Precision at the Limit: A Strategic Guide to Method Validation for Low-Concentration Analytes
This article provides a comprehensive framework for validating the precision of analytical methods at low concentration levels, a critical challenge for researchers and drug development professionals.
Precision at the Limit: A Strategic Guide to Method Validation for Low-Concentration Analytes
Abstract
This article provides a comprehensive framework for validating the precision of analytical methods at low concentration levels, a critical challenge for researchers and drug development professionals. Aligned with modern ICH Q2(R2) and FDA guidelines, the content explores foundational principles, methodological applications for HPLC and immunoassays, troubleshooting strategies for common pitfalls, and a complete validation protocol. By synthesizing regulatory standards with practical case studies, this guide empowers scientists to generate reliable, high-quality data for pharmacokinetic studies, biomarker quantification, and impurity profiling, ensuring both regulatory compliance and scientific rigor.
The Critical Challenge: Understanding Precision and Accuracy at Low Concentrations
In the field of analytical method validation, precision is a fundamental parameter that confirms the reliability and consistency of measurement results. For researchers, scientists, and drug development professionals working with low concentration levels, a nuanced understanding of precision is not merely beneficial—it is critical for generating defensible data. Precision is quantitatively expressed as the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions [1] [2]. It is typically measured as a standard deviation, variance, or coefficient of variation (relative standard deviation) [3].
This parameter is systematically evaluated under three distinct tiers of conditions, each providing a different level of stringency and accounting for different sources of variability: Repeatability, Intermediate Precision, and Reproducibility [4] [3].
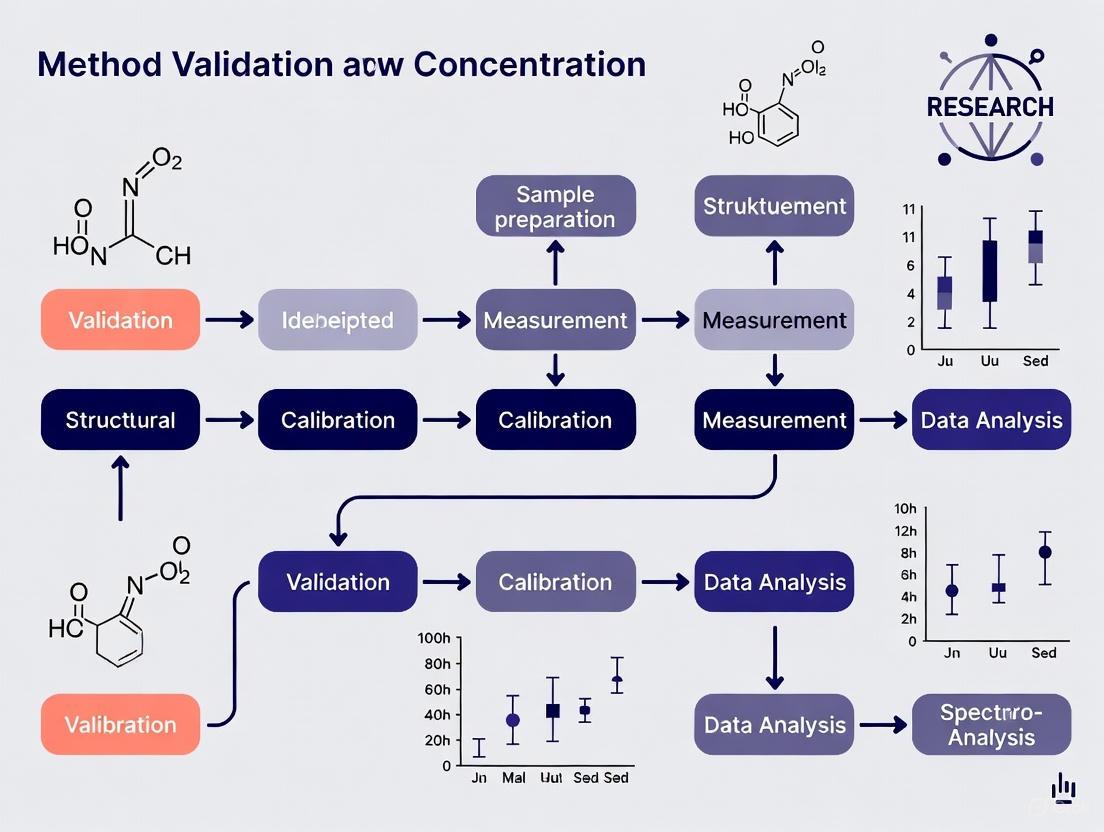
The logical relationship between these three tiers of precision can be visualized as a hierarchy of increasing variability and scope.
Detailed Definitions and Comparison
The following table provides a structured comparison of the three precision parameters, detailing the conditions and scope of each.
| Precision Parameter | Conditions | Scope of Variability Assessed | Typical Standard Deviation |
|---|---|---|---|
| Repeatability [4] [3] | Same procedure, operators, measuring system, operating conditions, location, and short period of time (e.g., one day or one analytical run). | The smallest possible variation; accounts for random noise under ideal, identical conditions. | Smallest |
| Intermediate Precision [4] [2] | Same laboratory and procedure over an extended period (e.g., several months) with deliberate changes such as different analysts, different equipment, different calibrants, different batches of reagents, and different columns. | Within-laboratory variability; accounts for random effects from factors that are constant within a day but change over time. | Larger than repeatability |
| Reproducibility [4] [2] [3] | Different laboratories, different operators, different measuring systems (possibly using different procedures), and an extended period of time. | Between-laboratory variability; provides the most realistic estimate of method performance in a multi-laboratory setting. | Largest |
Experimental Protocols for Determining Precision
For a method to be considered precise, its precision must be validated through controlled experiments. The protocols below outline the standard methodologies for assessing each tier of precision, with particular attention to the challenges of low-concentration analysis.
Protocol for Assessing Repeatability
Repeatability, or intra-assay precision, represents the best-case scenario for a method's performance and is expected to show the smallest possible variation [4] [3].
- Experimental Design: Analyze a minimum of nine determinations covering the specified range of the procedure. This is typically executed as three concentrations (low, mid, and high), each analyzed in triplicate, all within a single analytical run or day [2] [5].
- Sample Requirements: The sample must be homogeneous. For drug product assays, this involves multiple samplings from a single, well-mixed batch.
- Data Analysis: Calculate the mean, standard deviation, and relative standard deviation (%RSD) for the results at each concentration level. The %RSD is the primary metric for repeatability [2] [5].
- Low-Concentration Considerations: At the low end of the range, such as near the Limit of Quantitation (LOQ), the acceptance criteria for %RSD may be justifiably widened. A signal-to-noise (S/N) ratio of 10:1 is often used to define the LOQ, and the precision at this level should still be acceptable [2] [5].
Protocol for Assessing Intermediate Precision
Intermediate precision quantifies the "within-lab reproducibility" and is crucial for understanding the long-term robustness of a method in a single laboratory [4] [2].
- Experimental Design: Use an experimental design that incorporates the expected sources of laboratory variability. A common approach is to have two different analysts prepare and analyze replicate sample preparations over multiple days or weeks. Each analyst should use their own standards, solutions, and, if possible, different HPLC systems or key instruments [2].
- Variables Tested: The study should deliberately vary factors like the analyst, the instrument, the day, and batches of critical reagents [4].
- Data Analysis: The results are typically reported as %RSD, which now encompasses the variability from all the introduced factors. Some protocols also compare the mean values obtained by the two analysts using a statistical test (e.g., Student's t-test) to check for a significant difference [2].
Protocol for Assessing Reproducibility
Reproducibility is assessed through inter-laboratory collaborative studies and is generally required for method standardization or when a method will be used across multiple sites [4] [2].
- Experimental Design: A group of laboratories (e.g., 5-10) follows the same written analytical procedure. Each laboratory analyzes the same homogeneous test samples using its own analysts, equipment, and reagents.
- Sample and Standard Preparation: Each participating laboratory prepares its own standards and solutions independently.
- Data Analysis: The combined data from all laboratories is analyzed to determine the overall standard deviation, %RSD, and confidence intervals. The results provide a measure of the method's performance in a "real-world" multi-laboratory environment [2].
Experimental Data and Acceptance Criteria
Precision acceptance criteria are often concentration-dependent, which is especially critical for low-concentration studies. The following table summarizes typical data and criteria based on regulatory guidance and industry practices.
| Precision Level | Concentration Level | Typical Experimental Output | Common Acceptance Criteria (Chromatographic Assays) |
|---|---|---|---|
| Repeatability (n=6-9) [2] [5] | High (e.g., 100% of test concentration) | %RSD of multiple measurements | %RSD ≤ 1.0 - 2.0% |
| Low (e.g., near LOQ) | %RSD of multiple measurements | %RSD ≤ 5.0 - 20.0% [5] | |
| Intermediate Precision (Multi-day, multi-analyst) [2] | Overall (across all data) | Combined %RSD from all valid experiments | Overall %RSD ≤ 2.0 - 2.5% |
| Comparison of Means | Statistical test (e.g., t-test) p-value | p-value > 0.05 (no significant difference) | |
| Reproducibility (Multi-laboratory) [2] | Overall | Reproducibility Standard Deviation and %RSD | Criteria set by the collaborative study, generally wider than intermediate precision. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and instruments are fundamental for conducting precision studies, particularly in a chromatographic context for pharmaceutical analysis.
| Tool / Reagent | Critical Function in Precision Assessment |
|---|---|
| High-Performance Liquid Chromatography (HPLC/UHPLC) System [6] [7] | The primary instrument for separation, identification, and quantification of analytes. System suitability tests are run to ensure precision before a validation study. |
| Certified Reference Material (CRM) [3] | Provides an "accepted reference value" with established purity, essential for preparing known concentration samples to test accuracy and precision. |
| Chromatography Column [4] [2] | The stationary phase for separation. Using columns from different batches is a key variable in intermediate precision testing. |
| Mass Spectrometry (MS) Detector (e.g., LC-MS/MS) [2] [6] [7] | Provides superior specificity and sensitivity, crucial for confirming peak purity and accurately quantifying analytes at low concentrations. |
| Photodiode Array (PDA) Detector [2] | Used for peak purity assessment by comparing spectra across a peak, helping to demonstrate method specificity—a prerequisite for a precise assay. |
| High-Purity Solvents and Mobile Phase Additives | Consistent quality is vital for robust chromatographic performance and low background noise, directly impacting precision, especially at low concentrations. |
| CREBBP-IN-9 | CREBBP-IN-9, MF:C16H15N5O2S, MW:341.4 g/mol |
| Ivacaftor-d9 | Deutivacaftor (VX-561) |
A rigorous, tiered approach to precision—encompassing repeatability, intermediate precision, and reproducibility—is non-negotiable for building confidence in an analytical method. For researchers focused on low concentration levels, understanding the specific conditions and acceptance criteria for each parameter is paramount. A method that demonstrates tight repeatability but fails during intermediate precision testing is not robust and poses a significant risk to data integrity and regulatory submissions. Therefore, a well-designed validation strategy must proactively account for all expected sources of variability within the method's intended use environment, ensuring the generation of reliable and high-quality data throughout the drug development lifecycle.
In the field of analytical chemistry and bioanalysis, the reliable detection and quantification of substances at low concentrations is paramount for method validation, particularly in pharmaceutical development, clinical diagnostics, and environmental monitoring. The limit of detection (LOD) and limit of quantitation (LOQ) are two fundamental parameters that characterize the sensitivity and utility of an analytical procedure at its lower performance limits [8] [9]. These concepts are complemented by the quantification range (also known as the analytical measurement range), which defines the interval over which the method provides results with acceptable accuracy and precision [10].
Understanding the distinctions and relationships between these parameters is essential for researchers and scientists who develop, validate, and implement analytical methods. Proper characterization ensures that methods are "fit for purpose," providing reliable data that supports critical decisions in drug development, patient care, and regulatory submissions [8] [11]. This guide examines the regulatory definitions, calculation methodologies, and practical implications of LOD, LOQ, and the quantification range within the broader context of method validation for precision at low concentration levels.
Defining the Fundamental Parameters
Conceptual Definitions and Distinctions
The following table summarizes the core definitions and purposes of each key parameter:
| Parameter | Definition | Primary Purpose | Key Characteristics |
|---|---|---|---|
| Limit of Blank (LOB) | The highest apparent analyte concentration expected when replicates of a blank sample (containing no analyte) are tested [8]. | Distinguishes the signal produced by a blank sample from that containing a very low analyte concentration [8]. | - Estimates the background noise of the method- Calculated as: Mean~blank~ + 1.645(SD~blank~) [8] |
| Limit of Detection (LOD) | The lowest analyte concentration likely to be reliably distinguished from the LOB and at which detection is feasible [8]. | Confirms the presence of an analyte, but not necessarily its exact amount [9]. | - Greater than LOB [8]- Distinguishes presence from absence- Typically has a higher uncertainty than LOQ [9] |
| Limit of Quantitation (LOQ) | The lowest concentration at which the analyte can be reliably detected and quantified with acceptable precision and accuracy [8] [10]. | Provides precise and accurate quantitative measurements at low concentrations [9]. | - Cannot be lower than the LOD [8]- Predefined goals for bias and imprecision must be met [8]- Sometimes called the Lower Limit of Quantification (LLOQ) [10] |
| Quantification Range | The interval between the LOQ and the Upper Limit of Quantification (ULOQ) within which the analytical method demonstrates acceptable linearity, accuracy, and precision [10]. | Defines the working range of the method for producing reliable quantitative results. | - LOQ is the lower boundary [10]- Samples with concentrations >ULOQ require dilution [10]- Samples with concentrations |
Regulatory Context and Importance
Regulatory guidelines such as the International Conference on Harmonisation (ICH) Q2(R1) and various Clinical and Laboratory Standards Institute (CLSI) documents provide frameworks for determining these parameters [8] [11]. Proper establishment of LOD and LOQ is crucial for methods used in detecting impurities, degradation products, and in supporting pharmacokinetic studies where low analyte concentrations are expected [12] [10]. For potency assays, however, LOD and LOQ are generally not required, as these typically operate at much higher concentration levels [11].
The relationship between LOB, LOD, and LOQ can be visualized through their statistical definitions and their position on the concentration scale, as shown in the following conceptual diagram:
Methodologies for Determining LOD and LOQ
Various methodologies exist for determining LOD and LOQ, each with specific applications depending on the nature of the analytical method, the presence of background noise, and regulatory requirements [11]. The ICH Q2(R1) guideline suggests several acceptable approaches [11] [13]:
- Visual Evaluation: Direct assessment by analyzing samples with known concentrations and establishing the minimum level at which the analyte can be reliably detected or quantified [12] [11].
- Signal-to-Noise Ratio (S/N): Applicable to methods with a measurable baseline noise (e.g., chromatographic methods) [12] [11].
- Standard Deviation of the Blank and Slope of the Calibration Curve: A statistical approach utilizing the variability of the blank response and the sensitivity of the analytical method [12] [13].
Detailed Calculation Methods
Signal-to-Noise Ratio Approach
This approach is commonly used in chromatographic methods (HPLC, GC) where instrumental background noise is measurable [12] [11].
- LOD: Generally accepted signal-to-noise ratio of 2:1 or 3:1 [12] [9].
- LOQ: Generally accepted signal-to-noise ratio of 10:1 [12] [10].
The signal-to-noise ratio is calculated by comparing measured signals from samples containing low concentrations of analyte against the signal of a blank sample [12]. The LOD and LOQ are the concentrations that yield the stipulated S/N ratios.
Standard Deviation and Slope of the Calibration Curve
This is a widely used statistical method, defined in ICH Q2(R1), that can be applied to instrumental techniques [13] [14]. The formulas are:
Where:
- σ = the standard deviation of the response
- S = the slope of the calibration curve
The standard deviation (σ) can be estimated in different ways, leading to subtle variations in the method [13]:
- Standard deviation of the blank: Measuring replicates of a blank sample and calculating the standard deviation of the obtained responses [12].
- Standard error of the regression (residual standard deviation): The standard deviation of the y-residuals of the calibration curve, often considered the simplest and most practical approach as it is readily obtained from regression analysis [13] [14].
- Standard deviation of the y-intercept: Using the standard deviation of the y-intercept of regression lines [12].
The EP17 Protocol: LOB, LOD, and LOQ
The Clinical and Laboratory Standards Institute (CLSI) EP17 protocol provides a rigorous statistical framework, particularly relevant in clinical biochemistry [8]. This method explicitly incorporates the Limit of Blank (LOB) and uses distinct formulas:
- LOB = mean~blank~ + 1.645(SD~blank~) (assuming a Gaussian distribution) [8]
- LOD = LOB + 1.645(SD~low concentration sample~) [8]
The LOQ in this protocol is determined as the lowest concentration at which predefined goals for bias and imprecision (total error) are met, and it cannot be lower than the LOD [8]. A recommended number of replicates (e.g., 60 for establishment by a manufacturer, 20 for verification by a laboratory) is specified to ensure reliability [8].
Comparison of LOD/LOQ Determination Methods
The table below compares the performance of different methodological approaches as evidenced in recent scientific studies:
| Methodological Approach | Reported Performance Characteristics | Best-Suited Applications |
|---|---|---|
| Classical Strategy (Based on statistical concepts like SD/Slope or S/N) | Can provide underestimated values of LOD and LOQ; may lack the rigor of graphical tools [15]. | Initial estimates; methods where high precision at the very lowest limits is not critical. |
| Accuracy Profile (Graphical tool based on tolerance intervals) | Provides a relevant and realistic assessment of LOD and LOQ by considering the total error (bias + precision) over a concentration range [15]. | Bioanalytical method validation where a visual and integrated assessment of method validity is required. |
| Uncertainty Profile (Graphical tool based on β-content tolerance intervals and measurement uncertainty) | Considered a reliable alternative; provides precise estimate of measurement uncertainty. Values for LOD/LOQ are in the same order of magnitude as the Accuracy Profile [15]. | High-stakes validation requiring precise uncertainty quantification; decision-making on method validity based on inclusion within acceptability limits. |
A 2025 comparative study of these approaches for an HPLC method analyzing sotalol in plasma concluded that the graphical strategies (uncertainty and accuracy profiles) provide a more relevant and realistic assessment compared to the classical statistical strategy, which tended to underestimate the values [15].
Experimental Protocols and Validation
Standard Protocol for LOD/LOQ Determination via Calibration Curve
This protocol outlines the steps to determine LOD and LOQ using the standard deviation of the response and the slope of the calibration curve, in accordance with ICH Q2(R1) [13] [14].
Step 1: Prepare Calibration Standards Prepare a series of standard solutions at concentrations expected to be in the range of the LOD and LOQ. It is crucial that the calibration curve is constructed using samples within this range and not by extrapolation from higher concentrations [11] [13].
Step 2: Analyze Standards and Plot Calibration Curve Analyze the standards using the analytical method (e.g., HPLC, GC). Plot a standard curve with the analyte concentration on the X-axis and the instrumental response (e.g., peak area, absorbance) on the Y-axis [14].
Step 3: Perform Regression Analysis Use statistical software (e.g., Microsoft Excel's Data Analysis Toolpak) to perform a linear regression on the calibration data [14]. The key outputs required are:
- Slope (S) of the calibration curve.
- Standard Error (SE) or Residual Standard Deviation, which is used as the estimate for the standard deviation of the response (σ) [13] [14].
Step 4: Calculate LOD and LOQ Apply the regression outputs to the standard formulas:
Step 5: Experimental Verification The calculated LOD and LOQ values are estimates and must be experimentally confirmed [8] [13]. This involves:
- Preparing and analyzing a suitable number of replicates (e.g., n=5-6) at the calculated LOD and LOQ concentrations.
- For LOD: The analyte should be detected in the majority of these replicates, confirming reliable detection.
- For LOQ: The measurements must demonstrate acceptable precision and accuracy (e.g., ±20% CV and bias for bioanalytical methods at the LOQ level) [10]. If the results do not meet the predefined criteria, the LOQ must be re-estimated at a slightly higher concentration [8].
Essential Research Reagent Solutions
The following materials are critical for experiments aimed at determining LOD and LOQ, particularly in a bioanalytical context:
| Material / Solution | Function in LOD/LOQ Experiments |
|---|---|
| Blank Matrix (e.g., drug-free plasma, buffer) | Serves as the analyte-free sample for determining the baseline response, LOB, and for preparing calibration standards [8] [10]. |
| Primary Analyte Standard (High Purity) | Used to prepare accurate stock and working solutions for spiking into the blank matrix to create calibration curves [10]. |
| Internal Standard (e.g., stable isotope-labeled analog) | Added equally to all samples and standards to correct for variations in sample preparation and instrument response, improving precision [15]. |
| Calibration Standards (Series in blank matrix) | A sequence of samples with known concentrations, typically in the low range of interest, used to construct the calibration curve and calculate the slope (S) [10] [13]. |
| Quality Control (QC) Samples (at LOD/LOQ levels) | Independent samples used to verify that the calculated LOD and LOQ meet the required performance characteristics for detection, precision, and accuracy [8] [10]. |
The Quantification Range in Method Validation
Defining the Upper and Lower Limits
The quantification range, or analytical measurement range, is bounded by the Lower Limit of Quantification (LLOQ) and the Upper Limit of Quantification (ULOQ) [10]. While this guide focuses on precision at low levels, a complete method validation must also establish the ULOQ.
- LLOQ: As defined previously, it is the lowest concentration on the calibration curve that can be quantified with acceptable precision and accuracy (e.g., CV and bias ≤20%) and an analyte response typically at least 5 times that of a blank [10].
- ULOQ: The highest calibration standard where the analyte response is reproducible, and the precision and accuracy are within acceptable limits (e.g., ≤15% for bioanalytical methods) [10].
A critical rule in bioanalysis is that the calibration curve should not be extrapolated below the LLOQ or above the ULOQ. Samples with concentrations exceeding the ULOQ must be diluted, while those below the LLOQ are reported as such [10].
Establishing the Working Range
The process of establishing the full quantification range involves analyzing calibration standards across a wide concentration span and verifying the performance with QC samples at the low, middle, and high ends of the range. The "accuracy profile" is a modern graphical tool that combines bias and precision data to visually define the valid quantification range as the interval where the total error remains within pre-defined acceptability limits [15] [10].
The following diagram illustrates the logical workflow for establishing and validating the complete quantification range of an analytical method:
The precise determination of the Limit of Detection (LOD), Limit of Quantitation (LOQ), and the Quantification Range is a critical component of analytical method validation, especially for methods requiring precision at low concentration levels. While classical approaches based on signal-to-noise or standard deviation and slope provide a foundation, newer graphical tools like the uncertainty and accuracy profiles offer more realistic and integrated assessments by incorporating total error and tolerance intervals [15].
Researchers and drug development professionals must select the appropriate methodology based on the intended use of the method, regulatory requirements, and the necessary level of confidence. Ultimately, a well-validated method, with clearly defined and experimentally verified LOD, LOQ, and quantification range, is essential for generating reliable, high-quality data that supports scientific research and regulatory decision-making.
The Impact of Imprecision on Data Integrity in Pharmacokinetics and Biomarker Studies
In the rigorous world of drug development, data integrity serves as the foundational pillar for reliable scientific decision-making. Regulatory authorities like the US Food and Drug Administration (FDA) define data integrity as encompassing the accuracy, completeness, and reliability of data, which must be attributable, legible, contemporaneous, original, and accurate (ALCOA) throughout its lifecycle [16]. Within this framework, imprecision—the inherent variability in analytical measurements—poses a persistent challenge to data quality. In pharmacokinetic (PK) and biomarker studies, where critical decisions about drug safety and efficacy hinge on precise quantitative data, uncontrolled imprecision can compromise study outcomes, leading to incorrect dosage recommendations, misguided efficacy conclusions, and ultimately, threats to patient safety.
The regulatory landscape is increasingly focused on these issues. Recent FDA draft guidance emphasizes that data integrity concerns can significantly impact "application acceptance for filing, assessment, regulatory actions, and approval as well as post-approval actions" [16]. This guide systematically compares how imprecision manifests and impacts data integrity across pharmacokinetic and biomarker studies, providing researchers with experimental approaches for its quantification and control.
Quantifying Imprecision: Analytical Perspectives
Key Validation Parameters for Assessing Imprecision
Analytical method validation provides the primary defense against imprecision. According to established guidelines, six key criteria ensure methods are "fit-for-purpose," encapsulated by the mnemonic Silly - Analysts - Produce - Simply - Lame - Results, which corresponds to Specificity, Accuracy, Precision, Sensitivity, Linearity, and Robustness [1]. Among these, precision (the closeness of agreement between multiple measurements) directly quantifies random error, while accuracy (closeness to the true value) detects systematic error. Robustness measures the method's capacity to remain unaffected by small variations in parameters, acting as a proxy for its susceptibility to imprecision under normal operational variations [1].
The Concept of Experimental Resolution
A crucial but often overlooked metric is experimental resolution, defined as the minimum concentration gradient an assay can reliably detect within a specific range [17]. Unlike the Limit of Detection (LoD), which only identifies the lowest detectable concentration, experimental resolution specifies the minimum change in concentration that can be measured, making it a more dynamic indicator of an assay's discriminatory power. Research has demonstrated significant variations in experimental resolution across common laboratory methods:
- Biochemical tests and automatic hematology analyzers: Typically achieve a resolution of 10% (with some reaching 1%) [17].
- Classical chemical assays (e.g., gas chromatography): Can achieve a resolution as low as 1% [17].
- Immunoassays (manual ELISA): Show a surprisingly lower resolution of only 25% [17].
- qPCR assays: Demonstrate a resolution of 10% [17].
This variation highlights that assays traditionally considered "sensitive" may lack the resolution needed for fine discrimination between closely spaced concentrations, a critical factor in PK and biomarker analysis.
Comparative Analysis: PK vs. Biomarker Studies
The impact and implications of imprecision differ notably between pharmacokinetic and biomarker studies, as detailed in the table below.
Table 1: Comparative Impact of Imprecision in PK and Biomarker Studies
| Aspect | Pharmacokinetic (PK) Studies | Biomarker Studies |
|---|---|---|
| Primary Focus | Drug concentration (Absorption, Distribution, Metabolism, Excretion) [18] | Biological response indicators (e.g., PD-L1, TMB) [19] |
| Consequence of Imprecision | Incorrect half-life, clearance, and bioavailability estimates; flawed dosing regimens [20] | Misclassification of patient responders; incorrect predictive accuracy [19] [21] |
| Typical Analytical Techniques | LC-MS/MS, HPLC-UV, ELISA [18] [20] | Immunohistochemistry, sequencing, gene expression profiling, immunoassays [19] |
| Data Integrity Risk | Undermines bioequivalence and safety assessments; regulatory rejection [22] [16] | Compromised patient stratification; failed personalized medicine approaches [19] |
| Empirical Evidence | Formulation analysis methods require rigorous validation of precision for GLP compliance [20] | Combined biomarkers show superior predictive power (AUC: 0.75) over single biomarkers (AUC: 0.64-0.68) [19] |
Case Study: Imprecision in Biomarker Combinations
The superior performance of combined biomarkers underscores the additive effect of imprecision. A 2024 comparative study on NSCLC (Non-Small Cell Lung Cancer) demonstrated that while single biomarkers like PD-L1 IHC and tTMB had Area Under the Curve (AUC) values of 0.64 in predicting response to immunotherapy, a combination of biomarkers achieved a significantly higher AUC of 0.75 [19]. This enhancement results from the combination mitigating the individual imprecision of each standalone biomarker, leading to improved specificity, positive likelihood ratio, and positive predictive value [19].
Case Study: Imprecision in Exposure Biomarkers
A seminal study on prenatal methylmercury exposure revealed that the total imprecision of exposure biomarkers (25-30% for cord-blood mercury and nearly 50% for maternal hair mercury) was substantially higher than normal laboratory variability [21]. This miscalibration led to a significant underestimation of the true toxicity, causing derived exposure limits to be 50% higher than appropriate. After adjusting for this imprecision, the recommended exposure limit was set 50% lower than the prior standard [21]. This case powerfully demonstrates how unaccounted-for imprecision can directly impact public health guidelines.
Methodologies for Measuring and Controlling Imprecision
Experimental Protocol for Determining Experimental Resolution
The following workflow, adapted from published research, provides a robust method for quantifying the experimental resolution of an analytical assay [17].
The protocol involves creating a series of samples diluted in equal proportions (e.g., 10%, 25%, 50%) and measuring a target analyte (like Albumin initially) across the series [17]. A correlation analysis between the relative concentration and the measured value is performed. The dilution series is only accepted if the correlation shows a statistically significant linear relationship (p ≤ 0.01) [17]. The smallest concentration gradient that maintains this linearity is then defined as the experimental resolution for that assay [17].
Method Validation for Controlling Imprecision
For nonclinical dose formulation analysis—a critical component of PK studies—a full method validation is required. This process involves assessing several parameters to control imprecision [20]:
- Accuracy and Precision: Multiple sets of data are required, often using Quality Control (QC) samples at low, mid, and high concentrations to validate the method's reliability across the dynamic range [20].
- System Suitability Test (SST): Performed before each analytical run to ensure the instrument system is sufficiently sensitive, specific, and reproducible. Parameters include injection precision, theoretical plates, and tailing factor [20].
- Robustness Testing: Deliberately varying method parameters (e.g., pH, mobile phase composition) to ensure the method's performance remains unaffected by small, normal fluctuations [1].
Table 2: Essential Research Reagent Solutions for Method Validation
| Reagent / Solution | Critical Function | Role in Mitigating Imprecision |
|---|---|---|
| Certified Reference Standards | Provides analyte of known purity and concentration [20] | Serves as the benchmark for accuracy; establishes the conventional true value. |
| Matrix-Matched Quality Control (QC) Samples | QC samples prepared in the study vehicle/biological matrix [20] | Assesses accuracy and precision in the presence of matrix components, detecting interference. |
| Appropriate Formulation Vehicle | The excipient (e.g., methylcellulose, saline) used to deliver the test article [20] | Validated to ensure it does not interfere with the analysis, safeguarding specificity. |
| Stability Testing Solutions | Samples prepared and stored under defined conditions [20] | Evaluates the analyte's stability in solution, ensuring imprecision is not driven by analyte degradation. |
Regulatory Implications and Data Integrity Framework
The regulatory framework for data integrity explicitly compels sponsors and testing sites to create a culture of quality and implement risk-based controls to prevent and detect data integrity issues, including those stemming from undetected analytical imprecision [16]. Key requirements include:
- Comprehensive Data Governance: Managing data throughout its entire lifecycle to ensure it remains ALCOA-compliant [16] [23].
- Robust Quality Management Systems (QMS): Incorporating quality assurance (independent verification) and quality control (processes to identify issues) programs [16].
- Rigorous Audit Trails: For electronic data, audit trails must document who made changes, when, and why, providing transparency into data handling [16].
- Thorough Personnel Training: Ensuring all personnel interacting with data are trained on data integrity principles and their specific roles in upholding it [16].
Failure to address imprecision and maintain data integrity can lead to severe regulatory consequences, including refusal to file applications, withdrawal of approvals, and changes to product ratings [16].
Imprecision is an inherent part of any analytical measurement, but its impact on data integrity in pharmacokinetic and biomarker studies is too significant to be overlooked. As evidenced by the comparative data, unmitigated imprecision can distort critical study endpoints, from PK parameters like bioavailability to the predictive accuracy of biomarkers for cancer immunotherapy.
Proactive management through rigorous method validation, including the assessment of novel metrics like experimental resolution, is paramount. Furthermore, adopting a systematic data integrity framework aligned with regulatory guidance creates the necessary quality culture to detect and correct for imprecision early. By implementing the experimental protocols and validation strategies outlined in this guide, researchers and drug development professionals can significantly enhance the reliability of their data, ensuring that critical decisions on drug safety and efficacy are built upon a foundation of uncompromised integrity.
High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) remains a cornerstone technique in pharmaceutical analysis due to its robustness, reliability, and cost-effectiveness. The validation of these methods is paramount to ensure the accuracy, precision, and reproducibility of data, particularly when quantifying drugs in complex matrices like human plasma. This case study examines precision data from a validated HPLC-UV method for the determination of Cinitapride, a gastroenteric prokinetic agent, in human plasma [24]. The research is situated within a broader thesis on method validation, with a specific focus on the challenges and considerations for proving precision at low concentration levels, a common scenario in pharmacokinetic studies.
Cinitapride is a substituted benzamide that acts synergistically on serotonergic (5-HT2 and 5-HT4) and dopaminergic (D2) receptors within the neuronal synapses of the myenteric plexi [24]. The analyzed method employed a reversed-phase (RP) separation on a Nucleosil C18 (25 cm × 4.6 mm, 5 µm) column. The isocratic mobile phase consisted of 10 mM ammonium acetate (pH 5.2), methanol, and acetonitrile (40:50:10, v/v/v), with a flow rate of 1 mL/min and UV detection at 260 nm [24]. Sample preparation was achieved via liquid-liquid extraction (LLE) using tert-butyl methyl ether.
Comparative Analysis with Other HPLC Methods
To contextualize the performance of the Cinitapride method, it is instructive to compare its key validation parameters with those of a separate, recent HPLC-UV method developed for a Glycosaminoglycan (GAG) API in topical formulations, validated per ICH Q2(R2) guidelines [25].
Table 1: Comparison of HPLC-UV Method Validation Parameters
| Validation Parameter | Cinitapride in Human Plasma [24] | GAG API in Topical Formulations [25] |
|---|---|---|
| Linearity Range | 1 – 35 ng/mL | Not Specified (r = 0.9997) |
| Correlation Coefficient (r²/r) | r² = 0.999 | r = 0.9997 |
| Precision (Repeatability) | Intraday & Interday %CV ≤ 7.1% | %RSD < 2% for assay |
| Accuracy (% Recovery) | Extraction Recovery > 86.6% | Recovery range: 98–102% |
| Sample Preparation | Liquid-Liquid Extraction (LLE) | Direct dissolution / Extraction with organic solvent |
| Key Matrix | Human Plasma | Pharmaceutical Gel and Cream |
| Validation Guideline | US FDA | ICH Q2(R2) |
This comparison highlights several key differences dictated by the analytical challenge. The Cinitapride method deals with a much lower concentration range (ng/mL) in a complex biological matrix, which is reflected in its slightly higher, yet still acceptable, precision %CV (≤7.1%) and lower extraction recovery compared to the GAG method for formulated products. The GAG method, analyzing an API in a more controlled matrix, demonstrates the tighter precision (%RSD < 2%) and accuracy typically expected for drug substance and product testing [25].
Experimental Protocols
Detailed Methodology for the Cinitapride HPLC-UV Assay
The following protocols are reconstructed from the referenced study to provide a clear experimental workflow [24].
3.1.1 Materials and Reagents:
- Cinitapride reference standard (provided by Zydus Research Laboratories).
- Human plasma (obtained from Lion's Blood Bank, Guntur, India).
- HPLC-grade solvents: Methanol and Acetonitrile (Merck, Mumbai).
- Reagents: Analytical grade Ammonium Acetate and Triethyl amine (Merck, Mumbai).
- Water: Purified using a Milli-Q water purification system.
3.1.2 Instrumentation and Chromatographic Conditions:
- HPLC System: Shimadzu system equipped with an SPD-20A UV-Visible detector.
- Column: Nucleosil C18 (25 cm × 4.6 mm, 5 µm particle size).
- Mobile Phase: 10 mM Ammonium Acetate Buffer (pH 5.2) - Methanol - Acetonitrile (40:50:10, v/v/v).
- Flow Rate: 1.0 mL/min.
- Detection Wavelength: 260 nm.
- Injection Volume: 20 µL.
- Sample Temperature: Maintained at 10°C during extraction.
3.1.3 Sample Preparation Protocol (Liquid-Liquid Extraction):
- Spiking: Pipette 500 µL of drug-spiked human plasma into a polypropylene tube.
- Extraction: Add 3 mL of tert-butyl methyl ether to the tube, cap it, and vortex mix for 10 minutes.
- Centrifugation: Centrifuge the samples at 4000 rpm for 5 minutes at 10°C to separate the layers.
- Evaporation: Transfer the standard supernatant (organic layer) to a clean tube and evaporate to dryness at 40°C under a gentle stream of nitrogen gas.
- Reconstitution: Reconstitute the dried extract in 500 µL of the mobile phase.
- Injection: Inject a 20 µL aliquot into the HPLC system using a Hamilton syringe.
3.1.4 Precision and Accuracy Protocol:
- Quality Control (QC) Samples: Prepare low (LQC), medium (MQC), and high (HQC) quality control samples in plasma at concentrations of 3, 15, and 35 ng/mL, respectively, with six replicates each.
- Intraday Precision: Analyze all six replicates of each QC level on the same day.
- Interday Precision: Analyze all six replicates of each QC level on three different days.
- Calculation: For both intraday and interday studies, calculate the % Coefficient of Variation (%CV) for precision and the % Recovery of the nominal concentration for accuracy.
Experimental Workflow
The following diagram illustrates the logical flow of the experimental and validation process for the Cinitapride method.
Interpretation of Precision Data at Low Concentrations
Precision, which measures the closeness of agreement between a series of measurements, is critically tested at the lower limits of the analytical method. The data from the Cinitapride method reveals key insights for low-level quantification.
Precision Data Analysis
The precision was validated at three QC levels: LQC (3 ng/mL), MQC (15 ng/mL), and HQC (35 ng/mL). The results showed that the percent coefficient of variation (%CV) for both intraday and interday precision was ≤7.1% across all levels [24]. This demonstrates a consistent and reproducible performance.
Table 2: Precision and Recovery Data for Cinitapride HPLC-UV Method
| Quality Control Level | Concentration (ng/mL) | Intraday Precision (%CV) | Interday Precision (%CV) | Extraction Recovery (%) |
|---|---|---|---|---|
| LQC | 3.0 | ≤ 7.1% | ≤ 7.1% | > 86.6% |
| MQC | 15.0 | ≤ 7.1% | ≤ 7.1% | > 86.6% |
| HQC | 35.0 | ≤ 7.1% | ≤ 7.1% | > 86.6% |
Critical Considerations for Low-Concentration Precision
- Acceptance Criteria Context: While guidelines for assay of drug products often demand %RSD < 2.0% [26], a broader acceptance criterion is common for bioanalytical methods due to the complexity of the biological matrix and the very low analyte concentrations. A %CV of ≤7.1% at the LQC level, which is just three times the LOQ, is considered acceptable in many bioanalytical method validations and reflects the practical challenges of working at the method's lower limits [24].
- Impact of Sample Preparation: The liquid-liquid extraction recovery of >86.6% is a crucial factor contributing to the overall precision. High recovery indicates a clean and efficient extraction process, which minimizes analyte loss and reduces variability. Inefficient recovery can introduce significant error, especially at low concentrations where the absolute amount of analyte is small.
- System Suitability as a Foundation: The precision of the entire method is underpinned by the performance of the chromatographic system. The cited method reported a system suitability with a USP plate count of ≥5600 and a tailing factor of 1.05, indicating a highly efficient and symmetric peak [24]. This robustness is essential for obtaining reliable and precise data, particularly for low-concentration peaks where integration can be more challenging.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for developing and validating an HPLC-UV method like the one described for Cinitapride.
Table 3: Essential Research Reagents and Materials for HPLC-UV Method Validation
| Item | Function / Purpose | Example from Case Study |
|---|---|---|
| Analytical Reference Standard | Serves as the benchmark for identifying the analyte and constructing calibration curves. | Cinitapride working standard [24]. |
| Chromatography Column | The heart of the separation; its chemistry dictates selectivity, efficiency, and retention. | Nucleosil C18 column [24]. |
| HPLC-Grade Solvents | Used in mobile phase and sample preparation to minimize UV background noise and prevent system damage. | Methanol and Acetonitrile from Merck [24]. |
| Buffer Salts & pH Adjusters | Control the pH and ionic strength of the mobile phase, critical for reproducible retention of ionizable analytes. | 10 mM Ammonium Acetate, pH adjusted with Triethylamine [24]. |
| Sample Preparation Solvents | For extracting, precipitating, or diluting the analyte from the sample matrix. | Tert-butyl methyl ether for liquid-liquid extraction [24]. |
| Matrix Source | The blank biological or formulation matrix used for preparing calibration standards and validation samples. | Human plasma from a blood bank [24]. |
| D159687 | D159687, CAS:1155877-97-6, MF:C21H19ClN2O2, MW:366.8 g/mol | Chemical Reagent |
| dBET57 | dBET57, CAS:1883863-52-2, MF:C34H31ClN8O5S, MW:699.2 g/mol | Chemical Reagent |
This case study on the validated HPLC-UV method for Cinitapride provides a clear framework for interpreting precision data, with a special emphasis on low-concentration applications. The method demonstrates that with a robust chromatographic system (evidenced by high plate counts and low tailing) and an efficient sample preparation technique (LLE with >86% recovery), it is possible to achieve satisfactory precision (%CV ≤7.1%) even at concentrations as low as 3 ng/mL in a complex matrix like human plasma. This level of performance, when contextualized with appropriate acceptance criteria, meets the rigorous demands of bioanalytical method validation. The insights gained underscore the importance of a holistic validation approach where system suitability, sample preparation, and precision are intrinsically linked, providing a reliable foundation for quantitative analysis in pharmaceutical research and development.
Proven Methodologies: Designing and Executing Precision Studies for Sensitive Assays
Adhering to ICH Q2(R2) and FDA Guidelines for Analytical Method Validation
The International Council for Harmonisation (ICH) Q2(R2) guideline, along with its companion ICH Q14 on analytical procedure development, represents a fundamental modernization of analytical method validation requirements for the pharmaceutical industry [27]. Simultaneously, the U.S. Food and Drug Administration (FDA) has adopted these harmonized guidelines, making compliance with ICH standards essential for regulatory submissions in the United States [27] [28]. This updated framework shifts the paradigm from a prescriptive, "check-the-box" approach to a scientific, risk-based lifecycle model that begins with method development and continues throughout the method's entire operational lifespan [27] [29].
For researchers focused on precision at low concentration levels, this modernized approach provides a structured framework for demonstrating method reliability, particularly through enhanced attention to quantitation limits, sensitivity, and robustness [2] [1]. The guidelines emphasize building quality into methods from the outset rather than attempting to validate them after development, ensuring that analytical procedures remain fit-for-purpose in an era of advancing analytical technologies [27].
Core Validation Parameters: From Traditional to Updated Requirements
Fundamental Validation Characteristics
The validation parameters required under ICH Q2(R2) establish the performance characteristics that demonstrate a method is fit for its intended purpose [27]. While the core parameters remain consistent with previous guidelines, their application and interpretation have been refined to accommodate modern analytical techniques [30].
Table 1: Core Analytical Method Validation Parameters and Requirements
| Parameter | Definition | Typical Acceptance Criteria | Importance for Low Concentration Precision |
|---|---|---|---|
| Accuracy | Closeness of agreement between the true value and the value found [2] | 98-102% recovery for drug substances; 95-105% for drug products [30] | Ensures reliability of measurements at trace levels |
| Precision | Closeness of agreement between a series of measurements [2] | RSD ≤2.0% for assays; ≤5.0% for impurities [30] | Critical for demonstrating reproducibility at low concentrations |
| Specificity | Ability to assess unequivocally the analyte in the presence of interfering components [27] [2] | No interference from impurities, degradants, or matrix components [2] | Ensures target analyte response is distinguished from background noise |
| Linearity | Ability to obtain results directly proportional to analyte concentration [2] | Correlation coefficient (r²) with predefined acceptance criteria [31] | Establishes proportional response at low concentration ranges |
| Range | Interval between upper and lower concentrations with suitable precision, accuracy, and linearity [27] | Varies by application (e.g., 80-120% for assay; reporting threshold-120% for impurities) [28] | Defines the operational boundaries where method performance is validated |
| LOD/LOQ | Lowest concentration that can be detected (LOD) or quantified (LOQ) with acceptable accuracy and precision [2] | Signal-to-noise ratio of 3:1 for LOD; 10:1 for LOQ [2] | Fundamental for establishing method capability at trace levels |
Enhanced Approaches for Modern Analytical Techniques
The updated guidelines explicitly address modern analytical technologies that have emerged since the original Q2(R1) guideline was published [30]. This includes:
Multivariate analytical methods that employ complex calibration models, requiring validation approaches such as root mean square error of prediction (RMSEP) to demonstrate accuracy [28].
Non-linear calibration models commonly encountered in techniques like immunoassays, where traditional linearity assessments may not apply [28].
Advanced detection techniques including mass spectrometry and NMR, which may require modified validation approaches for specificity demonstration [28].
For researchers working with low concentration analyses, these expanded provisions allow for the application of highly sensitive techniques while maintaining regulatory compliance through appropriate validation strategies [30].
Experimental Protocols for Key Validation Parameters
Establishing Accuracy and Precision at Low Concentrations
Protocol for Accuracy Determination:
- Prepare a minimum of nine determinations across at least three concentration levels covering the specified range [2]
- For drug products, prepare synthetic mixtures spiked with known quantities of components [2]
- Compare results to a reference value or well-characterized alternative method [2]
- Report as percent recovery of the known, added amount, or as the difference between the mean and true value with confidence intervals [2]
Protocol for Precision Assessment:
- Repeatability (Intra-assay Precision): Analyze a minimum of nine determinations covering the specified range (three concentrations, three repetitions each) or a minimum of six determinations at 100% of the test concentration [2]
- Intermediate Precision: Establish through experimental design incorporating variations such as different days, analysts, or equipment [2] [32]
- Reproducibility: Conduct collaborative studies between different laboratories, particularly important for methods intended for regulatory submission [2]
Table 2: Experimental Design for Precision Studies at Low Concentrations
| Precision Type | Minimum Experimental Design | Statistical Reporting | Acceptance Criteria for Trace Analysis |
|---|---|---|---|
| Repeatability | 6 determinations at LOQ concentration | % RSD with confidence intervals | RSD ≤15% for trace analysis [31] |
| Intermediate Precision | 2 analysts preparing and analyzing replicate samples using different systems and reagents | % difference in mean values with Student's t-test | No statistically significant difference between analysts |
| Reproducibility | Collaborative testing between at least 2 laboratories | Standard deviation, RSD, confidence interval | Agreed upon between laboratories based on intended use |
Demonstrating Specificity and Robustness
Specificity Protocol:
- For chromatographic methods, demonstrate peak purity using photodiode-array detection or mass spectrometry [2]
- Conduct stress studies on samples (heat, light, pH, oxidation) to demonstrate separation of degradants from the analyte of interest [2]
- For impurity methods, spike drug substance or product with appropriate levels of impurities and demonstrate separation from main component and from each other [2]
Robustness Protocol:
- Identify critical method parameters (e.g., mobile phase pH, column temperature, flow rate) through risk assessment [27]
- Deliberately vary parameters within a predetermined range and monitor effects on method performance [1]
- Establish system suitability criteria based on robustness testing to ensure method reliability during routine use [28]
Determining Limit of Quantitation (LOQ) for Low Concentration Analysis
For researchers focused on precision at low concentrations, establishing a reliable LOQ is particularly critical. ICH Q2(R2) recognizes multiple approaches:
- Signal-to-Noise Ratio: Typically 10:1, appropriate for chromatographic methods where noise can be measured [2]
- Standard Deviation of Response and Slope: LOQ = 10(SD/S), where SD is the standard deviation of response and S is the slope of the calibration curve [2]
- Visual Evaluation: May be used for non-instrumental methods or when the previous approaches cannot be applied [31]
Once the LOQ is determined, analysis of an appropriate number of samples at this limit must be performed to fully validate method performance [2].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Method Validation
| Reagent/Material | Function in Validation | Critical Quality Attributes | Application in Low Concentration Analysis |
|---|---|---|---|
| Reference Standards | Provides known purity material for accuracy and linearity studies | Certified purity, stability, appropriate documentation | Essential for preparing known concentration samples for recovery studies |
| Chromatographic Columns | Stationary phase for separation | Lot-to-lot reproducibility, stability under method conditions | Critical for achieving sufficient resolution at low concentrations |
| MS-Grade Solvents | Mobile phase components for LC-MS methods | Low background, minimal ion suppression | Reduces chemical noise for improved signal-to-noise at trace levels |
| Sample Preparation Materials | Extraction, purification, and concentration of analytes | Selective extraction, minimal analyte adsorption, clean background | Enables pre-concentration of dilute samples and matrix interference removal |
| System Suitability Standards | Verifies system performance before validation runs | Stability, representative of method challenges | Confirms instrument sensitivity and resolution are adequate for validation |
| DBPR108 | DBPR108, CAS:1186426-66-3, MF:C16H25FN4O2, MW:324.39 g/mol | Chemical Reagent | Bench Chemicals |
| ABCB1-IN-1 | ABCB1-IN-1, CAS:1429239-98-4, MF:C33H31Cl2F3N6O3S2, MW:751.7 g/mol | Chemical Reagent | Bench Chemicals |
Implementing the Analytical Method Lifecycle Approach
The integration of ICH Q14 on analytical procedure development with ICH Q2(R2) validation creates a comprehensive lifecycle management framework [27] [29]. This approach consists of several key elements:
Analytical Target Profile (ATP)
The ATP is a prospective summary of the method's intended purpose and desired performance criteria, defined before method development begins [27]. For low concentration applications, the ATP should explicitly define:
- Required detection and quantitation limits based on the analytical need
- Acceptable precision at the low end of the measuring range
- Specificity requirements considering potential matrix interferences
Risk-Based Validation Strategy
A risk assessment approach helps identify potential method vulnerabilities and focus validation efforts on high-risk areas [30]. This is particularly important for low concentration methods where small variations can significantly impact results. The risk assessment should consider:
- Sample preparation variability at low concentrations
- Instrument sensitivity and detection capabilities
- Matrix effects that may disproportionately affect low concentration measurements
Continuous Performance Verification
The lifecycle approach continues after initial validation with ongoing monitoring of method performance during routine use [29]. This includes:
- Trend analysis of system suitability data
- Regular assessment of quality control sample results
- Periodic review to determine if revalidation is necessary
For low concentration methods, this continuous verification is essential to detect subtle changes in method performance that might affect data reliability [29].
Comparison of Traditional vs. Modernized Validation Approaches
Table 4: Evolution from Q2(R1) to Q2(R2) Validation Requirements
| Aspect | Traditional Approach (Q2(R1)) | Modernized Approach (Q2(R2)) | Impact on Low Concentration Analysis |
|---|---|---|---|
| Validation Scope | Primarily focused on chromatographic methods | Expanded to include modern techniques (multivariate, spectroscopic) | Enables use of more sensitive techniques with appropriate validation |
| Development Linkage | Validation separate from development | Integrated with development through ATP and enhanced approach | Builds quality in rather than testing it out |
| Linearity Assessment | Focus on linear responses only | Includes non-linear response models | Accommodates realistic response behavior at concentration extremes |
| Robustness Evaluation | Often performed after validation | Incorporated early in development with risk assessment | Identifies sensitivity issues before validation |
| Lifecycle Management | Limited post-approval change management | Continuous verification and knowledge management | Allows for method improvements based on performance monitoring |
Adherence to ICH Q2(R2) and FDA guidelines requires a fundamental shift from treating method validation as a one-time event to managing it as a continuous lifecycle process [27] [29]. For researchers focused on precision at low concentration levels, this modernized framework provides the structure to develop and validate robust, reliable methods while maintaining regulatory compliance.
Successful implementation requires:
- Early definition of the Analytical Target Profile with specific attention to low concentration requirements [27]
- Science- and risk-based approaches to validation study design [30]
- Thorough understanding of method capabilities and limitations, particularly at the lower end of the measuring range [2]
- Comprehensive documentation of validation experiments and results [32]
By embracing these principles, researchers can ensure their analytical methods not only meet regulatory expectations but also generate reliable, high-quality data—particularly critical when working at the challenging limits of detection and quantitation.
Method validation provides documented evidence that an analytical procedure is suitable for its intended purpose, ensuring the reliability of data during normal use [2]. For research focusing on precision at low concentration levels, a meticulously planned experimental design is not merely a regulatory formality but the cornerstone of scientific integrity. It guarantees that the method can consistently reproduce results with acceptable accuracy and precision, even near the limits of quantitation. This guide objectively compares experimental design parameters by examining data from validation studies conducted according to established guidelines, such as those from the International Council for Harmonisation (ICH) and the United States Pharmacopeia (USP) [2].
Comparative Experimental Data for Precision
The following tables summarize the experimental design requirements and typical performance outcomes for precision studies as per regulatory guidelines. These parameters are critical for assessing method performance at low concentration levels.
Table 1: Experimental Design Requirements for Precision Validation
| Precision Type | Minimum Number of Replicates | Minimum Concentration Levels | Key Statistical Reporting |
|---|---|---|---|
| Repeatability (Intra-assay) | 9 determinations total (e.g., 3 concentrations x 3 replicates each) or 6 determinations at 100% concentration [2] | 3 levels covering the specified range [2] | Percent Relative Standard Deviation (% RSD) [2] |
| Intermediate Precision | Replicate sample preparations by two different analysts using different equipment and days [2] | Typically at 100% of test concentration | % RSD and statistical comparison (e.g., Student's t-test) of results between analysts [2] |
Table 2: Example Acceptance Criteria for Precision
| Analytical Method Type | Target Precision (Repeatability) | Target Precision (Intermediate Precision) |
|---|---|---|
| Assay of Drug Substance | % RSD ≤ 1.0% - 2.0% | % RSD and mean difference between analysts within specified limits [2] |
| Impurity Quantification (at LOQ) | % RSD ≤ 5.0% - 10.0% | % RSD and mean difference between analysts within specified limits [2] |
Detailed Experimental Protocols
Protocol for Establishing Accuracy and Precision
Objective: To demonstrate the closeness of agreement between the measured value and an accepted reference value (accuracy) and the agreement between a series of measurements obtained from multiple sampling (precision) [2].
Methodology:
- Sample Preparation: Prepare a minimum of nine samples over a minimum of three concentration levels (e.g., 80%, 100%, 120% of the target concentration) covering the specified range of the procedure. This results in three concentrations with three replicates each [2].
- Analysis: Analyze all samples using the validated method.
- Data Analysis:
- Accuracy: Calculate the percent recovery of the known, added amount for each sample. Report the mean recovery and confidence intervals (e.g., ±1 standard deviation) for each concentration level [2].
- Precision (Repeatability): Calculate the % RSD for the results at each concentration level and across the entire study to demonstrate repeatability [2].
Protocol for Determining Limits of Detection and Quantitation
Objective: To determine the lowest concentration of an analyte that can be detected (LOD) and reliably quantified (LOQ) with acceptable precision and accuracy [2].
Methodology:
- Signal-to-Noise Ratio Approach:
- Prepare and analyze samples with known low concentrations of the analyte.
- LOD: The concentration at which the signal-to-noise ratio is approximately 3:1.
- LOQ: The concentration at which the signal-to-noise ratio is approximately 10:1 [2].
- Standard Deviation and Slope Method:
- Based on the formula:
LOD = 3.3(SD/S)andLOQ = 10(SD/S), where SD is the standard deviation of the response and S is the slope of the calibration curve [2]. - Regardless of the method used, the determined limits must be validated by analyzing an appropriate number of samples at the LOD and LOQ to confirm performance [2].
- Based on the formula:
Experimental Workflow and Signaling Pathways
The following diagram illustrates the logical sequence and decision-making process in a robust analytical method validation workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Method Validation Experiments
| Item | Function in Validation |
|---|---|
| Standard Reference Material | A substance with a known purity and composition, used as the primary standard to establish accuracy and prepare calibration curves [2]. |
| Drug Substance/Product | The actual sample matrix (e.g., active pharmaceutical ingredient, formulated product) used to test the method's specificity and accuracy in a relevant background [2]. |
| Known Impurities | Isolated impurities used to spike samples, allowing for the validation of the method's accuracy, precision, and specificity for impurity detection and quantification [2]. |
| Appropriate Chromatographic Column | The specific stationary phase (e.g., C18, phenyl) selected to achieve the required separation of analytes from each other and from matrix components, which is critical for demonstrating specificity [2]. |
| HPLC-Grade Solvents and Reagents | High-purity mobile phase components and buffers that ensure system suitability, reduce background noise, and provide reproducible chromatographic conditions essential for precision and robust results [2]. |
| DD-03-171 | DD-03-171, CAS:2366132-45-6, MF:C55H62N10O8, MW:991.1 g/mol |
| Desmethyl-VS-5584 | Desmethyl-VS-5584, MF:C16H20N8O, MW:340.38 g/mol |
In the pursuit of reliable analytical data, particularly for method validation focused on precision at low concentration levels, sample preparation is a critical first step. It aims to isolate analytes from complex matrices, reduce interference, and concentrate targets to detectable amounts, directly impacting a method's accuracy, sensitivity, and reproducibility. Among the various techniques available, Liquid-Liquid Extraction (LLE) and Solid-Phase Extraction (SPE) are two foundational approaches. This guide provides an objective comparison of their performance, supported by experimental data, to help researchers and drug development professionals select the appropriate technique for their specific application needs, especially when working with trace-level concentrations.
Fundamental Principles and Comparison
Liquid-Liquid Extraction (LLE) separates compounds based on their relative solubility in two immiscible liquids, typically an organic solvent and an aqueous phase. The core mechanism relies on partitioning, where the analyte distributes itself between the two phases based on its chemical potential, aiming for a state of lower free energy [33]. The efficiency is measured by the distribution ratio (D) and the partition coefficient (Kd), which are influenced by temperature, solute concentration, and the presence of different chemical species [33]. LLE is versatile and can handle compounds with different volatilities and polarities.
Solid-Phase Extraction (SPE) utilizes a solid sorbent material to selectively retain analytes from a liquid sample. After retention, interfering compounds are washed away, and the target analytes are eluted with a stronger solvent. SPE formats include cartridges, disks, and 96-well plates, and a wide variety of sorbent chemistries (e.g., C18, ion-exchange, mixed-mode) are available to cater to different analytes [34].
The following table summarizes the core characteristics of each technique:
Table 1: Fundamental Comparison of LLE and SPE
| Characteristic | Liquid-Liquid Extraction (LLE) | Solid-Phase Extraction (SPE) |
|---|---|---|
| Fundamental Principle | Partitioning between two immiscible liquid phases based on solubility [33] | Selective adsorption onto a solid sorbent, followed by washing and elution [34] |
| Primary Mechanism | Solubility and partitioning | Adsorption, chemical affinity (e.g., reversed-phase, ion-exchange) |
| Typical Throughput | Lower, manual process | Higher, potential for automation and 96-well plate formats [34] |
| Solvent Consumption | High | Lower, especially in micro-SPE formats [35] |
| Key Advantage | Simplicity, effective cleanup of complex matrices [33] | Selective, can be automated, lower solvent consumption [35] |
| Key Disadvantage | High solvent use, time-consuming, emulsion formation [35] | Can be prone to clogging, requires method development for sorbent selection |
Performance Data and Experimental Comparison
Quantitative Performance in Bioanalysis
A study comparing an optimized LLE method with a cumbersome combined LLE/SPE method for extracting D-series resolvins from cell culture medium demonstrated the potential of a well-designed LLE protocol. The results are summarized below:
Table 2: Performance Data for Resolvin Analysis using LLE [36]
| Performance Parameter | Optimized LLE Method | Combined LLE/µ-SPE Method |
|---|---|---|
| Linear Range | 0.1–50 ng mLâ»Â¹ | Not specified |
| Limit of Detection (LOD) | 0.05 ng mLâ»Â¹ | Not specified |
| Limit of Quantification (LOQ) | 0.1 ng mLâ»Â¹ | Not specified |
| Recovery (%) | 96.9 – 99.8% | ~42 – 64% |
The data shows that the optimized LLE method provided excellent recovery and sensitivity, outperforming the more complex combined method [36]. This highlights that for specific applications, a straightforward LLE can be superior to more complicated multi-step procedures.
Comparison of SPE Formats and LLE for a Cyanide Metabolite
A study on extracting the polar cyanide metabolite 2-aminothiazoline-4-carboxylic acid (ATCA) from biological samples compared a conventional SPE method with two magnetic carbon nanotube-assisted dispersive-micro-SPE (Mag-CNTs/d-µSPE) methods.
Table 3: Performance Data for ATCA Analysis using Different Methods [35]
| Extraction Method | Matrix | LOD (ng/mL) | LOQ (ng/mL) |
|---|---|---|---|
| Mag-CNTs/d-µSPE | Synthetic Urine | 5 | 10 |
| Mag-CNTs/d-µSPE | Bovine Blood | 10 | 60 |
| Conventional SPE | Bovine Blood | 1 | 25 |
The conventional SPE method showed a slightly better LOD in blood, but the Mag-CNTs/d-µSPE methods demonstrated great potential for extracting polar and ionic metabolites with the advantage of being less labor-intensive and consuming less solvent [35]. This illustrates how modern SPE formats can address some limitations of traditional methods.
Application in Environmental and Proteomic Analysis
A comparative study of LLE, SPE, and solid-phase microextraction (SPME) for multi-class organic contaminants in wastewater found that both LLE and SPE provided satisfactory and comparable performance for most compounds [37].
In proteomics, a comparison of two SPE-based sample preparation protocols (SOLAµ HRP SPE spin plates and ZIPTIP C18 pipette tips) for porcine retinal tissue analysis found no significant differences in protein identification numbers or the quantitative recovery of 25 glaucoma-related protein markers [34]. The key difference was in analysis speed and convenience, with the SOLAµ spin plate workflow being more amenable to semi-automation [34].
Detailed Experimental Protocols
This protocol is for the extraction of D-series resolvins (RvD1, RvD2, etc.) from Leibovitz’s L-15 complete medium.
- Step 1: Internal Standard Addition. Add a mixture of deuterated internal standards (e.g., RvD1-d5, RvD2-d5, RvD3-d5) to the sample. A factorial design can be used to optimize the internal standard concentration.
- Step 2: Extraction. Use a suitable organic solvent pair. The specific solvent was not detailed in the abstract, but common choices for LLE include chloroform/methanol or ethyl acetate.
- Step 3: Mixing and Centrifugation. Vigorously mix the sample and organic solvent, then centrifuge to achieve complete phase separation.
- Step 4: Collection and Evaporation. Collect the organic layer (extract) and evaporate to dryness under a gentle stream of nitrogen gas.
- Step 5: Reconstitution. Reconstitute the dried extract in a small volume of solvent compatible with the LC-MS/MS mobile phase.
- Step 6: Analysis. Analyze using Liquid Chromatography triple Quadrupole Mass Spectrometry (LC-MS/MS).
This protocol uses magnetic carbon nanotubes for dispersive micro-SPE.
- Step 1: Sample Pretreatment. Prepare the biological sample (e.g., blood) likely involving protein precipitation and centrifugation to obtain a clear supernatant.
- Step 2: Sorbent Addition. Add the magnetic carbon nanotubes (Mag-CNTs-COOH or Mag-CNTs-SO3H) to the sample supernatant.
- Step 3: Binding. Mix thoroughly to allow the analyte (ATCA) to adsorb onto the Mag-CNTs.
- Step 4: Separation. Use an external magnet to separate the Mag-CNTs (with bound analyte) from the sample solution. Discard the supernatant.
- Step 5: Washing. Wash the Mag-CNTs with a suitable solvent to remove weakly adsorbed interferents.
- Step 6: Desorption/Derivatization. For Mag-CNTs-COOH, a one-step desorption/derivatization is performed directly with a derivatization reagent. This step elutes the analyte and prepares it for GC-MS analysis in a single step.
- Step 7: Analysis. Analyze the derivatized eluate using Gas Chromatography-Mass Spectrometry (GC-MS).
Workflow Visualization
The following diagram illustrates the general decision-making and procedural workflow when choosing and applying LLE or SPE.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key materials and reagents used in the featured experiments.
Table 4: Key Research Reagent Solutions for Sample Preparation
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Deuterated Internal Standards | Correct for analyte loss during preparation; improve quantification accuracy. | RvD1-d5, RvD2-d5 used in LLE of resolvins for precise LC-MS/MS quantification [36]. |
| Magnetic Carbon Nanotubes (Mag-CNTs) | Dispersive micro-SPE sorbent; enables easy magnetic separation, high surface area for adsorption. | Mag-CNTs-COOH used for d-µSPE of ATCA from blood, enabling one-step derivatization/desorption [35]. |
| C18 Sorbent | Reversed-phase SPE sorbent; retains mid- to non-polar analytes from aqueous matrices. | ZIPTIP C18 pipette tips and SOLAµ HRP spin plates used for peptide desalting and purification in proteomics [34]. |
| Organic Solvents (e.g., Chloroform, Ethyl Acetate) | Extraction phase in LLE; dissolves and carries non-polar target analytes. | Used in LLE methods for resolvins and wastewater contaminants [36] [37]. |
| Buffers (e.g., Ammonium Acetate, Phosphate) | Control pH and ionic strength; critical for optimizing retention/elution in SPE and partitioning in LLE. | Phosphate buffer (5 µM) added to mobile phase in HILIC-MS to improve peak shape for polar metabolites [38]. |
| dMCL1-2 | dMCL1-2, MF:C61H66N10O12S, MW:1163.3 g/mol | Chemical Reagent |
| EF24 | EF24, CAS:342808-40-6, MF:C19H16ClF2NO, MW:347.8 g/mol | Chemical Reagent |
Both LLE and SPE are powerful techniques for obtaining clean samples. The choice between them is not a matter of which is universally better, but which is more suitable for the specific analytical challenge. LLE offers simplicity, low equipment costs, and highly effective cleanup for many applications, as demonstrated by its excellent performance in resolvin extraction [36]. SPE provides advantages in throughput, potential for automation, and lower solvent consumption, especially in modern formats like d-µSPE and 96-well plates [35] [34]. For methods requiring high precision at low concentrations, the decision should be guided by the nature of the analyte, the sample matrix, and the required throughput, with the understanding that both techniques, when properly optimized and validated, can deliver the rigorous performance demanded in research and drug development.
Chromatographic method development is a critical process in pharmaceutical analysis, requiring careful optimization of column chemistry, mobile phase composition, and detector parameters to achieve precise and accurate results, particularly at low analyte concentrations. Within the framework of method validation for precision at low concentration levels, each component of the high-performance liquid chromatography (HPLC) system contributes significantly to the overall method performance, sensitivity, and reliability.
This guide provides an objective comparison of available technologies and approaches for chromatographic optimization, supported by experimental data and structured within the rigorous requirements of analytical method validation. For researchers and drug development professionals, understanding these interrelationships is essential for developing robust methods that meet regulatory standards set forth by ICH Q2(R2) and FDA guidelines [27].
Column Chemistry Selection and Comparison
The stationary phase is the foundational element of chromatographic separation, directly influencing selectivity, efficiency, and resolution. Recent innovations in column technology have focused on improving peak shape, enhancing chemical stability, and reducing undesirable secondary interactions.
Table 1: Comparison of Modern HPLC Column Chemistries
| Column Type | Stationary Phase Chemistry | Key Characteristics | Optimal Application Areas |
|---|---|---|---|
| C18 | Octadecyl silane | High hydrophobicity; wide pH range (1-12 for modern phases); general-purpose workhorse | Pharmaceutical APIs, metabolites, environmental pollutants |
| Phenyl-Hexyl | Phenyl-hexyl functional groups | π-π interactions with aromatic compounds; enhanced polar selectivity | Metabolomics, isomer separations, hydrophilic aromatics |
| Biphenyl | Biphenyl functional groups | Combined hydrophobic, π-π, dipole, and steric interactions | Polar and non-polar compound analysis, complex mixtures |
| HILIC | Silica, amino, cyano, or diol | Hydrophilic interactions; retains polar compounds | Polar metabolites, carbohydrates, nucleotides |
| Inert Hardware | Various phases with metal-free hardware | Prevents adsorption of metal-sensitive analytes; improved recovery | Phosphorylated compounds, chelating analytes, biomolecules |
Advanced column technologies introduced in 2025 include superficially porous particles with fused-core designs that provide enhanced efficiency and improved peak shapes for basic compounds [39]. The trend toward inert hardware continues to gain momentum, addressing the critical need for improved analyte recovery for metal-sensitive compounds such as phosphorylated molecules and certain pharmaceuticals [39]. These columns feature passivated hardware that creates a metal-free barrier between the sample and stainless-steel components, significantly enhancing peak shape and quantitative recovery [39].
For method validation at low concentrations, specificity is paramount—the column must provide sufficient resolution to distinguish the analyte from potentially interfering components in the sample matrix [1]. The selection of appropriate column chemistry directly impacts this validation parameter, establishing the foundation for all subsequent optimization steps.
Mobile Phase Optimization Strategies
The mobile phase serves as the transport medium through the chromatographic system and plays an active role in the separation mechanism. Its composition critically influences retention, selectivity, and peak shape, making optimization essential for methods requiring precision at low concentrations.
Composition and Modifiers
In reversed-phase chromatography, the mobile phase typically consists of water mixed with polar organic solvents such as acetonitrile or methanol. The ratio of these components determines the elution strength, with higher organic percentages decreasing retention times [40]. Beyond basic solvent selection, strategic use of mobile phase additives can dramatically enhance separation quality:
- Acids and Bases: The inclusion of acids (e.g., formic acid) or bases helps regulate the pH of the mobile phase, controlling the ionization state of analytes and leading to sharper peaks and improved resolution [40].
- Ion-Pairing Reagents: These amphiphilic compounds consist of an ionic head and a hydrophobic tail. When added to the mobile phase, they bind to oppositely charged analytes, reducing their polarity and increasing retention for ionic compounds [40].
- Buffers: For biological or sensitive samples, buffers are added to maintain stable pH levels throughout the analysis, which is vital because pH fluctuations can cause changes in analyte stability and retention [40].
Systematic Optimization Approach
Gradient elution represents a powerful optimization technique where the mobile phase composition is varied throughout the analysis. By gradually increasing or decreasing the concentration of organic solvents, chromatographers can achieve better control over retention times and improve resolution between closely eluting compounds [40]. This approach is particularly valuable when analyzing complex mixtures containing components with a wide range of polarities.
The pH of the mobile phase deserves special consideration as it profoundly influences the ionization state of ionizable analytes, thereby affecting retention times and separation efficiency. For reproducible methods, the pH should be measured before adding organic solvents, as pH meters are calibrated for aqueous solutions and readings in mixed solvents can be inaccurate [40].
Table 2: Mobile Phase Optimization Parameters and Their Effects
| Parameter | Impact on Separation | Optimization Consideration |
|---|---|---|
| Organic Solvent Ratio | Higher organic concentration decreases retention | Adjust for optimal retention (k between 2-10) |
| pH | Controls ionization of acidic/basic compounds; affects selectivity | Set 2 units away from pKa for ionizable compounds |
| Buffer Concentration | Affects peak shape and retention of ionizable analytes | Typical 5-50 mM; avoid MS source contamination |
| Additives | Can improve selectivity, peak shape, and sensitivity | Ion-pairing reagents for ionic compounds |
| Flow Rate | Higher flow rates shorten analysis but may reduce resolution | Optimize for resolution vs. analysis time balance |
Experimental protocols for mobile phase optimization should employ a systematic approach, beginning with scouting gradients at different pH values to identify the optimal starting conditions [40]. Fine-tuning then focuses on isocratic conditions or shallow gradient slopes to maximize resolution of critical peak pairs. Throughout this process, method robustness should be evaluated by deliberately varying key mobile phase parameters (e.g., pH ± 0.2 units, organic composition ± 2-3%) to ensure the method can tolerate normal operational variations [1].
Detector Parameter Optimization
Detector settings significantly influence method sensitivity, especially critical for quantifying low-concentration analytes where precision is paramount. Modern HPLC detectors offer multiple adjustable parameters that must be optimized to achieve the desired signal-to-noise ratio.
Key Detector Parameters and Their Effects
A 2025 study using the Alliance iS HPLC System with PDA Detector demonstrated how systematic optimization of detector parameters produced a 7-fold increase in the USP signal-to-noise ratio compared to default settings [41]. The critical parameters and their impacts include:
- Data Rate: Defines how frequently the detector collects data, measured in hertz (Hz). The data rate should be set to yield 25-50 points across the narrowest peak in the chromatogram. Rates that are too low result in poorly defined peaks, while excessively high rates may increase noise [41].
- Filter Time Constant: Functions as a noise filter that removes high-frequency noise. Faster time constants produce narrower peaks but remove less baseline noise, while slower time constants result in broader peaks with decreased baseline noise [41].
- Slit Width: Determines the amount of light reaching the photodiode array sensor. Smaller slit widths improve resolution, while larger slit widths reduce noise and increase sensitivity at the cost of resolution [41].
- Absorbance Compensation: Provides a way to reduce non-wavelength dependent noise by collecting absorbance data over a user-specified wavelength range where there is little or no absorption and subtracting this average from the signal [41].
Experimental Protocol for Detector Optimization
The referenced study employed a systematic, one-variable-at-a-time approach to optimize detector parameters for the USP method for organic impurities in ibuprofen tablets [41]. The experimental sequence was designed to assess parameters with the greatest impact first:
- Data Rate Optimization: The 5-ppm ibuprofen system suitability solution was analyzed with data rates of 1, 2, 10, and 40 Hz, revealing 2 Hz as optimal with 31 points across the peak and a USP S/N ratio of 25 [41].
- Filter Time Constant Evaluation: With data rate fixed at 2 Hz, the solution was analyzed using slow, normal, fast, and no filter time constants, identifying the slow filter as providing the highest S/N ratio [41].
- Slit Width Assessment: Testing slit widths of 35 µm, 50 µm, and 150 µm showed the S/N ratio acceptance criteria was met with all widths, with only minor differences observed [41].
- Absorbance Compensation: Applying the default compensation wavelength range (310-410 nm) where no absorbance occurred resulted in a reduction in noise and a 1.5x increase in the S/N ratio [41].
Table 3: Detector Parameter Optimization Results (Alliance iS HPLC System with PDA)
| Parameter | Default Setting | Optimized Setting | Impact on S/N Ratio |
|---|---|---|---|
| Data Rate | 10 Hz | 2 Hz | Significant improvement |
| Filter Time Constant | Normal | Slow | Highest S/N obtained |
| Slit Width | 50 µm | 50 µm (no change) | Minimal impact |
| Resolution | 4 nm | 4 nm (no change) | Minimal impact |
| Absorbance Compensation | Off | On (310-410 nm) | 1.5x increase |
| Overall Method | Default parameters | Optimized parameters | 7x increase |
This experimental approach demonstrates that with minimal effort, detector parameters can be systematically optimized to yield substantial improvements in sensitivity—a critical consideration for methods targeting low concentration levels where precision is challenging to achieve.
Integrated Optimization Workflow
Successful chromatographic optimization requires a holistic approach that considers the synergistic relationships between column chemistry, mobile phase composition, and detector parameters. The following diagram illustrates the systematic workflow for achieving optimal method performance with precision at low concentrations:
Research Reagent Solutions
Table 4: Essential Research Reagents for Chromatographic Optimization
| Reagent/Category | Function/Purpose | Application Examples |
|---|---|---|
| High-Purity Water | Polar solvent in reversed-phase mobile phases | Base solvent for aqueous-organic mobile phases |
| HPLC-Grade Acetonitrile | Organic modifier for reversed-phase chromatography | Gradient elution of small molecules and pharmaceuticals |
| Formic Acid | Mobile phase additive to control pH and improve ionization | LC-MS applications for enhanced sensitivity |
| Ammonium Acetate/Formate | Buffer salts for pH control in mobile phases | Ionizable compound separation; LC-MS compatibility |
| Ion-Pairing Reagents | Enhance retention of ionic compounds | Separation of acids, bases, nucleotides |
| Reference Standards | Method development and validation | System suitability; accuracy determination |
Method Validation Framework
Within the context of method validation for precision at low concentration levels, chromatographic optimization must address specific performance characteristics outlined in ICH Q2(R2) guidelines [27]. The Analytical Target Profile (ATP) concept introduced in ICH Q14 provides a prospective summary of the method's intended purpose and should guide the optimization process [27].
The six key aspects of analytical method validation provide a framework for evaluating optimized methods [1]:
- Specificity: Ability to assess unequivocally the analyte in the presence of potentially interfering components.
- Accuracy: Closeness of agreement between the conventional true value and the value found.
- Precision: Degree of scatter between multiple measurements from the same homogeneous sample.
- Sensitivity: Lowest amount of analyte that can be detected and quantified with acceptable accuracy and precision.
- Linearity/Range: Ability to obtain results proportional to analyte concentration within a given range.
- Robustness: Capacity to remain unaffected by small variations in method parameters.
For low concentration applications, special attention should be paid to sensitivity parameters—Limit of Detection (LOD) and Limit of Quantitation (LOQ)—which are directly influenced by chromatographic optimization decisions [27]. The optimized detector parameters discussed in Section 4, combined with appropriate column chemistry and mobile phase composition, directly enhance these critical validation parameters.
Chromatographic optimization represents a multidimensional challenge requiring careful balancing of column chemistry, mobile phase composition, and detector parameters. When developing methods with precision at low concentration levels, each decision must be evaluated against validation parameters to ensure fitness for purpose.
The most effective optimization strategies follow a systematic approach, beginning with a clearly defined Analytical Target Profile and proceeding through sequential optimization of each chromatographic component. As demonstrated by experimental data, significant improvements in sensitivity (up to 7-fold increases in S/N ratio) can be achieved through targeted detector optimization, while proper selection of column chemistry and mobile phase composition establishes the foundation for robust separations.
For researchers and drug development professionals, this holistic approach to chromatographic optimization provides a pathway to developing reliable, validated methods capable of meeting the rigorous demands of modern pharmaceutical analysis, particularly when precision at low concentrations is required.
In the field of pharmaceutical development, the validation of analytical methods is paramount to ensure the reliability, accuracy, and precision of data used to make critical decisions about drug safety and efficacy. Within this framework, statistical analysis serves as the backbone for demonstrating that a method is fit for its intended purpose. Descriptive statistics—specifically the mean, standard deviation (SD), and percent coefficient of variation (%CV)—provide the fundamental metrics for quantifying the precision of an analytical procedure. Precision, defined as the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample, is a cornerstone of method validation [2]. This guide objectively compares different approaches for evaluating precision, with a specific focus on the challenges and solutions associated with low concentration levels, a common scenario in the analysis of impurities or drugs in biological matrices.
The International Conference on Harmonisation (ICH) Q2(R1) guideline categorizes precision into three tiers: repeatability (intra-assay precision), intermediate precision, and reproducibility [2] [32]. At each level, the calculation of mean, SD, and %CV is indispensable. The mean provides a measure of central tendency, the SD quantifies the absolute dispersion or variability in the data, and the %CV (calculated as (Standard Deviation / Mean) × 100%) expresses the relative variability, allowing for comparison across different concentration levels or methods [42]. This is particularly crucial at low concentrations, where the absolute variability might be small, but the relative impact on data interpretation can be significant. The following sections provide a detailed comparison of precision assessment methodologies, supported by experimental data and protocols.
Comparative Analysis of Precision Assessment Approaches
The evaluation of precision can be approached differently depending on the stage of method development, the criticality of the method, and available resources. The table below summarizes the key characteristics of three common approaches for assessing precision and estimating variability.
Table 1: Comparison of Approaches for Assessing Method Precision
| Approach | Description | Typical Context | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Traditional Validation Studies | A pre-defined, rigorous experiment to estimate repeatability and intermediate precision as per ICH guidelines [2] [32]. | Initial method validation; regulatory submission. | Provides a comprehensive and regulatory-accepted snapshot of method performance under controlled conditions. | Provides only a baseline estimate; may not reflect long-term performance or all real-world variability sources. |
| Continuous Performance Verification | Ongoing monitoring of method performance through quality control samples and control charts throughout the method's lifecycle [43]. | Routine use of a validated method in a quality control laboratory. | Enables ongoing assurance of precision; can detect trends or shifts in method performance over time. | Requires a robust data management system; long time-frame needed to collect sufficient data. |
| Novel Data Mining Methodology | Estimates method variability directly from results generated during routine execution, using replication strategies [43]. | Method lifecycle management; investigation of specific variability sources; method development. | Utilizes existing data, making it cost-effective; provides a realistic estimate of variability under actual operating conditions. | Requires careful experimental design; may be complex to implement for some method types. |
A practical example from a clinical diagnostic laboratory illustrates the application of the traditional approach. In a method validation for hemoglobin A1c (HbA1c), 40 patient samples were analyzed using both a new and an old method. The mean, standard deviation (SD), and coefficient of variation (%CV) were calculated to determine precision. The %CV was used to compare the mean value to the standard deviation and measure the dispersion of the test results, confirming the method's acceptability [42].
Experimental Protocols for Precision Determination
Protocol for Determining Repeatability (Intra-Assay Precision)
Repeatability expresses the precision under the same operating conditions over a short interval of time [2] [32]. The following protocol is aligned with ICH recommendations.
- Objective: To determine the precision of an analytical method under identical conditions, performed by the same analyst, using the same equipment and reagents in a single session.
- Materials and Reagents:
- Homogeneous stock solution of the analyte (e.g., drug substance) at a known concentration.
- Appropriate diluents and mobile phases as per the analytical method.
- Calibrated analytical instrument (e.g., HPLC system with UV detection).
- Procedure:
- Prepare a single homogeneous sample at a specific concentration within the method's range. For a comprehensive assessment, this is often done at a minimum of three concentrations (e.g., low, medium, and high) covering the specified range [2] [32].
- For each concentration level, inject or analyze this sample a minimum of six times [32].
- Perform all analyses in one sequence by one analyst using the same instrument and consumables.
- Data Analysis:
- For each set of replicates at a given concentration, calculate the Mean (average) measured concentration.
- Calculate the Standard Deviation (SD) of the replicate measurements.
- Calculate the %CV using the formula: %CV = (SD / Mean) × 100%.
- Report the individual results, mean, SD, and %CV for each concentration level. The %RSD is a typical measure for reporting repeatability [2].
Protocol for Determining Intermediate Precision
Intermediate precision expresses within-laboratory variations, such as different days, different analysts, or different equipment [2] [32].
- Objective: To assess the impact of random laboratory variations on the analytical results.
- Procedure:
- Prepare a homogeneous sample at a specific concentration (again, often evaluated at multiple levels).
- Have two different analysts perform the analysis on two different days.
- Each analyst uses their own standards and solutions and may use a different HPLC system of the same model [2].
- Each analyst should prepare and analyze a minimum of three replicates of the sample at each concentration level [32].
- Data Analysis:
- Collect all data from both analysts and days.
- The data can be analyzed using variance components (ANOVA) to partition the total variability into contributions from between-analyst, between-day, and residual (repeatability) variations [32].
- The overall intermediate precision can be reported as the combined %CV from these variance components.
- Alternatively, the %-difference in the mean values between the two analysts' results can be calculated and subjected to statistical testing (e.g., a Student's t-test) [2].
Visualizing the Statistical Workflow for Precision Analysis
The following diagram illustrates the logical workflow for conducting a full precision study, from experimental design to data analysis and interpretation, incorporating elements of both repeatability and intermediate precision.
Essential Research Reagent Solutions for Robust Statistical Analysis
The reliability of statistical calculations is directly dependent on the quality of the input data, which in turn is influenced by the reagents and materials used. The following table details key solutions required for generating high-quality data in chromatographic methods, which is a common analytical technique in pharmaceutical development.
Table 2: Key Research Reagent Solutions for Analytical Method Precision Studies
| Research Reagent Solution | Function in Precision Analysis |
|---|---|
| High-Purity Reference Standard | Serves as the basis for preparing known concentrations of the analyte. Its purity and stability are critical for accurate calculation of the mean and for determining recovery in accuracy studies, which underpin precision assessments [2]. |
| Chromatographic Mobile Phase Buffers | The composition and pH of the mobile phase (e.g., phosphate buffer) are critical for achieving consistent retention times and peak shape in HPLC. Inconsistent preparation can introduce significant variability, adversely affecting the standard deviation and %CV [44]. |
| Quality Control (QC) Samples | These are samples with known concentrations of the analyte, typically prepared at low, medium, and high levels within the calibration range. They are analyzed alongside test samples to continuously monitor the precision and accuracy of the method during its routine use [42] [43]. |
| System Suitability Solutions | A specific mixture containing the analyte and/or potential impurities used to verify that the chromatographic system is performing adequately before analysis. Parameters like retention time, tailing factor, and theoretical plates ensure the system itself is not a major source of variability before precision data is collected [2]. |
The statistical analysis of mean, standard deviation, and %CV is non-negotiable for demonstrating the precision of an analytical method, a requirement firmly embedded in regulatory guidelines. For researchers and scientists in drug development, selecting the appropriate approach for precision assessment—whether a traditional validation study, continuous monitoring, or a novel data-driven methodology—depends on the stage of the method's lifecycle and the specific questions being addressed. This is especially critical at low concentration levels, where method variability has a magnified impact on data interpretation. A rigorous, statistically sound precision study, supported by high-quality reagents and a clear understanding of variance components, provides the evidence needed to ensure that analytical methods produce reliable data. This reliability forms the foundation for making confident decisions in the drug development process, ultimately safeguarding public health.
Beyond the Basics: Troubleshooting Poor Precision and Optimizing Method Robustness
In the realm of diagnostic testing and bioanalytical method development, achieving precision at low concentration levels presents a formidable scientific challenge. The emergence of highly sensitive therapies, such as antibody-drug conjugates (ADCs) that target low-abundance biomarkers, has exposed significant limitations in traditional assay methodologies [45]. Variability in low-level assays not only compromises the reliability of experimental data but also carries profound implications for patient care, drug development, and regulatory decision-making. This guide objectively compares current approaches for identifying, quantifying, and mitigating the major sources of variability in low-level assays, with a specific focus on method validation parameters essential for ensuring precision at low concentration levels. By examining experimental data from recent studies and providing detailed protocols, this resource aims to equip researchers and drug development professionals with practical strategies to enhance the robustness of their low-level assays.
The fundamental challenge stems from the fact that many assays currently in widespread use were originally developed and validated for detecting high-abundance targets. When these same assays are repurposed for detecting low-level targets, they often demonstrate poor dynamic range and insufficient analytic sensitivity, leading to substantial inter-laboratory discrepancies [45]. For instance, in the case of HER2-low testing for breast cancer, conventional immunohistochemistry (IHC) assays exhibit detection thresholds ranging from 30,000 to 60,000 HER2 molecules per cell—sufficient for identifying HER2 overexpression (3+) but inadequate for accurately distinguishing HER2-low expression (1+ or ultra-low) critical for treatment selection with Trastuzumab deruxtecan [45]. This precision gap at low concentration levels necessitates a systematic approach to method validation specifically tailored to the challenges of low-level detection.
Analytic Sensitivity Limitations
The foundational source of variability in low-level assays stems from inherent limitations in analytic sensitivity. Traditional assay configurations often lack the necessary detection thresholds to reliably quantify low-abundance targets. The CASI-01 study, a comprehensive investigation involving 54 IHC laboratories across Europe and the U.S., revealed that conventional HER2 assays demonstrated high accuracy for identifying HER2 overexpression (3+) with 85.7% sensitivity and 100% specificity, but these same assays exhibited poor dynamic range for detecting HER2-low scores [45]. This performance gap directly impacts clinical decision-making, as retrospective analyses have found that approximately 30% of cases initially judged as HER2 0 were reclassified as HER2 1+ upon repeat staining with more sensitive methods [45].
The dynamic range problem is particularly pronounced when assays developed for detecting overexpression are repurposed for detecting low/very low expression levels. Such assays may miss tumors that express clinically relevant levels of biomarkers in the context of modern targeted therapies [45]. The detection threshold variability among laboratories—ranging from 30,000 to 60,000 HER2 molecules per cell in the case of HER2 testing—creates significant consistency challenges, especially in multi-center trials or when translating clinical trial findings to broader practice [45].
Technical and Operational Variability
Technical sources of variability encompass multiple facets of assay execution, including reagent lots, instrumentation differences, and operator technique. In large-scale studies, variability correlated to the veterinary practice conducting tests has been identified as potentially substantial [46]. Similarly, in mass spectrometry-based proteomics, instrument type significantly impacts low-level quantification, with linear ion traps (LITs) offering advantages for low-input samples compared to high-resolution instruments, particularly at or below 10 ng total protein input [47].
Operational variability extends to sample processing, staining protocols (in IHC), and data acquisition parameters. For instance, in targeted proteomics using parallel reaction monitoring (PRM), the width of isolation windows for precursor ions (typically 0.2 to 2 m/z FWHM) influences both specificity and sensitivity, with wider windows (e.g., 2 m/z) often used to capture multiple isotopes per precursor simultaneously to increase sensitivity for low-abundance targets [47]. These technical parameters must be carefully controlled and standardized to minimize their contribution to overall variability.
Interpretive and Readout Variability
The method of readout and interpretation introduces another significant source of variability, particularly in assays relying on subjective assessment. The CASI-01 study demonstrated that pathologist readout/scoring and its inter- and intra-observer reproducibility are problematic because accurate identification of low levels of protein expression is challenging for human observers [45]. This interpretive variability is compounded by the historical practice of grouping negative and very low expression categories together in proficiency testing, as was common with HER2 0 and 1+ scores [45].
The integration of objective readout methods, such as image analysis, can substantially mitigate this source of variability. Studies have shown that enhanced analytic sensitivity of IHC assays combined with image analysis achieves a six-fold improvement in dynamic range for detecting HER2-low scores compared to conventional methods with pathologist readout [45]. This demonstrates how the transition from subjective to objective assessment methods represents a critical strategy for reducing variability in low-level assays.
Reference Material-Based Validation
The use of well-characterized reference materials provides a powerful approach for identifying and quantifying variability sources in low-level assays. The CASI-01 study pioneered the application of newly developed IHC HER2 reference materials as an objective accuracy standard, establishing assay dynamic range as a critical new parameter for IHC assay performance evaluation [45]. This approach breaks new ground by providing an objective benchmark for assessing inter-laboratory and inter-assay variability.
Experimental Protocol: Reference Material Implementation
- Procurement and Characterization: Source reference materials with known target concentrations spanning the range of clinical interest, including very low levels. For HER2 testing, this included samples with expression levels from 0 to 3+ equally represented in tissue microarrays [45].
- Parallel Testing: Distribute identical reference materials to participating laboratories for testing using standardized protocols. The CASI-01 study employed tissue microarrays with 80 cores equally divided across HER2 scores (0-3+) shipped to 54 IHC laboratories [45].
- Calibration and Quantification: Quantify calibrator stain intensity using objective measures. For HER2 testing, this involved quantifying the number of HER2 molecules per cell using standardized approaches [45].
- Data Analysis: Compare results across sites, assays, and operators to identify variability sources. Statistical process control methods should be applied to establish acceptable performance boundaries.
The transformative impact of this approach lies in its ability to move beyond qualitative or relative assessments to truly quantitative evaluation of assay performance at low concentration levels. Without such reference standards, it is challenging to determine whether variability stems from the assay itself, reagent lots, instrumentation, or operator factors.
Machine Learning-Enhanced Performance Assessment
Machine learning approaches offer a sophisticated methodology for identifying subtle sources of variability in low-level assays by analyzing complex, multi-factor datasets. Banks et al. demonstrated this approach for bovine tuberculosis (bTB) testing, using exceptionally detailed testing records to develop models that identify variability sources and improve test interpretation [46].
Experimental Protocol: Machine Learning Integration
- Data Curation: Compile comprehensive testing datasets including all relevant metadata. For bTB testing, this included test results, farm characteristics, animal movements, veterinary practice information, and tuberculin batch data [46].
- Feature Engineering: Identify potential variability sources as model features. The bTB study included features such as test type, herd type, test reason, location, and historical test results [46].
- Model Training: Employ appropriate machine learning algorithms. The bTB study used a Histogram-based Gradient Boosted Tree (HGBT) model, with data split into training and testing sets (tests from 2020 onwards comprised the testing set) [46].
- Feature Importance Testing: Analyze the weighting of risk factors in the model to identify those most associated with variability in test performance [46].
This approach revealed that without compromising test specificity, test sensitivity could be improved so that the proportion of infected herds detected improved by over 5 percentage points, equivalent to 240 additional infected herds detected in one year beyond those detected by the standard test alone [46]. The model also identified specific factors suggesting that in some herds there was a higher risk of infection going undetected, highlighting previously unrecognized sources of variability [46].
Comparative Instrumentation Studies
For instrumentation-based assays, direct comparison of platform performance at low concentration levels is essential for identifying technology-specific variability sources. The study by Banks et al. on linear ion trap mass spectrometry provides a template for such comparative assessments [47].
Experimental Protocol: Instrument Comparison
- Sample Preparation: Prepare matched samples across a concentration range spanning low abundance levels. For proteomics, this included 1, 10, and 100 ng total protein inputs to model low abundant immune cell populations [47].
- Parallel Measurement: Analyze identical samples using different instrument platforms. The Q-LIT instrument was compared to Q-Orbitrap using wide-window DIA and targeted PRM experiments [47].
- Performance Metric Assessment: Evaluate key parameters including detection limits, quantitative linearity, and consistency. For the Q-LIT, this included assessing the ability to measure low-level proteins such as transcription factors and cytokines with quantitative linearity below two orders of magnitude in a 1 ng background proteome [47].
- Data Integration Consistency: Compare results between platforms, focusing on low-abundance targets where variability is most pronounced.
This approach revealed that from a 1 ng sample, clear consistency could be found between proteins in subsets of CD4+ and CD8+ T cells measured using high dimensional flow cytometry and LIT-based proteomics, demonstrating the utility of such comparative studies for validating performance at low concentration levels [47].
Comparative Performance Data: Assays and Platforms
Immunohistochemistry Platforms for Low-Level Protein Detection
Table 1: Comparison of IHC Approaches for Low-Level Protein Detection
| Platform/Assay Type | Detection Threshold | Dynamic Range | Sensitivity for Low Targets | Key Applications |
|---|---|---|---|---|
| Conventional Predicate Assays | 30,000-60,000 molecules/cell [45] | Limited for low scores [45] | Poor, missed ~30% of HER2-low cases [45] | HER2 overexpression (3+) detection [45] |
| High-Sensitivity Assays with Image Analysis | Not specified | 6-fold improvement over predicate [45] | Enhanced, correctly classified HER2-low cases [45] | HER2-low and ultra-low detection [45] |
| Machine Learning-Augmented Interpretation | Not applicable | Improved sensitivity by >5 percentage points [46] | Enhanced without compromising specificity [46] | Bovine tuberculosis testing, adaptable to other applications [46] |
Mass Spectrometry Platforms for Low-Input Proteomics
Table 2: Comparison of Mass Spectrometry Platforms for Low-Level Detection
| Platform Type | Optimal Input Range | Quantitative Linearity | Low-Abundance Protein Detection | Workflow Versatility |
|---|---|---|---|---|
| Triple Quadrupole (QqQ) | Not specified | Excellent for targeted SRM [47] | Sensitive but limited to targeted work [47] | Restricted to targeted proteomics [47] |
| Q-Orbitrap | ≥100 ng [47] | High with high mass accuracy [47] | Effective at higher inputs [47] | Global and targeted proteomics [47] |
| Hybrid Quadrupole-LIT (Q-LIT) | ≤10 ng, down to single cells [47] | Below two orders of magnitude in 1 ng background [47] | Can measure transcription factors and cytokines at 1 ng [47] | Both targeted and global proteomics [47] |
| Tribrid Instruments (Orbitrap with LIT) | Single-cell level [47] | Approximately 400 proteins from single cells [47] | Limited to most observable proteins [47] | Global proteomics with DIA [47] |
Strategies for Mitigating Variability in Low-Level Assays
Enhanced Sensitivity Assays with Image Analysis
The integration of enhanced sensitivity assays with automated image analysis represents a powerful strategy for mitigating variability in low-level detection. The CASI-01 study demonstrated that this combination overcame the dynamic range limitations of conventional HER2 assays for detecting HER2-low scores, achieving a six-fold improvement (p = 0.0017) [45]. This approach directly addresses the fundamental challenge of poor dynamic range in traditional assays designed for high-abundance targets.
Implementation requires carefully validated protocols for both the enhanced sensitivity assay and the image analysis component. For HER2 testing, this involved comparing conventional FDA-cleared HER2 assays with higher-sensitivity assays using both pathologist versus image analysis readouts [45]. The results demonstrated that image analysis can surpass pathologist readout accuracy in specific clinical contexts, particularly for distinguishing subtle differences in low-level expression [45]. This strategy transforms the assay from a qualitative "stain" to a quantitative "assay" approach incorporating calibration, reference standards, and analytic sensitivity metrics.
Reference Standard Implementation and Calibration
The systematic implementation of reference standards and calibration procedures provides a foundational strategy for reducing variability in low-level assays. The CASI-01 study introduced pivotal advancements in this area by establishing the importance of reporting IHC analytic sensitivity and the ability to demonstrate an assay dynamic range [45]. This represents a significant evolution from unregulated "stain" approaches to a robust "assay" model incorporating calibration, reference standards, analytic sensitivity metrics, and statistical process control [45].
Implementation Protocol:
- Reference Standard Selection: Choose standards with well-characterized low-level target concentrations that span the clinical range of interest.
- Calibration Curve Development: Establish calibration curves using reference standards to enable quantitative interpretation rather than relative scoring.
- Process Control Integration: Implement statistical process control to monitor assay performance over time and across lots.
- Inter-laboratory Standardization: Utilize common reference standards across laboratories to harmonize results.
This approach enables the transition from subjective scoring systems (e.g., 0, 1+, 2+, 3+) to truly quantitative measurements (e.g., molecules per cell), dramatically reducing interpretive variability and improving consistency across sites and over time [45].
Integrated Assay Development Workflows
For instrumentation-based assays, integrated workflows that facilitate rapid assay development and optimization can significantly reduce variability in low-level detection. The linear ion trap workflow described by Banks et al. provides a template for such an integrated approach, using a hybrid quadrupole-LIT instrument as a single platform for both library generation and targeted proteomics measurement [47].
This workflow includes automated software for scheduling parallel reaction monitoring assays (PRM) that enables consistent quantification across three orders of magnitude in a matched-matrix background [47]. By using a single instrument for both global (DIA) and targeted (PRM) proteomics, this approach reduces the variability introduced when transitioning between different platforms for assay development versus implementation.
The development of open-source software tools that directly schedule and optimize PRM assays from DDA and DIA libraries further enhances reproducibility and reduces technical variability [47]. Such integrated workflows demonstrate how technological advances coupled with optimized software solutions can mitigate multiple sources of variability in low-level assays.
Visualization of Variability Identification and Mitigation
Variability Mitigation Strategy Framework
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for Low-Level Assay Development
| Reagent/Material | Function | Application Examples | Critical Quality Attributes |
|---|---|---|---|
| Reference Standards | Calibration and accuracy assessment | HER2 reference materials for IHC standardization [45] | Well-characterized target concentration, stability |
| High-Sensitivity Detection Kits | Enhanced detection of low-abundance targets | High-sensitivity IHC assays for HER2-low detection [45] | Low detection threshold, wide dynamic range |
| Tissue Microarrays (TMAs) | Multi-sample parallel analysis | CASI-01 study with 80-core TMA for HER2 testing [45] | Well-characterized samples, representation of full expression range |
| Image Analysis Software | Objective quantification of assay results | Automated HER2 scoring to replace pathologist readout [45] | Algorithm accuracy, reproducibility, validation for low levels |
| Quality Control Materials | Ongoing performance monitoring | Statistical process control implementation [45] | Stability, consistency, representative of test conditions |
| Machine Learning Algorithms | Multi-factor performance analysis | Histogram-based Gradient Boosted Trees for test variability analysis [46] | Feature importance testing, model accuracy |
| Automated Assay Development Tools | Streamlined method optimization | PRM scheduling software for targeted proteomics [47] | Integration with instrumentation, optimization algorithms |
The identification and mitigation of variability sources in low-level assays represents a critical frontier in method validation for precision at low concentration levels. As demonstrated by comparative studies across multiple domains, conventional assays developed for high-abundance targets frequently prove inadequate for the precise quantification required by modern therapeutic and diagnostic applications. The integration of enhanced sensitivity methods, reference standards, objective readout technologies, and advanced computational approaches provides a multifaceted strategy for addressing these challenges.
The experimental data and protocols presented in this guide highlight both the substantial nature of the variability problem and the promising pathways toward solutions. From the six-fold improvement in dynamic range achieved through enhanced IHC assays with image analysis [45] to the >5 percentage point sensitivity improvement enabled by machine learning augmentation [46], these approaches demonstrate tangible progress in reducing variability while maintaining specificity. The continued development and implementation of these strategies will be essential for advancing precision medicine, particularly as therapies targeting increasingly low-abundance biomarkers continue to emerge.
As the field evolves, the systematic adoption of robust method validation frameworks specifically designed for low-level assays will be essential. This includes the incorporation of dynamic range as a critical performance parameter, the implementation of statistical process control, and the transition from qualitative to truly quantitative measurement approaches. Through these advances, researchers and drug development professionals can significantly enhance the reliability and reproducibility of low-level assays, ultimately supporting more precise therapeutic decisions and improved patient outcomes.
In the evolving landscape of precision medicine and pharmaceutical development, robustness testing has emerged as a critical component of method validation, particularly for analyses conducted at low concentration levels. Robustness is formally defined as "the ability of a statistical test or model to maintain its accuracy and reliability even when underlying assumptions or conditions are violated, or when data deviates from ideal settings" [48]. In analytical chemistry, this translates specifically to examining "the impact of small, deliberate variations in method parameters, such as changes in column type or temperature, on the reliability of analytical results" [48].
The fundamental importance of robustness stems from a simple but challenging reality: models and methods that perform excellently in controlled, ideal conditions often fail when confronted with the natural variability of real-world applications [49]. This is especially critical in precision medicine, where diagnostic and therapeutic decisions increasingly rely on sophisticated assays measuring biomarkers at minute concentrations [50]. A fragility in these methods can directly impact patient care, leading to misdiagnosis, inappropriate treatment selections, or failure to detect critical biomarkers.
The consequences of inadequate robustness testing are particularly pronounced in two key areas of modern pharmaceutical development. First, in precision oncology, where treatment selection increasingly depends on detecting low-frequency genetic variants or minimal residual disease, non-robust methods can lead to both false negatives (missing actionable mutations) and false positives (subjecting patients to ineffective treatments) [51]. Second, in emerging modalities like LNP-mRNA therapeutics, the complex composition requires multiple pharmacokinetic measurements where robustness becomes multidimensional—ensuring reliability across different analytical targets (encapsulated mRNA, lipid components) and methodological approaches [52].
Core Principles and Definitions
Discipline-Specific Perspectives on Robustness
While the core concept of robustness—maintaining performance under varying conditions—remains consistent, its operational definition and emphasis vary across scientific disciplines relevant to method validation.
Table: Robustness Definitions Across Scientific Disciplines
| Study Field | Definition of Robustness | Primary Focus |
|---|---|---|
| Analytical Chemistry | "Examines the impact of small, deliberate variations in method parameters on the reliability of analytical results" [48] | Method parameter stability |
| Quantitative Research | "Allows researchers to explore the stability of their main estimates to plausible variations in model specifications" [48] | Estimate stability across model specifications |
| Computational Reproducibility | "Modifying analytic choices and reporting their subsequent effects on estimates of interest" [48] | Sensitivity of results to analytical choices |
| Biology | "Evaluates the stability of biological systems across different levels of organization" [48] | System resilience across scales |
| Machine Learning | "Ensuring models stay reliable under messy, unpredictable, or adversarial conditions" [49] | Performance consistency in real-world conditions |
Robustness Versus Related Concepts
It is crucial to distinguish robustness from related methodological qualities, particularly in the context of low-concentration analyses:
- Robustness vs. Accuracy: A method can be accurate under ideal conditions but non-robust if small parameter variations significantly degrade performance [49]. Accuracy measures correctness under optimal conditions; robustness measures consistency under variable conditions.
- Robustness vs. Ruggedness: While sometimes used interchangeably, ruggedness typically refers to a method's resilience to environmental and operational changes between laboratories, instruments, or analysts, whereas robustness specifically addresses deliberate variations in method parameters [48].
- Robustness vs. Sensitivity: Sensitivity measures the ability to detect low concentrations, while robustness ensures this detection capability remains consistent despite methodological variations. A highly sensitive method may be fragile to small parameter changes.
Experimental Framework for Robustness Assessment
Systematic Parameter Variation Strategy
A structured approach to robustness testing involves identifying Critical Method Parameters (CMPs) and systematically varying them within realistic operating ranges. The experimental workflow follows a logical progression from parameter identification through final assessment.
Critical Method Parameters are those variables that, when varied within reasonable boundaries, could significantly impact method performance. For a liquid chromatography method, these typically include:
- Mobile phase pH (±0.1-0.3 units)
- Column temperature (±2-5°C)
- Flow rate (±5-10%)
- Gradient composition (±2-5% absolute)
- Detection wavelength (±2-3 nm for UV/VIS)
The selection of parameters and variation ranges should be based on scientific understanding of the method, prior knowledge of similar methods, and risk assessment of potential failure modes.
Experimental Design and Statistical Analysis
A well-designed robustness study employs statistical principles to efficiently evaluate multiple parameters while minimizing experimental runs. Fractional factorial designs are particularly valuable, allowing assessment of multiple parameters with a practical number of experiments.
For methods with 5-7 critical parameters, a Plackett-Burman design or fractional factorial design can efficiently estimate main effects while assuming interactions are negligible. The statistical analysis focuses on identifying parameters with significant effects on critical quality attributes, typically using analysis of variance (ANOVA) with a predetermined significance level (often α=0.05).
The output of this analysis is a quantitative understanding of which parameters require tight control versus those with wider operating ranges. This directly informs the method's control strategy and helps establish the method design space—the multidimensional combination of parameter ranges where method performance remains acceptable.
Comparative Analysis of Robustness Testing Methods
Statistical Techniques for Robustness Evaluation
Multiple statistical approaches exist for evaluating robustness, each with distinct strengths and applications in method validation.
Table: Statistical Techniques for Robustness Testing
| Technique | Methodology | Key Applications | Advantages | Limitations |
|---|---|---|---|---|
| Sub-sample Analysis [53] | Dividing data into sub-samples by time, demographics, or other factors | Detecting heterogeneity across patient populations or sample types | Reveals context-dependent performance issues | Requires sufficient data for meaningful sub-groups |
| Alternative Model Specifications [53] | Testing different mathematical models or transformations | Comparing linear vs. non-linear relationships in calibration curves | Identifies structural assumptions impacting results | Can over-complicate simple methods |
| Bootstrapping [53] | Resampling with replacement to create pseudo-datasets | Establishing confidence intervals for method parameters when theoretical distributions are unknown | Non-parametric approach, makes minimal assumptions | Computationally intensive for large datasets |
| Sensitivity Analysis [53] | Systematically varying parameters to measure effect size | Identifying which method parameters most impact results | Quantifies parameter importance, informs control strategy | May miss interactive effects between parameters |
Domain-Specific Robustness Considerations
The application of robustness testing varies significantly across different analytical contexts in pharmaceutical development and precision medicine.
Table: Domain-Specific Robustness Considerations
| Analytical Domain | Critical Parameters | Key Quality Attributes | Special Considerations |
|---|---|---|---|
| Chromatographic Methods [54] | Mobile phase pH, column temperature, flow rate, gradient profile | Retention time, peak symmetry, resolution, sensitivity | Column-to-column variability, mobile phase preparation consistency |
| PCR-Based Assays [52] | Primer annealing temperature, Mg²⺠concentration, template quality, enzyme lot | Amplification efficiency, specificity, limit of detection, Cq values | Contamination risks, enzyme stability, inhibition effects |
| LNP-mRNA PK Assays [52] | Sample collection conditions, RT efficiency, extraction recovery, matrix effects | mRNA integrity, accuracy, precision, sensitivity | mRNA stability in biological matrices, LNP stability during storage |
| Multi-omics Biomarkers [50] | Sample preparation, batch effects, normalization methods, platform differences | Reproducibility, classification accuracy, biomarker concordance | Integration across platforms, batch effect correction, data harmonization |
Case Studies in Robustness Testing
Robustness in PCR-Based Bioanalytical Methods
The development of reverse transcription quantitative PCR (RT-qPCR) assays for lipid nanoparticle-messenger RNA (LNP-mRNA) drug products illustrates sophisticated robustness considerations for cutting-edge modalities. These assays require careful attention to multiple technical factors that can impact reliability [52].
Critical robustness parameters for LNP-mRNA assays include:
- One-step vs. two-step RT-qPCR selection, balancing convenience against potential quantification biases
- Primer/probe design considerations, particularly for modified RNA sequences with enhanced stability
- Sample collection and processing conditions to preserve mRNA integrity in biological matrices
- Reference material characterization to ensure consistent quantification across assay runs
The experimental workflow for establishing RT-qPCR robustness involves testing these parameters across their expected operating ranges and measuring effects on critical quality attributes, particularly accuracy, precision, and sensitivity at the method's lower limit of quantification.
Robustness in Precision Medicine Applications
In precision oncology, robustness testing takes on additional dimensions beyond analytical performance. The fundamental concern is whether genomic-guided treatment recommendations remain consistent across different testing platforms, bioinformatic pipelines, and interpretation criteria [51].
A significant challenge in precision medicine is the transition from stratified medicine to true personalized medicine. Current approaches primarily stratify patients based on single biomarkers (e.g., specific mutations), but robust personalized medicine would require integrating multiple biomarker types—genomic, proteomic, metabolomic, histopathological, and clinical—to generate truly individualized predictions [51]. The robustness of such multidimensional models depends on the reliability of each component and their integration.
Recent initiatives highlight the importance of robustness in real-world clinical applications. Studies like the Pioneer 100 Wellness Project have demonstrated the feasibility of collecting dense molecular data, but the "key challenge is to fully integrate these diverse data types, correlate with distinct clinical phenotypes, and extract meaningful biomarker panels for guiding clinical practice" [55]. This integration requires robustness across measurement platforms, time, and patient populations.
Essential Research Reagents and Materials
The experimental evaluation of method robustness relies on carefully selected reagents and reference materials that ensure consistency throughout testing.
Table: Essential Research Reagents for Robustness Testing
| Reagent/Material | Function in Robustness Testing | Critical Quality Attributes | Application Examples |
|---|---|---|---|
| Certified Reference Materials [52] | Provides analytical standard for method qualification | Purity, concentration, stability, molecular weight | PK assays for LNP-mRNA therapeutics [52] |
| Quality-Controlled Enzymes | Ensures consistent reaction efficiency across method variations | Activity, specificity, lot-to-lot consistency | RT-qPCR for low-concentration biomarkers [52] |
| Standardized Biological Matrices | Evaluates matrix effects and selectivity | Composition, consistency, absence of interferents | Biomarker assays in patient samples [56] |
| Chromatographic Columns | Tests separation performance under varied conditions | Retention reproducibility, peak symmetry, pressure stability | HPLC method robustness testing [54] |
| Stabilized Sample Collection Systems [52] | Preserves analyte integrity during method parameter testing | Stabilizer effectiveness, compatibility with detection | Clinical sample collection for mRNA analysis [52] |
Implementation Roadmap and Best Practices
Structured Approach to Robustness Testing
Implementing effective robustness testing requires a systematic approach integrated throughout the method development lifecycle. The following roadmap provides a structured framework:
Early Risk Assessment: Identify potential critical parameters based on method principle, prior knowledge, and preliminary experiments.
Experimental Design Selection: Choose appropriate statistical design (full factorial, fractional factorial, Plackett-Burman) based on the number of parameters and resources.
Controlled Parameter Variation: Systematically vary parameters within predetermined ranges while measuring effects on quality attributes.
Statistical Analysis and Interpretation: Identify statistically significant and practically important effects using appropriate statistical methods.
Design Space Establishment: Define acceptable operating ranges for critical parameters based on empirical results.
Control Strategy Implementation: Incorporate robustness findings into method procedures, system suitability criteria, and training materials.
Continuous Monitoring: Track method performance during routine use to verify robustness and identify potential drift.
Common Pitfalls and Mitigation Strategies
Robustness testing implementation often encounters several challenges that can compromise results:
Overfitting Robustness Checks: Continuously adjusting tests until desired results are achieved, which masks underlying issues. Mitigation: Predefine acceptance criteria and experimental plans before testing begins [53].
Ignoring Data Quality: Conducting sophisticated robustness tests on fundamentally flawed or non-representative data. Mitigation: Implement rigorous data quality assessment before robustness evaluation [53].
Underpowered Experiments: Using insufficient sample sizes or parameter variations to detect practically important effects. Mitigation: Conduct power analysis or use established experimental design principles.
Misinterpreting Null Results: Assuming that non-significant results prove robustness rather than potentially indicating insensitive tests. Mitigation: Include positive controls and evaluate test sensitivity.
The implementation of robustness testing should be viewed as an investment in method reliability rather than a regulatory checkbox. As noted in machine learning contexts, "Robustness isn't built once. It's achieved through iterative testing, monitoring, and refinement" [49]. This iterative approach applies equally to analytical method development, particularly for methods supporting critical decisions in precision medicine and drug development.
Robustness testing represents a fundamental pillar of method validation, ensuring analytical reliability under the realistic variations encountered during routine application. For precision medicine applications—particularly those involving low-concentration biomarkers or complex therapeutic modalities like LNP-mRNA products—comprehensive robustness assessment is not optional but essential for generating trustworthy data.
The systematic evaluation of critical method parameters through structured experimental designs provides a scientific basis for establishing method design spaces and control strategies. This approach moves beyond simply verifying that a method works under ideal conditions to understanding how it behaves across its anticipated operational range.
As precision medicine continues its evolution from genetics-guided stratification toward truly personalized approaches integrating multi-omics data, environmental factors, and clinical parameters [55] [51], the importance of robustness will only increase. The successful implementation of these advanced precision medicine paradigms will depend fundamentally on the reliability of the underlying analytical methods across diverse populations, testing environments, and timepoints in the patient journey.
Therefore, robustness testing should be embraced as a core scientific discipline within method validation—one that provides the foundation for confident application of analytical methods in both regulatory decision-making and clinical practice.
Strategies for Improving Signal-to-Noise Ratio and Recovery at the LOQ
In analytical method validation, the Limit of Quantitation (LOQ) represents the lowest analyte concentration that can be quantitatively measured with acceptable precision and accuracy, crucial for reliable data in pharmaceutical development and bioanalysis [10]. Achieving robust performance at the LOQ requires optimizing the signal-to-noise ratio (S/N) and ensuring high analyte recovery, particularly from complex matrices like biological fluids [10] [57]. This guide compares established and emerging strategies to enhance these critical parameters, providing researchers with a structured framework for method optimization.
Comparative Analysis of Improvement Strategies
The table below summarizes the core strategies for improving S/N and recovery, comparing their key principles, typical applications, and inherent advantages or challenges.
| Strategy | Key Principle | Typical Application Context | Advantages & Challenges |
|---|---|---|---|
| Sample Pre-concentration [58] | Increases the absolute amount of analyte entering the analytical system. | Trace analysis in environmental samples (e.g., water), bioanalysis. | Advantage: Directly increases signal amplitude. Challenge: Potential for analyte loss or contamination during extra step. |
| Matrix-Matched Calibration (EC) [57] | Uses standards in a simulated sample matrix to correct for matrix-induced signal suppression or enhancement. | Analysis of complex matrices like virgin olive oil, biological fluids. | Advantage: Compensates for matrix effect, improving accuracy and effective recovery. Challenge: Requires a suitable, representative blank matrix. |
| Internal Standard Calibration (IC) [57] | Uses a chemically similar internal standard to correct for losses during sample preparation and instrument variability. | GC, LC, and MS analyses where precise quantification is critical. | Advantage: Corrects for both preparation and instrumental variance. Challenge: Requires careful selection of an appropriate internal standard. |
| Standard Addition Calibration (AC) [57] | Analyte is spiked at known concentrations into the actual sample, circumventing matrix effects. | Cases of strong or variable matrix effects where a blank matrix is unavailable. | Advantage: Highly accurate for specific sample. Challenge: Time-consuming; requires a separate calibration for each sample. |
| Instrument & Parameter Optimization [58] | Adjusting detector settings, injection volume, or using more sensitive instrumentation. | Universal, but particularly critical when operating near an instrument's detection capability. | Advantage: Directly improves S/N by increasing signal or reducing noise. Challenge: May require access to advanced instrumentation (e.g., HPLC-MS/MS). |
Detailed Experimental Protocols for Key Strategies
Protocol for External Matrix-Matched Standard Calibration
This protocol, adapted from research on volatile compounds in olive oil, is critical for achieving accurate recovery by compensating for matrix effects [57].
- Materials: Refined olive oil (or other appropriate blank matrix), pure analyte standards, appropriate solvents (e.g., ethyl acetate), dynamic headspace (DHS) sampler, Gas Chromatograph with Flame Ionization Detector (GC-FID).
- Procedure:
- Prepare Stock Solution: Dissolve the pure analyte in a suitable solvent to create a concentrated stock solution.
- Spike the Matrix: Serially dilute the stock solution using the refined olive oil matrix to create a calibration curve. The studied range was 0.1 to 10.5 mg/kg, with 14 concentration points [57].
- Sample Analysis: Analyze each matrix-matched standard in triplicate using the DHS-GC-FID method.
- Data Processing: Construct a calibration curve by plotting the peak areas against the known concentrations.
- Quantification: Interpolate the signals from unknown samples against this matrix-matched calibration curve to determine their concentration, which accounts for matrix-based recovery issues.
Protocol for Signal-to-Noise Ratio Calculation and Improvement
This method is foundational for establishing and optimizing the LOQ, defined as a S/N of 10:1 [10] [58].
- Materials: Blank sample (matrix without analyte), low-concentration analyte sample near the expected LOQ, analytical instrument (e.g., HPLC with UV detector).
- Procedure:
- Analyze Blank: Inject the blank sample and record the chromatogram. Measure the baseline noise (N). This can be the standard deviation (σ) of the blank signal or the peak-to-peak noise over a region equivalent to 20 times the peak width at half-height [10] [59].
- Analyze Low-Level Standard: Inject a sample with analyte concentration near the LOQ and record the analyte signal (S).
- Calculate S/N: Use the formulas ( \text{LOD} = 3 \times \frac{\sigma}{S} ) and ( \text{LOQ} = 10 \times \frac{\sigma}{S} ), where σ is the standard deviation of the blank and S is the mean signal of the low-level standard [58]. Alternatively, for chromatographic peaks, ( \text{S/N} = \frac{2H}{h} ), where H is the peak height and h is the peak-to-peak noise in a blank chromatogram [59].
- Improvement Actions: If the S/N is insufficient for a precise LOQ (i.e., below 10:1), employ strategies like sample pre-concentration (e.g., solid-phase extraction, evaporation) or instrument optimization (e.g., increasing injection volume, using a more sensitive detector like MS/MS) [58].
Protocol for Accuracy Profile Using Uncertainty and Tolerance Intervals
This advanced statistical graphical approach provides a rigorous assessment of method validity, including the LOQ, by considering both total error (bias + precision) [15].
- Materials: Validated analytical method, quality control (QC) samples at multiple concentration levels, including levels near the expected LOQ.
- Procedure:
- Define Acceptance Limits (λ): Set predefined accuracy limits (e.g., ±30% for LOQ levels, ±15% for higher concentrations) [10].
- Analyze QC Samples: Run a minimum of three series with duplicates per concentration level under intermediate precision conditions [15].
- Calculate Tolerance Intervals: For each concentration level, compute the two-sided β-content γ-confidence tolerance interval (e.g., β=90%, γ=95%), which defines the interval where a specified proportion of future results will fall [15].
- Construct the Profile: Plot the tolerance intervals (or expanded measurement uncertainty) against the concentration levels, overlaying the acceptance limits.
- Determine LOQ: The LOQ is the lowest concentration where the entire tolerance interval falls within the predefined acceptance limits, ensuring reliable quantification with stated accuracy and precision [15].
Strategic Decision Pathway for Method Improvement
The following diagram illustrates a logical workflow for selecting the most appropriate strategy based on the primary challenge encountered during method development.
Strategic Decision Workflow for LOQ Improvement
The Scientist's Toolkit: Key Research Reagent Solutions
The table below lists essential materials and their functions for implementing the strategies discussed in this guide.
| Item / Reagent | Primary Function in LOQ Improvement |
|---|---|
| Refined/Blank Matrix [57] | Serves as the base for preparing external matrix-matched calibration standards to correct for matrix effects and improve accuracy. |
| Pure Analyte Standards [57] | Used to create calibration curves in method development and for spiking in recovery experiments and standard addition. |
| Chemically Analogous Internal Standard [57] | Corrects for analyte loss during sample preparation and instrument variability, improving precision and accuracy. |
| Solid-Phase Extraction (SPE) Cartridges [58] | Used for sample clean-up and pre-concentration to increase the analyte concentration and reduce interfering matrix components. |
| Appropriate Solvents (e.g., Ethyl Acetate, Methanol) [57] [60] | Used for dissolving standards, sample extraction, and reconstitution, ensuring compatibility and high recovery. |
Selecting the optimal strategy for improving S/N and recovery at the LOQ depends on a clear diagnosis of the underlying issue, whether it is low signal, high noise, poor recovery, or significant matrix effects. External matrix-matched calibration offers a robust, general-purpose solution for many matrix-related challenges, while internal standardization is critical for correcting procedural variances. For the most challenging low-level quantitation, advanced statistical tools like the accuracy profile provide a comprehensive framework for defining a reliable and validated LOQ. By systematically applying these strategies, scientists can ensure their analytical methods meet the rigorous demands of precision and accuracy required in drug development and other critical research fields.
Managing Sample and Reagent Stability to Minimize Pre-Analytical Error
In the realm of method validation for precision at low concentration levels, managing pre-analytical variables represents a fundamental challenge that directly impacts data reliability, reproducibility, and clinical or research outcomes. Pre-analytical errors, encompassing all processes from sample collection to analysis, constitute a staggering 63.6-98.4% of all laboratory errors [61] [62], with unsuitable sample handling leading to unreliable results that compromise scientific conclusions and clinical decisions [63]. For researchers and drug development professionals working with low-concentration analytes, even minor degradation in sample or reagent integrity can disproportionately affect precision, potentially invalidating critical findings.
The stability of biological samples and analytical reagents is not merely a procedural concern but a foundational element of analytical validity. Contemporary studies demonstrate that coagulation factors like FV can degrade by up to 60% within 24 hours at room temperature [63], while biotherapeutics and vaccines exhibit complex degradation kinetics that traditional stability models often fail to predict accurately [64]. Within this context, this guide objectively compares established and emerging approaches to stability management, providing experimental frameworks to bolster precision in low-concentration method validation.
Comparative Analysis of Stability Management Approaches
The following analysis compares three distinct methodological approaches to stability management, evaluating their core principles, implementation requirements, and suitability for different research contexts.
Table 1: Comparison of Stability Management Approaches
| Approach | Core Principle | Data Requirements | Implementation Complexity | Best Suited Applications |
|---|---|---|---|---|
| Traditional Guideline-Based | Fixed stability criteria based on population data [63] | Historical stability data; guideline references (e.g., CLSI H-21) [63] | Low | Routine clinical assays; established biomarkers; quality control testing |
| Advanced Kinetic Modeling (AKM) | Arrhenius-based prediction from accelerated degradation studies [64] | Stability data from ≥3 temperatures; significant degradation (>20%) at high temperatures [64] | High | Biotherapeutics; vaccines; novel biomarkers; precision-critical assays |
| Factorial Design | Statistical identification of critical stability factors [65] | Controlled experimental data across multiple factor levels | Medium | Formulation screening; reagent development; method optimization |
Traditional Guideline-Based Stability Assessment
The guideline-based approach establishes fixed stability criteria derived from population studies and consensus documents. This method provides clear, actionable protocols for sample handling but may lack precision for novel analytes or specialized conditions.
Supporting Experimental Data: Studies validating this approach demonstrate that plasma for PT testing remains stable for 24 hours at room temperature or 24 hours refrigerated (2-8°C), while aPTT stability is limited to 4-8 hours under the same conditions [63]. Coagulation factors exhibit variable degradation, with FVIII and FIX activities remaining stable for ≤2 and ≤4 hours respectively at both 4°C and 25°C, while FV degrades rapidly with changes exceeding 60% after 24 hours at 25°C [63]. For long-term storage, samples maintain stability for up to 3 months at ≤-20°C and up to 18 months at ≤-70°C with degradation limited to <10% from fresh plasma values [63].
Advanced Kinetic Modeling (AKM) for Predictive Stability
AKM represents a paradigm shift from fixed stability criteria to compound-specific, mathematically-derived predictions. This approach employs phenomenological kinetic models that describe complex degradation pathways through Arrhenius-based parameters, enabling accurate shelf-life predictions from short-term accelerated stability studies [64].
Experimental Validation Protocol: The methodology requires:
- Accelerated Stability Studies: Samples are subjected to a minimum of three incubation temperatures (e.g., 5°C, 25°C, and 37°C/40°C) [64].
- Substantial Degradation Induction: A significant degradation (typically >20% of the measured attribute) must be achieved at elevated temperatures, exceeding the degradation expected at the end of shelf life under recommended storage conditions [64].
- High-Frequency Data Collection: A minimum of 20-30 experimental data points are collected across the temperature spectrum to ensure robust model fitting [64].
- Model Selection and Validation: Multiple kinetic models are screened using statistical parameters (Akaike Information Criterion - AIC, Bayesian Information Criterion - BIC), with the optimal model selected for its ability to accurately predict long-term stability under recommended storage conditions [64].
Comparative Performance Data: When applied to monoclonal antibodies (mAbs) and vaccines, AKM demonstrates exceptional predictive accuracy, with stability forecasts of up to 3 years showing excellent agreement with real-time experimental data [64]. This approach significantly outperforms traditional ICH-based methods, particularly for complex biomolecules with non-linear degradation patterns [64].
Factorial Design for Stability Study Optimization
Factorial analysis provides a strategic framework for identifying critical stability factors while reducing experimental burden. This statistical approach systematically evaluates multiple variables (e.g., batch, orientation, filling volume, drug substance supplier) to determine their individual and interactive effects on stability [65].
Experimental Implementation: Research demonstrates that applying factorial analysis to accelerated stability data enables researchers to identify worst-case scenarios and strategically reduce long-term stability testing by up to 50% without compromising reliability [65]. This approach has been successfully validated for parenteral dosage forms, including iron complexes and biologic solutions, where factors such as primary packaging and drug substance supplier were identified as critical stability factors [65].
Standardized Framework for Stability Assessment
The Stability Toolkit for the Appraisal of Bio/Pharmaceuticals' Level of Endurance (STABLE) provides a standardized framework for systematic stability assessment across five stress conditions: oxidative, thermal, acid-catalyzed hydrolysis, base-catalyzed hydrolysis, and photostability [66]. This tool employs a color-coded scoring system to quantify and compare stability, facilitating consistent evaluation across different compounds and laboratories.
Table 2: STABLE Framework Evaluation Criteria for Hydrolytic Degradation
| Stress Condition | Experimental Parameters | Stability Evaluation | High Stability Threshold |
|---|---|---|---|
| Acid-Catalyzed Hydrolysis | HCl concentration (0.1-1M), time, temperature, % degradation [66] | Scores based on degradation under progressive conditions | ≤10% degradation in >5M HCl for 24h under reflux [66] |
| Base-Catalyzed Hydrolysis | NaOH concentration (0.1-1M), time, temperature, % degradation [66] | Points assigned for resistance to alkaline conditions | Stable in 5M NaOH for 24h under reflux [66] |
| Oxidative Stability | Oxidizing agent concentration, time, temperature, % degradation | Relative resistance to oxidative stress | Minimal degradation under standard oxidative conditions |
| Thermal Stability | Temperature, time, % degradation | Maintenance of integrity at elevated temperatures | Minimal degradation at 40-60°C for 4 weeks |
| Photostability | Light intensity, wavelength, time, % degradation | Resistance to photodegradation | Minimal degradation under ICH Q1B conditions |
The following workflow diagram illustrates the strategic implementation of these stability assessment approaches within a method validation framework:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials represent critical components for conducting robust stability studies in method validation research.
Table 3: Essential Research Reagent Solutions for Stability Studies
| Reagent/Material | Function in Stability Assessment | Application Notes |
|---|---|---|
| Sample Release Reagents | Enable extraction of target molecules from complex matrices for stability analysis [67] | Critical for DNA, RNA, and protein stability studies; select based on extraction efficiency |
| Stress Testing Reagents | Induce controlled degradation for forced degradation studies [66] | Include HCl/NaOH (hydrolysis), Hâ‚‚Oâ‚‚ (oxidation); use high-purity grades |
| Stabilizing Additives | Inhibit specific degradation pathways in sample matrices | Protease inhibitors (protein stability), RNase inhibitors (RNA stability), antioxidants |
| Reference Standards | Provide benchmarks for quantifying degradation in stability studies | Use certified reference materials with documented stability profiles |
| Quality Control Materials | Monitor analytical performance throughout stability study | Should mimic test samples and cover measuring interval |
Effective management of sample and reagent stability is not a standalone activity but an integral component of method validation for precision at low concentration levels. The comparative data presented demonstrates that while traditional guideline-based approaches provide practical frameworks for established assays, advanced methods like AKM and factorial design offer superior predictive capability and efficiency for novel compounds and precision-critical applications. By implementing the standardized protocols, experimental frameworks, and reagent management strategies outlined in this guide, researchers can significantly reduce pre-analytical errors, enhance data reliability, and strengthen the scientific validity of their analytical methods across drug development and clinical research applications.
The Validation Blueprint: From Protocol to Report and Comparative Analysis
Developing a Comprehensive Validation Protocol with Pre-Defined Acceptance Criteria
Analytical method validation is a critical process in pharmaceutical development that provides documented evidence that a method is suitable for its intended purpose. In regulated environments, this process establishes, through laboratory studies, that the performance characteristics of the method meet requirements for analytical applications, ensuring reliability during normal use [2]. For precision at low concentration levels, establishing scientifically sound acceptance criteria becomes particularly crucial, as traditional measures of analytical goodness may fail to adequately demonstrate method suitability.
The validation process encompasses multiple performance characteristics that must be evaluated through structured experimental protocols. Governmental and regulatory agencies including the FDA and International Conference on Harmonization (ICH) have issued guidelines outlining requirements for method validation, with the USP designating legally recognized specifications for determining compliance with the Federal Food, Drug, and Cosmetic Act [2]. A well-defined and documented validation process not only demonstrates method suitability but also facilitates method transfer and regulatory compliance.
Core Validation Parameters and Acceptance Criteria
Defining Validation Performance Characteristics
Analytical method validation requires systematic evaluation of multiple interdependent performance parameters. These "Eight Steps of Analytical Method Validation" form the foundation of a comprehensive protocol [2]:
Figure 1. Analytical Method Validation Parameters Hierarchy.
Acceptance Criteria Framework for Precision at Low Concentrations
Establishing appropriate acceptance criteria requires moving beyond traditional measures like percentage coefficient of variation (%CV) and evaluating method performance relative to product specification limits. This tolerance-based approach is particularly critical for methods measuring low concentration levels where traditional metrics may be misleading [68].
Table 1. Recommended Acceptance Criteria for Low Concentration Assays
| Parameter | Traditional Approach | Tolerance-Based Approach | Recommended Criteria |
|---|---|---|---|
| Accuracy/Bias | % Recovery = (Measured/Standard)×100 | Bias % Tolerance = (Bias/Tolerance)×100 | ≤10% of Tolerance [68] |
| Repeatability | % RSD or CV = (Stdev/Mean)×100 | Repeatability % Tolerance = (Stdev×5.15)/(USL-LSL) | ≤25% of Tolerance (≤50% for bioassays) [68] |
| Specificity | Visual peak separation | Specificity/Tolerance ×100 | Excellent: ≤5%, Acceptable: ≤10% [68] |
| LOD | Signal-to-Noise (3:1) | LOD/Tolerance ×100 | Excellent: ≤5%, Acceptable: ≤10% [68] |
| LOQ | Signal-to-Noise (10:1) | LOQ/Tolerance ×100 | Excellent: ≤15%, Acceptable: ≤20% [68] |
For precision at low concentrations, the tolerance-based approach prevents the false indication that a method is performing poorly at low concentrations when it is actually performing excellently relative to the specification limits [68]. Conversely, at high concentrations, traditional %CV may indicate acceptable performance when the method is actually unsuitable for the intended product specifications.
Experimental Protocols for Validation Parameters
Accuracy and Precision Assessment
Accuracy is measured as the closeness of agreement between an accepted reference value and the value found in a sample, established across the method range [2]. For drug substances, accuracy measurements are obtained by comparison to a standard reference material or well-characterized method. For drug products, accuracy is evaluated by analyzing synthetic mixtures spiked with known quantities of components.
Experimental Protocol for Accuracy:
- Collect data from minimum of nine determinations over at least three concentration levels covering specified range
- Report as percent recovery of known, added amount, or difference between mean and true value with confidence intervals
- For low concentrations, apply tolerance-based criteria: Bias % of Tolerance ≤10% [68]
Precision encompasses three measurements: repeatability (intra-assay precision), intermediate precision (within-laboratory variations), and reproducibility (between laboratories) [2].
Experimental Protocol for Precision:
- Repeatability: Analyze minimum of nine determinations covering specified range (three concentrations, three repetitions each) or six determinations at 100% of test concentration
- Intermediate Precision: Use experimental design with different days, analysts, or equipment; two analysts prepare and analyze replicate samples using different HPLC systems
- Reproducibility: Collaborative studies between different laboratories using same experimental design
- Report as %RSD, with acceptance criteria of ≤25% of tolerance for repeatability [68]
Specificity, LOD/LOQ, and Linearity Protocols
Specificity ensures the method accurately measures the analyte in the presence of other components [2]. For chromatographic methods, specificity is demonstrated by resolution of closely eluted compounds and through peak purity tests using photodiode-array (PDA) detection or mass spectrometry (MS).
Experimental Protocol for Specificity:
- For identification: demonstrate ability to discriminate between compounds or compare to known reference materials
- For assay and impurity tests: show resolution of two most closely eluted compounds (typically major component and closely eluted impurity)
- Spike samples with available impurities/excipients and demonstrate assay unaffected
- Use PDA or MS detection for peak purity assessment
- Apply acceptance criteria: Specificity/Tolerance ×100 ≤10% [68]
Limits of Detection (LOD) and Quantitation (LOQ) establish the lowest concentrations detectable and quantifiable with acceptable precision and accuracy [2].
Experimental Protocol for LOD/LOQ:
- Determine via signal-to-noise ratios (3:1 for LOD, 10:1 for LOQ) or calculate using formula: LOD/LOQ = K(SD/S) where K=3 for LOD, 10 for LOQ; SD=standard deviation of response; S=slope of calibration curve
- Analyze appropriate number of samples at the calculated limit to validate method performance
- Apply acceptance criteria: LOD/Tolerance ×100 ≤10%; LOQ/Tolerance ×100 ≤20% [68]
Linearity and Range establish the method's ability to provide results proportional to analyte concentration within a defined interval [2].
Experimental Protocol for Linearity and Range:
- Evaluate using minimum of five concentration levels within specified range
- For assay of drug substance/drug product, range typically 80-120% of test concentration
- Report equation for calibration curve, coefficient of determination (r²), residuals, and the curve itself
- For low concentrations, extend range to include levels approaching LOD/LOQ
Comparative Method Performance Data
Traditional vs. Tolerance-Based Approach Comparison
Evaluating method performance using tolerance-based criteria rather than traditional metrics provides a more meaningful assessment of suitability for low concentration analysis.
Table 2. Method Performance Comparison at Low Concentration Levels
| Method Characteristic | Traditional Assessment | Tolerance-Based Assessment | Impact on OOS Rates |
|---|---|---|---|
| Repeatability (5% concentration) | %CV = 15% (appears poor) | %Tolerance = 20% (acceptable) | Low OOS risk despite high %CV |
| Accuracy at LLOQ | %Recovery = 85% (appears unacceptable) | %Margin = 8% (acceptable) | Suitable for intended use |
| Specificity with matrix interference | Resolution <2.0 (appears poor) | Interference ≤5% tolerance (acceptable) | Minimal impact on decision making |
| Linearity near LOD | R² = 0.985 (appears marginal) | Residuals ≤15% tolerance (acceptable) | Reliable detection at low levels |
The tolerance-based approach directly correlates method performance with its impact on out-of-specification (OOS) rates, providing a direct link between method error and product quality decisions [68]. Methods with excessive error will directly impact product acceptance OOS rates and provide misleading information regarding product quality.
Experimental Data for Precision at Low Concentrations
Experimental data demonstrates the critical relationship between method precision and capability at low concentration levels. The following data illustrates how method repeatability impacts OOS rates in parts per million (PPM), particularly relevant for precision at low concentrations.
Figure 2. Method Error Impact on Product Quality Decisions.
As method repeatability error increases, the OOS rate increases correspondingly [68]. For low concentration analyses, maintaining repeatability ≤25% of tolerance is essential for controlling OOS rates while ensuring accurate measurement of the analyte.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful validation of methods for precision at low concentrations requires specific, high-quality materials and reagents. The following toolkit outlines essential components for method validation experiments.
Table 3. Essential Research Reagent Solutions for Validation Studies
| Reagent/Material | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Reference Standard | Accuracy assessment; calibration curve establishment | Certified purity; stability; properly characterized |
| System Suitability Solutions | Verify system performance before validation runs | Precise composition; consistent response; stability |
| Placebo/Matrix Blanks | Specificity evaluation; interference assessment | Representative composition; analyte-free |
| Known Impurities/Related Substances | Specificity and LOD/LOQ determination | Certified identity and purity; stability |
| Sample Preparation Solvents | Extraction and dilution of low concentration samples | Appropriate purity; compatibility with method |
| Mobile Phase Components | Chromatographic separation | HPLC grade; low UV cutoff; specified pH |
| Stability Solutions | Evaluate method robustness under various conditions | Controlled storage conditions; documented preparation |
Regulatory Framework and Guidance Integration
Method validation must align with regulatory guidance from organizations including FDA, ICH, and USP. While ICH Q2 discusses what to quantify and report with implied acceptance criteria, USP <1225> emphasizes that acceptance criteria should be consistent with the method's intended use [68] [2]. USP <1033> further recommends justifying acceptance criteria based on the risk that measurements may fall outside product specifications [68].
The ICH Q9 Quality Risk Management guidance provides the framework for establishing acceptance criteria based on method impact on product quality decisions [68]. This risk-based approach is particularly important for methods measuring low concentration levels, where the relationship between method performance and product quality must be clearly established.
For precision at low concentrations, the integration of tolerance-based acceptance criteria with traditional performance parameters provides a comprehensive approach that ensures method suitability while maintaining regulatory compliance. This integrated approach directly addresses the challenges of low concentration analysis while providing documented evidence of method reliability throughout the product lifecycle.
Establishing a System Suitability Test (SST) to Ensure Ongoing Precision
System Suitability Testing (SST) serves as a critical quality control measure in analytical chromatography, verifying that the complete analytical system—comprising instrument, column, reagents, and software—is functioning within predefined performance limits immediately before sample analysis [69]. Unlike method validation, which proves a method is reliable in theory, SST demonstrates that a specific instrument on a specific day can generate high-quality data according to the validated method's requirements [69]. This distinction is crucial for maintaining ongoing precision in pharmaceutical analysis and drug development, particularly for methods measuring compounds at low concentration levels.
SST represents a proactive quality assurance measure that prevents wasted effort and protects data integrity by identifying system issues before sample analysis proceeds [69]. Regulatory agencies like the FDA, KFDA, and TGA mandate SST for regulated analyses, with pharmacopeias such as the United States Pharmacopoeia (USP) and European Pharmacopoeia providing specific guidelines for implementation [70] [71] [72]. The test is performed by injecting a reference standard and measuring the system's response against predefined acceptance criteria derived from method validation studies [69].
Critical SST Parameters for Precision Assessment
Comprehensive Parameter Table
System suitability evaluates multiple chromatographic parameters that collectively ensure analytical precision. The table below summarizes the key parameters, their definitions, and typical acceptance criteria:
| Parameter | Definition | Role in Precision | Typical Acceptance Criteria |
|---|---|---|---|
| Precision/Repeatability | Agreement between successive measurements from multiple injections of standard [70] | Ensures instrument provides consistent, reproducible results [69] | %RSD ≤2.0% for 5-6 replicates [70] |
| Resolution (Rs) | Degree of separation between two adjacent peaks [69] | Prevents co-elution interfering with accurate quantification [73] | Rs ≥1.5 between critical pairs [72] |
| Tailing Factor (T) | Measure of peak symmetry [69] | Affects integration accuracy and quantification [70] | 0.8 to 1.8 (USP general range) [72] |
| Theoretical Plates (N) | Column efficiency index [73] | Measures column performance and separation effectiveness [69] | Method-specific, e.g., N ≥4000 [72] |
| Signal-to-Noise Ratio (S/N) | Ratio of analyte signal to background noise [70] | Ensures detection capability at low concentrations [74] | S/N ≥10 for quantitation limit [72] |
| Capacity Factor (k') | Measure of compound retention [70] | Confirms appropriate retention and separation window [72] | Method-specific, established during validation [70] |
Parameter Selection Methodology
Selecting appropriate SST parameters depends on the analytical method's purpose. For assay methods, precision, tailing factor, and theoretical plates are typically included [72]. For impurity methods, resolution between critical pairs and signal-to-noise ratio for sensitivity determination become essential [72]. A robust SST should include at least two chromatographic parameters, with resolution mandatory when analyzing compounds with closely-eluting impurities [72].
The United States Pharmacopoeia (USP) General Chapter <621> provides regulatory guidance on SST parameters, with recent updates effective May 2025 enhancing requirements for system sensitivity (signal-to-noise ratio) and peak symmetry [71]. These changes reflect the ongoing harmonization between USP, European Pharmacopoeia, and Japanese Pharmacopoeia, emphasizing the global consensus on SST importance for ensuring data reliability [71].
SST Establishment and Experimental Protocol
Systematic Workflow for SST Implementation
The following diagram illustrates the comprehensive workflow for establishing and implementing System Suitability Testing:
SST Establishment and Implementation Workflow outlines the systematic process from method development through routine analysis.
Step-by-Step Experimental Protocol
Define SST Parameters During Method Validation: Select parameters based on method type (assay, impurity, content uniformity) [72]. For impurity methods with closely-eluting compounds, include resolution. Include column efficiency (theoretical plates) or tailing factor in all SST protocols [72].
Establish Acceptance Criteria Using Historical Data: Set criteria based on trend data from multiple method validation batches [72]. For precision, require %RSD ≤2.0% for 5-6 replicate injections of a standard solution [70]. For signal-to-noise ratio at the quantitation limit, require S/N ≥10 [72].
Prepare SST Solution: Use a reference standard or certified reference material qualified against primary standards [70]. The concentration should be representative of typical samples—for impurity methods, include a sensitivity solution at the quantitation limit [72]. Dissolve in mobile phase or similar solvent concentration to samples [70].
Perform System Suitability Test: Inject the SST solution in 5-6 replicates to assess precision [70]. For long analytical runs, perform SST at both beginning and end to monitor system performance over time [73].
Evaluate Results Against Criteria: Modern chromatography data systems automatically calculate SST parameters and compare them against predefined acceptance criteria [69]. Document all results, including any deviations.
Take Action Based on Outcome: If the system passes SST, proceed with sample analysis. If SST fails, immediately halt the run and begin troubleshooting [69]. Identify and correct the root cause (e.g., column degradation, mobile phase issues, instrument malfunctions) before re-running SST [69].
Essential Research Reagent Solutions
The following research reagents are fundamental for establishing and performing robust System Suitability Tests:
| Reagent/Material | Function in SST | Critical Specifications |
|---|---|---|
| Reference Standard | Primary SST component; assesses system performance [70] | High purity; qualified against primary standard; not from same batch as test samples [70] |
| SST Marker | Contains all analytes for comprehensive system assessment [72] | Includes critical peak pairs for resolution; stable; cost-effective [72] |
| Chromatography Column | Stationary phase for separation | Method-specific dimensions and chemistry; documented performance history |
| Mobile Phase Components | Liquid carrier for chromatographic separation | HPLC-grade solvents; fresh preparation; filtered and degassed |
| SST Solution Solvent | Dissolution medium for SST standard | Mobile phase or equivalent solvent system [70] |
Regulatory Framework and Compliance
System Suitability Testing is embedded within a strict regulatory framework. Regulatory agencies explicitly state that if an assay fails system suitability, the entire run is discarded, and no sample results are reported other than the failure itself [70]. This underscores the critical role of SST in protecting data integrity.
SST should not be confused with Analytical Instrument Qualification (AIQ). While AIQ proves the instrument operates as intended by the manufacturer across defined operating ranges, SST verifies that the specific method works correctly on the qualified system at the time of analysis [70]. Both are essential, with AIQ forming the foundation for reliable SST performance [70].
The USP General Chapter <621> specifically addresses chromatography and outlines allowable adjustments to methods to achieve system suitability without full revalidation [71]. Recent updates to this chapter emphasize the pharmacopeia's ongoing commitment to refining SST requirements to ensure analytical precision, particularly for methods detecting low concentration compounds [71].
Advanced Applications for Low-Level Concentration Analysis
For methods quantifying impurities or degradation products at low concentration levels, establishing appropriate detectability criteria in SST is paramount. A scientific approach involves using statistical tolerance intervals based on signal-to-noise ratio data collected during method validation [74] [75].
This advanced methodology involves:
- Performing replicate injections (n≥6) of samples at the limit of quantitation (LOQ) concentration during method validation
- Calculating the peak area to noise ratio for each injection
- Determining a one-sided lower tolerance limit using statistical methods
- Setting this calculated value as the SST system sensitivity criterion for all future analyses [75]
This approach provides a statistically sound basis for ensuring the system can reliably detect and quantify low-level compounds, addressing the challenge that instruments may perform differently while maintaining the original validated method's performance claims [75]. For impurity methods, this detectability SST criterion serves as an independent check that the system performance has not deteriorated beyond what was demonstrated in the original validation [74].
When developing SST for impurity methods, include resolution between the active ingredient and its closest-eluting impurity, tailing factor for the main analyte, and signal-to-noise ratio for the quantitation limit solution [72]. This comprehensive approach ensures the system can adequately separate, detect, and quantify both major and minor components throughout the method's lifetime.
Applying the Analytical Procedure Lifecycle Concept from ICH Q14
The International Council for Harmonisation (ICH) Q14 guideline, titled "Analytical Procedure Development," represents a fundamental evolution in pharmaceutical analysis. Published in its final version in November 2023 and effective since June 2024, this guideline introduces a systematic framework for developing and maintaining analytical procedures throughout their entire lifecycle [27] [76]. Together with the revised ICH Q2(R2) on validation, ICH Q14 moves the pharmaceutical industry from a prescriptive, "check-the-box" approach to a scientific, risk-based lifecycle model [27]. This paradigm shift emphasizes building quality into analytical methods from the very beginning rather than treating validation as a one-time event before routine use [77].
The core principle of ICH Q14 is to ensure that analytical methods remain "fit for purpose"—possessing the requisite specificity, accuracy, and precision over their intended range throughout their commercial application [78]. This guideline applies to analytical procedures used for release and stability testing of commercial drug substances and products, both chemical and biological/biotechnological, and can also be applied to other procedures within the control strategy following a risk-based approach [76]. For researchers and drug development professionals, understanding and implementing this lifecycle concept is crucial for ensuring long-term method reliability, particularly for challenging applications such as precision at low concentration levels.
Core Principles of the Analytical Procedure Lifecycle
The Foundation: Analytical Target Profile (ATP)
The Analytical Target Profile (ATP) serves as the cornerstone of the lifecycle approach [79]. It is a prospective summary that describes the intended purpose of an analytical procedure and its required performance characteristics [27]. By defining what the method needs to achieve before determining how to achieve it, the ATP ensures the method is designed to be fit-for-purpose from the outset [27].
For a quantification test, an ATP typically defines the required precision and accuracy. For example, it might state: "The test method must be able to quantify the active substance X in the presence of Y1, Y2,... over the range from A% to B% of the target concentration in the dosage form, with a precision of less than C% RSD, and an accuracy of less than D% error" [77]. This clear definition of requirements guides the entire development process and provides a benchmark for evaluating method performance throughout its lifecycle.
Traditional vs. Enhanced Approaches
ICH Q14 delineates two pathways for analytical procedure development:
- Traditional Approach: Follows minimal requirements, including identifying attributes requiring testing, selecting suitable technology, defining performance characteristics, and documenting the procedure [78].
- Enhanced Approach: Incorporates additional elements such as an ATP, structured risk assessments, multivariate experiments, and a defined analytical control strategy [78]. This approach provides greater scientific understanding and offers more regulatory flexibility for post-approval changes.
The enhanced approach aligns with Analytical Quality by Design (AQbD) principles, using systematic experimentation and risk management to establish a more robust method foundation [79]. This is particularly valuable for methods requiring high precision at low concentrations, where understanding parameter interactions is crucial.
Lifecycle Management and Continuous Improvement
A fundamental concept in ICH Q14 is that analytical procedure validation is not a one-time event but a continuous process that begins with method development and continues throughout the method's entire commercial application [27]. This includes managing post-approval changes through a science- and risk-based approach rather than through extensive regulatory filings [27]. The lifecycle concept enables continuous monitoring and improvement of method performance, ensuring methods remain robust as manufacturing processes evolve and new product variants emerge.
Table 1: Key Terminology in ICH Q14 Analytical Procedure Lifecycle
| Term | Definition | Significance in Lifecycle Approach |
|---|---|---|
| Analytical Target Profile (ATP) | A prospective summary of the analytical procedure's requirements and performance criteria [27] | Defines target method performance before development begins |
| Analytical Procedure Control Strategy | Set of controls from understanding of analytical procedure, including risk assessment and robustness [78] | Ensures ongoing method performance during routine use |
| Method Operable Design Region (MODR) | Established ranges of method parameters demonstrating robustness [79] | Provides flexibility in method operation within defined boundaries |
| Enhanced Approach | Systematic development approach using risk assessment and multivariate experimentation [78] | Enables greater scientific understanding and regulatory flexibility |
Implementation Framework: From Theory to Practice
Structured Implementation Workflow
Implementing the ICH Q14 lifecycle concept follows a structured workflow that transforms theoretical principles into practical application. Research indicates that a stepwise approach facilitates successful adoption across diverse industrial settings [79]:
- Method Request and ATP Definition: The process begins with a clear articulation of the analytical need, which is formalized through the ATP. The ATP should capture not only technical performance requirements (e.g., accuracy, precision) but also business needs [79].
- Risk Assessment and Knowledge Management: Using quality risk management principles (ICH Q9), potential sources of method variability are identified. This prioritizes parameters for experimental investigation [27].
- Systematic Experimentation: During method development, systematic approaches including Design of Experiments (DoE) evaluate the influence of method parameters on performance. This efficiently explores conditions and establishes a method operable design region [79].
- Control Strategy Implementation: A comprehensive control strategy is established, comprising suitable controls and System Suitability Tests (SSTs) to ensure the method consistently meets predefined criteria during routine use [78].
- Lifecycle Management: Once the method is operational, continuous monitoring and adjustment maintain performance over time, with a robust change management system for post-approval modifications [27].
Diagram 1: Analytical Procedure Lifecycle Workflow
ATP Development Process
The ATP development follows a structured process to ensure all critical requirements are captured. Research shows that a comprehensive ATP should consider not only ICH Q2(R2) performance characteristics but also business requirements and stakeholder needs [79]:
Diagram 2: ATP Development Process
Practical Tools for Implementation
Successful implementation of ICH Q14 requires practical tools and methodologies that simplify the adoption of AQbD principles. Recent research has addressed the challenge of translating theory into practice by providing ready-to-implement solutions [79]:
- Structured Risk Assessment Tools: Utilizing Failure Mode Effects Analysis (FMEA) to identify and prioritize potential sources of method variability.
- Experimental Design Templates: Pre-designed DoE templates for efficient investigation of method parameters and their interactions.
- Control Strategy Frameworks: Standardized approaches for defining system suitability tests and analytical procedure control strategies.
- Knowledge Management Systems: Structured documentation for capturing method development knowledge to support lifecycle management.
These tools help bridge the gap between theoretical concepts and real-world application, particularly for methods requiring high precision at low concentration levels where traditional approaches may be insufficient.
Comparative Analysis: Traditional vs. Lifecycle Approach
Method Development and Validation Comparison
The transition from traditional to lifecycle-based approaches represents a significant shift in pharmaceutical analysis. The table below summarizes key differences between these paradigms:
Table 2: Traditional vs. Lifecycle Approach Comparison
| Aspect | Traditional Approach | Lifecycle Approach (ICH Q14) |
|---|---|---|
| Development Philosophy | Sequential, empirical; often "one-factor-at-a-time" [78] | Systematic, science-based; multivariate experimentation [79] |
| Validation Timing | One-time event before routine use [77] | Continuous process throughout method lifetime [27] |
| Performance Documentation | Demonstration of acceptance criteria at fixed point [77] | Ongoing verification against ATP requirements [77] |
| Change Management | Often requires regulatory submission [27] | More flexible, science-based changes within approved design space [27] |
| Knowledge Building | Limited formal knowledge capture | Structured knowledge management supporting lifecycle [79] |
| Control Strategy | Fixed system suitability tests [78] | Dynamic control strategy based on risk assessment [78] |
| Regulatory Flexibility | Limited flexibility post-approval | Enhanced flexibility through established conditions [77] |
Impact on Precision at Low Concentration Levels
For methods requiring precision at low concentration levels, the lifecycle approach offers distinct advantages:
- Proactive Robustness Evaluation: Through systematic experimentation during development, factors affecting precision at low concentrations are identified and controlled [79].
- Science-based Setting of Limits: The ATP defines required precision at low levels prospectively, guiding development to meet these specific challenges [77].
- Enhanced Method Understanding: Multivariate studies reveal interactions between parameters that disproportionately affect low-level precision [79].
- Continuous Performance Verification: Ongoing monitoring detects precision deterioration at critical low concentrations before method failure occurs [27].
Essential Research Reagent Solutions
Implementing the ICH Q14 lifecycle approach requires specific reagents and materials that support robust method development and validation. The following table details key research reagent solutions essential for successful application of the guideline:
Table 3: Essential Research Reagent Solutions for ICH Q14 Implementation
| Reagent/Material | Function in Lifecycle Approach | Application Examples |
|---|---|---|
| Certified Reference Materials | Provide traceable standards for accuracy determination and ATP verification [77] | Quantification of accuracy against known standards throughout method lifecycle |
| Stable Isotope-Labeled Analytes | Enable precise measurement of recovery and detection capability at low concentrations | Evaluation of method precision and accuracy at low concentration levels |
| Matrix-Matched Quality Controls | Assess method performance in authentic sample matrices as emphasized by ICH Q2(R2) [77] | Precision studies under conditions representing actual patient specimens |
| Stability-Indicating Standards | Demonstrate method specificity and robustness for forced degradation studies | Verification of method stability-indicating capabilities throughout lifecycle |
| System Suitability Test Mixtures | Implement analytical procedure control strategy through verified performance checks [78] | Daily verification of method performance against ATP criteria |
Experimental Protocols for Lifecycle Implementation
Protocol for Method Comparison Studies
Method comparison studies are essential for estimating systematic error when introducing new methods or replacing existing ones. The ICH Q14 lifecycle approach enhances these studies through structured experimental design and data analysis techniques [80]:
- Sample Selection and Size: A minimum of 40 different patient specimens should be tested, selected to cover the entire working range of the method. Specimens should represent the spectrum of diseases expected in routine application. When assessing specificity differences between methods, 100-200 specimens may be needed [81].
- Experimental Design: Analyses should be performed over a minimum of 5 days, with 2-5 patient specimens per day, to minimize systematic errors that might occur in a single run. Duplicate measurements are recommended to identify sample mix-ups, transposition errors, and other mistakes [81].
- Data Analysis Approach: Graph results using difference plots (for methods expected to show one-to-one agreement) or comparison plots (for methods with different measurement principles). Calculate linear regression statistics (slope, y-intercept, standard deviation about the regression line) for wide analytical ranges, or average difference (bias) for narrow ranges [81].
Protocol for Design of Experiments (DoE)
DoE represents a core component of the enhanced approach in ICH Q14, enabling efficient investigation of multiple method parameters and their interactions:
- Parameter Selection: Based on risk assessment, identify critical method parameters (CMPs) requiring experimental investigation.
- Experimental Design: Utilize fractional factorial designs for screening experiments to identify influential factors, followed by response surface methodologies (e.g., central composite designs) for optimization.
- Design Space Establishment: Through systematic experimentation, establish a method operable design region (MODR) defining parameter ranges within which method performance remains acceptable.
- Model Verification: Confirm predictive models through verification experiments at selected conditions within the MODR.
Protocol for Lifecycle Management and Continuous Verification
Once a method is implemented, the ICH Q14 lifecycle approach requires ongoing verification of method performance:
- System Suitability Testing: Implement SSTs derived from method understanding during development. These tests should verify that the method continues to meet ATP requirements before each use [78].
- Quality Control Monitoring: Track quality control results over time using statistical process control techniques to detect trends or shifts in method performance.
- Periodic Assessment: Conduct periodic reviews of method performance against the ATP, incorporating data from routine testing, quality control, and any method changes.
- Change Management: Implement a science- and risk-based approach to method changes, utilizing prior knowledge and risk assessments to determine necessary verification studies.
The implementation of the ICH Q14 analytical procedure lifecycle concept represents a significant advancement in pharmaceutical analysis. By adopting a systematic, science-based approach to method development, validation, and ongoing performance verification, organizations can achieve more robust, reliable, and fit-for-purpose methods [27]. The lifecycle model provides a structured framework for building quality into methods from the outset, rather than attempting to validate quality at the end of development [79].
For researchers focused on precision at low concentration levels, the ICH Q14 framework offers particular value. The emphasis on systematic experimentation, risk-based parameter evaluation, and continuous performance monitoring directly addresses the challenges of low-level quantification. Furthermore, the regulatory flexibility afforded by the enhanced approach enables continuous improvement of methods throughout their lifecycle, allowing organizations to adapt to new technologies and evolving product understanding [77].
As the pharmaceutical industry continues to embrace these principles, the analytical procedure lifecycle concept will likely become the standard approach for ensuring method reliability, particularly for challenging applications requiring precision at low concentrations. The implementation roadmap, practical tools, and experimental protocols outlined in this guide provide a foundation for successful adoption of ICH Q14 across research and development organizations.
The accurate and precise quantification of analytes, particularly at low concentrations, is a cornerstone of research and development in pharmaceuticals and clinical diagnostics. The choice of analytical technique directly impacts the reliability of data, influencing decisions in drug development, therapeutic monitoring, and clinical diagnosis. This guide provides an objective comparison of the precision performance of three prevalent analytical platforms—High-Performance Liquid Chromatography (HPLC), Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS), and Immunoassays.
Within the framework of method validation, precision is defined as the closeness of agreement between independent test results obtained under stipulated conditions [82]. It is a critical parameter for assessing the reliability of an analytical method, especially when measuring biomarkers or drugs at trace levels. This analysis synthesizes experimental data and validation protocols to compare the precision of these techniques, providing a scientific basis for method selection.
Quantitative Precision Performance Data
The following tables summarize key quantitative findings from comparative studies, highlighting the precision characteristics of each analytical technique.
Table 1: Comparative Precision Data for Cyclosporine (CsA) and Tacrolimus (TAC) Monitoring [83]
| Analyte | Analytical Technique | Precision (Coefficient of Variation - CV%) | Experimental Context |
|---|---|---|---|
| Cyclosporine (CsA) | HPLC | Within-assay CV: 6.8%-7.6% (for controls) | Prospective comparative studies |
| Immunoassays (FPIA/AxSYM, CEDIA, EMIT) | Within-assay CV: 1.7%-11% (for controls); Between-assay CV: up to 8.9% at low CsA | Prospective comparative studies; Immunoassays consistently showed higher CVs than HPLC | |
| Tacrolimus (TAC) | HPLC-MS | Inter-assay CV: 5.7%-8.0% (for controls at 5-22 ng/mL) | Randomized Controlled Trial |
| Immunoassays (MEIA) | Inter-assay CV: 8.3%-13.7% (for controls at 5-22 ng/mL) | Randomized Controlled Trial; MEIA demonstrated higher imprecision |
Table 2: Precision Data from Individual Method Validation Studies
| Analyte | Analytical Technique | Precision (CV%) | Source |
|---|---|---|---|
| 25-Hydroxyvitamin D | LC-MS/MS | Intra-assay: <8.8%; Inter-assay: <13.2% | Comparison with immunoassays [84] |
| N-lactoyl-phenylalanine | LC-MS/MS | Overall precision: <8% | Validation for dried blood spot analysis [85] |
| LXT-101 (Peptide) | LC-MS/MS | Intra-batch: 3.23%-14.26%; Inter-batch: 5.03%-11.10% | Bioanalytical method validation [86] |
| Furosemide, related compounds, preservatives | HPLC | Precision (RSD): ≤ 2% | Pharmaceutical quality control [87] |
Experimental Protocols for Precision Assessment
The assessment of precision follows standardized validation protocols. The following workflow generalizes the process for determining intermediate precision, a key metric that captures variability over time within a single laboratory.
Detailed Methodology
The precision assessment is conducted according to established guidelines, such as those from the U.S. Food and Drug Administration (FDA) and international standards [82] [85] [86]. The core experimental steps include:
- Preparation of Quality Control (QC) Samples: QC samples are prepared at a minimum of three concentrations (low, medium, and high) spanning the calibration range of the method. These are typically spiked into the same matrix as the study samples (e.g., human serum, plasma) [84] [86].
- Analysis Schedule: The QC samples are analyzed in multiple replicates (e.g., n=5) in a single run (for within-run or repeatability precision) and over multiple, separate runs conducted on different days (for between-run or intermediate precision). Key factors like analyst, instrument, and reagent lot may be varied to assess intermediate precision [82].
- Data Calculation: For each QC concentration level, the mean concentration and standard deviation (SD) are calculated from the measured results. The precision is then expressed as the Coefficient of Variation (CV%), calculated as (SD / Mean) × 100% [83] [82].
- Acceptance Criteria: The calculated CV% is evaluated against pre-defined acceptance criteria, which are based on the intended use of the method. For bioanalytical methods, a common threshold for precision is a CV of ≤15%, often tightened to ≤20% at the Lower Limit of Quantification (LLOQ) [82] [86].
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of precise analytical methods relies on a suite of critical reagents and materials. The following table details key components and their functions in chromatographic and immunoassay workflows.
Table 3: Essential Reagents and Materials for Analytical Method Development
| Item | Function / Role | Application Context |
|---|---|---|
| Chromatography Column (e.g., C18) | Stationary phase for separating analytes based on chemical affinity; critical for resolution and peak shape. | HPLC & LC-MS/MS [84] [87] [86] |
| Stable Isotope-Labeled Internal Standard (IS) | Accounts for variability in sample preparation and ionization efficiency; improves accuracy and precision. | LC-MS/MS (Quantitative) [84] [85] |
| Mass Spectrometry Mobile Phase (e.g., 0.1% Formic Acid) | Ion-pairing agent to enhance analyte ionization in the mass spectrometer; improves sensitivity. | LC-MS/MS [88] [84] |
| Quality Control (QC) Materials | Used to monitor the performance of the assay during validation and routine analysis. | All Techniques [89] [82] |
| Capture & Detection Antibodies | Provide the basis for specificity by binding to the target protein or biomarker. | Immunoassays [90] |
| Calibrators | Series of samples with known analyte concentrations used to construct the standard curve. | All Techniques [89] [82] |
| Solid-State Nanopore & DNA Nanostructures | Acts as a highly specific sensing element for digital, single-molecule counting of proteins. | Digital Immunoassays [90] |
The experimental data consistently demonstrates a hierarchy in precision performance among the three techniques. LC-MS/MS generally offers the highest level of precision, particularly at low concentration levels, due to superior specificity and the use of stable isotope internal standards. HPLC also provides strong precision, often surpassing that of immunoassays. While Immunoassays offer high throughput and automation, they are more susceptible to matrix effects and cross-reactivity, leading to higher imprecision and analytical bias compared to chromatographic methods [83] [84].
The choice of method ultimately depends on the specific application, required sensitivity, available resources, and the necessity for throughput. For research and applications demanding the utmost precision at low concentrations, such as pharmacokinetic studies of novel drugs or quantification of low-abundance biomarkers, LC-MS/MS represents the gold standard. This analysis underscores the importance of rigorous method validation, including a thorough assessment of precision, to ensure the generation of reliable and meaningful data.
Conclusion
Validating method precision at low concentrations is not a mere regulatory hurdle but a fundamental scientific requirement for generating trustworthy data in critical areas like drug development and clinical diagnostics. Success hinges on a deep understanding of foundational concepts, the meticulous application of methodological best practices, proactive troubleshooting, and a rigorous, well-documented validation process. The adoption of a lifecycle approach, as championed by modern ICH Q2(R2) and Q14 guidelines, ensures methods remain fit-for-purpose. Future directions will be shaped by advanced chemometric models, the integration of green chemistry principles via White Analytical Chemistry (WAC) assessments, and a continued emphasis on risk-based strategies to enhance efficiency and reliability in biomedical research.
References
- 1. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 2. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 3. Precision [https://www.geoanalyst.org/precision/]
- 4. 4.1. Repeatability, intermediate precision and reproducibility [https://sisu.ut.ee/lcms_method_validation/41-precision-trueness-accuracy/]
- 5. SPE Method Validation Terms: Precision and Accuracy [https://www.phenomenex.com/our-company/phenomenex-blog/technique-blogs/sample-preparation/spe-method-validation-terms-accuracy-and-precision?srsltid=AfmBOorNcRFyPTQ_94K1gRPlhy-OZYyeBSZpFKeMp9_xIhZyKf2isbp6]
- 6. 2025 Trends In Pharmaceutical Analytical Methods ... [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 7. Process and Method Validation in IND Drug Development [https://improvedpharma.com/process-and-method-validation-ind-drug-development-building-robust-foundation/]
- 8. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 9. What is the difference between Limit of detection (LOD) and ... [https://blog.quality-pathshala.com/2023/08/10/what-is-the-difference-between-limit-of-detection-lod-and-limit-of-quantification/]
- 10. Limit of Quantitation - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/limit-of-quantitation]
- 11. Method Validation Essentials, Limit of Blank ... [https://www.biopharminternational.com/view/method-validation-essentials-limit-blank-limit-detection-and-limit-quantitation]
- 12. What is meant by the limit of detection and quantification (LOD ... [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/limit-of-detection-quantifcation]
- 13. Determining LOD and LOQ Based on the Calibration Curve [https://www.sepscience.com/hplc-solutions-126-chromatographic-measurements-part-5-determining-lod-and-loq-based-on-the-calibration-curve-6959]
- 14. Calculate LOD and LOQ with Microsoft Excel [https://bitesizebio.com/48459/excel-lod-loq/]
- 15. Comparison of approaches for assessing detection and ... [https://www.nature.com/articles/s41598-024-83474-5]
- 16. FDA Issues Draft Guidance on Data Integrity Considerations for Bioavailability and Bioequivalence Studies – Publications [https://www.morganlewis.com/pubs/2024/04/fda-issues-draft-guidance-on-data-integrity-considerations-for-bioavailability-and-bioequivalence-studies]
- 17. A method for measuring the experimental resolution ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8649380/]
- 18. Biomarkers in PK Assays: Enhancing Predictive Accuracy ... [https://swordbio.com/blog/biomarkers-in-pk-assays-enhancing-predictive-accuracy-in-clinical-trials/]
- 19. Prediction performance comparison of biomarkers for ... [https://pubmed.ncbi.nlm.nih.gov/38528429/]
- 20. NonClinical Dose Formulation Analysis Method Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2976985/]
- 21. Total imprecision of exposure biomarkers: implications for calculating exposure limits - PubMed [https://pubmed.ncbi.nlm.nih.gov/17492658/]
- 22. Data Integrity for In Vivo Bioavailability and Bioequivalence Studies | FDA [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/data-integrity-in-vivo-bioavailability-and-bioequivalence-studies]
- 23. FDA Releases Guidance on Data Integrity for In Vivo Bioavailability and Bioequivalence Studies [https://www.pharmtech.com/view/fda-releases-guidance-on-data-integrity-for-in-vivo-bioavailability-and-bioequivalence-studies]
- 24. Development and Validation of a High-Performance Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6136501/]
- 25. Validation of a Simple HPLC/UV Method for Assay and In ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11656206/]
- 26. HPLC Content Determination Method Validation [https://www.welch-us.com/blogs/knowleage-base/hplc-content-determination-method-validation-a-comprehensive-guide]
- 27. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 28. Highlights from FDA's Analytical Test Method Validation ... [https://www.propharmagroup.com/thought-leadership/fda-analytical-test-method-validation-guidance]
- 29. The ICH Q2(R2) Validation Shake-Up, Why Your Old ... [https://www.linkedin.com/pulse/ich-q2r2-validation-shake-up-why-your-old-playbook-wont-cut-enkrisi-5hpae]
- 30. What Is ICH Q2R2 Method Validation and Its Importance? [https://altabrisagroup.com/ich-q2r2-method-validation/]
- 31. Validation of Analytical Methods: A Review [https://www.gavinpublishers.com/article/view/validation-of-analytical-methods-a-review]
- 32. Analytical Methods: A Statistical Perspective on the ICH ... [https://www.biopharminternational.com/view/analytical-methods-statistical-perspective-ich-q2a-and-q2b-guidelines-validation-analytical-methods]
- 33. The Liquid-Liquid Extraction Guide [https://www.phenomenex.com/knowledge-center/spe-knowledge-center/overview-of-liquid-liquid-extraction-in-sample-preparation?srsltid=AfmBOorGTfxNPEsshTQ_YGPLgYDBFU14C5OhwZqJjUXYYk_dAkFSolXJ]
- 34. Comparison of Two Solid-Phase Extraction (SPE) Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6321002/]
- 35. Performance comparison between solid phase extraction and ... [https://jast-journal.springeropen.com/articles/10.1186/s40543-021-00296-0]
- 36. Validation of a Liquid–Liquid Extraction Method to Study ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10301472/]
- 37. Comparative evaluation of liquid–liquid extraction, solid ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914013007777]
- 38. Not (Only) Reversed-Phase Liquid Chromatography–Mass ... [https://www.chromatographyonline.com/view/not-only-reversed-phase-liquid-chromatography-mass-spectrometry-alternative-lc-ms-approaches]
- 39. Innovations in Liquid Chromatography: 2025 HPLC ... [https://www.chromatographyonline.com/view/innovations-in-liquid-chromatography-2025-hplc-column-and-accessories-review]
- 40. Mobile Phase Optimization: A Critical Factor in HPLC [https://www.phenomenex.com/knowledge-center/hplc-knowledge-center/mobile-phase-in-chromatography?srsltid=AfmBOooU_uXVGJkPCIhxHGP9o7xvxparF3tXwE80hY6eqMge1MBxB5Yj]
- 41. Optimization of Detector Parameters to Improve Sensitivity ... [https://www.waters.com/nextgen/ie/en/library/application-notes/2025/optimization-of-detector-parameters-to-improve-sensitivity-using-the-alliance-is-hplc-system-with-pda-detector.html?srsltid=AfmBOortBxYcU9jAFotKYHImIwEOAB-vKBKNumazSWIqLSngLCCnaIKg]
- 42. Eight Steps to Method Validation in a Clinical Diagnostic ... [https://clsjournal.ascls.org/content/31/1/43]
- 43. A practical approach to estimate analytical method ... [https://www.sciencedirect.com/science/article/pii/S0731708524003844]
- 44. Green and white analytical approach for parallel ... [https://www.nature.com/articles/s41598-025-07056-9]
- 45. New standards in HER2-low testing: the CASI-01 comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571579/]
- 46. Machine learning augmented diagnostic testing to identify ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1013651]
- 47. Rapid assay development for low input targeted ... [https://www.nature.com/articles/s41467-025-58757-8]
- 48. Ithy - Understanding Robustness Across Various Study Fields Tests [https://ithy.com/article/definitions-robustness-tests-fields-tm9cgeda]
- 49. Model robustness explained: methods , testing , and best practices [https://www.linkedin.com/pulse/model-robustness-explained-methods-testing-5lv0e]
- 50. Precision Medicine Trends 2025: Top 6 Powerful Positive ... [https://lifebit.ai/blog/precision-medicine-trends-2025/]
- 51. Precision cancer medicine 2025: some concerns - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439214/]
- 52. Technical Considerations of Pharmacokinetic Assays for ... [https://link.springer.com/article/10.1208/s12248-025-01122-w]
- 53. Implementing Robustness Checks: A Practical Guide to Model... [https://www.numberanalytics.com/blog/implementing-robustness-check-guide-model-evaluation]
- 54. Development and validation of a novel RP-HPLC method ... [https://www.sciencedirect.com/science/article/pii/S2211715625003650]
- 55. A roadmap to precision medicine through post-genomic ... [https://www.nature.com/articles/s41467-025-56442-4]
- 56. Population pharmacokinetics of penicillin G - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217478/]
- 57. Optimization of Calibration Strategies for the Quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524275/]
- 58. Practical Analysis of LOD and LOQ with Examples [https://www.chemistryjobinsight.com/2025/03/practical-analysis-lod-loq-method.html]
- 59. The Limit of Detection [https://www.chromatographyonline.com/view/limit-detection]
- 60. 4.4. Calibration Standards, Recovery, LOD and LOQ [https://bio-protocol.org/exchange/minidetail?id=11007680&type=30]
- 61. Pre-analytical phase errors constitute the vast majority of ... [https://pubmed.ncbi.nlm.nih.gov/40311145/]
- 62. Evaluating the total laboratory testing process and ... [https://link.springer.com/article/10.1007/s44250-025-00260-4]
- 63. May 2025: Sample Stability [https://www.aniara.com/blog/may-2025-sample-stability.html]
- 64. A universal tool for stability predictions of biotherapeutics ... [https://www.nature.com/articles/s41598-023-35870-6]
- 65. Use of Factorial Designs to Reduce Stability Studies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389050/]
- 66. Stability Toolkit for the Appraisal of Bio/Pharmaceuticals ... [https://www.mdpi.com/2673-4532/6/3/25]
- 67. Sample Release Reagents Market Growth Outlook 2025 [https://www.linkedin.com/pulse/sample-release-reagents-market-growth-outlook-2025-ai-vgtee/]
- 68. Establishing Acceptance Criteria for Analytical Methods [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 69. System Suitability Testing: Ensuring Reliable Results [https://www.labmanager.com/system-suitability-testing-ensuring-reliable-results-34248]
- 70. What are system suitability tests (SST) of analytical methods? [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/sst]
- 71. Are You Sure You Understand USP ? [https://www.chromatographyonline.com/view/are-you-sure-you-understand-usp-621-]
- 72. What Is System Suitability Test (SST) In HPLC And GC ... [https://pharmaguru.co/system-suitability-test/]
- 73. System Suitability in HPLC Analysis [https://www.pharmaguideline.com/2017/09/system-suitability-in-hplc-analysis.html]
- 74. Setting system suitability criteria for detectability in high- ... [https://pubmed.ncbi.nlm.nih.gov/11403474/]
- 75. Setting system suitability criteria for detectability in high- ... [https://www.sciencedirect.com/science/article/abs/pii/S0021967301006690]
- 76. ICH Q14 Analytical procedure development - Scientific guideline [https://www.ema.europa.eu/en/ich-q14-analytical-procedure-development-scientific-guideline]
- 77. What Did ICH Q14 Miss On Analytical Method Validation [https://www.bioprocessonline.com/doc/what-did-ich-q-miss-on-analytical-method-validation-0001]
- 78. ICH Q14 – latest guideline on analytical procedure ... [https://www.europeanpharmaceuticalreview.com/article/229300/ich-q14-latest-guideline-on-analytical-procedure-development/]
- 79. A Practical Approach to Implementing ICH Q14 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12449753/]
- 80. A practical guide to validation and verification of analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S006524231930006X]
- 81. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 82. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 83. Calcineurin Inhibitors for Renal Transplant [https://www.ncbi.nlm.nih.gov/books/NBK356382/table/results.t4/]
- 84. Comparison with Two Automated Immunoassays [https://www.annclinlabsci.org/content/46/6/645.full]
- 85. Proof-of-concept of a prior validated LC-MS/MS method for ... [https://www.frontiersin.org/journals/sports-and-active-living/articles/10.3389/fspor.2025.1600714/full]
- 86. Development and validation of an LC–MS/MS method ... [https://www.nature.com/articles/s41598-025-96764-3]
- 87. Simultaneous Development and Validation of an HPLC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12526389/]
- 88. Validation and clinical application of an LC-MS/MS method ... [https://www.sciencedirect.com/science/article/pii/S0731708525004340]
- 89. Quality Control in Immunoassays : Ensuring Accuracy , Reliability and... [https://www.linkedin.com/pulse/quality-control-immunoassays-ensuring-accuracy-reliability-saikat-pal-v5mvc]
- 90. Digital immunoassay for biomarker concentration quantification using... [https://www.nature.com/articles/s41467-021-25566-8?error=cookies_not_supported&code=82bfea9b-e357-4d24-b361-c13cf5e7ff5e]