Sample Integrity: A Scientist's Complete Guide to Preventing Contamination During Sample Preparation
This guide provides researchers, scientists, and drug development professionals with a comprehensive framework for safeguarding sample integrity from collection to analysis.
Sample Integrity: A Scientist's Complete Guide to Preventing Contamination During Sample Preparation
Abstract
This guide provides researchers, scientists, and drug development professionals with a comprehensive framework for safeguarding sample integrity from collection to analysis. Covering foundational principles, practical methodologies, advanced troubleshooting, and validation techniques, it addresses critical contamination risks in sensitive workflows like qPCR, cell culture, and low-biomass microbiome studies. By synthesizing current best practices and preventative strategies, the article empowers professionals to generate reproducible, reliable data and avoid the costly consequences of compromised samples.
Understanding the Enemy: Defining Contamination Sources and Impacts on Data Integrity
Contamination represents a critical and pervasive risk in scientific research and drug development, capable of compromising data integrity, invalidating experimental results, and derailing research projects. In pharmaceutical manufacturing alone, contamination issues have led to significant regulatory actions, including a documented case where 20% of bioreactor runs at a major facility were rejected over a 30-month period due to contamination concerns [1]. The challenges are particularly acute in low-biomass microbiome studies and biologics manufacturing, where even minimal contaminant introduction can disproportionately impact results. This technical guide examines the contamination landscape across research domains, provides detailed methodologies for contamination prevention and detection, and presents a comprehensive framework for safeguarding research integrity from sample preparation through data analysis. By implementing robust contamination control strategies, researchers can ensure data reliability and accelerate the development of safe, effective therapeutics.
The Contamination Landscape: Quantifying the Problem
Contamination manifests in multiple forms across research environments, each with distinct characteristics and impacts on data integrity.
Table 1: Types of Research Contamination and Their Impacts
| Contamination Type | Primary Sources | Key Impact on Research | Common Detection Methods |
|---|---|---|---|
| Microbial [1] | Raw materials, human operators, environment, process additives | Compromises cell cultures, alters biochemical assays, affects product safety and efficacy | Rapid microbiological methods, PCR, sterility testing [1] |
| Chemical [2] [3] | Residual solvents, heavy metals, extractables from materials | Causes chemical poisoning, alters reaction kinetics, introduces impurities | Spectroscopy, chromatography [2] |
| Cross-Contamination [4] | Well-to-well leakage, improper sample handling, equipment reuse | False positives/negatives, incorrect sample attribution, skewed population data | Sample tracking controls, unique tracers, historical data comparison [5] [4] |
| Data Contamination [6] | Evaluation data leakage into training sets for LLMs | Inflated performance metrics, unreliable capability assessment, inaccurate benchmarking | String matching, n-gram analysis, behavioral analysis [6] |
The market data for contamination detection reflects growing recognition of these challenges. The contamination detection in pharma products market is experiencing robust growth, with North America holding a dominant 45.2% market share in 2024 [3]. Segment analysis reveals that:
- By contamination type, chemical contamination detection held the largest revenue share (36.5%) in 2024, while microbial contamination detection is projected to be the fastest-growing segment from 2025 to 2035 [2].
- By technology, spectroscopy-based detection dominated (34.2% share) in 2024, with PCR and molecular diagnostics expected to register the fastest growth [3].
- By sample type, finished pharmaceutical products testing led (52.8% share) in 2024, while biologics & cell culture samples represent the fastest-growing segment [3].
Table 2: Contamination Detection Market Segmentation (2024)
| Segmentation Category | Dominant Segment (2024) | Market Share | Fastest-Growing Segment |
|---|---|---|---|
| Contamination Type | Chemical Contamination | 36.5% | Microbial Contamination |
| Detection Technology | Spectroscopy-Based | 34.2% | PCR & Molecular Diagnostics |
| Product & Service Type | Instruments | 49.6% | Consumables & Reagents |
| Sample Type | Finished Pharmaceutical Products | 52.8% | Biologics & Cell Culture Samples |
| End User | Pharmaceutical Companies | 63.4% | Biotechnology Companies |
Contamination Detection Methodologies
Advanced Detection Technologies
Modern contamination detection leverages multiple technological approaches, each with specific applications and limitations:
Molecular Detection Methods: PCR and molecular diagnostics represent the fastest-growing detection technology segment [3]. These methods enable highly sensitive identification of specific organisms and genetic markers through targeted amplification. For microbial detection, PCR assays can identify low levels of bacterial and mold contamination in therapeutic samples, comprising less than 10 CFU (colony-forming units) [2]. The methodology involves:
- Sample Preparation: DNA extraction using validated kits free of contaminating DNA [1]
- Amplification: Target-specific primer binding and thermal cycling
- Detection: Fluorescence measurement or gel electrophoresis for amplicon visualization
- Validation: Comparison with authenticated microbial cultures and USP standards [1]
Spectroscopy-Based Techniques: Spectroscopy dominates the detection technology landscape with a 34.2% market share [2]. Machine-learning aided UV absorbance spectroscopy has emerged as an advanced approach for identifying contamination during cell therapy product manufacture [2]. The experimental protocol involves:
- Sample Introduction: Minimal preparation with negligible sample volume requirements
- Spectral Analysis: Absorbance measurement across wavelength ranges
- Pattern Recognition: Machine learning algorithms to classify contamination signatures
- Validation: Cross-referencing with established contamination markers
Rapid Microbiological Methods: These innovative approaches reduce traditional culture times from days to hours through:
- ATP bioluminescence for viable organism detection
- Flow cytometry for cellular contamination identification
- Microscopy with advanced imaging for particulate contamination [1]
Historical Data Review for Anomaly Detection
Beyond technological detection methods, historical data review provides a powerful statistical approach for identifying contamination events. This methodology involves comparing reported data to previous analytical results for specific sampling locations [5]. The process requires a robust dataset (at least 4-5 previous results) and consistent sampling locations [5]. Implementation involves three primary approaches:
- Tabular Review: Direct numerical comparison of current results to historical data
- Historical Time Series: Graphical representation of data trends over time
- Statistical Approach: Establishing upper and lower control limits to flag outliers [5]
When historical review identifies anomalies, a thorough investigation includes examining laboratory data packages, evaluating seasonal trends, reviewing field measurements (pH, ORP, specific conductance), and assessing weather conditions [5]. Case studies demonstrate effectiveness, with one example identifying sample switch events during metals analysis that weren't apparent through standard quality control measures [5].
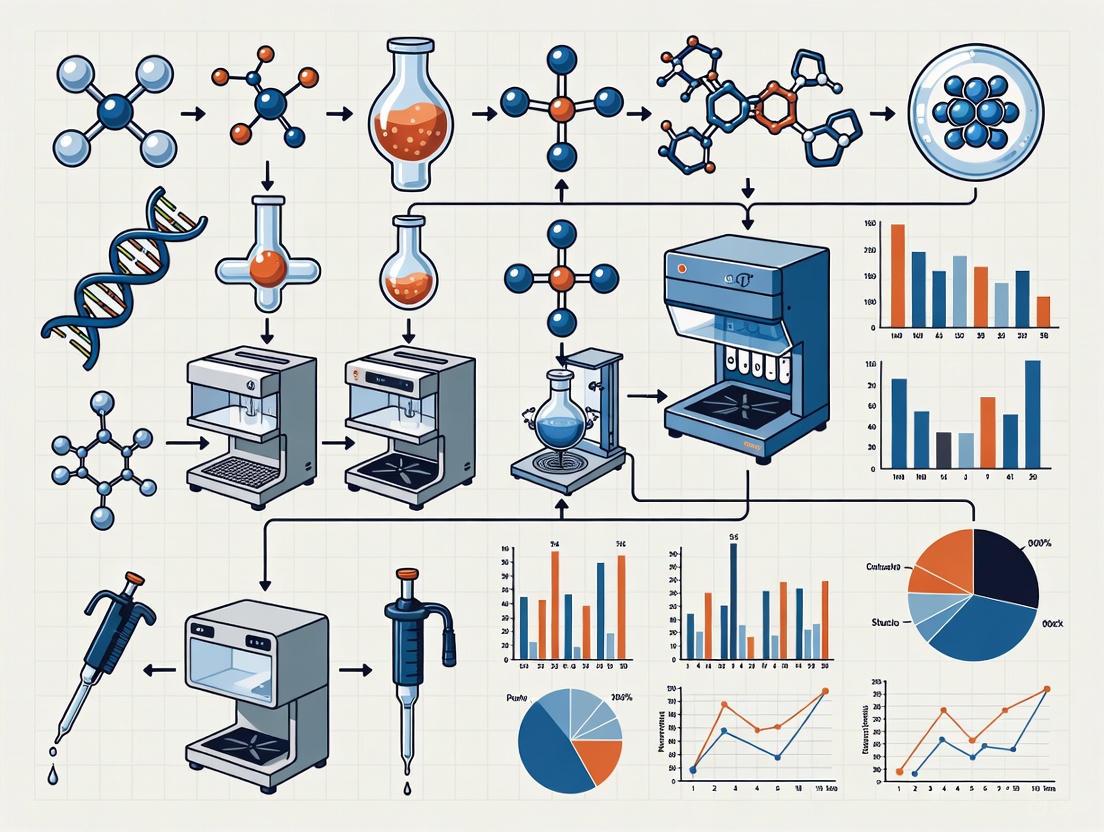
Diagram 1: Historical data review workflow for contamination detection.
Contamination Prevention Protocols
Sample Handling and Processing Guidelines
Effective contamination prevention begins with rigorous sample handling protocols, particularly critical in low-biomass research where contaminants can constitute most of the detected signal [4].
Sample Collection Protocols:
- Equipment Decontamination: Sequential treatment with 80% ethanol (to kill contaminating organisms) followed by nucleic acid degrading solution (to remove residual DNA) [4]
- Personal Protective Equipment (PPE): Utilization of gloves, goggles, coveralls, and shoe covers appropriate for the sampling environment to minimize human-derived contamination [4]
- Single-Use Materials: Implementation of DNA-free swabs and collection vessels when possible
- Pre-treatment of Storage Materials: Autoclaving or UV-C light sterilization of plasticware/glassware, maintained sealed until sample collection [4]
Laboratory Processing Controls:
- Environmental Monitoring: Risk-based monitoring programs with trending of data to identify potential contamination concerns before impacting processes [1]
- Control Samples: Inclusion of empty collection vessels, air-exposed swabs, and preservation solution aliquots processed alongside experimental samples [4]
- Process Validation: Regular validation of disinfection protocols using authenticated reference materials [1]
Decontamination Methodologies
Both manual and automated decontamination approaches play roles in contamination prevention, with selection dependent on application requirements.
Table 3: Automated Decontamination Method Comparison
| Method | Advantages | Disadvantages | Best Applications |
|---|---|---|---|
| Hydrogen Peroxide Vapor [7] | Excellent distribution, material compatibility, quick cycle times with active aeration, low-level safety sensors | Higher initial capital investment | Isolators, cleanrooms, regular production campaigns |
| UV Irradiation [7] | Speed, no requirement to seal enclosure | Prone to shadowing, may not kill spores, efficacy decreases with distance | Surface decontamination, supplemental cleaning |
| Chlorine Dioxide [7] | Highly effective microbe killing, quick with high concentrations | Highly corrosive, toxic (OEL <0.1 ppm), high consumables cost | Emergency decontamination, sealed environments |
| Aerosolized Hydrogen Peroxide [7] | Good material compatibility, effective microbe killing | Liquid droplets prone to gravity, relies on direct line of sight, longer cycle times | Small isolators, limited applications |
Manual Decontamination Protocols:
- Surface Disinfection: Application of validated disinfectants using spraying, mopping, and wiping techniques [7]
- Validation Requirements: Proof that selected disinfectant kills expected microbes after specified contact time [7]
- Limitations: Human variability in application, difficult validation, inconsistent coverage [7]
Automated Decontamination Advantages:
- Consistency and Repeatability: Same conditions replicated exactly in every cycle [7]
- Reduced Downtime: Faster cycle times compared to manual approaches [7]
- Enhanced Traceability: Monitoring and documentation of decontamination parameters [7]
- Operator Safety: Reduced chemical exposure and health risks [7]
Diagram 2: Comprehensive contamination prevention framework.
The Researcher's Toolkit: Essential Reagent Solutions
Implementing effective contamination control requires specific reagents and materials validated for research use.
Table 4: Essential Research Reagent Solutions for Contamination Control
| Reagent/Material | Primary Function | Application Protocol | Validation Requirements |
|---|---|---|---|
| Nucleic Acid Degrading Solutions [4] | Removal of contaminating DNA from surfaces and equipment | Apply after ethanol decontamination, followed by rinsing with DNA-free water | Demonstration of DNA removal without residual inhibitory effects on downstream applications |
| Authenticated Microbial Cultures [1] | Reference materials for method validation and quality control | Use as positive controls in detection assays following USP standards | Verification against USP microbiological standards for regulatory filings |
| DNA-Free Collection Vessels [4] | Prevention of sample contamination during collection and storage | Pre-treat with UV-C light or autoclaving, maintain sealed until use | Testing for nucleic acid contamination and microbial growth |
| Rapid Microbiology Test Kits [1] | Detection of microbial contamination in raw materials and process samples | Follow manufacturer protocols for sample processing and incubation | Comparison with traditional culture methods for sensitivity and specificity |
| Process Analytical Technology (PAT) Sensors [3] | Real-time monitoring of critical process parameters for contamination | Integration into manufacturing processes for continuous monitoring | Calibration against reference methods and demonstration of robustness |
| Cyclopropyl(phenyl)methanethiol | Cyclopropyl(phenyl)methanethiol|CAS 151153-46-7 | Bench Chemicals | |
| Methyl 3-fluoro-2-vinylisonicotinat | Methyl 3-fluoro-2-vinylisonicotinate|CAS 1379375-19-5 | Methyl 3-fluoro-2-vinylisonicotinate (CAS 1379375-19-5) is a versatile fluorinated building block for pharmaceutical and material science research. For Research Use Only. Not for human or animal use. | Bench Chemicals |
Case Studies: Contamination Consequences and Resolutions
Laboratory Sample Contamination
An environmental laboratory case study demonstrates how historical data review identified chromium data significantly higher than previously reported levels [5]. The investigation revealed:
- Anomaly Detection: Statistical outlier identification through comparison with historical trends
- Evidence Gathering: Parent sample results provided strong evidence of potential laboratory issues
- Corrective Action: Laboratory reanalysis confirmed contamination, leading to improved cleaning procedures and process updates [5]
- Systemic Resolution: Implementation of formal corrective action to address recurring contamination incidents
Sample Switch Incident
Historical data review identified a sample switch during metals analysis where results for "Well A" and "Well B" were swapped [5]. Key findings included:
- Pattern Recognition: Discrepancy identified through deviation from historical well-specific profiles
- Targeted Investigation: Issue confined to metals analysis, not observed in other analytical fractions
- Laboratory Confirmation: Reanalysis confirmed sample switch in metals laboratory
- Process Improvement: Formal corrective action implemented due to recurrence in the same department [5]
Contamination presents substantial risks to research integrity across scientific disciplines, with potential impacts ranging from data distortion to complete study invalidation. The increasing complexity of biological therapeutics and sensitivity of analytical methods heightens vulnerability to contamination effects. Effective contamination control requires a comprehensive, proactive strategy integrating prevention, monitoring, and detection components. By implementing robust sampling protocols, validated decontamination methodologies, systematic control measures, and advanced detection technologies, researchers can safeguard data integrity throughout the research lifecycle. As technological advancements continue to improve detection capabilities and prevention strategies, maintaining vigilance against contamination remains fundamental to producing reliable, reproducible research outcomes and ensuring the development of safe, effective pharmaceutical products.
Contamination represents a pervasive and critical challenge in scientific research, with the potential to compromise experimental integrity, skew analytical results, and generate misleading data. In the specific context of sample preparation—a foundational step across numerous scientific disciplines—contamination control transcends mere best practice to become an essential requirement for producing valid, reproducible science. This technical guide provides a comprehensive examination of contamination vectors within research environments, focusing particularly on three primary domains: environmental contaminants from pharmaceutical sources, analytical reagents and consumables, and physical cross-contamination between samples. The guide is structured within the broader thesis that proactive contamination prevention during sample preparation is not merely a technical consideration but a fundamental prerequisite for research quality and reliability. Through detailed analysis of contamination mechanisms, standardized protocols for detection and prevention, and curated toolkits of mitigation reagents, this document aims to equip researchers with the practical knowledge necessary to safeguard their experimental processes against increasingly complex contamination threats. By adopting the systematic framework presented herein, research professionals and drug development specialists can significantly enhance the validity of their analytical outcomes while contributing to the broader scientific goal of methodological rigor and reproducibility across experimental domains.
The environmental compartment represents a significant and often underestimated vector for contamination in analytical science, particularly concerning the pervasive presence of pharmaceuticals and their metabolites. Active Pharmaceutical Ingredients (APIs), along with their transformation products, enter environmental matrices through multiple pathways including industrial and hospital effluent, domestic wastewater treatment plant discharges, and agricultural runoff from treated animals [8]. These residues constitute a prominent group of contaminants contributing to the global chemical pollution crisis, with nearly 1,000 APIs or their transformation products already detected in natural environments globally, including over 700 within the European Union alone [9].
The concerning property of pharmaceutical contaminants lies in their intentional design to elicit specific biological responses by interacting with evolutionarily conserved molecular targets across diverse taxa [8]. The degree of interspecies conservation directly correlates with the risk of eliciting unintended pharmacological effects in non-target organisms, with documented effects occurring even at environmentally relevant concentrations (ng/L to μg/L range) [8]. Notable case examples illustrate the severe ecological consequences of such contamination events:
- Diclofenac: Off-label use of this non-steroidal anti-inflammatory drug caused catastrophic population declines (>99%) in Gyps vulture species across India and Pakistan due to renal failure following consumption of contaminated cattle carcasses [8] [9].
- Ivermectin: Detection in soil and water environments has raised concerns about its potential role as a source of single- or multi-drug resistance, in addition to its insecticidal effects on ecologically important species [8] [9].
- Amitriptyline: This antidepressant affects feeding behavior and reproduction in freshwater mollusks at low concentrations due to its action on highly conserved serotonin and norepinephrine transporters [9].
Table 1: Documented Ecological Impacts of Pharmaceutical Contaminants
| Pharmaceutical | Ecological Impact | Mechanism | Affected Organisms |
|---|---|---|---|
| Diclofenac | Population decline >99% | Renal failure | Gyps vulture species |
| Ivermectin | Ecosystem disruption, potential resistance development | Insecticidal activity | Dung beetles, aquatic organisms |
| Amitriptyline | Altered feeding/reproduction | Serotonin/norepinephrine transport disruption | Freshwater mollusks |
| Estrogenic APIs | Feminization | Vitellogenin upregulation | Male fish species |
The regulatory framework for managing environmental pharmaceutical contamination remains inconsistent. The European Union introduced mandatory chronic ecotoxicity testing for human medicines only in 2006, meaning most legacy drugs registered before this date lack comprehensive ecotoxicity data [8]. Consequently, only approximately 12% of all pharmaceuticals have a complete set of ecotoxicity data, with environmental risk assessment (ERA) data absent for 281 out of 404 APIs used in human medicines on the German market alone [8]. This significant knowledge gap underscores the critical importance of integrating One Health principles—recognizing the interconnectedness of human, animal, and environmental health—throughout drug development and environmental monitoring workflows.
Analytical Contamination Vectors in Sample Preparation
Within the laboratory environment, sample preparation represents a critical vulnerability point for contamination introduction, particularly through consumables, reagents, and procedural artifacts. Modern sample preparation workflows utilize increasingly sophisticated products that themselves present potential contamination vectors if not properly qualified and controlled. Solid-phase extraction (SPE) cartridges, QuEChERS (Quick, Easy, Cheap, Effective, Rugged, and Safe) kits, and automated sample preparation instrumentation each present distinct contamination risks that must be systematically managed.
Recent market introductions specifically target the analysis of persistent environmental contaminants like per- and polyfluoroalkyl substances (PFAS), which themselves represent significant analytical contaminants due to their pervasive presence in manufacturing materials and laboratory environments [10]. Key products introduced between 2024-2025 include:
- Captiva EMR-PFAS Food Cartridges: Designed for PFAS analysis in food matrices, these 6-mL cartridges utilize Enhanced Matrix Removal technology but risk introducing PFAS contamination from the cartridge materials if not properly quality-controlled [10].
- Resprep PFAS SPE: Dual-bed SPE cartridges containing weak anion exchange media and graphitized carbon black that may leach fluoropolymer contaminants during extraction [10].
- InertSep WAX FF/GCB and GCB/Wax FF: Featuring alternating bed configurations to provide different selectivity, these cartridges require verification of their "high purity sorbents" to ensure they do not contribute to the analytical background [10].
The increasing automation of sample preparation introduces additional contamination vector considerations. Instruments like the Sielc Samplify automated sampling system and Alltesta Mini-Autosampler, while improving reproducibility, present potential cross-contamination risks through shared fluidic paths, probe surfaces, and vial positioning systems [10]. These systems must incorporate rigorous cleaning protocols and contamination monitoring to prevent sample-to-sample carryover, particularly when handling high-concentration samples preceding low-concentration analyses.
Table 2: Recent Sample Preparation Products and Contamination Considerations
| Product | Type | Application | Potential Contamination Vectors |
|---|---|---|---|
| Captiva EMR-PFAS | SPE cartridge | PFAS in food | Leaching from cartridge materials |
| Resprep PFAS SPE | Dual-bed SPE | Aqueous/solid samples | Fluoropolymer components |
| InertSep WAX/GCB | SPE cartridge | EPA Method 1633 | Sorbent impurities |
| Q-Sep QuEChERS | Extraction salts | PFAS in food/feed | Salt purity, background contamination |
| Samplify | Automated sampler | Liquid sampling | Probe carryover, vial cross-contamination |
| Alltesta Mini-Autosampler | Multi-function autosampler | Fraction collection, reactor sampling | Fluid path memory effects |
Detection and Computational Assessment of Contamination
Robust contamination detection represents a critical component of comprehensive contamination control strategies. Next-generation sequencing (NGS) analysis, particularly in cancer research, has driven the development of sophisticated computational methods for identifying and quantifying sample cross-contamination [11]. These methods primarily leverage genetic data to detect anomalies indicative of contamination events, providing researchers with objective metrics for quality control.
The fundamental principle underlying computational contamination detection involves identifying deviations from expected genetic patterns. In NGS analysis, cross-contamination detection methods utilize variant allele frequency (VAF) distributions, single nucleotide variant (SNV) profiles, and population genetics statistics to identify admixed samples [11]. Key methodologies include:
- ConSPr (Contamination Source Predictor): Identifies potential contamination sources by analyzing shared genetic variants between samples.
- VAF-based methods: Detect contamination through shifts in variant allele frequency distributions that deviate from expected heterozygous or homozygous patterns.
- Population genetics approaches: Utilize deviations from Hardy-Weinberg equilibrium or anomalous linkage disequilibrium to identify contaminated samples.
- Similarity-based methods: Identify unexpectedly high genetic similarity between purportedly unrelated samples.
Different computational methods offer complementary strengths, with performance varying based on contamination level, sequencing depth, and the genetic characteristics of the samples involved. Integration of multiple approaches typically provides the most robust contamination detection, particularly for low-level contamination events that might evade detection by individual methods.
Beyond genetic analysis, analytical chemistry approaches employ blank samples, standard reference materials, and matrix spike recoveries to monitor for contamination throughout sample preparation workflows. For environmental pharmaceutical analysis, method blanks are essential for identifying contamination introduced during sample preparation, particularly when analyzing trace-level APIs. The implementation of quality control samples at frequencies recommended by regulatory methods (typically 5-10% of analytical batch size) provides statistical power to identify contamination events and maintain analytical integrity.
Experimental Protocols for Contamination Control
Standardized Environmental Risk Assessment Protocol
The European Medicines Agency's (EMA) guidelines advocate a tiered approach to Environmental Risk Assessment (ERA) for veterinary medicinal products, providing a structured framework for evaluating potential environmental contamination [8]. This protocol can be adapted more broadly for assessing contamination risks in research settings:
Phase I: Initial Exposure Assessment
- Evaluate the environmental exposure potential based on physiochemical characteristics, usage patterns, and disposal pathways
- Calculate Predicted Environmental Concentration (PEC) using standardized models
- Determine if PEC exceeds established thresholds (e.g., PECsoil ≥ 100 μg/kg)
- Products with limited environmental exposure conclude at Phase I
Phase II Tier A: Preliminary Hazard Assessment
- Generate ecotoxicity data using standard model organisms (e.g., Daphnia, algae, fish)
- Calculate Predicted No-Effect Concentration (PNEC)
- Compute PEC/PNEC ratio; proceed to Tier B if ratio >1
Phase II Tier B: Refined Assessment
- Conduct environmental fate studies (hydrolysis, photolysis, biodegradation)
- Perform prolonged ecotoxicity tests with more sensitive endpoints
- Refine PEC and PNEC values based on experimental data
Phase II Tier C: Field Validation
- Execute simulated field studies or mesocosm experiments
- Implement risk mitigation measures if unacceptable risks identified
- Weigh environmental risks against product benefits for approval decisions
Sample Preparation Contamination Control Protocol
Implementing rigorous contamination controls during sample preparation requires standardized procedures for reagent qualification, equipment maintenance, and process verification:
Reagent and Consumable Qualification
- Pre-screen all SPE cartridges and QuEChERS kits using method blanks
- Certify solvent purity through concentrated extracts analyzed by LC-MS/MS
- Establish vendor qualification protocols with acceptance criteria for background contamination
- Implement lot-testing requirements for critical consumables
Instrument Decontamination Procedure
- Execute between-sample needle washes with staggered solvent polarity (water → acetonitrile → methanol → isopropanol)
- Perform weekly system decontamination with 1% Contrad 70 or equivalent detergent
- Validate autosampler carryover using high-low concentration sequences
- Document decontamination efficacy in instrument logs
Process Blank Implementation
- Incorporate method blanks at frequency of 1 per 20 samples minimum
- Include extraction blanks, instrument blanks, and field blanks where applicable
- Establish investigation and corrective action procedures for blank contamination
- Track blank performance metrics for trend analysis
The Scientist's Toolkit: Research Reagent Solutions for Contamination Prevention
Implementing effective contamination control requires strategic selection and application of specialized reagents and materials. The following toolkit catalogs essential solutions for preventing, detecting, and mitigating contamination across sample preparation workflows.
Table 3: Research Reagent Solutions for Contamination Prevention
| Tool/Reagent | Function | Application Context | Contamination Control Mechanism |
|---|---|---|---|
| Captiva EMR-Lipid HF | Lipid removal cartridge | Fatty sample matrices | Size exclusion with hydrophobic interaction reduces co-extractives |
| Resprep FL+CarboPrep Plus | Dual-bed SPE cartridge | Organochlorine pesticides | Florisil + GCB combination enhances selectivity |
| InertSep QuEChERS kit | Multi-residue extraction | Pesticides, veterinary drugs, mycotoxins | Validated sorbent blends minimize interference |
| Q-Sep QuEChERS salts | Extraction salts | PFAS in food/feed | Certified PFAS-free composition |
| Samplify System | Automated sampling | Unattended liquid sampling | Probe cleaning protocol prevents carryover |
| Alltesta Mini-Autosampler | Multi-function autosampler | Microscale sample handling | Dedicated fluidic paths for different sample types |
| PFAS-free vials and caps | Sample containers | Trace-level PFAS analysis | Certified materials prevent background introduction |
| High-purity solvents | Extraction media | All sensitive applications | LC-MS grade with verified contamination profiles |
| Silanized glassware | Laboratory containers | Trace analysis | Prevents analyte adsorption to surfaces |
| Process blanks | Quality control | All analytical methods | Monitors systemic contamination |
| 1-Benzyl-n-methylcyclopentanamine | 1-Benzyl-N-methylcyclopentanamine|CAS 19166-01-9|RUO | Research-use 1-Benzyl-N-methylcyclopentanamine (CAS 19166-01-9). Explore its potential in scientific studies. For Research Use Only. Not for human consumption. | Bench Chemicals |
| (2S)-3-(bromomethyl)but-3-en-2-ol | (2S)-3-(bromomethyl)but-3-en-2-ol|High-Purity | Bench Chemicals |
The selection of appropriate contamination control reagents must be guided by the specific analytical context and potential contamination vectors. For PFAS analysis, this necessitates PFAS-free certified materials throughout the workflow, from SPE cartridges to collection vials [10]. For multi-residue methods targeting diverse analyte classes, balanced sorbent combinations like those in QuEChERS kits provide effective matrix cleanup while minimizing analyte loss [10]. The implementation of automated systems like the Samplify and Alltesta requires validation of cleaning protocols specific to the target analytes and matrices, with particular attention to carryover prevention in high-throughput environments where concentration ranges may vary significantly between samples.
Contamination control in sample preparation represents a multidimensional challenge requiring integrated strategies across environmental, analytical, and procedural domains. The contamination landscape is continuously evolving, driven by increasingly sensitive analytical techniques, expanding regulatory requirements, and growing recognition of the interconnectedness between research quality and environmental impact. Successful navigation of this landscape demands researcher vigilance, methodological rigor, and systematic implementation of the contamination prevention frameworks outlined in this guide. By adopting proactive contamination assessment protocols, leveraging appropriate reagent solutions, validating automated systems, and implementing robust quality control measures, research professionals can significantly enhance data reliability while contributing to the broader scientific goals of reproducibility and environmental stewardship. The principles articulated herein provide a foundational framework for developing contamination-resistant workflows capable of supporting the exacting requirements of modern analytical science across diverse application domains.
In clinical diagnostics and research, the integrity of laboratory results is paramount. The total testing process is a complex pathway that can be segmented into pre-analytical, analytical, and post-analytical phases. Among these, the pre-analytical phase—encompassing everything from test ordering and patient preparation to sample collection, handling, and transport—has been consistently identified as the most error-prone. A contemporary large-scale study analyzing over 11 million specimens found that a striking 98.4% of all laboratory errors occurred in the pre-analytical phase, impacting approximately 0.79% of all specimens [12]. This phase constitutes the fragile foundation upon which all subsequent analytical processes are built; when compromised, it undermines the entire diagnostic enterprise.
The significance of these errors extends beyond statistical concern—they directly threaten patient safety, research validity, and healthcare economics. With an estimated 60-70% of clinical decisions relying on laboratory results, pre-analytical errors can lead to misdiagnosis, inappropriate treatment, and compromised patient safety [13] [14]. This technical guide examines the mechanisms behind pre-analytical vulnerability, details evidence-based prevention strategies, and provides a contamination-focused framework for researchers and drug development professionals dedicated to sample integrity.
Quantitative Analysis of Pre-analytical Errors
Understanding the distribution and frequency of pre-analytical errors is essential for targeted quality improvement. The following table synthesizes data from recent studies on error rates across the testing continuum:
Table 1: Distribution of Errors in the Laboratory Testing Process
| Testing Phase | Error Rate (% of total errors) | Error Rate (Parts Per Million) | Most Common Error Types |
|---|---|---|---|
| Pre-analytical | 46-98.4% | 984,000 PPM | Hemolysis (69.6%), incorrect sample type, collection container errors, insufficient volume [12] [13] |
| Analytical | 0.5-13% | 5,000 PPM | Equipment malfunction, calibration issues, reagent problems [12] [14] |
| Post-analytical | 1.1-19% | 11,000 PPM | Transcription errors, delayed reporting, incorrect interpretation [12] [14] |
When examining specific pre-analytical error types, hemolysis emerges as the dominant concern. One comprehensive study documented 87,317 total errors, of which 60,748 (69.6%) were attributed to hemolysis impacting specimen integrity [12]. The high prevalence of hemolysis underscores the critical importance of proper phlebotomy technique and sample handling procedures. Excluding hemolysis, the remaining pre-analytical errors still account for 94.6% of non-hemolysis related errors, emphasizing that multiple failure points exist throughout the initial testing stages [12].
Table 2: Frequency of Specific Pre-analytical Error Types
| Error Category | Specific Error Types | Relative Frequency |
|---|---|---|
| Sample Collection | Incorrect patient identification, wrong collection tube, improper order of draw, hemolysis | High |
| Sample Handling | Improper mixing, incorrect storage temperature, prolonged transit time | Medium-High |
| Patient Preparation | Non-fasting, medication interference, improper posture | Medium |
| Sample Transport | Tube breakage, exposure to extreme temperatures, delayed delivery | Medium |
| Pre-labeling | Misidentification, wrong tube pre-labeling | Low-Medium |
The Contamination Pathway in Pre-analytical Processes
Contamination represents a particularly insidious category of pre-analytical error, with the potential to completely invalidate test results and derail research outcomes. In low-biomass microbiome studies, for instance, contaminants can disproportionately influence results, potentially leading to false conclusions about microbial presence [4]. The vulnerability of different sample types to contamination varies significantly, with some materials being exceptionally prone to interference.
Contamination can infiltrate samples at multiple points along the pre-analytical pathway, with different mechanisms operating at each stage:
- Sample Collection: Contamination from skin flora, improper sterilization of collection sites, or non-sterile collection devices [14]
- Sample Processing: Cross-contamination between samples during aliquoting, improper homogenization techniques, or use of contaminated tools [15]
- Reagents and Consumables: Impurities in chemicals, kit contaminants, or DNA/RNA contamination in supposedly sterile disposables [4] [16]
- Environmental Exposure: Airborne particles, contaminated work surfaces, or improper storage conditions [4]
The impact of these contaminants is magnified in molecular techniques like qPCR, where the extreme sensitivity of the method can amplify minuscule contaminating DNA fragments, generating false positives and compromising experimental validity [16]. For low-biomass samples, the contaminant "noise" can easily overwhelm the true biological "signal," leading to fundamentally flawed data interpretation [4].
The Pre-pre-analytical Concept
Recognizing that many errors occur before samples even reach the laboratory, experts have further divided the pre-analytical phase to highlight the "pre-pre-analytical" stage [17]. This sub-phase encompasses initial steps including test requesting, patient preparation, sample labeling, and primary collection. Errors introduced at this stage are particularly problematic as they often escape early detection and propagate through subsequent processes.
Professor Mario Plebani's concept of the "Five Rights" in the pre-pre-analytical phase emphasizes: right patient, right test, right time, right sample collection method, and right transportation [17]. Adherence to these principles establishes a foundation for quality that protects subsequent analytical processes.
Evidence-Based Strategies for Error Reduction
Structural and Process Interventions
Implementing a systematic framework for pre-analytical quality control can yield dramatic improvements in error rates. One recent study applied the Structure-Process-Outcome (SPO) model to pre-analytical quality management with significant success [13]. The intervention included:
- Structural Components: Formation of a multidisciplinary team, establishment of a grid management system with laboratory staff assigned to specific hospital areas, implementation of a non-punitive reporting system for non-compliant specimens, and creation of a dedicated specimen transport team [13]
- Process Components: Diverse training programs aligned with established guidelines, development of comprehensive standard operating procedures (SOPs), optimization of information processes with automated error interception, and introduction of barcode technology for patient and specimen identification [13]
This systematic intervention resulted in significantly lower rates of non-compliance across all measured parameters: sample type, collection container, volume, contaminated blood cultures, and coagulated samples (all p < 0.01) [13]. Additionally, the study documented improved nurse knowledge (Cohen's d = 0.44) and behaviors (Cohen's d = 1.56), along with enhanced operational standardization (92.5 ± 3.2 vs 85.7 ± 4.1), patient satisfaction (93.8% vs 87.2%), and clinical doctor trust (91.2% vs 84.5%) [13].
Diagram 1: SPO Model for Quality Management
Practical Contamination Control Protocols
Sample Collection and Handling
Proper blood collection techniques are fundamental to preventing common pre-analytical errors:
- Minimize Hemolysis: Limit tourniquet time, use appropriately sized needles, allow alcohol disinfectant to fully dry before venipuncture, avoid transferring blood from syringe to tube through a needle, and mix tubes by gentle inversion rather than shaking [14]
- Prevent Cross-Contamination: Adhere to correct order of draw (blood cultures → sodium citrate → gel → lithium heparin → EDTA), avoid collecting blood from intravenous lines or the same arm receiving IV fluids, and never transfer blood between tubes [14]
- Ensure Proper Timing: Collect time-sensitive tests (e.g., cortisol, therapeutic drug monitoring) at appropriate intervals, document drug administration times, and note patient position for affected tests [14]
Laboratory Processing Controls
For sample processing, particularly in sensitive molecular applications, implementing strict contamination control protocols is essential:
- Physical Separation: Establish dedicated pre- and post-amplification areas with separate equipment, supplies, and protective gear [16]. Maintain unidirectional workflow from clean to potentially contaminated areas [4] [16]
- Decontamination Procedures: Regularly clean work surfaces and equipment with 70% ethanol, followed by 10-15% fresh bleach solution for DNA removal, allowing 10-15 minutes contact time before wiping with deionized water [4] [16]
- Personal Protective Equipment: Use appropriate PPE including gloves, lab coats, and in some cases face masks or cleanroom suits to minimize human-derived contamination [4]
- Molecular Safeguards: Incorporate uracil-N-glycosylase (UNG) in qPCR master mixes to prevent carryover contamination from previous amplifications [16]
Essential Research Reagents and Solutions
Table 3: Key Reagents and Materials for Contamination Prevention
| Reagent/Material | Function in Contamination Control | Application Notes |
|---|---|---|
| Sodium Hypochlorite (Bleach) | DNA degradation and surface decontamination | Use 10-15% solution, prepare fresh regularly, 10-15 minute contact time [4] [16] |
| 70% Ethanol | Surface disinfection and microbial reduction | Effective for general lab cleaning; does not remove DNA [4] |
| UNG Enzyme | Degrades uracil-containing DNA from previous amplifications | Incorporated into qPCR master mixes; effective against carryover contamination [16] |
| DNA Removal Solutions | Eliminates contaminating DNA from surfaces | Commercial products like DNA Away; critical for DNA-free environments [15] |
| Aerosol-Resistant Filter Tips | Prevents aerosol contamination during pipetting | Essential for sensitive molecular workflows and sample preparation [16] |
Special Considerations for Research Settings
Low-Biomass Microbiome Studies
Research involving low-biomass samples presents unique pre-analytical challenges, as the contaminant signal can easily overwhelm the true biological signal. Consensus guidelines recommend:
- Comprehensive Controls: Include extraction controls, sampling controls (empty collection vessels, air swabs), and PCR controls to identify contamination sources [4]
- Rigorous Decontamination: Beyond standard sterilization, implement DNA removal protocols for all equipment and surfaces [4]
- Environmental Monitoring: Sample the laboratory environment and reagents to establish a contaminant profile [4]
Sample Homogenization Practices
The choice of homogenization method significantly impacts contamination risk:
- Stainless Steel Probes: Durable but require meticulous cleaning between samples, creating potential for cross-contamination and workflow bottlenecks [15]
- Disposable Plastic Probes: Eliminate cross-contamination risk but may lack durability for tough samples [15]
- Hybrid Probes: Combine stainless steel outer shafts with disposable plastic inner rotors, balancing durability and contamination control [15]
Validating cleaning procedures for reusable equipment is essential, including running blank solutions after cleaning to verify absence of residual analytes [15].
The predominance of pre-analytical errors in laboratory testing represents both a formidable challenge and a significant opportunity for quality improvement. The evidence is clear: approximately 75% of laboratory errors originate in the pre-analytical phase, with contamination constituting a major contributor to unreliable results [15]. Addressing this vulnerability requires a systematic approach that integrates structural organization, standardized processes, and continuous quality monitoring.
Successful pre-analytical quality management demands collaboration across disciplines—engaging clinicians, phlebotomists, laboratory scientists, and researchers in a unified system focused on specimen integrity [13] [17]. By adopting evidence-based frameworks like the SPO model, implementing rigorous contamination control protocols, and maintaining vigilance through comprehensive quality indicators, laboratories and research facilities can significantly reduce pre-analytical errors.
The journey toward pre-analytical excellence begins with recognition of a fundamental principle: no degree of analytical sophistication can compensate for a compromised sample. As Professor Plebani aptly observed, "good samples make good assays" [17]. In an era of increasingly sensitive analytical technologies and growing dependence on laboratory data for critical decisions, ensuring the integrity of the pre-analytical phase has never been more essential.
Diagram 2: Laboratory Testing Workflow Phases
Special Considerations for Low-Biomass and High-Sensitivity Applications
Low-biomass environments, which contain minimal native microbial content, present unique challenges for molecular analysis. These include certain human tissues (respiratory tract, placenta, blood), processed pharmaceuticals, drinking water, hyper-arid soils, and the deep subsurface [4] [18]. In these contexts, the DNA from contaminants originating from reagents, laboratory environments, or researchers can equal or exceed the target signal, fundamentally compromising data integrity and biological conclusions [4] [18]. The inherent sensitivity of next-generation sequencing, while powerful, becomes a double-edged sword, efficiently detecting both target sequences and contaminating DNA [19]. This technical guide outlines a systematic framework for preventing, identifying, and mitigating contamination throughout the experimental workflow, from sample collection to data analysis, ensuring the validity of results in low-biomass and high-sensitivity applications.
The table below summarizes the primary contamination types and their impacts:
Table 1: Contamination Types and Their Impacts in Low-Biomass Studies
| Contamination Type | Description | Primary Sources | Impact on Data |
|---|---|---|---|
| External Contaminant DNA | DNA introduced from sources other than the sample [18]. | Reagents, kits, laboratory environment, researchers [4] [18]. | Can be misinterpreted as a genuine signal, leading to false positives and skewed community profiles [18] [20]. |
| Cross-Contamination (Well-to-Well Leakage) | Transfer of DNA or sequence reads between samples processed concurrently [4] [20]. | Adjacent wells on sample plates, aerosol generation during liquid handling [4] [20]. | Creates artificial similarity between samples, obscuring true biological patterns and relationships [20]. |
| Host DNA Misclassification | Predominantly a concern in metagenomics; host DNA is misidentified as microbial [20]. | High abundance of host DNA in samples like human tissue or blood [20]. | Generates noise and can produce artifactual signals if confounded with a phenotype, impeding true signal detection [20]. |
A Proactive Framework for Contamination Prevention
A successful low-biomass study requires a proactive, preventative approach integrated into every stage of experimental design. Relying solely on post-hoc computational correction is insufficient.
Strategic Experimental Design
The single most important step is to avoid batch confounding, where the variable of interest (e.g., case vs. control status) is processed in separate batches [20]. When batches are confounded with the study groups, technical artifacts like varying contamination profiles or processing biases can create false associations [20]. Active randomization or tools like BalanceIT should be used to ensure that batches contain a similar ratio of all sample types and controls [20]. Furthermore, the analysis should assess the generalizability of results across batches to confirm findings are not batch-specific artifacts [20].
Rigorous Pre-Analytical and Laboratory Practices
Contamination control begins before a sample enters the laboratory. During sample collection, all equipment, tools, and vessels should be single-use and DNA-free where possible [4]. When reusables are necessary, thorough decontamination is critical. A two-step process of 80% ethanol (to kill organisms) followed by a nucleic acid degrading solution like sodium hypochlorite (bleach) or commercially available DNA removal products is recommended, as sterility alone does not guarantee the absence of cell-free DNA [4]. Personnel should use appropriate personal protective equipment (PPE) including gloves, cleansuits, and masks to act as a barrier against human-derived contamination from skin, hair, or aerosols generated by breathing [4].
Within the lab, meticulous practices continue. The use of disposable plastic consumables, such as homogenizer probes, can virtually eliminate the risk of cross-contamination between samples [15]. For reusable tools, validating cleaning procedures is essential. This can involve running a blank solution through the equipment after cleaning to check for residual analytes [15]. Laboratory surfaces should be routinely decontaminated with solutions like 70% ethanol or 10% bleach, with specialized products like DNA Away used to eliminate persistent nucleic acids [15]. When handling samples in multi-well plates, spinning down plates before seal removal and removing seals slowly and carefully can reduce the risk of well-to-well leakage [15].
Essential Validation and Control Methodologies
Implementing a Comprehensive Control Strategy
The use of process controls is non-negotiable for identifying the nature and extent of contamination [4] [20]. These controls should be included in every processing batch and carried through the entire experimental workflow alongside actual samples.
Table 2: Essential Process Controls for Low-Biomass Studies
| Control Type | Composition & Purpose | When to Collect/Use |
|---|---|---|
| Extraction Blank Control | An empty tube that undergoes the full DNA/RNA extraction process [18] [20]. | With every batch of extractions; identifies contaminants from reagents and the extraction process itself [21]. |
| No-Template Control (NTC) | A water sample included during the PCR amplification or library preparation step [20]. | With every amplification batch; identifies contaminants present in polymerase mixes and other amplification reagents [20]. |
| Sampling/Kit Control | An empty collection vessel or a swab exposed to the air in the sampling environment [4]. | During sample collection; identifies contaminants from collection kits and the sampling environment [4]. |
| Positive Control | A known, low-biomass mock community. Validates that the entire workflow can detect expected signals at relevant concentrations. | With each processing batch; assesses sensitivity and detects inhibition. |
It is crucial to collect multiple types of controls and to include them in every batch, as contamination profiles can vary over time and by location [20] [21]. The optimal number of controls is study-dependent, but at least two controls per type per batch are recommended to account for variability [20].
Cleaning Validation Protocol for Laboratory Equipment
For reusable laboratory equipment, a formal cleaning validation protocol ensures effective decontamination. The following methodology, adapted from pharmaceutical quality control, provides a structured approach [22].
- Identify a Worst-Case Active Pharmaceutical Ingredient (API) or Analytic: Select a molecule that is difficult to remove due to low water solubility and/or high potency. The rationale is that a protocol effective for the worst-case analyte will be effective for others [22]. For example, Oxcarbazepine, an anticonvulsant with very low water solubility (0.07 mg/mL), is often used as a benchmark [22].
- Establish Residue Acceptable Limits (RALs): Define a scientifically justified threshold for residual contamination. A common industry standard is 10 ppm of a substance, though study-specific limits based on toxicity or analytical sensitivity may be applied [22] [23].
- Select Solvents for Residue Recovery: Choose solvents that effectively solubilize the target analyte. For Oxcarbazepine, acetonitrile and acetone are suitable due to their high solubility for this compound and common availability [22].
- Perform Recovery Studies Using Swab and Rinse Methods:
- Swab Method: For flat or irregular surfaces (e.g., Petri dishes, spatulas). A polyester swab is pre-wetted with solvent, used to scrub a defined surface area (e.g., 100 cm²) with horizontal and vertical strokes, and then placed in a test tube for extraction before analysis [22].
- Rinse Method: For equipment with internal geometries (e.g., pipes, tubes). A defined volume of solvent (e.g., 10 mL) is agitated within the equipment to ensure contact with all surfaces, and the resulting solution is collected for analysis [22].
- Analyze and Document: Use sensitive analytical techniques (e.g., HPLC) to quantify residue levels. The protocol is validated if results are consistently below the established RAL. This process must be thoroughly documented [22] [23].
The workflow for this validation process is systematic and iterative.
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagent Solutions for Contamination Control
| Item | Function & Rationale | Example Application |
|---|---|---|
| Polyester Swabs | Surface sampling for cleaning validation; chosen for strength and consistency in residue recovery [22]. | Swabbing a 100 cm² area of a glass mortar after cleaning to validate Oxcarbazepine removal [22]. |
| DNA Degrading Solution | Chemically destroys contaminating DNA on surfaces and equipment, going beyond microbial killing [4]. | Decontaminating laboratory benches, pipettors, and reusable tools before setting up PCR reactions [4] [15]. |
| Ultra-Pure Solvents | High-purity acetonitrile and acetone used to dissolve and recover residual analytes during cleaning validation [22]. | Extracting API residues from a swab or as a rinse solvent for laboratory glassware [22]. |
| Disposable Homogenizer Probes | Single-use probes for sample homogenization that eliminate the risk of carryover contamination between samples [15]. | Processing multiple low-biomass tissue samples sequentially without a cleaning step [15]. |
| Phosphate-Free Detergent | Used in manual or automated cleaning of labware; phosphate-free formulations are more environmentally friendly [22]. | Cleaning glassware and stainless-steel equipment in an industrial laboratory washer [22]. |
| Spiro[3.5]nonane-9-carboxylic acid | Spiro[3.5]nonane-9-carboxylic Acid|CAS 1558342-25-8 | Buy Spiro[3.5]nonane-9-carboxylic acid (CAS 1558342-25-8), a C10H16O2 building block for research. For Research Use Only. Not for human or veterinary use. |
| 2,3,3-Trimethyl-5-phenyl-3H-indole | 2,3,3-Trimethyl-5-phenyl-3H-indole|CAS 294655-87-1 |
Data Analysis and Interpretation in a Contamination-Aware Context
Once data is generated, a contamination-aware analytical approach is vital. Data from all process controls must be integrated into the bioinformatic pipeline. Several computational tools can help statistically identify and subtract contaminant sequences based on their prevalence and abundance in controls compared to real samples [4] [20]. However, these methods have limitations, particularly when well-to-well leakage contaminates the negative controls themselves, violating their core assumptions [20]. Therefore, the most robust results are achieved when these tools are used to support conclusions based on a well-designed experiment with extensive controls, rather than to salvage a poorly controlled one.
Finally, reporting standards must be elevated. The research community is moving toward minimal reporting criteria, such as the "RIDE" checklist (Reporting of Ix-D-E), to ensure transparency [18] [19]. Authors should explicitly detail all controls used, the bioinformatic decontamination steps applied, and acknowledge the limitations of their study in the context of potential residual contamination. This level of transparency allows reviewers, editors, and the broader scientific community to accurately assess the validity of the findings.
Building Your Defenses: Practical Protocols for a Contamination-Free Workflow
In molecular biology and diagnostic laboratories, the exquisite sensitivity of polymerase chain reaction (PCR) and other amplification techniques makes them vulnerable to contamination from previously amplified products, known as amplicons. A typical PCR reaction can generate as many as 10^9 copies of a target sequence, and if aerosolized, even the smallest droplet can contain up to 10^6 amplification products [24]. Without proper controls, this buildup of aerosolized amplification products will contaminate laboratory reagents, equipment, and ventilation systems, ultimately leading to false-positive results that compromise research integrity and diagnostic accuracy [24].
Documented cases exist where false-positive PCR findings have led to serious consequences, including misdiagnosed cases of Lyme disease (one with fatal outcome) and formal retraction of published manuscripts [24]. Within the broader context of preventing contamination during sample preparation research, the strategic separation of pre- and post-amplification areas represents the most fundamental defense against amplicon carryover contamination. This whitepaper outlines an evidence-based, practical framework for implementing this critical separation, providing researchers, scientists, and drug development professionals with the knowledge to design laboratories that ensure data reliability and reproducibility.
Understanding Amplification Product Contamination
Amplicon carryover contamination represents the most significant challenge in laboratories performing nucleic acid amplification. The primary sources of contamination include:
- Previously amplified products: The vast quantity of amplicons generated in prior amplification reactions accumulates in the laboratory environment over time [24].
- Plasmid clones: Recombinant plasmids derived from previously analyzed organisms may be present in large numbers in the laboratory environment [24].
- Cross-contamination between samples: High concentrations of target organisms in clinical specimens can lead to contamination between samples during processing [24].
The vulnerability of amplification techniques stems from their designed sensitivity. When working with low-biomass samples, the contaminant "noise" can easily overwhelm the target "signal," leading to spurious results and incorrect conclusions [4]. This is particularly problematic in applications such as pathogen detection, microbial microbiome studies in low-biomass environments, and clinical diagnostics where results directly impact patient care [4].
Consequences of Contamination
The implications of amplification product contamination extend beyond wasted reagents and time:
- Compromised Research Integrity: Contamination can distort ecological patterns and evolutionary signatures, potentially misleading entire research fields [4].
- Diagnostic Errors: In clinical settings, false-positive results can lead to misdiagnosis and inappropriate treatment selection, with documented cases of patient harm [24].
- Reproducibility Crisis: Contamination contributes to the broader scientific reproducibility crisis, where published results cannot be replicated by other laboratories [4].
Core Principles of Laboratory Zoning
The Unidirectional Workflow
The foundational principle for preventing amplicon carryover contamination is implementing a strict unidirectional workflow. This means physically separating the laboratory into distinct areas and ensuring that personnel, samples, reagents, and equipment move in a single direction—from clean pre-amplification areas to contaminated post-amplification areas, with no backtracking [24].
All traffic must flow unidirectionally from reagent preparation to sample preparation, to amplification, and finally to amplification product analysis [24]. These areas should be optimally physically separated and preferably situated at a substantial distance from each other [24].
Detailed Zone Specifications
A properly designed amplification laboratory should include at a minimum four distinct physical areas:
1. Reagent Preparation Area (Clean Zone)
- Function: Preparation of master mixes, aliquoting of reagents, and storage of clean materials.
- Features: Positive air pressure relative to other areas, dedicated equipment, UV light source for decontaminating surfaces and equipment [24].
- Critical controls: Access restricted to personnel performing reagent preparation, dedicated laboratory coats and supplies.
2. Sample Preparation Area
- Function: Nucleic acid extraction from clinical or research specimens.
- Features: Physically separated from reagent preparation and amplification areas, dedicated equipment for extraction, biosafety cabinets for processing potentially infectious samples [24].
- Critical controls: Unidirectional movement of samples into this area only, no amplified products permitted.
3. Amplification Area
- Function: Setup of amplification reactions and running of thermal cyclers.
- Features: Restricted access, dedicated equipment, negative air pressure relative to cleaner areas.
- Critical controls: No sample extraction or reagent preparation permitted, physical separation from post-amplification areas.
4. Post-Amplification Analysis Area (Contaminated Zone)
- Function: Analysis of amplification products (e.g., gel electrophoresis, fragment analysis).
- Features: Physically isolated from all pre-amplification areas, dedicated equipment and supplies.
- Critical controls: No movement of materials or personnel back toward cleaner areas, distinct laboratory coats and equipment.
The following diagram illustrates the proper unidirectional workflow and critical control points in a separated lab design:
Laboratory Equipment and Environmental Controls
Specialized Containment Equipment
Proper selection of containment equipment is essential for protecting both samples and personnel. The table below compares the primary types of containment devices used in molecular biology laboratories:
Table 1: Comparison of Laboratory Containment Equipment
| Feature | Biological Safety Cabinet (Class II) | Laminar Flow Cabinet | Chemical Fume Hood |
|---|---|---|---|
| Primary Protection | Personnel, product, and environment [25] [26] | Product only [27] [25] | Personnel only [26] [28] |
| Air Filtration | HEPA-filtered intake and/or exhaust [25] [26] | HEPA-filtered supply air [27] | No filtration; direct exhaust [26] |
| Airflow Pattern | Laminar, sterile downflow [26] | Laminar flow (horizontal or vertical) [27] | Inward flow of unfiltered lab air [28] |
| Recirculation | Can recirculate HEPA-filtered air (Class II A) [26] | 100% recirculation within workspace [27] | No recirculation; 100% exhaust [28] |
| Ideal Use Case | Sample preparation for nucleic acid extraction [24] | Reagent preparation and master mix aliquoting [27] | Handling volatile chemicals during nucleic acid extraction [26] |
Environmental Monitoring and Decontamination
Rigorous environmental controls are essential for maintaining contamination-free pre-amplification areas:
- Surface Decontamination: Work stations should be cleaned with 10% sodium hypochlorite solution (bleach), which causes oxidative damage to nucleic acids, followed by ethanol removal of the bleach [24]. Note that bleach treatment renders specimens unsuitable for amplification, so it should only be used for surface decontamination [24].
- UV Irradiation: After packages have been opened, all pipettes and disposable devices should be stored in a UV light box. Preparation of amplification master mix and specimen processing should also be carried out in a UV light box [24]. UV light induces thymidine dimers and other covalent modifications in DNA that render contaminating nucleic acid inactive as a template for amplification [24].
- Air Quality Management: Proper ventilation with controlled air pressure differentials (positive pressure in clean areas, negative pressure in contaminated areas) helps prevent aerosolized amplicons from entering clean areas [24].
Procedural Controls and Best Practices
Personnel Management and Training
Human factors represent both the greatest contamination risk and the most powerful control point. Laboratory personnel must receive comprehensive training regarding:
- Awareness of Contamination Sources: Technologists must be alert to the possibility of transferring amplification products on their hair, glasses, jewelry, and clothing from contaminated rooms to clean rooms [24].
- Strict Adherence to Unidirectional Flow: Personnel should complete all tasks in one area before moving to the next, with no backtracking between areas [24].
- Proper Use of Personal Protective Equipment (PPE): Dedicated lab coats, gloves, and other PPE for each area, with color-coding to prevent accidental transfer between areas [4].
Mechanical and Chemical Barriers
Implementation of both mechanical and chemical barriers provides redundant protection against contamination:
- Physical Barriers: Strict separation of laboratory areas with necessary instruments, disposable devices, laboratory coats, gloves, aerosol-free pipettes, and ventilation systems dedicated to each area [24].
- Chemical Barriers: In addition to surface decontamination with bleach, incorporation of enzymatic inactivation methods such as uracil-N-glycosylase (UNG) provides pre-amplification sterilization of potential contaminants [24].
Practical Workflow Implementation
The following workflow diagram details the specific procedures and contamination controls for each laboratory zone:
Research Reagent Solutions and Materials
The following toolkit details essential materials and reagents for implementing effective contamination control in amplification laboratories:
Table 2: Essential Research Reagent Solutions for Contamination Control
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Uracil-N-Glycosylase (UNG) | Enzymatic degradation of carryover amplicons [24] | Incorporated into PCR mix; hydrolyzes uracil-containing contaminants from previous reactions [24] |
| dUTP | Substitute for dTTP in PCR reactions [24] | Allows incorporation of uracil into amplicons, making them susceptible to UNG degradation [24] |
| Sodium Hypochlorite (Bleach) | Surface decontamination [24] | 10% solution causes oxidative damage to nucleic acids; surfaces must be rinsed with ethanol after use [24] |
| HEPA Filters | Airborne particulate removal [27] [25] | Essential for BSCs and laminar flow cabinets; removes 99.97% of particles ≥0.3μm [27] |
| UV Light Source | Nucleic acid decontamination [24] | Induces thymidine dimers; used to sterilize surfaces and equipment in pre-amplification areas [24] |
| DNA-Decontaminating Solutions | Surface sterilization [4] | Commercial formulations or 80% ethanol followed by DNA removal solutions for sampling equipment [4] |
Validation and Quality Control Measures
Monitoring Contamination
Regular monitoring is essential for detecting contamination events before they compromise experimental results:
- Negative Controls: Multiple negative controls should be included in every amplification run, including no-template controls (NTC) that contain all reaction components except the target nucleic acid [24] [4].
- Environmental Monitoring: Regular swabbing of work surfaces and equipment in pre-amplification areas followed by amplification to detect amplicon contamination [24].
- Reagent Testing: Periodic testing of critical reagents (especially water and master mix components) for the presence of amplifiable nucleic acids [4].
Procedural Audits
Systematic reviews of laboratory procedures help maintain contamination control standards:
- Workflow Audits: Regular assessment of personnel movement and material transfer between areas to ensure compliance with unidirectional workflow [24].
- Equipment Calibration: Annual certification of biological safety cabinets and laminar flow cabinets to ensure proper airflow and filtration [25].
- Documentation Review: Maintenance of detailed records for reagent preparation, lot numbers, and quality control results to facilitate troubleshooting of contamination events [4].
Strategic laboratory design with strict physical separation of pre- and post-amplification areas represents the cornerstone of effective contamination prevention in molecular biology research and diagnostics. When implemented as part of a comprehensive approach that includes appropriate equipment selection, procedural controls, and rigorous quality monitoring, this separation provides the foundation for reliable, reproducible amplification results.
The unidirectional workflow principle, coupled with mechanical barriers, chemical decontamination, and enzymatic sterilization methods, creates a multi-layered defense against amplicon carryover contamination. As amplification technologies continue to evolve toward greater sensitivity and throughput, maintaining these fundamental contamination control practices becomes increasingly critical for research integrity and diagnostic accuracy.
By adopting the evidence-based strategies outlined in this whitepaper, researchers and laboratory managers can create environments that support robust molecular analysis while minimizing the risk of false-positive results due to amplification product contamination.
In sample preparation research, the integrity of scientific findings depends fundamentally on the effectiveness of decontamination protocols. Contaminating biological molecules, particularly DNA, can compromise experiments, lead to erroneous conclusions, and set back drug development timelines. Healthcare-associated infections (HAIs) remain a significant patient safety risk, with approximately 1.7 million cases reported annually in the United States alone, highlighting the critical importance of stringent environmental cleaning protocols [29]. The enduring challenge of infections caused by surface-surviving pathogens like Staphylococcus aureus and Clostridioides difficile demands a comprehensive approach to environmental design that supports optimal cleaning and disinfection protocols [29].
Within research laboratories, the challenge extends to invisible contaminants that can jeopardize months of careful work. DNA contamination presents particular difficulties for sensitive techniques like polymerase chain reaction (PCR) and next-generation sequencing. Recent studies have confirmed that bacterial DNA contamination is present in seven of nine commercially available PCR enzyme products, originating from a variety of bacterial species [30]. This contamination can lead to the false detection of bacterial communities in samples that should be sterile, potentially invalidating critical research findings in microbiome studies and drug development [30].
The interaction between surface materials and cleaning efficacy further complicates decontamination strategies. Research demonstrates that material characteristics such as porosity, texture, and chemical composition significantly affect pathogen survival and the success of disinfection efforts [29]. Nonporous, smooth materials in high-touch areas have been shown to support more effective infection prevention due to their compatibility with both chemical and non-chemical disinfection methods [29]. This technical guide provides researchers with evidence-based strategies for selecting and implementing decontamination protocols that protect sample integrity throughout the research workflow.
Decontamination Fundamentals: Principles and Definitions
Key Terminology and Mechanisms
Establishing effective decontamination protocols begins with understanding the precise terminology and mechanisms involved. According to Centers for Disease Control and Prevention (CDC) guidelines adopted in recent scientific reviews, the following definitions are essential [29]:
- Cleaning refers to the physical removal of soil, dust, and organic matter from surfaces, typically using water, detergents, and mechanical action. This process does not necessarily destroy microorganisms but reduces their numbers and removes organic material that might protect them.
- Disinfection refers to the use of chemical or physical agents (e.g., disinfectant wipes, sprays, or UV light) to kill or inactivate pathogenic microorganisms on surfaces. Unlike sterilization, disinfection does not eliminate all microorganisms but reduces them to a level safe for public health.
- Decontamination is a broader term that includes both cleaning and disinfection steps to render a surface safe for use.
- Sanitation is generally defined as reducing microbial contamination to a level considered safe by public health standards, often without specifying the methods used.
The efficacy of decontamination agents depends on their mechanism of action. Chemical disinfectants like sodium hypochlorite (bleach) exert their effects through protein denaturation and irreversible oxidation of organic compounds [31]. Alcohols, most effective at 60-90% concentration, cause membrane damage and protein denaturation, relying on water molecules for optimal virucidal activity [31]. Physical methods like UV radiation damage DNA through oxidation of bases, introducing single- and double-strand breaks in DNA molecules [32].
The Research Context: Special Considerations for Sample Preparation
In research environments, particularly those involving molecular techniques, decontamination requirements extend beyond pathogen control to include the elimination of trace nucleic acids that could contaminate sensitive experiments. The consequences of contamination are particularly severe in fields like microbiome research, forensic analysis, and drug development, where minute quantities of contaminating DNA can generate false results.
The stability and ubiquity of DNA in the environment make nucleic acid contamination of laboratory consumables and reagents nearly inevitable [30]. This has led to the coining of the term "kitome" – contaminating bacterial sequences that result from laboratory consumables and nucleic acid isolation kits [30]. Despite widespread knowledge of this issue, only a minority of microbiome papers report using methodology to control for contamination, and most studies lack specific negative controls [30].
The sensitivity of modern analytical techniques exacerbates these challenges. Improved typing kits for forensic analysis may allow STR profiling on DNA extracted from only a few cells, while mitochondrial DNA analysis permits testing of even lower DNA input amounts due to the high copy number of mtDNA in each cell [32]. At these sensitivity levels, eliminating potential sources of contamination through rigorous decontamination protocols becomes essential for research validity.
Quantitative Comparison of Decontamination Strategies
Chemical Agent Efficacy on Different Surface Types
The efficiency of decontamination strategies varies significantly based on the cleaning agent, application method, and surface material. A 2022 study systematically evaluated ten different cleaning strategies for their ability to remove contaminating DNA molecules from plastic, metal, and wood surfaces [32]. The results demonstrated substantial differences in DNA removal efficiencies between cleaning strategies and across different surfaces.
Table 1: Efficiency of Cleaning Strategies for Cell-Free DNA Removal Across Surfaces [32]
| Cleaning Agent | Plastic (% DNA Recovered) | Metal (% DNA Recovered) | Wood (% DNA Recovered) |
|---|---|---|---|
| No treatment (Control) | 100% | 100% | 100% |
| 70% Ethanol | 19.8% | 3.3% | 4.3% |
| UV Radiation (20 min) | 2.9% | 0.6% | 0.3% |
| Ethanol + UV | 0.9% | 0.2% | 0.1% |
| Fresh Bleach (0.54%) | 0.3% | 0.3% | 0.3% |
| Stored Bleach (0.4%) | 0.3% | 0.3% | 0.3% |
| 1% Virkon | 0.004% | 0.002% | 0.001% |
| 10% Trigene | 0.3% | 0.3% | 0.3% |
| DNA Remover | 0.2% | 0.03% | 0.01% |
For cell-free DNA, the most efficient cleaning strategies were sodium hypochlorite solutions (bleach) and Trigene, for which a maximum of 0.3% DNA was recovered on all three surfaces [32]. When testing with whole blood (cell-contained DNA), Virkon demonstrated superior efficacy, with a maximum of 0.8% of the deposited DNA recovered after decontamination [32]. The recoveries after using these effective cleaning strategies correspond to DNA from only a few cells, out of 60 ng of cell-free DNA or thousands of deposited blood cells [32].
Application Method Efficacy: Spraying vs. Wiping
The method of disinfectant application significantly impacts decontamination efficacy. A 2025 systematic review compared spraying disinfectants versus wiping for SARS-CoV-2 infection prevention, findings that have relevance for general decontamination protocols [31]. While the review found no direct human studies comparing spraying with wiping, it did identify important indirect evidence from laboratory studies.
Table 2: Efficacy Comparison of Spraying vs. Wiping Application Methods [31]
| Application Method | Conditions | Efficacy Results |
|---|---|---|
| Spraying (Dry Fog) | 8,700 ppm hypochlorous acid or 56,400 ppm hydrogen peroxide | Reduced infectious viral titer |
| Wiping | 1,000 ppm sodium hypochlorite for 1 minute | Completely reduced SARS-CoV-2 viruses on stainless steel |
| Wiping | 500 ppm bleach for 5 minutes | Completely reduced virus on kraft paper and polypropylene |
| Wiping | 1,000 ppm bleach for 5 minutes | No viruses detected on any surface |
The review concluded that both spraying disinfectants as dry fog and wiping have disinfectant effects on surfaces and materials, though wiping incorporates a mechanical component that may enhance efficacy [31]. During wiping, the disinfectant is spread and rubbed over the surface, which not only disinfects but also dislodges particles from the surface, potentially making it more effective than spraying alone [31]. However, wiping increases the likelihood of disinfectant contact with a person's skin, requiring appropriate personal protective equipment (PPE) [31].
Experimental Protocols for Decontamination Efficacy Testing
Standardized DNA Decontamination Testing Protocol
Based on methodologies from published studies, researchers can implement the following protocol to evaluate decontamination efficacy in their own laboratory settings [32]:
Materials and Reagents:
- Test surfaces (plastic, metal, wood) cut into standardized dimensions (e.g., 5×5 cm)
- DNA solutions (cell-free DNA and whole blood samples)
- Calibrated spray bottles for liquid cleaning agents
- Cotton swabs for sample collection
- DNA extraction kit (e.g., DNeasy Blood and Tissue Kit)
- Real-time PCR system and reagents for quantitative analysis
Procedure:
- Sample Application: Deposit 10 μL of DNA solution (e.g., 6 ng/μL) or whole blood in marked circles on test surfaces. Spread with a pipette tip within the circle and allow to dry for two hours.
- Decontamination Treatment: Apply liquid cleaning agents using one spray from a calibrated spray bottle. Wipe cleaned areas in three circular movements using dust-free paper. For most agents, allow surfaces to dry for 120 minutes. For Trigene, spray with a single spray of water before wiping, then wait 10 minutes.
- Sample Collection: Swab the entire marked area for each sample with a cotton swab moistened in 0.9% sodium chloride. Include positive controls (no decontamination) and negative controls (surfaces without DNA/blood addition).
- DNA Extraction and Quantification: Extract DNA using commercial kits, eluting in 100 μL final volume. Quantify mitochondrial DNA using real-time PCR with specific primers (e.g., mt-8294F/mt-8436R) [32].
- Data Analysis: Calculate cleaning efficiency as a percentage of positive controls. Apply statistical methods (e.g., 1.5× interquartile rule) to identify potential outliers in biological replicates.
This protocol enables standardized comparison of decontamination strategies across different laboratory environments and surface types, providing empirical data to inform facility-specific protocols.
Validation Protocol for PCR Reagent Contamination
To address the specific challenge of PCR reagent contamination identified in recent studies, implement the following quality control protocol [30]:
Materials:
- Multiple commercial PCR enzymes from different manufacturers
- PCR primers for bacterial 16S rRNA (e.g., V3-4 region)
- Gel electrophoresis system or capillary electrophoresis
- Sanger sequencing capabilities
Procedure:
- Reagent Testing: For each PCR enzyme, prepare two reaction sets: one with E. coli DNA as a positive control template, and one with nuclease-free water instead of template DNA.
- PCR Amplification: Perform amplification under manufacturer-recommended conditions using bacterial 16S rRNA primers.
- Contamination Detection: Separate PCR products by gel electrophoresis. Look for bands of equivalent size to the target region (approximately 500 bp) in water control reactions.
- Contaminant Identification: Excise bands from gels and submit for Sanger sequencing. Use BLAST analysis against GenBank to identify contaminating species.
This accessible protocol requires only endpoint PCR and Sanger sequencing, making it feasible for laboratories without access to expensive high-throughput sequencing infrastructure [30]. Regular implementation of this quality control measure ensures that contaminating DNA sequences can be identified and accounted for in experimental design and data interpretation.
Workflow Integration and Strategic Planning
Comprehensive Decontamination Workflow
The following workflow diagram illustrates a systematic approach to decontamination in research environments, integrating multiple strategies to address different contamination risks:
Diagram 1: Comprehensive Decontamination Decision Workflow
Decontamination in Multi-Product Biologics Facilities
For drug development professionals working in multi-product biologics facilities, cleaning validation presents unique challenges. These environments require demonstrating effective line clearance of one bioprocess before introducing a subsequent process to the shared facility [33]. The following strategic approach ensures both safety and efficiency:
Risk-Based Validation Framework:
- Implement health-based assessments using Acceptable Daily Exposure (ADE) or Permitted Daily Exposure (PDE) limits rather than arbitrary cleaning limits [33].
- Apply Maximum Allowable Carry Over (MACO) calculations that consider the amount of shared surface area in multiproduct facilities [33].
- Employ Failure Mode and Effects Analysis (FMEA) to systematically assess potential risks, mitigate them, and monitor outcomes [33].
Facility and Equipment Design Considerations:
- Design facility layout with operational segregation as a basic requirement [33].
- Select equipment with smooth, crevice-free, self-draining surfaces that are impervious to process streams and cleaning agents [33].
- Implement single-use systems where practical to reduce product-to-product cleaning requirements [33].
- Incorporate visual inspection as a mandatory component of cleaning validation programs [33].
This systematic approach to cleaning validation is particularly crucial for biologics APIs, which are often highly potent with very low clinical doses, requiring extremely sensitive analytical methods to verify cleaning efficacy [33].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Reagents and Equipment for Decontamination Protocols
| Item | Function | Application Notes |
|---|---|---|
| Sodium Hypochlorite (Bleach) | Chemical disinfection through protein denaturation | Effective at 0.5-1.0% concentration; completely eliminates DNA at 1000 ppm with 5-minute contact time [31] [32] |
| 70% Ethanol | Disinfection through membrane damage and protein denaturation | Effective for surface decontamination; less effective on cell-free DNA than bleach (3.3-19.8% DNA recovery) [32] |
| Hydrogen Peroxide Solutions | Oxidation of cellular components | Vapor phase systems effective for room decontamination; 56,400 ppm concentration reduced infectious viral titer in dry fog applications [31] |
| Virkon | Broad-spectrum disinfectant | Superior efficacy on cell-contained DNA in blood (0.8% recovery); 1% solution recommended [32] |
| Trigene | Disinfectant cleaner | Effective on cell-free DNA (0.3% recovery); requires water spray before wiping [32] |
| UV Radiation Chambers | DNA damage through base oxidation and strand breaks | 254 nm wavelength, 20+ minutes exposure; effective as part of combination approach [32] |
| DNA Remover | Specific DNA degradation | Specialized formulation for DNA contamination; effective across surfaces (0.01-0.2% recovery) [32] |
| Real-time PCR Systems | Quantification of residual DNA | Essential for validation studies; mitochondrial DNA assays provide high sensitivity [32] |
| Aerosol-Resistant Pipette Tips | Prevention of cross-contamination | Critical for maintaining sample integrity during liquid handling [32] |
| DNase Treatments | Enzymatic DNA degradation | Specifically targets double-stranded DNA; useful for treating PCR master mixes [30] |
| 2-(2-Chloropyridin-4-yl)propan-2-ol | 2-(2-Chloropyridin-4-yl)propan-2-ol, CAS:1240620-98-7, MF:C8H10ClNO, MW:171.62 | Chemical Reagent |
| (R)-5,6,7,8-tetrahydroquinolin-8-ol | (R)-5,6,7,8-Tetrahydroquinolin-8-ol|Enantiopure |
Emerging Trends and Future Directions
The field of decontamination continues to evolve with several emerging trends that will impact research environments. By 2025, technological innovations are expected to transform standard practices:
Advanced Decontamination Technologies:
- Automated and Robotic Systems: UV-C disinfection robots and automated vapor-phase hydrogen peroxide systems are becoming increasingly sophisticated, with integration of IoT and AI technologies leading to 30% increases in efficiency and 25% reductions in human error in pharmaceutical cleaning procedures [34].
- Smart Monitoring Systems: By 2025, 80% of pharmaceutical facilities are projected to implement real-time monitoring systems for decontamination processes, enabling continuous compliance with regulatory standards [34].
- Sustainable Formulations: Growing environmental concerns are driving development of eco-friendly decontamination agents. By 2025, 60% of pharmaceutical companies are estimated to switch to eco-friendly decontamination agents, resulting in a 40% reduction in harmful chemical discharge [34].
Enhanced Personal Protective Equipment: The emergence of smart PPE incorporating sensors that monitor environmental conditions, detect contaminants, and track wearer vital signs is expected to significantly enhance safety. By 2025, 75% of pharmaceutical facilities are projected to implement smart PPE systems, potentially reducing workplace accidents related to decontamination processes by 35% [34].
Advanced Contamination Control for Sensitive Techniques: As research techniques become more sensitive, decontamination protocols must evolve accordingly. The research community is developing:
- Standardized reference materials to enhance consistency, accuracy, and reproducibility across laboratories [35].
- Advanced microarray technologies with enhanced sensitivity for detecting short or mixed DNA sequences [35].
- Therapeutic oligonucleotide characterization methods to address samples influenced by medical treatments [35].
These advancements, coupled with the fundamental protocols outlined in this guide, provide researchers with a comprehensive framework for implementing effective decontamination strategies that protect sample integrity throughout the research workflow.
Personal Protective Equipment (PPE) and Aseptic Technique Mastery
In sample preparation research, the integrity of scientific data is fundamentally dependent on the purity of the biological materials under investigation. Contamination by microbial pathogens or environmental particulates can compromise experimental results, leading to erroneous conclusions, wasted resources, and delayed drug development timelines. Healthcare-associated infections demonstrate the severe consequences of protocol breaches, with over 2 million patients affected annually in the United States and nearly 99,000 deaths from preventable infections [36] [37]. Similarly, in research settings, laboratory-acquired infections and sample contamination represent significant preventable risks that can be mitigated through rigorous aseptic technique and appropriate personal protective equipment (PPE) use [38] [39].
Aseptic technique comprises the procedures and protocols that prevent contamination of research samples and protect personnel from exposure to hazardous materials. It forms the foundation of reliable science in biological research and processing [38]. This guide examines the critical integration of PPE within comprehensive aseptic practices, providing researchers with evidence-based methodologies to ensure sample integrity and personnel safety in pharmaceutical development and basic research contexts.
Table: Key Contamination Statistics in Healthcare and Research Settings
| Metric | Statistic | Source |
|---|---|---|
| Patients affected by healthcare-associated infections annually | Over 2 million | [37] |
| Annual deaths from healthcare-associated infections | Nearly 99,000 | [37] |
| Rate of healthcare-associated infections on any given day | 1 in 31 hospital patients | [37] |
| Reduction in neonatal intensive care unit (NICU) HCAIs via aseptic technique | 50% reduction | [37] |
| Reduction in surgical site infections (SSIs) via aseptic technique | 20% to 6% | [37] |
Fundamental Concepts: Definitions and Distinctions
Understanding Aseptic Technique in Research
Aseptic technique is a strict procedural framework designed to prevent contamination by disease-causing microbial pathogens in laboratory settings [37]. It serves a dual purpose: protecting the integrity of biological experiments and processes from environmental contamination, and safeguarding laboratory personnel from exposure to hazardous materials, including blood, bodily fluids, tissue, and cultured pathogens [37] [38]. The application of aseptic technique is fundamental to preventing laboratory-acquired infections and ensuring the validity of experimental results [39].
Distinguishing Between Clean, Aseptic, and Sterile
The terms "clean," "aseptic," and "sterile" represent distinct standards of control within the laboratory, each appropriate for different research contexts:
- Clean Technique: Focuses on reducing the overall number of germs rather than eliminating them completely. It involves hand washing, cleaning equipment, and often wearing non-sterile gloves. This approach is sufficient for general laboratory work where complete sterility is not required [40].
- Aseptic Technique: A stricter standard that aims to eliminate pathogens entirely. In practice, healthcare providers typically use the term "aseptic" to describe techniques and procedures, while "sterile" describes settings and instruments. Aseptic techniques create a controlled environment that minimizes the risk of contamination [40].
- Sterile Technique: The highest level of sterility, used in operating rooms and for certain sensitive laboratory procedures. Every instrument, drape, and glove is sterile, and personnel work within a fully sterile field to keep deep wounds and body cavities free from germs during major operations [37].
Table: Comparison of Technique Standards
| Technique | Objective | Typical Applications | Germ Elimination |
|---|---|---|---|
| Clean | Reduce overall germ count | General lab work, non-sterile procedures | No |
| Aseptic | Eliminate pathogens | Sample preparation, cell culture, media preparation | Yes |
| Sterile | Complete elimination of all microorganisms | Surgical procedures, certain sensitive lab work | Complete |
Personal Protective Equipment: Selection and Application
The Regulatory and Standards Framework
PPE used in laboratory settings as medical devices must comply with FDA regulations and applicable voluntary consensus standards for protection. These standards vary depending on the specific type of PPE and provide reasonable assurance that the device is safe and effective [41]. The Occupational Safety and Health Administration (OSHA) mandates that employers must provide appropriate PPE at no cost to employees whenever hazards are present that could cause injury or impair bodily functions through skin contact, inhalation, or absorption [39].
Comprehensive PPE Selection for Research Environments
Selecting appropriate PPE requires a thorough hazard assessment specific to the materials and procedures being performed. The following considerations guide appropriate PPE selection:
- Type of hazardous materials being used (biological, chemical, radiological, etc.) along with their concentration and quantity [39]
- Potential routes of exposure (inhalation, skin contact, mucous membrane exposure) [39]
- Permeation and degradation rates of PPE materials against specific hazardous substances [39]
- Length of time for the effective use of the PPE [39]
- Comfort and fit to ensure optimal protection and compliance [39]
Table: PPE Selection Guide for Laboratory Environments
| Protection Category | Equipment Types | Primary Function | Applicable Standards |
|---|---|---|---|
| Hand Protection | Exam gloves, sterile gloves, chemical-resistant gloves | Barrier against biological material, chemicals | 29 CFR 1910.138 [39] |
| Respiratory Protection | Masks, N95 respirators, PAPR | Protection against airborne pathogens, particulates | 29 CFR 1910.134 [36] [39] |
| Eye and Face Protection | Safety glasses, goggles, face shields | Protection from splashes, airborne droplets | 29 CFR 1910.133 [39] |
| Body Protection | Lab coats, gowns, aprons, coveralls | Barrier for clothing and skin against contamination | 29 CFR 1910.132 [39] |
| Foot Protection | Shoe covers, boots | Prevent transfer of hazardous materials | 29 CFR 1910.136 [39] |
| Hearing Protection | Earplugs, earmuffs | Prevention of noise-induced hearing loss | 29 CFR 1910.95 [39] |
Specialized PPE for Transmission-Based Hazards
When working with documented or suspected infectious pathogens, additional transmission-based precautions are necessary. These precautions are implemented based on the route of transmission and include specific PPE requirements [36]:
- Contact Precautions: Used for known or suspected infections with increased risk for contact transmission (e.g., draining wounds, fecal incontinence) or with epidemiologically important organisms. Required PPE includes gloves and gowns, plus dedicated equipment when possible [36].
- Droplet Precautions: Implemented for pathogens transmitted by large respiratory droplets generated by coughing, sneezing, or talking. Required PPE includes masks and goggles or face shields [36].
- Airborne Precautions: Necessary for known or suspected infection with pathogens transmitted by small respiratory droplets. Required PPE includes fit-tested N-95 respirators or powered air-purifying respirators (PAPR), plus airborne infection isolation rooms with closed doors [36].
Aseptic Technique Protocols: A Procedural Framework
Types of Aseptic Techniques in Research Practice
Different research scenarios require different levels of aseptic control. The main technical approaches include:
- Surgical Aseptic Technique: The highest level of sterility, used in operating rooms and certain sensitive laboratory procedures. Every instrument, drape, and glove is sterile, and personnel work within a fully sterile field, touching only sterile surfaces to keep deep wounds and body cavities free from germs during major operations [37].
- Standard Aseptic Technique (Clean Technique): Used for routine care and procedures where the goal is to reduce germs rather than eliminate them completely. This involves hand washing, cleaning equipment, and often wearing gloves. It's appropriate for dressing simple wounds, giving injections, and general sample handling where full surgical sterility isn't required [37].
- Aseptic Non-Touch Technique (ANTT): A clinical practice that mandates practitioners to avoid touching "critical parts" directly. In this technique, researchers handle IV lines, catheters, and other sensitive sites using sterile gloves or forceps, ensuring that only sterile tools or parts contact the patient or sample [37].
Step-by-Step Procedural Guide for Sample Preparation
Implementing aseptic technique requires meticulous attention to each phase of the experimental process:
Pre-Procedure Preparation
- Hand Hygiene: Perform appropriate hand hygiene using either soap and water or an alcohol-based hand rub containing at least 60% alcohol. Unless hands are visibly soiled, alcohol-based hand rub is preferred in most clinical situations due to evidence of improved compliance [36].
- Supply Gathering: Collect all necessary sterile instruments and supplies before beginning the procedure to minimize movement and potential contamination during the process [37].
- PPE Donning: Put on appropriate PPE in the correct sequence: gown first, followed by mask or respirator, eye protection, and finally gloves [37].
Sterile Field Establishment
- Surface Disinfection: Thoroughly disinfect all work surfaces with appropriate agents before introducing sterile materials [37].
- Aseptic Opening: Open sterile packages carefully, keeping unwrapped items clear of any non-sterile surfaces. Lay tools and supplies on a sterile drape or tray [37].
- Spatial Awareness: Avoid reaching or leaning over the sterile field, as any movement can introduce contaminants. Maintain awareness of sterile boundaries throughout the procedure [37].
Sample Handling and Processing
- Critical Part Identification: Identify and protect "critical parts" of equipment and samples that must remain sterile throughout the procedure [37].
- Instrument Handling: Use forceps or other sterile instruments instead of hands to manipulate samples and sensitive equipment when possible [37].
- Environmental Control: Limit entries and exits in the procedure room to reduce airflow disturbances. Keep doors closed and minimize conversation to reduce airborne particles [37].
Post-Procedure Protocols
- Waste Disposal: Immediately discard used materials into labeled biohazard containers according to institutional protocols [37].
- PPE Removal: Carefully remove gloves and other PPE using proper technique to prevent self-contamination. The sequence for removal is: gloves first, followed by gown, eye protection, and finally mask or respirator [36].
- Final Hand Hygiene: Wash hands thoroughly immediately after PPE removal and disposal [37].
- Documentation: Record procedure details and any notes on aseptic maintenance for quality control and process improvement [37].
Environmental Controls and Monitoring
Environmental controls are essential components of aseptic technique that extend beyond personal practice to include the entire laboratory environment:
- Physical Space Management: Implement cleanroom requirements where necessary, including appropriate air filtration, positive pressure rooms, and restricted access [38].
- Environmental Monitoring: Establish regular environmental monitoring protocols using settle plates, air samplers, and surface swabs to verify the effectiveness of aseptic controls [38].
- Equipment Maintenance: Regularly service and validate equipment such as biological safety cabinets, autoclaves, and HVAC systems to ensure proper function [39].
Essential Research Reagents and Materials
The following table details key research reagent solutions and materials essential for maintaining asepsis during sample preparation and experimental procedures:
Table: Essential Research Reagent Solutions for Aseptic Technique
| Item/Category | Function in Aseptic Technique | Application Examples |
|---|---|---|
| Alcohol-based Hand Rub | Reduces microbial load on hands when soap and water are not available; must contain at least 60% alcohol | Hand hygiene between tasks, after glove removal [36] |
| Antiseptic Skin Preparations | Reduces skin flora at procedure sites; requires adequate contact time to be effective | Patient skin preparation before injections, venipuncture, or surgical procedures [37] [40] |
| Sterile Gloves | Creates barrier between researcher and sample; prevents contamination of critical sites | Sample manipulation, sterile field setup, handling of sterile instruments [36] [37] |
| Biological Indicators | Verifies effectiveness of sterilization processes; provides confirmation of sterility | Autoclave validation, sterility assurance for instruments and materials [40] |
| Environmental Monitoring Materials | Assesses microbial contamination levels in the laboratory environment | Settle plates, air samplers, surface swabs for quality control [38] |
| Surface Disinfectants | Eliminates pathogens from work surfaces and equipment before procedures | Bench decontamination, equipment cleaning, spill management [37] |
Common Technique Errors and Corrective Strategies
Even experienced researchers can commit critical errors in aseptic technique. Recognizing and addressing these common mistakes is essential for maintaining contamination control:
- Hand Hygiene Violations: Inadequate hand washing between tasks, improper drying techniques, or wearing jewelry and long nails that can trap bacteria despite proper scrubbing [37].
- Contaminated Equipment Handling: Touching non-sterile surfaces (e.g., door handles, charts) after donning gloves, then handling sterile instruments; placing sterile tools on unclean surfaces; or mixing sterile and non-sterile items [37].
- Sterile Field Breaches: Leaning over sterile trays, dropping instruments below waist level, reusing syringes, or sharing disposables intended for single use [37].
- PPE Protocol Errors: Improper donning or removal of PPE that spreads pathogens to hands and clothing; reusing single-use masks; or working without adequate room ventilation [37].
When contamination occurs, immediate corrective action is required. Remain composed, inform all team members, discard all affected gloves, instruments, and supplies. The entire contaminated field is no longer usable, requiring setup of a fresh sterile area with new materials. Attempting to salvage contaminated items compromises patient safety and experimental integrity [37].
Training and Competency Assessment
Effective training programs are essential for maintaining aseptic technique mastery. The OSHA PPE Standard mandates that employers provide comprehensive training on proper selection, use, and maintenance of PPE, including understanding its limitations [39]. Training should be delivered through various methods such as videos, web-based presentations, group sessions, and handouts, with periodic refresher training as required [39].
Documentation and recordkeeping are critical components of an effective training program. Organizations must maintain records of all PPE training, including details of the information covered, the names of individuals trained, the type of training provided, and the training dates [39]. A new AABB publication emphasizes that "training on aseptic technique is critical to any biological laboratory, whether the lab is starting out or has been well established in practice. Having a guide to lay the groundwork or to review current practices is essential to having a highly successful lab" [38].
Mastery of personal protective equipment and aseptic technique represents a fundamental competency for researchers, scientists, and drug development professionals. The rigorous application of these practices protects both the integrity of valuable research samples and the safety of laboratory personnel. As Matthew Wilgo notes, "we all should be looking for opportunities for continuous improvement" in our aseptic practices [38]. Through consistent application of evidence-based protocols, comprehensive training, and vigilant monitoring, research facilities can maintain the highest standards of aseptic technique, ensuring the reliability of scientific data and accelerating the development of novel therapeutics.
In modern research and drug development, contamination control is a foundational element of data integrity and product safety. Human error remains the single largest risk vector in laboratory and production environments, potentially compromising sample integrity, experimental reproducibility, and patient safety. This technical guide examines how integrated strategies incorporating automation technologies and validated single-use consumables create robust barriers against contamination. By systematically addressing human factors at their source and eliminating cross-contamination pathways, organizations can achieve sustainable compliance, enhance operational efficiency, and protect valuable research outcomes throughout the sample preparation workflow.
The Critical Contamination Challenge in Sample Preparation
Contamination during sample preparation presents multifaceted risks that extend far beyond simple experimental inconvenience. The consequences encompass skewed experimental results, irreproducible data, compromised product safety, and significant financial losses due to compromised batches and regulatory actions [42] [15].
In pharmaceutical manufacturing alone, contamination repercussions include lost revenue from slowdowns, regulatory fines, and lasting reputational damage [42]. Perhaps more critically, up to 75% of laboratory errors occur during the pre-analytical phase, frequently stemming from improper handling, contamination, or suboptimal sample collection techniques [15]. These errors introduce unwanted variables that interfere with true signals, potentially masking target analytes or generating false positives that undermine research validity and therapeutic development [15].
The human element represents the most significant contamination risk. Personnel can unintentionally introduce errors through lapses in aseptic technique, incorrect sampling, or failure to follow established protocols, despite advanced automation and rigorous procedures [43]. In low-biomass microbiome studies, where target DNA signal minimally exceeds contaminant noise, even minimal human contact can drastically distort results and their interpretation [4]. These challenges necessitate a systematic approach combining technological solutions with human factors engineering.
The Human Error Vector: Analysis and Mitigation
Understanding Human Factors
Human errors in laboratory settings are rarely due to carelessness alone. More commonly, they stem from systemic weaknesses, inadequate training, process complexity, cognitive biases, and suboptimal workflow design [43]. For instance, a worker may inadvertently touch a critical surface in a cleanroom because procedures are unclear, or because the workflow requires excessive, complex hand movements [43].
Regulatory agencies including the FDA and EMA increasingly recognize that addressing human factors proactively is equally as important as controlling equipment or environmental risks [43]. Inspections often reveal repeated deviations, improper gowning, or environmental excursions where investigators determine whether these issues originated from systemic gaps or individual operator errors [43].
Strategic Mitigation Approaches
A comprehensive Contamination Control Strategy (CCS) must integrate multiple approaches to manage human-related risks effectively:
Enhanced Training and Competency Assessment: Personnel require training not only on standard operating procedures (SOPs) but also on the scientific rationale behind each step. Understanding the "why" behind procedures significantly improves adherence and reduces errors caused by performing routine tasks mechanically [43]. Competency assessments should be ongoing and incorporate direct observation, practical testing, simulated contamination events, and periodic retraining to combat knowledge decay over time [43].
Human-Centered Workflow Design: Processes should be designed with human factors in mind to reduce mistake likelihood. This includes ergonomic layout, clear labeling, logical step sequencing, minimizing manual interventions in critical areas, and reducing unnecessary complexity [43]. Well-designed workflows minimize hand movements, reduce cross-contamination opportunities, and enable operators to perform tasks efficiently and correctly [43].
SOP Usability Optimization: Complex or poorly written SOPs increase cognitive load and can lead to mistakes. CCS approaches advocate designing SOPs that are intuitive, with clear step-by-step instructions, visual aids, and checklists where appropriate [43]. SOPs should be tested with operators to ensure they are practical and easily understood in real-world conditions [43].
Performance Monitoring and Culture: Monitoring human performance through real-time observation, environmental monitoring data, deviation reviews, and batch record analysis helps identify error patterns for targeted improvement [43]. Fostering a culture of quality and accountability encourages personnel to follow procedures meticulously and report deviations without fear, recognizing that their actions directly impact product safety and research validity [43].
Automation Technologies for Contamination Control
Automation serves as a powerful tool to minimize human intervention in critical processes, thereby reducing contamination risks while improving efficiency and data integrity. Automated systems address several vulnerability points in sample preparation and manufacturing workflows.
Environmental Monitoring (EM) Systems
Automated EM systems enable real-time spotting and control of contamination threats from external sources such as air handling systems, particles, and microorganisms [42]. By maximizing quality control and incorporating automation into sample collection, data management, sample processing, tracking, trending, and reporting, these systems allow companies to easily confirm when processes are complete or determine when vital steps have been missed [42]. This automation moves beyond traditional, paper-based processes that are vulnerable to human error in documentation and timely trending of data [42].
Automated Contamination Control Programs
Comprehensive automated contamination control programs incorporate three key components that work synergistically [42]:
- Environmental Monitoring (EM): Controls contamination threats from external sources in real-time through automated sample collection and data management.
- Cleaning Validation (CVM): Ensures cleanrooms are properly cleaned and disinfected to prevent contamination from previous products, microorganisms, and residues through automated validation of cleaning processes.
- Water & Utility Monitoring (UM): Manages sampling, testing, and data collection for water systems, gases, and HVAC to prevent distribution contamination through automated pattern recognition.
These automated systems enable continuous monitoring of reliable and accurate data surrounding manufacturing processes, meeting regulatory expectations for data trending to monitor process control and identify operational weaknesses [42].
Automated Aseptic Processing
In aseptic processing environments, automation significantly reduces contamination risks associated with human operators. Technologies such as robotic gloveless isolators limit product exposure to operators, while automated filling systems, barcode verification, and real-time environmental monitoring alerts help maintain process integrity while minimizing human intervention [43] [44]. Well-designed automated systems reduce manual manipulations in critical areas, directly addressing the fact that personnel present the highest contamination risk in aseptic processing [44].
Table: Comparative Analysis of Automation Technologies
| Technology Type | Primary Contamination Control Benefit | Key Applications | Implementation Considerations |
|---|---|---|---|
| Automated Environmental Monitoring | Real-time contamination threat detection | Pharmaceutical manufacturing, cleanrooms | Integration with existing systems, data management infrastructure |
| Robotic Isolators | Elimination of human direct interaction with critical processes | Aseptic filling, sterile product manufacturing | High capital investment, validation requirements |
| Automated Data Collection & Trending | Prevents human error in documentation and data interpretation | Research laboratories, quality control labs | Regulatory compliance for electronic records |
| Water & Utility Monitoring Systems | Continuous quality assurance of critical utilities | Pharmaceutical production, biotechnology manufacturing | Sensor calibration, maintenance protocols |
Single-Use Consumables: Strategic Implementation
Cross-Contamination Prevention
Single-use systems have gained substantial acceptance in biopharmaceutical manufacturing and research environments over the last decade, particularly as companies increase product diversity and implement shorter, multi-product runs [45]. These disposable systems replace traditional stainless steel bioprocessing equipment with disposable alternatives, offering significant contamination control advantages [45].
The most prominent benefit of single-use consumables is dramatic reduction of cross-contamination risk. When process equipment is used to produce more than one product, unwanted contamination may reduce production yields by requiring additional purification steps, or result in potentially fatal consequences for patients [45]. Single-use systems substantially reduce or eliminate the need for Clean-in-Place (CIP) procedures that consume large amounts of caustics, acids, and Water-for-Injection (WFI) while requiring regular testing to verify effectiveness [45].
Material Considerations and Extractables/Leachables
While single-use systems offer significant contamination control advantages, they introduce different considerations, particularly regarding extractables and leachables. Extractables are chemical compounds that can potentially migrate from product contact material into a solvent under worst-case conditions, while leachables are compounds that actually migrate into the biopharmaceutical under normal conditions of use [45].
The potential impact of leachables on drug products includes concerns about quality, safety, and efficacy. Documented cases include therapeutic proteins reacting with acrylic acid that leached from prefilled syringes, and cell growth being impacted by degradation products of antioxidants from irradiated polyethylene films in bioreactors [45]. A comprehensive assessment of single-use systems should include:
- Material Composition Analysis: Understanding the polymers present (silicone, polypropylene, nylon, etc.) and their potential extractables [45].
- Toxicological Risk Assessment: Applying methodologies like Cramer classification, quantitative structure-activity relationships (QSAR), and Threshold of Toxicological Concern (TTC) to evaluate potential health impacts [45].
- Compatibility Testing: Ensuring materials are compatible with process solutions and do not introduce harmful leachables.
Table: Common Single-Use System Polymers and Associated Extractables
| Polymer Type | Common Component Applications | Typical Extractables Identified | Risk Mitigation Approaches |
|---|---|---|---|
| Silicone | Tubing, gaskets | Cyclosiloxanes (D3-D6) | Vendor qualification, pre-use flushing |
| Polypropylene | Connectors, containers | Antioxidant breakdown products, dimethylbenzaldehyde isomers | Material screening, process validation |
| Nylon | Clamps, fittings | Caprolactam (monomer), 1,4-butanediol | Alternative polymer selection, extraction studies |
Sterilization Methodologies for Single-Use Consumables
Sterilization is a critical aspect of single-use consumable implementation, with several technologies available, each with distinct advantages and limitations [46]:
Gamma Irradiation: The most established method, using electromagnetic radiation from radionuclides like Cobalt-60. Gamma rays penetrate through most single-use system components without being retained by materials, leaving no residual radioactivity. A typical minimum dose of 25 kGy can achieve a Sterility Assurance Level (SAL) of 10â»â¶, meaning there is less than one chance in a million that a single viable microorganism is present on the sterilized item [47] [46].
Electron Beam (E-Beam): Another form of ionizing radiation using a stream of electrons. Due to their mass and charge, electrons are less effective at penetrating materials compared to gamma rays, making e-beam more suitable for smaller, less-complex consumables [46].
X-ray Irradiation: An emerging alternative that offers excellent penetration capabilities similar to gamma irradiation but with electricity as the source rather than radioactive isotopes. While technologically promising, limited commercial capacity currently exists [46].
Ethylene Oxide (EtO): A gas sterilization method with a long history of use in the medical device industry. EtO is less ideal for single-use systems with complex fluid paths because ensuring all internal surfaces receive adequate gas exposure can be challenging [46].
Each sterilization method must be validated according to standards such as ISO 11137 for ionizing radiation to ensure consistent delivery of the minimum required sterilizing dose without adversely impacting material properties [46].
Integrated Methodologies and Experimental Protocols
Comprehensive Contamination Control Strategy Implementation
Implementing a robust contamination control strategy requires systematic integration of both automated systems and single-use technologies. The following workflow illustrates the logical relationship between strategy components:
Low-Biomass Sample Handling Protocol
For research involving low-biomass samples where contamination risks are magnified, specific stringent protocols must be followed [4]:
Pre-Sampling Preparation:
- Verify DNA-free status of sampling reagents through quality control testing.
- Decontaminate all reusable equipment with 80% ethanol followed by nucleic acid degrading solution.
- Use pre-treated (autoclaved or UV-C sterilized) plasticware or glassware, sealed until use.
- Implement appropriate personal protective equipment (PPE) including gloves, goggles, coveralls, and masks.
Sample Collection:
- Minimize sample handling and exposure to potential contamination sources.
- Use single-use, DNA-free collection vessels whenever possible.
- Collect comprehensive controls including empty collection vessels, air exposure samples, and swabs of PPE/surfaces.
Sample Processing:
- Process samples in controlled environments (cleanrooms, laminar flow hoods).
- Implement physical separation of pre- and post-amplification samples in PCR workflows.
- Use aerosol-resistant pipette tips to prevent cross-contamination between samples.
Documentation and Tracking:
- Maintain detailed records of sample preparation processes, including tools, reagents, and environmental conditions.
- Document all potential contamination risk points and mitigation measures.
Sterilization Validation Framework
For organizations implementing single-use consumables, establishing a robust sterilization validation framework is essential [47]:
Material Compatibility Assessment:
- Evaluate polymer compatibility with intended sterilization method.
- Conduct accelerated aging studies to assess material degradation post-sterilization.
- Establish maximum acceptable radiation dose for material integrity.
Sterilization Process Qualification:
- Determine product bioburden through comprehensive testing.
- Establish minimum sterilization dose required to achieve target Sterility Assurance Level (SAL).
- Verify dose distribution throughout product load using dosimetry.
Routine Monitoring:
- Implement batch-by-batch sterility testing where required.
- Conduct regular audits of sterilization facility quality systems.
- Maintain documentation for each sterilization cycle.
Essential Research Reagent Solutions
Implementing effective contamination control requires specific materials and reagents designed to maintain sample integrity throughout preparation and analysis. The following toolkit outlines essential solutions:
Table: Research Reagent Solutions for Contamination Control
| Product Category | Specific Examples | Function in Contamination Control | Application Notes |
|---|---|---|---|
| Sample Homogenization Probes | Stainless steel, disposable plastic (Omni Tips), hybrid probes | Prevent cross-contamination between samples during homogenization | Disposable probes eliminate cleaning requirements; hybrid options balance durability and contamination control [15] |
| Nucleic Acid Decontamination Reagents | DNA Away, sodium hypochlorite (bleach) solutions | Remove contaminating DNA from surfaces and equipment | Essential for DNA-free environments in PCR and molecular biology workflows [15] |
| High-Purity Solvents & Acids | Double-distilled acids in PFA/FEP bottles | Minimize introduction of trace metal contaminants | Critical for trace element analysis by ICP-MS; avoid glass containers [48] |
| Sterile Single-Use Labware | Pipettes with polypropylene/fluoropolymer tips | Prevent extractable metals and particulate contamination | Avoid pipettes with external stainless steel tip ejectors for trace metal analysis [48] |
| Personal Protective Equipment | Powder-free nitrile gloves, cleanroom garments | Reduce human-derived contamination (skin cells, hair, aerosols) | Powder particles can contaminate samples; proper gowning techniques are essential [48] [4] |
| Environmental Monitoring Systems | Automated EM systems, real-time particulate sensors | Continuous monitoring of cleanroom and controlled environments | Provides immediate alerting for environmental excursions [42] |
Future Trends and Strategic Directions
The contamination control landscape continues to evolve, with several emerging trends shaping future approaches:
Sterilization Technology Diversification: While gamma irradiation remains dominant, capacity constraints are driving adoption of alternative technologies including X-ray and advanced electron beam systems [46]. This diversification enhances supply chain resilience while maintaining sterility assurance.
Sustainable Single-Use Solutions: Environmental concerns regarding plastic waste are accelerating development of biodegradable polymers and advanced recycling technologies for single-use consumables [49] [44]. Future systems will balance contamination control with environmental responsibility.
AI-Enhanced Contamination Prediction: Artificial intelligence and machine learning are being applied to predict contamination risks through pattern recognition in environmental monitoring data, enabling proactive intervention before contamination events occur [49].
Advanced Material Science: New polymer formulations with reduced extractables and improved radiation resistance are under development, addressing one of the primary limitations of current single-use systems [45] [46].
The global single-use consumables market reflects these trends, projected to grow from US$2.99 billion in 2024 to US$13.83 billion by 2034, representing a compound annual growth rate of 16.56% [49]. This expansion demonstrates increasing recognition of the critical role these technologies play in contamination control across research and pharmaceutical manufacturing.
Integrating automation technologies with strategically selected single-use consumables represents the most effective approach to minimizing human error and cross-contamination in research and pharmaceutical manufacturing. This comprehensive strategy addresses contamination risks at multiple levels: reducing direct human intervention through automation, eliminating cross-contamination pathways through disposable systems, and implementing continuous monitoring for immediate detection of control breaches.
Organizations that successfully implement these integrated contamination control frameworks achieve not only enhanced regulatory compliance and reduced observation rates, but also improved research data quality, manufacturing efficiency, and ultimately, greater patient safety. As technologies continue to advance, the ongoing refinement of these approaches will further strengthen contamination prevention capabilities across the research and development continuum.
In laboratory science, the integrity of research data is fundamentally established during the initial stages of sample handling. Proper techniques in pipetting and storage are not merely procedural steps but critical interventions that determine the validity of experimental outcomes. This is especially crucial in pharmaceutical development and clinical diagnostics, where contamination control directly impacts product safety and patient diagnoses [15] [50]. Studies indicate that up to 75% of laboratory errors originate in the pre-analytical phase, often stemming from improper sample handling and contamination [15]. This guide provides a comprehensive framework for mastering sample handling techniques, with a specific focus on preventing contamination throughout the research workflow. By implementing these evidence-based practices, researchers can significantly enhance data accuracy, experimental reproducibility, and ultimately, the reliability of scientific conclusions.
Mastering Pipetting Techniques to Prevent Cross-Contamination
Pipetting represents one of the most frequent yet potentially hazardous procedures in sample preparation. Aerosols, which are suspensions of solid or liquid particles in gas formed during pipetting, serve as the primary contamination vector [51]. Understanding and mitigating the three primary contamination pathways is essential for any rigorous laboratory practice.
Understanding Contamination Pathways and Prevention Strategies
Pipette-to-Sample Contamination: This occurs when a contaminated pipette or pipette tip introduces contaminants into a clean sample. Prevention requires selecting tips with appropriate purity certifications (e.g., DNase, RNase, and endotoxin-free), using filter tips or positive displacement tips, regularly changing tips between samples, and performing routine decontamination of pipettes through autoclaving or disinfection [51] [52].
Sample-to-Pipette Contamination: This pathway involves sample or aerosols entering the pipette body itself, potentially contaminating the instrument and affecting future use. Risk is minimized by releasing the pipette push-button slowly to reduce aerosol formation, maintaining the pipette in a vertical position during use to prevent liquid ingress, and consistently using filter tips to create a barrier against aerosols [51] [52].
Sample-to-Sample Contamination (Carry-over): This common issue happens when residue from one sample is transferred to subsequent samples. The most effective prevention is always changing pipette tips after each sample, without exception. Additionally, using filter tips and regularly decontaminating pipettes when contamination is suspected are essential practices [51] [52].
Pipette Tip Selection Guide
Table 1: Pipette tip purity grades and their appropriate applications
| Purity Grade | Certification Level | Recommended Applications |
|---|---|---|
| No Certification | No purity testing | Non-critical applications where enzymatic or chemical contaminants will not affect results |
| Certified Pure | Certified free of specific contaminants (DNase, RNase, endotoxins) | Molecular biology techniques (PCR, DNA/RNA work), cell culture, endotoxin-sensitive applications |
| Sterilized | Sterilized to be free of microbial life | Microbiology, sterile cell culture techniques, and any work requiring aseptic conditions |
High-quality tips manufactured from 100% virgin polypropylene are recommended to minimize potential leachables—trace chemicals from materials or manufacturing that can contaminate samples [51].
Establishing Comprehensive Environmental Controls for Sample Integrity
Beyond manual techniques, the laboratory environment itself plays a decisive role in preserving sample integrity. Effective environmental control requires a systematic approach addressing multiple physical and atmospheric factors.
Critical Environmental Control Parameters
Table 2: Environmental factors affecting sample integrity and their control measures
| Environmental Factor | Impact on Sample Integrity | Recommended Control Measures |
|---|---|---|
| Temperature Variation | Accelerates degradation pathways; causes protein denaturation and chemical breakdown [50] | Continuous temperature monitoring systems (CTMS); deviation alarms; backup power sources; thermal gradient mapping |
| High Relative Humidity | Promotes microbial growth; affects hygroscopic materials; causes condensation [50] | Dehumidification systems; vapor barriers; desiccant materials; maintain 30-60% RH |
| Low Relative Humidity | Causes desiccation and sample concentration; potential for electrostatic discharge [50] | Humidification systems; sealed container use |
| Oxygen Exposure | Oxidative degradation of sensitive compounds (lipids, vitamins) [50] | Inert gas purging (nitrogen/argon); sealed, light-proof vials |
| Airborne Contaminants | Introduces particulate, microbial, and volatile organic compound (VOC) contamination [50] | HEPA filtration; appropriate air change rates (15-20 changes/hour); pressure differential zoning |
| Light Exposure | Initiates photodegradation of light-sensitive compounds [50] | Amber/opaque storage containers; UV-blocking window films; minimized light exposure time |
Laboratory Design and Workflow Considerations
Strategic laboratory design provides the physical infrastructure necessary for maintaining sample integrity through zoning and workflow segregation. This involves establishing dedicated, physically separated areas for incompatible activities such as reagent preparation, high-volume DNA amplification, and initial sample accessioning [50]. For instance, facilities performing food testing must strictly separate raw sample handling from finished product analysis areas to prevent microbial or allergen carryover [50].
Surface selection also plays a crucial role, with non-porous, chemically resistant materials like epoxy or resin-based bench tops and coved flooring being preferred as they limit crevices where pathogens or chemical residues can accumulate [50]. Furthermore, managing personnel flow through access controls and gowning protocols serves as essential barriers to maintain controlled environments [50].
Essential Research Reagent Solutions and Laboratory Tools
The selection of appropriate tools and reagents constitutes a fundamental aspect of contamination prevention. Each component must be chosen based on the specific application and potential contamination risks.
Table 3: Essential laboratory tools for contamination prevention
| Tool/Reagent Category | Specific Examples | Function & Contamination Control Rationale |
|---|---|---|
| Pipette Tips | Filter tips; Certified pure tips; Positive displacement tips | Create physical barrier against aerosols; prevent introduction of enzymatic contaminants or leachables [51] |
| Homogenizer Probes | Stainless steel (with rigorous cleaning); Disposable plastic probes (Omni Tips); Hybrid probes (Omni Tip Hybrid) | Balance durability against cross-contamination risk; disposable options eliminate cleaning bottlenecks and contamination risks [15] |
| Decontamination Solutions | 70% ethanol; 5-10% bleach; DNA Away; RNase decontamination solutions | Remove or inactivate specific contaminants from surfaces and equipment; specialized formulas target molecular contaminants [15] |
| Sample Storage Vessels | Amber/opaque vials; Sealed containers for humidity control; Inert gas-purged containers | Protect against photodegradation; prevent desiccation or hydration; minimize oxidative damage [50] |
| Surface Materials | Epoxy/resin bench tops; Cove d flooring; Stainless steel surfaces | Non-porous, easy-to-clean materials prevent accumulation of contaminants in crevices [50] |
Experimental Protocols for Validation and Quality Control
Implementing rigorous validation protocols ensures that contamination control measures are effective and consistently applied.
Protocol 1: Validating Homogenizer Probe Cleaning Efficacy
Purpose: To verify that cleaning procedures for reusable homogenizer probes effectively remove residual analytes, preventing sample-to-sample contamination [15].
Methodology:
- Process a sample containing a known, detectable analyte concentration using the homogenizer probe.
- Perform the established cleaning procedure according to laboratory SOP.
- Homogenize a blank solution (the solvent without analytes) using the same cleaned probe.
- Analyze the blank solution using appropriate analytical methods (e.g., UV-Vis, HPLC, PCR) to detect any residual analyte.
- The cleaning is validated if analyte levels in the blank are below the assay's limit of detection or at an acceptable threshold that will not impact downstream analysis [15].
Protocol 2: Continuous Temperature Monitoring System (CTMS) Verification
Purpose: To confirm that storage units maintain specified temperature setpoints, preventing sample degradation due to thermal variation [50].
Methodology:
- Place calibrated temperature sensors at critical locations within the storage unit (typically determined through prior thermal mapping).
- Record temperature at frequent intervals (e.g., every 5 minutes) using a validated CTMS.
- Configure alarms to trigger at levels that allow for intervention before sample integrity is compromised (e.g., a "high warning" alarm set slightly below the critical maximum limit).
- Maintain detailed records of all temperature monitoring data and any deviations for audit purposes.
- Implement escalation protocols for after-hours response to temperature deviations, including backup power sources for critical storage units [50].
Visualizing Contamination Pathways and Prevention Workflows
The following diagrams illustrate key contamination pathways and systematic approaches to their prevention, providing clear visual references for laboratory implementation.
Pipetting Contamination Pathways
Environmental Controls Integration Framework
Mastering sample handling requires a systematic integration of proper technique, environmental control, and validated protocols. By understanding specific contamination pathways in pipetting, implementing comprehensive environmental monitoring, selecting appropriate tools and reagents, and establishing rigorous validation protocols, research laboratories can significantly enhance data quality and reproducibility. The interconnected nature of these controls means that weakness in any single component can compromise the entire system. Therefore, a culture of continuous monitoring, documentation, and improvement is essential for maintaining the integrity of samples from collection through analysis, ultimately supporting the generation of reliable, defensible scientific data in pharmaceutical development and research settings.
Diagnosing and Solving Common Contamination Problems in the Lab
Interpreting Negative Controls and No Template Controls (NTCs)
In molecular biology, the exquisite sensitivity of techniques like polymerase chain reaction (PCR) allows for the detection of just a few copies of a nucleic acid sequence. However, this same sensitivity makes these methods exceptionally vulnerable to contamination, which can lead to false-positive results and compromise research integrity. Within a robust contamination prevention framework, Negative Controls and No Template Controls (NTCs) serve as critical sentinels. They are indispensable tools for validating experimental results, ensuring that the amplified signal genuinely originates from the sample and not from contaminating nucleic acids present in reagents, the environment, or laboratory equipment. The proper implementation and interpretation of these controls form the foundation of reliable data in sample preparation research, diagnostic development, and drug discovery pipelines.
Defining the Controls: Purpose and Composition
Understanding the distinct roles of different negative controls is the first step in designing a foolproof contamination monitoring strategy.
Table 1: Key Negative Control Types in Molecular Assays
| Control Type | Composition | Purpose | Interpretation of a Positive Result |
|---|---|---|---|
| No Template Control (NTC) [53] | Contains all PCR reaction components (master mix, primers, probes, water) except the DNA/RNA template. | Detects contamination within the PCR reagents or the reaction setup process. | Indicates that one or more reagents or consumables are contaminated with the target nucleic acid. |
| Negative Control (Extraction) [54] | A known negative sample or blank (e.g., water) that is carried through the entire nucleic acid extraction and purification process alongside real samples. | Monitors for cross-contamination during the sample preparation and nucleic acid extraction steps. | Suggests that contamination occurred during the extraction process, potentially from a contaminated reagent or carryover from a previous sample. |
| Positive Control [54] | A sample with a known quantity of the target sequence. | Verifies that the entire assay process, from extraction to amplification, is functioning correctly. | A failure to amplify indicates a problem with the assay itself, such as reagent degradation or instrument failure. |
Interpreting Control Results and Troubleshooting
The data from your controls provide a direct assessment of your assay's cleanliness. A systematic approach to interpretation is crucial.
Expected Results and Baseline Interpretation
In a perfectly clean and optimized assay:
- The Positive Control must yield a positive amplification signal.
- The NTC and Negative Extraction Control must show no amplification [55] [56].
Any amplification signal in the NTC is a clear red flag, signifying that contamination is present. The pattern of amplification can offer clues about the source of the contamination [53]:
- Random Amplification in NTCs: If some NTC replicates amplify at varying cycle threshold (Ct) values and others do not, the contamination likely occurred randomly during plate loading, possibly from aerosol contamination or pipette carryover [53].
- Consistent Amplification in NTCs: If all NTC replicates amplify with similar Ct values, it points to systematic reagent contamination. One of the core reaction components (e.g., water, master mix, or primers) is contaminated with the target sequence [53].
Table 2: Troubleshooting Amplification in No Template Controls (NTCs)
| Observed Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Primer-Dimer Formation (SYBR Green assays only) [53] | Self-annealing of primers, generating a low-level background signal. | Optimize primer concentrations [53]. Redesign primers to minimize complementarity. |
| Random Contamination (Aerosols or carryover) [53] [57] | Contaminated pipettes, bench surfaces, or splashing during sample handling. | Use aerosol-resistant filter tips [57]. Decontaminate surfaces with 10-15% fresh bleach solution [57] [56]. Maintain a unidirectional workflow [56]. |
| Systematic Reagent Contamination [53] | A contaminated batch of water, master mix, or primers. | Aliquot all reagents to avoid repeated freeze-thaw cycles [57]. Test reagents in small batches to identify and replace the contaminated component. |
| PCR Product Carryover [53] [57] | Contamination of pre-PCR areas with amplicons from previous reactions. | Incorporate uracil-N-glycosylase (UNG) into the protocol [53] [57]. Physically separate pre- and post-PCR areas [57] [56]. |
Decision Workflow for Interpreting Controls
The following diagram outlines a systematic decision-making process for investigating and resolving issues identified by negative controls and NTCs.
Experimental Protocols for Validation and Monitoring
Implementing these controls requires integration into standardized, repeatable protocols. The following methodologies are adapted from validated industrial and research practices.
Protocol for a Contamination Check Assay
This protocol is designed to systematically identify the source of contamination when an NTC repeatedly tests positive [53] [57].
- Objective: To pinpoint the specific reagent or component causing amplification in the NTC.
- Experimental Setup:
- Prepare a master mix excluding one component at a time (e.g., a mix without primers, a mix without probe, a mix without water).
- For each "missing component" mix, add the omitted component from a fresh, uncontaminated stock.
- Include a positive control with all components to ensure assay functionality.
- Run the assay in duplicate on a real-time PCR instrument.
- Interpretation: The reaction tube that fails to amplify (i.e., shows a negative result) pinpoints the contaminated component. For example, if the reaction without primers added from the new stock is negative, but the others are positive, the original primer stock is contaminated.
Standardized NTC Integration in a qPCR Workflow
This protocol ensures consistent monitoring in every run, as demonstrated in quality control testing for pathogens [55].
- Sample and Control Placement:
- The NTC should be included on every reaction plate.
- It is recommended to run NTCs in duplicate to distinguish random from systematic contamination [55].
- Place NTCs in different locations on the plate (e.g., beginning, middle, end) to detect localized contamination events.
- Reaction Composition:
- The NTC well contains the same volume of master mix, primers, probes, and water as the test samples.
- The template DNA is replaced with an equivalent volume of PCR-grade water.
- Thermal Cycling: The NTC is subjected to the exact same thermal cycling conditions as all other samples on the plate [55].
The Scientist's Toolkit: Essential Reagents and Materials
A successful contamination control strategy relies on the correct use of specialized reagents and laboratory materials.
Table 3: Research Reagent Solutions for Contamination Prevention
| Item | Function in Contamination Control |
|---|---|
| Aerosol-Resistant Filter Pipette Tips [57] | Preents aerosols from entering the pipette shaft, thereby protecting reagents and samples from cross-contamination. |
| PCR-Grade Water [57] | Nuclease-free and certified to contain no contaminating DNA or RNA, making it safe for preparing master mixes and NTCs. |
| Uracil-N-Glycosylase (UNG) / UDG Enzyme [53] [57] | A enzymatic carryover prevention system. It degrades PCR products from previous reactions that contain dUTP, preventing their re-amplification. |
| 10-15% Fresh Bleach Solution [57] [56] | A critical surface decontaminant. It effectively degrades DNA and RNA on bench tops, equipment, and other touch points. |
| Aliquoted Reagents [57] | Storing reagents (primers, master mix, water) in small, single-use volumes prevents the contamination of an entire stock and limits freeze-thaw cycles. |
| Dedicated Lab Coats and Gloves [57] [56] | PPE designated exclusively for the pre-PCR area prevents the introduction of amplicons from post-PCR areas. |
| 1-(2-Phenylindolizin-3-yl)ethanone | 1-(2-Phenylindolizin-3-yl)ethanone, CAS:38320-58-0, MF:C16H13NO, MW:235.286 |
Strategic Integration into a Broader Prevention Framework
Interpreting controls is only one component of a holistic contamination prevention strategy, which must be embedded in the laboratory's physical design and workflow.
Laboratory Design and Workflow
The most effective way to prevent contamination is through physical separation, creating a unidirectional workflow that moves from clean to dirty areas [57] [56].
Key Principles:
- Pre-PCR Area: This dedicated space, ideally with separate rooms for master mix preparation and sample handling, is for all activities involving open tubes of template-free reagents and raw samples [57] [56]. Equipment and consumables here must never enter a post-PCR area.
- Post-PCR Area: This physically separated room houses the thermal cyclers and equipment for analyzing PCR products. Tubes containing amplicons should never be opened in the pre-PCR area [57] [56].
- Unidirectional Workflow: Personnel and materials must flow from pre-PCR to post-PCR, never in reverse, without thorough decontamination [57] [56].
Building a Culture of Contamination Awareness
Ultimately, technical controls are only as strong as the laboratory culture that supports them. Researchers must be trained to view contamination as a constant risk and to adopt proactive habits: frequently changing gloves, using proper pipetting techniques to avoid splashing, and meticulously decontaminating workspaces before and after use [57] [56]. By framing the interpretation of NTCs and negative controls not as a failure, but as a critical diagnostic tool, laboratories can build a robust defense against contamination, ensuring the integrity of their research and the development of reliable diagnostics and therapeutics.
This guide provides a systematic framework for researchers to identify and eliminate contamination sources during sample preparation, a critical phase where up to 75% of laboratory errors originate [15]. Effective contamination management is fundamental to ensuring data integrity, reproducibility, and the success of downstream experiments and drug development processes.
Recognizing the pattern of contamination is the first step in tracing its origin. The table below outlines common contamination signatures and their most likely sources.
Table 1: Contamination Patterns and Associated Sources
| Contamination Pattern | Probable Sources | Impact on Sample Integrity |
|---|---|---|
| Cross-contamination between samples | Improperly cleaned or reused tools (e.g., homogenizer probes) [15], aerosol generation during pipetting, inadequate workflow separation [58]. | Skewed data, false positives/negatives, compromised reproducibility [15]. |
| Widespread microbial or DNA/RNA contamination | Contaminated water or reagent supplies [58], non-sterile labware, compromised environment (airborne particles, surfaces) [15]. | Altered microbial assays, failed PCR analyses, masked target analytes [15]. |
| Consistent background contamination in controls | Contaminated water or buffer stocks [58], improperly sterilized equipment, leaching from plasticware. | Inability to establish a reliable baseline, invalidated experimental results [15]. |
| Introduction of specific host signals (e.g., human, bird, cow) | Direct environmental sources (e.g., fecal matter from humans, birds, livestock) [59] [60], sample handling without proper PPE [58]. | Misidentification of contamination sources in environmental or biological studies [60]. |
Methodologies for Source Identification
Once a pattern is recognized, targeted methodologies can be employed to confirm the contamination source.
Microbial Source Tracking (MST)
Microbial Source Tracking is a powerful tool for identifying biological contamination origins, especially in environmental and water quality research. It leverages the distinct microbial communities, or "fingerprints," associated with different hosts and environments [60].
- Principle: Different pollution sources (e.g., livestock, urban runoff, agricultural fertilizer) harbor unique microbial communities. By comparing the microbial profile of a contaminated sample to a library of known source profiles, the primary contributor can be identified [59] [60].
- Protocol: Two primary genome-based approaches are used:
- qPCR-based MST: This method uses quantitative polymerase chain reaction (qPCR) to detect and quantify host-specific genetic markers (e.g., bacterial genes associated with humans, birds, or cows). It is highly sensitive and provides quantitative data on the contribution of each source [59].
- Sequencing-based MST: This involves high-throughput sequencing (e.g., 16S rRNA gene amplicon sequencing) of the sample's entire microbial community. Machine learning classification systems, like SourceTracker, then use a Bayesian approach to determine the proportion of the sample's community that comes from each potential source environment [60].
- Application Example: In a study of Vaughn Bay, both qPCR and sequencing-based MST identified birds and humans as the primary sources of fecal contamination. Sequencing was recommended for large-scale source identification, followed by targeted qPCR for precise quantification [59].
Environmental and Tool Monitoring
Proactive monitoring helps identify contamination vectors before they compromise critical samples.
- Principle: Systematically test the laboratory environment and tools to ensure they are not contributing contaminants.
- Protocols:
- Water Purity Check: If all samples, including negative controls, show contamination, test the water supply. Use an electroconductivity meter to detect chemical impurities or culture media to test for microbial growth [58].
- Tool and Surface Decontamination Check: After cleaning reusable tools like stainless steel homogenizer probes, run a blank solution through them to test for residual analytes [15]. Swab surfaces and use specialized decontamination solutions (e.g., DNA Away) and test for residual contaminants [15].
- Air Quality Verification: Ensure laminar flow hoods and HEPA filters are functioning correctly to prevent airborne contamination [58].
Contamination Source Identification Workflow
The following diagram provides a logical workflow for tracing the source of contamination based on the observed pattern.
Experimental Protocols for Contamination Identification
Protocol for SourceTracker Analysis
This protocol uses sequencing data to quantitatively apportion contamination among potential sources [60].
- Sample Collection: Collect triplicate samples from both contaminated "sink" sites (e.g., downstream river water) and potential "source" sites (e.g., livestock land, urban runoff, agricultural areas).
- DNA Extraction & Sequencing:
- Filter samples through 0.22 μm cellulose acetate filters.
- Extract genomic DNA using a commercial kit (e.g., FastDNA Spin Kit).
- Amplify the V3-V4 region of the 16S rRNA gene using primers 338F and 806R.
- Sequence the amplicons on a platform like Illumina MiSeq PE250.
- Bioinformatic Analysis:
- Process raw sequences to filter for quality and assign to Operational Taxonomic Units (OTUs) at 97% identity.
- Classify OTUs taxonomically using a reference database (e.g., Silva v128).
- SourceTracker Execution:
- Input the normalized OTU tables for both source and sink samples into the SourceTracker algorithm.
- Use default parameters: rarefaction depth=1,000, burn-in=100, restart=10, alpha=0.001, beta=0.01.
- Run multiple iterations (e.g., five) and average the results to obtain the proportional contribution of each source to the sink samples.
Protocol for Tool and Reagent Contamination Check
A simple protocol to verify the cleanliness of reusable laboratory tools [15].
- Principle: Flushing a cleaned tool with a blank solution and analyzing the effluent for residual contaminants.
- Procedure:
- Preparation: Clean the reusable tool (e.g., stainless steel homogenizer probe) according to the standard laboratory protocol.
- Blank Flush: Homogenize or flush the tool with a known clean, blank solution (e.g., purified water or appropriate buffer).
- Analysis: Analyze the blank effluent using a sensitive method relevant to the analytes typically processed (e.g., spectrophotometry, qPCR, microbial plating).
- Interpretation: The presence of target analytes in the blank indicates inadequate cleaning and a high risk of cross-contamination.
Research Reagent Solutions for Contamination Control
The following table details essential materials and reagents used in the featured experiments for contamination prevention and analysis.
Table 2: Key Research Reagent Solutions for Contamination Control
| Item | Function/Application | Example Use Case |
|---|---|---|
| Disposable Homogenizer Probes (e.g., Omni Tips) | Single-use probes to eliminate cross-contamination between samples during homogenization [15]. | Processing multiple sensitive biological samples in sequence. |
| Hybrid Homogenizer Probes | Combine a reusable stainless steel shaft with a disposable plastic rotor, offering durability while minimizing contamination risk [15]. | Homogenizing tough or fibrous samples where pure plastic probes may lack robustness [15]. |
| Specialized Decontamination Solutions (e.g., DNA Away) | Chemically degrade and remove specific residual contaminants, such as DNA, from lab surfaces and equipment [15]. | Preparing a DNA-free workspace for PCR or other sensitive molecular biology techniques. |
| HEPA Filters & Laminar Flow Hoods | Create a sterile workspace by removing 99.9% of airborne particulates and microbes, preventing environmental contamination [58]. | Sample transfers, cell culture work, and any open-container manipulations. |
| Automated Liquid Handlers | Enclosed systems that automate pipetting, drastically reducing human error and cross-contamination [58]. | High-throughput screening assays and repetitive sample plating. |
| SourceTracker Software | A Bayesian algorithm for identifying sources of contaminants by comparing microbial community fingerprints [60]. | Apportioning pollution in environmental water samples to specific upstream sources (e.g., agriculture, industry). |
Proactive Contamination Prevention Strategies
Preventing contamination is more efficient than tracing it. Key strategies include:
- Workflow Automation: Implementing automated liquid handling systems within enclosed hoods significantly reduces human error and cross-contamination [58].
- Rigorous Tool Management: Choose probe types based on workload: disposable probes for high-throughput sensitive work, and rigorously validated cleaning protocols for reusable probes [15].
- Environmental Control: Use laminar flow hoods with HEPA filters and UV lights. Maintain strict cleaning schedules for surfaces and equipment with appropriate disinfectants [15] [58].
- Personal Protective Equipment (PPE): Mandate lab coats, gloves, and closed-toe shoes. Change gloves between samples and never reuse disposable gloves [58].
Decontaminating Equipment and Reclaiming a Contaminated Workspace
In sample preparation research, the integrity of scientific data is fundamentally dependent on the prevention and control of contamination. The inadvertent introduction of physical, chemical, or microbiological contaminants can compromise samples, leading to inaccurate analytical results, failed experiments, and invalid conclusions. Effective decontamination of equipment and reclamation of workspaces are therefore not merely housekeeping tasks but critical scientific procedures that underpin research quality and reproducibility. This guide provides an in-depth technical framework for researchers and drug development professionals to manage contamination risks, with a specific focus on maintaining the fidelity of sample preparation processes. A proactive contamination control strategy (CCS), as emphasized in modern regulatory guidance like EU GMP Annex 1, is essential for any laboratory aiming to produce reliable and meaningful data [61].
Risk Assessment and Contamination Typology
Before implementing decontamination protocols, a thorough risk assessment must be conducted to identify the nature and source of contamination. This assessment directly informs the selection of appropriate decontamination agents and methods.
Table 1: Classification and Characteristics of Common Laboratory Contaminants
| Contaminant Type | Examples | Potential Sources in Sample Prep | Primary Concerns |
|---|---|---|---|
| Chemical | Per- and polyfluoroalkyl substances (PFAS), solvents, lubricants, cleaning agents [10] [62] | Impure reagents, carryover from previous samples, leaching from equipment, cleaning residues | Sample interference, inaccurate chromatographic or spectroscopic results, chemical exposure hazards |
| Particulate | Dust, fibers, skin cells, pollen, foreign objects [62] | Unclean air, shedding from personnel clothing or equipment, poor housekeeping | Physical interference, clogging of instrumentation (e.g., HPLC, UHPLC), sample adulteration |
| Microbiological | Bacteria, moulds, spores, yeasts [62] | Personnel, non-sterile surfaces, contaminated water or reagents, air | Sample degradation, introduction of enzymatic activity, false positives in bioassays |
| Cross-Contamination | Carryover of a previous batch, different product, or foreign starting material [62] | Inadequate equipment cleaning, shared use of non-dedicated tools, improper storage | Batch failure, erroneous potency or purity results, product mix-ups |
Decontamination Agents and Methodologies
Chemical Disinfectants and Their Applications
Selecting the correct chemical agent is crucial for effective decontamination. The choice depends on the target microorganism, the presence of organic material, and the material compatibility of the equipment being treated.
Table 2: Properties and Uses of Common Laboratory Disinfectants
| Disinfectant | Optimum Concentration | Spectrum of Activity | Advantages | Disadvantages & Safety Concerns | Common Laboratory Applications |
|---|---|---|---|---|---|
| Alcohols (Ethyl, Isopropyl) | 60%–90% (v/v) [63] | Bactericidal, tuberculocidal, fungicidal, virucidal (lipophilic viruses); not sporicidal [63] | Fast-acting, no toxic residue, inexpensive | Evaporates quickly; not effective against bacterial spores; flammable; can swell/harden rubber and plastics [63] | Disinfection of small surfaces (e.g., stoppers, stethoscopes), external surfaces of equipment [63] |
| Hypochlorites (e.g., Bleach) | Varies by application; 5.25%-6.15% is common household bleach [63] | Broad spectrum, including spores at high concentrations [63] | Fast-acting, inexpensive, unaffected by water hardness | Corrosive to metals; inactivated by organic matter; releases toxic gas if mixed with ammonia or acid; bleaches fabrics [63] | Surface disinfection, especially in spill situations involving high-risk biological material |
| Chlorine Dioxide | ~140 ppm for general disinfection [63] | Effective against bacteria, Mycobacterium, and spores with sufficient contact time [63] | Retains activity longer than hypochlorites; less corrosive | Must be prepared fresh; can damage some plastics with long-term use [63] | High-level disinfection of heat-sensitive equipment like flexible endoscopes in washer-disinfectors [63] [64] |
| Hydrogen Peroxide | Varies (e.g., for vapor phase) | Broad-spectrum, sporicidal | Leaves no residue; effective in vapor phase for room decontamination | Can be corrosive; requires specialized equipment for vapor generation | Surface disinfection, sterilization of isolators and chambers via vaporized hydrogen peroxide (VHP) |
| Quaternary Ammonium Compounds (QACs) | Varies by formulation | Bactericidal, fungicidal, virucidal (lipophilic viruses); not sporicidal [64] | Good cleaning properties; low odor; surface compatible | Easily inactivated by organic matter and anionic detergents; not sporicidal [64] | General surface cleaning and disinfection in non-critical areas |
Modern Decontamination Technologies
Beyond liquid chemicals, several advanced technologies enhance decontamination efficacy:
- Superoxidized Water: Generated by electrolysis of saline, producing a mixture of hypochlorous acid and chlorine. Its antimicrobial activity is strongly affected by the concentration of available free chlorine and is effective for disinfecting delicate instruments like endoscopes [63] [64].
- Gaseous Hydrogen Peroxide: Used in automated systems for bio-decontamination of rooms, isolators, and complex equipment. Enzyme indicator systems are available to validate and monitor the process [61].
- Ductless Fume Hoods: These systems use advanced filtration (e.g., activated carbon for chemicals, HEPA for particulates) to remove hazardous vapors and particles from the workspace, recirculating clean air. They are energy-efficient and offer flexibility in lab layout. Crucially, they must be matched to the specific chemicals in use, as the filters are application-dependent [65] [66].
Experimental Protocols for Decontamination and Reclamation
General Workflow for Reclaiming a Contaminated Workspace
The following diagram outlines the logical decision-making process for responding to and recovering from a contamination incident.
Contamination Response Workflow
Detailed Protocol: Solid-Phase Extraction (SPE) Cartridge Cleaning and PFAS Decontamination
1. Objective: To decontaminate reusable SPE manifolds and adjacent workspace from PFAS carryover, which can cause significant interference in subsequent analyses of other samples [10].
2. Principle: PFAS are persistent environmental contaminants. Dedicated equipment is ideal, but when reclamation is necessary, a rigorous solvent cleaning protocol is required to displace and dissolve PFAS residues from glass, metal, and plastic surfaces.
3. Materials:
- Reusable SPE manifold (glass, PTFE components)
- Methanol (HPLC grade)
- Acetonitrile (HPLC grade)
- Isopropyl alcohol (Reagent grade)
- Deionized water (PFAS-free if possible)
- Nitrile gloves, lab coat
- Glass wash bottles and dedicated clean glassware
4. Procedure:
- Isolation: Remove the contaminated manifold from the general work area. If possible, perform all cleaning steps in a fume hood designated for solvent use.
- Disassembly: Dismantle the manifold completely, separating glass barrels, PTFE frits, valves, and vacuum chambers.
- Solvent Rinsing:
- First Wash: Thoroughly rinse all components with methanol to dissolve and remove the majority of PFAS compounds. Collect all waste solvent appropriately.
- Second Wash: Perform a second rinse with acetonitrile to address PFAS that may be less soluble in methanol.
- Third Wash: Rinse with isopropyl alcohol to displace water-miscible solvents and prepare for a final water rinse.
- Aqueous Rinsing: Rinse all components generously with copious amounts of deionized water to remove any residual solvents and salts.
- Drying: Air-dry the components in a clean, dust-free environment or use a stream of clean, oil-free nitrogen gas.
- Validation: To validate the decontamination, process a blank sample (e.g., pure water or methanol) through the cleaned manifold and analyze it using the intended LC-MS/MS method. The chromatogram should show no detectable PFAS peaks above the method's limit of quantification.
5. Workspace Decontamination: Wipe down all surrounding surfaces (bench, fume hood interior, tools) with methanol followed by isopropyl alcohol. Replace any disposable liners. For persistent contamination, consider using a specialized PFAS cleaning solution or commercially available pre-saturated wipes.
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Contamination Control
| Reagent/Material | Technical Function | Application Example |
|---|---|---|
| Captiva EMR Cartridges (e.g., for PFAS, Mycotoxins, Lipids) [10] | Enhanced Matrix Removal; pass-through cleanup cartridges that selectively bind and remove specific classes of matrix interferents. | Simplifying sample prep for LC-MS/MS analysis by eliminating manual QuEChERS steps, reducing matrix effects, and minimizing environmental waste [10]. |
| Resprep PFAS SPE Cartridge [10] | Dual-bed solid-phase extraction cartridge with weak anion exchange and graphitized carbon black for selective PFAS extraction and cleanup. | Preparation of aqueous and solid samples for EPA Method 1633, which measures up to 40 PFAS in various matrices [10]. |
| Isopropyl Alcohol (70-90% v/v) [63] | Protein denaturation, leading to bactericidal, tuberculocidal, fungicidal, and virucidal (for lipid viruses) action. | Routine disinfection of non-critical surfaces like benchtops, instrument exteriors, and rubber stoppers. |
| Sodium Hypochlorite Solution (Bleach, 0.5-1%) [63] | Oxidative destruction of cellular components; broad-spectrum activity including against spores with sufficient concentration and contact time. | Decontamination of spills involving biological materials or for surface disinfection in high-risk areas. |
| Ductless Fume Hood with Chemical Filtration [65] [66] | Protects the operator and the laboratory environment by capturing and removing hazardous chemical vapors and particulates through adsorption/filtration, recirculating clean air. | Provides a contained, clean workspace for sample preparation steps involving volatile organic solvents or powdered materials, without the cost and infrastructure of ducted hoods. |
| Modern Microbial Method (MMM) Kits (e.g., ATP bioluminescence, solid-phase cytometry) [61] | Rapid detection and enumeration of viable microorganisms, offering faster results than traditional culture-based methods. | Rapid verification of cleaning efficacy on equipment surfaces and monitoring of the laboratory environment for microbial contamination. |
Prevention: Integrating Decontamination into a Holistic Contamination Control Strategy
Preventing contamination is far more effective than responding to it. A robust Contamination Control Strategy (CCS) should be multi-faceted and integrated into all aspects of laboratory operations [62] [61].
- Facility and Airflow Design: Utilize positive pressure cleanrooms to exclude particles and bacteria when product protection is critical (e.g., sterile product processing). Use negative pressure rooms with dust extraction to contain product dust and prevent cross-contamination during processing of dry oral products like tablets. Always keep doors closed to maintain pressure differentials [62].
- Personnel Practices: Enforce strict gowning procedures, proper hand hygiene, and comprehensive training on contamination risks and standard operating procedures (SOPs). Personnel are a primary source of microbial and particulate contamination [62].
- Raw Material and Storage Control: Store materials off the floor, clean spills immediately, and ensure all containers are clearly labeled. Implement a first-expired-first-out (FEFO) system and maintain strict separation between quarantined, approved, and rejected materials [62].
- Validated Cleaning and Disinfection Procedures: Develop and adhere to written SOPs for cleaning equipment and facilities. The frequency and rigor of cleaning should be risk-based. Employ line clearance procedures before starting a new batch to prevent cross-contamination [62].
- Leverage Modern Microbial Methods (MMMs): Implement technologies like ATP bioluminescence for rapid cleaning verification, flow cytometry for rapid water bioburden analysis, or air particle counters with intrinsic fluorescence for real-time monitoring of air quality. These methods provide faster results, enabling proactive intervention and continuous improvement of the CCS [61].
Decontaminating equipment and reclaiming a contaminated workspace are foundational to the integrity of sample preparation research. A systematic approach—beginning with risk assessment, followed by the application of validated protocols using appropriate agents, and culminating in verification of efficacy—is non-negotiable. Furthermore, by integrating these reactive measures into a proactive, holistic Contamination Control Strategy that encompasses facility design, personnel training, and modern monitoring technologies, research laboratories can significantly reduce the frequency and impact of contamination events. This disciplined approach ensures the generation of high-quality, reliable data, safeguards the well-being of personnel, and ultimately accelerates the pace of scientific discovery and drug development.
Optimizing Cleaning Validation for Reusable Labware and Instruments
In sample preparation research, the integrity of scientific data is fundamentally dependent on the cleanliness of reusable labware and instruments. Cleaning validation provides documented evidence that a cleaning procedure consistently removes contaminants to predetermined acceptable levels, thereby preventing cross-contamination and false results [67]. For researchers and drug development professionals, a robust cleaning validation program is not merely a regulatory formality but a critical component of the Contamination Control Strategy (CCS) that ensures the reliability and reproducibility of experimental outcomes [68].
The consequences of inadequate cleaning are severe. Contaminants from improperly cleaned tools can alter results, compromise reproducibility, and reduce the sensitivity of analytical methods [15]. In pharmaceutical development, this can lead to product recalls or public health crises [69]. This guide outlines a science-based framework for optimizing cleaning validation specifically for research environments, providing detailed protocols and acceptance criteria to safeguard sample integrity from preparation to analysis.
Regulatory Framework and Acceptance Criteria
While research laboratories may not operate under the same strict Good Manufacturing Practice (GMP) regulations as pharmaceutical production, the principles from agencies like the FDA, EMA, and WHO provide a essential foundation for establishing scientifically sound cleaning protocols [70]. These guidelines emphasize a risk-based approach where the rationale for residue limits must be logical, practical, achievable, and verifiable [23].
Key Regulatory Principles
Regulatory bodies focus on several core expectations for cleaning validation [23] [67]:
- Written Procedures: Detailed Standard Operating Procedures (SOPs) for cleaning processes.
- Validation Protocols: Pre-approved plans specifying sampling procedures, analytical methods, and acceptance criteria.
- Documented Evidence: Final validation reports with data demonstrating residues are reduced to an "acceptable level."
- Lifecycle Management: Ongoing monitoring and periodic revalidation to ensure continued control.
Defining Acceptance Criteria
Establishing scientifically justified acceptance criteria is fundamental. The following table summarizes common approaches for setting residue limits in pharmaceutical and research contexts:
Table 1: Acceptance Criteria Approaches for Cleaning Validation
| Basis for Criteria | Typical Limit | Application Context | Considerations |
|---|---|---|---|
| Analytical Detection | 10 ppm [23] | General pharmaceutical manufacturing | Must verify method sensitivity is sufficient for risk level |
| Toxicological Assessment | 1/1000 of normal therapeutic dose [23] | API and potent compound manufacturing | Requires health-based exposure limit (HBEL) calculation [68] |
| Visual Inspection | No visible residue [23] | Standardized light intensity (≥750 lux) [71] | Considered insufficient as sole criteria by EMA [68] |
| Microbiological | 3-log reduction (cleaning), 6-log reduction (disinfection) [72] | Reusable devices/semi-critical labware | Must validate method recovery efficiency [72] |
For research laboratories, the most practical approach often combines visual inspection with analytical detection limits appropriate for the sensitivity of downstream assays. The criteria should be established based on the analytical technique's detection limit and the potential for the residue to interfere with research outcomes [15].
Cleaning Validation Methodology
A structured methodology ensures cleaning processes are consistently effective. The following workflow outlines the comprehensive validation lifecycle, from initial planning to ongoing monitoring.
Diagram 1: Cleaning Validation Lifecycle Workflow
Phase 1: Process Design and Development
The foundation of successful cleaning validation is established in the planning phase.
Developing the Validation Protocol
Create a comprehensive protocol that specifies [67]:
- Objective and Scope: Clearly define what equipment and residues the validation will cover.
- Responsibilities: Identify who performs, reviews, and approves each activity.
- Sampling Plan: Specify swab, rinse, or placebo sampling locations and methods.
- Analytical Methods: Define test methods with demonstrated sensitivity and specificity.
- Acceptance Criteria: Establish scientifically justified limits for all residue types.
Conducting Risk Assessment
A thorough risk assessment identifies worst-case scenarios and critical control points [71]. Key factors to evaluate include:
- Equipment Design: Complex geometries, dead legs, rough surfaces (Ra ≤ 0.8 µm ideal), and difficult-to-dismantle components increase risk [72] [71].
- Residue Properties: Poor solubility, high potency, and strong adhesion to surfaces make residues harder to remove.
- Process Parameters: Time between processing and cleaning, soil drying, and campaign length affect cleaning efficacy [23].
Phase 2: Performance Qualification
This phase provides documented evidence that the cleaning process consistently meets acceptance criteria.
Sampling Methods and Techniques
Selecting appropriate sampling methods is critical for accurate residue detection:
Table 2: Sampling Methods for Cleaning Validation
| Method | Procedure | Best For | Limitations |
|---|---|---|---|
| Swab Sampling | Use validated swab (e.g., polyester, cotton) on defined area (e.g., 10×10 cm); extract in suitable solvent [67] | Direct surface sampling of critical, hard-to-clean areas [23] | Operator dependent; may miss residues in inaccessible areas; requires recovery validation |
| Rinse Sampling | Collect final rinse water or solvent after cleaning; analyze for residues [23] | Large surface areas; complex equipment; inaccessible systems (CIP) | Dilution effect may reduce sensitivity; may not detect insoluble residues |
| Placebo Sampling | Run inert material through equipment after cleaning; analyze for carried-over residues [70] | Demonstrating absence of cross-contamination in manufacturing | Less applicable to labware; may not contact all surfaces |
Analytical Method Validation
Any analytical method used (HPLC, TOC, conductivity) must be validated for this specific application. Key validation parameters include [68] [23]:
- Detection and Quantitation Limits: Must be sufficiently sensitive to detect residues below the acceptance criterion.
- Specificity: Ability to detect target analyte in the presence of other components.
- Recovery Efficiency: Demonstrate consistent residue recovery from surfaces (typically >80% for swab sampling) [71].
- Linearity and Range: Response should be proportional to analyte concentration across the expected range.
Phase 3: Ongoing Verification and Monitoring
Cleaning validation is not a one-time event. Implement continuous monitoring to ensure the process remains in control [71]:
- Periodic Testing: Schedule routine testing at defined intervals based on risk assessment.
- Alert and Action Limits: Set limits (e.g., 70% of action level) for trending purposes.
- Visual Inspection: Require visual inspection under adequate lighting (≥750 lux) after every cleaning cycle [71].
- Change Control: Revalidate when significant changes occur (equipment, process, or product).
Experimental Protocols for Validation Studies
Protocol 1: Swab Recovery Efficiency Study
This foundational study validates the ability to recover residues from specific surface materials.
Objective: To determine the percentage of residue recovered from coupon surfaces representing equipment materials using the selected swabbing technique.
Materials:
- Table 4: Research Reagent Solutions for Recovery Studies
- Coupons (e.g., 10×10 cm) of relevant materials (316L stainless steel, borosilicate glass, PTFE)
- Standard solution of target analyte at known concentration
- Validated swabs (e.g., polyester tip with plastic handle)
- Appropriate extraction solvent
- Certified analytical equipment (HPLC, TOC analyzer, spectrophotometer)
Table 3: Research Reagent Solutions for Recovery Studies
| Item | Function | Key Considerations |
|---|---|---|
| Polyester Swabs | Physical removal and retention of residues from surfaces | Low extractable background; confirmed material compatibility with solvents [15] |
| Extraction Solvent | Dissolving residues from swabs for analysis | Must completely dissolve analyte without interfering with detection method |
| Standard Solutions | Quantifying recovery efficiency | Certified reference materials with known purity and concentration |
| Coupon Materials | Representing equipment surfaces | Must match actual equipment composition and surface finish (Ra) |
Procedure:
- Clean all coupons thoroughly and verify absence of interference.
- Apply known quantity of standard solution (e.g., 100 μL) to coupon surface and spread evenly.
- Allow solvent to evaporate completely under controlled conditions.
- Swab the entire surface systematically using predefined pattern and pressure.
- Transfer swab to container with exact volume of extraction solvent.
- Agitate/swirl for defined time to extract residues.
- Analyze extract and quantify recovered residue.
- Calculate recovery percentage: (Recovered Amount / Applied Amount) × 100.
Acceptance Criteria: Recovery should be consistent and typically >80% with relative standard deviation (RSD) <15% between replicates [71].
Protocol 2: Cleaning Efficacy under Worst-Case Conditions
This protocol challenges the cleaning process with the most difficult-to-remove residues.
Objective: To demonstrate that the cleaning procedure effectively removes residues under worst-case conditions.
Materials:
- Actual equipment or representative coupons
- Standardized soil load (e.g., 1-4 g/ft²) [71]
- Cleaning agents and tools specified in SOP
- Sampling materials (swabs, rinse containers)
- Analytical equipment
Procedure:
- Prepare standardized soil with target analyte at maximum expected concentration.
- Apply soil to equipment/coupons and allow to dry for maximum dirty hold time.
- Execute cleaning procedure according to SOP, documenting all parameters (time, temperature, concentration).
- Sample using all relevant methods (swab, rinse).
- Analyze samples for residue levels.
- Repeat for three consecutive successful cycles [67].
Acceptance Criteria: All analyte levels must be below established limits; equipment must be visually clean; microbial counts must meet pre-defined criteria.
Risk Assessment and Equipment Considerations
A science-based risk assessment is essential for focusing validation efforts on the highest priority areas.
Equipment Design and Complexity
Equipment characteristics significantly impact cleanability. High-risk features include [72] [71]:
- Long, Narrow Lumens: Difficult for brushes to reach interior surfaces.
- Hinges, Crevices, and Dead Legs: Trap soil and resist cleaning flow.
- Rough Surface Finishes: Ra > 0.8 µm provides more adhesion sites for residues.
- Mixed Material Construction: Different thermal expansion and chemical compatibility.
- Complex Assemblies: Require disassembly for proper cleaning.
For high-risk equipment, consider design modifications, custom cleaning tools, or dedication to specific high-risk applications [72].
Manual vs. Automated Cleaning
Both manual and automated cleaning methods require validation, but present different challenges:
Table 4: Comparison of Cleaning Methods for Labware
| Parameter | Manual Cleaning | Automated Cleaning |
|---|---|---|
| Validation Focus | Operator technique, training, consistency [71] | Parameter control (time, temperature, flow rate) [71] |
| Key Variables | Brush type, pressure, pattern, detergent contact time | Spray coverage, impingement, chemical concentration, rinse cycles |
| Advantages | Adaptable to complex geometries; immediate visual feedback [73] | Consistent, reproducible cycles; reduced operator dependency [73] |
| Documentation | Detailed SOPs with photographs; training records [23] | Electronic batch records with parameter monitoring [68] |
Application-Specific Validation Guidelines
Reusable Medical Devices and Surgical Instruments
The validation requirements for reusable devices are well-established and can inform laboratory instrument validation [72] [74]:
- Critical Devices (contact sterile body areas): Must be cleaned and sterilized (SAL 10â»â¶) [72].
- Semi-critical Devices (contact mucous membranes): Require cleaning and high-level disinfection (6-log reduction) [72].
- Non-critical Devices (contact intact skin): Require cleaning and low/intermediate-level disinfection [72].
Acceptance criteria typically include visual cleanliness, 3-log microbial reduction for cleaning, and specific residue limits (e.g., protein <6.4 μg/cm², hemoglobin <2.2 μg/cm²) [72].
Complex Laboratory Instruments
For specialized instruments like homogenizers, HPLC systems, or mass spectrometers:
- Homogenizer Probes: Risk of sample carryover is high. Use disposable probes (e.g., Omni Tips) for sensitive applications or validate cleaning with tough residues [15].
- Chromatography Systems: Focus on solvent compatibility and flushing volumes for needle seats, flow paths, and injection valves.
- Mass Spectrometers: Avoid high-salt or non-volatile additives that can contaminate ion sources.
Implementing a robust cleaning validation program for reusable labware and instruments is fundamental to research integrity. By adopting a risk-based approach, establishing scientifically justified acceptance criteria, and implementing a validation lifecycle with ongoing monitoring, research facilities can significantly reduce contamination risks during sample preparation. The methodologies and protocols outlined in this guide provide a framework for developing customized validation programs that protect research investments, ensure data reliability, and support regulatory compliance where required. As research methods evolve toward greater sensitivity, the importance of proven cleaning efficacy will only increase, making cleaning validation an essential discipline rather than an optional precaution.
This guide provides researchers and scientists with a systematic framework for identifying and investigating water, air, and HVAC systems as potential sources of contamination during sample preparation. Recognizing the signs of environmental contamination is crucial for ensuring data integrity, reproducibility, and the validity of experimental outcomes.
Prompt identification of contamination relies on recognizing specific, often overlapping, indicators from your samples and laboratory environment.
Table 1: Signs and Suspect Sources of Contamination
| Observed Indicator | Potential Source | Key Details & Common Contaminants |
|---|---|---|
| Unusual Taste/Smell | Water System [75] | Metallic, oily, fishy taste; chlorine or sulfur (rotten egg) smell. |
| Cloudy/Foamy Water | Water System [75] | Cloudiness that does not dissipate can indicate bacterial presence. |
| Blackening/Sediment | Water System [75] | Visible dirt or sediments in water or sinks. |
| Unexplained Results | All Sources [15] | False positives, false negatives, or altered baseline results in assays. |
| Compromised Reproducibility | All Sources [15] | Inability to replicate experimental results across different batches or days. |
| Reduced Assay Sensitivity | All Sources [15] | Target analytes are masked or diluted by contaminants. |
| Persistent Dust or Odors | HVAC System [76] | Dust levels uncontrollable by cleaning; unpleasant, persistent odors in the lab. |
| Dirty Vents/Filter Bypass | HVAC System [76] | Dirt streaks on or around filters and vents indicate system intake of contaminants. |
Diagnostic Experimental Protocols
When contamination is suspected, targeted sampling and analysis can confirm the source.
Investigating Water as a Source
Water is a universal solvent and a common vector for contaminants that can interfere with sensitive assays.
Protocol: Comprehensive Water Quality Testing [75] [77]
- Sample Collection: Collect water from the point of use (e.g., lab faucets, water purification unit outlets) into sterile, appropriate containers. Flush the line for several minutes before collecting to avoid stagnant water. For process control of purification systems, sample from various points in the distribution system [77].
- Visual and Olfactory Inspection: Note any cloudiness, particulates, or unusual odors immediately upon collection [75].
- Cultural Methods: Plate water samples on general culture media (e.g., Tryptic Soy Agar, Reasoner's 2A Agar) and incubate. Growth indicates non-sterile water and the presence of viable microorganisms [78].
- Chemical and Molecular Analysis:
- Conductivity/TOC: Use an electroconductive meter to check for ionic impurities and Total Organic Carbon (TOC) analyzers [78].
- PCR Testing: If DNA/RNA contamination is suspected, use PCR with water as the template to check for amplifiable nucleic acids [15].
- Broad-Spectrum Analysis: Techniques like gas chromatography-mass spectrometry (GC-MS) can identify a wide range of organic chemical contaminants [15].
Airborne contamination includes viable (bacteria, fungi, viruses) and non-viable (dust, chemicals) particulates.
Protocol: Airborne Microbiological Sampling [77] [79]
- Objective: To quantify and qualify viable airborne particles in the laboratory environment.
- Principle: Air is drawn at a known flow rate, and particles are captured on a solid medium (agar) or in a liquid for subsequent analysis.
- Method Selection:
- Sieve Impactors: A common choice where air is drawn through perforations in a cover and impacts a nutrient agar plate. Viable organisms are collected and can be cultured. Example: STA (Slit-to-Agar) Samplers [77].
- Liquid Impingement: Air is bubbled through a liquid medium, which captures particles. The liquid can then be cultured or analyzed via PCR, offering higher concentration efficiency for low-bioburden environments [80] [79].
- Centrifugal Samplers: Use an internal propeller to draw air and centrifugal force to impact particles onto a nutrient agar strip [77].
- Settle Plates: Passive method using open agar plates to measure sedimenting particles over several hours. Less quantitative but useful for long-term monitoring [77].
Protocol: HVAC System Inspection [76]
- Visual Inspection: Examine supply vents, return grilles, and filters for dust buildup, dirt trails, or microbial growth.
- Filter Assessment: Check for ill-fitting filters that allow "bypass" of unfiltered air, indicated by dirt streaks around the filter frame [76].
- Ductwork Inspection: Look for leaks in ducts, especially in return air pathways, which can draw unfiltered, contaminated air from building cavities (e.g., attics) into the system [76].
- Evaporator Coil Examination: This component, often wet from condensation, is a prime site for microbial growth (e.g., mold) and should be inspected if musty odors are present [76].
Mitigation and Prevention Strategies
Once a source is identified, implement these targeted corrective and preventive actions.
Table 2: Mitigation Strategies for Identified Contamination Sources
| Contamination Source | Corrective Actions | Preventive Strategies |
|---|---|---|
| Water System | Service or repair water purification systems; replace filters and resin beds [78]. | Use certified high-purity water (e.g., Type I); routinely test water quality; establish a scheduled maintenance plan for purification equipment [78]. |
| Laboratory Air | Decontaminate surfaces with appropriate agents (e.g., 70% ethanol, DNA Away) [15]. | Use HEPA-filtered laminar flow hoods for sample handling; install air filters; maintain positive room pressure [78]. |
| HVAC System | Seal leaks in ducts and around filter banks; clean contaminated evaporator coils and ductwork [76]. | Upgrade to higher-efficiency filters (e.g., MERV 13-16); implement a regular HVAC maintenance schedule; ensure proper filter installation and sealing [76] [81]. |
| General Lab Practice | Investigate and decontaminate tools implicated in cross-contamination [15]. | Automate liquid handling; use disposable consumables; wear proper PPE; establish unidirectional workflows; validate cleaning protocols for reusable tools [15] [78]. |
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Materials for Contamination Control
| Item | Function in Contamination Control |
|---|---|
| HEPA Filter | Removes 99.9% of airborne particulates (including microbes) from air supplied to laminar flow hoods and cleanrooms [78]. |
| Sterile Culture Media | Used in settle plates and air samplers to capture and grow viable airborne microorganisms for analysis [77]. |
| Liquid Impingement Samplers | Capture and concentrate airborne particles into a liquid matrix (hydrosol) for downstream cultural or molecular analysis (e.g., PCR) [80]. |
| Decontamination Solutions | Specific agents like DNA Away eliminate residual molecular analytes (e.g., DNA) from surfaces and equipment to prevent cross-contamination [15]. |
| High-Purity Water | Deionized or distilled water with verified purity is used for reagent preparation to prevent the introduction of contaminants from the water itself [78]. |
| Automated Liquid Handler | Enclosed systems with HEPA filtration and UV light that minimize human error and reduce sample-to-sample cross-contamination [78]. |
Proactive environmental monitoring and a disciplined approach to laboratory workflows are fundamental to preventing contamination. By integrating these diagnostic protocols and mitigation strategies, researchers can safeguard their samples, ensuring the generation of accurate, reliable, and reproducible scientific data.
Proving Your Process: Controls, Validation, and Comparative Method Analysis
In the field of biopharmaceutical research and manufacturing, the prevention of microbial contamination represents a fundamental requirement for ensuring product quality, patient safety, and regulatory compliance. Unlike medicines synthesized through highly controlled chemical processes, biopharmaceuticals involve dynamic biological systems that present unique vulnerabilities to contamination [1]. This inherent risk necessitates a proactive, risk-based strategy where comprehensive control measures play an indispensable role. Contamination events can originate from a multitude of sources—including raw materials, process inputs, manufacturing environments, and personnel—and can compromise products at any stage from cell-line development through fill–finish [1]. Within this context, a robust framework incorporating blanks, negative controls, and positive controls functions as the scientific backbone of an effective contamination control strategy, providing the necessary data to validate processes, detect deviations, and ultimately prevent compromised products from reaching patients.
The strategic implementation of these controls shifts the quality paradigm from reactive detection to proactive prevention. As noted in industry discussions, the biopharmaceutical industry increasingly recognizes that it is more effective to focus on preventive work covering an entire manufacturing process than to rely solely on final-product testing [1]. This whitepaper provides an in-depth examination of how blanks, negative controls, and positive controls serve as critical technical tools within this preventive framework, offering detailed methodologies, implementation protocols, and scientific rationale for their application in contamination-sensitive research and development environments.
Theoretical Foundations: Definitions and Functions
Positive Controls
Positive controls are samples or materials treated in a manner known to produce a positive result, thereby confirming that an experimental procedure is capable of detecting the target under investigation when it is present [82] [83]. These controls verify that all components of a testing system—reagents, instruments, and protocols—are functioning correctly. In practice, a positive control demonstrates that the experimental setup can indeed produce expected results under ideal conditions, thus validating the entire testing methodology. For example, in a Western blot experiment designed to detect a specific protein, a cell lysate known to express the protein of interest would serve as an effective positive control [82]. The appearance of the expected band on the blot confirms that the procedure, antibodies, and detection reagents are all working properly.
Negative Controls
Negative controls consist of samples treated identically to experimental samples but lacking the critical component being tested, thereby not expected to produce the measured effect [82] [83]. These controls are essential for demonstrating that any observed changes in the experiment are specifically due to the experimental variable rather than extraneous factors such as nonspecific binding, contamination, or procedural artifacts. Returning to the Western blot example, a negative control might be a cell lysate from cells that do not express the target protein [82]. The absence of a band in this lane confirms that detected signals in experimental samples are specific to the protein of interest rather than resulting from nonspecific antibody binding or other experimental artifacts.
Blanks
Blanks represent a specialized category of negative controls specifically designed to trace sources of artificially introduced contamination and account for background signals throughout the analytical process [84]. These analyte-free samples are collected, stored, treated, and analyzed in a manner as close as possible to authentic samples to identify contamination sources and methodological artifacts. As outlined in chromatography literature, blanks serve the vital function of distinguishing true analyte signals from interference, thereby ensuring the integrity of quantitative results [84]. Proper handling and treatment of blanks is essential, as analytical results are often calculated by subtracting the blank's contribution from the sample's analytical signal.
Table 1: Summary of Control Types and Their Primary Functions
| Control Type | Primary Function | Expected Result | Significance of Deviation |
|---|---|---|---|
| Positive Control | Verify experimental system functionality | Positive signal/result | Experimental system failure; results invalid |
| Negative Control | Detect nonspecific effects or contamination | No signal/result | Contamination or nonspecific effects present |
| Blank | Identify source and magnitude of background interference | Minimal to no signal | Specific contamination source or interference present |
Classification and Implementation of Blanks
Blanks can be categorized according to their specific purpose within the analytical workflow, with each type accounting for potential contamination introduced at different stages. The comprehensive use of multiple blank types enables researchers to pinpoint the exact source of contamination or interference, whether it originates from reagents, sampling equipment, the environment, or sample processing.
Types of Blanks and Their Applications
Method Blank: Composed of the sample matrix (absent the analyte) with all reagents from the analytical procedure in appropriate concentrations, the method blank serves to identify background contamination or interferences in the analytical system itself [84].
Field Blank: Subjected to the complete sample lifecycle—including collection, transportation, preservation, storage, and laboratory analysis—this comprehensive blank identifies contaminants or errors introduced during sample collection and handling [84].
Equipment Blank: Processed through sample collection equipment in a manner identical to authentic samples, this blank specifically identifies contamination derived from sampling apparatus [84].
Reagent Blank: Containing all analytical reagents in the same proportions specified in the method (but not carried through the complete analysis), this blank specifically measures interferences and contamination originating from the chemicals and analytical systems used [84].
Trip Blank: Particularly valuable for volatile compounds or those susceptible to degradation from light exposure, bacterial action, or freeze-thaw cycles, trip blanks accompany samples from collection to laboratory to account for changes during transport [84].
The relationship between these blank types and their coverage across the analytical process is visualized in the following workflow:
Establishing Detection Limits Through Blanks
Blanks play a fundamental role in determining the sensitivity of an analytical method through the statistical determination of detection limits. The Limit of Blank (LOB) represents the highest apparent analyte concentration observed in replicate measurements of blank samples, calculated as LOB = meanâ‚—â‚ₙₖ + 1.645(SDâ‚—â‚ₙₖ) [84]. This parameter establishes the threshold at which a signal can be distinguished from background noise. Building upon the LOB, the Limit of Detection (LOD) defines the lowest analyte concentration that can be reliably distinguished from the LOB, calculated as LOD = LOB + 1.645(SDₗₒ𓌠ð’¸â‚’â‚™ð’¸â‚‘ₙₜᵣâ‚ₜᵢₒₙ ð“ˆâ‚ₘₚₗₑ) [84]. These statistically derived parameters, intimately connected to blank measurements, provide the objective foundation for establishing an assay's detection capabilities and ensuring results fall within a validated range.
Table 2: Blank Types and Their Specific Applications in Contamination Control
| Blank Type | Composition & Treatment | Primary Contamination Source Identified | Acceptance Criteria |
|---|---|---|---|
| Method Blank | Sample matrix absent analyte, all reagents, full analytical procedure | Laboratory reagents, glassware, analytical system | < ½ lower limit of quantification |
| Field Blank | Analyte-free media, full sample lifecycle from collection to analysis | Sampling equipment, containers, preservatives, transport | < ½ lower limit of quantification |
| Reagent Blank | All analytical reagents in specified proportions, incomplete processing | Chemical contaminants, reagent impurities | Signal absent or minimal |
| Equipment Blank | Blank solution processed through sampling equipment | Sampling apparatus, carryover contamination | < ½ lower limit of quantification |
| Trip Blank | Blank accompanying samples from collection to lab | Transport conditions, degradation during transit | Stability of blank confirmed |
Implementation Strategies for Positive and Negative Controls
Selection and Validation of Control Materials
The implementation of effective positive and negative controls requires careful selection of appropriate biological materials and rigorous validation protocols. For immunological techniques such as Western blotting, flow cytometry, and immunohistochemistry, recommended control materials include:
Cell Lines with Endogenous Expression: Cell lines that naturally express the target antigen serve as optimal positive controls, while those confirmed to lack expression provide reliable negative controls [85]. For example, in validating a CD19 monoclonal antibody, the RAJI Burkitt's lymphoma cell line (CD19-positive) serves as a positive control, while JURKAT (T-cell lymphoma) and U937 (monocytic) cell lines function as negative controls [85].
Transfected Cells: Cells transfected with cDNA encoding the target antigen provide valuable positive controls, while cells transfected with empty vector alone serve as corresponding negative controls [85]. A critical prerequisite for this approach is confirming that host cells do not endogenously express the target protein or highly related cross-reactive proteins.
Tissue Microarrays (TMAs) : For immunohistochemistry applications, TMAs containing cores from multiple deliberately chosen tissues enable simultaneous validation across both positive control tissues (known to express the target) and negative control tissues (confirmed to lack the protein) on a single slide [85].
Purified Proteins: Purified proteins or peptides serve as ideal positive controls in techniques including Western blotting and ELISA, providing precise verification of antibody specificity and detection system functionality [82].
Control Strategies for Specific Methodologies
Western Blot Controls: Beyond standard positive and negative controls for the target protein, Western blotting requires additional controls for technical validation. Loading control antibodies, which recognize constitutively expressed housekeeping proteins (e.g., β-actin, tubulin, GAPDH), verify equal protein loading across samples [82]. These controls must be selected to have different molecular weights than the target protein to prevent signal overlap, and their consistent expression across experimental conditions must be confirmed.
Microbiological Testing Controls: In microbiological quality control, rapid microbiological methods (RMMs) increasingly complement traditional culture-based techniques. These methods—including technologies based on intrinsic fluorescence, bioluminescence, flow cytometry, and polymerase chain reaction (PCR)—require appropriate biological standards for validation [1] [61]. The implementation of reliable, authenticated reference materials is essential for confirming that these detection systems function as intended and provide accurate contamination monitoring [1].
The following diagram illustrates a comprehensive experimental workflow integrating multiple control types:
Experimental Protocols and Methodologies
Protocol for Blank Implementation in Analytical Chemistry
Objective: To identify and quantify sources of contamination and interference in liquid chromatography analysis through comprehensive blank implementation.
Materials:
- High-purity solvents (methanol, acetonitrile, water)
- Analytical standards (target analytes)
- Sample collection apparatus
- Glassware (vials, volumetric flasks)
- Preservatives (if used in method)
- UHPLC system with appropriate detector
Procedure:
- Calibration Blank Preparation: Prepare analyte-free media matching the sample matrix for instrument calibration and establishing baseline signals.
Field Blank Collection: Expose analyte-free media to the sampling environment using identical containers and procedures as actual samples.
Equipment Blank Processing: Pass blank solution through all sampling equipment following the same protocol used for authentic samples.
Method Blank Analysis: Subject the blank matrix with all analytical reagents through the complete sample preparation and analysis procedure.
Reagent Blank Testing: Analyze all reagents in appropriate concentrations without complete processing to identify reagent-derived contaminants.
Trip Blank Accompaniment: Transport analyte-free media alongside actual samples from collection site to laboratory under identical conditions.
Acceptance Criteria: All blank samples should demonstrate target analyte concentrations less than half the lower limit of quantification. Any deviation requires investigation into contamination sources before proceeding with sample analysis [84].
Protocol for Antibody Validation with Positive and Negative Controls
Objective: To validate antibody specificity for flow cytometry applications using appropriate cellular controls.
Materials:
- Antibody of interest with appropriate isotype control
- Positive control cell line with confirmed target expression
- Negative control cell line confirmed lacking target expression
- Flow cytometry staining buffer (PBS with 1% BSA)
- Fixation buffer (if required)
- Flow cytometer with appropriate configuration
Procedure:
- Cell Preparation: Harvest positive control, negative control, and experimental cells, ensuring consistent handling and viability.
Antibody Staining:
- Aliquot approximately 1×10ⶠcells per sample tube
- Add optimal antibody dilution to experimental and positive control tubes
- Add isotype control to separate aliquots
- Incubate 30 minutes at 4°C in the dark
- Wash cells twice with flow cytometry buffer
- Resuspend in appropriate volume for analysis
Flow Cytometry Analysis:
- Establish instrument settings using unstained cells
- Analyze negative control cells first to establish background fluorescence
- Analyze positive control to confirm detection capability
- Finally analyze experimental samples
- Collect sufficient events for statistical analysis (typically 10,000 events per sample)
Interpretation Criteria:
- Positive control must demonstrate expected staining pattern and intensity
- Negative control should show minimal to no specific staining
- Experimental samples falling between these thresholds require further optimization
- Isotype control should match negative control staining profile [85]
Essential Research Reagent Solutions
The implementation of robust control strategies requires access to high-quality, well-characterized reagents. The following table summarizes essential materials and their functions in establishing effective controls:
Table 3: Essential Research Reagents for Control Implementation
| Reagent Category | Specific Examples | Primary Function | Technical Considerations |
|---|---|---|---|
| Validated Cell Lines | RAJI (Burkitt's lymphoma), JURKAT (T-cell lymphoma), HEK293T (transfection host) | Positive and negative controls for protein expression | Confirm endogenous expression status; verify authentication |
| Control Lysates & Extracts | Whole cell lysates, nuclear extracts, tissue homogenates | Loading controls; method specificity verification | Ensure protein integrity; confirm lot-to-lot reproducibility |
| Purified Proteins | Immunoglobulin standards, recombinant antigens, peptide fragments | Positive controls for immunoassays; standard curves | Verify purity; confirm structural integrity and functionality |
| Loading Control Antibodies | Anti-β-actin, anti-tubulin, anti-GAPDH | Normalization of protein loading in Western blot | Select different molecular weight than target protein |
| Low Endotoxin Reagents | Low endotoxin IgG, certified endotoxin-free water | Controls for biological assays; minimize background activation | Critical for cell culture applications; validate via LAL test |
| Authentication Standards | USP microbiological standards, ATCC reference strains | Method validation; regulatory compliance | Required for regulatory filings; ensure traceability |
Integration into Comprehensive Quality Systems
The strategic implementation of blanks, negative controls, and positive controls must be integrated within a holistic contamination control strategy that encompasses all aspects of the biomanufacturing process. As emphasized in current quality frameworks, this includes systematic assessment of risks from process inputs, raw materials, manufacturing environments, personnel, and utilities [1]. Modern Microbial Methods (MMMs)—including technologies based on intrinsic fluorescence, viability staining, flow cytometry, and PCR—can enhance detection capabilities when properly validated with appropriate controls [61]. These methods offer significant advantages over traditional approaches, including shorter time to detection, continuous monitoring capabilities, and enhanced sensitivity for detecting viable but non-culturable organisms [61].
A successful control strategy aligns with the principles of quality by design, incorporating controls during development stages rather than as retrospective additions. This proactive approach requires thorough understanding of potential failure modes and contamination sources, enabling the implementation of targeted controls at critical process points. Furthermore, the selection of control materials should reflect the intended application, with appropriate consideration of matrix effects, processing conditions, and analytical requirements. By embedding robust control methodologies throughout the development and manufacturing continuum, organizations can establish scientifically sound, defensible quality systems that reliably detect deviations, prevent contamination events, and ultimately ensure product safety and efficacy.
Validating Cleaning Protocols for Reusable vs. Disposable Tools
In sample preparation for drug development, the integrity of research data and safety of pharmaceutical products are paramount. Contamination from laboratory tools and equipment represents a significant risk, potentially compromising experimental results and leading to costly batch failures. The core challenge lies in implementing and validating cleaning protocols that reliably prevent cross-contamination, whether using reusable or disposable tools. Within shared research facilities, where products with different therapeutic properties and potencies are handled, the uncontrolled release of dust, residues on equipment, or contamination from personnel can pose a serious risk [86]. This guide provides a structured, technical framework for validating cleaning processes, ensuring that cleaning procedures are not just performed, but are scientifically demonstrated to be effective and reproducible, thereby safeguarding research outcomes and patient safety.
Contamination Risks: Reusable vs. Disposable Tools
Evidence of Contamination in Reusable Tools
Recent studies underscore the persistent contamination risks associated with reusable medical and research tools, even after cleaning procedures are followed.
- A 2025 microbiological analysis of reusable tourniquets found significant bacterial loads, with contamination levels varying by setting. The average bacterial count was 545 CFU/cm² in the emergency department and 101 CFU/cm² in the operating theatre, demonstrating that the environment of use significantly impacts contamination levels [87]. The study concluded that these devices, despite frequent use and contact with patients' skin, are often overlooked in infection control protocols, highlighting a critical gap in contamination prevention strategies [87].
- A multicenter study on reusable electroencephalography (EEG) electrodes revealed that, despite a standardized cleaning process involving scrubbing, soaking, and disinfection with a bleach-based product, 25% of cleaned electrodes (31 out of 124) had positive bacterial cultures [88]. Furthermore, epithelial cells were found on 60.5% of the electrodes, indicating that cleaning procedures were sufficient to remove blood but inadequate for ensuring optimally clean surfaces [88].
The Single-Use Alternative
Single-use, or disposable, devices are defined as those intended for use on one patient during a single procedure. They are not designed to be reprocessed (cleaned, disinfected, or sterilized) for use on another patient [89]. The U.S. Centers for Disease Control and Prevention (CDC) recommends using single-use devices for one patient only and then disposing of them appropriately [89]. Devices without reprocessing instructions should be considered single-use by default [89]. Such devices are often not heat-tolerant and cannot be reliably cleaned, making them a straightforward choice for eliminating the risk of cross-contamination via equipment. However, their environmental impact and life-cycle costs must be considered.
Table 1: Quantitative Comparison of Contamination Findings
| Device Studied | Setting | Key Contamination Findings | Implication for Sample Preparation |
|---|---|---|---|
| Reusable Tourniquets [87] | Emergency Department & Operating Theatre | Avg. 545 CFU/cm² (ED) and 101 CFU/cm² (OT) on surfaces. | Surface contamination is context-dependent and can be significant. |
| Reusable EEG Electrodes [88] | Four Hospital Epilepsy Units | 25% with bacterial growth; 60.5% with epithelial cells post-cleaning. | Cleaning protocols can be inadequate even when followed meticulously. |
Regulatory and Conceptual Framework for Cleaning Validation
Regulatory Foundations
The U.S. Food and Drug Administration (FDA) mandates that equipment used in the production, processing, or holding of drug products must be cleaned, maintained, and sanitized at appropriate intervals to prevent contamination that would alter the safety, identity, strength, quality, or purity of the product [23] [90]. The FDA's expectation is that cleaning procedures are validated, not just performed. Key requirements include:
- Written Procedures: Establishing detailed Standard Operating Procedures (SOPs) for equipment cleaning that address different scenarios (e.g., between batches of the same product vs. between different products) [23].
- Validation Protocols: Preparing specific, written validation protocols for each piece of equipment or manufacturing system before studies are performed. These must address sampling procedures and analytical methods [23].
- Data-Driven Reporting: A final, management-approved validation report that states whether the cleaning process is valid, supported by scientific data showing the system consistently meets pre-determined specifications [23].
Defining Cleaning Validation
Cleaning validation is the process of providing documented evidence that a cleaning procedure reproducibly removes residues, including Active Pharmaceutical Ingredients (APIs), chemical impurities, and microbes, to a pre-defined acceptable level, thereby preventing cross-contamination [90]. This is distinct from routine cleaning; it is a rigorous, documented scientific study that proves the cleaning process's effectiveness.
Designing a Cleaning Validation Protocol
Acceptance Criteria: Setting the Bar for Cleanliness
Establishing scientifically justified acceptance criteria is the cornerstone of any validation protocol. These criteria are typically multi-faceted.
Table 2: Cleaning Validation Acceptance Criteria
| Criterion Type | Standard Acceptance Limit | Rationale & Application |
|---|---|---|
| Physical | No visible residues on equipment under controlled lighting [90]. | A fundamental, qualitative assessment that must be passed before other tests. |
| Chemical | - ≤ 10 ppm of a product in another product.- ≤ 0.1% of the normal therapeutic dose in the maximum daily dose of another product [90]. | Prevents significant chemical carryover between product batches, protecting patient safety. |
| Microbial | - ≤ 20 CFU for bacterial counts.- ≤ 2 CFU for molds.- ≤ 25 CFU/25cm² in a sample [90]. | Controls bioburden, which is critical for non-sterile products and to ensure subsequent sterilization is effective. |
The FDA does not set universal acceptance specifications, acknowledging the wide variation in equipment and products. Instead, the firm's rationale for residue limits "should be logical based on the manufacturer's knowledge of the materials involved and be practical, achievable, and verifiable" [23].
Sampling Methods: How to Test for Residues
There are two generally accepted sampling methods for cleaning validation, each with distinct advantages.
- Direct Surface Sampling (Swab Method): This method involves using a sterile material to systematically rub a defined surface area. The swab is then extracted with a solvent and the solution is analyzed [90]. Its primary advantage is the ability to target worst-case, hard-to-clean areas (e.g., corners, crevices, blades) that might not be effectively assessed by rinse methods.
- Indirect Sampling (Rinse Method): This technique uses a solvent like water to rinse the cleaned equipment. The solvent is then collected and tested for traces of contaminants [90]. It is particularly useful for sampling large surface areas and complex systems with internal piping that are not easily accessible for swabbing.
Cleaning Methods
The choice of cleaning method depends on the equipment's design, nature of the residue, and facility capabilities. Common methods in pharmaceutical and research settings include:
- Clean-in-Place (CIP): Uses fixed spray devices and recirculation pumps to clean equipment without disassembly [90].
- Clean-out-of-Place (COP): Involves disassembling equipment and cleaning parts in automated cabinet or tunnel washers [90].
- Ultrasonic Washing: Effective for intricate parts by using cavitation to dislodge residues [90].
- Manual Cleaning: Often the most difficult to validate, it involves techniques like wiping, sink brushing, and equipment brushing. It requires highly detailed and controlled SOPs to ensure reproducibility [23] [90].
A Step-by-Step Experimental Protocol for Validation
The following protocol provides a detailed methodology for validating a cleaning process, incorporating elements from regulatory guidance and industry best practices [23] [90].
Phase 1: Pre-Validation Planning
- Define the Objective: State the purpose clearly: "To provide documented evidence that the [name of equipment] cleaning procedure using [method] effectively reduces [specific residue] to levels below established acceptance criteria."
- Establish a Validation Team: Appoint responsibilities to representatives from Quality Assurance, Production/Analytical Development, and Microbiology.
- Select the "Worst-Case" Scenario: Justify the choice of the most challenging residue to clean. A Worst Case Index (WCI) can be calculated based on factors like:
- Solubility: Residues with low solubility in the cleaning agent are harder to remove (e.g., a score of 1 for "practically insoluble") [90].
- Potency: Highly potent compounds require stricter limits.
- Equipment Geometry: Complex equipment with hard-to-reach areas presents a greater cleaning challenge.
- Develop the Validation Protocol: This formal document must be approved before execution and must specify:
- Equipment and surfaces to be sampled.
- The specific cleaning procedure to be validated.
- Sampling methods (swab and/or rinse) and locations.
- Analytical methods and their validation data (e.g., Specificity, Limit of Quantitation).
- Pre-defined acceptance criteria (see Table 2).
Phase 2: Execution and Data Collection
- Soil the Equipment: Apply a known quantity of the "worst-case" residue to predetermined, critical areas of the equipment.
- Execute the Cleaning Process: Perform the cleaning procedure exactly as defined in the SOP, documenting all critical parameters (e.g., time, temperature, cleaning agent concentration, flow rates).
- Sample the Equipment: After cleaning, collect samples from the pre-defined locations using the swab and/or rinse methods as per the protocol. Include both worst-case locations and representative surfaces.
- Analyze Samples: Analyze all samples for the target residues (chemical and microbial) using the validated analytical methods.
- Perform a Visual Inspection: Under controlled lighting, inspect the equipment for any visible residues. This is a pass/fail criterion that must be met.
- Compile and Analyze Data: Gather all data from the execution phase, including analytical results, executed batch records, and observation sheets.
- Prepare the Final Validation Report: The report must summarize the study, present all data, and provide a clear conclusion stating whether the cleaning process is validated (i.e., it met all pre-defined acceptance criteria).
- Manage Deviations: Any deviation from the protocol must be documented and its impact on the study assessed.
- Obtain Formal Approval: The report requires final approval by the Validation Team and Quality Assurance.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Cleaning Validation
| Item | Function & Rationale |
|---|---|
| Sterile Swabs | For direct surface sampling. Must be made of a material that does not interfere with the analysis (e.g., synthetic tip with plastic or metal shaft). |
| Recovery Solvent | A solvent used to extract residues from the swab. It must be capable of dissolving the target residue and be compatible with the analytical method (e.g., HPLC). |
| Validated Cleaning Agents | Detergents and disinfectants whose effectiveness and lack of interference have been scientifically demonstrated. Their residues must also be removable [23]. |
| Culture Media | Columbia agar blood medium or other appropriate media used for microbial analysis to determine bioburden (CFU) after cleaning [87]. |
| Reference Standards | Highly purified samples of the target residue (API, impurity) used to calibrate analytical instruments and quantify residue levels accurately. |
Revalidation and Ongoing Control
A cleaning process is not validated once and forgotten. A state of control must be maintained through periodic revalidation. Revalidation is required when there is a critical change that could impact cleaning effectiveness [90]. Key triggers include:
- A critical change in the equipment itself.
- A change in the cleaning process or cleaning agent.
- A change in the drug formulation or the introduction of a new product with higher potency or lower solubility.
- Based on a pre-defined schedule (e.g., annually).
- As indicated by the historical data from routine monitoring.
In the high-stakes environment of pharmaceutical research and drug development, preventing contamination is not a matter of chance but of scientifically rigorous proof. The choice between reusable and disposable tools involves a complex trade-off between contamination risk, environmental impact, and cost. For reusable equipment, a robust cleaning validation program—built on justified acceptance criteria, appropriate sampling methods, and a disciplined experimental protocol—provides the documented evidence required to ensure data integrity and product safety. By adhering to this structured framework, scientists and researchers can confidently mitigate the risk of cross-contamination, ensuring that their sample preparation supports the development of safe and effective medicines.
In research and drug development, the integrity of sample preparation is paramount. Contamination at this initial stage can compromise data, derail experiments, and invalidate months of work, with studies indicating that up to 75% of laboratory errors originate in the pre-analytical phase [15]. The choice of homogenizer probe—a fundamental tool in sample prep—is a critical decision point in safeguarding against these risks. Professionals are presented with three primary technologies: traditional stainless steel, modern disposable (single-use) probes, and innovative hybrid systems that aim to merge their benefits.
This analysis provides a technical evaluation of these probe types, framing the comparison within the essential context of contamination prevention. It synthesizes current data and protocols to guide researchers, scientists, and drug development professionals in making evidence-informed decisions that balance performance, cost, efficiency, and environmental impact.
Detailed Analysis of Probe Types
Stainless Steel Probes
Stainless steel probes are the durable, traditional workhorses of the laboratory. Crafted from materials like high-grade stainless steel or titanium, they are built to withstand repeated use, rigorous cleaning, and sterilization cycles, including autoclaving [15] [91].
- Contamination Risk Profile: The primary contamination risk for stainless steel probes is cross-contamination between samples due to improper or inadequate cleaning [15]. Residual analytes or biological material can adhere to the probe surface, leading to false positives or skewed results in subsequent experiments. As one scientist notes, "The risk of residual analytes affecting downstream results was always at the back of my mind" when using these probes [15].
- Mitigation Protocols: Mitigating this risk requires stringent and validated cleaning procedures. This often involves running a blank solution through the homogenizer after cleaning to verify the absence of residual contaminants [15]. These cleaning and validation processes are time-consuming and contribute significantly to the probe's total cost of ownership.
Disposable (Single-Use) Probes
Disposable probes, such as plastic Omni Tips, are designed for a single application and are then discarded [15]. They are typically made from advanced polymers and composites, arriving pre-sterilized and ready for use [92] [91].
- Contamination Risk Profile: Single-use probes offer the highest level of protection against cross-contamination. By eliminating the reuse of equipment, they "virtually eliminate the risk of cross-contamination" between samples [15]. This is particularly critical for sensitive assays, such as PCR, where trace contaminants like amplicons can severely impact results [15].
- Mitigation Protocols: The contamination mitigation protocol is inherent to the product's design: use a new, sterile probe for each sample. This eliminates the need for cleaning validation between samples, drastically reducing downtime and simplifying the workflow [15] [93].
Hybrid Probes
Hybrid probes represent an engineered compromise, designed to capture the advantages of both stainless steel and disposable systems. A common design involves a stainless steel outer shaft for durability, combined with disposable plastic internal components that contact the sample [15].
- Contamination Risk Profile: The contamination risk is significantly lowered compared to fully reusable systems. The parts of the probe most likely to retain sample residue are disposed of after each use, minimizing the potential for carryover.
- Mitigation Protocols: Cleaning is still required for the reusable external components, but the process is less intensive than for a full stainless steel probe. The disposable internals handle the primary contamination risk, streamlining the overall decontamination workflow [15].
Comparative Data and Decision Framework
To facilitate an objective comparison, the following tables summarize key quantitative and qualitative metrics across the three probe types.
Table 1: Quantitative Comparison of Probe Types
| Characteristic | Stainless Steel | Disposable | Hybrid |
|---|---|---|---|
| Initial Probe Cost | Higher | Lower | Moderate |
| Cost per Use (Long-Term) | Lower (high volume) | Higher | Moderate |
| Cleaning Time per Sample | High (30+ minutes) [15] | None | Low |
| Risk of Cross-Contamination | Higher (if cleaning fails) | Virtually Eliminated [15] | Low |
| Environmental Waste | Low | High [92] | Moderate |
| Durability with Tough Samples | Excellent | Limited [15] | Good |
Table 2: Qualitative Comparison and Best-Fit Applications
| Characteristic | Stainless Steel | Disposable | Hybrid |
|---|---|---|---|
| Tactile Feedback/Performance | Excellent, preferred for fine procedures [91] | Can lack rigidity and feedback [91] | Good |
| Operational Workflow | Slow turnaround between samples [15] | Fastest turnaround; high efficiency [15] [92] | Faster than stainless steel |
| Ideal Use Case | Low-volume labs; very tough, fibrous samples; where cost-per-use is critical | High-volume labs; sensitive assays (e.g., PCR, cell culture); multi-product facilities [15] [93] | Labs needing balance of durability and contamination control |
The following diagram synthesizes the key decision-making factors into a logical workflow to guide probe selection.
Experimental Protocols for Contamination Control
Implementing rigorous, documented protocols is non-negotiable for maintaining sample integrity. The following section outlines standard methodologies for working with different probe systems and validating their cleanliness.
Protocol 1: Sample Homogenization with Single-Use Probes
Objective: To homogenize a tissue sample using a disposable probe while preventing contamination and analyte loss.
- Preparation: Don appropriate personal protective equipment (PPE). Clean the work surface and homogenizer base with a disinfectant like 70% ethanol or a specialized solution (e.g., DNA Away for molecular biology work) [15].
- Setup: Select a new, sterile disposable probe from its packaging. Attach it securely to the handheld homogenizer drive unit according to the manufacturer's instructions.
- Homogenization: Place the sample tube in a stable holder. Immerse the probe into the sample buffer and initiate homogenization using predetermined parameters (e.g., speed, duration, pulsation).
- Disposal: Carefully remove the probe, ensuring any droplets fall back into the tube. Detach the probe and dispose of it according to laboratory biohazard waste protocols [92].
- Post-Processing: Centrifuge the homogenate if required (e.g., to pellet debris). Proceed with downstream analysis.
Protocol 2: Cleaning and Sterilization of Stainless Steel Probes
Objective: To thoroughly clean and sterilize a reusable stainless steel probe to prevent cross-contamination between samples.
- Initial Rinse: Immediately after use, rinse the probe with deionized water to remove gross sample material.
- Detergent Cleaning: Immerse and scrub the probe in a warm, mild laboratory detergent solution. Use a soft brush to clean intricate parts.
- Rinse: Perform a thorough rinsing with copious amounts of purified water to remove all detergent residues.
- Sterilization: Sterilize the probe using an autoclave (e.g., 121°C for 20 minutes) or by immersing in a suitable chemical sterilant, followed by a rinse with sterile water or ethanol to remove sterilant residue [92] [91].
- Storage: Allow the probe to dry completely in a clean, dust-free environment before storage.
Protocol 3: Validation of Cleaning Efficacy
Objective: To verify that a cleaned reusable probe is free of contaminating residues that could affect subsequent experiments.
- Blank Run (Control): After cleaning and sterilizing the probe, homogenize a blank solution (the typical sample buffer without the analyte) using the standard protocol [15].
- Analysis: Subject this blank homogenate to the same downstream analysis as your actual samples (e.g., PCR, chromatography, spectrometry).
- Interpretation: A negative result in the blank confirms the efficacy of the cleaning protocol. A positive signal indicates residual contamination, necessitating a review and improvement of the cleaning procedure.
The Scientist's Toolkit: Essential Reagents for Contamination Control
The following table details key reagents and materials used in sample preparation and contamination prevention, as referenced in the experimental protocols.
Table 3: Research Reagent Solutions for Contamination Control
| Reagent/Material | Function in Contamination Control |
|---|---|
| 70% Ethanol | A widely used disinfectant for cleaning laboratory surfaces, instrument exteriors, and non-critical items to reduce microbial load [15]. |
| DNA Away (or equivalent) | A specialized decontamination solution designed to degrade and remove residual DNA from lab surfaces and equipment, crucial for PCR and other molecular biology techniques [15]. |
| Laboratory Detergents | Used for the manual cleaning of reusable tools like stainless steel probes to remove proteins, lipids, and other biological residues [15]. |
| Pre-sterilized Disposable Probes | Single-use homogenizer tips that eliminate the risk of cross-contamination by providing a new, sterile fluid path for every sample [15]. |
| Blank Solution (Buffer) | Used in validation protocols to test for the presence of residual contaminants on cleaned equipment or in reagents after cleaning procedures [15]. |
| Bleach (5-10% Solution) | A powerful chemical sterilant and disinfectant used to decontaminate surfaces and, in some cases, equipment, though it can be corrosive [15]. |
The choice between stainless steel, disposable, and hybrid homogenizer probes is a strategic one with significant implications for data integrity, operational efficiency, and cost. There is no universal solution; the optimal choice is dictated by specific research priorities.
- Stainless steel probes offer durability and a low cost-per-use for high-volume processing of tough samples but demand rigorous cleaning protocols to mitigate a higher inherent risk of cross-contamination.
- Disposable probes provide the highest guarantee against cross-contamination and maximize workflow speed, making them ideal for sensitive assays and multi-product facilities, though they incur recurring costs and generate more waste.
- Hybrid probes present a balanced alternative, reducing contamination risk and cleaning time while maintaining robustness for challenging samples.
A practical, forward-looking approach for many labs may be a hybrid strategy within the laboratory itself: reserving disposable probes for highly sensitive or critical experiments, and employing stainless steel or hybrid systems for less sensitive, high-volume work. This balanced approach allows researchers to uphold the highest standards of sample integrity while managing economic and environmental impacts effectively.
Leveraging Enzymatic Decontamination like Uracil-N-Glycosylase (UNG) in qPCR
In the realm of quantitative polymerase chain reaction (qPCR) research, the extreme sensitivity of the technique is a double-edged sword. While it enables the detection of minute amounts of nucleic acids, this very sensitivity makes experiments vulnerable to contamination, particularly from amplification products of previous PCRs, a phenomenon known as carry-over contamination [94] [16]. Such contamination is a pervasive source of false-positive results, compromising data integrity and potentially derailing scientific conclusions [95]. Within a robust sample preparation framework, physical separation of workspaces and meticulous laboratory practices are fundamental first lines of defense [16] [57]. However, these measures alone cannot address contamination that has already been introduced into reaction components. This is where enzymatic decontamination strategies, specifically the use of uracil-N-glycosylase (UNG), provide a powerful biochemical solution integrated directly into the qPCR reaction itself [94] [96].
The UNG method is an elegant enzymatic strategy designed to selectively degrade contaminating DNA from past amplifications before they can be copied in the current qPCR run [95]. For practical purposes in qPCR, the terms UNG and uracil-DNA glycosylase (UDG) are often used interchangeably, as they perform the same core function. Technically, UNG refers to Family I of the broader UDG enzyme superfamily [94]. This guide will delve into the mechanism, implementation, and practical considerations of leveraging UNG to safeguard your qPCR results, providing a critical layer of quality control in sample preparation research.
The Mechanism of Action of UNG/UDG
Biochemical Principle
Uracil-N-glycosylase (UNG) is a DNA repair enzyme that initiates the base excision repair pathway. Its biological function is to excise uracil bases that have been misincorporated into DNA, a lesion that can arise from the deamination of cytosine [94] [97]. The enzyme catalyzes the hydrolysis of the N-glycosylic bond between the uracil base and the deoxyribose sugar in the DNA backbone [94]. This reaction results in the release of free uracil and creates an apyrimidinic (AP) site within the DNA strand. These AP sites are alkali-labile and are readily cleaved under the elevated temperature and pH conditions of the PCR initial heating step, leading to the fragmentation of the DNA strand [94] [95]. Crucially, this cleavage prevents DNA polymerases from elongating beyond the damaged site, thereby blocking the amplification of the contaminated template.
Application in qPCR Workflow
The application of UNG in qPCR involves a two-step process that seamlessly integrates into a standard amplification protocol, as illustrated in the workflow below.
The strategic power of this method lies in its selectivity. UNG specifically targets DNA containing uracil. It does not affect natural DNA containing thymine, the dUTP nucleotide itself, or other reaction components like Taq polymerase [94]. Furthermore, the enzyme is fully inactivated during the initial high-temperature denaturation step of the PCR cycle, ensuring it does not degrade the newly synthesized uracil-containing products of the current amplification reaction [16] [98].
UNG in Next-Generation Sequencing (NGS) for FFPE Samples
The Problem of Artifactual Mutations
The utility of enzymatic decontamination extends beyond routine qPCR into sophisticated areas like next-generation sequencing (NGS), particularly when working with challenging sample types such as formalin-fixed paraffin-embedded (FFPE) tissues [99]. DNA extracted from FFPE tissues is notoriously degraded and damaged. A major type of damage is the hydrolytic deamination of cytosine to uracil and of 5-methylcytosine to thymine [99]. During subsequent PCR amplification in the NGS workflow, DNA polymerase reads these uracil bases as thymine and incorporates adenine opposite them. This process leads to C:G > T:A artifactual transitions in the sequencing data, which can be misinterpreted as false positive somatic mutations—a critical problem in precision oncology where accurate variant calling is essential for therapeutic decisions [99].
UDG Treatment as a Solution
Pretreating FFPE DNA with UDG (UNG) before multiplex PCR and library construction has been demonstrated as an effective solution to this problem. The enzyme excises the uracil bases resulting from cytosine deamination, preventing the C:G > T:A artifacts from being fixed in the amplified sequencing library [99]. A 2019 study in Applied Cancer Research systematically evaluated this approach and yielded compelling quantitative data on its efficacy, summarized in the table below.
Table 1: Quantitative Reduction of Sequencing Artifacts with UDG Treatment in FFPE Samples [99]
| Metric | Untreated Samples (Mean) | UDG-Treated Samples (Mean) | Percentage Reduction | p-value |
|---|---|---|---|---|
| Total Number of Variants | 82 | 12 | 85% | Not specified |
| Number of Transitions | 157.7 | 18.8 | 88% | < 0.0007 |
| Number of Transversions | Not specified | Not specified | 5.5% (not consistent) | 0.3774 (not significant) |
| Transition/Transversion (Ts/Tv) Ratio | High | Low | 75% | < 0.0007 |
| Mean Variant Allele Frequency (VAF) | 10.5% | 36.0% | Not applicable | < 0.0001 |
The data shows that UDG treatment causes a dramatic and statistically significant reduction in transition mutations, which are the hallmark of cytosine deamination, without consistently affecting transversion mutations. Furthermore, the significant increase in the mean Variant Allele Frequency (VAF) after treatment indicates that the removed variants were predominantly low-frequency artifacts, thereby enriching the data for true, clonal mutations [99]. The following workflow diagram outlines the key steps in incorporating UDG treatment into an NGS protocol for FFPE samples.
Experimental Protocols and Methodologies
Protocol for qPCR Carryover Contamination Control
Implementing UNG in qPCR requires minor modifications to a standard protocol. The following is a detailed methodology based on established practices [94] [96].
- Step 1: Reaction Assembly with dUTP. Prepare the master mix as usual, but substitute dTTP with a dNTP mix that contains dUTP. Research indicates that a mixture of dUTP and a small amount of dTTP (e.g., 175 µM dUTP and 25 µM dTTP) can ensure robust amplification while still allowing effective decontamination [96]. Include 0.5-1.0 unit of UNG enzyme per reaction. Assemble all other components, including primers, buffer, and template DNA.
- Step 2: UNG Incubation. After assembling the reaction but before starting the thermocycling program, incorporate an incubation step at 50°C for 2 minutes [94]. During this step, UNG is active and will scan the reaction mix, excising uracil bases from any contaminating PCR products from previous runs.
- Step 3: Enzyme Inactivation and Amplification. Initiate the standard thermocycling program. The initial denaturation step at 95°C serves two purposes: it denatures the template DNA and simultaneously irreversibly inactivates the UNG enzyme [94] [16]. This prevents it from degrading the new uracil-containing amplicons synthesized during the current PCR. Proceed with the remaining cycles as normal.
Protocol for UDG Treatment of FFPE DNA for NGS
For reducing sequencing artifacts in FFPE-derived DNA, the treatment occurs prior to the library amplification step [99].
- Step 1: Sample Preparation. Extract genomic DNA from FFPE tumor tissues using a dedicated kit (e.g., QIAamp DNA FFPE Tissue Kit). Quantify the DNA using a fluorometric method (e.g., Qubit dsDNA HS Assay).
- Step 2: Enzymatic Treatment. For a 15 µL reaction containing 10-15 ng of FFPE DNA, add 0.5 µL (1 unit/µL) of a commercial UDG enzyme [99]. Incubate the reaction at 37°C for 30 minutes.
- Step 3: Enzyme Inactivation. Heat the reaction to 95°C for 5 minutes to completely inactivate the UDG enzyme [99].
- Step 4: Library Construction and Sequencing. Use the treated DNA for the subsequent multiplex PCR and NGS library preparation steps according to the chosen protocol (e.g., using an Ion AmpliSeq Library Kit). Sequence the libraries and analyze the data, comparing the results to an untreated control to assess the reduction in artifactual variants.
Practical Considerations and Limitations
While UNG/UDG is a powerful tool, researchers must be aware of its specific limitations and application requirements to use it effectively.
Table 2: Research Reagent Solutions for UNG/UDG-Based Decontamination
| Reagent / Solution | Function in Protocol | Key Considerations |
|---|---|---|
| UNG/UDG Enzyme | Catalyzes the hydrolysis of uracil-containing DNA to prevent amplification of contaminants. | Heat-labile versions from Atlantic cod are available for one-step RT-PCR. E. coli UNG is not fully inactivated and can degrade products over time [94]. |
| dUTP Nucleotide | Incorporated into PCR amplicons in place of dTTP, making them susceptible to future UNG degradation. | For optimal amplification efficiency, use a mixture of dUTP and a small amount of dTTP (e.g., 175µM dUTP + 25µM dTTP) [96]. |
| Master Mix with UNG/dUTP | A pre-formulated solution containing polymerase, buffer, dNTPs (including dUTP), and UNG enzyme. | Simplifies workflow and ensures component compatibility. Check manufacturer's specifications for incubation times and temperatures [94] [98]. |
| No Template Control (NTC) | A quality control reaction containing all components except the DNA template. | Essential for monitoring contamination; amplification in NTC indicates potential contamination of reagents [16] [98]. |
- When to Avoid UNG: UNG is not suitable for all applications. It should not be used in experiments where the amplicon itself is the desired product for downstream applications like cloning if there will be a significant delay before use, as residual enzyme activity could degrade the product [94]. It is also not recommended for one-step RT-PCR with E. coli UNG, as the enzyme will degrade the dU-containing cDNA synthesized during reverse transcription. The solution is to either perform two-step RT-PCR or use a heat-labile UNG [94]. Furthermore, UNG will degrade the template in nested PCR if the first-round products contain dUTP and should not be used with bisulfite-treated DNA, as bisulfite conversion creates uracil residues from unmethylated cytosines [94].
- Primer and Template Design: For UNG to efficiently degrade primer-dimers, primers should contain dA-nucleotides near their 3' ends [94]. The sequence being amplified should ideally be rich in dA and dT nucleotides to ensure sufficient dU incorporation for subsequent degradation [94].
Incorporating uracil-N-glycosylase (UNG) into the qPCR workflow provides a robust, enzymatic barrier against one of the most common sources of false-positive results: carryover contamination from previous amplifications. Its utility further extends to improving the accuracy of NGS from FFPE samples by dramatically reducing artifactual C:G > T:A transitions. When combined with rigorous laboratory practices—including physical separation of pre- and post-amplification areas, use of dedicated equipment and protective gear, and diligent cleaning with reagents like bleach and ethanol—UNG decontamination forms an integral component of a comprehensive contamination prevention strategy [16] [100] [57]. By understanding its mechanism, adhering to validated protocols, and acknowledging its limitations, researchers and drug development professionals can leverage UNG to significantly enhance the reliability and integrity of their molecular data.
In the pursuit of scientific discovery, preventing contamination during sample preparation is not merely a technical task—it is a fundamental requirement for ensuring data integrity. A robust framework of documentation and Standard Operating Procedures (SOPs) transforms this requirement into a sustainable practice, safeguarding research from pre-analytical errors that can compromise up to 75% of laboratory results [15]. This guide details how to build this framework, ensuring your work is both reproducible and ready for rigorous audit.
The Critical Link: Documentation, SOPs, and Contamination Control
A Contamination Control Strategy (CCS) is a systematic, risk-based approach to identifying, assessing, and mitigating contamination risks across the entire product or research lifecycle [101] [102]. Within this strategy, SOPs and documentation serve as the critical bridge between theory and practice. They provide the definitive "how-to" for contamination prevention, ensure consistent execution across different personnel and time, and create a verifiable record for troubleshooting and audits.
The terms repeatability and reproducibility are key metrics for quality. Repeatability refers to obtaining the same results when the same experiment is performed under identical conditions (same team, same setup). Reproducibility is the ability of a different research team, using the same methods, to attain the same results from a published paper [103]. Comprehensive SOPs are the foundation for achieving both, providing the detailed methodology that allows others to replicate your work faithfully.
Core Elements of Effective SOPs for Sample Preparation
Effective SOPs transform best practices into actionable, unambiguous instructions. The following elements are crucial for SOPs focused on contamination-prone sample preparation processes.
Essential SOP Components
A well-structured SOP must clearly define its purpose, scope (personnel, processes, and equipment covered), and detailed, step-by-step procedures. It should list all required materials and reagents, including quality specifications (e.g., DNA-free). Furthermore, it must outline safety precautions and specify all documentation and records to be maintained [104].
Key Protocols for Contamination Prevention
- Personal Protective Equipment (PPE) and Aseptic Technique: SOPs must mandate proper gowning and the use of gloves, lab coats, and masks. Crucially, they should state that disposable gloves are not reused and are changed when moving between samples or after touching potentially contaminated surfaces [105] [4].
- Equipment Cleaning and Sterilization: SOPs must define rigorous cleaning schedules, methods, and documentation. For example, an SOP for a handheld homogenizer probe would specify that a stainless-steel probe must be cleaned and then validated with a blank solution to ensure no residual analytes are present before the next use [15]. Protocols should specify the use of DNA-degrading solutions like bleach or commercial products for surfaces and equipment when working with sensitive assays [4].
- Use of Controlled Environments: SOPs for laminar flow hoods or cleanrooms should include steps for regular performance checks, such as ensuring HEPA filters are functional and the work surface is properly sterilized with UV light and disinfectants before and after use [105] [104].
- Management of Research Reagents: The quality of water and reagents is a frequent source of contamination. SOPs must require that reagents are verified for purity and that water purification systems are regularly serviced. Testing water with culture media or an electroconductive meter can be specified as a control measure [105].
The diagram below illustrates the interconnected lifecycle of how SOPs and documentation directly support contamination control and lead to reliable outcomes.
Research Reagent and Material Solutions
The following table details essential items for preventing contamination during sample preparation, particularly in sensitive microbiome studies [106] [4].
| Item | Function in Contamination Control |
|---|---|
| Single-Use, DNA-Free Consumables (e.g., swabs, tubes) | Prevents introduction of contaminating DNA from reusable equipment; ensures sterile starting point for sample collection [4]. |
| Nucleic Acid Degrading Solutions (e.g., bleach, DNA Away) | Removes persistent cell-free DNA from surfaces and equipment that autoclaving or ethanol alone may not eliminate [15] [4]. |
| Disposable Homogenizer Probes (e.g., Omni Tip) | Virtually eliminates cross-contamination between samples during the homogenization step, a high-risk process [15]. |
| Personal Protective Equipment (PPE) (gloves, masks, coveralls) | Acts as a barrier to contamination from human operators, including skin cells, hair, and aerosol droplets [105] [4]. |
| Automated Liquid Handling Systems | Reduces human error and cross-contamination via enclosed, HEPA-filtered hoods and precise, touch-free liquid transfers [105]. |
Implementing a Documentation System for Audit-Readiness
Beyond SOPs, a comprehensive documentation system captures the entire story of an experiment, making it transparent and verifiable.
The Chain of Custody
A complete Chain of Custody is essential for tracking biosamples. It logs every action performed on a sample, who performed it, and when. This is critical for tracing the history of a sample and identifying the source of any potential contamination [107]. A Laboratory Information Management System (LIMS) is often used to automate this tracking, recording sample check-in/check-out, location changes, and the creation of sub-samples or aliquots [107].
Environmental and Process Monitoring Records
Maintaining records of environmental conditions is a key part of a CCS [101] [102]. This includes data from continuous monitoring of critical parameters like:
- Differential pressure in cleanrooms
- Particulate levels in air
- Temperature for storage units and incubators These records provide objective evidence that the controlled environment was maintained within specified limits throughout the experimental process.
The Role of Controls and Their Documentation
Including and meticulously documenting controls is arguably the most important practice for validating results, especially in low-biomass studies [4]. Records must detail the type of control used and its result.
- Negative Controls: Exposed to all the same reagents and environments as the actual sample but without the sample material itself. They are critical for identifying reagent or process-derived contamination [4].
- Positive Controls: Samples with known target analytes, used to confirm that the entire experimental process worked as expected.
Validation and Continuous Improvement
An effective CCS is not static. SOPs and practices must be regularly validated and improved based on data.
Audits and Gap Analysis
Conducting regular and surprise audits ensures ongoing adherence to protocols [101]. A systematic gap analysis against standards (e.g., EU GMP Annex 1) helps identify weaknesses in the contamination control strategy and prioritizes improvements [101].
Investigating Deviations
When contamination occurs or a process fails, a thorough investigation guided by a formal deviation SOP is necessary. This involves root cause analysis to determine if the cause was a failure to follow an SOP or a weakness in the SOP itself, leading to targeted corrective and preventive actions (CAPAs) [102].
The workflow below outlines the major control points in a sample preparation process, from collection to storage, highlighting where specific controls and documentation are critical.
In the context of contamination prevention, documentation and SOPs are the backbone of scientific rigor. They provide the structure to systematically minimize risks, the evidence to prove data integrity, and the foundation for continuous improvement. By implementing a living Contamination Control Strategy grounded in detailed, followed, and meticulously recorded procedures, researchers and drug development professionals can confidently produce data that is not only reliable and reproducible but also fully prepared to withstand the scrutiny of any audit.
Conclusion
Preventing contamination during sample preparation is not a single action but a holistic, disciplined approach integrated into every stage of the research workflow. By understanding contamination sources, implementing rigorous methodologies, adeptly troubleshooting issues, and validating processes with appropriate controls, scientists can protect the integrity of their most valuable asset: their samples. Adopting these practices is fundamental for generating trustworthy, reproducible data that accelerates drug development, validates clinical findings, and upholds the highest standards of scientific research. Future directions will likely see greater integration of automation and smart lab design to further minimize human-dependent error, pushing the boundaries of sensitivity and reliability in biomedical science.
References
- 1. Comprehensive Microbial Control Strategy [https://www.bioprocessintl.com/qa-qc/beyond-traditional-microbiology-testing-developing-a-comprehensive-strategy-for-microbial-control-and-detection]
- 2. Contamination Detection in Pharma Products Market 2025 ... [https://www.towardshealthcare.com/insights/contamination-detection-in-pharma-products-market-sizing]
- 3. Contamination Detection in Pharmaceutical Products Market [https://www.globenewswire.com/news-release/2025/10/30/3177319/0/en/Contamination-Detection-in-Pharmaceutical-Products-Market-In-Depth-Insights-from-Towards-Healthcare.html]
- 4. Guidelines for preventing and reporting contamination in ... [https://www.nature.com/articles/s41564-025-02035-2]
- 5. Unlocking Data Integrity: How Historical Data Review ... [https://www.envstd.com/unlocking-data-integrity-september-2025/]
- 6. A Comprehensive Survey of Contamination Detection ... [https://arxiv.org/html/2404.00699v4]
- 7. Contamination Control Strategies [https://www.ecolab.com/articles/2025/04/contamination-control-strategies]
- 8. Assessing Environmental Risks during the Drug Development ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11019539/]
- 9. Environmental impacts of drugs against parasitic vector-borne ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11555358/]
- 10. New Sample Preparation Products and Accessories for ... [https://www.chromatographyonline.com/view/new-sample-preparation-products-and-accessories-for-2024-2025]
- 11. A comprehensive performance evaluation, comparison ... [https://www.sciencedirect.com/science/article/pii/S1532046424000431]
- 12. Pre-analytical phase errors constitute the vast majority of ... [https://pubmed.ncbi.nlm.nih.gov/40311145/]
- 13. Application Effectiveness of a Pre-Analytical Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11927499/]
- 14. Preparation for blood tests: what can go wrong before the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377977/]
- 15. How to Reduce Sample Contamination [https://blog.omni-inc.com/blog/how-to-reduce-sample-contamination]
- 16. Avoiding Contamination | Thermo Fisher Scientific - ES [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/good-laboratory-practice-avoid-contamination-qpcr-experiments.html]
- 17. The importance of the pre-pre-analytical phase | LabLeaders [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/importance-pre-pre-analytical-phase.html]
- 18. Contamination in Low Microbial Biomass Microbiome Studies: Issues and Recommendations - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0966842X18302531]
- 19. Contamination in Low Microbial Biomass Microbiome Studies: Issues and Recommendations - PubMed [https://pubmed.ncbi.nlm.nih.gov/30497919/]
- 20. Planning and analyzing a low-biomass microbiome study [https://pmc.ncbi.nlm.nih.gov/articles/PMC12445924/]
- 21. Laboratory contamination over time during low-biomass sample analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/30887686/]
- 22. Cleaning validation in pharmaceutical quality control ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229404/]
- 23. Validation of Cleaning Processes (7/93) [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/inspection-guides/validation-cleaning-processes-793]
- 24. Preventing PCR Amplification Carryover Contamination in ... [https://www.annclinlabsci.org/content/34/4/389.long]
- 25. Biological Safety Cabinets and Laminar Flow Cabinets [https://ba.auburn.edu/rms/laboratory-safety/biological-safety/biological-safety-cabinets-and-laminar-flow-cabinets/]
- 26. Fume Hood vs. Biosafety Cabinet: What to Use & When [https://www.nuaire.com/en/resources/fume-hood-vs-biosafety-cabinet]
- 27. Biological Safety Cabinet, Fume Hood or Laminar Airflow ... [https://www.discoveryscientificsolutions.com/item/44]
- 28. Biological safety cabinet vs fume hood: Quick comparison [https://labs-usa.com/2025/11/04/biological-safety-cabinet-vs-fume-hood/amp/]
- 29. Surface materials and cleaning efficacy in healthcare [https://www.sciencedirect.com/science/article/abs/pii/S0360132325006596]
- 30. Bacterial DNA Contamination of Commercial PCR Enzymes [https://www.mdpi.com/2076-2607/13/4/732]
- 31. Systematic review of surface disinfection: Spraying versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12104846/]
- 32. Evaluation of Different Cleaning Strategies for Removal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8775027/]
- 33. Managing Cleaning Validation in Multi-Product Biologics ... [https://www.biopharminternational.com/view/managing-cleaning-validation-multi-product-biologics-facilities]
- 34. Pharma Decontamination Safety Guide 2025 - QUALIA [https://qualia-bio.com/blog/pharma-decontamination-safety-guide-2025/]
- 35. Degraded DNA Analysis Techniques: Purification, ... [https://www.sepscience.com/degraded-dna-analysis-techniques-purification-characterization-and-forensic-workflows-12020]
- 36. Chapter 4 Aseptic Technique - Nursing Skills - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK593203/]
- 37. What Is Aseptic Technique? 2025 Guide to Infection Control [https://learntastic.com/blog/what-is-aseptic-technique]
- 38. New AABB Publication Offers Practical Insights on Aseptic ... [https://www.aabb.org/news-resources/news/article/2025/07/16/new-aabb-publication-offers-practical-insights-on-aseptic-technique-for-laboratory-professionals]
- 39. A framework for personal protective equipment use in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12310650/]
- 40. Aseptic Technique: What It Is & What To Know [https://my.clevelandclinic.org/health/treatments/aseptic-technique]
- 41. Personal Protective Equipment for Infection Control [https://www.fda.gov/medical-devices/general-hospital-devices-and-supplies/personal-protective-equipment-infection-control]
- 42. Article Release: Why an Automated Contamination Control ... [https://ntint.com/news/why-an-automated-contamination-control-program-is-a-must-for-pharmaceutical-product-safety/]
- 43. Managing Human Error in Pharma Contamination Control [https://www.pharmanow.live/hr-in-pharma/human-factors-contamination-control]
- 44. Automating Aseptic Processing Reduces Contamination Risk [https://www.pharmtech.com/view/automating-aseptic-processing-reduces-contamination-risk]
- 45. Three steps to contamination control when utilising single ... [https://www.a3p.org/en/contamination-control-single-use/]
- 46. Sterilization Trends for Single-Use Consumables [https://www.biopharminternational.com/view/sterilization-trends-for-single-use-consumables]
- 47. Guide to Irradiation and Sterilization Validation of Single- ... [https://www.bioprocessintl.com/single-use/guide-to-irradiation-and-sterilization-validation-of-single-use-bioprocess-systems]
- 48. Contamination Control During Sample Preparation for ... [https://www.spectroscopyonline.com/view/contamination-control-during-sample-preparation-for-trace-element-analysis-of-electronic-cigarette-aerosol-with-inductively-coupled-plasma-mass-spectrometry-part-1]
- 49. Single-Use Consumables Market Size 2024 to 2034 [https://www.towardshealthcare.com/insights/single-use-consumables-market-sizing]
- 50. Environmental Controls for Sample Integrity [https://www.labmanager.com/environmental-controls-for-sample-integrity-34507]
- 51. Preventing Contamination in Pipetting [https://www.labmanager.com/preventing-contamination-in-pipetting-5195]
- 52. Preventing cross-contamination [https://www.thermofisher.com/us/en/home/life-science/lab-plasticware-supplies/lab-plasticware-supplies-learning-center/lab-plasticware-supplies-resource-library/fundamentals-of-pipetting/proper-pipetting-techniques/preventing-cross-contamination.html]
- 53. Amplification of the No Template Control (NTC) [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/real-time-pcr-troubleshooting-tool/gene-expression-quantitation-troubleshooting/amplification-no-template-control.html]
- 54. The Key to Strong Oncology LDT Validation? Start with ... [https://www.referencemedicine.com/blog/the-key-to-strong-oncology-ldt-validation-start-with-the-right-samples]
- 55. Development of real-time PCR methods for quality control ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1572201/full]
- 56. 6 Ways to Minimize Contamination during PCR [https://www.labclinics.com/2019/07/22/six-ways-to-minimize-contamination-during-pcr/?lang=en]
- 57. How to Avoid Contamination in Your qPCR Experiments [https://rheniumbio.co.il/how-to-avoid-contamination-in-your-qpcr-experiments/]
- 58. How to Avoid Contamination in Lab Samples [https://www.aurorabiomed.com/how-to-avoid-contamination-in-lab-samples/?srsltid=AfmBOoqSHwiznWEUpV9QLsZxR2sOw-2rhJpZW5g-pnxpb6m1LHbR5Jsa]
- 59. Microbial source tracking and identification of fecal ... [https://pubmed.ncbi.nlm.nih.gov/39366578/]
- 60. Microbial source tracking identifies ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2023.1111297/full]
- 61. Modern Microbial Methods Supporting a Contamination ... [https://www.pda.org/pda-letter-portal/home/full-article/modern-microbial-methods-support-of-a-contamination-control-strategy]
- 62. Basic Overview of Contamination Control in GMP Facility [https://www.gmpsop.com/basic-overview-of-contamination-control-in-gmp-facility/]
- 63. Chemical Disinfectants | Infection Control [https://www.cdc.gov/infection-control/hcp/disinfection-sterilization/chemical-disinfectants.html]
- 64. Antimicrobial biocides in the healthcare environment: efficacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1661639/]
- 65. Lab Efficiency: Integrating Fume Hoods for Safety [https://usa.erlab.com/integrating-ducted-filtered-ductless-fume-hoods-total-lab-efficiency-safety/]
- 66. The Case for Ductless Fume Hoods [https://aircleansystems.com/news/maximizing-laboratory-safety-and-efficiency]
- 67. Cleaning validation protocol for pharmaceutical industry [https://www.gmpsop.com/cleaning-validation-protocol/]
- 68. Cleaning Validation Guidelines 2025 [https://www.leucine.io/cleaning-validation-blogs/cleaning-validation-guidelines]
- 69. Preventing Microorganism Contamination in Starting Active ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12298561/]
- 70. 2025 Cleaning Validation Guide [https://contractorplus.app/blog/cleaning-validation]
- 71. Cleaning Methodology and Validation Best Practices [https://www.gxpcellators.com/cleaning-methodology-and-validation-best-practices-document/]
- 72. Reusable Device Validations [https://pacificbiolabs.com/reusable-device-validations/]
- 73. How are Surgical Instruments Cleaned and Disinfected? [https://www.steris.com/healthcare/knowledge-center/infection-prevention/cleaning-and-disinfecting-surgical-instruments]
- 74. Validations for Reusable Hospital-Made or Clinical-Trial ... [https://www.nelsonlabs.com/understanding-reprocessing-validations-for-reusable-medical-devices-made-by-hospitals-or-used-for-clinical-trials/]
- 75. 7 Signs Your Tap Water Might Be Contaminated [https://www.benchmarkenvironmental.com/7-signs-tap-water-contaminated/]
- 76. Sources of Contamination in HVAC Systems [https://nadca.com/blog/sources-contamination-hvac-systems]
- 77. Methods of Environmental Monitoring: Water vs. Air Sampling [https://millstonemedical.com/methods-of-environmental-monitoring-water-vs-air-sampling/]
- 78. How to Avoid Contamination in Lab Samples [https://www.aurorabiomed.com/how-to-avoid-contamination-in-lab-samples/?srsltid=AfmBOopCdocpb0FE8oi3nH9l4I5AILpYfD-zoFsyM3NR5-h2Y_glfpDe]
- 79. F. Environmental Sampling | Infection Control [https://www.cdc.gov/infection-control/hcp/environmental-control/environmental-sampling.html]
- 80. Mechanisms, Techniques and Devices of Airborne Virus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10138381/]
- 81. Pathogen Mitigation Technologies in HVAC Air Filtration - XRAY [https://xray.greyb.com/hvac/pathogen-mitigation-air-filtration]
- 82. Positive and Negative Controls [https://www.rockland.com/resources/positive-and-negative-controls/?srsltid=AfmBOor7-fJjRBTYd8_uPwOmnEll8YMGXTIStP14vK9KfDt9bReWBJ8N]
- 83. What are Positive and Negative Controls? [https://scienceready.com.au/pages/positive-and-negative-controls?srsltid=AfmBOorY-LtDTn4X2i2tWRWNEI8nQ6ON9PMmYgv6hcOezAPjYgKhAD9X]
- 84. The Vital Role of Blanks in Sample Preparation [https://www.chromatographyonline.com/view/vital-role-blanks-sample-preparation]
- 85. Positive and negative controls for antibody validation [https://www.euromabnet.com/guidelines/positive-negative-controls.php]
- 86. Cross-contamination Risk Assessment using FMEA tool [https://jddtonline.info/index.php/jddt/article/view/6765]
- 87. Reusable Tourniquets as Potential Transmitters of Infection [https://pubmed.ncbi.nlm.nih.gov/39858920/]
- 88. Study Examines Contamination of Reusable EEG Equipment [https://consultqd.clevelandclinic.org/study-examines-contamination-of-reusable-eeg-equipment]
- 89. Best Practices for Single-Use (Disposable) Devices [https://www.cdc.gov/dental-infection-control/hcp/dental-ipc-faqs/single-use-devices.html]
- 90. Cleaning Validation: Protocol & Guidelines [https://safetyculture.com/topics/cleaning-validation]
- 91. The Right Choice: Disposable vs. Reusable Surgical ... [https://lenoxsurgical.com/Blogs/33_the-right-choice-disposable-vs-reusable-surgical-instruments.html]
- 92. Single-Use Surgical Instruments: Pros, Cons, and Future ... [https://beauty-teck.com/blog/single-use-surgical-instruments-pros-cons-and-future-trends]
- 93. Why Single-Use Bioreactors Are Revolutionizing Cell ... [https://cellculturecompany.com/why-single-use-bioreactors-are-revolutionizing-cell-culture-in-2025/]
- 94. What is UNG/UDG? [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/real-time-pcr-basics/what-is-ung-udg.html]
- 95. Use of uracil DNA glycosylase to control carry-over ... [https://pubmed.ncbi.nlm.nih.gov/2227421/]
- 96. Minimizing PCR Cross-Contamination using GoTaq® DNA ... [https://www.promega.com/resources/pubhub/enotes/minimizing-pcr-crosscontamination-using-gotaq-dna-polymerase-with-dutp-and-ung/]
- 97. DNA Repair Enzyme Uracil DNA Glycosylase Is ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC103999/]
- 98. Controlling for contamination in qPCR testing - LGC [https://blog.biosearchtech.com/how-to-control-for-contamination-in-qpcr-testing]
- 99. Use of uracil-DNA glycosylase enzyme to reduce DNA-related ... [https://appliedcr.biomedcentral.com/articles/10.1186/s41241-019-0075-2]
- 100. DNA decontamination methods for internal quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6816905/]
- 101. 9 Tips to Improve Your Contamination Control Strategy (CCS) [https://dycem.com/blog/9-tips-to-improve-your-contamination-control-strategy-ccs/]
- 102. Contamination Control Strategies: A Path for Quality & Safety [https://www.pda.org/pda-letter-portal/home/full-article/contamination-control-strategies-a-path-for-quality-safety]
- 103. Repeatability vs. Reproducibility | Technology Networks [https://www.technologynetworks.com/informatics/articles/repeatability-vs-reproducibility-317157]
- 104. 食å“实验室常è§ä»ªå™¨è®¾å¤‡æ“作规程有哪些? - 知识概念 [https://lab.jgvogel.cn/c/2021-05-09/1108092.shtml]
- 105. How to Avoid Contamination in Lab Samples [https://www.aurorabiomed.com/how-to-avoid-contamination-in-lab-samples/?srsltid=AfmBOor-jzQRj4rR0xdqxDTgnTaWqxntHoKg6lWwBa7ofHM3noC8TriG]
- 106. å°¾èœå †è‚¥å¾®ç”Ÿç‰©ç»„ æ · å“å– æ · 方法 —BIO-101 [https://en.bio-protocol.org/bio101/e2003366]
- 107. Keeping Track of Biosamples [https://www.autoscribeinformatics.com/resources/blog/keeping-track-of-biosamples]