Verifying Functional Sensitivity: A Practical Guide to Establishing Interassay Precision Profiles for Robust Bioanalytical Methods
This article provides a comprehensive guide for researchers and drug development professionals on verifying functional sensitivity through interassay precision profiles.
Verifying Functional Sensitivity: A Practical Guide to Establishing Interassay Precision Profiles for Robust Bioanalytical Methods
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on verifying functional sensitivity through interassay precision profiles. It covers foundational principles distinguishing functional sensitivity from analytical sensitivity, details CLSI-aligned methodologies for precision testing, strategies for troubleshooting poor precision, and frameworks for statistical validation and comparison against manufacturer claims. The content synthesizes current guidelines, practical protocols, and emerging trends to equip scientists with the knowledge to reliably determine the lower limits of clinically reportable results for immunoassays and other bioanalytical methods, thereby ensuring data integrity and regulatory compliance in preclinical and clinical studies.
Functional Sensitivity vs. Analytical Sensitivity: Defining the Clinically Relevant Detection Limit
For researchers and drug development professionals, the journey from theoretical detection to clinically useful results is paved with critical performance verification. The terms "analytical sensitivity" and "functional sensitivity" represent fundamentally different concepts in assay validation, with the former describing pure detection capability and the latter defining practical utility in real-world settings. Analytical sensitivity, formally defined as the lowest concentration that can be distinguished from background noise, represents the assay's detection limit and is typically established by assaying replicates of a sample with no analyte present, then calculating the concentration equivalent to the mean counts of the zero sample plus 2 standard deviations for immunometric assays [1]. While this parameter provides fundamental characterization, its practical value is limited because imprecision increases dramatically as analyte concentration decreases, often making results unreliable even at concentrations significantly above the detection limit [1].
The critical limitation of analytical sensitivity led to the development of functional sensitivity, which addresses the essential question: "What is the lowest concentration at which an assay can report clinically useful results?" [1] Functional sensitivity represents the lowest analyte concentration that can be measured with acceptable precision and accuracy during routine operating conditions, typically defined by interassay precision profiles with a coefficient of variation (CV) not exceeding 20% for many clinical applications [1]. This distinction is not merely academic—it directly impacts clinical decision-making, therapeutic monitoring, and diagnostic accuracy across diverse applications from cardiac troponin testing to cancer biomarker detection and infectious disease diagnostics.
Key Concepts: Analytical vs. Functional Sensitivity
Fundamental Definitions and Distinctions
The transition from theoretical detection to clinical usefulness requires understanding both the capabilities and limitations of analytical methods. The following table summarizes the core differences between these two critical performance parameters:
| Parameter | Analytical Sensitivity | Functional Sensitivity |
|---|---|---|
| Definition | Lowest concentration distinguishable from background noise [1] | Lowest concentration for clinically useful results with acceptable precision [1] |
| Common Terminology | Detection limit, limit of detection (LOD) [1] [2] | Lower limit of quantitation (LLOQ) [3] |
| Calculation Method | Mean of zero sample ± 2 SD (depending on assay type) [1] | Concentration where CV reaches predetermined limit (typically 20%) [1] |
| Primary Focus | Signal differentiation from background [1] | Result reproducibility and reliability [1] |
| Clinical Utility | Limited - indicates detection capability only [1] | High - defines clinically reportable range [1] |
| Relationship to Precision | Not directly considered [1] | Defined by precision profile [1] |
| Typical Value Relative to Detection Limit | Lower concentration [1] | Higher concentration (often significantly above detection limit) [1] |
The Precision Profile: Connecting Imprecision to Clinical Usefulness
The precision profile provides the crucial link between theoretical detection and clinical usefulness by graphically representing how assay imprecision changes with analyte concentration [1]. As concentration decreases toward the detection limit, imprecision increases rapidly, creating a zone where detection is theoretically possible but clinically unreliable. Functional sensitivity establishes the boundary of this zone by defining the concentration at which imprecision exceeds a predetermined acceptability threshold [1].
The selection of an appropriate CV threshold (commonly 20% for TSH assays) determines where functional sensitivity is established along the precision profile [1]. This threshold represents the maximum imprecision tolerable for clinical purposes, balancing analytical capabilities with medical decision requirements. For a sample with a concentration at the functional sensitivity limit, a 20% CV implies that 95% of expected results from repeat analyses would fall within ±40% of the mean value (±2 SD) [1]. This degree of variation has significant implications for interpreting serial measurements and detecting clinically meaningful changes in analyte concentration.
Experimental Approaches for Verification
Protocol for Determining Functional Sensitivity
Establishing functional sensitivity requires a methodical approach focusing on interassay precision across the measuring range. The following workflow outlines the key steps:
Step 1: Define Performance Goal - Establish the maximum acceptable interassay CV representing the limit of clinical usefulness for the specific assay and its intended application. While a 20% CV has been widely used since the concept's origin in TSH testing, this threshold should be determined based on clinical requirements for each specific assay [1]. Some applications may tolerate higher imprecision while others require more stringent limits.
Step 2: Identify Target Concentration Range - Based on prior studies, package insert data, and estimates from the assay's precision profile, identify a concentration range bracketing the predetermined CV limit [1]. Technical services can often assist in identifying this target range.
Step 3: Prepare Test Samples - Ideally, use several undiluted patient samples or pools of patient samples with concentrations spanning the target range. If these are unavailable, reasonable alternatives include patient samples diluted to appropriate concentrations or control materials within the target range [1]. If dilution is necessary, select diluents carefully as routine sample diluents may have measurable apparent concentrations that could bias results.
Step 4: Execute Interassay Precision Testing - Analyze samples repeatedly over multiple different runs, ideally over a period of days or weeks to properly assess day-to-day precision [1]. A single run with multiple replicates does not provide a valid assessment of functional sensitivity, as it fails to capture the interassay variability encountered in routine use.
Step 5: Calculate CV at Each Concentration - For each sample tested, calculate the CV as (standard deviation/mean) × 100%. This quantifies the interassay precision at each concentration level across the evaluated range.
Step 6: Determine Functional Sensitivity - Identify the concentration at which the CV reaches the predetermined performance goal. If this concentration doesn't coincide exactly with one of the tested levels, it can be estimated by interpolation from the study results [1].
Comparison of Verification Protocols
Different assay performance characteristics require distinct verification approaches, as summarized in the following table:
| Verification Type | Protocol Focus | Sample Requirements | Key Output |
|---|---|---|---|
| Analytical Sensitivity | Distinguishing signal from background [1] | 20 replicates of true zero concentration sample [1] | Concentration equivalent to mean zero ± 2 SD [1] |
| Functional Sensitivity | Interassay precision at low concentrations [1] | Multiple samples across target range, analyzed over different runs [1] | Lowest concentration with acceptable CV [1] |
| Lower Limit of Reportable Range | Performance across reportable range [1] | 3-5 samples spanning entire reportable range [1] | Verified concentration range with clinically useful performance [1] |
| Spike Recovery | Accuracy in sample matrix [3] [2] | Samples spiked with known analyte concentrations [2] | Percent recovery (target: 80-120%) [3] |
| Dilutional Linearity | Sample dilution integrity [3] | Spiked samples diluted through ≥3 dilutions [3] | Recovery across dilutions (target: 80-120%) [3] |
Advanced Verification Techniques
Modern verification approaches incorporate sophisticated methodologies to ensure assay reliability:
LLOQ Verification - The Lower Limit of Quantification represents the lowest point on the standard curve where CV <20% and accuracy is within 20% of expected values [3]. This parameter aligns closely with functional sensitivity and is verified through precision and accuracy profiles.
Inter- and Intra-Assay Precision - Inter-assay precision involves analyzing the same samples on multiple plates over multiple days to ensure reproducibility, with acceptable values typically within 20% across experiments [3]. Intra-assay precision tests multiple samples in replicate on the same plate, with %CV ideally less than 10% [2].
Specificity Testing - For high-sensitivity applications, specificity is demonstrated through spike recovery experiments where the analyte is added at the lower end of the standard curve to ensure accurate measurements in real sample matrices [3] [2]. A minimum of 10 samples are typically spiked with acceptable recovery between 80-120% [3].
Case Studies & Applications
High-Sensitivity Cardiac Troponin Testing
Recent verification studies demonstrate the critical importance of functional sensitivity in cardiac biomarker testing. A 2025 study of the novel Quidel TriageTrue hs-cTnI assay for implementation in rural clinical laboratories exemplifies rigorous verification in practice [4]. The precision study was performed over 5-6 days with 5 replicates daily using quality control materials and patient plasma pools corresponding to clinical decision thresholds. The assay demonstrated a coefficient of variation (CV) <10% near the overall 99th percentile upper reference limit (URL), confirming its functional sensitivity meets the requirements for high-sensitivity troponin testing [4]. The study further established >90% analytical concordance at the 99th percentile URL and <10% risk reclassification compared to established hs-cTnI assays, validating its clinical utility [4].
Emerging Technologies and Applications
CRISPR-Based Detection Systems - Advanced molecular diagnostics now incorporate functional sensitivity principles through innovative designs. A programmable AND-logic-gated CRISPR-Cas12 system for SARS-CoV-2 detection achieves exceptional sensitivity (limit of detection: 4.3 aM, ~3 copies/μL) while maintaining 100% specificity through dual-target collaborative recognition [5]. This approach significantly enhances detection specificity and anti-interference capability through target cross-validation, demonstrating how functional reliability can be engineered into diagnostic systems.
Dual-Functional Probes for Cancer Detection - Novel detection platforms integrate multiple technologies to enhance sensitivity and specificity. A dual-functional aptamer sensor based on Au NPs/CDs for detecting MCF-7 breast cancer cells achieves sensitive detection by recognizing MUC1 protein on cell surfaces while integrating inductively coupled plasma mass spectrometry (ICP-MS) and fluorescence imaging technology [6]. This combination enhances sensitivity, specificity, and accuracy for breast cancer cell detection, with Mendelian randomization analysis further verifying MUC1's potential as a biomarker for multiple cancers [6].
AI-Enhanced Drug Response Prediction - The PharmaFormer model demonstrates how advanced computational approaches can predict clinical drug responses through transfer learning guided by patient-derived organoids [7]. This clinical drug response prediction model, based on custom Transformer architecture, was initially pre-trained with abundant gene expression and drug sensitivity data from 2D cell lines, then fine-tuned with limited organoid pharmacogenomic data [7]. The integration of both pan-cancer cell lines and organoids of a specific tumor type provides dramatically improved accurate prediction of clinical drug response, highlighting how data integration enhances functional prediction capabilities [7].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful verification of functional sensitivity requires specific reagents and materials designed to challenge assay performance under realistic conditions:
| Tool/Reagent | Function in Verification | Key Considerations |
|---|---|---|
| True Zero Concentration Sample | Establishing analytical sensitivity [1] | Appropriate sample matrix is essential; any deviation biases results [1] |
| Patient-Derived Sample Pools | Assessing functional sensitivity [1] | Multiple individual samples spanning target concentration range [1] |
| Quality Control Materials | Precision verification [4] | Concentrations near clinical decision points [4] |
| Sample Diluents | Preparing concentration gradients [1] | Routine diluents may have measurable apparent concentration; select carefully [1] |
| Reference Standards | Accuracy determination [8] | Characterized materials for spike recovery studies [2] |
| Matrix-Matched Materials | Specificity assessment [2] | Evaluate interference from sample components [2] |
| GDC-0349 | GDC-0349, CAS:1207360-89-1, MF:C24H32N6O3, MW:452.5 g/mol | Chemical Reagent |
| Setanaxib | Setanaxib, CAS:1218942-37-0, MF:C21H19ClN4O2, MW:394.9 g/mol | Chemical Reagent |
The distinction between analytical and functional sensitivity represents more than technical semantics—it embodies the essential transition from theoretical detection capability to clinically useful measurement. While analytical sensitivity defines the fundamental detection limits of an assay, functional sensitivity establishes the practical boundaries of clinical usefulness based on reproducibility requirements. This distinction becomes particularly critical at low analyte concentrations where imprecision increases rapidly, potentially compromising clinical interpretation even when detection remains technically possible.
For researchers and drug development professionals, rigorous verification of functional sensitivity through interassay precision profiles provides the evidence base needed to establish clinically reportable ranges. The continuing evolution of detection technologies—from high-sensitivity immunoassays to CRISPR-based molecular diagnostics and AI-enhanced prediction models—further emphasizes the importance of defining and verifying functional performance characteristics. By implementing systematic verification protocols that challenge assays under conditions mimicking routine use, the field advances toward more reliable, reproducible, and clinically meaningful measurement systems that ultimately support improved diagnostic and therapeutic decisions.
For researchers and scientists in drug development and clinical diagnostics, understanding the lower limits of an assay's performance is critical for generating reliable data. The terms analytical sensitivity, functional sensitivity, and interassay precision are fundamental performance metrics, yet they are often confused or used interchangeably. This guide clarifies these core definitions, compares their performance characteristics, and provides the experimental protocols required for their verification. Framed within the broader thesis of verifying functional sensitivity with interassay precision profiles, this article serves as a practical resource for validating assay performance.
Core Definitions and Comparative Analysis
The table below provides a concise comparison of these three critical performance metrics.
Table 1: Core Performance Metrics Comparison
| Metric | Definition | Primary Focus | Typical Determination | Clinical Utility |
|---|---|---|---|---|
| Analytical Sensitivity [1] [9] | The lowest concentration of an analyte that can be distinguished from background noise (a blank sample). | Detection Limit | Mean signal of zero sample ± 2 SD (for immunometric/competitive assays); also known as the Limit of Detection (LoD) [1]. | Limited; indicates presence/absence but does not guarantee clinically reproducible results [1]. |
| Functional Sensitivity [1] [9] | The lowest concentration at which an assay can report clinically useful results, defined by an acceptable level of imprecision (e.g., CV ≤ 20%). | Clinical Reportability | The concentration at which the interassay CV meets a predefined precision goal (often 20%) [1] [9]. | High; defines the lower limit of the reportable range for clinically reliable results [1]. |
| Interassay Precision [10] | The reproducibility of results when the same sample is analyzed in multiple separate runs, over days, and often by different technicians. | Run-to-Run Reproducibility | Coefficient of variation (CV%) calculated from results of a sample tested across multiple independent assays [10]. | High; ensures consistency and reliability of results over time in a clinical or research setting [10]. |
Experimental Protocols for Determination
Accurate determination of each metric requires specific experimental designs and statistical analysis.
Determining Analytical Sensitivity (Limit of Detection)
Objective: To verify the lowest concentration distinguishable from a zero calibrator (blank) [1].
Protocol:
- Sample Preparation: Use a true zero concentration sample with an appropriate sample matrix. Any other type of sample may bias the results [1].
- Replication: Assay 20 replicates of the zero sample in a single run [1].
- Calculation:
- Calculate the mean and standard deviation (SD) of the measured counts (or signals) from the replicates.
- For immunometric ("sandwich") assays, the Analytical Sensitivity is the concentration equivalent to the mean signal of the zero sample + 2 SD.
- For competitive assays, it is the concentration equivalent to the mean signal - 2 SD [1].
This protocol provides an initial estimate for comparison with manufacturer claims. A robust assessment requires multiple experiments across several kit lots [1].
Determining Functional Sensitivity
Objective: To establish the lowest analyte concentration that can be measured with a defined interassay precision (e.g., CV ≤ 20%) [1] [9].
Protocol:
- Set Precision Goal: Define the maximum acceptable interassay CV (e.g., 20%) based on the assay's intended clinical application [1].
- Sample Selection: Ideally, use several undiluted patient samples or pools with concentrations spanning the expected target range near the limit. If unavailable, patient samples diluted to these concentrations or control materials are alternatives [1].
- Longitudinal Testing: Analyze these samples repeatedly over multiple different runs (e.g., over days or weeks). A single run of replicates is insufficient, as it does not capture day-to-day variability [1].
- Data Analysis:
- For each sample, calculate the mean, standard deviation, and CV% of the results from all runs.
- Plot the CV% against the mean concentration for each sample to create a precision profile.
- The Functional Sensitivity is the lowest concentration at which the CV meets the predefined goal (e.g., 20%), which can be estimated by interpolation [1].
Determining Interassay Precision
Objective: To measure the total variability of an assay across separate runs under normal operating conditions [10].
Protocol:
- Sample Selection: Use at least two levels of quality control materials or patient samples (e.g., low, medium, and high concentrations) [11].
- Testing Schedule: Include the samples in multiple independent assay runs. This should involve different calibrations, different days, and ideally different operators [11] [10].
- Replication: A common design is to test each sample in duplicate or triplicate over five consecutive days [11].
- Calculation:
- Pool all results for a given sample from all runs.
- Calculate the overall mean and standard deviation.
- The Interassay CV% is calculated as: (Overall Standard Deviation / Overall Mean) × 100 [10].
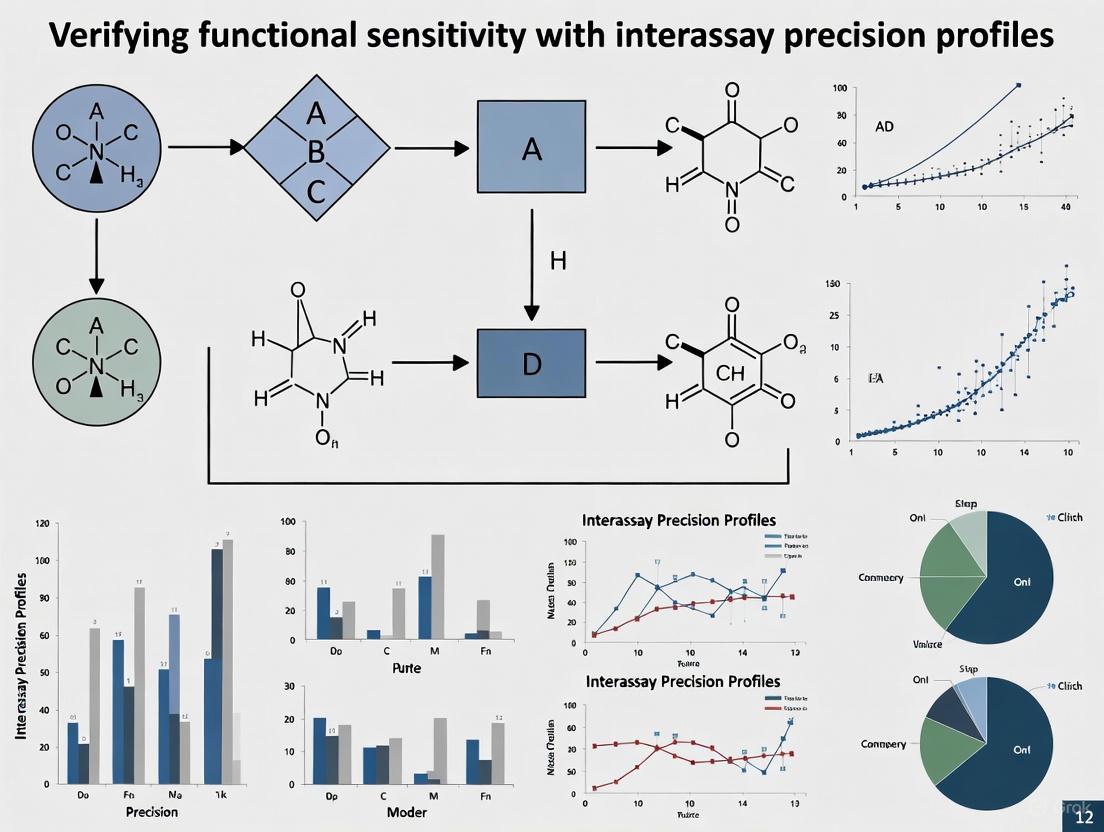
Diagram 1: Experimental protocol workflows for determining key assay performance metrics.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key materials required for the experiments described above.
Table 2: Essential Research Reagents and Materials
| Item | Function / Critical Note |
|---|---|
| True Zero Calibrator | A sample with an appropriate matrix confirmed to contain no analyte. Crucial for a valid Analytical Sensitivity (LoD) study [1]. |
| Patient-Derived Sample Pools | Undiluted patient samples or pools with analyte concentrations in the low range are the ideal material for Functional Sensitivity studies [1]. |
| Quality Control (QC) Materials | Commercially available or internally prepared controls at low, medium, and high concentrations are essential for assessing Interassay Precision [11]. |
| Appropriate Diluent | If sample dilution is necessary, the choice of diluent is critical to avoid bias; routine sample diluents may have low apparent analyte levels [1]. |
| Precision Profiling Software | Software capable of calculating CV%, generating precision profiles, and performing interpolation is needed for data analysis [1]. |
| GNF-5837 | GNF-5837, CAS:1033769-28-6, MF:C28H21F4N5O2, MW:535.5 g/mol |
| LolCDE-IN-3 | LolCDE-IN-3, MF:C20H21N3O2, MW:335.4 g/mol |
Current Data and Application in High-Sensitivity Assays
The concepts of functional sensitivity and interassay precision are actively applied in cutting-edge research, particularly in the validation of high-sensitivity cardiac troponin (hs-cTn) assays. A 2025 study on hs-cTnI assays provides a relevant example of performance verification in a clinical context [11].
Table 3: Performance Data from a 2025 hs-cTnI Assay Study
| Performance Metric | Verified Value | Experimental Method |
|---|---|---|
| Limit of Blank (LoB) | Determined statistically | Two blank samples measured 30 times over 3 days [11]. |
| Limit of Detection (LoD) | 2.5 ng/L | Two samples near the estimated LoD measured 30 times over 3 days [11]. |
| Functional Sensitivity (LoQ at CV=20%) | Interpolated from precision profile | Samples at multiple low concentrations (2.5-17.5 ng/L) analyzed over 3 days; CV calculated for each [11]. |
| Interassay Precision | CV% reported for three levels | Three concentration levels analyzed in triplicate over five consecutive days [11]. |
This study underscores the hierarchy of these metrics: the LoD (Analytical Sensitivity) is the bare minimum for detection, while the Functional Sensitivity (the concentration at a CV of 20%) defines the practical lowest limit for precise quantification, directly informed by Interassay Precision data [11]. This relationship is foundational to verifying functional sensitivity with interassay precision profiles.
The Critical Role of the Precision Profile in Functional Sensitivity Determination
In the field of clinical laboratory science and biotherapeutic drug monitoring, functional sensitivity represents a critical performance parameter defined as the lowest analyte concentration that an assay can measure with an interassay precision of ≤20% coefficient of variation (CV) [12]. This parameter stands distinct from the lower limit of detection (LoD), which is typically determined by measuring a zero calibrator and represents the smallest concentration statistically different from zero. Unlike LoD, functional sensitivity reflects practical usability under routine laboratory conditions, making it fundamentally more relevant for clinical applications where reliable quantification at low concentrations directly impacts therapeutic decisions [12].
The precision profile, also known as an imprecision profile, serves as the primary graphical tool for determining functional sensitivity. Originally conceived by Professor R.P. Ekins in an immunoassay context, this profile expresses the precision characteristics of an assay across its entire measurement range [13]. By converting complex replication data into an easily interpreted graphical summary, precision profiles enable scientists to identify the precise concentration at which an assay transitions from reliable to unreliable measurement. For researchers and drug development professionals, this tool is indispensable for validating assay performance, particularly when monitoring biologic drugs like adalimumab and infliximab, where precise quantification of drug levels and anti-drug antibodies (ADAs) directly informs treatment optimization [14].
Experimental Protocols for Precision Profiling
Foundational Methodological Approach
The determination of functional sensitivity through precision profiling follows established clinical laboratory guidelines with specific modifications for comprehensive profile generation. The Clinical and Laboratory Standards Institute (CLSI) EP5-A guideline provides the foundational experimental design, recommending the analysis of replicated specimens over 20 days with two runs per day and two replicates per run [12] [13]. This structured approach yields robust estimates of both within-run (repeatability) and total (interassay) CVs, with the latter being most relevant for functional sensitivity determination.
The experimental workflow begins with preparation of multiple serum pools or control materials spanning the assay's anticipated measuring range, with particular emphasis on concentrations near the expected lower limit. These materials are typically analyzed in singleton or duplicate across multiple batches, incorporating multiple calibration events and reagent lot changes to capture real-world variability [13]. The resulting CV values are plotted against mean concentration values, generating the precision profile curve. The functional sensitivity is then determined by identifying the concentration where this curve intersects the 20% CV threshold [12].
Direct Variance Function Estimation
Modern implementations often employ direct variance function estimation to construct precision profiles. This approach fits a mathematical model to replicated results without requiring precisely structured data, allowing laboratories to merge method evaluation data with routine internal quality control (QC) data [13]. A commonly used three-parameter variance function is:
σ²(U) = (β₠+ β₂U)ᴶ [13]
Where U represents concentration, βâ‚, β₂, and J are fitted parameters, and σ²(U) is the predicted variance. This model offers sufficient curvature to describe variance relationships for both competitive and immunometric immunoassays. Once fitted, the model generates a smooth precision profile across the entire assay range, from which functional sensitivity is easily determined [13].
Comparative Analysis of Assay Performance
Case Study: Third Generation Allergen-Specific IgE Assay
The development of a third generation chemiluminescent enzyme immunoassay for allergen-specific IgE (sIgE) on the IMMULITE 2000 system demonstrates the critical importance of precision profiling in functional sensitivity determination. This assay incorporated a true zero calibrator, enabling reliable quantification at concentrations previously inaccessible to earlier assay generations [12].
Table 1: Functional Sensitivity Comparison - IgE Assays
| Assay Generation | Detection Limit (kU/L) | Functional Sensitivity (kU/L) | Measuring Range (kU/L) | Key Innovation |
|---|---|---|---|---|
| First Generation (mRAST) | ~0.35 | Not determined | 0.35-100 | Radioisotopic detection, single calibrator |
| Second Generation (CAP System) | 0.35 | ~0.35 (extrapolated) | 0.35-100 | Enzyme immunoassay, WHO standardization |
| Third Generation (IMMULITE 2000) | <0.1 | 0.2 | 0.1-100 | True zero calibrator, liquid allergens, automated washing |
As illustrated in Table 1, the third generation assay demonstrated a functional sensitivity of 0.2 kU/L, a significant improvement over second generation assays that treated their lowest calibrator (0.35 kU/L) as both the detection limit and functional sensitivity [12]. The precision profile for this assay (Figure 2 in the original study) showed total CVs meeting NCCLS I/LA20-A performance targets, with ≤20% at low concentrations (near 0.35 kU/L) and ≤15% at medium and high concentrations [12].
Case Study: i-Tracker Drug & Anti-Drug Antibody Assays
A 2025 validation study of the i-Tracker chemiluminescent immunoassays (CLIA) for adalimumab, infliximab, and associated anti-drug antibodies further exemplifies the application of precision profiling in biotherapeutic monitoring. This automated, cartridge-based system demonstrated up to 8% imprecision across clinically relevant analyte ranges [14].
Table 2: Precision Profiles - i-Tracker Assays on IDS-iSYS Platform
| Analyte | Within-Run Precision (% CV) | Total Precision (% CV) | Functional Sensitivity | Drug Tolerance of Total ADA Assay |
|---|---|---|---|---|
| Adalimumab | ≤5% (across range) | ≤8% (across range) | Established per CLSI guidelines | Detected ADAs in supratherapeutic drug concentrations |
| Infliximab | ≤5% (across range) | ≤8% (across range) | Established per CLSI guidelines | Demonstrated higher ADA detection rate vs. reference method |
| Total Anti-Adalimumab | Data included in total precision | Similar profile to drug assays | Determined from precision profile | >85% qualitative agreement with reference method |
| Total Anti-Infliximab | Data included in total precision | Similar profile to drug assays | Determined from precision profile | <60% negative agreement with reference method |
The i-Tracker validation emphasized that robust analytical performance, including functional sensitivity determination via precision profiling, suggests "potential for clinical application" for monitoring adalimumab- and infliximab-treated patients [14]. The study also highlighted how method comparisons reveal functional differences between assay formats, an essential consideration when transitioning between platforms for therapeutic drug monitoring [14].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Essential Research Reagents for Precision Profiling Studies
| Reagent/Material | Function/Application | Example from Literature |
|---|---|---|
| Liquid Allergens | Maintain natural protein conformations for optimal antibody binding in IgE assays | IMMULITE 2000 sIgE assay [12] |
| Biotinylated Allergens | Enable immobilization on streptavidin-coated solid phases | IMMULITE 2000 sIgE assay [12] |
| ADA Reference Materials | Polyclonal or monoclonal antibodies for spiking experiments | i-Tracker validation using polyclonal anti-adalimumab [14] |
| Drug Biosimilars | Enable preparation of calibrators and spiked samples at known concentrations | i-Tracker validation using adalimumab/ infliximab biosimilars [14] |
| Zero Calibrator | Establishes true baseline for curve fitting and low-end quantification | Third generation IgE assay with true zero calibrator [12] |
| Stable Serum Pools | Multiple concentrations for precision profiling across measuring range | CLSI EP5-A guideline implementation [13] |
| Chemiluminescent Substrate | Signal generation with broad dynamic range | Acridinium ester in i-Tracker; adamantyl dioxetane in IMMULITE [14] [12] |
| Monoclonal Anti-IgE Antibody | Specific detection of bound IgE in sandwich assays | Alkaline phosphatase-labeled anti-IgE in IMMULITE 2000 [12] |
| GS-441524 | GS-441524, CAS:1191237-69-0, MF:C12H13N5O4, MW:291.26 g/mol | Chemical Reagent |
| Lenacapavir | Lenacapavir, CAS:2189684-45-3, MF:C39H32ClF10N7O5S2, MW:968.3 g/mol | Chemical Reagent |
Visualization of Precision Profile Concepts
Experimental Workflow for Precision Profiling
Precision Profile Interpretation
Implications for Clinical Application & Drug Development
The strategic application of precision profiling extends beyond analytical validation to directly impact patient care in biotherapeutic monitoring. For drugs like adalimumab and infliximab, where therapeutic trough levels correlate with clinical efficacy and anti-drug antibodies cause secondary treatment failure, establishing reliable functional sensitivity enables clinicians to make informed dosage adjustments and treatment strategy pivots [14]. The i-Tracker validation study exemplifies this principle, demonstrating how robust precision profiles support the clinical application of automated monitoring systems [14].
Furthermore, precision profiling reveals critical differences between assay methodologies that directly impact clinical interpretation. The observed discrepancy between i-Tracker and reference methods for anti-infliximab antibody detection (<60% negative agreement) underscores how functional sensitivity differences can significantly alter patient classification [14]. This highlights the essential role of precision profiling in method comparison and selection for therapeutic drug monitoring programs, particularly as laboratories transition to increasingly automated platforms promising improved operational efficiency [14].
In the pharmaceutical and drug development industries, the reliability of analytical data is the foundation of quality control, regulatory submissions, and ultimately, patient safety. Researchers and scientists navigating this landscape must adhere to a harmonized yet complex framework of regulatory guidelines. The International Council for Harmonisation (ICH), the U.S. Food and Drug Administration (FDA), and the Clinical and Laboratory Standards Institute (CLSI) provide the primary guidance for assay validation, ensuring that analytical procedures are fit for their intended purpose [15].
A modern understanding of assay validation has evolved from a one-time event to a continuous lifecycle management process, a concept reinforced by the simultaneous release of the updated ICH Q2(R2) and the new ICH Q14 guidelines [15]. This shift emphasizes a more scientific, risk-based approach, encouraging the use of an Analytical Target Profile (ATP)—a prospective summary of the method's intended purpose and desired performance characteristics [15]. For studies focused on verifying functional sensitivity with interassay precision profiles, these guidelines provide the structure for designing robust experiments and demonstrating the requisite analytical performance for regulatory acceptance.
Comparative Analysis of Key Guidelines
The following table summarizes the scope and primary focus of the major regulatory guidelines relevant to assay validation.
Table 1: Key Regulatory Guidelines for Assay Validation
| Guideline | Issuing Body | Primary Focus and Scope |
|---|---|---|
| ICH Q2(R2): Validation of Analytical Procedures [16] | International Council for Harmonisation (ICH) | Provides a global framework for validating analytical procedures; covers fundamental performance characteristics for methods used in pharmaceutical drug development [15] [16]. |
| ICH M10: Bioanalytical Method Validation and Study Sample Analysis [17] | ICH (adopted by FDA) | Describes recommendations for method validation of bioanalytical assays (chromatographic & ligand-binding) for nonclinical and clinical studies supporting regulatory submissions [17]. |
| CLSI EP15: User Verification of Precision and Estimation of Bias [18] | Clinical and Laboratory Standards Institute (CLSI) | Provides a protocol for laboratories to verify a manufacturer's claims for precision and estimate bias; designed for use in clinical laboratories [18]. |
| FDA Guidance on Bioanalytical Method Validation for Biomarkers [19] | U.S. Food and Drug Administration (FDA) | Provides recommendations for biomarker bioanalysis; directs use of ICH M10 as a starting point, while acknowledging its limitations for biomarkers [19]. |
Detailed Comparison of Validation Parameters
While all guidelines aim to ensure data reliability, the specific parameters and acceptance criteria can vary based on the assay's intended use. The table below delineates the core validation parameters as described in these documents.
Table 2: Core Validation Parameters Across Guidelines
| Validation Parameter | ICH Q2(R2) Context [15] | ICH M10 Context [17] | CLSI EP15 Context [18] | Relevance to Functional Sensitivity |
|---|---|---|---|---|
| Accuracy | Closeness between test result and true value. | Recommended for bioanalytical assays. | Estimated as "bias" against materials with known concentrations. | Confirms measured concentration reflects true level at low concentrations. |
| Precision | Degree of agreement among repeated measurements. Includes repeatability, intermediate precision. | Required, with specific focus on incurred sample reanalysis for some studies. | Verified through a multi-day experiment to estimate imprecision. | Directly measured via interassay precision profiles to determine functional sensitivity. |
| Specificity | Ability to assess analyte unequivocally in presence of potential interferents. | Assessed for bioanalytical assays. | Not a primary focus of the EP15 verification protocol. | Ensures precision profile is not affected by matrix interferences at low analyte levels. |
| Linearity & Range | Interval where linearity, accuracy, and precision are demonstrated. | The working range must be validated. | Range verification is implied through the use of multiple samples. | Defines the assay's quantitative scope and the lower limit of quantitation. |
| Limit of Quantitation (LOQ) | Lowest amount quantified with acceptable accuracy and precision. | Established during method validation. | Not directly established; protocol verifies performance near claims. | Functional sensitivity is the practical LOQ based on interassay precision (e.g., ≤20% CV). |
Experimental Protocols for Assessing Functional Sensitivity
Protocol 1: Establishing the Interassay Precision Profile
The interassay precision profile is a critical tool for determining the functional sensitivity of an assay, which is defined as the lowest analyte concentration that can be measured with a specified precision (e.g., a coefficient of variation (CV) of 20%) across multiple independent runs [20].
Detailed Methodology:
- Sample Preparation: Prepare a minimum of 8-10 samples of the analyte spanning the expected low end of the working range, including concentrations below the anticipated functional sensitivity. A pool of the authentic biological matrix is strongly recommended to reflect true assay conditions [20].
- Experimental Design: Analyze each sample in duplicate or triplicate in at least 5-6 independent analytical runs conducted by different analysts over different days. This design captures between-run variance, a key component of interassay precision [18] [20].
- Data Analysis:
- For each concentration level, calculate the mean, standard deviation (SD), and CV%.
- Plot the CV% (y-axis) against the mean concentration (x-axis) to generate the precision profile.
- The functional sensitivity is the concentration at which the precision profile intersects the pre-defined CV acceptability criterion (e.g., 20% CV).
Protocol 2: Comparison of Methods for Systematic Error
This protocol estimates the systematic error (bias) of a new test method against a comparative method, which is essential for contextualizing functional sensitivity data [20].
Detailed Methodology:
- Sample Selection: Analyze a minimum of 40 different patient specimens to cover the entire working range of the method, with a focus on the medically relevant decision levels [20].
- Experimental Execution: Analyze each specimen by both the test and comparative methods within a short time frame (ideally within 2 hours) to maintain specimen stability. The experiment should be conducted over multiple days (minimum of 5) to incorporate routine source of variation [20].
- Statistical Analysis:
- For a wide analytical range: Use linear regression analysis (
Y_test = a + b * X_comparative) to estimate the slope (b) and y-intercept (a). The systematic error (SE) at a critical medical decision concentration (Xc) is calculated asSE = (a + b*Xc) - Xc[20]. - For a narrow analytical range: Calculate the average difference (bias) between the test and comparative methods using a paired t-test [20].
- For a wide analytical range: Use linear regression analysis (
The workflow below illustrates the key stages of this comparative method validation.
Figure 1: Method Comparison Experiment Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting robust assay validation studies, particularly those focused on precision and sensitivity.
Table 3: Essential Reagents and Materials for Validation Studies
| Item | Function in Validation |
|---|---|
| Authentic Biological Matrix | Serves as the sample matrix for preparing calibration standards and quality controls; critical for accurately assessing matrix effects, specificity, and functional sensitivity [20]. |
| Reference Standard | A well-characterized analyte of known purity and concentration used to prepare calibration curves; its quality is fundamental for establishing accuracy and linearity [15]. |
| Stable, Pooled Patient Samples | Used in interassay precision profiles to measure total assay variance over time; the foundation for determining functional sensitivity [20]. |
| Quality Control (QC) Materials | Samples with known (or assigned) analyte concentrations analyzed in each run to monitor the stability and consistency of the assay's performance over time [18]. |
| Surrogate Matrix | Used when the authentic matrix is difficult to obtain or manipulate; allows for the preparation of calibration standards, though parallelism must be demonstrated to ensure accuracy [19]. |
| GS-6620 | GS-6620, CAS:1350735-70-4, MF:C29H37N6O9P, MW:644.6 g/mol |
| GS-9191 | GS-9191, CAS:859209-84-0, MF:C37H51N8O6P, MW:734.8 g/mol |
Navigating the regulatory context of ICH, CLSI, and FDA guidelines is paramount for successful drug development. ICH Q2(R2) and M10 provide the comprehensive, foundational framework for validating new methods, while CLSI EP15 offers an efficient pathway for verifying performance in a local laboratory [18] [15] [21]. For the specific thesis context of verifying functional sensitivity, the interassay precision profile is the cornerstone experiment. It directly measures the assay's reliability at low analyte concentrations and provides concrete data on its practical limits of quantitation. By designing studies that align with these harmonized guidelines and incorporating a rigorous, statistically sound assessment of precision, researchers can generate defensible data that withstands regulatory scrutiny and advances the development of safe and effective therapies.
A Step-by-Step Protocol for Generating Interassay Precision Profiles and Calculating Functional Sensitivity
The accuracy and reliability of bioanalytical data in drug development hinge on the rigorous selection and characterization of patient samples, controls, and matrices. Within the critical context of verifying functional sensitivity—the lowest analyte concentration that can be measured with acceptable precision, often defined by an interassay precision profile (e.g., CV ≤20%)—the choice of materials directly impacts the robustness of this determination. This guide objectively compares the performance of various sample types and analytical platforms, providing a framework for selecting the right materials to ensure data integrity across different stages of method validation and application.
Experimental Protocols for Performance Comparison
To ensure a fair and objective comparison of analytical performance, standardized experimental designs are crucial. The following protocols, drawn from recent studies, provide a framework for generating comparable data on sensitivity, precision, and accuracy.
Protocol for High-Throughput Molecular Detection System Validation
This protocol, based on a study evaluating an automated system for pathogen nucleic acid detection, outlines a comprehensive validation strategy [22].
- Sample Types: Use a panel of clinically characterized residual patient samples (e.g., plasma, oropharyngeal swabs) and internationally recognized reference standards (e.g., WHO International Standards) [22].
- Experimental Design:
- Concordance & Accuracy: Analyze a minimum of 40 patient specimens covering the assay's working range, comparing results to a validated reference method. For quantitative assays, test samples at multiple concentrations (e.g., five gradients) in replicate [22] [20].
- Precision Profile: Perform both intra-assay (within-run) and interassay (between-run, over ≥5 days) precision testing. Calculate the coefficient of variation (CV) for each concentration level to establish the functional sensitivity (the concentration at which CV reaches 20%) [22].
- Linearity: Serially dilute reference materials in a negative matrix to create a concentration series. Assess the linear correlation coefficient (|r|) to confirm the assay's quantitative range [22].
- Carryover & Interference: Test samples in a high-low sequence to detect carryover contamination and spike potential interferents to assess specificity [22].
Protocol for Targeted Mass Spectrometry Assay Development
This protocol, derived from a study on hemoglobinopathy screening, details the creation of a multiplexed targeted assay [23].
- Sample Preparation: Punch discs from dried blood spots (DBS) or extract from liquid matrices. Denature proteins, then reduce and alkylate disulfide bonds. Digest proteins with trypsin and desalt the resulting peptides [23].
- Selection of Internal Standards: Synthesize stable isotope-labeled versions of target peptides (e.g., for wild-type and mutant globin chains) to use as internal standards for precise quantification [23].
- Mass Spectrometry Optimization:
- Method Development: By direct infusion, optimize precursor and product ion transitions (quantifier and qualifier), collision energy, and other MS parameters for each peptide.
- Scheduled SRM: Use a triple quadrupole mass spectrometer coupled to UHPLC. Develop a scheduled Selected Reaction Monitoring (SRM) method based on the optimized retention time of each peptide [23].
- Data Analysis: Calculate ratios of endogenous to internal standard peptide peaks. Determine globin chain ratios (e.g., α:β) to identify thalassemias and confirm the presence of variant-specific mutant peptides [23].
Comparative Performance Data
The selection of biological matrices and analytical platforms significantly influences key performance metrics. The following tables summarize experimental data comparing these variables across different applications.
Table 1: Comparison of Biological Matrices for Therapeutic Drug Monitoring (TDM)
Data synthesized from a systematic review of UHPLC-MS/MS methods for antipsychotic drug monitoring [24].
| Matrix | Recovery (%) | Matrix Effects | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Plasma/Serum | >90% (High) | Minimal | High analytical reliability, standard for pharmacokinetic studies | Invasive collection, requires clinical setting |
| Dried Blood Spots (DBS) | Variable | Moderate | Less invasive, stable for transport, low storage volume | Hematocrit effect, variable recovery, requires validation |
| Whole Blood | Variable | Significant | Reflects intracellular drug concentrations | Complex matrix, requires extensive sample cleanup |
| Oral Fluid | Variable | Moderate | Non-invasive collection, correlates with free drug levels | Contamination risk, variable pH and composition |
Table 2: Analytical Performance of Different Platform Types
Data compiled from evaluations of molecular detection and MS-based systems [22] [23] [24].
| Performance Metric | High-Throughput Automated PCR [22] | LC-MS/MS for Hemoglobinopathies [23] | UHPLC-MS/MS for Antipsychotics (Plasma) [24] |
|---|---|---|---|
| Analytes | EBV DNA, HCMV DNA, RSV RNA | Hemoglobin variants (HbS, HbC, etc.), α:β globin ratios | Typical & Atypical Antipsychotics and Metabolites |
| Interassay Precision (CV) | <5% | <20% | Typically <15% |
| Limit of Detection (LoD) | 10 IU/mL for DNA targets | Not specified | Compound-specific, generally in ng/mL range |
| Throughput | High (~2000 samples/day) | Medium (Multiplexed in single run) | Medium to High |
| Key Strength | Full automation, minimized contamination | Multiplexing, high specificity for variants | Gold standard for specificity and metabolite detection |
Visualizing Experimental Workflows
The diagrams below illustrate the logical flow of key experimental protocols described in this guide.
Diagram 1: Molecular System Validation Workflow
Diagram 2: Targeted MS Assay Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
A successful experiment depends on the quality and appropriateness of its core components. This toolkit details essential materials for the featured methodologies.
Table 3: Key Research Reagent Solutions
| Item | Function & Role in Experimental Integrity |
|---|---|
| International Reference Standards (WHO IS) [22] | Provide a universally accepted benchmark for quantifying analyte concentration, ensuring accuracy and enabling cross-laboratory and cross-study comparability. |
| Stable Isotope-Labeled Internal Standards (SIS) [23] | Account for variability during sample preparation and MS analysis by behaving identically to the native analyte, thereby improving quantification accuracy and precision. |
| Characterized Patient Samples [22] [25] | Serve as the ground truth for validating assay concordance and specificity. A well-characterized panel covering the pathological range is crucial for a realistic performance assessment. |
| Negative Matrix (e.g., Normal Plasma) [22] | Used as a diluent for preparing calibration curves and for assessing assay specificity and potential background signal, establishing the baseline "noise" of the assay. |
| Certified Detection Kits & Reagents [22] | Assay-specific reagents (e.g., primers, probes, antibodies) whose lot-to-lot consistency is critical for maintaining the validated performance of the method over time. |
| GS-9901 | GS-9901, CAS:1640247-87-5, MF:C22H17ClFN9O, MW:477.9 g/mol |
| GSK2236805 | GSK2236805, CAS:1256390-53-0, MF:C42H52N8O8, MW:796.9 g/mol |
In the field of clinical laboratory science, the Clinical and Laboratory Standards Institute (CLSI) provides critical guidance for evaluating the performance of quantitative measurement procedures. For researchers conducting functional sensitivity with interassay precision profiles research, understanding the distinction between two key documents—EP05-A2 and EP15-A2—is fundamental to proper experimental design. These protocols establish standardized approaches for precision assessment, yet they serve distinctly different purposes within the method validation and verification workflow. EP05-A2, titled "Evaluation of Precision Performance of Quantitative Measurement Methods," is intended primarily for manufacturers and developers seeking to establish comprehensive precision claims for their diagnostic devices [26]. In contrast, EP15-A2, "User Verification of Performance for Precision and Trueness," provides a streamlined protocol for clinical laboratories to verify that a method's precision performance aligns with manufacturer claims before implementation in patient testing [18] [27].
The evolution of these guidelines reflects an ongoing effort to balance scientific rigor with practical implementation. Earlier editions of EP05 served both manufacturers and laboratory users, but the current scope has narrowed to focus primarily on manufacturers establishing performance claims [28] [29]. This change clarified the distinct needs of manufacturers creating claims versus laboratories verifying them, with EP15-A2 now positioned as the primary tool for end-user laboratories [28]. For research on functional sensitivity, which requires precise understanding of assay variation at low analyte concentrations, selecting the appropriate protocol is essential for generating reliable, defensible data.
Key Comparisons Between EP05-A2 and EP15-A2
The following table summarizes the fundamental differences between these two precision evaluation protocols:
| Feature | EP05-A2 | EP15-A2 |
|---|---|---|
| Primary Purpose | Establish precision performance claims [28] | Verify manufacturer's precision claims [18] |
| Intended Users | Manufacturers, developers [28] | Clinical laboratory users [18] |
| Experimental Duration | 20 days [30] | 5 days [30] [18] |
| Experimental Design | Duplicate analyses, two runs per day for 20 days [30] | Three replicates per day for 5 days [30] |
| Levels Tested | At least two concentrations [30] | At least two concentrations [30] |
| Statistical Power | Higher power to characterize precision [30] | Lower power, suited for verification [18] |
| Regulatory Status | FDA-recognized for establishing performance [28] | FDA-recognized for verification [18] [27] |
Beyond these operational differences, the conceptual framework of each protocol aligns with its distinct purpose. EP05-A2 employs a more comprehensive experimental design that captures more sources of variation over a longer period, resulting in robust precision estimates suitable for product labeling [30]. EP15-A2 utilizes a pragmatic verification approach that efficiently confirms the method operates as claimed without the resource investment of a full precision establishment [30] [18]. For researchers investigating functional sensitivity, this distinction is crucial—EP05-A2 would be appropriate when developing new assays or establishing performance at low concentrations, while EP15-A2 would suffice when verifying that an implemented method meets sensitivity requirements for clinical use.
Detailed Experimental Protocols
EP05-A2 Experimental Methodology
The EP05-A2 protocol employs a rigorous experimental design intended to comprehensively capture all potential sources of variation in a measurement procedure. The recommended approach requires testing at minimum two concentrations across the assay's measuring range, as precision often differs at various analytical levels [30]. The core design follows a "20 × 2 × 2" model: duplicate analyses in two separate runs per day over 20 days [30]. This extended timeframe is deliberate, allowing the experiment to incorporate typical operational variations encountered in routine practice, including different calibration events, reagent lots, operators, and environmental fluctuations.
Critical implementation requirements include maintaining at least a two-hour interval between runs within the same day to ensure distinct operating conditions [30]. Each run should include quality control materials different from those used for routine quality monitoring, and the test materials should be analyzed in a randomized order alongside at least ten patient samples to simulate realistic testing conditions [30]. This comprehensive approach generates approximately 80 data points per concentration level (20 days × 2 runs × 2 replicates), providing substantial statistical power for reliable precision estimation across multiple components of variation.
EP15-A2 Experimental Methodology
The EP15-A2 protocol employs a streamlined experimental design focused on practical verification rather than comprehensive characterization. The protocol requires testing at two concentration levels with three replicates per level over five days [30] [18]. This condensed timeframe makes the protocol feasible for clinical laboratories to implement while still capturing essential within-laboratory variation. The experiment generates 15 data points per concentration level (5 days × 3 replicates), sufficient for verifying manufacturer claims without the resource investment of a full EP05-A2 study.
A key feature of EP15-A2 is its statistical verification process. If the calculated repeatability and within-laboratory standard deviations are lower than the manufacturer's claims, verification is successfully demonstrated [30]. However, if the laboratory's estimates exceed the manufacturer's claims, additional statistical testing is required to determine whether the difference is statistically significant [30]. This approach acknowledges that limited verification studies have reduced power to definitively reject claims, protecting against false rejections of adequately performing methods while still identifying substantially deviant performance.
Statistical Analysis and Data Interpretation
Precision Component Calculations
Both EP05-A2 and EP15-A2 employ analysis of variance (ANOVA) techniques to partition total variation into its components, though the specific calculations differ slightly due to their different experimental designs. For EP15-A2, the key precision components are calculated as follows:
Repeatability (within-run precision) is estimated using the formula: [ sr = \sqrt{\frac{\sum{d=1}^D \sum{r=1}^n (x{dr} - \bar{x}d)^2}{D \cdot (n - 1)}} ] Where D is the total number of days, n is the number of replicates per day, (x{dr}) is the result for replicate r on day d, and (\bar{x}_d) is the average of all replicates on day d [30].
Within-laboratory precision (total precision) incorporates both within-run and between-day variation and is calculated as: [ sl = \sqrt{sr^2 + \frac{n \cdot sb^2}{n}} ] Where (sb^2) is the variance of the daily means [30].
For functional sensitivity research, typically defined as the analyte concentration at which the coefficient of variation (CV) reaches 20%, these precision components are particularly valuable. The CV, calculated as (CV = \frac{s}{\bar{x}} \times 100\%) where s is the standard deviation and (\bar{x}) is the mean, allows comparison of precision across concentration levels [30]. By establishing precision profiles across multiple concentrations, researchers can identify the functional sensitivity limit where imprecision becomes unacceptable for clinical use.
Data Evaluation and Acceptance Criteria
The evaluation approach differs significantly between the two protocols based on their distinct purposes. For EP05-A2, the resulting precision estimates are typically compared to internally defined quality goals or regulatory requirements appropriate for the intended use of the assay [28]. Since EP05-A2 is used to establish performance claims, the results directly inform product specifications and labeling.
For EP15-A2, verification is achieved through a two-tiered approach: if the laboratory's calculated repeatability and within-laboratory standard deviations are less than the manufacturer's claims, performance is considered verified [30]. If the laboratory's estimates exceed the manufacturer's claims, a statistical verification value is calculated using the formula: [ Verification\ Value = \sigmar \cdot \sqrt{\frac{C}{\nu}} ] Where (\sigmar) is the claimed repeatability, C is the 1-α/q percentage point of the Chi-square distribution, and ν is the degrees of freedom [30]. This approach provides statistical protection against incorrectly rejecting properly performing methods when using the less powerful verification protocol.
Experimental Workflow and Pathway
The following diagram illustrates the decision pathway for selecting and implementing the appropriate CLSI precision protocol:
Essential Research Reagent Solutions
The following table details key materials required for implementing CLSI precision protocols:
| Reagent/Material | Function in Precision Studies | Protocol Requirements |
|---|---|---|
| Pooled Patient Samples | Matrix-matched materials for biologically relevant precision assessment [30] | Preferred material for both EP05-A2 and EP15-A2 [30] |
| Quality Control Materials | Stable materials for monitoring assay performance over time [30] | Should be different from routine QC materials used for instrument monitoring [30] |
| Commercial Standard Materials | Materials with assigned values for trueness assessment [30] | Used when pooled patient samples are unavailable [30] |
| Calibrators | Materials used to establish the analytical measurement curve [30] | Should remain constant throughout the study when possible [30] |
| Patient Samples | Native specimens included to simulate routine testing conditions [30] | EP05-A2 recommends at least 10 patient samples per run [30] |
Application to Functional Sensitivity Research
For researchers investigating functional sensitivity with interassay precision profiles, both EP05-A2 and EP15-A2 provide methodological frameworks, though for different phases of assay development and implementation. Functional sensitivity, typically defined as the lowest analyte concentration at which an assay demonstrates a CV of 20% or less, requires precise characterization of assay imprecision across the measuring range, particularly at low concentrations.
The EP05-A2 protocol is ideally suited for establishing functional sensitivity during assay development or when validating completely new methods [28]. Its extended 20-day design comprehensively captures long-term sources of variation that significantly impact precision at low analyte concentrations. The robust dataset generated enables construction of precise interassay precision profiles that reliably demonstrate how CV changes with concentration, allowing accurate determination of the functional sensitivity limit.
The EP15-A2 protocol serves well for verifying that functional sensitivity claims provided by manufacturers are maintained in the user's laboratory setting [18]. While less powerful than EP05-A2 for establishing performance, its condensed 5-day design provides sufficient data to confirm that claimed sensitivity thresholds are met under local conditions. This verification is particularly important for assays measuring low-abundance analytes like hormones or tumor markers, where maintaining functional sensitivity is critical for clinical utility.
When designing functional sensitivity studies, researchers should consider that precision estimates from short-term EP15-A2 verification should not typically be used to set acceptability limits for internal quality control, for which longer-term assessment is recommended [30]. Additionally, materials selected for precision studies should ideally be pooled patient samples rather than commercial controls alone, as they better reflect the matrix effects encountered with clinical specimens [30].
In the context of verifying functional sensitivity with interassay precision profiles, assessing the precision of an analytical method is a fundamental step to confirm its suitability for use. Precision refers to the closeness of agreement between independent measurement results obtained under stipulated conditions and is solely related to random error, not to trueness or accuracy. A robust precision assessment is critical in fields like drug development and functional drug sensitivity testing (f-DST), where it helps personalize the choice among cytotoxic drugs and drug combinations for cancer patients by ensuring the reliability of the in-vitro diagnostic test methods [31].
A trivial approach to estimating repeatability (within-run precision) involves performing multiple replicate analyses in a single run. However, this method is insufficient as the operating conditions at that specific time may not reflect usual operating parameters, potentially leading to an underestimation of repeatability. Therefore, structured protocols that span multiple days and runs are essential for a realistic and accurate estimation of both repeatability and total within-laboratory precision [30].
Comparison of Experimental Protocols for Precision Verification
The Clinical and Laboratory Standards Institute (CLSI) provides two primary protocols for determining precision: EP05-A2 for validating a method against user requirements, and EP15-A2 for verifying that a laboratory's performance matches manufacturers' claims. The table below summarizes the core requirements of each protocol.
Table 1: Comparison of CLSI Precision Evaluation Protocols
| Feature | EP05-A2 Protocol (Method Validation) | EP15-A2 Protocol (Performance Verification) |
|---|---|---|
| Primary Purpose | Validate a method against user-defined requirements; often used by reagent/instrument suppliers [30]. | Verify that a laboratory's performance is consistent with manufacturer claims [30]. |
| Recommended Use | For in-house developed methods requiring a higher level of proof [30]. | For verifying methods on automated platforms using manufacturer's reagents [30]. |
| Testing Levels | At least two levels, as precision can differ over the analytical range [30]. | At least two levels [30]. |
| Experimental Design | Each level run in duplicate, with two runs per day over 20 days (minimum 2 hours between runs) [30]. | Each level run with three replicates over five days [30]. |
| Additional Samples | Include at least ten patient samples in each run to simulate actual operation [30]. | Not specified in the provided results. |
| Data Review | Data must be assessed for outliers [30]. | Data must be assessed for outliers [30]. |
Detailed Experimental Methodology
Core Protocol for Multi-Day, Multi-Run Replicates
The following workflow details the general procedure for conducting a multi-day precision study, which forms the basis for both EP05-A2 and EP15-A2 protocols.
Data Analysis and Calculation Procedures
After data collection, the following statistical calculations are performed to derive estimates of precision. The formulas for calculating repeatability (Sr) and within-laboratory precision (Sl) are based on analysis of variance (ANOVA) components [30].
Table 2: Formulas for Calculating Precision Metrics
| Metric | Formula | Description |
|---|---|---|
| Repeatability (Sr) | ( sr = \sqrt{\frac{\sum{d=1}^{D} \sum{r=1}^{n} (x{dr} - \bar{x}_d)^2}{D(n-1)}} ) | Estimates the within-run standard deviation. Here, (D) is the total days, (n) is replicates per day, (x{dr}) is result for replicate (r) on day (d), and (\bar{x}d) is the average for day (d) [30]. |
| Variance of Daily Means (s₆²) | ( sb^2 = \frac{\sum{d=1}^{D} (\bar{x}_d - \bar{\bar{x}})^2}{D-1} ) | Estimates the between-run variance. Here, (\bar{\bar{x}}) is the overall average of all results [30]. |
| Within-Lab Precision (Sl) | ( sl = \sqrt{sr^2 + s_b^2} ) | Estimates the total standard deviation within the laboratory, combining within-run and between-run components [30]. |
The data analysis process, from raw data to final verification, can be visualized as the following logical pathway:
Quantitative Data and Results Comparison
The application of these protocols and calculations yields concrete data for comparing performance. The following table presents a summary of hypothetical experimental data collected for calcium according to an EP15-A2-like protocol, showing the results from three replicates over five days for a single level [30].
Table 3: Example Experimental Data and Precision Calculations for Calcium
| Day | Replicate 1 (mmol/L) | Replicate 2 (mmol/L) | Replicate 3 (mmol/L) | Daily Mean (x̄d) |
|---|---|---|---|---|
| 1 | 2.015 | 2.013 | 1.963 | 1.997 |
| 2 | 2.019 | 2.002 | 1.979 | 2.000 |
| 3 | 2.025 | 1.959 | 2.000 | 1.995 |
| 4 | 1.972 | 1.950 | 1.973 | 1.965 |
| 5 | 1.981 | 1.956 | 1.957 | 1.965 |
| Overall Mean (x̿) | 1.984 |
Calculated Precision Metrics from this Dataset [30]:
- Repeatability (Sr): 0.023 mmol/L
- Within-Laboratory Precision (Sl): 0.027 mmol/L
When the estimated repeatability (e.g., 0.023 mmol/L) is greater than the manufacturer's claimed value, a statistical test is required to determine if the difference is significant. This involves calculating a verification value. If the estimated repeatability is less than the claimed value, precision is considered consistent with the claim [30].
The Scientist's Toolkit: Research Reagent Solutions
The successful execution of precision studies, particularly in advanced fields like functional drug sensitivity testing (f-DST), relies on specific materials and reagents.
Table 4: Essential Materials for Precision Studies and Functional Testing
| Item | Function |
|---|---|
| Pooled Patient Samples | Serves as a test material with a matrix closely resembling real patient specimens; used to assess precision under realistic conditions [30]. |
| Quality Control (QC) Materials | Used to monitor the stability and performance of the assay during the precision study; should be different from the routine QC used for instrument control [30]. |
| Cytotoxic Agents | Drugs like 5-FU, oxaliplatin, and irinotecan; used in f-DST to expose patient-derived cancer tissue to measure individual vulnerability and therapy response [31]. |
| Stem Cell Media | Used in f-DST to culture and expand processed cancer specimens (e.g., organoids, tumoroids) into a sufficient number of testable cell aggregates [31]. |
| Commercial Standard Material | Provides a known value for validation and calibration, helping to ensure the accuracy of measurements throughout the precision assessment [30]. |
| GSK5852 | GSK5852, CAS:1331942-30-3, MF:C27H25BF2N2O6S, MW:554.4 g/mol |
| GSK2838232 | GSK2838232, CAS:1443460-91-0, MF:C48H73ClN2O6, MW:809.6 g/mol |
Calculating Interassay Precision (%CV) and Plotting the Precision Profile
In the rigorous field of analytical method validation, demonstrating that an assay is reproducible over time is paramount. Interassay precision, also referred to as intermediate precision, quantifies the variation in results when an assay is performed under conditions that change within a laboratory, such as different days, different analysts, or different equipment [8]. It is a critical component for verifying the functional sensitivity and reliability of an assay throughout its lifecycle.
The most common statistical measure for expressing this precision is the percent coefficient of variation (%CV), a dimensionless ratio that standardizes variability relative to the mean, allowing for comparison across different assays and concentration levels [32]. It is calculated as:
%CV = (Standard Deviation / Mean) × 100% [32] [33]
The precision profile is a powerful graphical representation that plots the %CV of an assay against the analyte concentration. This visual tool is fundamental to research on functional sensitivity, as it helps identify the concentration range over which an assay delivers acceptable, reliable precision, thereby defining its practical limits of quantification [8].
This guide will objectively compare the performance of different analytical platforms by providing standardized protocols and presenting experimental data for calculating interassay %CV and constructing precision profiles.
Experimental Protocols for Determining Interassay Precision
A standardized methodology is essential for generating robust and comparable interassay precision data. The following protocol outlines the key steps.
Core Experimental Workflow
The general process for evaluating interassay precision involves repeated testing of samples across multiple independent assay runs.
Detailed Methodology
The workflow above is implemented through the following specific procedures:
Experimental Design: Prepare a set of samples spanning the expected concentration range of the assay, including quality control (QC) samples at low, medium, and high concentrations. The experiment should be designed to include a minimum of three independent assay runs conducted by two different analysts over several days [8] [34]. Each sample should be tested in replicates (e.g., n=3) within each run.
Assay Execution: For each independent run (representing one assay event), process all samples and QCs according to the standard operating procedure. Adherence to consistent technique is critical to minimize introduced variability. Key considerations include:
- Pipetting: Use calibrated pipettes and proper technique (e.g., pre-wetting tips, holding pipettes vertically) to ensure accuracy [32].
- Washing: Optimize and maintain a consistent wash protocol. Overly aggressive or inconsistent washing is a common source of high %CV [33].
- Incubation: Keep plates covered and in a stable environment away from drafts to prevent well drying and ensure even temperature distribution [32].
- Instrumentation: Use calibrated plate readers and ensure appropriate software settings. Checking instrument performance with empty wells or a non-adsorbing liquid can diagnose background noise issues [33].
Data Collection and Analysis: For each sample across the multiple assay runs, collect the raw measurement data (e.g., Optical Density for ELISA) or the calculated concentration.
- Calculate the Mean (µ) and Standard Deviation (σ): Compute these values for each sample using the results gathered from all independent runs.
- Compute %CV: For each sample, apply the formula: %CV = (σ / µ) × 100% [32].
Comparative Performance Data
Presenting data in a clear, structured format is key for objective comparison. The following tables summarize typical acceptance criteria and example experimental data from different assay platforms.
Interassay Precision Acceptance Criteria
Table 1: General guidelines for acceptable %CV levels in bioanalytical assays.
| Assay Type | Target Interassay %CV | Regulatory Context |
|---|---|---|
| Immunoassays (e.g., ELISA) | < 15% | Common benchmark for plate-to-plate consistency [32] [33] |
| Cell-Based Potency Assays | ≤ 20% | Demonstrates minimal variability in complex biological systems [34] |
| Chromatographic Methods (HPLC) | Varies by level | Based on validation guidelines; typically stricter for active ingredients [8] |
Example Experimental Data
Table 2: Example interassay precision data from an impedance-based cytotoxicity assay (Maestro Z platform) measuring % cytolysis at different Effector to Target (E:T) ratios. Data adapted from a validation study [34].
| E:T Ratio | Mean % Cytolysis | Standard Deviation | %CV |
|---|---|---|---|
| 10:1 | ~80% | To be calculated | < 20% |
| 5:1 | To be reported | To be calculated | < 20% |
| 5:2 | To be reported | To be calculated | < 20% |
| 5:4 | To be reported | To be calculated | < 20% |
Table 3: Simulated interassay precision data for a quantitative ELISA measuring a protein analyte, demonstrating the dependence of %CV on concentration.
| Sample / QC Level | Mean Concentration (ng/mL) | Standard Deviation (ng/mL) | %CV |
|---|---|---|---|
| Low QC | 5.0 | 0.8 | 16.0% |
| Mid QC | 50.0 | 4.0 | 8.0% |
| High QC | 150.0 | 10.5 | 7.0% |
| Calibrator A | 2.0 | 0.5 | 25.0% |
Constructing and Interpreting the Precision Profile
The precision profile transforms the tabulated %CV data into a visual tool that defines the usable range of an assay.
Workflow for Precision Profile
The process of building the profile involves specific data transformation and visualization steps.
Interpretation for Functional Sensitivity
The precision profile visually demonstrates a key principle: %CV is often concentration-dependent. As shown in the simulated ELISA data (Table 3), variability is typically higher at lower concentrations, where the signal-to-noise ratio is less favorable [8].
- Defining the Working Range: The profile plots the calculated %CV for each sample against its mean concentration. A regression curve is often fitted to these points. The functional sensitivity of the assay is frequently defined as the lowest concentration at which the curve intersects a predefined %CV acceptance threshold (e.g., 20%) [34]. Concentrations above this point are considered to be within the reliable quantitative range of the assay.
- Comparative Tool: When comparing assay platforms, a precision profile that maintains a lower %CV across a wider concentration range indicates a more robust and sensitive method. For instance, a well-validated impedance-based assay can show %CVs below 20% across all tested conditions, confirming its suitability for potency assessment [34].
The Scientist's Toolkit: Essential Reagents and Materials
Table 4: Key research reagent solutions and materials essential for conducting interassay precision studies.
| Item | Function / Application |
|---|---|
| Calibrated Pipettes | Ensures accurate and precise liquid handling; regular calibration is critical to minimize technical variability [32] [33]. |
| Quality Control (QC) Samples | Stable, well-characterized samples at known concentrations used to monitor assay performance and precision across runs [8]. |
| Cell-Based Assay Platform (e.g., Maestro Z) | Impedance-based system for label-free, real-time monitoring of cell behavior (e.g., cytotoxicity), used in advanced potency assay validation [34]. |
| CD40 Antibody Tethering Solution | Used in specific cell-based assays to anchor non-adherent target cells (e.g., Raji lymphoblast cells) to the well surface for impedance measurement [34]. |
| Precision Plates (e.g., CytoView-Z 96-well) | Specialized microplates with embedded electrodes for use in impedance-based systems [34]. |
| Plate Washer (Optimized) | Automated or manual system for consistent and gentle washing of ELISA plates; overly aggressive washing is a common source of high %CV [33]. |
In regulated bioanalysis, the Lower Limit of Quantification (LLOQ) represents the lowest concentration of an analyte that can be quantitatively determined with acceptable precision and accuracy. The Coefficient of Variation (CV%) acceptance criterion, commonly set at 20% for the LLOQ, is not an arbitrary choice but a scientifically and clinically grounded benchmark that defines the boundary of reliable quantification [35]. This concept is intrinsically linked to functional sensitivity, which extends beyond mere detection to define the lowest concentration at which an assay can deliver clinically useful results with consistent precision over time [1].
The establishment of a robust LLOQ is fundamental to data integrity across non-clinical and clinical studies, directly impacting the assessment of pharmacokinetics, bioavailability, and toxicokinetics [35]. This guide examines the experimental approaches, comparative performance, and practical implementation of CV acceptance criteria for establishing a reliable LLOQ that meets both scientific and regulatory standards.
Conceptual Foundation: Analytical vs. Functional Sensitivity
Understanding the distinction between different sensitivity measures is crucial for proper LLOQ establishment:
Analytical Sensitivity (Detection Limit): The lowest concentration that can be distinguished from background noise, typically determined by assaying replicates of a zero-concentration sample and calculating the concentration equivalent to the mean signal plus (for immunometric assays) or minus (for competitive assays) 2 standard deviations (SD) [1]. While this represents the assay's fundamental detection capability, it often lacks the precision required for clinical utility.
Functional Sensitivity: Originally developed for TSH assays, functional sensitivity is defined as "the lowest concentration at which an assay can report clinically useful results," characterized by good accuracy and a day-to-day interassay CV of 20% or less [1]. This concept addresses the critical limitation of analytical sensitivity by incorporating reproducibility into the performance equation, ensuring results are not just detectable but also clinically actionable.
The Practical Impact: A concentration might be detectable (above analytical sensitivity) but show such poor reproducibility that results like 0.4 µg/dL and 0.7 µg/dL cannot be reliably distinguished. Functional sensitivity ensures that results reported above the LLOQ are sufficiently precise for clinical decision-making [1].
Experimental Protocols for Establishing LLOQ
Core Protocol for Determining Functional Sensitivity (LLOQ)
The following methodology provides a robust framework for establishing the functional sensitivity of an assay, thereby defining its LLOQ.
Objective: To determine the lowest analyte concentration that can be measured with an interassay CV ≤ 20%, establishing the functional sensitivity of the method [1].
Materials & Reagents:
- Matrix-Matched Samples: Use true zero-concentration sample in the appropriate biological matrix (e.g., plasma, serum) [1].
- Calibrator Stock Solutions: Reference standard of known purity and stability [35].
- Quality Controls (QCs): Freshly prepared or pre-qualified frozen QCs at concentrations bracketing the expected LLOQ [36].
- Assay Reagents: All necessary antibodies, conjugates, buffers, and substrates specific to the assay format (e.g., ELISA, HPLC-MS/MS) [37].
Procedure:
- Sample Preparation: Prepare a series of samples (at least 5-6 concentrations) at low levels spanning the expected range of functional sensitivity. Ideally, use undiluted patient samples or patient pools. If unavailable, drug-free matrix samples spiked with the analyte are acceptable [1].
- Repeated Analysis: Analyze each sample repeatedly over a minimum of 6 different analytical runs, ideally conducted over several days or weeks by different analysts. This is critical for assessing day-to-day (interassay) precision [1]. A single run with multiple replicates is insufficient [1].
- Data Collection: Record the measured concentration for each replicate of every sample across all runs.
Data Analysis:
- For each concentration level, calculate the mean and standard deviation (SD) of all measurements across all runs.
- Compute the interassay CV% for each level using the formula: CV% = (SD / Mean) × 100.
- Plot the CV% against the mean concentration for each level. The functional sensitivity (LLOQ) is the lowest concentration at which the CV reaches the predetermined limit (e.g., 20%) [1]. This can be estimated by interpolation if it falls between tested levels.
Protocol for LLOQ Verification During Bioanalytical Method Validation
For formal method validation, the FDA guidance and bioanalytical consensus conferences recommend a specific approach to verify the LLOQ [35].
Objective: To verify that the LLOQ standard on the calibration curve meets predefined acceptance criteria for precision and accuracy during method validation [35].
Procedure:
- Calibration Curve: Construct a calibration curve using a minimum of 6-8 standards, including the proposed LLOQ, in the relevant biological matrix [35].
- LLOQ Assessment: Analyze a minimum of five determinations of the LLOQ sample [35].
- Signal Assessment: Confirm the analyte response at the LLOQ is at least five times the response of the blank (signal-to-noise ratio, S/N ≥ 5) [35].
- Precision and Accuracy: The LLOQ must demonstrate a precision of ±20% (CV%) and an accuracy of 80-120% [35].
Comparative Performance Data
The following tables summarize key acceptance criteria and intermethod performance data relevant to LLOQ establishment.
Table 1: Acceptance Criteria for Bioanalytical Method Validation (Small Molecules)
| Parameter | Acceptance Criteria | Context & Notes |
|---|---|---|
| LLOQ Precision (CV%) | ±20% | Applies to the lowest standard on the calibration curve [35]. |
| LLOQ Accuracy | 80–120% | Back-calculated concentration of the LLOQ standard [35]. |
| Dynamic Range Precision | ±15% | Applies to all standards above the LLOQ [35]. |
| Signal-to-Noise (LLOQ) | ≥ 5:1 | The analyte response should be at least five times the blank response [35]. |
| Quality Controls (QC) | ±15–20% | QCs (low, medium, high) during sample analysis; ±20% often applied at LLOQ-level QC [36]. |
Table 2: Intermethod Differences in Functional Sensitivity (Based on TSH Assay Study)
| Assay Generation | Stated Functional Sensitivity | Observed Performance in Clinical Labs | Impact on Diagnostic Accuracy |
|---|---|---|---|
| Third-Generation | 0.01 – 0.02 µIU/mL | Manufacturer's stated limit was rarely duplicated in clinical practice [38]. | Better pool rankings and fewer misclassifications of low-TSH sera as "normal" [38]. |
| Second-Generation | 0.1 – 0.2 µIU/mL | Performance variability and loss of specificity observed with some methods [38]. | Higher rate of misclassifying subnormal TSH values as normal, reducing cost-effectiveness [38]. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful LLOQ determination relies on high-quality materials and reagents. The following table details key solutions required for these experiments.
Table 3: Key Research Reagent Solutions for LLOQ Experiments
| Reagent/Material | Function & Importance | Critical Considerations |
|---|---|---|
| Reference Standard | The purified analyte of known identity and potency used to prepare calibrators. | Essential for accurate preparation of calibrators and QCs; purity and stability must be documented [35]. |
| Biological Matrix | The biological fluid (e.g., plasma, serum) that matches the study samples. | Critical for preparing matrix-matched standards and QCs to account for matrix effects [35]. A true zero sample is needed for analytical sensitivity [1]. |
| Quality Controls (QCs) | Independent samples of known concentration used to monitor assay performance. | Should be prepared, verified, and frozen to mimic study sample handling. Acceptance criteria for preparation should be stringent (e.g., ±10%) [36]. |
| Assay-Specific Antibodies/Reagents | Key binding reagents (e.g., capture/detection antibodies for ELISA). | Lot-to-lot consistency is vital for maintaining the established LLOQ and precision profile [37]. |
| Matrix Blank | A sample of the biological matrix without the analyte. | Used to confirm the absence of interference in the matrix and to assess background signal for S/N calculations [35]. |
Troubleshooting and Optimization Strategies
Even with a sound protocol, achieving a precise and robust LLOQ can present challenges. Here are common issues and their solutions:
High Imprecision at Low Concentrations:
Inability to Reach Target CV ≤ 20%:
- Cause: The assay's inherent imprecision may be too high at the desired concentration.
- Solution: Re-optimize critical assay parameters (e.g., incubation times, antibody concentrations). If re-optimization fails, report a higher, practically achievable LLOQ that meets the CV criterion, as this reflects the true functional sensitivity [1].
Discrepancy Between Labs:
- Cause: As highlighted in TSH assay studies, a manufacturer's stated functional sensitivity is often not duplicated in clinical labs due to differences in operators, equipment, and reagents [38].
- Solution: Each laboratory should independently verify or establish the functional sensitivity of an assay using a clinically relevant protocol with their own instrumentation and personnel [38].
Establishing the LLOQ with a 20% CV acceptance criterion is a foundational practice that bridges analytical capability and clinical utility. Moving beyond the theoretical "detection limit" to the practical "functional sensitivity" ensures that reported data are both reliable and meaningful for decision-making in drug development and diagnostics. By employing the experimental protocols, validation criteria, and troubleshooting strategies outlined in this guide, researchers can confidently set a robust LLOQ, ensuring the integrity of data generated from their bioanalytical methods.
Identifying and Resolving Common Pitfalls in Precision Testing and Sensitivity Verification
For researchers and scientists in drug development, analytical precision is a cornerstone of reliable data. Within the critical context of verifying functional sensitivity with interassay precision profiles, diagnosing the root causes of poor precision is paramount. Functional sensitivity, typically defined as the analyte concentration at which interassay precision meets a specific threshold (often a 20% coefficient of variation), is a key metric for determining the lowest measurable concentration of an assay with acceptable reproducibility. Poor precision directly compromises the accurate determination of this parameter, potentially leading to incorrect conclusions in pharmacokinetic studies, biomarker discovery, and therapeutic drug monitoring. This guide objectively compares common sources of imprecision—technical, reagent, and instrumental—and provides the experimental protocols to identify and address them.
Understanding Precision in the Laboratory
In experimentation, precision refers to the reproducibility of results, or the closeness of agreement between independent measurements obtained under stipulated conditions. It is solely related to random error and is distinct from accuracy, which denotes closeness to the true value [30] [39]. Precision is typically measured and expressed as the standard deviation (SD) or the coefficient of variation (CV), which is the standard deviation expressed as a percentage of the mean [30]. A lower CV indicates higher, more desirable precision.
When validating an assay, it is essential to assess both repeatability (within-run precision) and within-laboratory precision (total precision across multiple runs and days) [30]. This comprehensive assessment is fundamental for establishing reliable interassay precision profiles, which plot precision (CV) against analyte concentration and are used to determine functional sensitivity [11].
A Framework of Common Causes and Solutions
Poor precision can stem from a variety of interconnected factors. The table below summarizes the primary technical, reagent, and instrumental causes and their corresponding mitigation strategies.
Table 1: Common Causes of Poor Precision and Recommended Solutions
| Category | Specific Cause | Impact on Precision | Recommended Solution |
|---|---|---|---|
| Technical | Inconsistent wet chemical sample preparation [40] | High variability due to manual handling errors. | Automate sample preparation; follow strict, documented protocols [40]. |
| Inadequate analyst training & expertise [40] | Introduces operator-dependent variability. | Invest in comprehensive training and ongoing professional development [40]. | |
| Suboptimal data analysis model selection [41] | Poor parameter estimation and fit for bounded data. | Use bounded integer (BI) models for composite scale data instead of standard continuous variable models [41]. | |
| Reagent | Low purity grade reagents [40] | Contamination leads to high background and variable results. | Use high-purity grade reagents with low background levels of the analyte [40]. |
| Improper reagent storage and handling [40] | Degradation over time causes reagent instability. | Utilize dedicated storage and monitor expiration dates; avoid cross-contamination [40]. | |
| Lot-to-lot variability of reagents [11] | Shifts in calibration and assay response between lots. | Conduct thorough verification of new reagent lots against the previous lot [11]. | |
| Instrumental | Improper instrument calibration [40] | Drift over time or incorrect standards cause systematic and random error. | Perform regular calibration using appropriate, properly prepared standards [40]. |
| Lack of proactive maintenance [40] | Deterioration of instrument components increases noise. | Implement a proactive maintenance schedule with the manufacturer or supplier [40]. | |
| Variable environmental conditions [40] | Temperature, humidity, and pressure fluctuations affect instrument performance. | Monitor and maintain stable, clean laboratory conditions [40]. |
Experimental Protocols for Precision Verification
Adhering to standardized protocols is critical for a robust assessment of precision. The following methodologies, derived from CLSI guidelines, are essential for diagnosing imprecision and verifying manufacturer claims.
CLSI EP05-A2 Protocol for Precision Validation
The EP05-A2 protocol is used to validate a method against user-defined precision requirements and is typically employed by reagent and instrument suppliers [30].
- Objective: To comprehensively estimate repeatability and within-laboratory precision.
- Procedure:
- Perform the assessment on at least two concentration levels (e.g., low and high) as precision can differ across the analytical range.
- For each level, run samples in duplicate.
- Conduct two runs per day, separated by at least two hours.
- Repeat this process over 20 days.
- Include at least ten patient samples in each run to simulate actual operation.
- Change the order of analysis of test materials and quality control (QC) each day.
- Data Analysis: Use analysis of variance (ANOVA) to separate and calculate the variance components for repeatability (within-run) and within-laboratory precision (total). The repeatability SD ((sr)) is derived from the within-run variability, while the within-laboratory SD ((sl)) is calculated by combining within-run and between-run variances: (sl = \sqrt{sb^2 + \frac{sr^2}{n}}), where (sb^2) is the variance of the daily means and (n) is the number of replicates per day [30].
CLSI EP15-A2 Protocol for Precision Verification
The EP15-A2 protocol is designed for laboratories to verify that a method's precision is consistent with the manufacturer's claims [30].
- Objective: To verify manufacturer-stated repeatability and within-laboratory precision with a simpler experiment.
- Procedure:
- Test at least two concentration levels.
- For each level, run three replicates per day.
- Repeat this process over five days.
- Data Analysis: Calculate repeatability and within-laboratory precision as in the EP05-A2 protocol. Compare the estimated values to the manufacturer's claims. If the verified values are lower, the method is acceptable. If they are higher, a statistical test must be performed to check if the difference is significant. The verification value can be calculated as: ( \text{Verification Value} = \sigmar \cdot \sqrt{\frac{C}{v}} ), where ( \sigmar ) is the claimed repeatability, ( C ) is the chi-square value, and ( v ) is the degrees of freedom [30].
Table 2: Key Experimental Parameters for CLSI Precision Protocols
| Protocol | Purpose | Levels | Replicates per Run | Runs per Day | Duration | Statistical Output |
|---|---|---|---|---|---|---|
| EP05-A2 | Full precision validation | At least 2 | 2 | 2 | 20 days | Repeatability SD, Within-lab SD |
| EP15-A2 | Manufacturer claim verification | At least 2 | 3 | 1 | 5 days | Verified Repeatability, Verified Within-lab SD |
Establishing the Link to Functional Sensitivity
The interassay precision profile is a direct tool for determining an assay's functional sensitivity. The process involves measuring precision at progressively lower analyte concentrations to find the limit of quantitation (LoQ).
- Protocol for Functional Sensitivity (LoQ) Verification:
- Prepare a series of serum samples with concentrations at multiples of the limit of detection (LoD) (e.g., 1x, 2x, 3x LoD) [11].
- Analyze these samples using a single reagent batch. Test each sample multiple times per day (e.g., five times) over several days (e.g., three consecutive days) [11].
- For each concentration level, calculate the mean, standard deviation, and precision (CV).
- Generate a precision curve by plotting the CV against the analyte concentration.
- The functional sensitivity, or LoQ, is defined as the lowest analyte concentration that can be measured with an interassay precision (CV) of 20% (or another pre-defined threshold, such as 10%) [11]. This is determined directly from the precision curve.
This workflow directly connects the assessment of interassay precision to a key assay performance metric, underscoring why diagnosing poor precision is a prerequisite for defining an assay's reliable working range.
Precision Diagnosis and Functional Sensitivity Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials crucial for conducting precision experiments and troubleshooting.
Table 3: Essential Research Reagent Solutions for Precision Analysis
| Item | Function in Precision Analysis | Critical Consideration |
|---|---|---|
| Pooled Patient Samples | Used as test material for precision protocols; provides a biologically relevant matrix [30]. | Should be different from quality control materials used for routine instrument control [30]. |
| Quality Control (QC) Materials | Monitors assay performance and stability during precision experiments [30]. | Use at multiple levels (e.g., low, medium, high); different from test materials [30]. |
| High-Purity Calibration Standards | Used for regular instrument calibration to ensure accurate and precise readings [40]. | Must be properly prepared and stabilized; incorrect standards cause calibration errors [40]. |
| High-Purity Reagents & Acids | Used in sample preparation (e.g., digestion, oxidation) and assay workflows [40]. | Low purity grades can introduce contamination, increasing background noise and variability [40]. |
| Appropriate Glassware | Used for sample preparation, storage, and measurement (e.g., volumetric flasks, pipettes) [39]. | Must be clean and dedicated to mercury analysis to prevent cross-contamination [40]. Use volumetric pipettes for precise transfers [39]. |
Comparative Analysis of Diagnostic Strategies
The choice of diagnostic strategy can significantly impact the perceived precision and functional sensitivity of an assay, especially in clinical applications. The following table compares different diagnostic approaches for a single analyte, high-sensitivity cardiac troponin I (hs-cTnI), highlighting the inherent trade-offs between sensitivity and positive predictive value.
Table 4: Comparison of Four Diagnostic Strategies for hs-cTnI in NSTEMI Rule-Out [11]
| Diagnostic Strategy | Principle | Sensitivity | Positive Predictive Value (PPV) | Overall F1-Score |
|---|---|---|---|---|
| Limit of Detection (LoD) | Rule-out if admission hs-cTnI (0h) < 2 ng/L [11]. | 100% | 14.0% | Not Reported |
| Single Cut-off | Rule-out if hs-cTnI (0h) < the 99th percentile URL [11]. | Lower than LoD Strategy | Higher than LoD Strategy | Not Reported |
| 0/1-Hour Algorithm | Combines baseline hs-cTnI and absolute change after 1 hour [11]. | High | High | High |
| 0/2-Hour Algorithm | Combines baseline hs-cTnI and absolute change after 2 hours [11]. | 93.3% | Not Explicitly Stated | 73.68% |
This comparison illustrates that a method with seemingly perfect sensitivity (LoD strategy) may have unacceptably low precision in its diagnostic prediction (low PPV). The more complex algorithms (0/1h and 0/2h), which incorporate precision over time (delta values), provide a more balanced and clinically useful performance, as reflected in the higher F1-score [11].
Interassay Precision Profile Concept
Diagnosing poor precision requires a systematic approach that investigates technical, reagent, and instrumental factors. By employing standardized experimental protocols like CLSI EP05-A2 and EP15-A2, researchers can not only pinpoint sources of imprecision but also generate the essential interassay precision profiles needed to verify an assay's functional sensitivity. This rigorous process ensures that data generated in drug development is reliable, reproducible, and fit for purpose, ultimately supporting robust scientific conclusions and regulatory decision-making.
In the pursuit of reliable scientific data, particularly in verifying functional sensitivity with interassay precision profiles, three technical pillars form the foundation of robust results: pipetting technique, sample pre-treatment, and reagent stability. Functional sensitivity, defined as the lowest analyte concentration that can be measured with an interassay precision of ≤20% CV (Coefficient of Variation), is a critical metric for assessing assay performance in low-concentration ranges [1]. Variations in manual pipetting introduce an often unquantified source of error that can compromise the precision profiles used to establish this sensitivity [42]. Simultaneously, optimized sample pre-treatment protocols are essential for ensuring efficient analyte recovery and minimizing matrix effects, directly impacting the accuracy of low-level measurements [43]. Furthermore, the stability of critical reagents governs the consistency of assay performance over time, a non-negotiable requirement for generating reproducible interassay precision data [44] [45]. This guide provides a systematic comparison of optimization strategies across these three domains, offering experimental protocols and data-driven insights to enhance the reliability of your bioanalytical methods.
Pipetting Technique: Mastering the Fundamentals of Liquid Handling
Assessing and Minimizing Pipetting Variation
Pipetting is a ubiquitous yet potential source of significant analytical variation. Understanding and controlling this variation is paramount when characterizing an assay's functional sensitivity, where imprecision must be rigorously quantified. The two most common methods for assessing pipetting performance are gravimetry and spectrophotometry [42].
Gravimetric Method: This approach measures the mass of a dispensed liquid, most commonly water, to determine both accuracy (closeness to the expected value) and precision (coefficient of variation of replicate measurements) [42]. The protocol involves:
- Setting Up: Use an analytical balance, pre-conditioned tips, and the liquid to be tested in a controlled environment.
- Taking Measurements: Dispense the target volume into a weighing boat multiple times (e.g., n=10), recording the mass for each dispense.
- Calculating Results: Calculate the average mass, convert to volume using the liquid's density, and compare to the target for accuracy. Precision is expressed as the CV% of the replicate volumes. This method is highly sensitive to environmental factors like temperature and humidity, and the balance's inherent error must be factored in, especially for low volumes [42].
Spectrophotometric Method: This method uses a dye solution, and the absorbance of the pipetted dye is measured to determine the dispensed volume. It offers higher throughput and is particularly suitable for testing multi-channel pipettes [42].
Table 1: Comparison of Common Pipetting Assessment Methods
| Method | Readout | Throughput | Best For | Key Limitations |
|---|---|---|---|---|
| Gravimetry | Mass (converted to volume) | Low | Training; testing diverse liquid types (viscous, volatile) | Affected by environment; tedious for multi-channel pipettes [42] |
| Spectrophotometry | Absorbance (converted to volume) | High | Routine checks; multi-channel pipettes | Limited to compatible liquids [42] |
Manual, Semi-Automated, and Automated Pipetting Systems
The choice of liquid handling technology directly impacts throughput, reproducibility, and ergonomics. The optimal system depends on the number of samples, required throughput, and the need for walk-away automation [46].
Table 2: Comparison of Liquid Handling Technologies
| Parameter | Manual Pipetting | Semi-Automated Pipetting | Automated Pipetting |
|---|---|---|---|
| Number of Samples | Small (< 10) | Medium (10 - 100) | High (> 100) |
| Throughput | Up to 10 samples/hour | Up to 100 samples/hour | More than 100 samples/hour |
| Reproducibility | Low (subject to human technique) | High | High |
| RSI Risk | Yes | Potentially | No |
| Labor Costs | High | Moderate | Low |
| Best Use Case | Simple, low-throughput applications | Repetitive protocols requiring high reproducibility | High-throughput screening; full walk-away automation [46] |
Pipetting Technology: Air Displacement, Positive Displacement, and Acoustic Energy
Different liquid classes require different pipetting technologies to maintain accuracy, especially at low volumes critical for functional sensitivity determination.
- Air Displacement Pipettes: These are the most common type, using an air cushion to move liquid. They are highly accurate for standard aqueous solutions above 2 µL but are challenged by volatile, viscous, or hot/cold liquids due to the compressibility of the air cushion [42] [46].
- Positive Displacement Pipettes: These systems use a piston that makes direct contact with the liquid, making them agnostic to liquid properties like viscosity and vapor pressure. They are essential for accurate pipetting of sub-microliter volumes of challenging liquids and eliminate the risk of cross-contamination when used with disposable tips [42] [46].
- Acoustic Technology: This non-contact method uses sound energy to transfer nanoliter-sized droplets. It is a go-to method for low-volume reagent dispensing and assay miniaturization, with built-in droplet verification. However, it is less suitable for larger volumes or in-well mixing [46].
Sample Pre-treatment: Optimizing Analyte Recovery and Stability
A Protocol for Rapid and Sensitive Hair Analysis
An optimized sample pre-treatment protocol is illustrated by a validated method for quantifying cocaine and its metabolites in hair using GC-MS/MS [43]. This protocol ensures efficient analyte extraction and purification, which is critical for achieving a low limit of quantification (LOQ) of 0.01 ng/mg.
Detailed Experimental Protocol [43]:
- Decontamination: Hair samples are washed with three subsequent dichloromethane washes to remove external contaminants.
- Incubation and Stabilization: Samples are incubated for one hour with a specialized M3 buffer to promote analyte solubilization and stabilization.
- Extraction: The extracts are purified using Solid-Phase Extraction (SPE).
- Derivatization: The purified extracts are chemically derivatized to improve their volatility and detection characteristics for GC-MS/MS analysis.
- Analysis: Extracts are injected into the GC-MS/MS system operating in Multiple Reaction Monitoring (MRM) mode, monitoring characteristic ion transitions for high sensitivity and selectivity.
Performance Data: The method was validated showing linearity from the LLOQ to 10 ng/mg for cocaine and its metabolites. Intra-assay and inter-assay precision were <15%, and accuracy was within ±6.6%, demonstrating the robustness required for reliable low-level detection [43].
Reagent Stability: Ensuring Consistent Assay Performance Over Time
The Critical Role of Reagent Management
Critical reagents, such as antibodies, binding proteins, and conjugated antibodies, are biological entities whose properties can change over time, directly impacting the accuracy and precision of an assay [44] [47]. For functional sensitivity, which is determined from interassay precision profiles, consistent reagent performance across multiple runs and over long durations is absolutely essential. A well-defined critical reagent management strategy is needed to characterize these reagents, monitor their stability, and manage lot-to-lot changes [44] [47]. Best practices include:
- Early Characterization: Define physico-chemical attributes and functionality early in development [47].
- Bridging Studies: Perform experiments to compare new reagent lots against the current one, ensuring consistent assay performance [44].
- Inventory Management: Plan for sufficient supply and track assay performance trends to monitor reagent quality over time [47].
Designing and Executing Stability Studies
Stability assessment confirms that the analyte concentration and reagent immunoreactivity remain constant under specified storage conditions. According to regulatory guidance, to conclude stability, the difference between the result for a stored sample and a fresh sample should not exceed ±15% for chromatographic assays or ±20% for ligand-binding assays [45].
Key steps for a stability study include:
- Define Scope: The study should cover all conditions samples and reagents will encounter (e.g., bench-top, freeze-thaw, long-term frozen) [45].
- Set Duration: The storage duration tested should be at least equal to the maximum period study samples will be stored [45].
- Prepare Samples: Use a minimum of two concentration levels (low and high) in the appropriate matrix [45].
- Analyze and Compare: Analyze stored samples and compare the results to an appropriate reference (e.g., nominal concentration or fresh samples) [45].
Stability testing can be accelerated (using increased stress from heat or humidity) or conducted in real-time under specified storage conditions. While accelerated studies provide early insights, real-time studies are definitive for establishing shelf life [48].
Table 3: Key Reagents and Materials for Bioanalytical Optimization
| Item | Function in Optimization | Key Considerations |
|---|---|---|
| Analytical Balance | Core instrument for gravimetric pipette calibration. | Sensitivity and precision must be fit-for-purpose, especially for low-volume work [42]. |
| Multichannel Electronic Pipette | Increases throughput and reproducibility for microplate-based assays. | Systems like the INTEGRA ASSIST can automate protocols, reducing human error and RSI risk [49]. |
| Positive Displacement Tips | Enable accurate pipetting of challenging liquids (viscous, volatile). | More expensive than standard tips, but essential for specific applications [42] [46]. |
| Stabilization Buffer (e.g., M3) | Promotes analyte solubilization and stabilization during pre-treatment. | Critical for achieving high recovery of target analytes from complex matrices [43]. |
| Certified Reference Materials | Used for instrument calibration and assessing method accuracy. | Sourced from international bodies like NIST to ensure traceability and validity [42]. |
| Characterized Critical Reagents | Antibodies, proteins, and other binding agents central to assay performance. | Require thorough characterization and a lifecycle management strategy to ensure lot-to-lot consistency [44] [47]. |
The successful verification of an assay's functional sensitivity is a direct reflection of the robustness of its underlying techniques. As detailed in this guide, this requires a holistic approach that integrates accurate and precise pipetting, an optimized and efficient sample pre-treatment protocol, and a rigorous program for critical reagent stability management. By systematically implementing the optimization strategies and experimental protocols outlined herein—from selecting the appropriate liquid handling technology and validating its performance, to designing comprehensive stability studies—researchers and drug development professionals can significantly enhance the quality and reliability of their bioanalytical data. This, in turn, ensures that the determined functional sensitivity is a true and dependable measure of the assay's capability at the limits of detection.
Addressing Challenges in Low-Level Sample Handling and Matrix Effects
In the realm of pharmaceutical research and clinical diagnostics, the reliable measurement of low-concentration analytes is paramount for accurate decision-making. The concept of functional sensitivity—defined as the lowest analyte concentration that can be measured with an interassay coefficient of variation (CV) ≤20%—serves as a critical benchmark for determining the practical lower limit of an assay's reporting range [1]. Unlike analytical sensitivity (detection limit), which merely represents the concentration distinguishable from background noise, functional sensitivity reflects clinically useful performance where results maintain sufficient reproducibility for interpretation [1].
The path to achieving reliable functional sensitivity is fraught with technical challenges, particularly from matrix effects—the collective influence of all sample components other than the analyte on measurement quantification [50]. In liquid chromatography-mass spectrometry (LC-MS), these effects most commonly manifest as ion suppression or enhancement when matrix components co-elute with the target analyte and alter ionization efficiency in the source [51] [50]. The complex interplay between low-abundance analytes and matrix constituents can severely compromise key validation parameters including precision, accuracy, linearity, and sensitivity, ultimately undermining the reliability of functional sensitivity claims [50].
Table 1: Key Definitions in Sensitivity and Matrix Effect Analysis
| Term | Definition | Clinical/Research Significance |
|---|---|---|
| Functional Sensitivity | Lowest concentration measurable with ≤20% interassay CV [1] | Determines practical lower limit for clinically reliable results |
| Analytical Sensitivity | Lowest concentration distinguishable from background noise [1] | Theoretical detection limit with limited practical utility |
| Matrix Effects | Combined effects of all sample components other than the analyte on measurement [50] | Primary source of inaccuracy in complex sample analysis |
| Ion Suppression/Enhancement | Alteration of ionization efficiency for target analytes by co-eluting matrix components [50] | Common manifestation of matrix effects in LC-MS |
Experimental Protocols for Assessing Matrix Effects
Post-Column Infusion for Qualitative Assessment
The post-column infusion method, pioneered by Bonfiglio et al., provides a qualitative assessment of matrix effects across the chromatographic timeline [50]. This protocol involves injecting a blank sample extract into the LC-MS system while simultaneously infusing a standard solution of the analyte post-column via a T-piece connection [50]. The resulting chromatogram reveals regions of ion suppression or enhancement as deviations from the stable baseline signal, effectively mapping matrix interference landscapes [50].
Protocol Steps:
- Prepare blank matrix extract from the same biological matrix as study samples
- Configure LC-MS system with T-piece connection between column outlet and MS inlet
- Establish constant infusion of analyte standard at a concentration within the analytical range
- Inject blank matrix extract while monitoring analyte signal
- Identify retention time zones with signal deviation >±10% as regions with significant matrix effects
This approach proved particularly valuable in a systematic study of 129 pesticides across 20 different plant matrices, where it enabled researchers to visualize matrix effects independently of specific retention times and understand the relationship between molecular functional groups and matrix-dependent ionization [50].
Quantitative Assessment Methods
For quantitative assessment of matrix effects, two established protocols provide complementary data:
The post-extraction spike method developed by Matuszewski et al. compares the detector response for an analyte in a pure standard solution versus the same analyte spiked into a blank matrix sample at identical concentrations [50]. The matrix effect (ME) is calculated as: [ ME (\%) = \left( \frac{\text{Peak area in spiked matrix}}{\text{Peak area in standard solution}} - 1 \right) \times 100] Values significantly different from zero indicate ion suppression (negative values) or enhancement (positive values) [50].
Slope ratio analysis extends this assessment across a concentration range by comparing calibration curves prepared in solvent versus matrix [50]. The ratio of slopes provides a semi-quantitative measure of overall matrix effects: [ ME = \frac{\text{Slope of matrix-matched calibration}}{\text{Slope of solvent calibration}}]
Table 2: Comparison of Matrix Effect Assessment Methods
| Method | Type of Data | Blank Matrix Required | Primary Application |
|---|---|---|---|
| Post-Column Infusion | Qualitative (identification of affected regions) | Yes (or surrogate) | Method development troubleshooting |
| Post-Extraction Spike | Quantitative (single concentration) | Yes | Method validation |
| Slope Ratio Analysis | Semi-quantitative (concentration range) | Yes | Method validation and comparison |
| Relative ME Evaluation | Quantitative (lot-to-lot variability) | Multiple lots | Quality control across sample sources |
Establishing Functional Sensitivity Through Interassay Precision Profiles
The Critical Role of Precision Profiling
Functional sensitivity is determined through the construction of interassay precision profiles, which graphically represent how measurement imprecision changes across analyte concentrations [1] [13]. These profiles are generated by repeatedly measuring human serum pools containing low analyte concentrations over 4-8 weeks using multiple reagent lots in several clinical laboratories [38]. The functional sensitivity is identified as the concentration where the interassay CV reaches 20%, representing the boundary of clinically useful measurement [1].
Research comparing TSH immunometric assays revealed that manufacturer-stated functional sensitivity limits are rarely duplicated in clinical practice [38]. This discrepancy highlights the necessity for laboratories to independently verify functional sensitivity using clinically relevant protocols. Studies demonstrated that assays capable of "third-generation" functional sensitivity (0.01-0.02 mIU/L) provided better discrimination between subnormal and normal TSH values compared to those with "second-generation" sensitivity (0.1-0.2 mIU/L) [38].
Practical Implications for Diagnostic Accuracy
The functional sensitivity threshold directly impacts diagnostic accuracy and cost-effectiveness of testing strategies [38]. When functional sensitivity is inadequately characterized, misclassification of patient samples can occur. In one study, measurement of TSH in human serum pools by 16 different methods revealed that some assays could not reliably distinguish subnormal from normal values, potentially leading to clinical misinterpretation [38].
The precision profile concept extends beyond immunoassays to any measurement system where precision varies with analyte concentration [13]. Direct variance function estimation using models such as: [ \sigma^2(U) = (\beta1 + \beta2U)^J] where U is concentration and β1, β2, and J are parameters, has been shown to effectively describe variance relationships for both competitive and immunometric assays [13].
Strategic Approaches to Minimize Matrix Effects
Chromatographic and Sample Preparation Solutions
Chromatographic separation optimization represents the first line of defense against matrix effects. By achieving baseline resolution of analytes from matrix components, particularly phospholipids in biological samples, analysts can minimize co-elution phenomena that drive ionization effects in MS detection [50]. This includes optimizing mobile phase composition, gradient profiles, and column chemistry to shift analyte retention away from regions of high matrix interference identified through post-column infusion studies [51] [50].
Selective sample preparation techniques significantly reduce matrix complexity prior to analysis. Recent advances in molecular imprinted technology (MIP) promise unprecedented selectivity in extraction, though commercial availability remains limited [50]. More conventionally, protein precipitation, liquid-liquid extraction, and solid-phase extraction continue to serve as workhorse techniques for matrix simplification. The effectiveness of any clean-up procedure must be balanced against potential analyte loss, particularly critical for low-level compounds [50].
Internal Standardization and Alternative Detection Strategies
The internal standard method stands as one of the most effective approaches for compensating for matrix effects when accurate quantification is paramount [51]. By adding a known amount of a structurally similar compound (ideally stable isotope-labeled version of the analyte) to every sample, analysts can normalize for variability in ionization efficiency [51]. The calibration curve is then constructed using peak area ratios (analyte to internal standard) versus concentration ratios, effectively canceling out matrix-related suppression or enhancement [51].
For methods where sensitivity requirements are less stringent, alternative detection principles may offer reduced susceptibility to matrix effects. Atmospheric pressure chemical ionization (APCI) typically exhibits less pronounced matrix effects compared to electrospray ionization (ESI), as ionization occurs in the gas phase rather than liquid phase [50]. Similarly, evaporative light scattering (ELSD) and charged aerosol detection (CAD) present different vulnerability profiles, though they face their own limitations regarding mobile phase additives that can influence aerosol formation [51].
Matrix Effect Mitigation Strategy Selection
Comparative Performance of Mitigation Strategies
Systematic Evaluation of Compensation Approaches
The effectiveness of matrix effect mitigation strategies varies significantly based on the analytical context, particularly the required sensitivity and availability of blank matrix [50]. When sensitivity is crucial, approaches focused on minimization through MS parameter optimization, chromatographic conditions, and clean-up procedures typically yield superior results [50]. Conversely, when working with complex matrices where blank material is accessible, compensation strategies utilizing internal standardization and matrix-matched calibration often provide better accuracy [50].
Research comparing ME across different matrices revealed that most pharmaceutical compounds exhibited similar matrix effect profiles within the same matrix regardless of structure, but demonstrated significantly different profiles when moving between urine, plasma, and environmental matrices [50]. This underscores the importance of matrix-specific method validation rather than assuming consistent performance across sample types.
Table 3: Performance Comparison of Matrix Effect Mitigation Strategies
| Strategy | Mechanism | Advantages | Limitations | Suitable Context |
|---|---|---|---|---|
| Chromatographic Optimization | Separation of analyte from interfering matrix components | Does not require additional reagents or sample processing | Limited by inherent chromatographic resolution | All methods, particularly during development |
| Stable Isotope IS | Normalization using deuterated analog | Excellent compensation for ionization effects | High cost, limited availability for some analytes | Quantitation requiring high accuracy |
| Matrix-Matched Calibration | Matching standards to sample matrix | Compensates for constant matrix effects | Requires blank matrix, may not address lot-to-lot variation | Available blank matrix |
| Alternative Ionization (APCI) | Gas-phase ionization mechanism | Less susceptible to phospholipid effects | May not suit all analytes, different selectivity | Problematic compounds in ESI |
| Selective Extraction (MIP) | Molecular recognition-based clean-up | High selectivity, potential for high recovery | Limited commercial availability, development time | Complex matrices with specific interferences |
Impact on Functional Sensitivity and Data Quality
The successful implementation of matrix effect mitigation strategies directly influences achievable functional sensitivity and overall data quality. In a notable example from Snyder et al.' transcriptional landscape study, batch effects from different sequencing instruments and channels initially led to misleading conclusions—samples clustered by species rather than tissue type [52]. After applying ComBat batch correction, the data correctly grouped by tissue type, demonstrating how technical artifacts can obscure biological signals [52].
Chromatographic data quality similarly benefits from systematic approaches to matrix challenges. Supporting "first-time-right" peak integration through optimized methods and modern instrumentation reduces the need for repeated data reprocessing that raises regulatory concerns [53]. Regulatory agencies have noted instances where data were reprocessed 12 times with only the final result reported, highlighting the importance of robust methods that deliver reliable initial integration [53].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Key Research Reagent Solutions for Matrix Effect Management
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Normalization for recovery and ionization efficiency | Ideal compensation method when available; should be added early in sample preparation |
| Matrix-Matched Calibration Standards | Compensation for consistent matrix effects | Requires well-characterized blank matrix; must demonstrate similarity to study samples |
| Molecularly Imprinted Polymers | Selective extraction of target analytes | High potential selectivity; limited commercial availability currently |
| Quality Control Materials | Monitoring long-term precision profiles | Should mimic study samples; used for functional sensitivity verification |
| Post-column Infusion Standards | Mapping matrix effect regions | Qualitative assessment; identifies problematic retention time windows |
Successfully addressing challenges in low-level sample handling and matrix effects requires a systematic, multi-faceted approach that integrates strategic experimental design with appropriate analytical techniques. The establishment of reliable functional sensitivity through interassay precision profiling provides the critical foundation for determining the practical quantitation limits of any method [1]. Meanwhile, comprehensive matrix effect assessment using both qualitative (post-column infusion) and quantitative (post-extraction spike, slope ratio analysis) approaches enables researchers to identify and mitigate sources of inaccuracy [50].
The most robust methods typically combine minimization strategies (chromatographic optimization, selective clean-up) with compensation approaches (internal standardization, matrix-matched calibration) tailored to the specific analytical context and sensitivity requirements [50]. By implementing these practices within a framework of rigorous validation, researchers can achieve reliable low-level quantitation capable of supporting critical decisions in drug development and clinical diagnostics.
Implementing Risk-Based Approaches and Quality by Design (QbD) Principles
The pharmaceutical and clinical trial landscape is undergoing a significant paradigm shift, moving away from traditional quality verification methods toward a systematic approach that builds quality in from the outset. This transition is embodied in two complementary frameworks: Quality by Design (QbD) and Risk-Based Quality Management (RBQM). QbD is a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and control based on sound science and quality risk management [54]. When applied to clinical trials, QbD focuses on designing trials that are fit-for-purpose, ensuring that data collected are of sufficient quality to meet the trial's objectives, provide confidence in the results, support good decision-making, and adhere to regulatory requirements [55].
The International Council for Harmonisation (ICH) has cemented these approaches in recent guidelines. ICH E8(R1) emphasizes the importance of good planning and implementation in the QbD of clinical studies, focusing on essential activities and engaging stakeholders including patient representatives [56]. The newly finalized ICH E6(R3) guideline on Good Clinical Practice (GCP), published by the FDA in September 2025, fully integrates these concepts into the clinical trial framework, representing a significant evolution from previous versions [57]. These guidelines recognize that increased testing does not necessarily improve product quality—quality must be designed into the product and process rather than merely tested at the end [54].
Table 1: Core Concepts in Modern Clinical Trial Quality Management
| Concept | Definition | Key Components | Regulatory Foundation |
|---|---|---|---|
| Quality by Design (QbD) | A systematic approach to ensuring quality is built into the clinical trial process from the beginning | Identification of Critical-to-Quality factors (CtQs); Quality Target Product Profile (QTPP); proactive risk management | ICH E8(R1); ICH E6(R3) |
| Risk-Based Monitoring (RBM) | An approach to monitoring clinical trials that focuses resources on the areas of highest risk | Centralized monitoring; reduced source data verification; key risk indicators | ICH E6(R2); ICH E6(R3) |
| Risk-Based Quality Management (RBQM) | A comprehensive system for managing quality throughout the clinical trial lifecycle | Risk assessment; risk control; risk communication; risk review | ICH E6(R3); ICH Q9 |
Core Principles and Regulatory Framework
Quality by Design (QbD) Elements and Implementation
The implementation of QbD in clinical trials involves a series of structured elements that ensure quality is systematically built into the trial design. First and foremost is the identification of Critical-to-Quality factors (CtQs)—these are the essential elements that must be right to ensure participant safety and the reliability of trial results [56] [58]. These CtQs form the basis for the Quality Target Product Profile (QTPP), which is a prospective summary of the quality characteristics of a drug product that ideally will be achieved to ensure the desired quality, taking into account safety and efficacy [54].
In practice, QbD involves engaging stakeholders, including patient representatives, early in the trial design process to ensure the trial meets patient needs and safety priorities [56]. This approach reduces risks of adverse events by designing trials with CtQs in mind from the beginning, rather than attempting to inspect quality in at the end of the process [56]. The application of QbD principles also enables the optimization of trial design and treatment protocols based on accumulated knowledge and ensures reliable data collection that conforms to established quality attributes [56].
Risk-Based Approaches: RBM and RBQM
Risk-Based Monitoring (RBM) and Risk-Based Quality Management (RBQM) represent the operational execution of QbD principles throughout the clinical trial lifecycle. RBM is specifically focused on monitoring activities, advocating for a targeted approach that concentrates resources on the areas of highest risk to participant safety and data integrity, moving away from traditional 100% source data verification [56] [58].
RBQM constitutes a broader framework that encompasses RBM while adding comprehensive risk management throughout the trial. It involves a continuous cycle of planning, implementation, evaluation, and improvement to ensure the trial is conducted in a way that meets regulatory requirements and produces reliable results [56]. A core principle of RBQM is risk proportionality—ensuring that oversight and the level of resources applied to managing risks are commensurate with their potential to affect participant protection and result reliability [55].
ICH E6(R3) Updates and Regulatory Expectations
The recently published ICH E6(R3) guideline represents a significant advancement in the formalization of QbD and risk-based approaches. This update emphasizes that quality should be designed into trials from the beginning by identifying Critical-to-Quality factors that directly affect participant safety and data reliability [57]. The guideline calls for oversight that is proportionate to risk, moving away from one-size-fits-all monitoring toward greater reliance on centralized monitoring, targeted oversight, and adaptive approaches [57].
Regulatory agencies including the FDA, MHRA, and Health Canada have endorsed these approaches through various guidance documents, promoting flexible and proportionate trial design and conduct that enables innovation while safeguarding participant protections and ensuring data reliability [55]. These agencies recognize that the multifaceted and complex nature of modern clinical trials, encompassing diverse patient populations, novel operational approaches, and advanced technologies, necessitates this updated approach to quality management [55].
Diagram 1: Evolution of Good Clinical Practice Guidelines toward QbD and Risk-Based Approaches
Functional Sensitivity and Interassay Precision in Diagnostic Verification
The Role of Functional Assays in Drug Development
Functional assays provide critical insights into the biological activity of therapeutic candidates, serving as a bridge between molecular promise and biological confirmation. Unlike binding assays that merely confirm molecular interaction, functional assays measure whether a molecular interaction triggers a meaningful biological response [59]. These assays answer fundamental questions about drug candidates: Does the antibody activate or inhibit a specific cell signal? Can it block a receptor-ligand interaction? Does it mediate immune responses like antibody-dependent cellular cytotoxicity (ADCC) or complement-dependent cytotoxicity (CDC)? [59]
The importance of functional assays is highlighted by the fact that antibodies with excellent binding affinity may fail in clinical trials due to poor functional performance [59]. Functional testing helps mitigate this risk by providing real-world performance data early in development, enabling better candidate selection and reducing late-stage failures. These assays are particularly crucial for demonstrating therapeutic relevance to regulatory bodies, who require proof that a drug candidate performs as intended through its mechanism of action [59].
Interassay Precision and Functional Sensitivity
Interassay precision profiles and functional sensitivity determinations are essential for establishing the reliability of diagnostic and functional assays. Functional sensitivity is specifically defined as the concentration at which the interassay coefficient of variation (CV) is ≤20% [38]. This parameter is crucial for determining the lowest reliable measurement an assay can provide, which directly impacts diagnostic accuracy and clinical utility.
Research on immunometric assays for thyrotropin (TSH) has revealed that manufacturer-stated functional sensitivity limits are rarely duplicated in clinical practice, highlighting the importance of independent verification [38]. Studies comparing multiple methods across different laboratories have demonstrated that some assays cannot reliably distinguish subnormal from normal values, leading to potential misclassification of patient results [38]. This underscores the necessity for laboratories to independently establish an assay's functional sensitivity using clinically relevant protocols rather than relying solely on manufacturer claims.
Impact on Diagnostic Accuracy and Cost-Effectiveness
Intermethod and interlaboratory differences in functional sensitivity directly impact both the diagnostic accuracy and cost-effectiveness of testing strategies [38]. Research has demonstrated that assays capable of "third-generation" functional sensitivity (0.01-0.02 mIU/L for TSH) provide better pool rankings and fewer misclassifications of low-concentration samples compared to assays with "second-generation" functional sensitivity (0.1-0.2 mIU/L) [38].
These findings highlight the importance of both assay robustness and appropriate sensitivity determination in clinical practice. Manufacturers are encouraged to assess functional sensitivity more realistically and improve assay robustness to ensure that performance potential is consistently met across different laboratory environments [38]. This alignment between claimed and actual performance is essential for maintaining diagnostic accuracy in real-world settings.
Table 2: Comparison of Functional Assay Types in Drug Development
| Assay Type | Key Measurements | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Cell-Based Assays | ADCC, CDC, receptor internalization, apoptosis, cell proliferation | Mechanism of action confirmation; immune effector function; cytotoxicity assessment | Physiologically relevant context; comprehensive functional readout | More complex; longer duration; higher variability |
| Enzyme Activity Assays | Substrate conversion rates; inhibition constants (Ki); IC50 values | Enzyme-targeting therapeutics; lead optimization | Quantitative; rapid; suitable for high-throughput screening | May not capture cellular context |
| Blocking/Neutralization Assays | Inhibition of ligand-receptor binding; viral entry blocking | Infectious disease; autoimmune disorders; cytokine-targeting therapies | Direct measurement of therapeutic mechanism | May require specialized reporter systems |
| Signaling Pathway Assays | Phosphorylation status; reporter gene activation; pathway modulation | Targeted therapies; immune checkpoint inhibitors | Specific mechanism insight; sensitive detection | Focused on specific pathways only |
Experimental Approaches and Methodologies
Functional Assay Protocols and Methodologies
Functional assay protocols vary based on the specific therapeutic modality and mechanism of action being evaluated. For antibody-based therapies, common functional assays include cell-based cytotoxicity assays to evaluate ADCC and CDC, where target cells expressing the antigen of interest are incubated with the therapeutic antibody and appropriate effector cells or complement sources [59]. These assays typically measure specific cell killing through detection methods such as lactate dehydrogenase (LDH) release, caspase activation for apoptosis, or flow cytometry with viability dyes.
Signaling pathway assays often utilize reporter gene systems where cells are engineered to express luciferase or other reporter proteins under the control of response elements from relevant pathways [59]. For example, a PD-1/PD-L1 blocking antibody assay might use a T-cell line engineered with a NFAT-responsive luciferase reporter to measure T-cell activation upon checkpoint blockade. These assays provide quantitative readouts of pathway modulation and can be adapted for high-throughput screening of candidate molecules.
Neutralization assays evaluate the ability of therapeutic antibodies to inhibit biological interactions, such as ligand-receptor binding or viral entry [59]. These typically involve pre-incubating the target (e.g., cytokine, virus) with the antibody before adding to reporter cells or systems. Inhibition is measured through reduced signal compared to controls, providing IC50 values that reflect functional potency.
Precision Medicine Applications
Functional precision medicine represents a powerful application of these assay methodologies, particularly in oncology. Studies have demonstrated that ex vivo drug sensitivity testing of patient-derived cells can effectively guide therapy selection for aggressive hematological cancers [60]. In one approach, researchers tested the effects of more than 500 candidate drugs on leukemic cells from 186 patients with relapsed acute myeloid leukemia (AML), integrating drug sensitivity data with genomic and molecular profiling to assign therapy recommendations [60].
This functional precision medicine approach demonstrated remarkable success, with an overall response rate of 59% in a late-stage refractory AML population that had exhausted standard treatment options [60]. The methodology provides clinically actionable results within three days—significantly faster than comprehensive genomic profiling—making it feasible for medical emergencies such as acute leukemia [60]. This demonstrates how functional assays can bridge the gap between molecular findings and clinical application in real-time treatment decisions.
Interassay Precision Profiling Methodology
Establishing reliable interassay precision profiles requires systematic evaluation across multiple runs, operators, and reagent lots. The recommended methodology involves constructing clinically relevant precision profiles using human serum pools or other biologically relevant matrices measured over an extended period (4-8 weeks) by multiple methods in different laboratories [38]. This approach captures real-world variability and provides a realistic assessment of functional sensitivity.
The protocol should include testing in at least four to eight clinical laboratories plus the manufacturer's facility to adequately assess interlaboratory variability [38]. Each method should be evaluated using multiple reagent lots to account for lot-to-lot variation. Statistical analysis focuses on determining the concentration at which the interassay coefficient of variation crosses the 20% threshold—the established definition of functional sensitivity for many diagnostic assays [38].
Diagram 2: Interassay Precision Profiling Workflow for Functional Sensitivity Verification
Comparative Performance Data
QbD and RBQM Implementation Outcomes
The implementation of QbD and risk-based approaches has demonstrated significant benefits across clinical trial phases. In Phase 1 trials, QbD principles help ensure participant safety and trial validity by designing trials with Critical-to-Quality factors in mind and reducing risks of adverse events [56]. Risk-Based Monitoring in this early phase focuses on reducing risks to participant safety and ensuring trial validity by monitoring high-risk areas and collecting data to ensure participant safety [56].
In Phase 2 trials, the benefits expand to include optimization of trial design and treatment protocols based on earlier phase feedback, ensuring reliable data collection that conforms to CtQs [56]. By Phase 3, the cumulative effect of QbD implementation ensures the reproducibility and consistency of results while minimizing risks of product failure and regulatory noncompliance [56]. Throughout all phases, RBQM provides a framework for continuous evaluation and optimization of resource allocation based on risk assessment [56].
Functional Precision Medicine Outcomes
Comparative studies of functional versus genomics-based precision medicine reveal striking differences in actionability rates. While genomic approaches typically yield actionable findings in a minority of patients, functional drug sensitivity testing has demonstrated the ability to identify potentially actionable drugs for almost all patients (98%) in studies of relapsed AML [60]. This significantly higher actionability rate highlights the complementary value of functional assessment alongside genomic characterization.
In observational clinical studies where patients were treated with functionally recommended drugs, the outcomes have been impressive, particularly considering the late-stage, refractory nature of the diseases treated. The reported 59% overall response rate in advanced AML patients, with some successfully bridged to curative stem cell transplantation, demonstrates the clinical utility of this approach [60]. Additionally, the rapid turnaround time of functional assays (as little as three days for some platforms) provides a practical advantage over more comprehensive genomic profiling, especially in acute clinical scenarios [60].
Industry Adoption and Implementation Gaps
Despite demonstrated benefits and regulatory encouragement, implementation of QbD and RBQM approaches remains inconsistent across the industry. Research indicates that Risk-Based Quality Management is still only implemented in approximately 57% of trials on average, with smaller organizations particularly lagging in adoption [58]. Knowledge gaps and change-management hurdles are frequently cited as barriers to broader implementation.
Even when RBQM is formally implemented, key elements are often underutilized. Surveys across thousands of trials have found that centralized monitoring adoption and the shift away from heavy source data verification remain patchy, limiting the full benefits that QbD promises [58]. This implementation gap persists despite clear regulatory direction and evidence of effectiveness, suggesting that cultural and operational barriers remain significant challenges.
Table 3: Comparison of Traditional vs. QbD/RBQM Approaches in Clinical Trials
| Parameter | Traditional Approach | QbD/RBQM Approach | Impact and Evidence |
|---|---|---|---|
| Quality Focus | Quality verification through extensive endpoint checking | Quality built into design; focused on Critical-to-Quality factors | Reduced protocol amendments; improved data reliability [58] |
| Monitoring Strategy | Heavy reliance on 100% source data verification | Risk-based monitoring; centralized statistical monitoring | 30-50% reduction in monitoring costs; earlier issue detection [56] [58] |
| Resource Allocation | Uniform allocation across all trial activities | Proportional to risk; focused on critical data and processes | More efficient use of resources; better risk mitigation [55] |
| Patient Engagement | Limited patient input in trial design | Active patient representative engagement in design | Reduced participant burden; improved recruitment and retention [55] |
| Regulatory Compliance | Focus on meeting minimum requirements | Systematic approach to ensuring fitness for purpose | Reduced findings in inspections; smoother regulatory reviews [57] |
Essential Research Reagents and Solutions
The implementation of robust functional assays and precision medicine approaches requires carefully selected research reagents and solutions that ensure reliability and reproducibility. The following toolkit represents essential materials for conducting these advanced assessments:
Table 4: Essential Research Reagent Solutions for Functional Assays
| Reagent/Solution Category | Specific Examples | Function and Application | Critical Quality Attributes |
|---|---|---|---|
| Viability/Cytotoxicity Detection | LDH assay kits; ATP detection reagents; caspase activation assays; flow cytometry viability dyes | Measure cell health and death endpoints in functional assays | Sensitivity; linear range; compatibility with assay systems |
| Reporter Gene Systems | Luciferase substrates (e.g., luciferin); fluorescent proteins (GFP, RFP); β-galactosidase substrates | Quantify pathway activation and transcriptional activity in signaling assays | Signal-to-noise ratio; stability; non-toxicity to cells |
| Cytokine/Chemokine Detection | Multiplex immunoassays; ELISA kits; electrochemiluminescence platforms | Profile immune responses and inflammatory mediators in functional assays | Cross-reactivity; dynamic range; sample volume requirements |
| Cell Culture Media and Supplements | Serum-free media; defined growth factors; cytokine cocktails; selection antibiotics | Maintain primary cells and engineered cell lines for functional testing | Lot-to-lot consistency; growth support capability; defined composition |
| Signal Transduction Reagents | Phospho-specific antibodies; pathway inhibitors/activators; protein extraction buffers | Detect and manipulate signaling pathways in mechanistic studies | Specificity; potency; compatibility with detection platforms |
The integration of Quality by Design principles and risk-based approaches represents a fundamental evolution in how clinical trials are conceptualized, designed, and executed. The publication of ICH E6(R3) provides a clear regulatory framework for this transition, emphasizing quality built into trials from the beginning through identification of Critical-to-Quality factors and application of proportionate, risk-based oversight strategies [57]. When properly implemented, these approaches yield significant benefits including enhanced participant protection, more reliable results, reduced operational burden, and increased efficiency.
The verification of functional sensitivity through interassay precision profiling provides a critical foundation for diagnostic and therapeutic assessment, ensuring that measurements are both accurate and clinically meaningful. As functional precision medicine continues to evolve, with drug sensitivity testing enabling personalized therapy selection for cancer patients, the importance of robust, well-characterized assay systems becomes increasingly evident [60]. The demonstrated success of these approaches—with actionability rates exceeding 98% in some studies and response rates of 59% even in refractory populations—highlights their transformative potential [60].
While implementation challenges remain, particularly regarding cultural change and operational adaptation, the direction of travel is clear. Regulatory agencies globally are aligning around these modernized approaches, creating an environment that encourages innovation while maintaining rigorous standards for participant safety and data integrity [55]. As the industry continues to embrace QbD and risk-based methodologies, clinical trials will become increasingly efficient, informative, and patient-centered, ultimately accelerating the development of new therapies for those in need.
Statistical Verification, Comparative Analysis, and Leveraging Digital Tools
In the field of clinical diagnostics, high-sensitivity cardiac troponin T (hs-cTnT) assays have become indispensable tools for the rapid diagnosis of acute coronary syndromes. Regulatory bodies like the European Society of Cardiology recommend strict criteria for hs-cTnT assays, requiring a coefficient of variation (CV) of <10% at the 99th percentile upper reference limit (URL) and measurable values below this limit in >50% of healthy individuals [61]. While manufacturers provide performance specifications for these assays, independent statistical verification is a critical scientific practice that ensures reliability in real-world clinical and research applications. This verification process involves rigorous comparison of empirical performance data against manufacturer claims across multiple analytical parameters, with functional sensitivity—defined by interassay precision profiles—serving as a cornerstone metric for assay reliability near critical clinical decision points.
Comparative Analytical Performance of hs-cTnT Assays
Experimental Design for Method Comparison
A comprehensive 2025 study directly compared the performance of the new Sysmex HISCL hs-cTnT assay against the established Roche Elecsys hs-cTnT assay, following Clinical and Laboratory Standards Institute (CLSI) guidelines [61]. The experimental protocol utilized anonymized, deidentified leftover sera stored at -70°C if not immediately analyzed. For the method comparison, 2,151 samples were analyzed on both the Sysmex HISCL and Roche Elecsys analyzers. The statistical analysis included Passing-Bablok regression to assess agreement and Bland-Altman analysis to evaluate bias between the two methods [61].
The verification of analytical performance parameters followed established clinical laboratory standards:
- Limit of blank (LoB) and limit of detection (LoD) were determined according to CLSI EP17-A2 guidelines
- Functional sensitivity (CV of 20% and 10%) was established by serially diluting control reagents and testing each point 20 times to determine the mean value with associated CV%
- Precision was assessed using two levels of control material run five times daily over five days following CLSI EP05-A3 guidelines
- 99th percentile URLs were derived from a cardio-renal healthy population (n=1,004) with no history of hypertension, diabetes, and eGFR ≥60 mL/min/1.73 m² [61]
Quantitative Performance Comparison
Table 1: Analytical Performance Parameters of Sysmex HISCL vs. Roche hs-cTnT Assays
| Performance Parameter | Sysmex HISCL hs-cTnT | Roche Elecsys hs-cTnT |
|---|---|---|
| Limit of Blank | 1.3 ng/L | Not specified in study |
| Limit of Detection | 1.9 ng/L | Established reference method |
| Functional Sensitivity (20% CV) | 1.8 ng/L | Not specified in study |
| Functional Sensitivity (10% CV) | 3.3 ng/L | Not specified in study |
| Assay Time | 17 minutes | 9 minutes |
| Measurement Range | 2-10,000 ng/L | Not specified in study |
| Precision at 99th Percentile | CV <10% | CV <10% |
| Claimed Limit of Quantitation | 1.5 ng/L | Not specified in study |
Table 2: Method Comparison and 99th Percentile URL Findings
| Comparison Metric | Findings | Clinical Significance |
|---|---|---|
| Passing-Bablok Regression | Excellent agreement (r=0.95) with Roche hs-cTnT | Supports interchangeable use in clinical practice |
| Bland-Altman Analysis (≤52 ng/L) | Mean absolute difference of 3.5 ng/L | Good agreement at clinically relevant concentrations |
| Bland-Altman Analysis (>52 ng/L) | Mean difference of 2.8% | Minimal proportional bias at higher concentrations |
| 99th URL (Overall) | 14.4 ng/L | Provides population-specific reference value |
| 99th URL (Male) | 17.0 ng/L | Gender-specific cutoffs enhance diagnostic accuracy |
| 99th URL (Female) | 13.9 ng/L | Addresses known gender differences in troponin levels |
The method comparison data revealed excellent correlation between the Sysmex HISCL and Roche assays (r=0.95), with clinically acceptable differences across the measurement range [61]. The derivation of gender-specific 99th percentile URLs represents a significant advancement in personalized cardiovascular risk assessment, as the study established values of 17.0 ng/L for males and 13.9 ng/L for females, reflecting intrinsic biological differences in troponin distribution [61].
Statistical Verification Methodology
Fundamental Principles of Analytical Verification
Statistical verification of manufacturer claims requires a clear distinction between analytical performance validation and diagnostic performance assessment. As highlighted in veterinary clinical pathology literature—where principles directly translate to human diagnostics—analytical performance validation establishes that a method operates within specifications, while diagnostic performance evaluation determines how well a method differentiates between diseased and non-diseased individuals [62]. For verification of manufacturer claims, the focus remains primarily on analytical performance parameters including accuracy, precision, linearity, and sensitivity.
The methodological framework for statistical verification should include:
- Method comparison studies to identify bias between the test method and an established comparative method
- Precision profiles to establish functional sensitivity across the assay range
- Robust statistical analysis including regression analysis, difference plots, and confidence interval estimation
- Clinical relevance assessment of any identified biases beyond mere statistical significance [62]
Experimental Protocols for Verification Studies
For independent verification of manufacturer claims, specific experimental protocols should be implemented:
Precision Profile Protocol:
- Prepare replicate samples at multiple concentrations across the assay range (minimum 9 determinations over 3 concentration levels)
- Analyze samples over multiple runs, days, and operators to capture interassay variability
- Calculate CV% at each concentration level and plot against concentration
- Determine functional sensitivity as the concentration corresponding to 10% CV [8] [63]
Method Comparison Protocol:
- Select appropriate sample set representing clinical measurement range
- Analyze all samples using both reference and test methods
- Utilize Passing-Bablok regression to account for non-constant variance and outliers
- Perform Bland-Altman analysis to quantify bias across concentration levels
- Establish equivalence or superiority margins based on clinical requirements [61] [62]
Linearity and Range Verification Protocol:
- Prepare samples at minimum of 5 concentration levels across claimed range
- Analyze in triplicate and plot observed vs. expected values
- Calculate regression statistics including slope, intercept, and coefficient of determination (r²)
- Verify that precision, accuracy, and linearity remain acceptable across entire range [8]
Visualizing Statistical Verification Workflows
Precision Profile Analysis Diagram
Statistical Verification Workflow
Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for hs-cTnT Assay Verification
| Reagent/Material | Specifications | Function in Verification |
|---|---|---|
| hs-cTnT Calibrators | Sysmex HISCL troponin T hs C0-C5 calibrators; human serum-based (C1-C5) | Establish calibration curve; valid for 30 days post-reconstitution |
| Control Materials | Sysmex HISCL control reagents at multiple concentration levels | Monitor assay precision and accuracy across measurement range |
| Matrix Diluent | Sysmex HISCL diluent solution | Sample preparation and serial dilution for precision profiles |
| Human Serum Samples | Deidentified leftover sera; stored at -70°C | Method comparison using real clinical specimens |
| Mobile Phase Components | Ethanol and 0.03M potassium phosphate buffer (pH 5.2) | Chromatographic separation in reference methods |
| Extraction Solvents | Diethyl ether and dichloromethane | Liquid-liquid extraction for sample preparation |
| Reference Method Reagents | Roche Elecsys hs-cTnT assay components | Establish comparative method for verification studies |
Impact of Biological Variables on Assay Performance
Beyond core analytical verification, the 2025 Sysmex HISCL validation study importantly assessed the effect of biological variables on hs-cTnT measurements. The research demonstrated that hs-cTnT concentrations increased with both advancing age and declining renal function (measured by eGFR) [61]. This finding has crucial implications for the statistical verification process:
Age-Dependent Variations:
- Hs-cTnT baselines show progressive elevation across age decades
- Verification studies should include age-stratified analysis
- Reference intervals may require age-adjusted thresholds
Renal Function Considerations:
- Hs-cTnT increases by approximately 8.2% for every 5 mL/min/1.73 m² decrease in eGFR
- Patients with end-stage renal disease show elevated hs-cTnT in 39-98% of cases
- Verification in renal-impaired populations requires separate assessment [61]
These biological influences highlight that statistical verification must extend beyond analytical performance to encompass clinical covariates that significantly impact measured values in patient populations.
Independent statistical verification of manufacturer claims remains an essential component of assay validation in clinical and research settings. The 2025 evaluation of the Sysmex HISCL hs-cTnT assay demonstrates a comprehensive approach to verifying functional sensitivity through interassay precision profiles and method comparison studies. The establishment of gender-specific 99th percentile URLs (17.0 ng/L for males, 13.9 ng/L for females) provides population-relevant decision thresholds that account for biological variability [61].
For researchers and drug development professionals, these verification protocols ensure that diagnostic assays perform reliably in critical clinical decision-making contexts. The experimental frameworks and statistical methodologies outlined provide a robust template for evaluating manufacturer claims across diverse analytical platforms and diagnostic applications. As high-sensitivity troponin assays continue to evolve, maintaining rigorous independent verification standards will be paramount for advancing cardiovascular diagnostics and optimizing patient care pathways.
In the rigorous field of drug development, verifying functional sensitivity and understanding interassay precision are foundational to ensuring the reliability of bioanalytical data. This guide provides a structured framework for comparing the performance of different assay platforms, moving beyond theoretical specifications to empirical, data-driven evaluation. Such comparative analysis is critical for researchers and scientists who must select the most appropriate and robust assay for their specific context, whether for pharmacokinetic studies, biomarker validation, or potency testing [64] [65]. The process of benchmarking systematically identifies the strengths and weaknesses of available alternatives, enabling informed procurement and deployment decisions that directly impact research quality and regulatory success [66].
This article outlines a comprehensive experimental protocol for benchmarking assays, presents simulated comparative data for key platforms, and provides resources to standardize evaluation across laboratories. By framing this within the broader thesis of verifying functional sensitivity—the lowest analyte concentration an assay can measure with acceptable precision—we emphasize the critical role of interassay precision profiles in quantifying an assay's practical operating range [64].
Experimental Protocol for Assay Benchmarking
A robust benchmarking methodology requires a standardized protocol to ensure fair and reproducible comparisons. The following workflow provides a detailed, step-by-step guide for evaluating assay performance. The diagram below visualizes this multi-stage process.
Sample Preparation and Experimental Setup
Materials:
- Analyte of Interest: A purified, well-characterized reference standard.
- Biological Matrix: Use a consistent, relevant matrix (e.g., human serum, plasma, cell lysate) pooled and confirmed to be free of the target analyte or interfering substances.
- Assay Platforms: The assays and instrumentation platforms to be compared (e.g., ELISA, MSD, Gyrolab, Ella).
- Quality Controls (QCs): Prepare independent QC samples at low, medium, and high concentrations across the expected dynamic range. These are distinct from the calibrators used to generate the standard curve.
Methodology:
- Sample Serial Dilution: Create a serial dilution of the reference standard in the relevant biological matrix. The dilution should span the entire claimed dynamic range of the assays being tested, from above the upper limit of quantification (ULOQ) to below the expected lower limit of quantification (LLOQ).
- Replication Strategy: For each assay platform, a minimum of n=5 independent runs should be performed. Each run must include a full set of calibrators, QCs, and the serial dilution samples in duplicate. This replication is essential for generating statistically significant interassay precision data.
- Execution: Strictly adhere to the manufacturer's protocols for each platform. All assays for a single run should be performed by the same analyst using the same reagent lots to minimize intra-assay variability. Environmental conditions (e.g., incubation temperature, timing) must be meticulously controlled.
Data Analysis and Performance Metrics
Key Metrics to Calculate:
- Interassay Precision (%CV): Calculate the coefficient of variation (%CV) for each QC and sample concentration across the n=5 independent runs. The formula is (Standard Deviation / Mean) × 100.
- Interassay Accuracy (%Bias): Calculate the percentage bias from the theoretical (spiked) concentration for each QC sample. The formula is ((Mean Observed Concentration - Theoretical Concentration) / Theoretical Concentration) × 100.
- Functional Sensitivity (LLOQ): The lowest analyte concentration that can be quantitatively measured with an interassay %CV ≤ 20% (or another pre-defined acceptance criterion, e.g., 25% for ligand-binding assays) and accuracy within ±20% of the theoretical value.
- Dynamic Range: The span of concentrations from the LLOQ to the ULOQ, where the ULOQ is defined as the highest concentration measurable with acceptable precision and accuracy.
- Robustness: Evaluate the assay's performance against edge cases or minor, deliberate variations in protocol (e.g., slight changes in incubation time or temperature) [66].
The precision and accuracy data are then used to construct interassay precision profiles, which are scatter plots of %CV versus analyte concentration. These profiles visually define the functional sensitivity and the usable range of the assay.
Comparative Performance Data
The following tables summarize simulated experimental data for four common immunoassay platforms, benchmarking them against critical performance parameters. This data illustrates the type of structured comparison required for objective evaluation.
Table 1: Key Performance Metrics for Immunoassay Platforms (Simulated Data)
| Platform | Dynamic Range | Functional Sensitivity (LLOQ) | Interassay Precision (%CV) | Interassay Accuracy (%Bias) | Sample Volume (μL) | Hands-on Time (Min) |
|---|---|---|---|---|---|---|
| Traditional ELISA | 3-4 logs | 15-50 pg/mL | 10-15% (Mid-range) | ±8% (Mid-range) | 50-100 | 180-240 |
| MSD (Meso Scale Discovery) | 4-5 logs | 1-5 pg/mL | 6-10% (Mid-range) | ±5% (Mid-range) | 10-25 | 120-180 |
| Gyrolab | 3-4 logs | 0.5-2 pg/mL | 5-8% (Mid-range) | ±4% (Mid-range) | 1-5 | 30-60 |
| Ella (ProteinSimple) | 3-4 logs | 2-10 pg/mL | 7-12% (Mid-range) | ±6% (Mid-range) | ~10 | <10 |
Table 2: Simulated Interassay Precision Profile Data for a 10 pg/mL QC Sample
| Platform | Theoretical Conc. (pg/mL) | Mean Observed Conc. (pg/mL) | Standard Deviation | Interassay %CV | Interassay %Bias | n |
|---|---|---|---|---|---|---|
| Traditional ELISA | 10.00 | 10.85 | 1.52 | 14.0 | +8.5 | 5 |
| MSD | 10.00 | 9.95 | 0.70 | 7.0 | -0.5 | 5 |
| Gyrolab | 10.00 | 10.40 | 0.62 | 6.0 | +4.0 | 5 |
| Ella | 10.00 | 9.65 | 0.87 | 9.0 | -3.5 | 5 |
The data in these tables highlights the inherent trade-offs. While the Gyrolab platform demonstrates superior sensitivity and precision with minimal sample volume, its throughput can be a limiting factor. MSD offers a wide dynamic range and strong performance, whereas Ella significantly reduces hands-on time through automation. The Traditional ELISA, while often more accessible and lower in cost, generally shows higher variability and requires more sample and labor [67].
The Scientist's Toolkit: Essential Research Reagents and Materials
The reliability of any benchmarking study is contingent on the quality of its core components. Below is a list of essential materials and their functions in bioanalytical assay comparisons.
Table 3: Key Research Reagent Solutions for Assay Benchmarking
| Item | Function in Benchmarking | Critical Quality Attributes |
|---|---|---|
| Reference Standard | Serves as the definitive material for preparing known concentrations of the analyte to establish calibration curves and QCs. | High purity (>95%), confirmed identity and stability, and precise concentration. |
| Quality Control (QC) Samples | Independent samples of known concentration used to monitor the accuracy and precision of each assay run across the dynamic range. | Should be prepared independently from calibration standards; stability and homogeneity are critical. |
| Critical Reagents | Assay-specific components such as antibodies, enzymes, substrates, and labels that directly determine assay performance. | High specificity, affinity, and lot-to-lot consistency. Requires rigorous characterization. |
| Biological Matrix | The background material (e.g., serum, plasma, buffer) that mimics the sample environment. Used for diluting standards. | Should be well-characterized and, if possible, analyte-free to avoid background interference. |
| Precision Profile Software | Statistical software (e.g., R, PLA, GraphPad Prism) used to calculate metrics (%CV, %Bias) and generate precision profiles. | Ability to handle 4-5 parameter logistic (4PL/5PL) curve fitting and precision profile analysis. |
Visualization of the Precision Profile Concept
The interassay precision profile is the cornerstone of functional sensitivity verification. It provides a direct visual representation of an assay's performance across its measuring range. The following diagram illustrates the logical relationship between raw data, the precision profile, and the final determination of functional sensitivity.
As depicted, the process begins with raw data from multiple runs. The interassay %CV is calculated for each concentration level and plotted to create the precision profile. The point where this profile intersects the pre-defined acceptance criterion (e.g., the 20% %CV line) definitively establishes the Functional Sensitivity (LLOQ) of the assay. This empirical method is far more reliable than relying on manufacturer claims or data from a single experiment [64].
The verification of functional sensitivity is a critical component in the development and validation of cell-based assays, serving as a cornerstone for reliability in both clinical diagnostics and biomedical research. This parameter, defined by the lower limit of quantification (LLOQ) where an assay can maintain acceptable precision (typically <20-25% coefficient of variation), establishes the minimum concentration at which an analyte can be reliably measured [68]. For researchers and drug development professionals working with immunoassays and high-sensitivity flow cytometry, establishing robust functional sensitivity remains challenging due to biological variability, matrix effects, and technological limitations.
The framework for verifying functional sensitivity relies heavily on constructing interassay precision profiles through repeated measurements of samples with varying analyte concentrations. These profiles graphically represent the relationship between precision and concentration, allowing for the determination of the LLOQ at the point where precision falls below an acceptable threshold [68] [69]. This article applies this framework through comparative case studies across different platforms and applications, providing experimental data and methodologies to guide assay selection and validation.
Case Study 1: High-Sensitivity Flow Cytometry for Rare Cell Detection
Experimental Protocol and Validation Framework
This case study examines the validation of a high-sensitivity flow cytometry (HSFC) protocol for detecting follicular helper T (Tfh) cells, which typically constitute only 1-3% of circulating CD4+ T cells in healthy adults [68]. The validation followed CLSI H62 guidelines and incorporated rigorous precision testing to establish functional sensitivity.
- Sample Preparation: Residual peripheral blood samples (N=17) were stabilized with TransFix to preserve rare cell populations. To increase the proportion of Tfh cells for LLOQ determination, CD4+ T cells were isolated using the EasySep Isolation Kit before analysis [68].
- Cell Staining and Analysis: A multicolor antibody panel was used to identify Tfh cells (CD3+/CD4+/CXCR5+) and their subtypes. A minimum of 100,000 cells were acquired per sample using a Navios flow cytometer, with a target CV of 10% for Tfh cell frequency [68].
- Precision and Sensitivity Assessment: Intra-assay precision was determined from three replicates in a single run, while interassay precision was assessed from three replicates across four different runs. The LLOQ was established using residual cells from CD4 isolation as low-level samples [68].
Performance Data and Functional Sensitivity
Table 1: Precision Data for High-Sensitivity Tfh Cell Detection [68]
| Precision Type | Sample | Absolute Count of Tfh Cells (/μL)* | %CV - Tfh Cells | %CV - Tfh1 Cells | %CV - Tfh17 Cells |
|---|---|---|---|---|---|
| Intra-Assay | Sample-1 | 1,186 | 1.67 | 3.57 | 7.64 |
| Sample-2 | 130 | 0.56 | 0.82 | 1.34 | |
| Sample-3 | 29 | 1.29 | 0.21 | 4.68 | |
| Inter-Assay | Sample-1 | 1,068 | 2.19 | 8.53 | 16.0 |
| Sample-2 | 128 | 3.13 | 4.99 | 4.50 | |
| Sample-3 | 29 | 6.51 | 7.13 | 9.48 |
*Average value of all replicates for each sample
The data demonstrated excellent intra-assay precision for Tfh cells (%CV <10% even at low levels). While inter-assay precision showed greater variability, particularly for Tfh subtypes, the %CV for total Tfh cells remained below 10% for two samples and at 6.51% for the lowest-count sample, confirming the assay's robust functional sensitivity down to approximately 29 Tfh cells/μL [68]. The successful validation highlighted that strategic approaches, such as using pre-enriched cell fractions, can facilitate LLOQ establishment even in resource-limited settings.
Reagent Solutions for High-Sensitivity Flow Cytometry
Table 2: Key Research Reagent Solutions for HSFC
| Item | Function | Example from Case Study |
|---|---|---|
| Cell Stabilization Reagent | Preserves cell surface epitopes and viability for delayed testing. | TransFix (Cytomark) [68] |
| Cell Isolation Kit | Enriches target cell populations to facilitate LLOQ determination. | EasySep Isolation Kit (STEMCELL Technologies) [68] |
| Multicolor Antibody Panel | Enables simultaneous identification of multiple cell populations and subtypes. | Antibodies against CD3, CD4, CXCR5, CCR6, CXCR3 (BD Biosciences) [68] |
| Viability Dye | Distinguishes live from dead cells to improve analysis accuracy. | Viability aqua dye [68] |
Case Study 2: Flow Cytometry vs. Commercial Immunoassays for SARS-CoV-2 T-Cell Response
Experimental Protocol and Comparison Framework
This study compared an in-house flow cytometry intracellular cytokine staining (FC-ICS) assay with the commercially available QuantiFERON SARS-CoV-2 Test (QF) for detecting SARS-CoV-2-Spike-reactive T cells in vaccinated individuals [70].
- FC-ICS Protocol: Heparinized whole blood was stimulated for 6 hours with overlapping peptides spanning the SARS-CoV-2 Spike protein. After stimulation, cells were stained for surface markers (CD3, CD4, CD8) and intracellular IFN-γ, then analyzed on a flow cytometer. Results were expressed as the frequency of IFN-γ-producing CD4+ or CD8+ T cells [70].
- QF Protocol: Whole blood was incubated in QF tubes (Ag1 and Ag2) for 16-24 hours. Plasma IFN-γ concentrations were then measured via ELISA [70].
- Comparison Methodology: The qualitative (positive/negative) and quantitative results from both platforms were compared using positive percent agreement (PPA), negative percent agreement (NPA), and correlation analysis [70].
Performance Data and Functional Sensitivity Analysis
Table 3: Comparison of FC-ICS and QuantiFERON Assay Performance [70]
| Assay | Positive Results (n) | Positive Percent Agreement (PPA) | Negative Percent Agreement (NPA) | Correlation with Paired Assay |
|---|---|---|---|---|
| FC-ICS (CD4+) | 134 | 83% | 7% | No significant correlation |
| QuantiFERON (Ag1) | 120 | 83% | 7% | No significant correlation |
The FC-ICS assay demonstrated significantly higher clinical sensitivity, detecting more positive responses (134 vs. 120) than the QF test. A notable finding was the poor negative percent agreement (7%), indicating that nearly all samples classified as negative by one test were positive by the other, with most discordant results being FC-ICS positive/QF negative [70]. This suggests the FC-ICS platform may have a lower functional sensitivity (LLOQ) for detecting weak T-cell responses. Furthermore, the lack of correlation between IFN-γ+ T-cell frequencies and IFN-γ concentrations underscored that these assays measure different biological endpoints and are not directly interchangeable [70].
Figure 1: Comparative experimental workflows for T-cell immunoassays. The FC-ICS and QuantiFERON assays differ fundamentally in methodology and output, explaining their differing sensitivities [70].
Case Study 3: Minimal Residual Disease Assessment in Multiple Myeloma
Experimental Protocol and Real-World Sensitivity
This case study evaluates the real-life performance of a next-generation flow (NGF) cytometry assay for minimal residual disease (MRD) detection in multiple myeloma, benchmarked against the International Myeloma Working Group (IMWG) sensitivity requirement of 10â»âµ (1 abnormal cell in 100,000 normal cells) [69].
- NGF-MRD Protocol: The EuroFlow Consortium's NGF method uses a 2-tube, 8-color antibody panel to identify aberrant plasma cell populations in bone marrow aspirates. The protocol mandates the acquisition of at least 10 million total cells to achieve a theoretical sensitivity of 10â»âµ [69].
- Data Analysis: A retrospective review of over 13,000 bone marrow specimens analyzed internally and externally was conducted. The median number of events collected and the corresponding real-world sensitivity were calculated [69].
Performance Data and Achieved Sensitivity
Table 4: Real-World Sensitivity of FC MRD Testing in Myeloma [69]
| Sample Origin | Median Events Collected | 25th-75th Percentile | Achieved Sensitivity |
|---|---|---|---|
| Internal Specimens | 8.3 × 10ⶠ| 6.3 × 10ⶠ- 9.4 × 10ⶠ| 2.4 × 10â»â¶ |
| External Specimens | 7.0 × 10ⶠ| 4.7 × 10ⶠ- 8.6 × 10ⶠ| 2.8 × 10â»â¶ |
The data confirmed that the real-life sensitivity of the NGF MRD assay consistently exceeded the IMWG-defined minimum, achieving a median sensitivity of 2.4 × 10â»â¶ to 2.8 × 10â»â¶, which is closer to the 10â»â¶ sensitivity of the FDA-approved NGS-based clonoSEQ assay [69]. This demonstrates that with standardized protocols and adequate cell acquisition, flow cytometry can deliver exceptionally high functional sensitivity in a clinical setting, enabling reliable detection of MRD for disease monitoring.
Cross-Platform Comparison and Technical Considerations
Integrated Performance Analysis
Table 5: Comparative Analysis of Flow Cytometry Applications
| Application | Key Metric | Reported Performance | Factors Influencing Functional Sensitivity |
|---|---|---|---|
| Rare Tfh Cell Detection [68] | Inter-assay Precision (%CV) | 2.19% - 6.51% (for Tfh cells) | Cell pre-enrichment, sample stabilization, gating strategy |
| SARS-CoV-2 Serology [71] | Intra-/Inter-plate %CV | 3.16% - 6.71% / 3.33% - 5.49% | Bead antigen immobilization, detection antibody specificity |
| SARS-CoV-2 T-cell FC-ICS [70] | Positive Detection Rate | Higher than QF assay (134 vs 120) | Peptide stimulation efficiency, cytokine detection threshold |
| Myeloma MRD [69] | Achieved Sensitivity | 2.4 × 10â»â¶ to 2.8 × 10â»â¶ | Total events acquired, antibody panel design |
Strategic Selection Framework
The choice between immunoassay platforms and flow cytometry depends on the specific research or clinical question. Bead-based flow cytometry immunoassays are ideal for high-throughput, multiplexed quantification of soluble analytes like cytokines, offering excellent reproducibility (CVs of 3-7%) [71] [72]. In contrast, cell-based flow cytometry is indispensable for cellular phenotyping, rare event detection, and functional assays like ICS, providing a higher sensitivity for detecting cellular immune responses compared to bulk cytokine measurement assays [73] [70]. For ultimate sensitivity in detecting residual disease, high-sensitivity flow cytometry protocols that maximize event acquisition are required [69].
Figure 2: A decision framework for selecting appropriate assay platforms based on research requirements and desired outcomes.
The case studies presented herein demonstrate that the framework for verifying functional sensitivity with interassay precision profiles is universally applicable across diverse flow cytometry and immunoassay platforms. The data confirm that high-sensitivity flow cytometry, when properly validated, can achieve exceptional precision for rare cell detection and surpass mandated sensitivity thresholds in clinical applications like MRD monitoring. Furthermore, comparisons with alternative immunoassay platforms reveal that methodology and readout fundamentally influence sensitivity, necessitating careful platform selection based on the specific biological question. For researchers and drug developers, these findings underscore the importance of rigorous, standardized validation incorporating precision profiles to establish the true functional sensitivity of an assay, thereby ensuring the reliability of data for both basic research and clinical decision-making.
In the demanding landscape of pharmaceutical development and quality control, the validation of analytical methods is paramount. It confirms that a procedure is fit for its intended purpose, ensuring the reliability of data that underpins critical decisions on drug safety, efficacy, and quality [74] [75]. Traditional validation approaches, while established, often struggle with the complexity and volume of modern analytical data. The core of this challenge lies in conclusively verifying performance characteristics such as functional sensitivity—the lowest analyte concentration that can be measured with clinically useful precision—a parameter far more informative than the basic detection limit [1] [9].
This guide explores the transformative role of Digital Validation Tools (DVTs) and Artificial Intelligence (AI) in overcoming these challenges. By automating complex statistical analyses and enabling a proactive, data-driven approach, these technologies are future-proofing the validation process, making it more robust, efficient, and aligned with the principles of Analytical Lifecycle Management [75] [76].
Core Concepts: Functional Sensitivity and the Analytical Target Profile
Distinguishing Sensitivity Measures
A critical step in method validation is understanding the hierarchy of sensitivity. As outlined in the International Council for Harmonisation (ICH) Q2(R1) guideline, validation requires assessing multiple interrelated performance characteristics [74] [75].
- Analytical Sensitivity (Limit of Detection, LoD): Defined as the lowest concentration that can be distinguished from background noise. It is a measure of detectability but offers no guarantee of reliable quantification [1] [9].
- Functional Sensitivity: This concept, developed for clinical assays like TSH, moves beyond mere detection. It is defined as the lowest concentration at which an assay can report clinically useful results, with useful results being determined by an acceptable level of imprecision, typically a maximum coefficient of variation (CV) of 20% [1]. This represents the practical lower limit of the reportable range.
- Limit of Quantification (LoQ): The lowest level of analyte that can be quantified with acceptable precision and trueness. Functional sensitivity is closely related to the LoQ, as both define a lower limit for reliable numerical results [75] [9].
Table 1: Comparison of Key Sensitivity and Precision Parameters in Method Validation.
| Parameter | Formal Definition | Key Objective | Typical Assessment |
|---|---|---|---|
| Analytical Sensitivity (LoD) | Lowest concentration distinguishable from background noise [1]. | Establish detection capability. | Measured by assaying a blank sample, calculating mean + 2 standard deviations (for immunometric assays) [1]. |
| Functional Sensitivity | Lowest concentration measurable with a defined precision (e.g., CV ≤ 20%) [1]. | Determine the clinically useful reporting limit. | Achieved by repeatedly testing low-concentration samples over multiple runs and identifying where the inter-assay CV meets the target [1]. |
| Precision (Repeatability) | Closeness of agreement between a series of measurements from multiple sampling under identical conditions [74]. | Measure intra-assay variability. | Expressed as the CV% between a series of measurements from the same homogeneous sample [74]. |
| Intermediate Precision | Closeness of agreement under varying conditions (different days, analysts, equipment) [74]. | Measure inter-assay variability in a single lab. | Incorporates random events and is crucial for establishing the robustness of a method and its functional sensitivity [74]. |
The Analytical Target Profile (ATP) as a Validation Framework
The Analytical Target Profile (ATP) is a foundational concept in a modern, quality-by-design approach to validation. The "ATP states the required quality of the reportable value produced by an analytical procedure in terms of the target measurement uncertainty (TMU)" [76]. Instead of validating a specific method, the ATP defines the performance requirements upfront. Any method that can meet these TMU criteria is deemed suitable. This shifts the focus from a retrospective "tick-box" exercise to a proactive design process, where precision requirements like those for functional sensitivity are derived from the specification limits critical to patient safety and product quality [76].
The Digital Toolbox: A Comparative Guide
The market offers a range of tools, from enterprise data intelligence platforms to specialized AI-powered automation software. The choice depends on the specific validation and data governance needs.
Table 2: Comparison of Digital Validation and Data Intelligence Tools.
| Tool Name | Primary Focus | Key AI/Validation Features | Reported Benefits & Use Cases |
|---|---|---|---|
| Collibra Data Intelligence Cloud [77] | Enterprise metadata management and governance. | Automated metadata harvesting, policy-driven validation rules, AI-powered data quality scoring. | Ensures metadata adherence to predefined standards; provides a holistic view of data lineage for compliance. |
| Atlan [77] | Modern data catalog with built-in validation. | Automated metadata extraction, customizable data quality checks, AI-powered classification. | Facilitates collaborative data quality workflows; enforces metadata rules directly within the data catalog. |
| Informatica [78] [77] | Comprehensive data integration and quality. | Robust data cleansing and profiling, machine learning-powered metadata discovery and validation. | Scalable for large enterprises; integrates validation throughout the data lifecycle. |
| Mabl [79] | Autonomous test automation for software. | AI-driven test creation from plain English, self-healing tests, autonomous root cause analysis. | Reduces test maintenance burden; autonomously generates and adapts test suites. |
| BlinqIO [79] | AI-powered test generation. | Generates test scenarios and code from requirements, self-healing capabilities, "virtual testers." | Integrates with development workflows (e.g., Cucumber); significantly boosts test creation efficiency. |
Experimental Protocols Enabled by DVTs
Digital tools standardize and expedite core validation experiments. Below is a detailed protocol for establishing functional sensitivity, a task greatly enhanced by DVTs.
Protocol: Determining Functional Sensitivity via Interassay Precision Profiles
- Objective: To determine the lowest analyte concentration at which the interassay (intermediate) precision has a coefficient of variation (CV) of ≤ 20% [1].
- Sample Preparation: Prepare a series of samples (e.g., patient serum pools or spiked samples) with analyte concentrations spanning the expected low end of the measuring range. Using a true zero (blank) sample is insufficient for this determination [1].
- Experimental Design:
- Analyze each sample in multiple replicates (e.g., n=2-3) over at least 10-20 independent runs performed on different days, by different analysts, and using different equipment where applicable [74] [1].
- This design directly incorporates the variables defining "intermediate precision" as per ICH Q2(R1) [74].
- Data Collection: For each sample at each concentration level, record the measured analyte concentration from every run.
- Statistical Analysis (Automated by DVT):
- For each concentration level, calculate the mean and standard deviation (SD) of all results across all runs.
- Calculate the CV% for each concentration level using the formula: CV% = (Standard Deviation / Mean) * 100 [74].
- Determination of Functional Sensitivity:
AI-Driven Transformation of Validation Workflows
Artificial Intelligence is not just automating existing tasks but fundamentally reshaping the validation workflow from a linear, sequential process to an intelligent, iterative cycle.
Key AI applications in this lifecycle include:
- Predictive Modeling for ATP: AI models can analyze historical validation data to recommend scientifically sound TMU and functional sensitivity targets during the ATP phase, moving beyond arbitrary "capability-based" limits [76].
- Automated Data Analysis: Tools can automatically ingest data from analytical instruments, calculate complex statistical parameters like interassay CV%, generate precision profiles, and compare results against the ATP's acceptance criteria, drastically reducing human effort and error [78] [80].
- Continuous Monitoring and Self-Healing: In advanced applications, AI can monitor control charts and method performance in real-time, flagging deviations or "drift" before they lead to out-of-specification (OOS) results. Some test automation platforms even feature "self-healing" scripts that can adapt to minor changes in the analytical system [79].
The Scientist's Toolkit: Essential Digital Research Reagents
Just as a laboratory requires high-quality physical reagents, a modern validation scientist requires a suite of digital "reagents" – software and data solutions that are essential for conducting rigorous, AI-enhanced validation studies.
Table 3: Key Digital "Research Reagent" Solutions for Modern Validation.
| Tool Category | Specific Examples | Function in Validation |
|---|---|---|
| AI-Powered Spreadsheet Assistants | Numerous.ai [80] | Validates, cleans, and structures data directly within spreadsheets (Excel/Sheets); uses pattern recognition to find hidden errors. |
| Automated Test Agents | Mabl, testers.ai [79] | Acts as an autonomous test engineer; generates and executes test cases based on requirements, covering edge cases and statistically likely bugs. |
| Metadata & Governance Platforms | Collibra, Informatica [78] [77] | Ensures data integrity and compliance by automatically enforcing metadata validation rules and tracking data lineage across systems. |
| Statistical Computing Environments | R, Python (Pandas, SciPy) | Provides a flexible, scriptable environment for performing custom statistical analysis, including generating precision profiles and calculating TMU. |
| Electronic Lab Notebooks (ELN) | Many commercial solutions | Provides a structured, digital framework for documenting the entire validation lifecycle, ensuring data traceability and ALCOA+ principles. |
The convergence of Digital Validation Tools and Artificial Intelligence marks a pivotal shift in pharmaceutical analysis. By moving from static, document-centric validation to a dynamic, data-driven lifecycle managed by intelligent tools, organizations can effectively future-proof their quality control systems. The ability to automatically verify critical parameters like functional sensitivity against a predefined Analytical Target Profile ensures methods are not only validated but remain robust and reliable throughout their entire use. For researchers and drug development professionals, embracing these technologies is no longer optional but essential for achieving new levels of efficiency, compliance, and most importantly, confidence in the data that safeguards public health.
Conclusion
Verifying functional sensitivity through robust interassay precision profiles is not merely a regulatory checkbox but a fundamental practice for ensuring the reliability of data used in critical drug development decisions. This synthesis of foundational concepts, methodological rigor, troubleshooting acumen, and statistical validation empowers scientists to confidently define the lower limits of their assays. Future directions will be shaped by the increasing adoption of digital validation tools for enhanced data integrity and efficiency, the application of AI for predictive modeling of assay performance, and the need to adapt these principles for novel modalities like cell and gene therapies. Mastering this process is essential for delivering clinically meaningful and trustworthy bioanalytical results.
References
- 1. Analytical Sensitivity, Functional Sensitivity [https://www.dpcweb.com/documents/news&views/spring01/performancemeasures.html]
- 2. Is Your ELISA Kit Qualified and Validated? [https://www.thermofisher.com/blog/behindthebench/is-your-elisa-kit-qualified-and-validated/]
- 3. Importance of Verification for High-Sensitivity Immunoassays [https://www.sigmaaldrich.com/US/en/technical-documents/product-supporting/smc-technologies/importance-of-verification-for-high-sensitivity-immunoassays?srsltid=AfmBOoqmavM6lF1eChe6b3LOVrJwNts6u82K_bPAhHzp9FzevqIE8s5X]
- 4. Verification of a Novel High Sensitivity Troponin I Assay for ... [https://pubmed.ncbi.nlm.nih.gov/40697011/]
- 5. Sensitive Detection of SARS-CoV-2 Using a ... [https://www.sciencedirect.com/science/article/abs/pii/S0925400525014078]
- 6. Dual-functional probe for sensitive detection of MCF-7 cells ... [https://www.nature.com/articles/s41598-025-90575-2]
- 7. PharmaFormer predicts clinical drug responses through ... [https://www.nature.com/articles/s41698-025-01082-6]
- 8. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 9. How do analytical, diagnostical, and functional sensitivity differ? [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/sensitivities]
- 10. The precision study: examining the inter- and intra-assay ... [https://pubmed.ncbi.nlm.nih.gov/24088217/]
- 11. Clinical performance validation and four diagnostic ... [https://www.nature.com/articles/s41598-025-99273-5]
- 12. Development and Validation of a Third Generation ... [https://www.annclinlabsci.org/content/34/1/67.full]
- 13. Imprecision Profiling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556580/]
- 14. Validation of the i-Tracker Drug and Total Anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523426/]
- 15. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 16. Q2(R2) Validation of Analytical Procedures March 2024 [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2r2-validation-analytical-procedures]
- 17. M10 Bioanalytical Method Validation and Study Sample ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m10-bioanalytical-method-validation-and-study-sample-analysis]
- 18. EP15 | User Verification of Precision and Estimation of Bias [https://clsi.org/shop/standards/ep15/]
- 19. FDA Guidance for Industry on Bioanalytical Method ... [https://labs.iqvia.com/blog/fda-guidance-bioanalytical-method-validation-biomarkers]
- 20. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 21. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 22. Comprehensive performance evaluation of a high ... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1609142/full]
- 23. A Mass Spectrometry–Based Multiplexed Targeted Assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597561/]
- 24. UHPLC-MS/MS for Antipsychotic Drug Monitoring [https://www.mdpi.com/2077-0383/14/21/7544]
- 25. Data Collection Theory in Healthcare Research: The Minimum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9680355/]
- 26. CLSI EP05-A2 - Evaluation of Precision Performance ... [https://webstore.ansi.org/standards/clsi/clsiep05a2?srsltid=AfmBOopzX4wPc3rkypvU8ue71k8mNbtKhvuw_P2lGS_C77HGeEAnN0N5]
- 27. CLSI EP15-A2 - User Verification of Performance for ... [https://webstore.ansi.org/standards/clsi/clsiep15a2?srsltid=AfmBOoolzsWxBIKkBAj74jlX3-JMrKpG-9yDNpSE1qGdbRxpSiTgLJiF]
- 28. EP05 | Evaluation of Precision of Quantitative ... [https://clsi.org/shop/standards/ep05/]
- 29. CLSI faces the Challenge of Quality - Westgard QC [https://www.westgard.com/essays/trends/essay112.html]
- 30. Evaluating Assay Precision - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556577/]
- 31. testing - Wikipedia Functional drug sensitivity [https://en.wikipedia.org/wiki/Functional_drug_sensitivity_testing]
- 32. %CV in ELISA: How to Reduce Them and Why They're ... [https://www.enzo.com/note/cv-in-elisa-how-to-reduce-them-and-why-theyre-important/]
- 33. ELISA Assay Qualification: Precision & Reproducibility Tips [https://www.cygnustechnologies.com/evaluating-precision-and-reproducibility-in-your-elisa?srsltid=AfmBOoqqvFC5tdr5Dv5yjTUbSPFsQnwYtx2DtTnRPQLzMhv_r6Vztv9s]
- 34. Validation of an impedance-based in vitro potency assay ... [https://www.axionbiosystems.com/resources/application-note/validation-impedance-based-vitro-potency-assay-repeatability-and]
- 35. Are You Validating Methods for Bioanalytical Samples? [https://www.chromatographyonline.com/view/are-you-validating-methods-bioanalytical-samples]
- 36. Large Molecule Run Acceptance: Recommendation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3933574/]
- 37. ELISA Assay Qualification: Precision & Reproducibility Tips [https://www.cygnustechnologies.com/evaluating-precision-and-reproducibility-in-your-elisa?srsltid=AfmBOoq4iZHP0QFHHffdUgv1TEj6nfnyUy4S_obqcJMQ0I_uBmfYMhYF]
- 38. Interlaboratory/intermethod differences in functional sensitivity ... [https://pubmed.ncbi.nlm.nih.gov/7882510/]
- 39. Know Your Techniques: Accuracy, Precision, and Using the Right Instrument - inChemistry [https://inchemistry.acs.org/college-life/accuracy-vs-precision.html]
- 40. Five Possible Causes Why Lab Analysts Are Having Poor Precision in Mercury Analysis : NIC [https://www.hg-nic.com/poor-precision-mercury-analysis/]
- 41. Comparison of Precision and Accuracy of Five Methods to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7746559/]
- 42. Assessing variations in manual pipetting [https://pmc.ncbi.nlm.nih.gov/articles/PMC10569977/]
- 43. Optimization of a rapid sample pretreatment for the ... [https://pubmed.ncbi.nlm.nih.gov/34325248/]
- 44. Managing critical reagents through drug development [https://www.drugdiscoverytrends.com/managing-critical-reagents-through-drug-development/]
- 45. Stability: Recommendation for Best Practices and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4012051/]
- 46. Automated Pipetting Systems - Comparison Guide [https://www.sptlabtech.com/automated-pipetting-the-complete-guide]
- 47. Critical Reagents [https://www.bioagilytix.com/techniques/quality-systems/critical-reagents/]
- 48. Stable Ground—The Importance of Stability Testing for ... [https://www.genengnews.com/topics/bioprocessing/stable-ground-the-importance-of-stability-testing-for-custom-gmp-reagents/]
- 49. ASSIST | Automating multichannel pipettes | INTEGRA [https://www.integra-biosciences.com/united-states/en/pipetting-robots/assist]
- 50. Compensate for or Minimize Matrix Effects? Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412464/]
- 51. Matrix Effects on Quantitation in Liquid Chromatography [https://www.chromatographyonline.com/view/matrix-effects-on-quantitation-in-liquid-chromatography-sources-and-solutions]
- 52. 高通é‡æ•°æ®ä¸æ‰¹æ¬¡æ•ˆåº”的鉴定和处ç†- 系列总结和更新原创 [https://blog.csdn.net/qazplm12_3/article/details/140152645]
- 53. 色谱æˆåŠŸçš„工具。支æŒå¸¸è§„分æžä¸çš„æ•°æ®è´¨é‡çš„三ç§æ–¹æ³• [https://www.waters.com/blog/zh/tools-for-chromatographic-success-three-ways-to-support-data-quality-in-routine-analysis/?srsltid=AfmBOorj4yZ9ygqv_2BGCfDLUwMoiTMqkJlM2PuZz7g_Q5meNb25vUFS]
- 54. Understanding Pharmaceutical Quality by Design - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070262/]
- 55. Good Clinical Practice Insights from US FDA, MHRA UK, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616134/]
- 56. Synergy of QbD, RBM, and RBQM in Trials [https://cyntegrity.com/synergy-of-qbd-rbm-and-rbqm-in-trials/]
- 57. FDA Publishes ICH E6(R3): What it Means for U.S. Clinical ... [https://acrpnet.org/2025/09/16/fda-publishes-ich-e6r3-what-it-means-for-u-s-clinical-trials]
- 58. Quality by Design Is the Industry's Best Bet for Clinical Trials [https://www.tritrials.com/quality-by-design-is-the-industrys-best-bet-for-clinical-trials/]
- 59. Role of Functional Assays in Antibody-Based Drug ... [https://precisionantibody.com/the-role-of-functional-assays-in-antibody-based-drug-development/]
- 60. Functional precision medicine using drug sensitivity testing ... [https://ecancer.org/en/news/21269-functional-precision-medicine-using-drug-sensitivity-testing-enables-tailoring-of-therapy-for-leukaemia-patients]
- 61. Analytical Performance of the New Sysmex High-Sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346695/]
- 62. Differentiating between analytical and diagnostic ... [https://pubmed.ncbi.nlm.nih.gov/25257670/]
- 63. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 64. LLM benchmarks in 2025: What they prove and what your ... [https://www.lxt.ai/blog/llm-benchmarks/]
- 65. What is Comparative Analysis? Guide with Examples [https://dovetail.com/research/comparative-analysis/]
- 66. Benchmarking AI Agents in 2025: Top Tools, Metrics & ... [https://metadesignsolutions.com/benchmarking-ai-agents-in-2025-top-tools-metrics-performance-testing-strategies/]
- 67. 2025 search tool benchmark: key metrics to evaluate ... [https://www.glean.com/blog/2025-search-tool-benchmark-key-metrics-to-evaluate-accuracy-and-speed]
- 68. Validation of High-sensitivity Flow Cytometry for Reliable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10345173/]
- 69. Real-life sensitivity of flow cytometry minimal residual ... [https://www.nature.com/articles/s41408-024-01113-8]
- 70. Performance comparison of a flow cytometry immunoassay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8853233/]
- 71. A Novel Flow Cytometry Array for High Throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567774/]
- 72. Comparing Flow Cytometry QBeads PlexScreen Assays ... [https://www.sciencedirect.com/science/article/pii/S247255522206885X]
- 73. Performance of a flow cytometry-based immunoassay for ... [https://www.nature.com/articles/s41598-021-04565-1]
- 74. Tips and Tricks for Validation of Quality Control Analytical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6142742/]
- 75. Some good validation practices for analytical procedures [https://www.a3p.org/en/bonnes-pratiques-validation/]
- 76. Analytical Target Profile: establishment of precision ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708518315371]
- 77. Top 5 Metadata Validation Tools for 2025 [https://ones.com/blog/metadata-validation-tools-comparison-guide/]
- 78. Top 6 Automated Data Validation Tools for 2025 [https://aqua-cloud.io/automated-data-validation/]
- 79. 11 Best AI Test Automation Tools for 2025: The Third Wave [https://testguild.com/7-innovative-ai-test-automation-tools-future-third-wave/]
- 80. The Best 5 Data Validation Tools in 2025 [https://numerous.ai/blog/data-validation-tools]