preprocessing: Apply compensation and perform logicle transformation on the concatenated flow cytometry data files.
- Downsampling: Downsample live cell events from all samples to an equal number (e.g., 10,000 events per sample) to ensure equal weighting in the analysis.
- Dimensionality Reduction (UMAP): Run UMAP analysis with default settings (nearest neighbors: 15, minimum distance: 0.5) using the Euclidean distance function.
- Clustering (FlowSOM): Run the FlowSOM algorithm on the concatenated data. Perform meta-clustering to merge similar nodes, setting the number of meta-clusters based on the expected populations (e.g., 6).
- Visualization and Interpretation: Superimpose the FlowSOM clusters onto the UMAP plot. Generate a heatmap of surface marker expression to interpret the identity of the automated clusters.
Experimental Workflow and Signaling Pathway Diagrams
Experimental Workflow for Surface Marker Stability Analysis
PD-1/PD-L1 Signaling and Regulatory Mechanisms
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Pre- and Post-Thaw Surface Marker Analysis
| Reagent / Material | Function / Application | Example Product / Specification |
|---|---|---|
| Anti-Mouse CD274 (PD-L1) | Flow cytometric detection of mouse PD-L1 on activated splenocytes. | BD OptiBuild RB705, Clone MIH5 (Cat. No. 758168) [22] |
| Human Platelet Lysate (hPL) | Xeno-free cell culture medium supplement for clinical-grade MSC expansion. | GMP-grade, heparin-free (e.g., PLTGold from Sigma-Aldrich) [20] [19] |
| Cryopreservation Medium | Protects cells during freezing; composition critical for post-thaw recovery. | 50% DMEM, 40% FBS, 10% DMSO or Commercial Serum-Free Formulations [6] |
| Multicolor Flow Cytometry Antibody Panels | High-resolution immunophenotyping of complex co-expression patterns. | Pre-designed or custom panels with bright/dim markers resolved [19] |
| Viability Stain | Discrimination of live/dead cells for accurate flow cytometry gating. | Fixable Viability Stain 570 (BD Biosciences) [19] |
| Stain Buffer | Provides optimal pH and protein background for antibody staining. | BD Stain Buffer (BSA) (Cat. No. 554657) [22] |
| Finafloxacin hydrochloride | Finafloxacin hydrochloride, CAS:209342-41-6, MF:C20H20ClFN4O4, MW:434.8 g/mol | Chemical Reagent |
| Aminooxyacetic acid hemihydrochloride | Aminooxyacetic acid hemihydrochloride, CAS:2921-14-4, MF:C4H11ClN2O6, MW:218.59 g/mol | Chemical Reagent |
Cryopreservation is a fundamental process in biomedical research and clinical applications, enabling long-term storage of cellular specimens. However, the freeze-thaw process can introduce significant technical artifacts that compromise data integrity. This application note examines cryopreservation-induced cellular heterogeneity, focusing on measurable shifts in immune cell subpopulations and functional characteristics that are critical for accurate flow cytometry analysis and drug development research. We present standardized protocols and analytical frameworks to identify, quantify, and mitigate these effects, ensuring specimen quality and data reliability in both research and clinical settings.
Quantitative Analysis of Cryopreservation Effects
Impact on Cell Viability and Recovery
Table 1: Effects of Cryopreservation on PBMC Viability and Recovery Over Time
| Storage Duration | Post-Thaw Viability | Cell Recovery | scRNA-seq Capture Efficiency | Key Findings |
|---|---|---|---|---|
| 3 weeks (M0) | 91-97% [23] | N/R | N/R | Media with DMSO <7.5% show significant viability loss [24] |
| 6 months | Relatively stable [25] | N/R | Minimal decline [25] | Cell population composition remains stable [25] |
| 12 months | Relatively stable [25] [26] | N/R | ~32% decline [25] [26] | Transcriptome profiles show minimal perturbation [25] |
| 2 years | Maintained in CS10 & NutriFreez D10 [24] | Maintained in CS10 & NutriFreez D10 [24] | N/R | T-cell functionality preserved in optimal media [24] |
N/R = Not Reported in the cited studies
Shifts in Immune Cell Subpopulations
Table 2: Changes in Immune Cell Subpopulations Post-Cryopreservation
| Cell Type | Impact of Cryopreservation | Functional Consequences |
|---|---|---|
| Lymphocytes | Higher proportion in cryopreserved leukapheresis (66.59%) vs PBMCs (52.20%) [23] | Potential advantage for T-cell therapies [23] |
| T Cells | Proportion maintained post-thaw (42.01-51.21%) [23] | CAR-T manufacturing potential preserved [23] |
| Monocytes | No significant difference in proportion post-cryopreservation [23] | Maintained antigen presentation capability [25] |
| All Major Immune Cells (Monocytes, DCs, NK, CD4+ T, CD8+ T, B cells) | Population composition stable after 6 & 12 months [25] [26] | Minimal effects on overall immune profiling [25] |
Experimental Protocols
Optimized PBMC Cryopreservation and Thawing Protocol
Materials:
- Lymphocyte Separation Medium (e.g., Lymphoprep)
- Cryopreservation medium (e.g., CryoStor CS10 or FBS + 10% DMSO)
- Pre-warmed RP10 medium (RPMI1640 + 10% FBS + 10mM HEPES + 0.1 mg/mL Gentamycin)
- CryoELITE cryogenic vials
- Controlled-rate freezer (e.g., CryoMed Freezer)
- 37°C water bath
Procedure:
- Isolation: Isolate PBMCs from whole blood using density gradient centrifugation with Lymphocyte Separation Medium [25]
- Freezing Medium Preparation: Resuspend PBMCs at 100×10ⶠcells/mL in Recovery cell Culture Freezing Medium or similar cryoprotectant [25]
- * Controlled-Rate Freezing*:
- Thawing:
Flow Cytometry Staining with Blocking Protocol
Materials:
- Mouse serum (Thermo Fisher, cat. no. 10410)
- Rat serum (Thermo Fisher, cat. no. 10710C)
- Tandem stabilizer (BioLegend, cat. no. 421802)
- Brilliant Stain Buffer (Thermo Fisher, cat. no. 00-4409-75)
- FACS buffer (PBS + 2% BSA)
- FC-blocking medium (BD Biosciences, cat. no. 564219)
- Fluorochrome-conjugated antibodies
Procedure:
- Sample Preparation: Dispense cells into V-bottom, 96-well plates (5×10âµ-1×10ⶠcells/well) and centrifuge at 300 × g for 5 minutes [27]
- Blocking:
- Surface Staining:
- Washing and Acquisition:
Signaling Pathways and Molecular Mechanisms
Cryopreservation Stress Pathways: This diagram illustrates the molecular mechanisms through which cryopreservation induces cellular stress, leading to transcriptomic changes and functional effects, along with potential mitigation strategies.
Research Reagent Solutions
Table 3: Essential Reagents for Cryopreservation and Flow Cytometry
| Reagent Category | Specific Products | Function & Application |
|---|---|---|
| Cryopreservation Media | CryoStor CS10 [24], NutriFreez D10 [24], FBS + 10% DMSO [25] | Cell protection during freeze-thaw cycle; CS10 shows excellent 2-year viability [24] |
| Serum-Free Alternatives | Bambanker D10 [24], Stem-Cellbanker D0 [24] | Avoid FBS ethical concerns and variability; suitable for clinical applications [24] |
| Flow Cytometry Blocking | Mouse serum [27], Rat serum [27], Brilliant Stain Buffer [27] | Reduce non-specific antibody binding; improve signal-to-noise ratio [27] |
| Viability Assessment | Trypan Blue [25], Propidium Iodide [25], Live/Dead Fixable Violet [25] | Distinguish live/dead cells; assess cryopreservation success |
| Cell Separation | Lymphocyte Separation Medium [25], Lymphoprep [24] | PBMC isolation from whole blood prior to cryopreservation |
Workflow for Assessing Cryopreservation Effects
Cryopreservation Assessment Workflow: This workflow outlines the comprehensive process for evaluating cryopreservation-induced heterogeneity, from cell preparation through advanced analytical techniques.
This application note demonstrates that while cryopreservation inevitably induces cellular stress and some functional changes, optimized protocols can effectively minimize technical artifacts. Critical factors include the use of standardized cryopreservation media with appropriate DMSO concentrations (≥7.5%), implementation of controlled-rate freezing, proper thawing techniques, and rigorous blocking protocols for flow cytometry. By adopting these standardized methodologies, researchers can reliably preserve cell viability, maintain population heterogeneity, and ensure functional integrity for drug development and clinical applications.
Step-by-Step: Optimized Cryopreservation Protocols for High-Quality Flow Cytometry
Cryopreservation is a cornerstone technology for the long-term storage of cells in immunological research, clinical trials, and biobanking [28]. The stability of cell samples, particularly for subsequent flow cytometric analysis, is heavily dependent on the chosen cryopreservation protocol. The selection of an appropriate cryoprotectant is critical to maintain cell viability, recovery, and most importantly, the phenotypic and functional characteristics of the original cell population [29] [6]. This application note focuses on two pivotal variables in protocol optimization: the concentration of the penetrating cryoprotectant dimethyl sulfoxide (DMSO) and the choice between fetal bovine serum (FBS)-based and serum-free freezing media. Framed within the context of flow cytometry sample research, we provide a structured comparison of these conditions, supported by recent quantitative data and detailed, actionable protocols.
Comparative Data Analysis: DMSO Concentration and Media Composition
The decision between using a standard 10% DMSO concentration or a reduced 5% concentration, and between FBS-based or serum-free media, involves balancing cell recovery against potential toxicity and variability. The tables below summarize key findings from recent investigations to guide this decision.
Table 1: Impact of DMSO Concentration on Post-Thaw Outcomes in Different Cell Types
| Cell Type | DMSO Concentration | Key Findings | Source |
|---|---|---|---|
| Peripheral Blood Mononuclear Cells (PBMCs) | < 7.5% | Significant loss of cell viability; eliminated from study after initial assessment. | [28] |
| PBMCs | 10% | Maintained high cell viability and functionality over a 2-year cryostorage period. | [28] |
| Hematopoietic Stem Cells (HSCs) - Autologous Transplants | 10% (Standard) | No significant difference in CD34+ cell viability or engraftment kinetics compared to lower concentrations. | [30] |
| Hematopoietic Stem Cells (HSCs) - Autologous Transplants | 5% (Reduced) | No significant difference in CD34+ cell viability or engraftment kinetics compared to standard 10%. | [30] |
| Umbilical Cord Blood (UCB) Stem Cells | 2.5% + 30 mmol/L Trehalose | Higher cell viability and colony-forming units (CFUs), lower apoptosis rate post-thaw compared to 10% DMSO formulas. | [31] |
Table 2: Comparison of Serum-Free and FBS-Based Cryomedia for PBMCs
| Media Type | Specific Formulation | Performance Summary | Key Advantages | Source |
|---|---|---|---|---|
| Serum-Free | CryoStor CS10 (10% DMSO) | High viability & functionality comparable to FBS10 reference medium across 2 years. | Standardized, no batch variability, no import restrictions, avoids FBS ethical concerns. | [28] [29] |
| Serum-Free | NutriFreez D10 (10% DMSO) | High viability & functionality comparable to FBS10 reference medium across 2 years. | Standardized, no batch variability, no import restrictions, avoids FBS ethical concerns. | [28] |
| FBS-Based | 90% FBS + 10% DMSO | Effective for preservation but carries risk of unspecific immune activation and batch-to-batch variability. | Historically the "gold standard," rich in growth factors. | [28] [29] |
| Serum-Free with Reduced DMSO | 12.5% BSA + 6% HES + 5% DMSO | PBMC recovery >83%, viability >98%, optimal T-cell functionality in ELISpot. | Reduces cytotoxic and mutagenic DMSO content. | [29] |
Recommended Protocols for Flow Cytometry Sample Cryopreservation
Protocol A: Cryopreservation of PBMCs Using Serum-Free Media with 10% DMSO
This protocol is adapted from a 2025 study that validated long-term storage efficacy [28].
Step 1: Cell Preparation
- Isolate PBMCs from whole blood using density gradient centrifugation (e.g., Ficoll-Paque or Lymphoprep).
- Wash cells with HBSS or PBS and perform a final resuspension in a serum-free base medium at a high concentration (e.g., 40-100 x 10^6 cells/mL).
Step 2: Cryomedium Preparation
- Use a commercially available, pre-formulated serum-free cryomedium containing 10% DMSO, such as CryoStor CS10 or NutriFreez D10.
- Alternatively, prepare a serum-free formulation like GHRC-CryoMedium I (12.5% BSA Fraction V in RPMI-1640, supplemented with 20% DMSO as a concentrate) [29]. Chill the cryomedium at 4°C before use.
Step 3: Combining Cells and Cryomedium
- Add an equal volume of the chilled cryomedium dropwise to the cell suspension while gently mixing. This achieves a final cell concentration of 20 x 10^6 cells/mL and a final DMSO concentration of 10% (or as per the medium's specification).
- Dispense 1 mL aliquots into pre-cooled cryovials.
Step 4: Controlled-Rate Freezing
- Immediately place cryovials in a programmed freezing chamber or a CoolCell device and transfer to a -80°C freezer. A standard cooling rate is -1°C per minute.
- After 24 hours, transfer the vials to long-term storage in the vapor phase of liquid nitrogen.
Protocol B: Cryopreservation of PBMCs with Reduced DMSO (5%)
This protocol utilizes hydroxyethyl starch (HES) as an extracellular cryoprotectant to enable DMSO reduction, as validated in a 2011 study that remains relevant for its formulation [29].
Step 1: Cell Preparation
- Identical to Protocol A.
Step 2: Cryomedium Preparation
- Prepare a two-part, serum-free cryomedium.
- Part A: 12.5% Bovine Serum Albumin (BSA) Fraction V and 6% Hydroxyethyl Starch (HES) in RPMI-1640.
- Part B: 10% DMSO in RPMI-1640.
- Chill both parts at 4°C.
Step 3: Combining Cells and Cryomedium
- Resuspend the cell pellet in the chilled Part A solution at a concentration of 40 x 10^6 cells/mL.
- Add an equal volume of Part B dropwise while gently mixing. This yields a final concentration of 20 x 10^6 cells/mL, with 5% DMSO, 6.25% BSA, and 3% HES.
- Dispense into cryovials as in Protocol A.
Step 4: Controlled-Rate Freezing
- Identical to Protocol A.
Post-Thaw Processing for Flow Cytometry
A standardized thawing process is crucial for reliable flow cytometry results [28] [29].
- Thawing: Rapidly thaw cryovials in a 37°C water bath until only a small ice crystal remains.
- Dilution & Washing: Gently transfer the cell suspension to a tube containing 10 mL of pre-warmed thawing medium (e.g., IMDM or RPMI-1640 supplemented with 10% FBS and DNase at 10 µg/mL). DNase is critical to prevent cell clumping from released DNA.
- Centrifugation: Centrifuge at 400 x g for 5-10 minutes. Carefully decant the supernatant.
- Resuspension & Rest: Resuspend the cell pellet in an appropriate flow cytometry staining buffer or culture medium. For functional assays, it is recommended to let the cells recover in an incubator (37°C, 5% CO2) for several hours or overnight before proceeding with staining or stimulation.
The Scientist's Toolkit: Essential Reagents for Cryopreservation Research
Table 3: Key Research Reagent Solutions
| Reagent / Product | Function / Description | Example Use Case |
|---|---|---|
| CryoStor CS10 | A commercially available, GMP-manufactured, serum-free freezing medium containing 10% DMSO. | Optimal for long-term biobanking of PBMCs for clinical trials; ensures consistency and avoids FBS-related issues [28]. |
| Dimethyl Sulfoxide (DMSO) | A penetrating cryoprotectant that prevents intracellular ice crystal formation. | The most common cryoprotectant; used at 5-10% final concentration. Its cytotoxicity necessitates careful handling and potential reduction [32] [33]. |
| Hydroxyethyl Starch (HES) | A non-penetrating extracellular cryoprotectant that dehydrates cells and reduces the amount of ice formed. | Used in combination with penetrating agents like DMSO to allow for a reduction in DMSO concentration (e.g., from 10% to 5%) [29]. |
| Bovine Serum Albumin (BSA) | A protein supplement that provides a defined alternative to serum, acting as a buffering agent and providing colloidal protection. | Serves as the core protein component in many custom serum-free cryomedium formulations, replacing FBS [29]. |
| Recombinant Human Albumin | A chemically defined, animal-origin-free version of albumin for high-standard, xeno-free formulations. | Critical for manufacturing clinical-grade cell therapies where animal components must be excluded [34]. |
| DNase I | An enzyme that digests DNA released by dead and dying cells, preventing cell aggregation and clumping during thawing. | Added to the thawing and washing medium to significantly improve cell recovery and single-cell suspension quality for flow cytometry [28]. |
| (R)-Norfluoxetine | (R)-Norfluoxetine | High-Purity SSRI Enantiomer | (R)-Norfluoxetine, the less prevalent norfluoxetine enantiomer. For neuroscience & pharmacology research use only (RUO). Not for human or veterinary use. |
| Ethyl palmitate | Ethyl palmitate, CAS:628-97-7, MF:C18H36O2, MW:284.5 g/mol | Chemical Reagent |
Workflow and Decision Pathway
The following diagram illustrates the experimental workflow for cryopreservation and the key decision points for selecting between the protocols discussed in this note.
The optimal cryoprotectant protocol is determined by the specific requirements of the downstream flow cytometry application. For research demanding the highest consistency and freedom from animal components, particularly in clinical contexts, serum-free media with 10% DMSO (e.g., CryoStor CS10) are robust and well-validated choices. Where the objective is to minimize potential DMSO-related toxicity while maintaining good recovery and function, a serum-free formulation with 5% DMSO supplemented with HES presents a viable alternative. Adherence to the detailed protocols for freezing and, crucially, thawing will ensure the reliable preservation of cell viability and phenotypic integrity, thereby guaranteeing the quality of data derived from flow cytometric analysis.
Peripheral Blood Mononuclear Cells (PBMCs) are critical components of the immune system, comprising lymphocytes (T cells, B cells, and NK cells) and monocytes [35]. These cells are indispensable for immunological research, playing pivotal roles in studying immune function, disease mechanisms, drug efficacy, and vaccine responses [35]. The ability to isolate and cryopreserve PBMCs while maintaining their viability and functionality has revolutionized biomedical research, particularly in immunology, oncology, and cell therapy development [35] [36].
This application note provides a standardized, detailed protocol for isolating PBMCs from whole blood using density gradient centrifugation and subsequently cryopreserving them for long-term storage. The procedures outlined are specifically optimized to maintain cell viability, recovery, and functionality for downstream applications such as flow cytometry, ensuring reliable and reproducible results for researchers and drug development professionals [37].
Principles of PBMC Isolation
Density Gradient Centrifugation
Density gradient centrifugation separates blood components based on their inherent buoyant densities [38]. During centrifugation, gravitational forces separate cells through a density gradient medium, typically with a density of 1.077 g/mL [38] [39]. Heavier components such as granulocytes and erythrocytes sediment through the density gradient medium, while lower density mononuclear cells (lymphocytes and monocytes) remain at the plasma-gradient medium interface [38]. Platelets remain suspended in the plasma layer above the interface [39].
Table 1: Blood Component Distribution After Density Gradient Centrifugation
| Layer Position | Blood Component | Characteristics |
|---|---|---|
| Top Layer | Plasma & Platelets | Contains plasma proteins and suspended platelets |
| Intermediate Layer | PBMCs | Mononuclear cells at the plasma-gradient medium interface |
| Density Gradient Medium | - | Ficoll-Paque or Lymphoprep layer |
| Bottom Layer | Granulocytes & Erythrocytes | Higher density cells forming a pellet |
Research Reagent Solutions
Table 2: Essential Reagents for PBMC Isolation and Cryopreservation
| Reagent | Function | Application Notes |
|---|---|---|
| Density Gradient Medium (e.g., Ficoll-Paque, Lymphoprep) | Creates density barrier for cell separation | Use at density of 1.077 g/mL; pre-warm to 18-20°C [38] [39] |
| Dulbecco's Phosphate Buffered Saline (PBS) | Dilution and washing buffer | May be supplemented with 2% Fetal Bovine Serum (FBS) to protect cells [38] |
| Dimethyl Sulfoxide (DMSO) | Cryoprotectant | Prevents intracellular ice formation; typically used at 10% final concentration [40] |
| Fetal Bovine Serum (FBS) | Nutrient component in freezing media | Provides nutrients and protection during freezing; concern for lot-to-lot variability [40] |
| Serum-Free Cryopreservation Medium (e.g., CryoStor CS10) | Defined alternative to FBS-containing media | cGMP-manufactured, animal component-free formulation [40] |
Materials and Equipment
Required Materials
- Whole blood sample (anticoagulated with heparin, EDTA, or citrate)
- Density gradient medium: Lymphoprep (1.077 g/mL) or Ficoll-Paque [38] [39]
- Dulbecco's Phosphate Buffered Saline (PBS) with 2% Fetal Bovine Serum (PBS + 2% FBS) or appropriate culture medium
- Cryopreservation medium: CryoStor CS10 or 10% DMSO in 90% FBS [40]
- Cryogenic vials
- Centrifuge tubes (sizes based on blood volume)
- Sterile pipettes and tips
Equipment
- Centrifuge with swinging bucket rotor
- Isopropanol freezing container (e.g., Mr. Frosty, Corning CoolCell) or controlled-rate freezer
- Liquid nitrogen storage system
- 37°C water bath
- Laminar flow hood
- Microscope and hemocytometer
Methods
PBMC Isolation by Density Gradient Centrifugation
Blood Preparation and Density Gradient Setup
Temperature Equilibrium: Ensure all reagents and blood samples are at room temperature (18-20°C) before starting. Cold temperatures inhibit red blood cell aggregation, leading to poor separation and potential contamination of the PBMC fraction with red blood cells [39] [41].
Blood Dilution: Dilute the whole blood sample with an equal volume of PBS + 2% FBS or other suitable culture medium. For example, mix 10 mL of blood with 10 mL of dilution medium [38].
Density Medium Preparation: Add the appropriate volume of density gradient medium to a fresh centrifuge tube according to manufacturer's recommendations. Refer to Table 3 for recommended volumes based on blood sample size [38].
Layering Technique: Carefully layer the diluted blood sample over the density gradient medium. Take care not to mix the two layers. Using specialized tubes with inserts (e.g., SepMate) can simplify this step and prevent layer mixing [37].
Table 3: Recommended Volumes for Density Gradient Centrifugation Using Lymphoprep
| Blood Volume (mL) | PBS + 2% FBS (mL) | Lymphoprep (mL) | Tube Size (mL) |
|---|---|---|---|
| 1 | 1 | 1.5 | 5 |
| 2 | 2 | 3 | 14 |
| 3 | 3 | 3 | 14 |
| 4 | 4 | 4 | 14 |
| 5 | 5 | 10 | 50 |
| 10 | 10 | 15 | 50 |
| 15 | 15 | 15 | 50 |
Centrifugation and Cell Harvesting
Centrifugation Parameters: Centrifuge at 400-800 ×g for 20-40 minutes at room temperature with the brake OFF [38] [39]. The specific force and time may vary based on the density medium manufacturer's instructions. Using the brake can disrupt the gradient layers before complete separation.
Post-Centrifugation Layer Identification: After centrifugation, four distinct layers should be visible from top to bottom:
PBMC Harvesting: Carefully insert a pipette through the upper plasma layer directly to the mononuclear cell interface. Harvest the PBMCs by gently aspirating the cloudy layer. Alternatively, first remove the upper plasma layer and then collect the PBMC layer [38].
Cell Washing: Transfer the harvested PBMCs to a fresh tube and add at least 3 times the volume of PBS + 2% FBS or other appropriate buffer. Centrifuge at 300-500 ×g for 10 minutes at room temperature. Carefully remove the supernatant without disturbing the cell pellet. Repeat this washing step once more to remove residual density gradient medium and platelets [38] [39]. For applications requiring minimal platelet contamination, use lower centrifugal forces (60-100 ×g) during washing steps [39].
Cell Assessment: Resuspend the final PBMC pellet in an appropriate buffer for counting and viability assessment using trypan blue exclusion or automated cell counters.
PBMC Cryopreservation
Cryopreservation Protocol
Cell Concentration Adjustment: After isolation and washing, centrifuge PBMCs at 300 ×g for 10 minutes to obtain a cell pellet. Carefully remove the supernatant, leaving a small amount of medium to avoid disturbing the pellet. Resuspend the cell pellet by gently flicking the tube [40].
Cryopreservation Medium Preparation: Two primary options for cryopreservation media are recommended:
Option 1: Serum-Free Cryopreservation Medium
- Use commercial serum-free cryopreservation medium such as CryoStor CS10 (contains 10% DMSO) [40]
- Pre-cool medium to 2-8°C before use
- Add cold cryopreservation medium to achieve final cell concentration of 0.5-10 × 10ⶠcells/mL [40]
Option 2: Laboratory-Prepared Serum-Containing Medium
- Prepare 20% DMSO in FBS (use glass pipette for DMSO, do not place pure DMSO on ice) [40]
- Resuspend PBMC pellet in cold FBS to concentration of 1-20 × 10ⶠcells/mL
- Mix cells gently with equal volume of 20% DMSO in FBS for final concentration of 10% DMSO and 90% FBS, with final cell concentration of 0.5-10 × 10ⶠcells/mL [40]
Aliquoting and Equilibration: Rapidly transfer 1 mL of cell suspension to each cryovial. Incubate cells at 2-8°C for 10 minutes to allow cryoprotectant equilibration [40]. Work efficiently as prolonged DMSO exposure at room temperature can be cytotoxic [41].
Controlled-Rate Freezing: Use a controlled freezing rate of approximately -1°C/minute [35] [40]. This can be achieved using:
- Programmable controlled-rate freezer
- Isopropanol freezing container (e.g., Mr. Frosty, Corning CoolCell) placed in a -80°C freezer overnight [40]
Long-Term Storage: Transfer cryovials to vapor phase liquid nitrogen for long-term storage below -135°C [40]. Storage at -80°C is not recommended for long-term preservation [40]. Minimize exposure to room temperature during transfer by placing vials on dry ice.
Thawing and Post-Thaw Processing
Rapid Thawing: Remove cryovials from liquid nitrogen storage and immediately place in a 37°C water bath. Gently agitate until only a small ice crystal remains (approximately 1-2 minutes) [1]. Avoid complete thawing in the water bath to minimize DMSO toxicity.
Dilution and Washing: Immediately transfer the cell suspension to a 15 mL tube containing 10 mL of pre-warmed complete medium (e.g., RPMI 1640 with 10% FBS). Gently mix by pipetting 2-3 times [1]. Centrifuge at 300-500 ×g for 5-10 minutes at room temperature [1].
Cryoprotectant Removal: Carefully remove supernatant and resuspend cell pellet in fresh warm medium. Repeat washing step if necessary to ensure complete DMSO removal.
Viability Assessment: Assess cell viability using trypan blue exclusion, propidium iodide staining, or flow cytometry with viability dyes [35] [1]. Expected viability should typically exceed 85-90% with optimized protocols.
Critical Factors Affecting PBMC Quality
Pre-Isolation Considerations
- Anticoagulant Selection: Heparin, EDTA, citrate, ACD, and CPD are all acceptable anticoagulants, with citrate-stabilized blood potentially yielding higher quality RNA and DNA [39].
- Blood Storage Time: Process blood samples within 24 hours of collection for optimal results. Extended storage (>24 hours) increases granulocyte contamination and reduces viability [41].
- Temperature Consistency: Maintain consistent temperature (18-20°C) throughout isolation procedure for proper density-based separation [39] [41].
Factors Influencing Cryopreservation Success
Table 4: Key Factors Affecting Cryopreserved PBMC Viability and Recovery
| Factor | Optimal Condition | Impact on PBMC Quality |
|---|---|---|
| Cell Density at Freezing | 1-5 × 10ⶠcells/mL | Higher densities increase clumping; lower densities reduce recovery efficiency [35] |
| Cooling Rate | -1°C/minute | Faster rates cause intracellular ice formation; slower rates increase osmotic stress [35] [40] |
| Cryoprotectant Concentration | 10% DMSO | Lower concentrations provide inadequate protection; higher concentrations increase toxicity [40] |
| Thawing Rate | Rapid in 37°C water bath | Slow thawing promotes ice crystal formation and recrystallization damage [35] |
| Post-Thaw Processing | Immediate dilution and washing | Delayed cryoprotectant removal increases DMSO toxicity [35] [41] |
Quality Assessment and Troubleshooting
Viability and Functionality Assessment
Viability Testing: Use trypan blue exclusion or fluorescent viability dyes (propidium iodide, LIVE/DEAD stains) to determine post-thaw viability [35] [1]. Flow cytometry can provide more detailed analysis of viability across different cell subsets [1].
Functional Assays: Evaluate PBMC functionality through:
- Cytokine release assays (ELISA, intracellular cytokine staining)
- Proliferation assays (CFSE dilution)
- Stimulation with mitogens or antigens [35]
Population Composition: Use flow cytometry with antibody panels against CD3 (T cells), CD19 (B cells), CD56 (NK cells), and CD14 (monocytes) to verify maintenance of normal PBMC subset proportions after cryopreservation [1] [37].
Troubleshooting Common Issues
- Low Viability After Thawing: Ensure rapid thawing and immediate dilution of cryoprotectant. Verify controlled-rate freezing conditions and avoid prolonged storage at -80°C [35] [41].
- Granulocyte Contamination: Process blood samples promptly after collection (<24 hours). Consider using magnetic bead depletion (e.g., CD15 or CD16 MicroBeads) for heavily contaminated samples [41] [37].
- Excessive Platelet Contamination: Include additional low-speed centrifugation steps (60-100 ×g) to remove platelets without pelleting PBMCs [39].
- Poor Cell Recovery After Thawing: Optimize cell density at freezing and avoid excessive centrifugal forces during post-thaw washing [35].
This standardized protocol provides a comprehensive framework for isolating and cryopreserving PBMCs that maintains cell viability, functionality, and representative population distributions. The optimized procedures for density gradient centrifugation, controlled-rate freezing, and proper thawing techniques ensure reliable results for downstream applications including flow cytometry and functional immune assays. Following these detailed methods while adhering to critical timing, temperature, and handling considerations will enable researchers to build reproducible, high-quality PBMC repositories for immunological research and therapeutic development.
In cryopreservation for flow cytometry, maintaining cellular viability, surface marker integrity, and functional properties is paramount for generating reliable data. The freezing phase is particularly critical, where the rate of temperature decline must be carefully controlled to minimize intracellular ice crystal formation, which can compromise cell membranes and organelles. The consistent achievement of a -1°C/minute cooling rate has emerged as a gold standard for preserving a wide array of cell types, including sensitive peripheral blood mononuclear cells (PBMCs) and stem cells. This application note delineates detailed protocols and comparative data for achieving this optimal rate using three common laboratory tools: Mr. Frosty (isopropanol-based) containers, CoolCell (alcohol-free) devices, and programmable freezers. By standardizing this process, researchers in drug development and basic research can ensure high post-thaw viability and functionality of cells destined for flow cytometric analysis.
Principles and Comparative Analysis of Freezing Methods
Controlled-rate freezing operates on the principle of allowing sufficient time for water to migrate out of cells before freezing, thereby reducing lethal intracellular ice crystal formation. The -1°C/minute rate is ideal for many mammalian cells as it balances the risk of ice formation with the damaging effects of prolonged exposure to hypertonic conditions [42] [43]. While programmable freezers offer precise, user-defined control, passive devices like Mr. Frosty and CoolCell leverage the thermal properties of specific materials to approximate this rate in a standard -80°C freezer.
The table below summarizes the key characteristics of the three primary methods for achieving a -1°C/minute cooling rate:
Table 1: Comparative Analysis of Controlled-Rate Freezing Methods
| Feature | Mr. Frosty (Isopropanol-Based) | CoolCell (Alcohol-Free) | Programmable Freezer |
|---|---|---|---|
| Cooling Mechanism | Isopropanol chamber | Thermo-conductive alloy core [44] | Compressed, forced-air nitrogen [42] |
| Cooling Rate | ~-1°C/minute | Consistent -1°C/minute [44] | User-programmable (e.g., -1°C/minute) [42] |
| Cost | Low initial, recurring (isopropanol) | Moderate one-time cost [44] | High capital investment |
| Ease of Use | Simple, requires isopropanol refills | Simple, "set-and-forget" [44] | Complex, requires protocol programming |
| Reproducibility | Moderate (varies with isopropanol age) | High, proven reproducibility [44] | Very High |
| Best For | Labs with intermittent freezing needs | Labs requiring high reproducibility without recurring costs [44] | High-throughput labs, sensitive cell types |
Detailed Experimental Protocols
General Cell Preparation for Cryopreservation
Proper cell preparation is a prerequisite for successful cryopreservation, regardless of the freezing method employed.
- Cell Harvesting: Culture cells to their optimal logarithmic growth phase. For adherent cells, wash with PBS, trypsinize, and neutralize with culture medium. For suspension cells, proceed directly to centrifugation [42].
- Cell Counting and Viability Check: Determine cell concentration and viability using a hemocytometer or automated cell counter. Cell viability should be at least 75-90% prior to cryopreservation [42] [45].
- Centrifugation: Centrifuge the cell suspension at 300 × g for 5 minutes at room temperature. Carefully decant the supernatant [42].
- Resuspension in Freezing Medium: Resuspend the cell pellet in an appropriate, pre-cooled cryoprotectant medium at a typical density of 1 × 10^6 cells/mL [42]. Gently loosen the pellet by pipetting to ensure a single-cell suspension.
- Common Freezing Media Formulations:
- For cells in serum-containing cultures: 90% Fetal Bovine Serum (FBS) + 10% DMSO [42].
- For cells in serum-free cultures: 90% conditioned medium + 10% DMSO [42].
- Commercial serum-free media: Use ready-to-use, serum-free alternatives like CryoStor CS10 to avoid lot-to-lot variation and safety concerns associated with FBS [46].
- Common Freezing Media Formulations:
- Aliquoting: Quickly aliquot 1 mL of the cell suspension into pre-labeled cryogenic vials. Cells should not be kept in DMSO-containing medium at room temperature for more than 10 minutes to minimize cytotoxicity [42].
Protocol A: Controlled Cooling Using a CoolCell Device
The CoolCell utilizes a proprietary alcohol-free design to provide a highly consistent freezing rate [44].
- Equipment Preparation: Ensure the CoolCell is at room temperature prior to use.
- Loading: Place the sealed cryovials into the vial holes of the CoolCell module.
- Freezing: Immediately transfer the entire CoolCell unit to a -80°C freezer. The device's thermo-conductive core and insulated housing will ensure a cooling rate of -1°C/minute [44].
- Storage: After 24 hours, promptly remove the vials from the CoolCell and transfer them to a long-term storage location in liquid nitrogen or a -150°C freezer. Do not store vials at -80°C for extended periods, as viability will decline [42].
Protocol B: Controlled Cooling Using a Mr. Frosty Device
The Mr. Frosty uses isopropanol as a heat sink to moderate the cooling rate.
- Equipment Preparation: Bring the Mr. Frosty container to room temperature. Fill the outer chamber with fresh or freshly recharged isopropanol to the indicated level. Using old isopropanol can compromise the cooling rate.
- Loading: Place the sealed cryovials into the vial holes, ensuring they are surrounded by the isopropanol chamber.
- Freezing: Immediately transfer the entire Mr. Frosty unit to a -80°C freezer. The isopropanol will facilitate an approximate cooling rate of -1°C/minute.
- Storage: After 24 hours, promptly remove the vials and transfer them to long-term liquid nitrogen storage [42].
Protocol C: Controlled Cooling Using a Programmable Freezer
This method offers the highest level of control and is ideal for standardizing protocols across multiple labs or for freezing particularly sensitive cell types.
- Protocol Programming: Input a controlled-rate freezing protocol into the programmable freezer. A standard protocol is:
- Start at 4°C.
- Hold at 4°C for 5-10 minutes.
- Cool from 4°C to -40°C at a rate of -1°C/minute [42].
- Cool from -40°C to -100°C or lower at a faster rate (e.g., -5°C to -10°C/minute).
- Loading: Place the sealed cryovials into the chamber of the programmable freezer and start the program.
- Transfer and Storage: Once the program is complete, quickly transfer the cryovials to long-term liquid nitrogen storage.
The following workflow diagram illustrates the decision-making process for selecting and implementing the appropriate controlled-rate freezing method:
The Scientist's Toolkit: Essential Materials and Reagents
Successful cryopreservation relies on a suite of specialized reagents and tools. The following table catalogs the essential components for a controlled-rate freezing workflow.
Table 2: Key Research Reagent Solutions for Controlled-Rate Freezing
| Item | Function/Description | Example/Catalog |
|---|---|---|
| Cryoprotectant (DMSO) | Penetrating agent; reduces intracellular ice crystal formation [42]. | Dimethyl sulfoxide (DMSO) |
| Cryoprotectant (Glycerol) | Alternative penetrating cryoprotectant for DMSO-sensitive cells [42]. | Glycerol |
| Serum-Free Freezing Medium | Ready-to-use, defined formulation; avoids FBS variability [46]. | CryoStor CS10 [46] |
| Specialized Freezing Media | Cell-type-specific optimized formulations. | STEMdiff, MesenCult [46] |
| Cryogenic Vials | Temperature-resistant polypropylene vials for -196°C [44]. | Corning Bar Coded Vials [44] |
| Controlled-Rate Freezer | Active device for precise, programmable cooling profiles [42]. | Programmable Freezer |
| Passive Freezing Container | Alcohol-free device for consistent -1°C/min in -80°C freezer [44]. | Corning CoolCell [46] [44] |
| Liquid Nitrogen Storage | Long-term preservation of frozen cell stocks at -196°C or below [42]. | Liquid Nitrogen Dewar |
| 2'-O-Methylguanosine | 2'-O-Methylguanosine | RNA Nucleoside | RUO | High-purity 2'-O-Methylguanosine for RNA research. Explore its role in oligonucleotide synthesis & therapeutics. For Research Use Only. |
| 4-Methoxyphenethyl alcohol | 4-Methoxyphenethyl Alcohol | High-Purity Reagent | High-purity 4-Methoxyphenethyl alcohol for research (RUO). A key intermediate for organic synthesis and fragrance development. Not for human or veterinary use. |
Troubleshooting and Optimization for Flow Cytometry
Even with standardized protocols, issues can arise. The table below outlines common problems and their solutions to ensure high-quality cells for flow cytometry.
Table 3: Troubleshooting Guide for Controlled-Rate Freezing
| Problem | Potential Cause | Solution |
|---|---|---|
| Low Post-Thaw Viability | Suboptimal freezing rate; intracellular ice damage [42]. | Verify cooling device function (e.g., CoolCell alloy core, fresh isopropanol for Mr. Frosty) [44]. |
| Low Post-Thaw Viability | Cells were in poor health or low viability pre-freeze [42]. | Freeze cells only at high viability (>75-90%) during log-phase growth [42] [45]. |
| Low Post-Thaw Viability | Excessive exposure to cytotoxic cryoprotectant (e.g., DMSO) [42]. | Limit time in DMSO at room temperature to <10 min; thaw rapidly [42]. |
| High Background in Flow Cytometry | Cell debris from dead/damaged cells. | Optimize freezing protocol to improve viability; use a dead cell exclusion dye during staining. |
| Altered Surface Marker Expression | Cryo-injury or activation (e.g., in platelets) [47]. | Consider alternative cryoprotectants; validate antibody binding after fixation [46] [47]. |
| Poor Recovery/Clumping | High cell concentration during freezing; ice crystal damage. | Freeze at recommended density (~1x10^6 cells/mL); use serum or albumin in medium [42]. |
The rigorous application of controlled-rate freezing protocols is a cornerstone of reproducible research involving cryopreserved cells for flow cytometry. By understanding the principles, meticulously following the detailed protocols for CoolCell, Mr. Frosty, or programmable freezers, and utilizing the appropriate toolkit of reagents, researchers can reliably achieve the critical -1°C/minute cooling rate. This ensures the preservation of high cell viability, antigen integrity, and physiological function, thereby underpinning the reliability and significance of downstream immunophenotyping and functional assays in both basic science and drug development.
Within the context of cryopreservation protocols for flow cytometry research, the post-thaw phase is critically vulnerable. The recovery of viable, functionally intact cells is not a passive outcome but a direct consequence of meticulously controlled thawing and washing procedures. For researchers and drug development professionals, standardizing these techniques is paramount to ensuring that the data generated by flow cytometry accurately reflects the biological reality of the pre-cryopreserved sample, rather than artifacts introduced by suboptimal thawing. The core principle underpinning proper thawing is the rapid transition of the sample from its frozen state to a physiologically compatible liquid state, followed by the careful yet prompt removal of cytotoxic cryoprotectants like Dimethyl Sulfoxide (DMSO) [48]. This application note details the scientific rationale and provides definitive protocols to maximize post-thaw cell recovery for flow cytometry analysis.
The Science of Post-Thaw Cell Recovery
The process of freezing and thawing subjects cells to a series of physical and chemical stresses, including ice crystal formation, osmotic shock, and exposure to cryoprotectants that are toxic at elevated temperatures. The immediate goal of thawing is to minimize the duration of these stresses.
The Imperative of Rapid Thawing
Rapid thawing, typically achieved by immersing the cryovial in a 37°C water bath, is crucial to prevent the growth of small, intracellular ice crystals into larger, damaging crystals—a phenomenon known as recrystallization [48]. A slow thawing process increases the time cells spend in a hypertonic, potentially toxic environment, leading to reduced viability and compromised function.
The Necessity of Post-Thaw Processing
Following thawing, the cryoprotectant must be removed. DMSO, while essential for successful freezing, becomes cytotoxic upon warming and can rapidly induce apoptosis in sensitive cell populations if not promptly diluted and washed away [49]. Furthermore, the presence of DMSO and cell debris from non-viable cells can profoundly impact flow cytometry data by increasing background noise, causing non-specific antibody binding, and altering light scatter properties [48]. Effective post-thaw washing is therefore not merely a matter of cell yield but is fundamental to assay specificity and sensitivity.
Quantitative studies on human bone marrow-derived mesenchymal stem cells (hBM-MSCs) demonstrate that cryopreservation significantly reduces cell viability and metabolic activity immediately after thawing, with some attributes requiring more than 24 hours to recover [49]. This underscores the sensitivity of cellular systems and the importance of optimizing every step to reduce initial damage.
Table 1: Quantitative Impact of Cryopreservation and Thawing on Cell Attributes (Based on hBM-MSC Data [49])
| Cell Attribute | Immediate Post-Thaw (0-4 hours) | 24 Hours Post-Thaw | Long-Term Impact (Beyond 24 hours) |
|---|---|---|---|
| Viability | Reduced | Recovered to near-normal levels | Variable by cell line |
| Apoptosis Level | Increased | Dropped, but may remain elevated | Variable by cell line |
| Metabolic Activity | Impaired | Remained lower than fresh cells | Variable by cell line |
| Adhesion Potential | Impaired | Remained lower than fresh cells | Variable by cell line |
| Proliferation Rate | Not significantly different from fresh cells | Not significantly different from fresh cells | Not significantly different from fresh cells |
| CFU-F Ability | N/A | N/A | Reduced in some cell lines |
Established and Novel Thawing & Washing Methodologies
The following protocols outline both a standard method for general use and a novel, gentler method specifically developed for sensitive cell populations like hematopoietic progenitor cells from apheresis products.
Basic Protocol: Standard Rapid Thaw and Centrifugation Wash
This is a widely used method for robust cell types, emphasizing speed to minimize DMSO exposure [48].
Materials:
- Water bath, calibrated to 37°C
- Pre-warmed complete culture medium
- Centrifuge
- FACS buffer (e.g., PBS with 1% FBS or BSA)
Method:
- Rapid Thaw: Remove the cryovial from liquid nitrogen storage. Immediately and gently agitate it in a 37°C water bath until only a small ice crystal remains (approximately 1-2 minutes). It is critical to submerge only the vial's bottom and cap area to prevent contamination [48].
- Initial Dilution: Wipe the vial with 70% ethanol. Gently transfer the thawed cell suspension to a sterile tube containing a pre-warmed volume of culture medium that is at least 10 times the volume of the cell suspension. This gradual dilution reduces osmotic shock.
- Centrifugation: Centrifuge the cell suspension at 200-400 x g for 5-10 minutes at room temperature to pellet the cells.
- Supernatant Removal: Carefully decant or pipette off the supernatant, which contains the diluted DMSO and dead cells.
- Resuspension and Washing: Gently resuspend the cell pellet in a generous volume of pre-warmed FACS buffer or culture medium. Repeat the centrifugation and supernatant removal steps for a second wash.
- Final Resuspension: Resuspend the final cell pellet in an appropriate volume of FACS buffer or culture medium for counting and subsequent flow cytometry staining.
Advanced Protocol: 3-Step Sequential Dilution Method
Recent research has demonstrated that the mechanical stress of immediate, large-volume dilution and centrifugation can induce iatrogenic (lab-induced) cell death. A novel 3-step method was developed for cryopreserved apheresis products, showing significant improvements in viability measurements for white blood cells, hematopoietic progenitor cells (HPCs), and T cells [50].
Materials:
- Water bath, calibrated to 37°C
- Dilution solution: 1% Human Albumin in Dextran 40 (10% Low Molecular Weight Dextran in 0.9% NaCl)
Method:
- Rapid Thaw: As per the basic protocol, rapidly thaw the cryovial in a 37°C water bath.
- Step-wise Dilution: Instead of a single large-volume dilution, perform three sequential, gentle dilutions.
- First Dilution: Add a volume of the 1% Human Albumin/Dextran solution equal to one-third of the thawed sample volume.
- Incubation: Wait for 5 minutes at room temperature.
- Second Dilution: Add another volume of dilution solution equal to one-third of the original sample volume.
- Incubation: Wait for another 5 minutes.
- Third Dilution: Add a final volume of dilution solution equal to one-third of the original sample volume.
- Incubation: Wait for a final 5 minutes.
- Final Preparation for Flow Cytometry: Perform an additional 1:10 dilution with FACS buffer to achieve the desired cell concentration for flow cytometry analysis. This results in a total cumulative dilution of approximately 1:20, effectively removing DMSO while minimizing osmotic shock [50].
Table 2: Comparison of Post-Thaw Washing Methods
| Parameter | Standard Centrifugation Wash | 3-Step Sequential Dilution [50] |
|---|---|---|
| Core Principle | Rapid, physical removal of DMSO via centrifugation | Slow, osmotic equilibration to minimize shock |
| Key Reagent | Culture Medium / FACS Buffer | 1% Human Albumin in Dextran 40 |
| Typical Process Time | ~30 minutes | ~15-20 minutes (plus 15 min incubation) |
| Reported Impact on Viability | Can be lower due to mechanical stress | Significant increase in WBC, HPC, and T cell viability |
| Reported Data Precision | Higher variability (standard deviation) | More precise viability measurements (reduced SD) |
| Best Suited For | Robust, adherent cell lines (e.g., many cultured cell lines) | Sensitive, primary, non-adherent cells (e.g., HPCs, PBMCs, apheresis products) |
Integrated Workflow for Flow Cytometry
The diagram below illustrates the complete decision-making workflow for thawing and preparing cells for flow cytometry, integrating both standard and advanced protocols.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for Post-Thaw Processing
| Reagent / Material | Function / Purpose | Key Considerations |
|---|---|---|
| Dimethyl Sulfoxide (DMSO) | Penetrating cryoprotectant that reduces intracellular ice crystal formation. | Cytotoxic upon warming; must be promptly and thoroughly removed post-thaw [49] [48]. |
| Polyampholyte-based Solutions | Emerging cryopreservative that enables rapid washout (<30 min) for "blood-on-demand" applications [51]. | May offer a faster, less damaging alternative to glycerol for RBCs and other sensitive cells. |
| 1% Human Albumin in Dextran 40 | Isotonic dilution solution that provides colloidal support, reducing osmotic shock during DMSO removal [50]. | Critical component of the high-viability 3-step dilution method for apheresis products and HPCs. |
| FACS Buffer (PBS + 1% FBS/BSA) | Standard buffer for washing and resuspending cells for flow cytometry. | Low protein content minimizes background autofluorescence. Contains sodium azide for inhibition of internalization. |
| Viability Dyes (e.g., PI, 7-AAD, DAPI) | Fluorescent dyes that are excluded by live cells with intact membranes; used to gate out dead cells during analysis. | Essential for accurate flow cytometry, as dead cells bind antibodies non-specifically [48]. |
| Fc Receptor Blocking Reagent (e.g., normal serum) | Blocks non-specific antibody binding to Fc receptors on immune cells, improving signal-to-noise ratio [27]. | Use serum from the same species as the staining antibodies (e.g., rat serum for mouse samples). |
| Brilliant Stain Buffer | Contains compounds that prevent fluorescence resonance energy transfer (FRET) between certain tandem dyes (e.g., Brilliant Violet dyes). | Mandatory for panels containing polymer dyes to prevent spurious signal and data artifacts [27]. |
| Tandem Stabilizer | A commercial additive that helps prevent the degradation of tandem fluorophores (e.g., PE-Cy7, APC-Cy7). | Degradation can cause false-positive signals in the detector for the constituent fluorophore [27]. |
| Casopitant Mesylate | Casopitant Mesylate | NK1 Receptor Antagonist | RUO | Casopitant mesylate is a potent, selective NK1 receptor antagonist for neuroscience research. For Research Use Only. Not for human or veterinary use. |
| Pentyl 4-hydroxybenzoate | Pentyl 4-hydroxybenzoate | High-Purity Grade | Pentyl 4-hydroxybenzoate for antimicrobial & preservative research. High-purity, For Research Use Only. Not for human consumption. |
Within the broader thesis of cryopreservation protocol research for flow cytometry, a one-size-fits-all approach is a critical pitfall. Specialized cell samples—spleen cells, Hematopoietic Stem Cells (HSCs), and Leukapheresis products—each possess unique biological and physical characteristics that demand tailored cryopreservation and processing strategies. Spleen cells, as a model for solid lymphoid tissue, require effective mechanical dissociation and often red blood cell lysis [52] [53]. HSCs, typically collected via apheresis, are defined by their CD34+ phenotype and have strict clinical dose and viability thresholds for transplantation, necessitating highly controlled freezing rates and defined cryoprotectant compositions [54] [55]. Leukapheresis products, serving as the starting material for advanced therapies like CAR-T, present the challenge of bulk cryopreservation with minimal loss of T-cell fitness and function [23]. This Application Note details sample-specific protocols and quantitative benchmarks to guide researchers and drug development professionals in optimizing the quality and analytical fidelity of these distinct sample types for flow cytometric analysis.
Sample-Specific Cryopreservation Protocols
Spleen Cell Isolation and Cryopreservation
The isolation of murine splenocytes is a foundational technique for immunology research. The following protocol ensures a high yield of viable cells suitable for subsequent cryopreservation and flow cytometric analysis [52] [53].
Isolation Methodology:
- Mechanical Disaggregation: Place the harvested spleen in a petri dish containing 5 mL of cold RPMI 1640 medium or Hank's Balanced Salt Solution (HBSS). Using the flat end of a sterile syringe plunger, gently grind the spleen against a 70 µm cell strainer to release the cells [52].
- Washing and Clarification: Rinse the strainer with additional medium, then transfer the cell suspension to a 15 mL conical tube. Allow large tissue clumps to sediment for about a minute or use a Pasteur pipette to remove aggregates [52].
- Red Blood Cell (RBC) Lysis: Centrifuge the cell suspension and discard the supernatant. Resuspend the pellet in 2-5 mL of cold 1x RBC lysis buffer and incubate on ice for 5 minutes. Stop the reaction by adding a large volume of cold PBS or medium and centrifuging [53].
- Cell Counting: Resuspend the final pellet in a known volume of medium and perform a cell count and viability analysis using trypan blue exclusion or an automated cell counter.
Cryopreservation Protocol:
- Freezing Medium: Resuspend the final cell pellet in freezing medium, such as RPMI 1640 supplemented with 20% Fetal Calf Serum (FCS) and 10% DMSO [52]. For serum-free conditions, adaptations using 7% DMSO can be used [52].
- Cell Concentration: Adjust the cell concentration to between 5 and 25 million cells per milliliter [52].
- Freezing: Aliquot 1 mL of cell suspension into cryovials. Use a controlled-rate freezing container (e.g., "Mr. Frosty") and place it immediately in a -80°C freezer for a minimum of 4 hours [52].
- Long-term Storage: For long-term storage, transfer cryovials to a -150°C freezer or liquid nitrogen vapor phase after the initial freezing [52].
Hematopoietic Stem Cell (HSC) Processing and Cryopreservation
HSC grafts for transplantation require rigorous, standardized protocols to ensure engraftment potency. The following guidelines are based on clinical standards from the EBMT handbook [54].
Pre-freezing Handling:
- Time to Preservation: Cryopreservation should be performed within 48 hours of collection, and must not exceed 72 hours. For storage over 24 hours prior to freezing, the nucleated cell (NC) concentration should not exceed 2 × 10^8/mL [54].
- Quality Assessment: Before freezing, the product's volume, nucleated cell count, and CD34+ cell count must be enumerated, typically following ISHAGE guidelines [54] [55].
Cryopreservation Protocol:
- Final Formulation: The maximum NC concentration in the final product should be ≤4 × 10^8/mL. The product is diluted with a cryoprotectant solution containing 5–10% DMSO and 0.05–0.25 mL of ACD-A stabilizer solution per mL of transplant [54].
- Controlled-Rate Freezing: Freezing must be performed at a controlled rate of 1–2 °C per minute [54].
- Storage: Cryopreserved bags must be stored in the vapour phase of liquid nitrogen at ≤ -140 °C to ensure long-term viability [54].
Thawing and Infusion:
- At the time of transplantation, cryopreserved bags are thawed at the patient's bedside. The product should be reinfused within a maximum of 20 minutes after thawing using a standard transfusion filter. Washing to remove DMSO is not routinely recommended due to the risk of HSC loss [54].
Leukapheresis Product Cryopreservation for Advanced Therapies
Cryopreserved leukapheresis is emerging as a critical raw material for decentralized CAR-T manufacturing. The protocol below is optimized for maintaining T-cell quality and function [23].
Pre-processing and Formulation:
- Impurity Reduction: Implement a centrifugation step to reduce non-cellular impurities like red blood cells and platelets, which can impact post-thaw T-cell viability [23].
- Cryoprotectant: Use clinical-grade cryoprotectant CS10 (10% DMSO). The formulation must account for the high cell density and ensure a final DMSO concentration of ≥7.5% in the cryomedium [23].
- Cell Concentration and Volume: Target a cell concentration of ~5 × 10^7 cells/mL, with a formulation volume of 20 mL per bag, aiming for ≥1 × 10^9 cells per bag as a Critical Quality Attribute (CQA) [23].
Freezing and Thawing:
- Time-Sensitive Freezing: The interval from cryoprotectant addition to the initiation of controlled-rate freezing should be strictly limited to ≤120 minutes [23].
- Thawing and Washing: Thaw cells rapidly in a 37°C water bath. For post-thaw analysis or processing, a gentle, step-wise dilution method is superior to quick washing. A novel 3-step method involves slowly diluting the thawed sample to 1:2 by three separate additions of 1/3 sample volume of 1% Human Albumin in Dextran 40, with 5-minute intervals between additions, followed by a final 1:10 dilution for analysis. This method significantly improves viability measurements for white blood cells, HPCs, and T-cells compared to standard washing [50].
Comparative Analysis and Data Presentation
The success of adapted protocols is quantified through key metrics like viability, recovery, and phenotypic composition. The tables below summarize expected outcomes for each sample type.
Table 1: Key Cryopreservation Parameters and Benchmarks for Specialized Samples
| Parameter | Spleen Cells | HSCs (Clinical Graft) | Leukapheresis (for CAR-T) |
|---|---|---|---|
| Target Cell Concentration | 5-25 x 10^6 cells/mL [52] | ≤4 x 10^8 NC/mL [54] | ~5 x 10^7 cells/mL [23] |
| Key Cryoprotectant | 10% DMSO in RPMI+20% FCS [52] | 5-10% DMSO + ACD-A [54] | 10% DMSO (CS10) [23] |
| Freezing Rate | In insulated container at -80°C [52] | Controlled-rate, 1-2 °C/min [54] | Controlled-rate, initiated ≤120 min from CPA addition [23] |
| Post-Thaw Viability Benchmark | Not explicitly stated | >70% NC viability (clinical release) [54] | ≥90% [23] |
| Post-Thaw Recovery/Cell Dose | Not explicitly stated | ≥2.0 x 10^6 CD34+/kg bw (Auto-HCT) [54] | High recovery, phenotype comparable to fresh [23] |
Table 2: Post-Thaw Phenotypic and Functional Outcomes from Recent Studies
| Sample Type | Study Findings | Reference |
|---|---|---|
| Leukapheresis | Post-thaw viability 90.9-97.0%; lymphocyte proportion (66.59%) higher than in cryopreserved PBMCs (52.20%); compatible with multiple CAR-T platforms (non-viral, lentiviral). | [23] |
| HSCs (Autologous) | Flow cytometry of CD34+ subpopulations feasible after 4-15 years of cryostorage. A high ratio of primitive Lympho-Myeloid Primitive Progenitors (LMPPs) correlated with faster neutrophilic granulocyte and leukocyte engraftment. | [55] |
| PBMCs (Research) | Optimized cryopreservation showed minimal effects on PBMC viability, population composition, and transcriptomic profiles after 6 or 12 months of storage, despite a reduction in scRNA-seq cell capture efficiency at 12 months. | [1] |
The following workflow diagram synthesizes the critical procedural steps and decision points for processing these specialized samples.
The Scientist's Toolkit: Essential Reagents and Materials
Successful protocol adaptation relies on the use of specific, high-quality reagents. The following table lists essential items for working with these specialized samples.
Table 3: Essential Research Reagent Solutions for Specialized Sample Cryopreservation
| Reagent/Material | Function/Application | Sample Type |
|---|---|---|
| 70 µm Cell Strainer | Mechanical disaggregation of solid tissue to create a single-cell suspension. | Spleen Cells [52] [53] |
| RBC Lysis Buffer | Lyses contaminating red blood cells post-isolation to purify leukocytes. | Spleen Cells [53] |
| CD34 Enumeration Kit (ISHAGE) | Standardized quantification of viable CD34+ HSCs by flow cytometry for dose calculation. | HSCs [54] [55] |
| Controlled-Rate Freezer | Ensures reproducible and optimal cooling rate (1-2°C/min) for high-value clinical samples. | HSCs, Leukapheresis [54] [23] |
| CS10 Cryoprotectant | Clinical-grade, serum-free freezing medium containing 10% DMSO, optimized for leukocytes. | Leukapheresis [23] |
| 1% Human Albumin in Dextran 40 | Wash medium for gentle, step-wise dilution of thawed samples, improving viability assessment. | Leukapheresis, HSCs [50] |
| Viability Stain (7-AAD/Propidium Iodide) | Flow cytometric exclusion of dead cells during analysis or quality control. | All [54] [55] [1] |
| Benzothiazole-d4 | Benzothiazole-d4 | Deuterated Reagent | Supplier | High-purity Benzothiazole-d4 internal standard for LC-MS/MS. For Research Use Only (RUO). Not for human or veterinary diagnostics or therapeutics. |
| Phellamurin | Phellamurin | High-Purity Reference Standard | Phellamurin, a natural dihydroflavonol. Explore its research applications in cytoprotection and senescence. For Research Use Only. Not for human or veterinary use. |
The adaptation of cryopreservation protocols for spleen cells, HSCs, and leukapheresis products is not merely a technical detail but a fundamental determinant of experimental and clinical success. As demonstrated, spleen cells require robust isolation and standard cryopreservation, HSCs demand rigorous, clinically validated processes with controlled freezing, and leukapheresis products benefit from advanced formulations and gentle post-thaw handling to preserve their therapeutic potential. Adhering to these sample-specific principles ensures that cellular integrity and function are maintained, thereby guaranteeing the reliability of subsequent flow cytometric analysis and the efficacy of resulting cell-based therapies. The standardized protocols and quantitative benchmarks provided here offer a framework for researchers and drug development professionals to achieve consistent and high-quality results in their cryopreservation workflows.
Troubleshooting Common Pitfalls and Optimizing Post-Thaw Viability for Flow Cytometry
The success of scientific research and clinical applications in immunology and cell therapy fundamentally depends on the integrity of cryopreserved cellular samples. For flow cytometry studies, which provide multiparametric identification and quantification of single cells, low post-thaw viability poses a significant barrier to obtaining reliable, reproducible data [6]. This application note examines the primary technical factors governing cell viability after cryopreservation and thawing: freezing rate, cell concentration, and dimethyl sulfoxide (DMSO) toxicity. These factors profoundly influence the quantitative and phenotypic characteristics of immune cells, particularly T-cell subsets, which are critical for reflecting differences between healthy individuals and patients with immune diseases [6]. We provide a detailed, evidence-based analysis to guide researchers and drug development professionals in diagnosing and solving the most common challenges in cryopreservation protocols for flow cytometry samples.
The Multifactorial Nature of Post-Thaw Viability
The viability of cells after thawing is not determined by a single factor but by a complex interplay of physical and chemical stresses imposed during the cryopreservation workflow. The diagram below illustrates the core relationships between the key factors and their collective impact on cell viability.
Figure 1: Logical relationship between key stressors and the ultimate outcome of low post-thaw viability. Inappropriate freezing rates, toxic effects of Cryoprotective Agents (CPAs) like DMSO, and high cell concentration act in concert to induce distinct cellular injuries that collectively diminish viability.
Quantitative Analysis of Key Factors
The Dual Role of DMSO: Cryoprotection and Toxicity
Dimethyl sulfoxide is the most common permeating cryoprotective agent. Its efficacy and toxicity are concentration-dependent. It protects cells by depressing the freezing point of water, increasing membrane permeability, and facilitating vitrification—the formation of a glassy, non-crystalline state that prevents lethal ice crystal formation [13]. However, DMSO is inherently toxic to cells, and this toxicity is a major contributor to low post-thaw viability and adverse effects in patients receiving cellular therapies [30].
Table 1: Impact of DMSO Concentration on Cell Viability and Function
| DMSO Concentration | Cell Viability & Recovery | Functional Impacts & Clinical Outcomes |
|---|---|---|
| 10% (Standard) | Lower lymphocyte and neutrophil viability compared to 4-5% [56]. | Higher frequency of infusion-related adverse effects (nausea, vomiting, cardiovascular events) [30]. |
| 5% - 7.5% | Highest viability of neutrophils and lymphocytes [56]. Optimal CD34+ cell viability in autologous HSC grafts [30]. | Faster hematopoiesis reconstitution; no significant difference in platelet/neutrophil engraftment vs. 10% [30]. |
| 2% - 4% | Decreased viability of neutrophils and lymphocytes [56]. | Slightly increased CXCL8 and decreased CXCL4 levels; minor effects on other soluble mediators [56]. |
The evidence suggests that reducing DMSO concentration from 10% to 5% can enhance cell viability without compromising engraftment potential, while simultaneously reducing the risk of adverse clinical effects [30]. The mechanism of DMSO toxicity involves pore formation in biological membranes at around 10% concentration, which, while advantageous for water exchange, can lead to membrane disintegration at higher, toxic levels [13].
Optimizing the Freezing Rate: Slow vs. Rapid Cooling
The cooling rate is a critical parameter that determines whether water inside the cell forms damaging ice crystals or undergoes protective vitrification. Two primary methods are employed: slow-cooling and rapid-cooling (vitrification).
Table 2: Comparison of Slow-Cooling and Rapid-Cooling (Vitrification) Methods
| Parameter | Slow-Cooling | Rapid-Cooling (Vitrification) |
|---|---|---|
| Mechanism | Gradual dehydration of cells; minimizes intracellular ice by allowing water to exit [57]. | Ultra-fast cooling solidifies solution into a glassy state without ice crystal formation [58]. |
| Cooling Rate | Approximately 1-2°C/min [13] [58]. | Exceedingly high (>100°C/min), often by direct contact with liquid nitrogen [58]. |
| CPA Concentration | Lower (e.g., 10% DMSO) [13]. | Very high, requiring CPA mixtures to avoid toxicity [58] [57]. |
| Reported Outcomes | - 75.5% UCB-MNC viability [58].- Routine method for HSCs, MSCs [13] [57]. | - 91.9% UCB-MNC viability [58].- Superior for oocytes, embryonic stem cells [58]. |
| Key Challenges | Cell death from osmotic stress and "solution effects" in critical temperature zone (-15°C to -60°C) [58]. | High CPA toxicity risk; requires precise optimization of CPA cocktail and exposure time [58] [57]. |
A study on umbilical cord blood mononucleated cells (UCB-MNCs) found that rapid-cooling yielded significantly higher post-thaw viability (91.9%) than slow-cooling (75.5%) [58]. However, this came with a significant trade-off: the enumeration of CD34+ hematopoietic stem cells was much higher in the slow-cooled population, and the rapid-cooled cells showed a significantly higher level of oxidative stress (malondialdehyde) [58]. This highlights that the "optimal" method is cell-type specific.
The Overlooked Factor: Cell Concentration
The concentration of cells during cryopreservation is a frequently overlooked variable that significantly impacts quality. Research on peripheral blood stem cells (PBSCs) has demonstrated that storage time and high cell concentration act synergistically to reduce graft quality [59].
Key Findings:
- Viable CD34+ Cells & Colony-Forming Units (CFU): No significant losses were observed in the first 24 hours of storage at both low and high total nucleated cell (TNC) concentrations. However, after 48 hours, these variables decreased significantly at high TNC concentrations [59].
- Synergistic Detriment: The negative effect of storage time is markedly amplified by high cell concentration. This is likely due to increased metabolic waste, signaling crosstalk, and cumulative stress responses in densely packed samples [59].
Therefore, for both short-term fresh storage and long-term cryopreservation, using lower cell concentrations is recommended to maintain the viability and functional capacity of the cellular product.
Detailed Experimental Protocols for Optimization
Protocol: Evaluating DMSO Toxicity in PBSC Grafts
This protocol is adapted from a clinical study that investigated the effect of DMSO concentration on leukocyte viability and soluble mediators [56].
Objective: To determine the optimal DMSO concentration for cryopreserving autologous peripheral blood stem cell grafts that maximizes CD34+ cell and leukocyte viability while minimizing the release of inflammatory mediators.
Materials:
- Research Reagent Solutions:
- DMSO: Cryoprotective agent.
- Plasma-Lyte A or similar isotonic solution: Base for cryomedium.
- Flow Cytometry Reagents: Antibodies for CD34, CD45, and a viability dye (e.g., 7-AAD).
- ELISA Kits: For quantifying soluble mediators (e.g., IL-6, TNF-α, CXCL8, CCL5).
Methodology:
- Sample Preparation: Collect peripheral blood autografts via apheresis and divide them into aliquots.
- Cryomedium Preparation: Prepare separate cryopreservation media with final DMSO concentrations of 2%, 4%, 5%, and 10% in Plasma-Lyte A.
- Cryopreservation: Mix the cell products with the respective cryomedium. Use a controlled-rate freezer, cooling at approximately 1-2°C/min, and store the samples in liquid nitrogen vapor phase for a defined period (e.g., 5-6 years).
- Post-Thaw Analysis:
- Thawing: Rapidly thaw samples in a 37°C water bath.
- Viability Assay: Assess the viability of neutrophils, lymphocytes, and CD34+ cells using flow cytometry with a viability dye.
- Soluble Mediator Analysis: Centrifuge the thawed samples and use ELISA to measure the concentration of leukocyte- and platelet-derived soluble mediators in the supernatant.
Expected Outcomes: The highest viability for both neutrophils and lymphocytes is typically observed with 4% and 5% DMSO, while 2% and 10% show decreased viability. Most soluble mediator levels remain stable across concentrations, except for slightly increased CXCL8 and decreased CXCL4 with 2% DMSO [56].
Protocol: Comparing Slow-Cooling vs. Rapid-Cooling for UCB-HSCs
This protocol is based on a study that directly compared the two freezing methods for umbilical cord blood hematopoietic stem cells [58].
Objective: To scientifically compare the effectiveness of slow-cooling and rapid-cooling in preserving the life and function of hematopoietic stem cells contained in umbilical cord blood mononucleated cells.
Materials:
- Research Reagent Solutions:
- Ficoll-Hypaque: For density-gradient isolation of mononucleated cells (MNCs).
- Phosphate Buffer Saline human Albumin (PBShA): For cell washing and suspension.
- Cryoprotectant Cocktail: Typically 10% DMSO for slow-cooling; a higher concentration mixture (e.g., multi-molar DMSO and ethylene glycol) for rapid-cooling.
Methodology:
- Sample Collection & Isolation: Collect umbilical cord blood and isolate MNCs using Ficoll-Hypaque density-gradient centrifugation.
- Cryopreservation Groups:
- Slow-Cooling Group: Mix the MNC suspension with freezing solution (e.g., 10% DMSO). Place cryovials in a controlled-rate freezer programmed to cool at -2°C/min to -70°C before transfer to liquid nitrogen.
- Rapid-Cooling Group: Mix the MNC suspension with a vitrification solution containing high concentrations of cryoprotectants. Enclose the sample in a suitable device (e.g., straws) and plunge directly into liquid nitrogen.
- Thawing: Rapidly thaw all samples in a 37°C water bath. Dilute the thawed product gradually with a buffered solution containing protein (e.g., albumin) to reduce osmotic shock.
- Post-Thaw Assessment:
- Cell Viability: Determine using Trypan Blue exclusion or an automated cell counter.
- Oxidative Stress: Quantify malondialdehyde (MDA) content as a marker of lipid peroxidation.
- Apoptosis Level: Assess via a DNA fragmentation assay (e.g., TUNEL).
- HSC Potency: Enumerate CD34+ cells by flow cytometry and perform a colony-forming unit (CFU) assay.
Expected Outcomes: The rapid-cooling method is expected to yield significantly higher MNC viability but also a higher level of oxidative stress and a potentially lower recovery of functional CD34+ cells compared to the slow-cooling method [58].
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Cryopreservation Studies
| Reagent/Material | Function & Application | Specific Examples & Notes |
|---|---|---|
| Permeating CPAs | Small molecules that enter cells, depress freezing point, and promote vitrification [13]. | DMSO, Glycerol (GLY), Ethylene Glycol (EG), Propylene Glycol (PG). DMSO is most common but has toxicity concerns [13]. |
| Non-Permeating CPAs | Large molecules that act extracellularly, increasing solution viscosity and mitigating osmotic shock [13]. | Hydroxyethyl Starch, Sucrose, Trehalose, Raffinose. Often used in combination with permeating CPAs to allow lower, less toxic concentrations [13] [30]. |
| Cryopreservation Media | The solution containing CPAs and nutrients for freezing. | Often includes a base solution (e.g., Plasma-Lyte A, culture media like DMEM), 5-10% DMSO, and a source of protein (e.g., 40% FBS) [6] [60]. |
| Viability Stains | To distinguish live from dead cells in post-thaw analysis. | Trypan Blue (hemocytometer), DAPI, 7-AAD (flow cytometry). Critical for assessing protocol success [6] [58]. |
| Flow Cytometry Antibodies | For immunophenotyping and quantifying specific cell populations post-thaw. | Antibodies against CD3, CD4, CD8 (T-cells), CD34 (HSCs), CD45 (pan-leukocyte). Essential for tracking recovery of target cells [6] [60]. |
Integrated Workflow for High Post-Thaw Viability
The following workflow synthesizes the critical steps and decision points from sample preparation to post-thaw analysis, integrating the optimal practices for each key factor discussed.
Figure 2: An optimized end-to-end workflow for cryopreservation, integrating best practices for cell concentration, DMSO usage, freezing rate, and post-thaw handling to maximize cell viability and functionality.
Achieving consistently high post-thaw viability for flow cytometry samples requires a meticulous, evidence-based approach that simultaneously addresses freezing rate, cell concentration, and DMSO toxicity. No single universal protocol exists; optimization is cell-type specific. However, the collective evidence strongly supports a shift towards lower DMSO concentrations (e.g., 5%), careful consideration of cooling rates with a preference for controlled slow-freezing for many primary cells, and the use of lower cell concentrations during freezing. Furthermore, post-thaw processing, including gradual dilution and immediate analysis, is critical for an accurate assessment of cell quality. By systematically diagnosing and troubleshooting these key factors as outlined in this application note, researchers and clinicians can significantly enhance the reliability of their cryopreserved samples, thereby ensuring the integrity of downstream flow cytometry data and the success of clinical cell therapies.
Cryopreservation of peripheral blood mononuclear cells (PBMCs) and other cell types is a fundamental procedure in immunology and cell therapy research, enabling the standardization of experiments and the creation of biobanks for clinical trials [61] [25]. However, the freezing and thawing processes can introduce significant phenotypic inconsistencies that compromise data integrity. These artifacts, primarily marker down-regulation and non-specific staining, pose substantial challenges for accurate flow cytometry analysis and can lead to erroneous biological interpretations [61] [25]. This Application Note details evidence-based strategies to mitigate these effects, providing researchers with standardized protocols to preserve cellular integrity and antigen expression post-cryopreservation. The guidance is framed within a broader thesis on optimizing cryopreservation protocols to enhance reproducibility in flow cytometry-based research and drug development.
Quantitative Impact of Cryopreservation on Cellular Phenotype
Understanding the specific quantitative changes induced by cryopreservation is crucial for developing effective mitigation strategies. The following table summarizes key phenotypic alterations observed in cryopreserved PBMCs as reported in recent studies.
Table 1: Documented Effects of Cryopreservation on PBMC Phenotype and Function
| Parameter Assessed | Reported Change | Experimental Context | Citation |
|---|---|---|---|
| Cell Viability | Decreased viability post-thaw | PBMCs cryopreserved with 10% DMSO; assessed with Solution 13/acridine orange staining | [61] |
| CD4+ T-cell Population | Significant decrease (p=0.0078) | Flow cytometry analysis of PBMCs after cryopreservation | [61] |
| FoxP3 Expression | Significant decrease (p=0.0312) | Gene expression analysis in PBMCs; Treg population count remained unchanged | [61] |
| IL-1β Expression | Increased expression | Gene expression analysis post-cryopreservation | [61] |
| Treg Suppressive Function | Unchanged | Suppression of anti-CD3/CD28-antibody-stimulated PBMC proliferation was equivalent between fresh and frozen Tregs | [61] |
| scRNA-seq Cell Capture | ~32% reduction after 12 months | Reduced capture efficiency despite stable transcriptome profiles and cell viability | [25] |
| Major Immune Cell Populations | Minimal change in composition | Six major types (monocytes, DCs, NK, CD4+ T, CD8+ T, B cells) identified in both fresh and cryopreserved samples | [25] |
| Transcriptome Profiles | Minimal perturbation | AP-1 complex, stress response, and calcium ion response genes showed small-scale changes (<2 folds) | [25] |
Strategic Framework for Mitigation
The following workflow outlines a comprehensive strategy for preventing phenotypic inconsistencies, from sample preparation to data acquisition.
Detailed Experimental Protocols
Optimized PBMC Cryopreservation Protocol
Principle: Maintain cell viability and antigen integrity through controlled-rate freezing and appropriate cryoprotectants [61] [25].
Materials:
- Cryoprotectant: CryoStor CS10 or equivalent GMP-grade freezing medium [62]
- Alternative: Culture medium (e.g., RPMI-1640) supplemented with 10% DMSO and 10-20% FBS [61] [63]
- Controlled-rate freezing device: CryoMed Freezer or Mr. Frosty freezing container
- Cryogenic vials
Procedure:
- Cell Preparation: Start with high-viability PBMCs (>90%) isolated via density gradient centrifugation (Ficoll-Paque Plus or Lymphoprep) [63] [25].
- RBC Removal: Treat cell pellets with ACK lysing buffer for 10 minutes at room temperature to remove contaminating red blood cells that can affect cell counting and assay performance [61]. Wash twice with PBS.
- Cryoprotectant Resuspension: Resuspend cell pellet in pre-chilled cryopreservation medium at a concentration of 5-10 × 10^6 cells/mL [61] [63]. Gently mix to ensure homogeneous cell distribution.
- Aliquoting: Dispense 1 mL of cell suspension into each cryogenic vial.
- Controlled-Rate Freezing:
- Using programmable freezer: Employ a optimized freezing rate (e.g., 1.0°C/min to -4°C, then 25.0°C/min to -40°C, 10.0°C/min to -12°C, 1.0°C/min to -40°C, and 10.0°C/min to -90°C) [25].
- Using passive freezing device: Place vials in a Mr. Frosty container and store at -80°C for 24 hours.
- Long-Term Storage: Transfer vials to liquid nitrogen vapor phase (-161°C to -196°C) for long-term storage [25].
Thawing and Recovery Protocol for Optimal Anticity Preservation
Principle: Minimize osmotic stress and allow cellular recovery to restore membrane integrity and antigen expression [25].
Materials:
- Water bath (37°C)
- Pre-warmed recovery medium: RPMI-1640 supplemented with 10% FBS, 10 mM HEPES, and gentamycin [25]
- Benchtop centrifuge
Procedure:
- Rapid Thaw: Retrieve vial from liquid nitrogen and immediately place in a 37°C water bath with gentle agitation until only a small ice crystal remains (approximately 1-2 minutes) [25].
- Gentantle Transfer: Transfer the cell suspension to a 15 mL tube containing 10 mL of pre-warmed recovery medium. This gradual dilution reduces osmotic shock.
- Centrifugation: Centrifuge at 500 × g for 5 minutes at room temperature [25].
- Resuspension and Resting: Gently resuspend the cell pellet in fresh pre-warmed recovery medium. A critical step is to allow cells to rest in culture medium for at least 4 hours at 37°C, 5% CO2 before staining. This recovery period allows for the re-internalization of surface antigens that may have been internalized during the freezing process [25].
Staining Protocol to Minimize Non-Specific Staining
Principle: Block Fc receptors and use viability dyes to eliminate false-positive signals from dead cells [64] [65].
Materials:
- Viability dye: Live/Dead Fixable Violet Dead Cell Stain Kit or equivalent [25]
- Fc receptor blocking solution: Human Fc Block or purified anti-CD16/32 [66]
- Staining buffer: PBS with 2% BSA or FBS
- Antibody panels
Procedure:
- Viability Staining: Resuspend cell pellet in PBS containing a viability dye (e.g., 1 μL dye per 1 × 10^6 cells). Incubate for 30 minutes on ice, protected from light [25].
- Wash: Add 2 mL staining buffer and centrifuge at 500 × g for 5 minutes. Discard supernatant.
- Fc Receptor Blocking: Resuspend cell pellet in 100 μL staining buffer containing Fc block (10 μL per 1 × 10^6 cells). Incubate for 10 minutes at room temperature [66] [25].
- Surface Antigen Staining: Add pre-titrated antibody cocktails directly to the cell suspension without washing. Incubate for 20 minutes at 4°C, protected from light.
- Wash and Fix: Wash cells twice with staining buffer, then resuspend in fixation buffer if required.
- Intracellular Staining (if needed): For transcription factors like FoxP3, use the eBioscience FoxP3 Fix/Perm buffer set according to manufacturer's instructions with a 2-hour staining at 4°C [66].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for Mitigating Cryopreservation Artifacts
| Reagent / Solution | Function & Rationale | Example Products |
|---|---|---|
| Cryopreservation Media | GMP-grade solutions like CryoStor CS10 provide optimized composition to minimize freezing-induced stress and maintain consistent post-thaw recovery [62]. | CryoStor CS10, Recovery Cell Culture Freezing Medium |
| DMSO | Cryoprotective agent that prevents ice crystal formation. Standard concentration is 10% in culture medium or serum [61] [63]. | Laboratory-grade DMSO |
| ACK Lysing Buffer | Removes contaminating red blood cells post-isolation, improving accuracy of cell counting and reducing background in functional assays [61]. | Ammonium-Chloride-Potassium Lysing Buffer |
| Viability Stains | Critical for excluding dead cells during analysis, which are a major source of non-specific binding and false positives [25]. | Live/Dead Fixable Violet, Propidium Iodide, Acridine Orange/DAPI |
| Fc Receptor Blocking Solution | Blocks non-specific antibody binding via Fc receptors, significantly reducing background staining and improving signal-to-noise ratio [66] [25]. | Human Fc Block, purified anti-CD16/32 |
| Ficoll-Paque Plus | Density gradient medium for high-viability PBMC isolation from whole blood or apheresis products [63] [25]. | Ficoll-Paque Plus, Lymphoprep |
| FoxP3 Staining Buffer Set | Specialized buffers for transcription factor staining that require cell permeabilization while preserving antibody epitopes [66]. | eBioscience FoxP3 Fix/Perm buffer set |
Troubleshooting Phenotypic Inconsistencies
The following decision tree provides a systematic approach to diagnosing and resolving common issues related to cryopreservation artifacts.
Phenotypic inconsistencies arising from cryopreservation are manageable through a comprehensive understanding of the freezing and thawing processes and their effects on cellular integrity. The strategies outlined—employing optimized, controlled-rate freezing protocols; allowing adequate post-thaw recovery; implementing rigorous Fc receptor blocking; and utilizing viability dyes—collectively preserve antigen expression and minimize non-specific staining. By standardizing these practices, researchers can significantly enhance the reliability and reproducibility of flow cytometry data from cryopreserved samples, thereby strengthening both basic research findings and preclinical drug development workflows.
In the context of cryopreservation protocols for flow cytometry samples, maintaining high cell viability, recovery, and minimizing clumping is paramount for obtaining reliable data. Processing steps such as centrifugation, washing, and filtration are critical junctures where significant cell loss and aggregation can occur, potentially compromising downstream analyses like immunophenotyping. This application note provides detailed, optimized protocols to help researchers and drug development professionals preserve sample integrity from collection through post-thaw analysis. The guidance is framed within a broader research thesis on cryopreservation, emphasizing how optimized processing directly impacts data quality in flow cytometry, particularly for sensitive applications such as T-cell subset analysis [6] [41].
The following tables summarize key quantitative findings from the literature regarding the impact of different processing methods on cell recovery and viability.
Table 1: Impact of Processing Methods on Cell Recovery and Viability
| Processing Method | Cell Type | Key Outcome Metrics | Performance Results | Reference |
|---|---|---|---|---|
| Automated Spinning Membrane Filtration (Lovo) | HPCs (Hematopoietic Progenitor Cells) | Viable CD34+ Cell Recovery | Better recovery compared to COBE 2991 | [67] |
| CD34+ Viability | Maintained | [67] | ||
| DMSO Removal | ~97% eliminated | [67] | ||
| Traditional Centrifugation (COBE 2991) | HPCs | Viable CD34+ Cell Recovery | Lower than Lovo | [67] |
| CD3+ Cell Recovery | >50% (met internal specs) | [67] | ||
| Centrifugation Washing (Adhesive Patterning Model) | H9C2, MPCs, HUVECs | Cell Viability Post-Wash | >80% | [68] |
| Pattern Fidelity (Line Widths) | Effective for 50–200 μm | [68] |
Table 2: Effect of Pre-Processing Variables on Cell Recovery
| Variable | Condition | Impact on PBMC Recovery & Viability | Recommendation | |
|---|---|---|---|---|
| Blood Transport/Storage Temperature | Ambient (15-25°C), <24h | Preserves cell integrity | Use a validated temperature-controlled shipper. | [41] |
| 2-8°C for >24h | Increases granulocyte contamination in PBMC fraction | Avoid prolonged cold storage before separation. | [41] | |
| Density Gradient Centrifugation Temperature | Room Temperature (15-25°C) | Proper RBC aggregation, efficient PBMC separation | Allow blood and reagents to equilibrate to RT. | [41] |
| Cold (2-8°C) | Poor separation, RBC contamination in PBMC fraction | Avoid using cold blood/reagents. | [41] | |
| Post-Thaw Cell Washing | Automated System (Lovo) | High cell recovery, excellent DMSO removal | Ideal for standardizing processing of cryopreserved samples. | [67] |
Experimental Protocols
Optimized Centrifugation Washing for Cell Patterning and General Use
This protocol, adapted from studies on adhesive cell patterning, demonstrates the effective use of centrifugation to remove weakly adhered cells while preserving the viability and structure of the target population. The principle of using a controlled, perpendicular force for washing is highly applicable to general cell processing to minimize clumping and loss [68].
Materials:
- Cell suspension (e.g., H9C2 cardiomyoblasts, HUVECs, MPCs)
- Appropriate cell culture medium
- Phosphate Buffered Saline (PBS)
- Centrifuge with swing-bucket rotors for plates/tubes
- Multi-well culture plates or tubes
Method:
- Cell Seeding: Prepare your single-cell suspension and seed cells onto the desired substrate (e.g., collagen-I, Matrigel-coated surfaces, or standard culture plates) [68].
- Adhesion Period: Allow cells to adhere under standard culture conditions (e.g., 37°C, 5% CO₂) for the required time. For patterning systems, this enables strong binding in specific regions [68].
- Centrifugation Wash:
- Gently add the appropriate washing medium (e.g., PBS or culture medium) to the wells/tubes without disturbing the adhered cell layer.
- Load the plate or tube into a centrifuge with a swing-bucket rotor. Ensure the platform is balanced.
- Centrifuge at a defined, optimized force. The study on patterning cells used this step to selectively remove poorly adhered cells outside of patterned areas. For general applications, parameters must be optimized for each cell type and substrate. Typical ranges might be 100 – 500 x g for 3 – 10 minutes at room temperature.
- Post-centrifugation, carefully decant or aspirate the supernatant, which will contain the non-adherent or weakly adherent cells and debris.
- Analysis: The remaining adhered cells can be analyzed for viability, pattern fidelity, or used in downstream functional assays. The cited study confirmed no significant compromise in immediate cell viability or subsequent tube-forming ability for MPCs and HUVECs after this washing process [68].
Protocol for Thawing and Washing Cryopreserved PBMCs
This standard protocol is critical for flow cytometry sample preparation, focusing on rapid thawing and efficient DMSO removal to maximize recovery and minimize clumping caused by cell debris and cryoprotectant toxicity [41] [9].
Materials:
- Cryopreserved vial of PBMCs
- Water bath or automated thawing device (e.g., ThawSTAR)
- Pre-warmed complete culture medium (e.g., RPMI-1640 with 10% FBS)
- Centrifuge
- Benchtop centrifuge
Method:
- Rapid Thawing:
- Remove the vial from liquid nitrogen storage and immediately place it in a 37°C water bath or automated thawing device. Thaw just until no ice crystals are visible (approximately 2-3 minutes) [9].
- Gently agitate the vial to expedite thawing.
- Dilution and DMSO Reduction:
- Wipe the vial with 70% ethanol before opening.
- Transfer the thawed cell suspension to a sterile centrifuge tube.
- Slowly, drop-wise, add 10 mL of pre-warmed complete medium to the cell suspension while gently swirling the tube. This gradual dilution reduces osmotic shock.
- Centrifugation:
- Centrifuge the cell suspension at approximately 300 - 400 x g for 5 - 10 minutes at room temperature [41].
- Carefully aspirate the supernatant, which contains the DMSO and cell debris.
- Resuspension and Viability Assessment:
- Gently resuspend the cell pellet in a small volume of fresh, pre-warmed complete medium.
- Perform a cell count and viability assessment (e.g., using Trypan Blue exclusion).
- Optional Filtration (to Reduce Clumping):
- If cell clumping is observed, pass the cell suspension through a sterile cell strainer (e.g., 40μm nylon mesh) to obtain a single-cell suspension suitable for flow cytometry [41].
Workflow Visualization
The following diagram illustrates the decision-making workflow for selecting the optimal processing method to minimize cell loss and clumping, based on sample type and critical requirements.
Decision Workflow for Cell Processing Methods
The Scientist's Toolkit: Essential Reagent Solutions
Table 3: Key Reagents and Materials for Optimized Cell Processing
| Item | Function/Description | Application Notes |
|---|---|---|
| Density Gradient Medium (e.g., Ficoll-Paque, Histopaque) | Separates PBMCs from other blood components (RBCs, granulocytes) based on density via centrifugation. | Critical for isolating pure PBMCs from whole blood. Performance is highly dependent on using room temperature reagents [41]. |
| Defined Cryopreservation Media (e.g., CryoStor CS10) | Ready-to-use, serum-free freezing media containing DMSO. Provides a protective, defined environment during freeze-thaw, reducing background cell damage and clumping. | Preferred over lab-made FBS/DMSO mixes for consistency and safety, especially in regulated fields [9]. |
| Controlled-Rate Freezing Container (e.g., Mr. Frosty, CoolCell) | Provides a consistent cooling rate of approximately -1°C/min when placed in a -80°C freezer. Optimizes cell viability during freezing, reducing initial damage that leads to post-thaw clumping. | Essential for creating high-quality cell banks. Slow freezing minimizes intracellular ice crystal formation [9]. |
| Automated Cell Processing System (e.g., Lovo) | Uses spinning membrane filtration to wash cells and remove DMSO post-thaw in a closed, automated system. | Significantly improves recovery of viable CD34+ cells and removes >97% DMSO compared to traditional manual centrifugation, reducing operator-dependent variability and cell loss [67]. |
| Cell Strainers (e.g., 40μm Nylon Mesh) | Physically breaks apart cell aggregates by filtering the suspension, producing a single-cell suspension ideal for flow cytometry. | A simple and effective final step to mitigate clumping before sample analysis or staining [41]. |
Within the rigorous framework of cryopreservation research for flow cytometry, establishing robust pre-freeze quality control (QC) checkpoints is paramount. The integrity of downstream experimental data is wholly dependent on the quality of the cellular material preserved. This application note details the implementation of two critical pre-freeze QC assessments: cell viability analysis using Trypan Blue, 7-AAD, and Acridine Orange/Ethidium Bromide (AO/EB), and mycoplasma contamination testing. These checkpoints serve as essential gatekeepers, ensuring that only samples of verified quality and sterility enter long-term storage, thereby safeguarding precious research resources and ensuring the reliability of future flow cytometric analyses [69] [9].
Pre-Freeze Viability Assessment: A Comparative Analysis
Quantifying cell viability before cryopreservation establishes a crucial baseline, aids in optimizing cryopreservation protocols, and confirms that cells are in a healthy state for freezing. The selection of a viability assay depends on factors such as required accuracy, throughput, equipment availability, and compatibility with downstream applications [69].
The table below summarizes the key characteristics of three commonly used viability assays suitable for pre-freeze assessment.
Table 1: Comparison of Pre-Freeze Viability Assessment Methods
| Assay Feature | Trypan Blue Exclusion | 7-AAD Staining | Acridine Orange/EB Staining |
|---|---|---|---|
| Principle | Dye exclusion via intact plasma membrane | DNA intercalation in membrane-compromised cells | Differential uptake and fluorescence of viable vs. non-viable cells |
| Detection Method | Bright-field microscopy | Flow cytometry | Fluorescence microscopy |
| Key Reagents | 0.4% Trypan Blue solution [69] | 7-AAD Staining Solution [70] | 100 μg/mL AO & 100 μg/mL EB in PBS [71] [72] |
| Viable Cell Signal | Unstained (colorless) | 7-AAD negative (low fluorescence) | Green nuclear fluorescence (AO) |
| Non-Viable Cell Signal | Blue cytoplasmic staining | 7-AAD positive (high fluorescence) | Red/orange nuclear fluorescence (EB) [71] |
| Throughput | Low to moderate | High | Moderate |
| Primary Application | Quick, simple viability and concentration count | Objective, high-throughput viability gating in flow cytometry | Distinguishing live, apoptotic, and dead cells [72] |
Key Research Reagent Solutions
Successful implementation of these QC protocols relies on specific reagents. The following table outlines essential materials and their functions.
Table 2: Essential Research Reagents for Pre-Freeze Quality Control
| Reagent/Material | Function/Application | Example |
|---|---|---|
| Cryopreservation Medium | Provides a protective environment during freeze-thaw; often contains cryoprotectants like DMSO. | CryoStor CS10 [9] |
| Viability Dyes (7-AAD/PI) | Nucleic acid binding dyes for flow cytometry-based viability assessment. | BD Pharmingen 7-AAD Viability Staining Solution [70] [73] |
| Fixable Viability Dyes (FVD) | Amine-reactive dyes that covalently bind to dead cells; compatible with intracellular staining and fixation. | Invitrogen eFluor 780 Fixable Viability Dye [70] |
| Dual Fluorescence Stains (AO/EB) | Differential fluorescent staining for microscopic identification of live, apoptotic, and dead cells. | Lab-prepared solution of Acridine Orange & Ethidium Bromide [71] [72] |
| Mycoplasma Detection Kit | For specific and sensitive detection of mycoplasma contamination in cell cultures. | PCR-based detection kits [74] |
| Fc Receptor Blocking Reagent | Reduces non-specific antibody binding in flow cytometry, improving data quality. | Purified normal serum (e.g., Rat Serum, Mouse Serum) [27] |
Detailed Experimental Protocols
Protocol 1: Viability Assessment by Manual Trypan Blue Exclusion
This protocol provides a simple and cost-effective method for determining cell viability and concentration prior to cryopreservation [69].
- Step 1. Harvest and Dilution: Harvest the cells and centrifuge. Resuspend the cell pellet in an appropriate buffer, such as Hank's Balanced Salt Solution (HBSS). Dilute the sample based on the expected cell concentration [69].
- Step 2. Staining: Mix one part of the cell suspension with one part of 0.4% Trypan Blue solution (e.g., from Lonza). Allow the mixture to incubate for 1-2 minutes at room temperature. Note: Do not incubate for extended periods, as this can lead to false positives.
- Step 3. Loading and Counting: Carefully load a small volume (e.g., 10-20 μL) of the stained mixture into a hemocytometer. Using a light microscope at 40X magnification, count the number of unstained (viable) and blue-stained (non-viable) cells in the appropriate squares.
- Step 4. Calculation: Calculate the percentage of viable cells using the formula: (Number of Viable Cells / Total Number of Cells Counted) × 100 [69].
Protocol 2: Viability Staining with 7-AAD for Flow Cytometry
This protocol describes a flow cytometry-based viability assay that can be performed alone or combined with cell surface marker staining, providing an objective and high-throughput pre-freeze assessment [69] [70] [73].
- Step 1. Cell Preparation: After staining for surface antigens (if applicable), wash the cells 1-2 times with a flow cytometry staining buffer. Centrifuge at 300-500 × g for 5 minutes and carefully decant the supernatant [70].
- Step 2. Staining: Resuspend the cell pellet in an appropriate volume of staining buffer. Add 5 μL of 7-AAD Staining Solution per 100 μL of cell suspension. Vortex gently to mix.
- Step 3. Incubation and Analysis: Incubate the tubes for 5-15 minutes on ice or at room temperature, protected from light. Do not wash the cells after staining. Proceed to analyze the samples on a flow cytometer within 4 hours. Viable cells are identified as the 7-AAD negative population [70].
Protocol 3: Mycoplasma Detection by DNA Staining with Confocal Microscopy
This protocol utilizes a colocalization method with Hoechst 33342 (DNA dye) and Wheat Germ Agglutinin (WGA, membrane dye) to accurately detect mycoplasma contamination on the surface of host cells, minimizing false positives from cytoplasmic DNA [74].
- Step 1. Cell Culture and Staining: Grow test cells on confocal dishes. Stain the cells with WGA Oregon Green 488 conjugate (e.g., 5 μg/mL) for 15 minutes at 37°C to label the cell membrane. Wash the cells twice with 1X PBS.
- Step 2. DNA Staining: Subsequently, stain the cells with Hoechst 33342 (e.g., 1 μg/mL) for 15 minutes at 37°C, protected from light. Wash the cells twice with 1X PBS to remove excess dye.
- Step 3. Imaging and Analysis: Capture images using a confocal microscope with a 60x oil-immersion objective. Process images using software like ImageJ. True mycoplasma contamination is indicated by the colocalization of Hoechst (blue) and WGA (green) signals on the host cell membrane, forming a tight ring. The absence of blue fluorescence on the membrane surface indicates a mycoplasma-free culture [74].
The following diagram illustrates the integration of these quality control checkpoints into a pre-freeze workflow for cell processing.
Diagram 1: Integrated Pre-freeze QC Workflow
Implementing a standardized pre-freeze protocol incorporating viability assessment and mycoplasma testing is a critical investment in research quality. By establishing these checkpoints, researchers can create high-quality, reliable cell banks, ensuring that cryopreserved samples remain a robust resource for generating reproducible and meaningful flow cytometry data [69] [9] [74].
Validating Your Protocol: Stability, Functionality, and Advanced Analytical Comparisons
Cryopreservation of peripheral blood mononuclear cells (PBMCs) is a fundamental practice in immunological research and clinical trials, enabling the decoupling of sample collection from complex analytical procedures. This process facilitates multi-center trials, allows batch analysis to reduce inter-assay variability, and permits longitudinal studies by banking samples for future investigation [28]. However, the impact of long-term cryostorage on cell viability, phenotypic composition, and transcriptomic integrity remains a significant concern, as suboptimal preservation can introduce substantial artifacts in downstream assays. This application note synthesizes recent evidence to evaluate the stability of cryopreserved PBMCs over 6, 12, and 24 months, providing validated protocols and analytical frameworks for researchers requiring reliable long-term sample preservation. Within the broader thesis on cryopreservation protocols for flow cytometry samples, this work establishes critical timelines for sample stability and identifies key vulnerable parameters that require monitoring in quality-controlled biobanking operations.
Quantitative Stability Assessment Across Storage Durations
The following tables consolidate empirical data on PBMC stability across multiple studies, providing a comprehensive reference for expected outcomes at standard storage intervals.
Table 1: Temporal Evolution of PBMC Viability and Recovery Metrics
| Storage Duration | Cell Viability | Recovery Rate/Number of Sequenced Cells | Key Observations | Citation |
|---|---|---|---|---|
| 6 months | Relatively stable across major immune cell types | ~32% reduction in scRNA-seq cell capture efficiency after 12 months (measured relative to fresh) | Minimal transcriptome perturbation; cell population composition preserved | [25] |
| 12 months | Relatively stable across major immune cell types | Significant reduction post-thaw in total cell number; CD4+ T cells most affected | AP-1 complex, stress response, and calcium ion response genes showed small-scale changes (<2-fold) | [25] [75] |
| 24 months | High viability maintained in CS10 and NutriFreez D10 media | Not specified | Media with <7.5% DMSO showed significant viability loss and were eliminated | [28] |
Table 2: Phenotypic Stability of Major PBMC Populations After Cryopreservation
| Cell Type | Tolerance to Cryopreservation | Key Phenotypic Changes | Functional Impact | Citation |
|---|---|---|---|---|
| CD4+ T cells | Most significantly affected | Significant reduction post-thaw | ROS-induced cell death; reduced IL-2 secretion and proliferation | [75] |
| CD8+ T cells | Moderate tolerance | Less reduction compared to CD4+ T cells | Relatively maintained | [75] |
| Monocytes | More tolerant | Population maintained | Viability and frequency relatively stable | [25] [75] |
| B cells | More tolerant | Population maintained | Viability and frequency relatively stable | [25] [75] |
| NK cells | More tolerant | Population maintained | Viability and frequency relatively stable | [25] [75] |
| NKT cells | More tolerant | Population maintained | Not specified | [75] |
Experimental Protocols for Stability Assessment
PBMC Isolation, Cryopreservation, and Thawing
Materials:
- Lymphocyte Separation Medium (e.g., Lymphoprep, Ficoll)
- Cryopreservation medium (e.g., CryoStor CS10, NutriFreez D10, or FBS with 10% DMSO)
- Programmable freezer (e.g., CryoMed Freezer) or isopropanol container (e.g., CoolCell)
- Liquid nitrogen storage system
- Pre-warmed RP10 medium (RPMI1640 with 10% FBS, 10mM HEPES, 0.1mg/mL Gentamycin)
- 37°C water bath
Procedure:
- PBMC Isolation: Layer leukocyte suspension or whole blood onto Lymphocyte Separation Medium at a 1:1.5 ratio [75]. Centrifuge at 400-700 × g for 25-30 minutes at room temperature with brake disengaged [25] [75]. Collect PBMC layer and wash with PBS 2-3 times at 500 × g for 5-10 minutes [25] [75].
Cryopreservation: Resuspend PBMCs at 10-12 × 10^6 cells/mL in cryopreservation medium [25] [28]. Dispense 1mL aliquots into cryovials. Freeze using controlled-rate freezing: 1°C/min to -4°C, 25°C/min to -40°C, 10°C/min to -12°C, 1°C/min to -40°C, and 10°C/min to -90°C [25]. Alternatively, use isopropanol containers at -80°C for 24 hours before transferring to vapor-phase liquid nitrogen [28].
Thawing and Recovery: Rapidly thaw cryovials in 37°C water bath until small ice crystal remains [25]. Transfer cell suspension to 15mL tube containing 10mL pre-warmed RP10 medium with DNase I (10μg/mL) [28]. Centrifuge at 500 × g for 5 minutes at room temperature. Resuspend pellet in fresh medium and repeat wash step. Perform viability assessment via trypan blue exclusion or propidium iodide staining [25].
Whole Blood Cryopreservation (CryoSCAPE Protocol)
Materials:
- Sodium heparin blood collection tubes
- Freezing medium: 15% DMSO diluted with CryoStor preservation medium
- RBC lysis buffer
- DNase I solution
- Slow freezing container
Procedure:
- Blood Collection and Mixing: Collect whole blood in sodium heparin tubes. Mix blood 1:1 with 15% DMSO freezing medium by inversion to achieve final 7.5% DMSO concentration [76].
Cryopreservation: Transfer 5mL aliquots to cryopreservation tubes. Place in slow freezing container and store at -80°C or transfer to liquid nitrogen after 24 hours [76].
Thawing and PBMC Enrichment: Thaw samples in 37°C water bath. Perform RBC lysis using appropriate buffer. Incubate with DNase I solution to reduce clumping. Enrich PBMCs using FACS or magnetic bead depletion to remove granulocytes and dead cells [76].
Assessment of Cell Viability and Phenotype
Flow Cytometry Protocol:
- Viability Staining: Resuspend 2 × 10^6 cells in 1mL PBS. Add 1μL Live/Dead Fixable Violet Dead Cell Stain. Incubate on ice for 30 minutes protected from light [25].
Surface Marker Staining: Wash cells with 2% BSA wash medium. Block with FC-blocking medium for 10 minutes at room temperature. Stain with antibody cocktail (e.g., CD3-FITC, CD16/56-PE, CD45-PerCP-Cy5.5, CD4-PE-Cy7, CD19-APC, CD8-APC-Cy7) for 20 minutes at 4°C [25].
Processing and Analysis: Lyse cells with FACS lysing solution, wash twice, and resuspend in 500μL wash medium. Acquire data on flow cytometer and analyze using appropriate software (e.g., Cytoexpert, Kaluza) [25] [75].
Functional Assays
T Cell Proliferation and Cytokine Production:
- Proliferation Assay: Incubate PBMCs (5 × 10^5 cells/mL) with 2μmol/L CFSE at 37°C for 20 minutes. Wash with pre-cooled PBS and culture in RPMI 1640 with 10% FBS. Stimulate with CD3 (2μg/mL) and CD28 (1μg/mL) antibodies for 72 hours. Analyze CFSE dilution by flow cytometry [75].
- Intracellular Cytokine Staining: Culture lymphocytes with cell activation cocktail (PMA and ionomycin) and Brefeldin A (5μg/mL) for 5 hours. Perform surface staining, then fix and permeabilize cells using intracellular staining kit. Stain intracellular cytokines (e.g., IL-2) and analyze by flow cytometry [75].
Transcriptomic Analysis
Single-Cell RNA Sequencing:
- Library Preparation: Prepare single-cell suspensions with >90% viability. For 10× Genomics platform, resuspend cells at 1000-1200 cells/μL in RPMI or DMEM with 2% FBS [77]. Generate single-cell whole transcriptome libraries using appropriate kits (e.g., BD Rhapsody WTA Amplification Kit) [75].
- Sequencing and Data Analysis: Sequence libraries on Illumina NovaSeq platform (2 × 150 bp). Process raw data using appropriate pipelines (e.g., BD Rhapsody analysis pipeline, Seurat package). Perform dimensionality reduction, clustering, and differential expression analysis [25] [75].
Signaling Pathways in Cryopreservation-Induced Stress
The following diagram illustrates the primary molecular pathways implicated in cryopreservation-associated stress responses, particularly the mechanisms underlying CD4+ T cell vulnerability:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Cryopreservation and Assessment
| Reagent Category | Specific Product/Composition | Function and Application | Performance Notes |
|---|---|---|---|
| Serum-Based Freezing Media | 90% FBS + 10% DMSO | Traditional reference medium; cryoprotection | Effective but raises ethical concerns and batch variability [28] |
| Serum-Free Freezing Media | CryoStor CS10 | Xeno-free medium with 10% DMSO; cryoprotection | Maintains high viability and functionality over 24 months [28] |
| Serum-Free Freezing Media | NutriFreez D10 | Animal-protein-free medium with 10% DMSO; cryoprotection | Comparable to FBS-based media for long-term preservation [28] |
| Cell Separation Media | Lymphocyte Separation Medium (Ficoll) | Density gradient medium for PBMC isolation | Standard for PBMC isolation from whole blood [25] [75] |
| Viability Assessment | Trypan Blue / Propidium Iodide | Membrane integrity dyes for viability staining | Standard viability assessment pre- and post-cryopreservation [25] |
| Advanced Viability Staining | Live/Dead Fixable Violet Stain | Fixable viability dye for flow cytometry | Distinguishes live/dead cells in immunophenotyping panels [25] |
| Cell Activation Reagents | PMA/Ionomycin + Brefeldin A | T cell stimulation and protein transport inhibition | Enables intracellular cytokine detection by flow cytometry [75] |
| Proliferation Tracking | CFSE | Cell division tracking dye | Measures T cell proliferation capacity post-thaw [75] |
This application note provides comprehensive evidence that PBMCs can maintain viability, phenotypic integrity, and transcriptome profiles through 12 months of cryopreservation when optimized protocols are employed. While scRNA-seq cell capture efficiency may decrease by approximately 32% after 12 months, the transcriptome profiles themselves show minimal perturbation with only small-scale changes in stress response genes [25]. Critically, CD4+ T cells demonstrate particular vulnerability to cryopreservation-induced stress, primarily through ROS-mediated pathways [75]. For studies requiring storage beyond 12 months, serum-free media with 10% DMSO (CryoStor CS10, NutriFreez D10) maintain cell viability and functionality through 24 months, whereas media with DMSO concentrations below 7.5% show significant viability loss [28]. These findings provide a robust framework for designing longitudinal studies and biobanking operations, emphasizing the importance of standardized protocols, appropriate cryopreservation media selection, and targeted monitoring of vulnerable cell populations to ensure data reliability across extended storage intervals.
Cryopreservation is a critical step in the pipeline of cellular therapy and biomedical research, enabling cell transport, banking, and the availability of off-the-shelf therapeutic products [78]. However, the freezing and thawing processes impose severe stresses that can compromise key cellular functions beyond mere membrane integrity. For cell-based therapies and advanced research applications, confirming that post-thaw cells retain their functional capacity is paramount. This application note details standardized protocols and analytical frameworks for assessing three fundamental pillars of cellular function post-threservation: differentiation potential, proliferation capacity, and wound healing/migration capability. These functional validation assays are essential for ensuring that cryopreserved cells, particularly those destined for flow cytometry analysis or therapeutic use, maintain their biological relevance and experimental utility.
Quantitative Assessment of Post-Thaw Recovery
The recovery of cellular attributes after thawing is a time-dependent process. A comprehensive quantitative assessment of human Bone Marrow-derived Mesenchymal Stem Cells (hBM-MSCs) reveals the dynamic nature of this recovery. The data below, derived from discrete analysis of three donor cell lines, provides a clear timeline of functional restoration [78].
Table 1: Temporal Recovery of hBM-MSC Attributes Post-Thaw
| Cell Attribute | Immediately (0h) Post-Thaw | 4 Hours Post-Thaw | 24 Hours Post-Thaw | Beyond 24 Hours Post-Thaw |
|---|---|---|---|---|
| Viability | Reduced | Intermediate | Recovered to pre-freeze levels | Maintained |
| Apoptosis Level | Increased | Elevated | Decreased | Stable |
| Metabolic Activity | Impaired | Impaired | Remains lower than fresh cells | Variable recovery by cell line |
| Adhesion Potential | Impaired | Impaired | Remains lower than fresh cells | Variable recovery by cell line |
| Proliferation Rate | Not Applicable | Not Applicable | Not Applicable | Comparable to fresh cells |
| CFU-F Ability | Not Applicable | Not Applicable | Not Applicable | Reduced in 2 of 3 cell lines |
| Differentiation Potential | Not Applicable | Not Applicable | Not Applicable | Variably affected (cell line-dependent) |
Experimental Protocols for Functional Validation
Protocol 1: Assessment of Differentiation Potential
The ability of stem cells, such as MSCs, to differentiate into multiple lineages is a cornerstone of their functional identity. This protocol outlines the steps to validate this potential post-thaw.
Materials:
- Post-thaw MSCs (e.g., hBM-MSCs)
- Osteogenic Differentiation Medium (e.g., StemPro Osteogenesis Differentiation Kit)
- Chondrogenic Differentiation Medium (e.g., StemPro Chondrogenesis Differentiation Kit)
- Adipogenic Differentiation Medium (optional)
- Multi-well cell culture plates (e.g., 12-well plates)
- 2% Alizarin Red S solution (for osteogenic staining)
- 1% Alcian Blue solution (for chondrogenic staining)
- 4% Paraformaldehyde (PFA)
Method:
- Thaw and Plate Cells: Thaw cryopreserved MSCs and seed them in standard growth medium at a density of 5,000 cells/cm². Allow the cells to adhere and recover for 24 hours [78].
- Induce Differentiation: After 24 hours, replace the growth medium with specific differentiation induction media (osteogenic or chondrogenic). Maintain control cells in standard growth medium.
- Maintain Cultures: Culture the cells for 2-4 weeks, changing the differentiation media every 3-4 days.
- Fix and Stain: At the end of the differentiation period, wash the cells with PBS and fix with 4% PFA for 15 minutes.
- Analysis: Qualitatively assess differentiation by visual observation of staining. For quantitative analysis, the dyes can be eluted and measured spectrophotometrically.
Protocol 2: Measurement of Proliferation and Clonogenic Capacity
Proliferation is a fundamental indicator of cellular health. This protocol combines simple population doubling assessment with the more sensitive Colony-Forming Unit-Fibroblast (CFU-F) assay, which measures the clonogenic potential of a cell population.
Materials:
- Post-thaw cells
- Appropriate growth medium
- 0.25% (w/v) trypsin-EDTA
- Phosphate-Buffered Saline (PBS), no calcium, no magnesium
- Cell counter (e.g., automated cell counter or hemocytometer)
- 6-well or 10 cm cell culture dishes
- Crystal Violet or Methylene Blue stain (for CFU-F)
Method: A. Population Doubling Assessment
- Seed Cells: After thawing and a brief recovery (e.g., 4-24h), seed cells at a known, low density (e.g., 5,000 cells/cm²) in culture flasks [78].
- Harvest and Count: Once cells reach ~70-80% confluence, detach them using 0.25% trypsin-EDTA, neutralize with complete medium, and perform a cell count using an automated cell counter or hemocytometer [78].
- Calculate: The population doubling time can be calculated from the initial and final cell numbers and the time in culture.
B. Colony-Forming Unit (CFU-F) Assay
- Seed at Clonal Density: After thawing, seed cells at a very low density (e.g., 100-1,000 cells) in a 10 cm dish or 6-well plate to allow for isolated colony formation.
- Culture: Incubate the cells for 10-14 days, changing the medium every 3-4 days, to allow for the formation of distinct colonies derived from single progenitor cells.
- Stain and Count: After the incubation period, wash the cells with PBS, fix with 4% PFA or methanol, and stain with 0.5% Crystal Violet or Methylene Blue. Count the number of colonies (typically defined as aggregates of >50 cells). The CFU-F efficiency is calculated as (number of colonies / number of cells seeded) * 100%.
Protocol 3: Wound Healing / Scratch Migration Assay
The wound healing assay is a classic, straightforward method to quantitatively measure the collective migration of cells in two dimensions, a key function for therapeutic cells involved in tissue repair.
Materials:
- Confluent monolayer of post-thaw cells (adherent cell type)
- 12-well or 24-well cell culture plates
- Serum-free medium
- 200 µL sterile pipette tip
- PBS
- Light microscope with digital camera
- Image analysis software (e.g., ImageJ)
Method:
- Prepare Confluent Monolayer: Seed post-thaw cells in a multi-well plate and culture until they form a 100% confluent monolayer. To minimize the confounding effects of proliferation, serum-starve the cells (e.g., by replacing the medium with serum-free medium) for 24 hours prior to wounding [80].
- Create a "Wound": Using a sterile 200 µL pipette tip, create a scratch along the entire diameter of the well. Hold the tip perpendicular to the plate bottom and apply consistent, firm pressure to ensure a clean, uniform wound [81] [80].
- Tip: For increased consistency across multiple wells, consider using commercial inserts that create a standardized gap upon removal [81].
- Wash and Add Medium: Gently wash the well with PBS 1-2 times to remove any dislodged cells and debris. Add fresh serum-free medium (or medium containing the desired test compounds) [80].
- Image Acquisition: Immediately after scratching (time 0), use a light microscope with a digital camera to capture images of the wound at several marked locations per well. Carefully mark these locations on the bottom of the plate for precise re-imaging [80].
- Monitor Closure: Return the plate to the incubator and re-image the exact same locations at regular intervals (e.g., every 4, 8, 12, and 24 hours) until the wound has closed.
- Quantitative Analysis:
- Using ImageJ or similar software, measure the width of the wound gap at each time point.
- Calculate the percentage of wound closure at time t using the formula: % Wound Closure = (Wound Width at 0h - Wound Width at t) / Wound Width at 0h × 100 [80].
- The migration rate can be expressed as the change in wound width per unit time.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of functional validation assays requires high-quality, standardized reagents. The following table details key solutions and materials used in the protocols described above.
Table 2: Essential Research Reagent Solutions for Post-Thaw Functional Assays
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| DMSO-Free Cryopreservation Solutions | Alternative to DMSO to reduce cytotoxicity and improve post-thaw function. May contain sugars, sugar alcohols, and small molecules. | Sucrose/Glycerol/Creatine (SGC); Sucrose/Mannitol/Creatine (SMC) [79] |
| Lineage-Specific Differentiation Media | To induce and support differentiation into specific cell lineages for functional potency testing. | StemPro Osteogenesis/Chondrogenesis/Adipogenesis Kits [79] |
| Specific Staining Reagents | To visualize and quantify successful differentiation outcomes. | Alizarin Red S (calcium deposits); Alcian Blue (proteoglycans) [79] |
| Commercial Wound Creation Inserts | To create highly standardized and reproducible cell-free gaps for migration assays, minimizing initial variability. | ibidi, Cell Biolabs, or Platypus Technologies inserts [81] |
| Flow Cytometry Antibody Panels | For immunophenotyping to confirm cell identity and characterize surface markers pre- and post-assay. | Positive (CD73, CD90, CD105) and negative (CD14, CD34, CD45) MSC markers [78] |
| High-Throughput Imaging Systems | For automated, quantitative imaging of wound closure and cell proliferation in multi-well formats. | Compatible with 12-well to 96-well plates; live-cell imaging capability [82] |
Functional validation of post-thaw cells is a non-negotiable step in ensuring the reliability of research data and the efficacy of cellular therapeutics. The assays detailed herein—differentiation, proliferation/clonogenicity, and wound healing—provide a robust framework for confirming that critical cellular functions survive the rigors of cryopreservation. The quantitative data clearly shows that a 24-hour post-thaw recovery period is insufficient for the full restoration of all cellular attributes, such as metabolic activity and adhesion potential [78]. Therefore, the timing of functional assessment must be carefully considered based on the intended application. By integrating these standardized protocols and quality control measures, researchers and drug development professionals can significantly enhance the reproducibility and clinical relevance of their work with cryopreserved cells.
Comparative Analysis of Manual Gating vs. Automated Algorithmic Tools (UMAP, FlowSOM) for Analyzing Cryopreserved Samples
The analysis of cryopreserved samples using flow cytometry represents a cornerstone of modern immunological research and clinical diagnostics. This process has traditionally relied on manual gating, a technique where researchers sequentially isolate cell populations of interest based on their protein marker expression visualized on two-dimensional scatter plots [83]. While this method offers analysts direct control, it introduces significant challenges, including subjective bias, time-intensive processes, and difficulty in analyzing high-dimensional data [6] [84].
The emergence of automated algorithmic tools like FlowSOM and UMAP has revolutionized this workflow. These computational approaches enable high-dimensional, unbiased analysis of cytometry data, offering enhanced reproducibility and the capacity to identify novel cellular patterns [83] [6]. The pressing question for researchers is how these methods compare when applied to the analysis of cryopreserved samples, where the freezing and thawing processes may alter cell integrity and marker expression.
This application note provides a detailed, evidence-based comparison of these methodologies, offering structured protocols and quantitative data to guide researchers in selecting the appropriate analytical framework for their cryopreserved sample analysis.
Comparative Performance Analysis
Evaluations across multiple studies have demonstrated that automated algorithmic analysis and manual gating can reach similar biological conclusions when analyzing cryopreserved samples, though their operational characteristics differ significantly.
Quantitative Comparison of Gating Methods
Table 1: Performance Characteristics of Gating Methods for Cryopreserved Samples
| Method Characteristic | Manual Gating | Automated Algorithmic Analysis |
|---|---|---|
| Analysis Time | Time-consuming, sequential 2D plot analysis [6] | Rapid, parallel processing of multiple parameters [6] |
| Subjectivity | High (dependent on operator experience) [6] [84] | Low (algorithm-driven, reproducible) [6] [84] |
| Dimensionality Capability | Limited to 2D visualization, requiring multiple plots [6] | High-dimensional analysis in a single output [6] |
| Reproducibility | Variable between operators [83] [85] | High when parameters are maintained [6] |
| Detection of Novel Populations | Limited to known, anticipated populations | Enhanced through unbiased clustering [6] |
| Required Expertise | Deep domain knowledge, gating experience | Computational literacy, statistical understanding |
| Data Visualization | Sequential 2D dot plots | UMAP projections, heatmaps, meta-cluster analyses [6] |
A comprehensive 2024 evaluation of gating methods across six diverse datasets found that several automated tools, including FlowSOM, demonstrated strong performance in reproducing manual gating results when using manual gates as ground truth [83]. This suggests that automated methods can achieve comparable population identification to experienced human analysts.
Research specifically comparing these methodologies on cryopreserved samples has revealed convergent findings. A 2025 study examining cryopreserved mouse spleen cells for T-cell subsets found that both manual gating and automated analysis reached similar conclusions regarding population proportions and spatial relationships following short-term cryopreservation (2 weeks) [6] [84]. Both methods detected significant changes with increasing cryopreservation time and freeze-thaw cycles, suggesting these alterations represent genuine biological effects rather than methodological artifacts [6].
The primary advantage of automated analysis lies in its enhanced objectivity and ability to intuitively highlight spatial positional variations between cell populations [84]. This capability is particularly valuable for detecting subtle phenotypic shifts in cryopreserved samples that might be overlooked in sequential 2D manual gating.
Detailed Experimental Protocols
Sample Preparation and Cryopreservation Protocol
The integrity of downstream analysis, regardless of analytical method, depends heavily on proper sample preparation and cryopreservation techniques.
Table 2: Essential Reagents for Cryopreservation and Flow Cytometry
| Reagent/Category | Specific Examples | Function/Purpose |
|---|---|---|
| Cryopreservation Media | Freezing Media (50% DMEM, 40% FBS, 10% DMSO) [6] | Protects cells during freezing process; maintains viability |
| Viability Stains | DAPI, Propidium Iodide, Live/Dead Fixable Violet Stain [6] [1] | Distinguishes live from dead cells for accurate analysis |
| Antibody Panels | CD3, CD4, CD8, CD25, CD45, CD19, CD16/56 [6] [1] | Identifies specific cell surface and intracellular markers |
| RBC Lysis Buffer | Commercial lysing solutions | Removes red blood cells from tissue suspensions |
| Cell Staining Buffer | PBS with BSA | Provides appropriate medium for antibody binding |
| Fixation Reagents | BD FACS Lysing Solution [1] | Preserves cellular integrity for later analysis |
Protocol Workflow:
Detailed Procedures:
Sample Collection & Single-Cell Suspension Preparation:
- Harvest tissue (e.g., mouse spleen) and place in cold PBS [6].
- Gently grind tissue through a 70μm strainer to create a single-cell suspension.
- Centrifuge at 500× g for 5 minutes at 4°C and discard supernatant.
- Resuspend pellet in 2mL red blood cell (RBC) lysis buffer, incubate at room temperature for 2 minutes, then add 2mL PBS to stop lysis [6].
- Centrifuge again, resuspend in PBS, and count cells.
Cryopreservation Process:
- Resuspend cell pellet at 400-600×10^6 cells/mL in ice-cold freezing media (e.g., 50% DMEM, 40% FBS, 10% DMSO) [6].
- Alternatively, for whole blood cryopreservation, mix blood 1:1 with 15% DMSO freezing media to achieve a final 7.5% DMSO concentration [76].
- Transfer 1mL aliquots to cryovials and place in a controlled-rate freezing container.
- Store at -80°C or in liquid nitrogen for long-term preservation.
Thawing and Staining:
- Rapidly thaw cryovials in a 37°C water bath until a small ice crystal remains [6] [76].
- Transfer cell suspension to a tube containing 10mL pre-warmed complete media (e.g., RP10).
- Centrifuge at 500× g for 5 minutes and discard supernatant.
- Resuspend in PBS and stain with viability dye (e.g., Live/Dead Fixable Violet Stain) on ice for 30 minutes, protected from light [1].
- Wash with staining buffer (PBS with BSA), then incubate with FC block for 10 minutes.
- Stain with surface antibody cocktail for 20 minutes at 4°C.
- Fix cells if necessary, wash twice, and resuspend in buffer for acquisition.
Data Analysis Workflows
Manual Gating Protocol:
- Import acquired FCS files into analysis software (e.g., FlowJo, FACSDiva).
- Create a sequential gating hierarchy:
- Begin with FSC-A vs. SSC-A to gate on total cells, excluding debris.
- Proceed to FSC-A vs. FSC-H to exclude doublets.
- Gate on viability dye-negative populations to select live cells.
- Create successive 2D plots for marker combinations (e.g., CD3 vs. CD4, CD8 vs. CD25) to identify target populations [6].
- Record population percentages and absolute counts for statistical analysis.
Automated Algorithmic Analysis Protocol:
- Data Preprocessing:
- Concatenate FCS files from different experimental groups in FlowJo.
- Downsample to an equal number of events (e.g., 10,000 per sample) to normalize representation [6].
- Apply arcsinh transformation to improve population visualization [86].
- Perform automated compensation to correct for spectral overlap.
FlowSOM Analysis:
- Run FlowSOM on the concatenated, preprocessed data.
- Set the number of metaclusters (e.g., 6 for basic T-cell subsets) [6].
- Generate a minimal spanning tree (MST) visualization of cell populations.
- Interpret metaclusters based on marker expression heatmaps.
UMAP Visualization:
- Run UMAP with default settings (nearest neighbors=15, minimum distance=0.5) using Euclidean distance [6].
- Overlay FlowSOM cluster identities onto UMAP plots.
- Color-code populations by experimental conditions or marker expression.
Critical Considerations for Cryopreserved Samples
Impact of Cryopreservation on Data Quality
The cryopreservation process itself introduces variables that can affect downstream analysis regardless of the gating method employed:
Cell Viability and Recovery: Studies report slight decreases in cell number and viability after freeze-thaw cycles, with more significant changes observed with increasing cryopreservation duration [6] [84]. These effects necessitate careful viability staining and incorporation of viability parameters in both manual and automated gating strategies.
Antigen Integrity: Research suggests that cryopreservation may alter the molecular conformation of some surface markers, potentially affecting antibody binding efficiency and fluorescence intensity [84]. This underscores the importance of validating antibody panels specifically for use with cryopreserved samples.
Transcriptomic Stability: While optimized cryopreservation protocols demonstrate minimal effects on PBMC viability and population composition over 6-12 months, studies note reduced single-cell RNA sequencing cell capture efficiency after extended cryopreservation (∼32% reduction after 12 months) [1]. This highlights considerations for multi-omic studies utilizing cryopreserved samples.
Method Selection Guidelines
Optimal Use Cases for Manual Gating:
- Small-scale studies with limited sample numbers
- Targeted analysis of well-defined populations
- When computational resources or expertise are limited
- Quality control checks of automated findings
Optimal Use Cases for Automated Algorithmic Tools:
- Large-scale studies requiring high-throughput analysis [82]
- Discovery-phase research aiming to identify novel cell populations
- Complex multi-parameter panels (>10 colors) [87]
- Studies requiring high reproducibility across multiple analysts
- When analyzing subtle phenotypic shifts in cell populations [6]
Hybrid Approach: Many advanced flow cytometry laboratories now employ a hybrid strategy, using automated tools for primary population identification followed by manual verification of key populations. This approach leverages the strengths of both methodologies while mitigating their respective limitations.
The comparative analysis of manual gating and automated algorithmic tools for analyzing cryopreserved samples reveals a nuanced landscape where method selection should be guided by specific research objectives and practical constraints. While both approaches can generate concordant biological conclusions regarding cell population frequencies in cryopreserved samples, automated methods offer significant advantages in reproducibility, throughput, and ability to visualize complex high-dimensional relationships.
For researchers working within the context of cryopreservation protocol development, incorporating automated analytical tools like FlowSOM and UMAP provides an objective framework for assessing the functional impact of protocol modifications on immune cell composition and phenotype. The protocols and comparative data presented herein offer a foundation for implementing these advanced analytical techniques, potentially enhancing the reliability and discovery potential of flow cytometry studies utilizing cryopreserved samples.
Cryopreservation is a critical process in biomedical research and clinical applications, serving as the cornerstone for maintaining cell viability, functionality, and genetic stability over time. For flow cytometry samples—where accurate quantification of cell populations depends entirely on sample integrity—implementing robust, standardized cryopreservation protocols is paramount. The transition from research-grade to clinical-grade cryopreservation requires adherence to rigorous quality management systems, validated reagents, and standardized operating procedures that ensure both reproducibility and compliance with regulatory standards.
This application note examines current clinical practices in cryopreservation, focusing on two commercially available, validated media: CryoStor CS10 and NutriFreez D10 Cryopreservation Medium. By benchmarking against protocols from active transplant centers and leveraging data from controlled studies, we provide a comprehensive framework for implementing clinical-standard cryopreservation protocols specifically optimized for flow cytometry sample preparation.
Commercial Cryopreservation Media: Comparative Analysis
Key Commercial Formulations
Table 1: Commercial Cryopreservation Media Specifications
| Parameter | CryoStor CS10 | NutriFreez D10 |
|---|---|---|
| DMSO Concentration | 10% | 10% |
| Formulation Base | Serum-free, animal component-free | Serum-free, protein-free, animal component-free |
| Special Additives | Not specified | Methylcellulose |
| Primary Cell Applications | Human pluripotent stem cells (hESC, iPSC), sensitive cell types | Mesenchymal stem cells, pluripotent stem cells, PBMCs, T cells (CAR-T, TILs) |
| Quality Standards | cGMP manufactured | cGMP, ISO 13485, Drug Master File available |
| Regulatory Status | For research use | CE IVD Class I, US FDA IVD notified |
| Key Validation | Optimized for slow cooling protocols | Superior recovery in hPSCs vs. serum-containing media |
Data sourced from manufacturer specifications and product information sheets [88] [89] [90].
Performance Characteristics
Both CryoStor CS10 and NutriFreez D10 are chemically defined, serum-free formulations containing 10% DMSO, aligning with current trends toward xeno-free cell culture and preservation systems. This characteristic is particularly valuable for clinical applications where animal-derived components pose regulatory concerns and potential batch-to-batch variability.
Independent validation studies demonstrate the efficacy of these formulations. For NutriFreez D10, research conducted at the Research and Development Center for Cell Therapy (Japan) showed it provided the best recovery rate for human pluripotent stem cells after thawing compared to other media [88] [89]. Similarly, evaluation at the Ottawa Hospital Research Institute indicated that mesenchymal stem cells cryopreserved in NutriFreez D10 exhibited the best post-thaw viability [88].
Clinical Protocols from Transplant Centers
Quality Management in Cryopreservation
Transplant centers operate under stringent quality management systems that provide valuable models for research laboratories aiming to implement clinical standards. The Organisation for Economic Development and Co-operation (OECD) Best Practice Guidelines for Biological Resource Centres (BRCs) establish comprehensive frameworks for maintaining biological materials, emphasizing the need for validated preservation methodologies and strain stability [91]. These guidelines encompass:
- Laboratory design and procedural requirements
- Handling, authenticity, preservation and distribution procedures
- Data recording, validation and access
- Compliance with national and international regulations
- Auditing and accreditation procedures
Implementation of these standards often occurs alongside ISO certifications (9000:2000 series, 17025) or specific national standards like the French NF S96-900 [91].
Resource-Constrained Protocol Optimization
A two-year study at a tertiary healthcare facility in North India demonstrated that optimized "dump freezing" (passive cooling) protocols coupled with rigorous quality assurance can achieve excellent outcomes despite resource limitations. Their approach included:
- Simplified cryopreservation protocol using DMSO, hydroxyethyl starch (HES), and human albumin in fixed ratios
- Double verification by two technical staff at each procedural step
- Comprehensive staff training with regular refresher courses and feedback mechanisms
- Routine quality control measuring post-thaw viability and sterility
This protocol yielded remarkable results: average post-thaw viability of 94.9% and 100% engraftment success across 78 thawed collections, while reducing cryopreservation costs by more than half (from $1250 to $550 per procedure) [92].
Utilization of Cryopreserved Hematopoietic Stem Cells
A 20-year retrospective analysis of hematopoietic stem cell transplantation practices revealed important insights for cryopreservation strategy optimization. The study found that only 1.6% of patients (26 of 1598) required additional HSC infusions (either stem cell boosts or second transplants), despite standard practice of storing excess cells. This suggests that implementing limited-duration storage policies (e.g., one year) for excess cells may represent a cost-effective strategy without compromising patient care, though the authors note this may change with emerging therapies like CAR-T treatments [92].
Detailed Experimental Protocols
Cryopreservation Protocol for hPSCs using CryoStor CS10
Workflow: hPSC Cryopreservation with CryoStor CS10
Materials:
- CryoStor CS10 (catalog #07930, STEMCELL Technologies)
- Gentle Cell Dissociation Reagent (catalog #07174, STEMCELL Technologies)
- mTeSR Plus culture medium (catalog #100-0276, STEMCELL Technologies)
- Cryogenic vials (e.g., Corning Cryogenic Vials with Orange Caps)
- 15 mL conical tubes
- 2 mL sterile pipette tips
- Isopropanol freezing container (e.g., Nalgene)
- -150°C freezer or liquid nitrogen vapor tank
Procedure:
- Pre-freezing Preparation: Identify and remove regions of differentiation by scraping with a pipette tip or aspiration. Work quickly to minimize time outside the incubator (under 15 minutes).
- Cell Dissociation: Aspirate remaining medium and add 1 mL Gentle Cell Dissociation Reagent per well of a 6-well plate. Incubate at room temperature for 5-8 minutes, monitoring dissociation microscopically.
- Cell Harvesting: Aspirate GCDR and add 1 mL mTeSR Plus. Gently detach colonies by scraping, preserving large cell aggregates. Transfer aggregates to a 15 mL conical tube.
- Centrifugation: Centrifuge at 300 × g for 5 minutes at room temperature. Gently aspirate supernatant while keeping the pellet intact.
- Cryomedium Addition: Add 1 mL cold CryoStor CS10 per well harvested to the pellet. Wipe the outside of the bottle with 70% ethanol before opening.
- Resuspension: Gently dislodge the pellet using a 2 mL serological pipette, minimizing break-up of cell aggregates.
- Aliquoting: Transfer cell suspension to cryopreservation vials using a 2 mL serological pipette.
- Freezing: Implement one of two cooling methods:
- Controlled-rate cooling: Reduce temperature at approximately -1°C/min, followed by long-term storage at -135°C or colder.
- Passive cooling: Hold at -20°C for 2 hours, then -80°C for 2 hours, followed by long-term storage at -135°C or colder.
- Record Keeping: Document vial identification, cell type, passage number, date, and freezing parameters [90].
Quality Assessment Protocol for Post-Thaw Analysis
Workflow: Post-Thaw Quality Assessment
Procedure:
- Thawing: Rapidly thaw cryovials in a 37°C water bath with gentle agitation until only a small ice crystal remains.
- Dilution: Transfer cell suspension to a 15 mL conical tube containing 10 mL pre-warmed culture medium dropwise with gentle mixing.
- Centrifugation: Centrifuge at 300 × g for 5 minutes. Aspirate supernatant carefully.
- Viability Assessment: Resuspend cell pellet in appropriate buffer for flow cytometry analysis. Use viability dyes (e.g., 7-AAD, propidium iodide) according to manufacturer protocols.
- Flow Cytometry Panel: Include markers specific to your cell type and application. For stem cells, consider surface markers (e.g., CD34 for HSCs, SSEA-4 for pluripotent stem cells) and functional assays.
- Sterility Testing: Aliquot a sample for sterility testing according to ISO 13408 standards [88] [92] [93].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Clinical-Standard Cryopreservation
| Reagent Category | Specific Products | Function & Application |
|---|---|---|
| cGMP Cryomedia | CryoStor CS10, NutriFreez D10 | Serum-free, defined formulations for consistent performance across cell types |
| Dissociation Reagents | Gentle Cell Dissociation Reagent, Trypsin-EDTA | Enable gentle cell harvesting while preserving viability and surface markers |
| Viability Assays | 7-AAD, Propidium Iodide, Trypan Blue | Assess membrane integrity and post-thaw recovery |
| Flow Cytometry Markers | CD34, CD45, CD3, CD19, SSEA-4 | Characterize cell populations and differentiate lineages |
| Quality Control Tools | Sterility test kits, Mycoplasma detection | Ensure sample purity and prevent contamination |
| Cryogenic Supplies | Controlled-rate freezer, Cryogenic vials | Maintain consistent cooling rates and secure storage |
Implementation in Flow Cytometry Research
Implementation of clinical standards in research cryopreservation requires particular attention to several factors critical for flow cytometry applications:
Impact on Surface Marker Detection
Cryopreservation can significantly affect antigen presentation and detection in flow cytometry. The optimized formulations of CryoStor CS10 and NutriFreez D10 demonstrate reduced impact on surface marker integrity compared to traditional serum-containing media. When establishing new protocols, researchers should:
- Validate antibody binding post-thaw for critical markers
- Include viability staining in all panels to exclude dead cells from analysis
- Compare fresh vs. frozen samples from the same source during protocol optimization
- Consider intracellular vs. surface markers as they may be differentially affected
Quality Control Integration
Regular quality control measures adapted from clinical practice should include:
- Routine viability assessment using flow-based methods (e.g., 7-AAD exclusion)
- Sterility testing according to ISO 13408 standards for aseptic processing [93]
- Documentation practices tracking passage number, freeze date, and performance metrics
- Regular equipment calibration including freezer temperature monitoring and validation
Adopting clinical standards for cryopreservation in flow cytometry research enhances experimental reproducibility, cell sample quality, and data reliability. The validated performance of commercial media like CryoStor CS10 and NutriFreez D10, combined with quality management principles from transplant centers, provides researchers with a robust framework for optimizing their cryopreservation protocols. Implementation of these practices is particularly valuable for multi-center studies, long-term projects, and research with potential translational applications, where sample consistency and viability are paramount to scientific validity.
Conclusion
Effective cryopreservation is a cornerstone of reliable flow cytometry, enabling robust, reproducible data from complex samples. By integrating optimized protocols that carefully manage freezing rates and cryoprotectant choice, researchers can successfully preserve cell viability, phenotype, and function over the long term. The adoption of standardized practices, coupled with rigorous validation using both traditional and advanced computational analysis methods, is crucial for minimizing technical variability. Future directions will focus on the development of fully defined, serum-free freezing media, the refinement of automated analysis pipelines to objectively assess cryopreservation effects, and the establishment of universal guidelines to ensure consistency across research and clinical applications, thereby strengthening the translational potential of cell-based studies.
References
- 1. The effects of cryopreservation on PBMCs transcriptome ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1690316/full]
- 2. Flow Cytometric Immunophenotyping: Minimal Differences in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11505181/]
- 3. Toward Optimal Cryopreservation and Storage for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5180082/]
- 4. Standardization and performance evaluation of mononuclear ... [https://bmcimmunol.biomedcentral.com/articles/10.1186/1471-2172-7-29]
- 5. Viable Cryopreservation Strategy for Extending the Timeframe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109437/]
- 6. The Effect of Cryopreservation on Tâ€Cell Subsets by Flow ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11821723/]
- 7. Optimizing and standardizing the cryopreservation of ... [https://www.insights.bio/cell-and-gene-therapy-insights/webinars/336/Optimizing-and-standardizing-the-cryopreservation-of-cellular-samples-new-data-a]
- 8. AI and Flow Cytometry Workshop [https://www.nist.gov/news-events/events/2025/06/ai-and-flow-cytometry-workshop]
- 9. Protocols and Best Practices for Freezing Cells [https://www.stemcell.com/cryopreservation-basics-protocols-and-best-practices-for-freezing-cells]
- 10. Ice Inhibition for Cryopreservation: Materials, Strategies, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7967093/]
- 11. Protecting Cell Viability During Cryopreservation [https://www.azenta.com/learning-center/blog/considerations-protecting-cell-viability-during-cryopreservation]
- 12. The Impact of Varying Cooling and Thawing Rates on ... [https://www.nature.com/articles/s41598-019-39957-x]
- 13. Cryopreservation: An Overview of Principles and Cell- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7995302/]
- 14. Comprehensive evaluation of the effects of long-term ... [https://bmcimmunol.biomedcentral.com/articles/10.1186/s12865-022-00505-4]
- 15. Impact of Cryopreservation on Viability, Phenotype, and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.765667/full]
- 16. PBMC Isolation and Cryopreservation Protocol [https://anilocus.com/pbmc-isolation-and-cryopreservation-protocol/?srsltid=AfmBOooyA9KlpsYrKdwRTd62KdDwFOwZeJqD9802MAHpiw5guF_r8ZxL]
- 17. Cryopreservation as a Key Element in the Successful ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2020.592242/full]
- 18. Umbilical cord tissue–derived mesenchymal stromal cells ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324916305874]
- 19. Distinct Dominant Lineage from In Vitro Expanded Adipose ... [https://www.mdpi.com/2073-4409/11/7/1236]
- 20. Identification and validation of multiple cell surface markers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4982273/]
- 21. Technical pitfalls when collecting, cryopreserving, thawing ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1382192/full]
- 22. RB705 Rat Anti-Mouse CD274 (PD-L1) [https://www.bdbiosciences.com/en-tw/products/reagents/flow-cytometry-reagents/research-reagents/single-color-antibodies-ruo/RB705-Rat-Anti-Mouse-CD274-(PD-L1).758168]
- 23. a multi-platform comparative study | Scientific Reports [https://www.nature.com/articles/s41598-025-14865-5]
- 24. Evaluation of the viability and functionality of human ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1627973/full]
- 25. The effects of cryopreservation on PBMCs transcriptome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575299/]
- 26. The effects of cryopreservation on PBMCs transcriptome ... [https://pubmed.ncbi.nlm.nih.gov/41181136/]
- 27. Optimization of the Blocking and Signal Preservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462741/]
- 28. Evaluation of the viability and functionality of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12355051/]
- 29. Standardized Serum - Free Cryomedia Maintain Peripheral Blood... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3178417/]
- 30. Impact of lower concentrations of dimethyl sulfoxide on ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924000537]
- 31. Comparison of the Effects of Different Cryoprotectants on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4685149/]
- 32. Optimization of Human Peripheral Blood Mononuclear ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3920500/]
- 33. Strategies in developing dimethyl sulfoxide (DMSO) [https://pmc.ncbi.nlm.nih.gov/articles/PMC9579275/]
- 34. Impact of serum ‑ free on the expansion and functionality of... media [https://www.spandidos-publications.com/10.3892/ijmm.2023.5261]
- 35. Cryopreserved PBMC Considerations | Immune System ... [https://sanguinebio.com/blog/cryopreserved-pbmc-considerations/?srsltid=AfmBOopoFFMvowjERaJvXruh9T8wBUGrRsmRFUa7n13sKgT88sZUHpav]
- 36. Why Separate Peripheral Blood Mononuclear Cells [https://www.akadeum.com/blog/pbmc-isolation-methods-isolation-white-blood-cells/?srsltid=AfmBOooeM5HjmdQBT6oxQjiKzZpY6V_xql7buIXKvuNaZ2Xybpk1Vm3v]
- 37. Human PBMC Isolation, Freezing, Thawing, Sourcing, and ... [https://www.stemcell.com/pbmc]
- 38. Protocol for Isolating Mononuclear Cells from Whole Blood [https://www.stemcell.com/isolating-mononuclear-cells-from-whole-blood-by-density-gradient-centrifugation.html]
- 39. Recommended Standard Method for Isolating ... [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/clinical-testing-and-diagnostics-manufacturing/hematology/recommended-standard-method?srsltid=AfmBOoo2HNSy81-ukZqDrUeJdr8GLbIQ15CY3SlagrMLN3AdgVSNpD22]
- 40. Protocol for Cryopreserving PBMCs [https://www.stemcell.com/how-to-cryopreserve-pbmcs.html]
- 41. Optimizing PBMC Viability and Recovery: Updated Best ... [https://cgt.global/pbmc-viability-and-recovery/]
- 42. Cryopreservation protocol | Abcam [https://www.abcam.com/en-us/technical-resources/protocols/cryopreservation-of-mammalian-cell-lines]
- 43. PBMC Storage - Cryopreservation & Controlled-Rate ... [https://researchdonors.co.uk/2025/02/18/the-importance-of-cryopreservation-solutions-and-controlled-rate-freezing-in-pbmc-storage/]
- 44. Storage and Preservation | Cryogenic | Corning CoolCell [https://www.corning.com/emea/en/products/life-sciences/products/general-labware/cryogenic-storage.html]
- 45. Optimizing PBMC Cryopreservation and Utilization for ... [https://www.mdpi.com/2076-393X/13/7/765]
- 46. Refrigerate, Freeze, or Fix Cells for Flow Cytometry ... [https://www.stemcell.com/fridge-freeze-or-fix-cells.html]
- 47. Innovations in Platelet Cryopreservation: Evaluation of DMSO ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563202/]
- 48. Flow Cytometry Sample Preparation: Best Practices [https://kcasbio.com/blogs/sample-preparation-for-flow-cytometry-best-practices/]
- 49. Quantitative assessment of the impact of cryopreservation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7734731/]
- 50. A 3-step method for preparing cryopreserved samples of ... [https://pubmed.ncbi.nlm.nih.gov/38606842/]
- 51. Rapid post-thaw isolation of red blood cells from ... [https://www.sciencedirect.com/science/article/pii/S0011224025001014]
- 52. Isolation, freezing, and thawing of splenocytes [https://www.mabtech.com/knowledge-hub/isolation-freezing-and-thawing-splenocytes]
- 53. Mouse Spleen Cell Isolation Protocol [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/immunology-at-work/immunology-protocols/mouse-spleen-cell-isolation-protocol.html]
- 54. Processing, Cryopreserving, and Controlling the Quality of HSC [https://www.ncbi.nlm.nih.gov/books/NBK608252/]
- 55. Flow Cytometric Characterization of Hematopoietic Stem ... [https://pubmed.ncbi.nlm.nih.gov/37899990/]
- 56. Use of different DMSO concentrations for cryopreservation ... [https://pubmed.ncbi.nlm.nih.gov/19878061/]
- 57. Effects, methods and limits of the cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-024-03954-3]
- 58. A comparison of cryopreservation methods: Slow-cooling vs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3196719/]
- 59. Effects of cell concentration, time of fresh storage, and ... [https://www.sciencedirect.com/science/article/abs/pii/S1473050221002986]
- 60. CONSISTENTLY ACHIEVING > 90% VIABILITY OF ... [https://www.sciencedirect.com/science/article/abs/pii/S1465324924003086]
- 61. Phenotypic and functional comparisons between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576105/]
- 62. Cryopreservation does not change the performance and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9663191/]
- 63. Simplified mass cytometry protocol for in-plate staining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9092992/]
- 64. Data analysis in flow cytometry [https://www.abcam.com/en-us/technical-resources/guides/flow-cytometry-guide/data-analysis-in-flow-cytometry]
- 65. Flow Cytometry Application Notes [https://www.thermofisher.com/ng/en/home/life-science/cell-analysis/flow-cytometry/flow-cytometry-learning-center/flow-cytometry-resource-library/flow-cytometry-application-notes.html]
- 66. A Beginner's Guide To Analyzing and Visualizing Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5765874/]
- 67. Study of a new device for washing and concentrating ... [https://www.sciencedirect.com/science/article/pii/S1465324921007465]
- 68. Improvement of cellular pattern organization and clarity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11823422/]
- 69. Assessment and Comparison of Viability Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10872314/]
- 70. BestProtocols: Viability Staining Protocol for Flow Cytometry [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/viability-staining-flow-cytometry.html]
- 71. Cell apoptosis assay by dual AO/EB staining and flow ... [https://bio-protocol.org/exchange/minidetail?id=3643840&type=30]
- 72. Selected novel 5'-amino-2'-hydroxy-1, 3-diaryl-2-propen- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4849104/]
- 73. Flow Cytometry Using the 7-AAD Cell Viability Staining [https://bio-protocol.org/exchange/minidetail?id=10503487&type=30]
- 74. A new method for detecting mycoplasma in cell cultures ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270630/]
- 75. Impacts of cryopreservation on phenotype and functionalit... [https://www.degruyterbrill.com/document/doi/10.2478/jtim-2023-0136/html?lang=en&srsltid=AfmBOoqPxzwQtEZEJes6V8GlSDCj-b8R5Ec49YFc3xVUFI7rQWEJKerS]
- 76. CryoSCAPE: Scalable immune profiling using cryopreserved ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-06010-z]
- 77. Immune Monitoring and Flow Cytometry - Sample ... [https://cinj.org/research/immune-monitoring-and-flow-cytometry-sample-preparation]
- 78. Quantitative assessment of the impact of cryopreservation on ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-020-02054-2]
- 79. Improved Post-Thaw Function and Epigenetic Changes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5466057/]
- 80. Wound healing assay [https://www.abcam.com/en-us/technical-resources/protocols/wound-healing-assay]
- 81. An introduction to the wound healing assay using live-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5154238/]
- 82. A robust pipeline for high-content, high-throughput ... [https://www.sciencedirect.com/science/article/pii/S2667237523002837]
- 83. manual gating, unsupervised clustering, and auto-gating - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11630031/]
- 84. The Effect of Cryopreservation on T-Cell Subsets by Flow ... [https://pubmed.ncbi.nlm.nih.gov/39749863/]
- 85. Critical assessment of automated flow cytometry data ... [https://www.nature.com/articles/nmeth.2365]
- 86. Multidimensional data analysis algorithms facilitate and ... [https://www.sciencedirect.com/science/article/pii/S0093691X25001190]
- 87. Beyond the Limits: How Is Spectral Flow Cytometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248732/]
- 88. NutriFreez® D10 Cryopreservation Medium [https://shop.sartorius.com/us/p/nutrifreez-d10-cryopreservation-medium/NutriFreez_D10_Cryopreservation_Medium]
- 89. 01-0020 - NutriFreezâ„¢ D10 Cryopreservation Medium [https://www.reprocell.com/product-catalog/cryopreservation-media/nutrifreez-d10-cryopreservation-medium]
- 90. Protocol for Cryopreserving hPSCs with CryoStor® CS10 [https://www.stemcell.com/how-to-cryopreserve-human-pluripotent-stem-cells.html]
- 91. Implementing Best Practices and Validation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3353557/]
- 92. The 51st Annual Meeting of the European Society for Blood ... [https://www.nature.com/articles/s41409-025-02659-2]
- 93. Sartorius NutriFreez D10 Cryopreservation Medium, PRF [https://store.reprocell.com/cryopreservation-media-c7/nutrifreez-d10-cryopreservation-medium-phenol-red-free-p513]