Advanced HPLC Methods for Simultaneous Determination of Cardiovascular Drugs in Human Plasma: Development, Validation, and Application
This article provides a comprehensive resource for researchers and pharmaceutical scientists on developing and validating High-Performance Liquid Chromatography (HPLC) methods for the simultaneous quantification of cardiovascular drugs in human plasma.
Advanced HPLC Methods for Simultaneous Determination of Cardiovascular Drugs in Human Plasma: Development, Validation, and Application
Abstract
This article provides a comprehensive resource for researchers and pharmaceutical scientists on developing and validating High-Performance Liquid Chromatography (HPLC) methods for the simultaneous quantification of cardiovascular drugs in human plasma. Covering foundational principles to advanced applications, it details innovative methodologies including dual UV/fluorescence detection and HPLC-MS/MS for enhanced sensitivity and specificity. The content explores method optimization using green chemistry principles, troubleshooting common challenges, and rigorous validation per ICH, FDA, and EMA guidelines. It also presents comparative analyses of various techniques (RP-HPLC, MEKC) and discusses the critical role of therapeutic drug monitoring in personalizing treatment for hypertension, heart failure, and other cardiovascular diseases to improve patient outcomes.
The Critical Need for Plasma Drug Monitoring in Cardiovascular Disease Management
Global Burden of Cardiovascular Diseases and Polypharmacy Trends
The rising global burden of cardiovascular diseases (CVDs) presents a critical public health challenge, driving increased reliance on pharmacotherapy and leading to concerning polypharmacy trends. Recent projections indicate that between 2025 and 2050, the global cardiovascular prevalence will increase by approximately 90.0%, with an estimated 35.6 million cardiovascular deaths in 2050 alone [1]. This escalating disease burden necessitates complex medication regimens, particularly for secondary prevention of atherosclerotic cardiovascular disease (ASCVD).
Concurrent with rising CVD prevalence, medication use patterns have shifted significantly. A 25-year national trends study in the United States revealed that 48.7% of adults use at least one prescription medication, while 11.1% experience polypharmacy (concurrent use of ≥5 medications), with both metrics showing significant increases over the study period [2]. These trends underscore the urgent need for advanced analytical methods to monitor drug therapy and optimize treatment outcomes in patients with cardiovascular conditions.
Global Burden of Cardiovascular Diseases
Current Prevalence and Future Projections
Cardiovascular diseases remain the leading cause of mortality and disability worldwide. Analysis of historical data from the Global Burden of Disease study provides concerning projections for the coming decades [1]:
Table 1: Projected Global Cardiovascular Disease Burden (2025-2050)
| Metric | 2025 Baseline | 2050 Projection | Percentage Change |
|---|---|---|---|
| Total CVD Deaths | 20.5 million | 35.6 million | +73.4% |
| Crude DALYs | - | - | +54.7% |
| Age-Standardized Mortality | - | - | -30.5% |
| Age-Standardized DALYs | - | - | -29.6% |
The disparity between crude and age-standardized metrics indicates that the ageing global population is a primary driver of increasing CVD prevalence, rather than increasing age-specific risk [1]. Ischemic heart disease is projected to remain the leading cause of cardiovascular deaths, accounting for approximately 20 million deaths by 2050.
Key Risk Factors and Regional Variations
High systolic blood pressure persists as the predominant cardiovascular risk factor, projected to drive 18.9 million deaths in 2050 [1]. Other significant risk factors include dietary risks, high cholesterol, and high body-mass index, the latter showing particularly rapid increase in certain regions.
Significant geographical disparities exist, with the Central Europe, Eastern Europe, and Central Asia super-region projected to incur the highest age-standardized cardiovascular mortality rate in 2050 (305 deaths per 100,000 population) [1]. This regional variation highlights the need for targeted, context-specific interventions.
Polypharmacy Trends in Cardiovascular Care
Prevalence and Demographic Patterns
Polypharmacy has become increasingly prevalent in CVD management, particularly as treatment guidelines recommend multi-drug regimens for ASCVD secondary prevention. Recent studies demonstrate notable patterns across demographic groups [2]:
Table 2: Polypharmacy Patterns in Cardiovascular Care
| Demographic Factor | Pattern | Prevalence Ratio |
|---|---|---|
| Sex | Women have higher prevalence | PR=1.15 (vs men) |
| Race/Ethnicity | Black adults have lower prevalence but faster increasing rates | PR=0.92 (vs White adults) |
| Socioeconomic Status | Inverse association with family income | p<0.001 |
| Temporal Trend | Consistent increases across all subgroups | p<0.001 for trend |
The steeper increases in medication use among men and Black adults are narrowing historical demographic gaps in medication exposure [2].
Mortality Risk and Confounding Factors
The relationship between polypharmacy and mortality requires careful interpretation due to substantial confounding. A recent Danish study illustrated that basic adjustment for comorbidities markedly attenuated the association between polypharmacy and mortality, reducing the odds ratio from 10.39 (95% CI: 9.79-11.03) to 1.34 (95% CI: 1.25-1.43) in community-dwelling older adults [3]. This suggests that the association is strongly influenced by underlying morbidity rather than medication count alone.
Therapeutic Strategies and Fixed-Dose Combinations
Fixed-Dose Combination (FDC) Therapy
Fixed-dose combination therapy, also known as polypill therapy, has emerged as a promising strategy to address both CVD burden and polypharmacy challenges. FDCs typically combine at least one blood pressure-lowering drug with one lipid-lowering drug in a single pill [4].
A recent meta-analysis of 26 randomized trials (n=27,317 participants) demonstrated that FDC therapy was associated with [4]:
- Lower LDL cholesterol and systolic blood pressure
- Higher medication adherence rates
- 11% lower risk of all-cause mortality in primary prevention populations (5.6% vs 6.3%)
- 29% lower risk of fatal and nonfatal ASCVD events (6.1% vs 8.4%)
Implementation in Challenging Settings
Humanitarian settings present particular challenges for CVD management. A pre-post implementation study in Lebanese clinics serving Syrian refugees demonstrated that introducing FDC medications (atorvastatin, aspirin, ramipril) improved medication adherence by 23%, reduced non-HDL cholesterol by 0.28 mmol/L, and lowered systolic blood pressure by 2.89 mm Hg over 12 months [5]. This evidence supports wider implementation of FDC strategies in resource-limited settings.
HPLC Method for Simultaneous Determination of Cardiovascular Drugs
Analytical Challenges and Requirements
The increasing complexity of cardiovascular pharmacotherapy necessitates robust analytical methods for therapeutic drug monitoring. Simultaneous determination of multiple cardiovascular drugs presents significant challenges due to their diverse chemical structures and physicochemical properties.
An innovative high-performance liquid chromatography (HPLC) method with dual detection has been developed specifically for quantifying cardiovascular drugs in human plasma, addressing the need for therapeutic drug monitoring in polypharmacy patients [6].
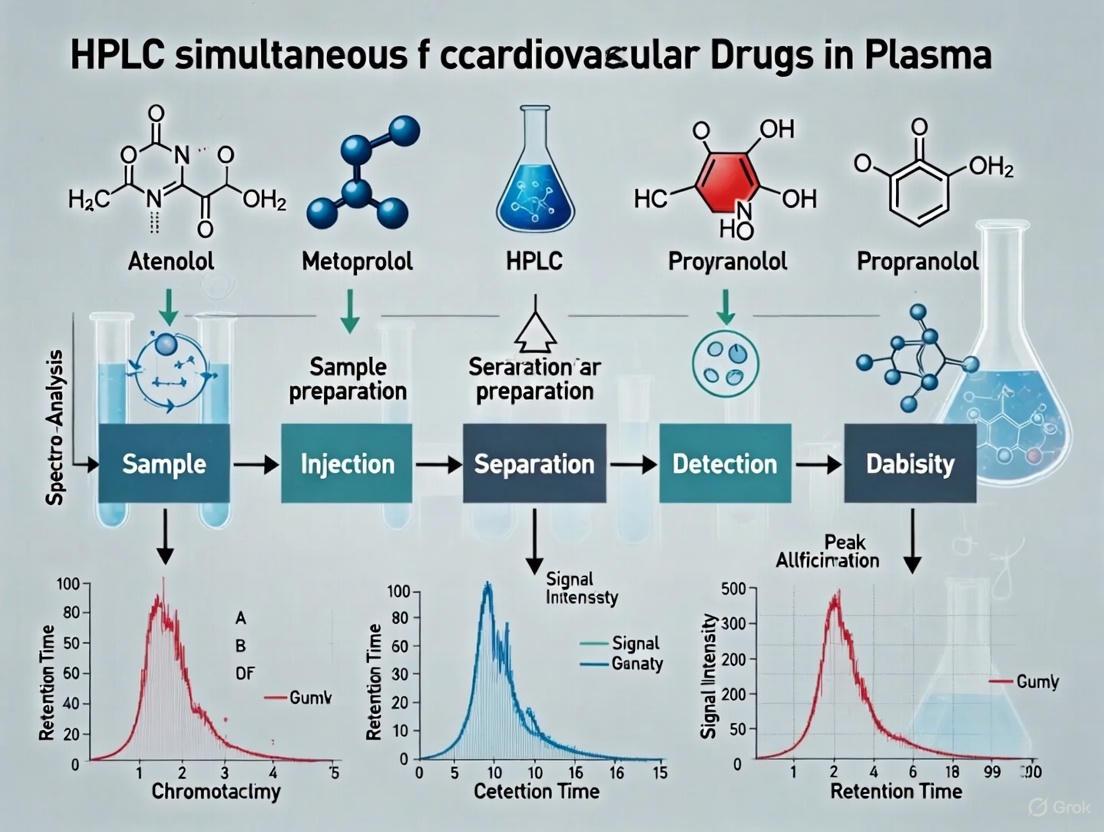
Diagram 1: CVD Management and Analytical Method Interrelationship
Developed HPLC Method for Cardiovascular Drugs
A highly sensitive HPLC method was developed for the concurrent determination of four cardiovascular drugs: bisoprolol (BIS), amlodipine besylate (AML), telmisartan (TEL), and atorvastatin (ATV) in human plasma [6].
Table 3: HPLC Method Parameters for Cardiovascular Drug Analysis
| Parameter | Specification | Experimental Condition |
|---|---|---|
| Column | Thermo Hypersil BDS C18 | 150 × 4.6 mm, 5.0 μm |
| Mobile Phase | Ethanol:buffer (40:60) | 0.03 M potassium phosphate buffer (pH 5.2) |
| Flow Rate | 0.6 mL/min | Isocratic elution mode |
| Detection | Dual detection system | UV (210-260 nm) and fluorescence |
| Runtime | <10 minutes | Economical for routine analysis |
| Linearity Range | Drug-dependent | BIS/AML: 5-100 ng/mL; TEL: 0.1-5 ng/mL; ATV: 10-200 ng/mL |
The method was validated according to International Council for Harmonisation (ICH) guidelines and demonstrated excellent accuracy, precision, and sensitivity suitable for therapeutic drug monitoring in clinical settings [6].
Experimental Protocol: HPLC Method for Cardiovascular Drugs
Materials and Reagents
Chemical Standards:
- Bisoprolol fumarate (99.24% purity)
- Amlodipine besylate (99.78% purity)
- Telmisartan (99.69% purity)
- Atorvastatin calcium trihydrate (99.13% purity)
Solvents and Buffers:
- Ethanol (HPLC grade)
- Potassium dihydrogen phosphate (for 0.03 M buffer, pH 5.2)
- Diethyl ether and dichloromethane (extraction solvents)
Biological Matrix:
- Human plasma (stored at -20°C until analysis)
Sample Preparation Protocol
The sample preparation employs a two-step liquid-liquid extraction (LLE) technique [6]:
Protein Precipitation:
- Combine 200 μL plasma + 50 μL working standard + 600 μL absolute ethanol
- Vortex mix thoroughly
- Centrifuge at 3500 rpm for 2 minutes
First Extraction:
- Add 1.0 mL diethyl ether to supernatant
- Vortex for 5 minutes
- Centrifuge at 3500 rpm for 5 minutes at 0°C
- Collect organic phase
Second Extraction:
- Add 0.5 mL dichloromethane to remaining aqueous phase
- Vortex for 5 minutes
- Centrifuge at 3500 rpm for 5 minutes at 0°C
- Collect organic phase
Evaporation and Reconstitution:
- Combine organic phases
- Evaporate under nitrogen stream at 40°C
- Reconstitute residue in 500 μL ethanol
- Vortex for 2 minutes
- Inject 20 μL into HPLC system
Instrumentation and Chromatographic Conditions
HPLC System: Waters Alliance 2695 HPLC system equipped with:
- Auto-sampler injector
- Quaternary solvent delivery pump
- Column temperature controller
- Dual detection: Photodiode array detector + Multi-wavelength fluorescence detector
Fluorescence Detection Parameters [6]:
- Bisoprolol: λex/λem = 227/298 nm
- Telmisartan: λex/λem = 294/365 nm
- Atorvastatin: λex/λem = 274/378 nm
- Amlodipine: λex/λem = 361/442 nm
Diagram 2: HPLC Analytical Workflow for Cardiovascular Drugs
Method Validation
The method was comprehensively validated according to ICH guidelines [6]:
- Linearity: Established over concentration ranges relevant to therapeutic monitoring
- Accuracy and Precision: Evaluated through recovery studies and relative standard deviation
- Specificity: Assessed by comparing chromatograms of blank plasma with spiked samples
- Sensitivity: Determined through limit of detection and quantification measurements
- Stability: Confirmed under various storage conditions
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for HPLC Analysis of Cardiovascular Drugs
| Reagent/Material | Function | Application Note |
|---|---|---|
| Hypersil BDS C18 Column | Stationary phase for chromatographic separation | 150 × 4.6 mm, 5 μm particle size provides optimal resolution [6] |
| Ethanol (HPLC Grade) | Mobile phase component, sample reconstitution | More sustainable alternative to acetonitrile [6] |
| Potassium Dihydrogen Phosphate | Buffer component for mobile phase | Maintains pH at 5.2 for optimal separation [6] |
| Diethyl Ether & Dichloromethane | Liquid-liquid extraction solvents | Efficient extraction of multiple drug classes [6] |
| Human Plasma | Biological matrix for method validation | Sourced from accredited blood banks [6] |
| Fluorescence Detector | Enhanced specificity and sensitivity | Multi-wavelength capability for diverse analytes [6] |
Application in Cardiovascular Research and Clinical Practice
The simultaneous HPLC method for cardiovascular drugs addresses critical needs in both research and clinical settings:
Clinical Research Applications:
- Therapeutic drug monitoring in polypharmacy patients
- Drug interaction studies in complex regimens
- Adherence assessment in clinical trials
- Pharmacokinetic studies of fixed-dose combinations
Public Health Implications:
- Monitoring medication safety in vulnerable populations
- Evaluating prescribing patterns across demographic groups
- Informing strategies to mitigate polypharmacy risks
- Supporting implementation of fixed-dose combination therapies
The method's capability to quantify drugs from different cardiovascular classes simultaneously makes it particularly valuable for studying patients on ASCVD secondary prevention regimens, who often require multiple medications targeting different pathological pathways [5] [4].
The escalating global burden of cardiovascular diseases and concurrent rise in polypharmacy present interconnected challenges requiring innovative approaches to medication management and monitoring. Advanced analytical methods, such as the HPLC technique described herein, provide essential tools for therapeutic drug monitoring in patients with complex cardiovascular medication regimens.
Fixed-dose combination therapies represent a promising strategy to mitigate polypharmacy-associated challenges while improving cardiovascular outcomes. The validated HPLC method for simultaneous determination of multiple cardiovascular drugs in plasma supports both clinical management and research initiatives aimed at optimizing therapy for the growing population of patients with cardiovascular diseases.
As CVD prevalence continues to rise globally, particularly with aging populations, the integration of robust analytical methods with evidence-based therapeutic strategies will be essential for addressing the dual challenges of cardiovascular disease burden and appropriate polypharmacy management.
Cardiovascular diseases (CVDs) remain the leading cause of global mortality, accounting for approximately 17.9 million deaths annually [7]. Effective management of these conditions relies heavily on pharmacotherapy, with key drug classes including beta-blockers, calcium channel blockers (CCBs), angiotensin II receptor blockers (ARBs), and statins forming the cornerstone of treatment [8] [9] [10]. The therapeutic monitoring of these medications is crucial for optimizing efficacy and minimizing adverse effects, particularly given that patients often require multi-drug regimens [6]. This application note details the pharmacology and presents optimized high-performance liquid chromatography (HPLC) protocols for the simultaneous determination of these cardiovascular drugs in plasma, supporting advanced research and drug development initiatives.
Pharmacological Profiles of Major Cardiovascular Drug Classes
Beta-Blockers (β-Adrenergic Receptor Antagonists)
Beta-blockers function as competitive antagonists at β-adrenergic receptors, effectively reducing sympathetic nervous system activity [11]. Their primary therapeutic effects include reducing heart rate, blood pressure, and myocardial contractility. These drugs are highly heterogeneous with varying potency, selectivity, and pharmacokinetic profiles [11].
- Generations and Selectivity: First-generation beta-blockers (e.g., propranolol) are non-selective, affecting both β1 and β2 receptors. Second-generation agents (e.g., metoprolol, bisoprolol) demonstrate cardioselectivity (preferential β1 blockade), while third-generation drugs (e.g., carvedilol) feature additional vasodilatory properties via α1-adrenergic receptor blockade [11] [7].
- Toxicological Considerations: Beta-blocker poisoning can lead to fatal hypotension and cardiac rhythm disturbances, necessitating highly sensitive analytical methods for detection in biological samples, with therapeutic concentrations typically ranging from 0.001–5 µg/mL [11].
Calcium Channel Blockers (CCBs)
CCBs inhibit the inward movement of calcium through L-type voltage-gated calcium channels in vascular smooth muscle and cardiac cells, resulting in vasodilation and reduced cardiac contractility [8] [12].
- Classification: CCBs are categorized into dihydropyridines (e.g., amlodipine, nifedipine) which primarily act as peripheral vasodilators, and non-dihydropyridines (e.g., verapamil, diltiazem) which predominantly affect cardiac conduction and contractility [8] [12].
- Cardiovascular Effects: DHP-CCBs exert potent vasodilatory effects with minimal direct cardiac impact, making them particularly effective for hypertension management. Non-DHP-CCBs demonstrate strong inhibitory effects on the sinoatrial and atrioventricular nodes, making them useful for rate control in atrial arrhythmias [8] [12].
Angiotensin II Receptor Blockers (ARBs)
ARBs selectively inhibit the binding of angiotensin II to the angiotensin type 1 (AT1) receptor, leading to vasodilation, reduced aldosterone secretion, and decreased blood pressure [9] [13].
- Mechanism of Action: By blocking AT1 receptors, ARBs prevent the vasoconstrictive, sodium-retentive, and aldosterone-secreting effects of angiotensin II. This mechanism differs from ACE inhibitors as ARBs do not inhibit bradykinin breakdown, resulting in a lower incidence of cough as a side effect [9].
- Pharmacokinetics: ARBs exhibit variable oral bioavailability and high plasma protein binding (often >95%). Most undergo hepatic metabolism, with several (e.g., candesartan cilexetil, olmesartan medoxomil) administered as prodrugs [9].
Statins (HMG-CoA Reductase Inhibitors)
Statins competitively inhibit HMG-CoA reductase, the rate-limiting enzyme in cholesterol biosynthesis, leading to increased LDL receptor expression and enhanced clearance of LDL cholesterol from the bloodstream [14] [10].
- Chemical Considerations: Statins exist in active hydroxy acid forms and inactive lactone forms, which can interconvert in vivo and during sample analysis, presenting a significant analytical challenge that must be controlled during method development [10].
- Therapeutic Applications: These drugs are cornerstone therapies for hypercholesterolemia and atherosclerosis prevention, with atorvastatin and simvastatin among the most commonly prescribed agents [7] [10].
Table 1: Key Pharmacological Properties of Cardiovascular Drug Classes
| Drug Class | Primary Mechanism | Therapeutic Applications | Common Agents |
|---|---|---|---|
| Beta-Blockers | β-adrenergic receptor antagonism | Hypertension, heart failure, angina, arrhythmias | Bisoprolol, carvedilol, metoprolol [11] [7] |
| Calcium Channel Blockers | L-type calcium channel blockade | Hypertension, angina, arrhythmias | Amlodipine, diltiazem, verapamil [8] [12] |
| ARBs | AT1 receptor blockade | Hypertension, heart failure, diabetic nephropathy | Telmisartan, valsartan, losartan [9] [13] |
| Statins | HMG-CoA reductase inhibition | Hypercholesterolemia, atherosclerosis prevention | Atorvastatin, simvastatin [14] [10] |
Table 2: Pharmacokinetic Properties of Selected Cardiovascular Drugs
| Drug | Bioavailability | Protein Binding | Elimination Half-life | Key Metabolites |
|---|---|---|---|---|
| Amlodipine | 64-90% | >95% | 35-50 hours | Inactive metabolites [12] |
| Telmisartan | 42-58% | >99% | ~24 hours | None significant [9] |
| Bisoprolol | ~90% | ~30% | 10-12 hours | Mostly unchanged [6] |
| Atorvastatin | ~14% | >98% | 14 hours | Active ortho- and para-hydroxy metabolites [10] |
| Valsartan | ~25% | ~95% | 6 hours | None significant [9] |
Analytical Challenges in Simultaneous Determination
The simultaneous quantification of multiple cardiovascular drugs presents several analytical challenges that must be addressed through careful method development:
- Wide Polarity Range: The diverse chemical structures across drug classes result in compounds with significantly different polarities, complicating chromatographic separation [7] [6].
- Variable Concentration Ranges: Therapeutic plasma concentrations vary considerably between drugs (e.g., ng/mL for some ARBs vs. µg/mL for some beta-blockers), requiring methods with broad dynamic range [11] [6].
- Matrix Effects: Plasma components can cause significant ionization suppression or enhancement in mass spectrometric detection, necessitating effective sample cleanup and appropriate internal standards [11] [6].
- Metabolic Interconversion: Statins particularly present challenges due to pH-dependent interconversion between their active acid and inactive lactone forms, which can occur during sample preparation, storage, and analysis [10].
HPLC Method for Simultaneous Determination in Plasma
Chromatographic Conditions
- Column: Thermo Hypersil BDS C18 (150 × 4.6 mm, 5 μm) or equivalent reverse-phase column [6]
- Mobile Phase: Gradient system combining methanol or acetonitrile with aqueous buffer (e.g., phosphate buffer, pH 3-5.2) [7] [6]
- Flow Rate: 0.6-1.0 mL/min
- Column Temperature: 25-35°C
- Injection Volume: 20 μL
- Detection: Dual detection approach utilizing UV (210-260 nm) for separation verification and fluorescence detection with compound-specific wavelengths for enhanced sensitivity and specificity [6]
Table 3: Optimized Fluorescence Detection Parameters
| Analyte | Excitation Wavelength (nm) | Emission Wavelength (nm) |
|---|---|---|
| Bisoprolol | 227 | 298 |
| Amlodipine | 361 | 442 |
| Telmisartan | 294 | 365 |
| Atorvastatin | 274 | 378 |
Sample Preparation Protocol
Liquid-Liquid Extraction Procedure:
Protein Precipitation: Add 600 μL of absolute ethanol to 200 μL of plasma sample and 50 μL of working internal standard solution. Vortex mix for 30 seconds and centrifuge at 10,000 × g for 2 minutes to precipitate proteins [6].
Primary Extraction: Transfer supernatant to a clean tube and add 1.0 mL of diethyl ether (first extraction solvent). Vortex mix for 5 minutes and centrifuge at 3,500 rpm for 5 minutes at 0°C. Carefully collect the organic layer [6].
Secondary Extraction: Add 0.5 mL of dichloromethane (second extraction solvent) to the remaining aqueous layer. Vortex mix for 5 minutes and centrifuge at 3,500 rpm for 5 minutes at 0°C. Combine this organic layer with the first extract [6].
Evaporation and Reconstitution: Evaporate the combined organic extracts to dryness under a gentle stream of nitrogen at 40°C. Reconstitute the residue in 500 μL of mobile phase or ethanol, vortex for 2 minutes, and inject 20 μL into the HPLC system [6].
Method Validation Parameters
The developed method should be validated according to ICH guidelines with the following performance characteristics:
- Linearity: Calibration curves spanning relevant concentration ranges (e.g., 5-100 ng/mL for bisoprolol and amlodipine, 0.1-5 ng/mL for telmisartan, 10-200 ng/mL for atorvastatin) with correlation coefficients (R²) >0.995 [6].
- Precision and Accuracy: Intra-day and inter-day precision (RSD%) within 1.7-12.3% and accuracy (RE%) within -14.4 to 14.1% for quality control samples [11].
- Recovery: Extraction efficiency of 80.0-119.6% for all analytes [11].
- Limit of Quantification: LOQ values of 0.1-0.5 ng/mL for sensitive detection of beta-blockers, with similar sensitivity achievable for other drug classes [11].
Signaling Pathways and Experimental Workflow
Diagram 1: Key Pharmacological Mechanisms of ARBs and CCBs
Diagram 2: Comprehensive Sample Preparation and Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Cardiovascular Drug Analysis
| Reagent/Material | Function/Application | Specifications/Alternatives |
|---|---|---|
| C18 Chromatography Column | Reverse-phase separation of analytes | Thermo Hypersil BDS C18 (150 × 4.6 mm, 5 μm) or ZORBAX Extend-C18 [7] [6] |
| Mass Spectrometry System | Highly sensitive detection and quantification | UHPLC-QqQ-MS/MS for multi-analyte determination [11] [15] |
| Solid Phase Extraction Cartridges | Sample clean-up and analyte concentration | Discovery DSC-18 or equivalent C18 sorbent [14] |
| Deuterated Internal Standards | Quantification accuracy and matrix effect compensation | Atenolol-d7, metoprolol-d7, propranolol-d7 for beta-blockers [11] |
| Mobile Phase Components | Chromatographic separation | HPLC-grade methanol, acetonitrile, ammonium acetate, phosphate buffers [14] [6] |
| Extraction Solvents | Liquid-liquid extraction of analytes from plasma | Diethyl ether, dichloromethane, ethyl acetate [11] [6] |
The simultaneous determination of multiple cardiovascular drugs in plasma requires careful consideration of both pharmacological properties and analytical parameters. The HPLC method detailed herein provides a robust framework for the sensitive and selective quantification of beta-blockers, calcium channel blockers, ARBs, and statins in biological matrices. The incorporation of dual detection approaches (UV and fluorescence) enhances method versatility, while optimized sample preparation minimizes matrix effects and maintains analyte stability. This comprehensive analytical protocol supports advanced cardiovascular drug research, therapeutic drug monitoring, and drug development applications, contributing to optimized pharmacotherapy for cardiovascular diseases.
Principles of Therapeutic Drug Monitoring (TDM) for Personalized Treatment
Therapeutic Drug Monitoring (TDM) represents a critical component of personalized medicine, enabling clinicians to individualize drug dosing regimens based on measured drug concentrations in biological fluids. For cardiovascular diseases (CVDs)—the leading cause of global mortality—TDM is particularly valuable given the narrow therapeutic index and significant pharmacokinetic variability of many cardiovascular drugs [6]. The implementation of TDM helps bridge the gap between empirical dosing and personalized therapeutic strategies, optimizing efficacy while minimizing adverse drug reactions.
High-Performance Liquid Chromatography (HPLC) has emerged as a cornerstone analytical technology for TDM due to its specificity, sensitivity, and ability to simultaneously quantify multiple drugs and their metabolites. The development of robust HPLC methods for cardiovascular drug monitoring allows researchers and clinicians to obtain precise pharmacokinetic data, establishing concentration-effect relationships that form the scientific basis for dose individualization [16]. This document outlines fundamental principles and detailed protocols for implementing HPLC-based TDM of cardiovascular drugs in plasma, providing a framework for advancing personalized treatment in cardiovascular medicine.
Analytical Principles and Method Selection
Chromatographic Separation Fundamentals
Reverse-phase high-performance liquid chromatography (RP-HPLC) is widely utilized in pharmaceutical analysis for efficient separation and precise quantification of active pharmaceutical ingredients in complex matrices like plasma [6]. The separation mechanism relies on the differential partitioning of analytes between a polar mobile phase and a non-polar stationary phase, typically consisting of C18-bonded silica. Effective separation of cardiovascular drugs requires careful optimization of several chromatographic parameters, including mobile phase composition, pH, column temperature, and flow rate.
The selection of detection method depends on the physicochemical properties of the target analytes and the required sensitivity. While ultraviolet (UV) detection provides broad applicability and cost-effectiveness for many cardiovascular drugs, fluorescence detection (FLD) offers enhanced sensitivity and specificity for analytes with native fluorescence or those that can be derivatized [6]. Mass spectrometry (MS) detection provides superior selectivity and sensitivity for complex TDM applications requiring quantification of multiple drugs and metabolites [17] [18].
Key Validation Parameters for TDM Methods
Bioanalytical methods for TDM must undergo rigorous validation to ensure reliability of the generated data. The International Council for Harmonisation (ICH) guidelines define key validation parameters that must be established for any HPLC method used in TDM [6] [19]:
- Selectivity and Specificity: The method must accurately quantify the target analyte without interference from endogenous plasma components, metabolites, or concomitant medications [19].
- Linearity and Range: The relationship between analyte concentration and detector response must be linear across the clinically relevant concentration range [19].
- Accuracy and Precision: Method accuracy (closeness to true value) and precision (reproducibility) must be demonstrated at multiple concentration levels [18] [19].
- Limit of Quantification (LOQ): The lowest concentration that can be quantitatively measured with acceptable accuracy and precision [19].
- Recovery and Matrix Effects: The efficiency of analyte extraction from plasma and the impact of plasma components on ionization efficiency (for MS detection) must be characterized [18].
Experimental Protocols for HPLC-Based TDM
Sample Preparation Techniques
Proper sample preparation is crucial for removing interfering matrix components and concentrating analytes to detectable levels. The following protocols describe two effective sample preparation techniques for cardiovascular drugs in plasma.
Liquid-Liquid Extraction (LLE) Protocol
This protocol, adapted from a validated method for simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin [6], provides high recovery for a broad range of cardiovascular drugs:
- Sample Pretreatment: Transfer 200 µL of plasma sample to a clean glass tube. Add 600 µL of absolute ethanol and 50 µL of working standard solution (internal standard). Vortex mix for 30 seconds.
- Protein Precipitation: Centrifuge the mixture at 6000 rpm for 2 minutes at 4°C. Collect the supernatant.
- First Extraction: Add 1.0 mL of diethyl ether (first extraction solvent) to the supernatant. Vortex mix for 5 minutes. Centrifuge at 3500 rpm for 5 minutes at 0°C. Transfer the organic layer to a clean test tube.
- Second Extraction: Add 0.5 mL of dichloromethane (second extraction solvent) to the remaining aqueous layer. Vortex mix for 5 minutes. Centrifuge at 3500 rpm for 5 minutes at 0°C. Combine this organic layer with the first extract.
- Concentration: Evaporate the combined organic extracts under a gentle stream of nitrogen at 40°C.
- Reconstitution: Reconstitute the residue in 500 µL of ethanol or mobile phase. Vortex for 2 minutes. Transfer to HPLC vials for analysis.
QuEChERS Extraction Protocol
The QuEChERS (Quick, Easy, Cheap, Effective, Rugged, and Safe) approach provides a simplified extraction procedure suitable for multiple cardiovascular drugs [18]:
- Sample Preparation: Transfer 1 mL of plasma to a 15-mL centrifuge tube.
- Extraction: Add 3 mL of acetonitrile and vortex vigorously for 1 minute.
- Salting Out: Add 400 mg of anhydrous magnesium sulfate and 20 mg of C18 sorbent. Shake vigorously for 30 seconds.
- Phase Separation: Centrifuge at 5000 rpm for 5 minutes.
- Collection: Transfer the supernatant (organic layer) to a clean tube.
- Concentration: Evaporate under nitrogen stream at 40°C.
- Reconstitution: Reconstitute the residue in 200 µL of mobile phase. Vortex mix and filter through a 0.22 µm membrane before HPLC analysis.
HPLC-FLD Analysis of Cardiovascular Drugs
This protocol details a highly sensitive method for simultaneous quantification of four cardiovascular drugs using HPLC with fluorescence detection [6]:
Chromatographic Conditions
- Column: Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 µm)
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in 40:60 ratio
- Flow Rate: 0.6 mL/min
- Injection Volume: 20 µL
- Column Temperature: 25-35°C
- Run Time: <10 minutes
- Detection: Fluorescence detection with wavelength programming:
- Bisoprolol: 227 nm excitation / 298 nm emission
- Telmisartan: 294 nm excitation / 365 nm emission
- Atorvastatin: 274 nm excitation / 378 nm emission
- Amlodipine: 361 nm excitation / 442 nm emission
Analytical Procedure
- Mobile Phase Preparation: Prepare 0.03 M potassium dihydrogen phosphate buffer and adjust to pH 5.2 using phosphoric acid or sodium hydroxide. Mix with ethanol in 60:40 ratio (buffer:ethanol). Filter through 0.45 µm membrane and degas by sonication for 15 minutes.
- System Equilibration: Equilibrate the HPLC system with mobile phase for at least 30 minutes at 0.6 mL/min until stable baseline is achieved.
- Calibration Standards: Prepare calibration standards in drug-free plasma at concentrations spanning the expected therapeutic range:
- Bisoprolol: 5-100 ng/mL
- Amlodipine: 5-100 ng/mL
- Telmisartan: 0.1-5 ng/mL
- Atorvastatin: 10-200 ng/mL
- Sample Analysis: Inject processed samples and calibration standards. Monitor detector response and record peak areas for each analyte.
- Quantification: Calculate sample concentrations using the calibration curve constructed from peak areas of standards.
Table 1: Analytical Performance of HPLC-FLD Method for Cardiovascular Drugs [6]
| Analyte | Linear Range (ng/mL) | LLOQ (ng/mL) | Precision (% RSD) | Accuracy (%) |
|---|---|---|---|---|
| Bisoprolol | 5-100 | 5 | <5% | 94.5-105.2 |
| Amlodipine | 5-100 | 5 | <5% | 95.8-104.3 |
| Telmisartan | 0.1-5 | 0.1 | <8% | 92.7-107.5 |
| Atorvastatin | 10-200 | 10 | <6% | 96.2-103.8 |
UPLC-MS/MS Method for Multiplexed TDM
For laboratories equipped with mass spectrometry capabilities, UPLC-MS/MS provides enhanced sensitivity and specificity for multiplexed TDM applications:
- Column: Agilent Poroshell 120 EC-C18 (4.6 × 100 mm, 2.7 µm)
- Mobile Phase: Methanol and 0.1% formic acid in water
- Gradient Program: Linear gradient from 20% to 95% methanol over 8 minutes
- Flow Rate: 0.4 mL/min
- Injection Volume: 5 µL
- Column Temperature: 40°C
- Ionization Mode: ESI positive ion mode
- Detection: Multiple Reaction Monitoring (MRM)
Mass Spectrometry Parameters
Optimize MS parameters for each analyte, including declustering potential, collision energy, and collision cell exit potential. Use stable isotope-labeled internal standards for each analyte when available to correct for matrix effects and recovery variations.
Table 2: Linear Ranges for Cardiovascular Drugs by UPLC-MS/MS [18]
| Analyte | Linear Range (ng/mL) | LLOQ (ng/mL) |
|---|---|---|
| Nisoldipine | 0.05-4.0 | 0.05 |
| Metoprolol | 0.05-4.0 | 0.05 |
| Prazosin | 0.05-4.0 | 0.05 |
| Atenolol | 0.5-40 | 0.5 |
| Bisoprolol | 0.5-40 | 0.5 |
| Propranolol | 0.5-40 | 0.5 |
| Rosuvastatin | 0.5-40 | 0.5 |
| Atorvastatin | 0.5-40 | 0.5 |
| Fluvastatin | 5.0-400 | 5.0 |
Workflow Visualization
HPLC-TDM Workflow: This diagram illustrates the sequential steps in the HPLC-based TDM process, from sample collection to clinical reporting.
Research Reagent Solutions
Table 3: Essential Reagents and Materials for HPLC-TDM of Cardiovascular Drugs
| Category | Specific Reagents/Materials | Function | Application Notes |
|---|---|---|---|
| HPLC Columns | Thermo Hypersil BDS C18 [6] | Chromatographic separation | 150 mm × 4.6 mm, 5.0 µm particle size |
| Agilent Poroshell 120 EC-C18 [18] | Fast separation with UPLC-MS/MS | 4.6 × 100 mm, 2.7 µm core-shell particles | |
| Chromolith HighResolution RP-18 [16] | High-throughput analysis | Monolithic column for fast separations | |
| Extraction Sorbents | C18 [18] | Lipophilic compound retention | Used in QuEChERS for plasma cleanup |
| Anhydrous MgSO₄ [18] | Water removal in QuEChERS | Promotes phase separation | |
| Mobile Phase Components | Potassium phosphate buffer [6] | Aqueous mobile phase component | Typically 0.03-0.05 M, pH 3-5.2 |
| Methanol, Acetonitrile [18] [20] | Organic modifiers | Varying proportions for optimal separation | |
| Triethylamine [20] | Peak shape modifier | Reduces tailing of basic compounds | |
| Internal Standards | Stable isotope-labeled analogs [17] | Quantification standardization | Corrects for variability in extraction and ionization |
| Extraction Solvents | Diethyl ether, Dichloromethane [6] | Liquid-liquid extraction | Sequential extraction for comprehensive recovery |
| Acetonitrile [18] | Protein precipitation | Effective for broad range of cardiovascular drugs |
Implementation in Clinical Research
Method Validation and Quality Control
Prior to clinical implementation, the HPLC method must undergo comprehensive validation following ICH guidelines [19] and FDA recommendations for bioanalytical methods. Key validation experiments include:
- Selectivity Assessment: Analyze blank plasma samples from at least six different sources to demonstrate absence of interfering peaks at the retention times of target analytes and internal standards [18].
- Linearity Evaluation: Prepare and analyze calibration standards at 6-8 concentration levels across the expected range. The correlation coefficient (r) should be ≥0.99 [6] [18].
- Precision and Accuracy: Assess using quality control samples at four concentration levels (LLOQ, low, medium, high) with at least five replicates per level. Accuracy should be 85-115% of nominal values, with precision <15% RSD [18].
- Stability Studies: Evaluate analyte stability under various conditions including benchtop, processed sample, freeze-thaw, and long-term storage [6].
Practical Considerations for Method Development
Successful implementation of HPLC-TDM methods requires attention to several practical aspects:
- Matrix Effects: Particularly important for MS detection. Evaluate by comparing analyte response in post-extraction spiked samples versus neat solutions [18]. Use stable isotope-labeled internal standards to compensate for suppression/enhancement effects.
- Carryover Assessment: Inject blank samples after the highest calibration standard. Carryover should not exceed 20% of the LLOQ for analytes and 5% for internal standards [18].
- System Suitability: Establish criteria for retention time stability, peak symmetry, theoretical plates, and resolution. Monitor these parameters daily to ensure consistent system performance [6].
HPLC-based methods provide robust, sensitive, and specific approaches for TDM of cardiovascular drugs, enabling personalized treatment optimization. The protocols outlined in this document provide a foundation for developing and implementing HPLC-TDM methods in both research and clinical settings. As cardiovascular pharmacotherapy continues to evolve with new drug combinations and novel therapeutic agents, these analytical approaches will play an increasingly important role in ensuring therapeutic efficacy while minimizing adverse drug reactions through precision dosing.
Therapeutic drug monitoring (TDM) and pharmaceutical quality control require precise analytical methods capable of quantifying multiple analytes in complex biological matrices. High-performance liquid chromatography (HPLC) has emerged as a cornerstone technique for the simultaneous determination of cardiovascular drugs in plasma, offering the selectivity, sensitivity, and robustness necessary for reliable results in both clinical and research settings [6] [21]. The implementation of reversed-phase HPLC (RP-HPLC) methods enables researchers to overcome significant challenges associated with matrix effects, spectral overlap, and the diverse physicochemical properties of cardiovascular pharmaceuticals [22] [6]. This application note details the strategic advantages of HPLC and provides validated protocols for the simultaneous analysis of multiple cardiovascular drugs in plasma, supporting critical research in drug development and personalized medicine.
Key Advantages of HPLC in Multi-Drug Analysis
HPLC offers several distinct advantages over other analytical techniques for simultaneous multi-drug determination in complex matrices like plasma:
- Superior Selectivity: Chromatographic separation enables accurate quantification of structurally similar compounds without derivatization, resolving matrix interferences that compromise spectrophotometric determinations [22].
- High Efficiency: Simultaneous determination methods significantly reduce analysis time and costs by quantifying multiple compounds in a single run compared to multiple separate analyses [22] [23].
- Enhanced Accuracy: Minimizing errors associated with sample preparation and handling as all analytes are processed under identical conditions [23].
- Proven Versatility: RP-HPLC can handle a wide range of analytes, from small molecules to larger biomolecules, across diverse pharmaceutical classes [23].
The following table summarizes key performance metrics from recent HPLC methods developed for cardiovascular drug analysis:
Table 1: Performance Metrics of HPLC Methods for Cardiovascular Drug Analysis
| Analytical Target | Linear Range (ng/mL) | Correlation Coefficient (r²) | Analysis Time (min) | Reference |
|---|---|---|---|---|
| Bisoprolol | 5-100 | ≥0.999 | <10 | [6] |
| Amlodipine | 5-100 | ≥0.999 | <10 | [6] |
| Telmisartan | 0.1-5 | ≥0.999 | <10 | [6] |
| Atorvastatin | 10-200 | ≥0.999 | <10 | [6] |
| Amlodipine (CCB Panel) | 10-50 µg/mL | ≥0.9989 | 7.6 | [24] |
| Nifedipine (CCB Panel) | 10-50 µg/mL | ≥0.9989 | 7.6 | [24] |
Experimental Protocols
Method for Simultaneous Analysis of Four Cardiovascular Drugs in Plasma
This validated protocol enables the simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin in human plasma, combining high sensitivity with robust performance [6].
Instrumentation and Chromatographic Conditions
- HPLC System: Waters Alliance 2695 HPLC system equipped with auto-sampler, quaternary pump, and thermostatted column compartment
- Detection: Waters 2475 Multi-Wavelength Fluorescence Detector with optimized excitation/emission wavelengths:
- Bisoprolol: 227/298 nm
- Amlodipine: 361/442 nm
- Telmisartan: 294/365 nm
- Atorvastatin: 274/378 nm
- Supplementary UV detection: 210-260 nm range for separation verification [6]
- Column: Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 μm)
- Mobile Phase: Isocratic elution with ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in 40:60 ratio
- Flow Rate: 0.6 mL/min
- Injection Volume: 20 μL
- Column Temperature: 25-35°C [6]
Sample Preparation Protocol: Liquid-Liquid Extraction
Diagram: Plasma Sample Preparation Workflow
Calibration Standard Preparation
- Stock Solutions (100 μg/mL): Accurately weigh 10 mg of each reference standard into separate 100 mL volumetric flasks. Dissolve in and dilute to volume with ethanol [6].
- Working Solutions (10 μg/mL): Dilute stock solutions 1:10 with ethanol.
- Calibration Standards: Prepare by spiking drug-free plasma with appropriate volumes of working solutions to generate concentrations within the validated ranges:
- Bisoprolol and Amlodipine: 5-100 ng/mL
- Telmisartan: 0.1-5 ng/mL
- Atorvastatin: 10-200 ng/mL [6]
Method Validation Parameters
The method was validated according to International Council for Harmonisation (ICH) guidelines, demonstrating:
- Linearity: Correlation coefficients (r²) ≥ 0.999 across specified ranges [6]
- Precision: Relative standard deviation (RSD) < 1.1% for all analytes [6] [24]
- Accuracy: Recovery rates consistent with accepted pharmaceutical standards [6]
- Specificity: No interference from plasma matrix components or drug metabolites
Alternative Solid-Phase Extraction Protocol for Broader Applications
For laboratories preferring solid-phase extraction, this alternative protocol based on clinical TDM research provides reliable sample clean-up [21].
SPE Procedure Using Monolithic C18-Silica Cartridges
- Cartridge Preparation: Use monolithic C18-silica disk centrifugal spin-cartridges (MonoSpin C18). Pre-treat with sequential passage of 500 μL each of acetonitrile and water via centrifugation at 5,000 rpm for 1 minute [21].
- Sample Loading: Filter patient serum through 0.45 μm syringe filter. Load 150 μL filtered serum onto pre-treated cartridge via centrifugation for 3 minutes [21].
- Washing: Pass 500 μL water through cartridge via centrifugation for 2 minutes.
- Elution: Pass 150 μL aqueous 50% acetonitrile (for most drugs) or 30% acetonitrile (for vancomycin) through cartridge via centrifugation for 1 minute. Collect eluate for HPLC analysis [21].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents and Materials for HPLC Analysis of Cardiovascular Drugs
| Item | Specification | Function/Application | Example Sources |
|---|---|---|---|
| HPLC System | Binary or quaternary pump, auto-sampler, column oven, detector | Separation and quantification core system | Agilent, Waters, Shimadzu, Hitachi [21] [25] |
| Analytical Column | C18 or C8, 100-150 mm × 4.6 mm, 3-5 μm | Stationary phase for compound separation | Thermo Hypersil BDS C18, Luna C8, Zorbax SB [6] [24] |
| Fluorescence Detector | Multi-wavelength with programmable Ex/Em | Sensitive detection of native-fluorescent compounds | Waters 2475, Agilent DAD/FLD [6] |
| Reference Standards | Pharmaceutical grade, purity ≥98% | Method development, calibration, quality control | Sigma-Aldrich, pharmaceutical manufacturers [6] [24] |
| Solvents | HPLC grade methanol, acetonitrile, ethanol | Mobile phase components, sample preparation | Sigma-Aldrich, Honeywell [6] [24] |
| Buffer Salts | Analytical grade potassium phosphate, triethylamine | Mobile phase modifiers, pH control | Sigma-Aldrich, Scharlab [6] [24] |
| Sample Preparation | C18 SPE cartridges, filtration units | Matrix clean-up, analyte concentration | MonoSpin C18, 0.45 μm membrane filters [21] |
Method Optimization and Troubleshooting
Critical Method Optimization Parameters
Successful implementation of simultaneous multi-drug analysis requires careful optimization of several key parameters:
- Mobile Phase Composition: The ratio of organic to aqueous components significantly impacts separation efficiency. Typical mobile phases combine water with methanol or acetonitrile, often with pH modifiers like 0.1% ortho-phosphoric acid (pH 3.0) or triethylamine (pH 3.06) to improve peak shape and resolution [22] [24].
- Column Selection: C18 columns provide excellent retention for most cardiovascular drugs. For compounds with specific interaction issues (e.g., dihydropyridines with silanol groups), C8 or phenyl columns may offer superior performance [24].
- Temperature Control: Maintaining column temperature between 25-35°C ensures retention time reproducibility and optimal separation efficiency [6].
- Detection Wavelength Optimization: Using diode array detectors to identify optimal wavelengths for multi-component analysis, or employing fluorescence detection with carefully selected Ex/Em pairs for enhanced sensitivity and specificity [6].
Advanced Applications: Monitoring In-Vitro Release Profiles
The versatility of HPLC methods extends beyond simple quantification to more complex applications like dissolution testing and content uniformity studies. As demonstrated in neuromodulating drug research, properly developed HPLC methods can monitor in-vitro release profiles, providing critical data for pharmaceutical development and quality control [26].
Diagram: HPLC Method Development and Application Workflow
HPLC methodologies provide robust, sensitive, and efficient solutions for the simultaneous analysis of multiple cardiovascular drugs in complex biological matrices. The protocols detailed in this application note demonstrate practical approaches that balance analytical performance with practical implementation considerations. The dual-detection approach combining UV and fluorescence detection offers particularly enhanced specificity for cardiovascular drug panels with diverse chemical structures. As pharmaceutical research advances toward more personalized medicine approaches, these HPLC methods will continue to play a critical role in therapeutic drug monitoring, pharmacokinetic studies, and quality control of fixed-dose combination products. The ongoing development of greener chromatographic methods with reduced environmental impact represents an important future direction for the field, aligning with broader sustainability initiatives in pharmaceutical analysis [26] [24].
Within pharmaceutical analysis, particularly for the monitoring of cardiovascular drugs in biological matrices like plasma, the selection of an appropriate analytical technique is paramount. The complexity of plasma, coupled with the need to detect drugs at low concentrations, demands methods that are sensitive, selective, and robust. This document provides a comparative overview of three prominent chromatographic techniques—High-Performance Liquid Chromatography (HPLC), Micellar Electrokinetic Chromatography (MEKC), and HPLC coupled with tandem mass spectrometry (HPLC-MS/MS)—framed within the context of a thesis focused on the simultaneous determination of cardiovascular drugs in plasma.
The management of cardiovascular diseases (CVDs) often involves polytherapy, necessitating analytical methods capable of monitoring multiple drugs simultaneously [6] [7]. The techniques discussed herein each offer distinct advantages and limitations for this challenging application, impacting factors such as method greenness, sensitivity, and operational complexity.
Technique Summaries and Comparative Tables
The core characteristics, advantages, and limitations of each technique are summarized in the table below for a direct comparison.
Table 1: Core Characteristics of HPLC, MEKC, and HPLC-MS/MS
| Feature | HPLC | MEKC | HPLC-MS/MS |
|---|---|---|---|
| Principle | Separation based on partitioning between stationary and liquid mobile phases. | Separation based on differential partitioning between micelles and an aqueous buffer in an electric field. | HPLC separation followed by gas-phase ion separation and highly specific mass detection. |
| Key Strength | Robustness, wide applicability, and high preparative capacity. | High separation efficiency with minimal solvent consumption (green chemistry). | Exceptional sensitivity, selectivity, and specificity for complex matrices. |
| Key Limitation | Lower sensitivity and selectivity compared to MS detection; higher solvent consumption. | Generally lower sensitivity than LC-MS; potential for matrix interference in plasma. | High instrument cost, operational complexity, and requires skilled personnel. |
| Typical Analysis Time | <10 min for fast methods [6] | ~10 min or less [7] [27] | Varies, but can be very fast with modern UHPLC systems. |
| Solvent Consumption | Moderate to High (mL/min) | Very Low (µL/min) | Moderate (mL/min), but can be reduced with UHPLC. |
| Cost | Moderate | Low | High (capital and maintenance) |
The performance of each technique for quantifying cardiovascular drugs in plasma is highly application-dependent. The following table compiles representative validation data from recent studies.
Table 2: Performance Comparison for Cardiovascular Drug Analysis in Plasma
| Technique | Analytes (Example) | Linear Range (ng/mL) | Limit of Detection (LOD) | Reference |
|---|---|---|---|---|
| HPLC-FLD | Bisoprolol, Amlodipine | 5 - 100 ng/mL | Not specified, but LLOQ was 5 ng/mL | [6] |
| MEKC-UV | Ezetimibe, Atorvastatin, Rosuvastatin | 10,000 - 100,000 ng/mL (bulk analysis) | 0.42 - 0.75 µg/mL | [27] |
| HPLC-MS/MS | Bisoprolol, Atorvastatin, etc. | 0.5 - 40 ng/mL | LLOQ: 0.5 ng/mL | [18] |
| HPLC-MS/MS | Nisoldipine, Metoprolol | 0.05 - 4.0 ng/mL | LLOQ: 0.05 ng/mL | [18] |
| UPLC-MS/MS | Atenolol, Propranolol, Atorvastatin | 0.5 - 40 ng/mL | LLOQ: 0.5 ng/mL | [28] |
Detailed Experimental Protocols
Protocol: HPLC-FLD for Cardiovascular Drugs in Plasma
This protocol is adapted from a validated method for the concurrent determination of bisoprolol (BIS), amlodipine (AML), telmisartan (TEL), and atorvastatin (ATV) in human plasma [6].
- Instrumentation: HPLC system (e.g., Waters Alliance 2695) equipped with a Fluorescence Detector (FLD) and a C18 column (e.g., Thermo Hypersil BDS C18, 150 mm × 4.6 mm, 5 μm).
- Research Reagent Solutions:
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in a 40:60 ratio.
- Extraction Solvents: Absolute ethanol, diethyl ether, dichloromethane.
- Standard Solutions: Stock solutions (100 µg/mL) of each drug in ethanol, further diluted to working concentrations.
Table 3: Key Reagents for HPLC-FLD Protocol
| Reagent/Material | Function | Specifications/Notes |
|---|---|---|
| C18 Chromatographic Column | Analytical separation of drugs | 150 mm × 4.6 mm, 5 μm particle size |
| Potassium Dihydrogen Phosphate | Preparation of mobile phase buffer | Adjust to pH 5.2; 0.03 M concentration |
| Ethanol (HPLC Grade) | Organic modifier in mobile phase; protein precipitation | Sustainable solvent alternative to acetonitrile |
| Diethyl Ether & Dichloromethane | Liquid-liquid extraction of drugs from plasma | Removes proteins and interferences |
| Drug Standards | For calibration and quantification | Certified reference materials with known purity |
Chromatographic Conditions:
- Flow Rate: 0.6 mL/min
- Injection Volume: 20 µL
- Column Temperature: 25-35°C
- Elution: Isocratic
- FLD Wavelengths: Optimized for each drug (e.g., 227/298 nm for BIS, 361/442 nm for AML).
Sample Preparation (Liquid-Liquid Extraction):
- To 200 µL of plasma, add 600 µL of absolute ethanol and 50 µL of working standard solution.
- Vortex and centrifuge the mixture to precipitate proteins.
- Add 1.0 mL of diethyl ether (first extraction solvent), vortex for 5 min, and centrifuge at 3500 rpm for 5 min at 0°C.
- Transfer the organic layer to a clean tube.
- Add 0.5 mL of dichloromethane (second extraction solvent) to the remaining plasma, vortex, and centrifuge as before.
- Combine the organic layers from both extractions and evaporate to dryness under a gentle nitrogen stream at 40°C.
- Reconstitute the dry residue in 500 µL of ethanol, vortex, and inject 20 µL into the HPLC system.
Method Validation Highlights: The method was validated per ICH guidelines, demonstrating linearity (e.g., 5–100 ng/mL for BIS and AML), accuracy, precision, and a short run time of less than 10 minutes [6].
Protocol: MEKC for Cardiovascular Drugs and a Nutraceutical
This protocol is based on a green MEKC method for the simultaneous analysis of eight cardiovascular drugs and the nutraceutical vincamine [7].
- Instrumentation: Capillary Electrophoresis system (e.g., Agilent 7100) with a DAD detector and a fused silica capillary (50 cm total length, 50 µm internal diameter).
- Research Reagent Solutions:
- Background Electrolyte (BGE): 50 mM Borate buffer (pH 9) containing 50 mM Sodium Lauryl Sulphate (SLS) and 10% acetonitrile as an organic modifier.
Capillary Conditions:
- Voltage: 30 kV
- Injection: Hydrodynamic, 50 mbar for 10 s
- Detection: DAD, wavelengths optimized for each drug
- Capillary Preparation: Daily rinse with 0.5 M NaOH (15 min), water (15 min), and conditioning with BGE.
Sample Preparation:
- For pharmaceutical formulations, powder from crushed tablets is dissolved and sonicated in methanol, then filtered and diluted with a water-methanol mixture to the required concentration.
- For plasma analysis, the study notes application in rat plasma, requiring a sample preparation step (e.g., protein precipitation or extraction) prior to dilution and analysis [7].
Protocol: HPLC-MS/MS for Multi-Drug Therapeutic Drug Monitoring
This protocol outlines a high-sensitivity approach using QuEChERS extraction for the determination of nine cardiovascular drugs in human plasma [28] [18].
- Instrumentation: UPLC-MS/MS system (e.g., Sciex Triple Quadrupole) with an electrospray ionization (ESI) source and a C18 column (e.g., Agilent Poroshell 120 EC-C18, 4.6 × 100 mm, 2.7 μm).
- Research Reagent Solutions:
- Mobile Phase: Methanol and 0.1% formic acid in water.
- Extraction Kit: QuEChERS salts and sorbents.
MS/MS Conditions:
- Ionization Mode: ESI-positive
- Detection Mode: Multiple Reaction Monitoring (MRM)
- Monitor specific precursor-product ion transitions for each analyte and internal standard.
Sample Preparation (QuEChERS):
- To a plasma sample, add 3 mL of acetonitrile.
- Add salting agents (400 mg anhydrous MgSO4) and a sorbent (20 mg C18) for clean-up.
- Vortex vigorously to ensure proper partitioning and clean-up.
- Centrifuge the mixture to separate the phases.
- Transfer the supernatant (acetonitrile layer) for analysis or further dilution.
Method Validation Highlights: The method showed high sensitivity with LLOQs as low as 0.05 ng/mL for some drugs, accuracy between 94.15-110.62%, and precision (RSD) <15% [18].
Workflow and Decision Pathway Visualizations
Technique Selection Workflow
The following diagram outlines a logical decision pathway for selecting the most appropriate analytical technique based on research goals and constraints.
Sample Preparation and Analysis Workflow
This diagram illustrates the general workflow for bioanalysis, from sample collection to data analysis, highlighting technique-specific steps.
The choice between HPLC, MEKC, and HPLC-MS/MS for the simultaneous determination of cardiovascular drugs in plasma is a trade-off between sensitivity, specificity, operational cost, and alignment with green chemistry principles.
- HPLC with FLD/UV remains a robust, cost-effective choice for monitoring drugs at moderate concentrations (ng/mL to µg/mL), especially when methods are optimized for short run times and sustainable solvents [6].
- MEKC stands out for its minimal solvent consumption and high separation efficiency, making it an excellent green alternative for applications where its sensitivity is sufficient, such as in pharmaceutical formulation analysis [7] [27].
- HPLC-MS/MS is the unequivocal gold standard for ultra-sensitive and highly specific quantification in complex biological matrices, capable of reaching sub-ng/mL levels essential for advanced pharmacokinetic studies and therapeutic drug monitoring of multiple agents [28] [18].
For a thesis focused on developing new HPLC methods, this landscape suggests that while conventional HPLC is highly viable, incorporating green solvent principles and exploring hybrid techniques or sophisticated detection systems could represent the future direction of the field.
Developing and Implementing Robust HPLC Methods for Multi-Drug Analysis
The simultaneous determination of multiple cardiovascular drugs in human plasma represents a significant analytical challenge in therapeutic drug monitoring and pharmacokinetic studies. The complexity of the biological matrix, coupled with the diverse chemical properties of different drug classes, demands meticulous optimization of chromatographic conditions. This application note details a standardized protocol for the development of a robust, sensitive, and environmentally conscious high-performance liquid chromatography (HPLC) method, framed within broader thesis research on analytical method development for cardiovascular drug monitoring. The optimization of three critical parameters—column selection, mobile phase composition, and pH—is explored to achieve efficient separation, precise detection, and quantitative analysis of target analytes in spiked human plasma.
Current Methodologies in Cardiovascular Drug Analysis
Recent scientific literature demonstrates a trend towards green analytical chemistry principles and the use of fluorescence detection for enhanced sensitivity in complex biological matrices. Key developments include methods for simultaneous determination of drug combinations.
Table 1: Recent HPLC Methods for Simultaneous Determination of Cardiovascular Drugs in Plasma
| Drugs Analyzed | Stationary Phase | Mobile Phase Composition | pH | Detection | Linear Range | Citation |
|---|---|---|---|---|---|---|
| Bisoprolol, Amlodipine, Telmisartan, Atorvastatin | Thermo Hypersil BDS C18 (150 x 4.6 mm, 5 µm) | Ethanol: 0.03 M Potassium Phosphate Buffer (40:60, v/v) | 5.2 | FLD (Multiple λex/λem) | BIS, AML: 5-100 ng/mLTEL: 0.1-5 ng/mLATV: 10-200 ng/mL | [6] [29] |
| Felodipine, Metoprolol | Inertsil C18 (150 x 4.6 mm, 5 µm) | Ethanol: 30 mM KH₂PO₄ Buffer (40:60, v/v) | 2.5 | FLD | FDP: 0.01-1.00 µg/mLMTP: 0.003-1.00 µg/mL | [30] |
| Carvedilol, Hydrochlorothiazide, Impurities | YMC Triart-Phenyl (150 x 4.6 mm, 5 µm) | Gradient: 0.1% Formic Acid (A) and Ethanol (B) | ~2.8* | PDA (254 nm) | HCT, CAR: 0.1-100 µg/mLImpurities: 0.05-10 µg/mL | [31] |
| Five Cardiovascular Agents | SinoChrom ODS-BP C18 (150 x 4.6 mm, 5 µm) | Gradient: 50 mM KH₂PO₄ Buffer (A) and Acetonitrile (B) | ~4.7* | PDA (280 nm) | 6.0-240.0 µg/mL (varies by drug) | [32] |
Note: *pH estimated from mobile phase description. FLD: Fluorescence Detection; PDA: Photodiode Array Detection.
Critical Aspects of Chromatographic Optimization
Column Selection Strategy
The selection of an appropriate stationary phase is the foundational step in method development. The goal is to achieve sufficient resolution of all analytes from each other and from endogenous plasma components.
- Column Chemistry: The C18 (ODS) column is the most widely used workhorse in reversed-phase HPLC for cardiovascular drugs, offering strong hydrophobic retention and a wide application range [6] [30]. For more complex separations involving impurities or metabolites, specialized columns like phenyl [31] or C8 [33] can provide different selectivity based on π-π interactions or lesser hydrophobicity, respectively.
- Column Dimensions: A column dimension of 150 mm x 4.6 mm i.d. packed with 5 µm particles is a standard and effective choice, providing a good balance between analysis time, resolution, and backpressure [6] [32] [30]. Shorter columns or smaller particles (e.g., 3 µm) can be used for faster separations but may require instrument modifications to handle extra-column volume [34].
- Pore Size: For small molecule drugs, a pore size of 60–150 Å is ideal, as it provides a high surface area for interaction, leading to better efficiency and resolution [34].
Table 2: Research Reagent Solutions for HPLC Method Development
| Reagent / Material | Function / Role | Example from Literature |
|---|---|---|
| C18 Chromatographic Column | Reversed-phase separation; primary interaction with analytes based on hydrophobicity. | Thermo Hypersil BDS C18 [6] |
| Organic Solvents (HPLC Grade) | Mobile phase component; strength and selectivity modifier. | Ethanol [6] [31], Acetonitrile [32] |
| Buffer Salts (e.g., KH₂PO₄) | Mobile phase component; controls ionic strength and buffers pH. | Potassium Dihydrogen Phosphate [6] [30] |
| pH Adjusting Agents | Fine-tunes ionization state of analytes and stationary phase silanols. | Ortho-Phosphoric Acid [31] [30] |
| Extraction Solvents | Isolates analytes from the plasma matrix via liquid-liquid extraction. | Diethyl Ether, Dichloromethane [6] |
| Analytical Reference Standards | Qualification and quantification of target analytes; essential for calibration. | Drug standards with certified purity (≥99%) [6] [31] |
Mobile Phase Composition and pH Optimization
The mobile phase acts as the liquid carrier, and its composition is a powerful tool for manipulating retention, selectivity, and peak shape.
- Organic Modifier Selection: While acetonitrile is common [32] [33], there is a growing preference for ethanol as a green and less toxic alternative without compromising performance [6] [31] [30]. The ratio of organic to aqueous buffer typically ranges from 30:70 to 50:50, optimized to elute all compounds within a reasonable time window with baseline resolution.
- Buffer and pH Control: The use of a 10-50 mM phosphate buffer is prevalent for controlling pH and ionic strength [6] [32] [30]. The pH of the mobile phase is a critical parameter that dictates the ionization state of ionizable analytes, thereby profoundly affecting their retention. For example, methods developed at pH 5.2 [6] and pH 2.5 [30] demonstrate that the optimal pH is drug-dependent. A pH ~2-3 is often used to suppress the ionization of acidic silanol groups on the silica surface, improving peak shape for basic drugs.
- Elution Mode: Isocratic elution is suitable for simpler mixtures with analytes of similar polarity, offering runtime consistency and instrument simplicity [6] [30]. For complex mixtures with a wide polarity range, gradient elution is necessary, as it progressively increases the organic solvent strength to elute highly retained compounds within a manageable total run time [31] [32].
The following workflow diagrams the logical process for developing and optimizing an HPLC method for this application.
Diagram 1: A logical workflow for HPLC method development, highlighting column selection and pH screening as critical, iterative steps.
Detailed Experimental Protocol
Materials and Equipment
- HPLC System: Alliance 2695 HPLC system (Waters) or equivalent, equipped with a quaternary pump, auto-sampler, column oven, and a fluorescence detector (FLD) and/or photodiode array (PDA) detector [6] [30].
- Software: Empower or equivalent for data acquisition and processing.
- Columns: Thermo Hypersil BDS C18 column (150 mm × 4.6 mm, 5.0 µm) [6] or equivalent.
- Chemicals: HPLC-grade ethanol, potassium dihydrogen phosphate (KH₂PO₄), ortho-phosphoric acid (85%), and purified water. Drug reference standards of certified purity (≥99%).
- Biological Matrix: Drug-free human plasma, stored at -20°C until use.
Step-by-Step Chromatographic Method
This protocol is adapted from validated methods for the simultaneous determination of four cardiovascular drugs [6] [29].
Mobile Phase Preparation:
- Prepare 0.03 M potassium phosphate buffer by dissolving 4.08 g of KH₂PO₄ in 1 L of purified water.
- Adjust the pH to 5.2 using 1 M potassium hydroxide (KOH) or ortho-phosphoric acid as needed.
- Filter the buffer and HPLC-grade ethanol through a 0.45 µm or 0.22 µm membrane filter under vacuum.
- Mix the buffer and ethanol in a 60:40 (v/v) ratio. Degas the final mobile phase by sonication for 10-15 minutes.
Chromatographic Conditions:
- Column Oven Temperature: 25-35°C
- Flow Rate: 0.6 mL/min
- Injection Volume: 20 µL
- Detection:
- FLD: Program the detector with the following excitation/emission wavelengths for each drug, allowing for maximum sensitivity and specificity:
- Bisoprolol (BIS): 227 nm / 298 nm
- Telmisartan (TEL): 294 nm / 365 nm
- Atorvastatin (ATV): 274 nm / 378 nm
- Amlodipine (AML): 361 nm / 442 nm
- PDA: A scan from 210-260 nm can be used for monitoring separation and peak purity.
- FLD: Program the detector with the following excitation/emission wavelengths for each drug, allowing for maximum sensitivity and specificity:
Sample Preparation (Liquid-Liquid Extraction):
- Pipette 200 µL of plasma (calibrator, quality control, or unknown sample) into a microcentrifuge tube.
- Add 50 µL of working standard solution and 600 µL of absolute ethanol. Vortex mix for 1 minute. This step precipitates plasma proteins.
- Centrifuge the mixture at 3500 rpm for 2 minutes to pellet the precipitated proteins.
- Transfer the clear supernatant to a new tube. Add 1.0 mL of diethyl ether (first extraction solvent).
- Vortex mix vigorously for 5 minutes, then centrifuge at 3500 rpm for 5 minutes at 0°C.
- Carefully transfer the upper organic layer to a clean test tube.
- Add 0.5 mL of dichloromethane (second extraction solvent) to the remaining aqueous layer. Vortex for 5 minutes and centrifuge as before.
- Combine the organic layer from this second extraction with the first.
- Evaporate the combined organic extracts to dryness under a gentle stream of nitrogen at 40°C.
- Reconstitute the dry residue in 500 µL of ethanol, vortex for 2 minutes, and transfer to an HPLC vial for injection [6].
The sample preparation and analysis process is summarized in the following workflow.
Diagram 2: A detailed experimental workflow for sample preparation via liquid-liquid extraction and subsequent HPLC-FLD analysis.
Method Validation
The developed method must be validated according to International Council for Harmonisation (ICH) or FDA bioanalytical guidelines [6] [30]. Key parameters include:
- Linearity: Prepare calibration curves in plasma over the concentration ranges of 5–100 ng/mL for BIS and AML, 0.1–5 ng/mL for TEL, and 10–200 ng/mL for ATV. The correlation coefficient (r²) should be ≥0.99 [6].
- Precision and Accuracy: Assess intra-day and inter-day precision (expressed as %RSD) and accuracy (expressed as % nominal concentration) using quality control (QC) samples at low, medium, and high concentrations. %RSD should be ≤15%, and accuracy within ±15% of the nominal value.
- Specificity: Verify that the method can unequivocally assess the analytes in the presence of endogenous plasma components, which should not show significant interference at the retention times of the drugs.
- Recovery: Evaluate the extraction efficiency (recovery) of the LLE procedure by comparing the peak areas of extracted QC samples with those of post-extraction spiked samples at equivalent concentrations.
Concluding Remarks
The optimization of chromatographic conditions is paramount for developing a successful HPLC method for the simultaneous analysis of cardiovascular drugs in plasma. This application note demonstrates that a C18 column with dimensions of 150 x 4.6 mm and 5 µm particle size, a green ethanol-based mobile phase, and careful pH control around 5.2 form a highly effective and validated system. When coupled with a simple LLE and sensitive FLD detection, this approach yields a method that is specific, sensitive, precise, and accurate, suitable for therapeutic drug monitoring and supporting clinical pharmacology studies. Future work will focus on expanding the application of this optimized framework to include a wider panel of cardiovascular agents and their major metabolites.
The simultaneous monitoring of multiple cardiovascular drugs in biological matrices, such as plasma, is essential for therapeutic drug monitoring, pharmacokinetic studies, and ensuring patient safety. This process is complicated by the complex plasma matrix and the typically low concentrations of target analytes. Dual UV and fluorescence detection has emerged as a powerful strategy to overcome these challenges, offering enhanced specificity and sensitivity within a single analytical run. This application note details the development and validation of a highly sensitive High-Performance Liquid Chromatography (HPLC) method employing this dual-detection strategy for the concurrent quantification of four common cardiovascular drugs—bisoprolol, amlodipine, telmisartan, and atorvastatin—in human plasma [6] [29]. The protocol provides a robust framework for researchers and bioanalysts requiring high-quality data for drug development and clinical monitoring.
Experimental Protocol
Materials and Reagents
- Analytical Standards: Bisoprolol fumarate (BIS), amlodipine besylate (AML), telmisartan (TEL), and atorvastatin (ATV) with certified purities (>99%) [6].
- Solvents: Ethanol, dichloromethane, and diethyl ether (HPLC or AR grade).
- Water: Double-distilled or purified water (e.g., from a Millipore system).
- Buffer Salts: Potassium dihydrogen phosphate (KH₂PO₄).
- Biological Matrix: Drug-free human plasma. Store frozen at -20 °C until use [6].
Instrumentation and Chromatographic Conditions
- HPLC System: An Alliance 2695 HPLC system or equivalent, equipped with a quaternary pump, auto-sampler, and column oven [6].
- Detectors:
- Photodiode Array (PDA) Detector: Set to a monitoring wavelength of 240 nm for initial separation confirmation [6].
- Fluorescence Detector: Configured with specific excitation/emission (ex/em) wavelengths for each analyte [6]:
- BIS: 227 nm / 298 nm
- TEL: 294 nm / 365 nm
- ATV: 274 nm / 378 nm
- AML: 361 nm / 442 nm
- Data System: Waters Alliance software or equivalent for data acquisition and processing.
- Chromatographic Column: Thermo Hypersil BDS C18 column (150 mm × 4.6 mm, 5.0 μm particle size) or equivalent [6].
- Mobile Phase: Isocratic elution with a mixture of ethanol : 0.03 M potassium phosphate buffer, pH 5.2 (40:60, v/v) [6].
- Flow Rate: 0.6 mL/min [6].
- Injection Volume: 20 μL [6].
- Column Temperature: Maintained between 25–35 °C [6].
Sample Preparation: Liquid-Liquid Extraction
The following two-step liquid-liquid extraction (LLE) protocol is used for sample clean-up and pre-concentration [6]:
Preparation of Standard Solutions
- Stock Solutions (100 µg/mL): Accurately weigh 10 mg of each drug standard and dissolve in ethanol in a 100 mL volumetric flask. Bring to volume with ethanol [6].
- Working Solutions (10 µg/mL): Prepare by diluting the stock solutions with ethanol [6].
- Calibration Standards: Spike drug-free plasma with appropriate volumes of working solutions to create calibration curves within the following ranges [6]:
- BIS and AML: 5–100 ng/mL
- TEL: 0.1–5 ng/mL
- ATV: 10–200 ng/mL
Store all standard solutions at 2–8 °C.
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential materials and reagents for the analytical method.
| Item | Function / Role in the Protocol |
|---|---|
| Thermo Hypersil BDS C18 Column | Stationary phase for reverse-phase chromatographic separation of analytes [6]. |
| Ethanol (HPLC Grade) | Organic solvent component of the mobile phase; also used for preparing standard solutions and sample reconstitution [6]. |
| Potassium Phosphate Buffer | Aqueous component of the mobile phase; buffers the pH to 5.2 to optimize separation and peak shape [6]. |
| Diethyl Ether & Dichloromethane | Organic solvents used in the two-step LLE process to efficiently extract analytes from the plasma matrix [6]. |
| Fluorescence Detector | Provides highly specific and sensitive detection of native-fluorescent analytes (BIS, AML, TEL, ATV) at optimized wavelengths [6]. |
| PDA/UV Detector | Confirms effective chromatographic separation and provides a universal detection channel [6]. |
Results and Data Presentation
Method Validation Data
The developed method was validated according to International Council for Harmonisation (ICH) guidelines, demonstrating high sensitivity, accuracy, and precision [6].
Table 2: Analytical performance data for the four cardiovascular drugs.
| Analyte | Linear Range (ng/mL) | LLOQ (ng/mL) | Key Fluorescence Detection Wavelengths (Ex/Em) |
|---|---|---|---|
| Bisoprolol (BIS) | 5 – 100 | 5 | 227 nm / 298 nm |
| Amlodipine (AML) | 5 – 100 | 5 | 361 nm / 442 nm |
| Telmisartan (TEL) | 0.1 – 5 | 0.1 | 294 nm / 365 nm |
| Atorvastatin (ATV) | 10 – 200 | 10 | 274 nm / 378 nm |
The Dual Detection Workflow
The core of this strategy lies in the complementary use of two detection modes. The UV detector confirms baseline separation of all compounds, while the fluorescence detector, with its analyte-specific wavelengths, provides a second dimension of specificity, effectively isolating the target signal from potential matrix interferences.
Discussion and Application
The integration of dual detection successfully addresses key bioanalytical challenges. The fluorescence detector's primary role is to provide high specificity and sensitivity for quantitation, capitalizing on the native fluorescent properties of the target drugs. This significantly reduces the risk of false positives from co-eluting matrix components. The UV detector serves a confirmatory role, verifying the overall chromatographic performance and separation efficiency [6]. This dual-detection approach is particularly valuable for:
- Therapeutic Drug Monitoring (TDM): Precisely tracking drug levels in patients to ensure therapeutic efficacy and avoid toxicity.
- Pharmacokinetic Studies: Accurately characterizing the absorption, distribution, metabolism, and excretion (ADME) of drug candidates.
- Adherence Monitoring: Verifying patient compliance with complex multi-drug regimens for cardiovascular diseases.
The method is further characterized by its short chromatographic run time of less than 10 minutes, providing high throughput and economic value for routine analysis [6]. The LLE sample preparation is economical and effective, providing clean extracts suitable for the sensitive detection systems.
In the development of high-performance liquid chromatography (HPLC) methods for the simultaneous determination of cardiovascular drugs in human plasma, sample preparation is a critical step to isolate analytes from the complex biological matrix. Among various sample preparation techniques, liquid-liquid extraction (LLE) remains a widely used method due to its effectiveness, simplicity, and cost-efficiency [35] [6]. LLE separates compounds based on their relative solubility in two immiscible liquids, typically using an organic solvent to extract analytes from the aqueous plasma phase [35]. This technique is particularly valuable in bioanalytical methods for cardiovascular drug monitoring, where it effectively removes proteins and interfering components, thereby enhancing the sensitivity and specificity of the subsequent chromatographic analysis [6]. The following sections provide detailed application notes and protocols for implementing LLE in sample preparation workflows, with specific examples focused on the extraction of cardiovascular drugs from human plasma.
LLE Fundamentals and Rationale
LLE operates on the principle of differential solubility, where analytes partition between an aqueous sample (plasma) and a water-immiscible organic solvent based on their chemical properties [35]. The efficiency of extraction is governed by the partition coefficient, which is influenced by factors such as solvent selection, pH adjustment, and extraction time. A key advantage of LLE is its ability to provide effective sample cleanup, reducing matrix effects that can adversely affect chromatographic separation and detection [35] [6].
In the context of a broader thesis on HPLC method development for cardiovascular drugs, LLE offers several practical benefits. The technique is compatible with a wide range of cardiovascular medications with varying polarities, including beta-blockers, calcium channel blockers, angiotensin receptor blockers, and statins [6]. Furthermore, LLE can be easily optimized and scaled for high-throughput applications, making it suitable for therapeutic drug monitoring and pharmacokinetic studies where multiple samples need to be processed efficiently.
Comparative Performance of Extraction Techniques
The following table summarizes quantitative data comparing LLE with Supported Liquid Extraction (SLE) for the determination of rosuvastatin in plasma, highlighting key performance parameters [35].
Table 1: Comparison of LLE and SLE for Rosuvastatin Extraction from Plasma
| Validation Parameter | LLE Performance | SLE Performance |
|---|---|---|
| Extraction Recovery | 60% | 96.3% |
| Precision (RSD at 0.3 ng/mL) | 13.6% | 11.9% |
| Matrix Effect | -36.7% | 12.7% |
| Linearity Range | 0.1 - 50 ng/mL | 0.1 - 50 ng/mL |
| Relative Response in Clinical Samples | Baseline | 14.6% higher |
While SLE demonstrates superior performance in several parameters, LLE remains a valuable technique, particularly in resource-limited settings or for applications where the cost of specialized SLE equipment is prohibitive. The choice between extraction techniques should be guided by the specific requirements of the analytical method, including required sensitivity, available resources, and sample throughput needs [35].
Experimental Protocol: LLE for Cardiovascular Drugs
This protocol provides a detailed methodology for extracting multiple cardiovascular drugs from human plasma, adapted from published methods for the simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin [6].
Reagents and Materials
Table 2: Essential Research Reagents and Materials
| Item | Specification | Function/Purpose |
|---|---|---|
| Human Plasma | EDTA-anticoagulated | Biological matrix for analysis |
| Solvents | Ethanol, Diethyl Ether, Dichloromethane | Protein precipitation and analyte extraction |
| Centrifuge Tubes | 5-15 mL capacity | Sample processing and phase separation |
| pH Adjustment | Ammonium Acetate Buffer (100 mM, pH 3.5) | Optimizes ionization state for efficient extraction |
| Centrifuge | Capable of 16,000 × g | Accelerates phase separation |
| Nitrogen Evaporation System | With temperature control (40°C) | Concentrates extracts prior to analysis |
| Vortex Mixer | Variable speed | Ensures thorough mixing of samples |
| Analytical Standards | Bisoprolol, Amlodipine, Telmisartan, Atorvastatin | Reference compounds for quantification |
Step-by-Step Procedure
Sample Preparation: Thaw frozen plasma samples at room temperature. Vortex briefly to ensure homogeneity.
Aliquot Plasma: Transfer 200 µL of plasma into a clean centrifuge tube.
Protein Precipitation: Add 600 µL of absolute ethanol to the plasma. Vortex the mixture for 30 seconds, then centrifuge at 16,000 × g for 2 minutes to pellet precipitated proteins.
First Extraction: Transfer the supernatant to a new tube. Add 1.0 mL of diethyl ether (first extraction solvent). Vortex vigorously for 5 minutes, then centrifuge at 3,500 rpm for 5 minutes at 0°C.
Phase Separation: Carefully collect the organic (upper) layer and transfer it to a clean test tube.
Second Extraction: To the remaining aqueous layer, add 0.5 mL of dichloromethane (second extraction solvent). Vortex for 5 minutes, then centrifuge at 3,500 rpm for 5 minutes at 0°C.
Combine Extracts: Collect the organic layer and combine it with the previously collected diethyl ether fraction.
Concentration: Evaporate the combined organic extracts to dryness under a gentle stream of nitrogen at 40°C.
Reconstitution: Reconstitute the dry residue in 500 µL of ethanol. Vortex for 2 minutes to ensure complete dissolution.
Analysis: Transfer the reconstituted extract to an HPLC vial for analysis. The sample is now ready for injection into the HPLC system [6].
Method Optimization Notes
pH Adjustment: For acidic or basic compounds, adjust the pH of the plasma sample before extraction to suppress ionization of the analytes, thereby enhancing their partitioning into the organic phase. The required pH varies depending on the pKa of the target analytes [35] [36].
Solvent Selection: The choice of extraction solvent should be optimized based on the polarity of the target cardiovascular drugs. A mixture of solvents with different polarities may improve extraction efficiency for multiple analytes with diverse chemical properties [6] [37].
Extraction Time: Ensure consistent extraction times across all samples, as the duration of mixing can impact partitioning equilibrium and extraction efficiency [6].
The workflow for this LLE procedure is summarized in the following diagram:
Applications in Cardiovascular Drug Analysis
LLE has been successfully implemented in HPLC methods for various cardiovascular drugs, demonstrating its versatility across different drug classes:
Multiple Drug Monitoring: An HPLC method with dual detection utilized LLE for the simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin in human plasma, achieving linearity across clinically relevant concentration ranges (5-100 ng/mL for bisoprolol and amlodipine, 0.1-5 ng/mL for telmisartan, and 10-200 ng/mL for atorvastatin) [6].
Statin Analysis: For rosuvastatin determination, LLE demonstrated satisfactory performance with 60% extraction recovery and 13.6% precision, making it a viable option for therapeutic drug monitoring of this important lipid-lowering agent [35].
Broad Compatibility: The technique has been adapted for various cardiovascular medications, including beta-blockers, calcium channel blockers, and angiotensin receptor blockers, highlighting its flexibility in method development [6] [37].
Troubleshooting and Technical Considerations
Common Challenges and Solutions
Low Recovery: If extraction recovery is suboptimal, consider modifying the solvent system or incorporating pH adjustment to enhance partitioning of ionizable compounds [35] [6].
Matrix Effects: To minimize ion suppression or enhancement in mass spectrometric detection, ensure complete protein precipitation and efficient separation of organic and aqueous phases [35].
Evaporation Losses: When evaporating solvent, maintain a controlled temperature and avoid complete dryness for volatile compounds to prevent analyte loss [6].
Quality Control Measures
Internal Standards: Use appropriate internal standards (preferably stable isotope-labeled analogs) to correct for variability in extraction efficiency and matrix effects [35] [6].
Process Blanks: Include extraction blanks to monitor for contamination and ensure the cleanliness of the extraction process.
Quality Controls: Implement quality control samples at multiple concentrations to validate extraction consistency across batches [6].
LLE remains a fundamental sample preparation technique in bioanalytical method development for cardiovascular drugs in human plasma. While novel extraction technologies such as SLE offer improved performance in some aspects, LLE provides a cost-effective, robust, and widely accessible alternative that delivers satisfactory results for many applications. The protocol detailed in this document provides a reliable foundation for researchers developing HPLC methods for the simultaneous determination of cardiovascular drugs, with opportunities for further optimization based on specific analyte characteristics and methodological requirements.
The concomitant use of multiple drugs is a common strategy to manage cardiovascular diseases, a leading cause of global mortality. Therapeutic drug monitoring of these compounds in plasma is crucial for ensuring efficacy and safety. This application note details a highly sensitive, validated High-Performance Liquid Chromatography (HPLC) method with fluorescence detection for the simultaneous quantification of four key cardiovascular drugs—bisoprolol (BIS), amlodipine besylate (AML), telmisartan (TEL), and atorvastatin (ATV)—in human plasma. The method provides a robust, selective, and economical solution for pharmaceutical analysis and clinical research [38] [29].
Experimental Protocols
Reagents and Solutions
- Drug Standards: Bisoprolol, Amlodipine besylate, Telmisartan, and Atorvastatin reference standards.
- Solvents: Ethanol, dichloromethane, and diethyl ether (HPLC grade or equivalent).
- Buffer: 0.03 M Potassium dihydrogen phosphate (KH₂PO₄) buffer, adjusted to pH 5.2.
- Stock and Working Solutions: Prepare stock solutions of each drug at 100 µg/mL in ethanol. Subsequently, dilute these stocks with ethanol to obtain working solutions at 10 µg/mL. Store all standard solutions at 2–8 °C [38].
Instrumentation and Chromatographic Conditions
The methodology was developed using a Waters Alliance 2695 HPLC system, though equivalent systems can be employed.
- HPLC System: Equipped with a quaternary pump, auto-sampler, and column oven.
- Detector: Multi-wavelength fluorescence detector.
- Column: Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 µm) or equivalent.
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in a 40:60 ratio [38].
- Flow Rate: 0.6 mL/min [38].
- Injection Volume: 20 µL [38].
- Detection Wavelengths: The fluorescence detector was set at specific excitation/emission (ex/em) wavelengths for each analyte, as defined in Table 1 [38].
Sample Preparation: Liquid-Liquid Extraction
The following two-step liquid-liquid extraction (LLE) protocol is used for processing human plasma samples [38].
Method Validation
The method was validated according to International Council for Harmonisation (ICH) guidelines [38]. Key validation parameters are summarized below.
- Linearity and Calibration: Calibration curves were constructed for each analyte in spiked human plasma. The lower limit of quantification (LLOQ) was defined as the lowest concentration on the calibration curve that could be quantified with acceptable accuracy and precision [38].
- Accuracy and Precision: The intra-day and inter-day accuracy and precision were evaluated using quality control samples at multiple concentration levels.
- Selectivity: The selectivity of the method was confirmed by analyzing blank human plasma samples to ensure no endogenous compounds interfered with the analytes or the internal standard.
- Recovery: The extraction recovery for each analyte was determined by comparing the peak areas of extracted samples with those of post-extraction spiked samples.
Results and Data Presentation
Analytical Figures of Merit
The method demonstrated excellent performance characteristics for the simultaneous analysis of the four target drugs.
Table 1: Validation Parameters and Chromatographic Detection for the Four Cardiovascular Drugs
| Analyte | Linear Range (ng/mL) | LLOQ (ng/mL) | Fluorescence Detection (ex/em) |
|---|---|---|---|
| Bisoprolol (BIS) | 5 - 100 | 5 | 227 / 298 nm |
| Amlodipine (AML) | 5 - 100 | 5 | 361 / 442 nm |
| Telmisartan (TEL) | 0.1 - 5 | 0.1 | 294 / 365 nm |
| Atorvastatin (ATV) | 10 - 200 | 10 | 274 / 378 nm |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions and Materials
| Item | Function / Purpose |
|---|---|
| Thermo Hypersil BDS C18 Column | Stationary phase for reverse-phase chromatographic separation of the drug mixture [38]. |
| Ethanol & Phosphate Buffer | Components of the mobile phase; responsible for eluting the analytes from the column [38]. |
| Diethyl Ether & Dichloromethane | Organic solvents used in the two-step LLE process to efficiently extract the target drugs from the plasma matrix [38]. |
| Potassium Dihydrogen Phosphate | Used to prepare the aqueous component of the mobile phase, with pH critical for peak shape and separation [38]. |
| Reference Standards (BIS, AML, TEL, ATV) | Highly pure substances used to prepare calibration standards for accurate quantification [38]. |
Discussion
The described HPLC-FLD method provides a complete solution for the simultaneous quantification of four essential cardiovascular drugs in human plasma. The use of fluorescence detection after a simple LLE extraction significantly enhances method selectivity and sensitivity compared to UV detection alone, as it minimizes potential interference from complex plasma matrices [38]. The validated linear ranges and LLOQs are suitable for monitoring therapeutic concentrations, making this method applicable for bioequivalence studies, pharmacokinetic research, and therapeutic drug monitoring in clinical settings [38].
A key economical advantage of this protocol is the short chromatographic run time of less than 10 minutes, which enables high sample throughput [38]. Furthermore, the isocratic elution mode simplifies the instrumental setup and operation, making the method robust and easily transferable to other quality control or research laboratories. The method has demonstrated significant improvements in robustness, sensitivity, and accuracy over traditional approaches, making it a valuable tool for ensuring drug safety and quality assurance in both research and manufacturing environments [39].
Cardiovascular diseases (CVDs) remain the leading cause of death globally, accounting for approximately 17.9 million deaths annually [40]. Effective management often requires multi-drug therapy, creating a demand for analytical methods capable of simultaneous determination of cardiovascular drugs in biological matrices [7]. This case study details the development and validation of an eco-friendly bioanalytical reversed-phase high-performance liquid chromatography (RP-HPLC) method with fluorescence detection for the simultaneous quantification of two antihypertensive drugs—felodipine (FDP) and metoprolol (MTP)—in spiked human plasma [40].
The methodology aligns with the principles of Green Analytical Chemistry (GAC), emphasizing the reduction of hazardous solvent use, waste generation, and energy consumption without compromising analytical performance [41] [42]. This protocol is presented within the broader research context of developing sustainable HPLC methods for therapeutic drug monitoring and pharmacokinetic studies of cardiovascular agents.
Key Analytical Parameters and Method Performance
The green HPLC method was rigorously validated according to ICH Q2(R2) and FDA bioanalytical guidelines [40]. The tables below summarize the critical chromatographic conditions and validation results.
Table 1: Chromatographic Conditions for Felodipine and Metoprolol Analysis
| Parameter | Specification |
|---|---|
| Column | Inertsil C18 (150 mm × 4.6 mm ID; 5 µm particle size) |
| Mobile Phase | Ethanol: 30 mM KH₂PO₄ Buffer (pH 2.5 ± 0.1) (40:60, v/v) |
| Flow Rate | 1.0 mL/min |
| Temperature | Ambient |
| Detection (FLD) | Felodipine: λex/λem = 361/442 nm [6]; Metoprolol: Specific wavelengths optimized |
| Injection Volume | 20 µL |
| Internal Standard | Tadalafil (TDL) |
| Run Time | < 10 min [6] |
Table 2: Method Validation Results for API and Spiked Human Plasma
| Validation Parameter | Felodipine | Metoprolol |
|---|---|---|
| Linearity Range (µg/mL) | 0.01 – 1.00 | 0.003 – 1.00 |
| Correlation Coefficient (r²) | 0.9998 | 0.9999 |
| Intra-day Precision (% RSD) | ≤ 2.0% | ≤ 2.0% |
| Inter-day Precision (% RSD) | ≤ 2.0% | ≤ 2.0% |
| Accuracy (Nominal Concentration) | Within ±2% (Pure Form); Within ±10% (Plasma) | Within ±2% (Pure Form); Within ±10% (Plasma) |
| Greenness Assessment | AGREE, MoGAPI, and RGBfast tools confirmed eco-friendly nature [40] |
Experimental Protocols
Materials and Reagent Solutions
Table 3: Research Reagent Solutions and Essential Materials
| Item | Specification | Function/Purpose |
|---|---|---|
| Felodipine & Metoprolol | Certified purity (≥99.6%) by USP/BP methods [40] | Primary analytical standards for calibration |
| Tadalafil (TDL) | Certified purity (99.9%) | Internal Standard (IS) |
| Ethanol (HPLC Grade) | ≥99.8% [40] | Green organic solvent in mobile phase [43] |
| Potassium Dihydrogen Phosphate | ≥99.0% [40] | Buffer component for mobile phase |
| ortho-Phosphoric Acid | ≥85% [40] | Mobile phase pH adjustment |
| Human Plasma | Drug-free, from licensed provider (e.g., VACSERA) [40] | Biological matrix for method development |
| Logimax Tablets | 5 mg FDP & 50 mg MTP tartrate/tablet [40] | Pharmaceutical formulation for application |
Sample Preparation Protocol
Stock and Working Standard Solutions
- Stock Solutions (1 mg/mL): Accurately weigh 10 mg of FDP, MTP, and TDL (IS) into separate 10 mL volumetric flasks. Dissolve in a minimum amount of methanol and dilute to volume with ultrapure water [40].
- Working Solutions: Prepare working standard solutions from stock solutions by serial dilution with the mobile phase to obtain final concentrations of 100.00 µg/mL, 10.00 µg/mL, and 1.00 µg/mL for FDP, MTP, and TDL, respectively. Store all solutions at 5°C [40].
Plasma Sample Extraction
- Spiking: Transfer 200 µL of drug-free human plasma into a microcentrifuge tube.
- Internal Standard: Add a known volume of TDL working solution (e.g., 50 µL) [40].
- Calibration Standards/QCs: Spike with appropriate volumes of FDP and MTP working solutions to generate calibration standards (e.g., 0.003-1.00 µg/mL for MTP; 0.01-1.00 µg/mL for FDP) and Quality Control (QC) samples (Low, Mid, High) [40].
- Protein Precipitation: Add 600 µL of absolute ethanol to the plasma mixture. Vortex vigorously for 1-2 minutes to ensure complete mixing and protein precipitation [6].
- Centrifugation: Centrifuge the mixture at 3,500 - 6,000 rpm for 2-5 minutes at 0-5°C to pellet the precipitated proteins [40] [6].
- Supernatant Collection: Carefully transfer the clear supernatant to a clean test tube.
- Evaporation & Reconstitution: Evaporate the supernatant to dryness under a gentle stream of nitrogen at 40°C. Reconstitute the dry residue with 500 µL of the HPLC mobile phase, vortex for 2 minutes, and transfer to an HPLC vial for injection [6].
Instrumental Analysis and Methodology
- HPLC System Configuration: Use an Agilent 1200 series HPLC system (or equivalent) equipped with an isocratic pump, manual Rheodyne injector, and fluorescence detector (FLD) [40].
- Chromatographic Separation:
- Column: Maintain an Inertsil C18 column (150 mm × 4.6 mm ID; 5 µm) at ambient temperature.
- Mobile Phase: Pump a degassed mixture of ethanol and 30 mM potassium dihydrogen phosphate buffer (adjusted to pH 2.5 with ortho-phosphoric acid) in a 40:60 (v/v) ratio.
- Flow Rate: 1.0 mL/min.
- Injection Volume: 20 µL [40] [6].
- Detection: Set the FLD to the optimized excitation and emission wavelengths. While FDP is detected at 361/442 nm [6], specific wavelengths for MTP should be optimized during method development based on the instrument used.
- System Suitability Test (SST): Before sample analysis, perform an SST by making six replicate injections of a standard solution. The test is acceptable if the relative standard deviation (RSD) for peak areas is <2.0%, confirming system precision [44].
Greenness Assessment
The method's environmental friendliness was evaluated using multiple green assessment tools [40]:
- AGREE Calculator: Provides a comprehensive score based on all 12 principles of GAC [42].
- MoGAPI (Modified Green Analytical Procedure Index): Offers a visual and scoring-based evaluation of the entire analytical workflow [42].
- RGBfast Study: Assesses the method against the principles of White Analytical Chemistry, balancing Red (analytical performance), Green (environmental impact), and Blue (practical applicability) [7] [42].
Key green attributes of this method include:
- Eco-friendly Solvent: Substitution of toxic solvents like acetonitrile with the safer, bio-renewable ethanol [43].
- Reduced Waste Generation: The isocratic elution mode and efficient separation contribute to lower solvent consumption and waste production compared to conventional methods [41].
- Energy Efficiency: Operation at ambient temperature reduces energy consumption associated with column thermostat control [40].
Application in Pharmaceutical Analysis
The validated method was successfully applied to:
- Simultaneous Determination in Formulations: Analyze the commercial combined dosage form Logimax tablets. Ten tablets were weighed, powdered, and an amount equivalent to one tablet was dissolved and diluted to obtain final concentrations of 0.10 µg/mL of FDP and 1.00 µg/mL of MTP [40].
- Bioanalytical Application: Quantify FDP and MTP in spiked human plasma, demonstrating the method's suitability for pharmacokinetic, bioequivalence, and therapeutic drug monitoring studies [40]. The method proved robust, sensitive, and capable of handling the complex plasma matrix with high precision and accuracy.
Solving Common HPLC Challenges and Enhancing Method Performance
In the development of a high-performance liquid chromatography (HPLC) method for the simultaneous determination of cardiovascular drugs in plasma, achieving optimal separation efficiency is a fundamental challenge. Two prevalent issues—co-elution (where multiple analytes elute simultaneously) and broad peaks (which reduce sensitivity and resolution)—can compromise data accuracy and reliability [45] [46]. These challenges are particularly acute in bioanalytical applications, where complex plasma matrices and structurally similar drug molecules demand highly selective and robust methods [6].
This Application Note provides a structured, practical framework for diagnosing and resolving these separation inefficiencies. By integrating fundamental chromatographic principles with targeted optimization strategies, we present a comprehensive protocol to enhance method performance for the precise quantification of cardiovascular drugs.
Theoretical Foundations of Peak Resolution
The resolution (Rs) between two peaks is fundamentally described by the following equation, which isolates the three primary parameters that can be manipulated to improve separations [45]:
Where:
- N is the column efficiency (plate number), affecting peak width and sharpness.
- α (alpha) is the selectivity factor, representing the relative spacing between two peaks.
- k is the retention factor, describing how strongly an analyte is retained on the column.
This equation guides method development by indicating that improving resolution can be achieved by increasing column efficiency (N), enhancing selectivity (α), or optimizing retention (k) [45].
Diagnostic and Optimization Workflow
The following diagram illustrates a systematic workflow for diagnosing and resolving co-elution and broad peaks. This structured approach ensures efficient problem-solving by targeting the most likely causes first.
Addressing Co-elution by Enhancing Selectivity (α)
Co-elution occurs when analytes have insufficient chemical differentiation under the current chromatographic conditions. The primary strategy is to increase selectivity (α).
Mobile Phase Optimization
The mobile phase composition is the most powerful tool for altering selectivity [45] [47].
- Adjust Solvent Strength (%B): Modify the percentage of organic solvent (%B) to shift retention times (k). Reducing %B increases retention, potentially spacing out crowded peaks at the beginning of the chromatogram [45] [48].
- Change Organic Modifier: Different solvents interact uniquely with analytes and the stationary phase. If co-elution persists with acetonitrile, switch to methanol or tetrahydrofuran (THF) using solvent strength charts to approximate equivalent elution strength [45]. For example, 50% acetonitrile is roughly equivalent to 57% methanol or 35% THF in terms of elution strength [45].
- Control pH: For ionizable analytes (e.g., many cardiovascular drugs), pH is a critical parameter. Adjusting the buffer pH can significantly alter the ionization state of acids and bases, dramatically impacting retention and selectivity. Ensure the selected pH is stable and within the column's operating range [47] [49]. A well-chosen buffer (e.g., phosphate, acetate) is essential for maintaining consistent pH [47].
- Utilize Additives: Incorporate ion-pairing reagents for highly acidic or basic compounds that are difficult to retain. Additives like alkyl sulfonates can improve the retention and peak shape of basic compounds [47] [49].
Column Chemistry and Temperature
- Stationary Phase: Changing the bonded phase ligand (e.g., from C18 to C8, phenyl, or cyano) can drastically alter selectivity by introducing different chemical interactions (e.g., π-π interactions) [45] [49].
- Column Temperature: Elevated temperatures reduce mobile phase viscosity and can improve mass transfer, leading to sharper peaks. Temperature changes can also alter the relative retention (α) of ionizable compounds, resolving co-elutions [45] [48]. Example: Increasing the temperature from 70 °C to 100 °C successfully resolved overlapping peaks of amyloid β peptides [45].
Addressing Broad Peaks by Improving Efficiency (N)
Broad, inefficient peaks lack sharpness, reducing resolution and sensitivity. The primary strategy is to increase the plate number (N).
Column Parameters
- Particle Size: Columns packed with smaller particles (e.g., 1.8-3 µm) provide higher efficiency and sharper peaks compared to larger particles (e.g., 5 µm) due to reduced flow path heterogeneity [45] [48]. Example: A benzodiazepine mixture showed resolution improvement from 0.8 to 1.25 when a column with smaller particles was used [45].
- Column Length: Increasing column length provides more theoretical plates for separation. Doubling the column length from 100 mm to 200 mm improved the peak capacity by 40% in the separation of a protein digest [45]. Note that this also increases backpressure and analysis time.
Method Parameters
- Flow Rate: Lowering the flow rate can enhance efficiency by allowing more time for analyte mass transfer between the mobile and stationary phases, resulting in narrower peaks [48]. Find the optimal balance between resolution and analysis time.
- Column Temperature: As noted, higher temperatures can increase efficiency by improving diffusion rates [45].
- Injection Volume: Avoid mass overload, which can cause peak broadening and fronting. A general guideline is to inject 1-2% of the total column volume for sample concentrations around 1 µg/µL [48].
System Maintenance
- Extra-Column Effects: Instrument tubing with large internal diameters or long lengths, along with poorly matched detector flow cells, can contribute significantly to peak broadening before and after the column.
- Column Health: A degraded or contaminated column will lose efficiency over time, leading to broader peaks. Follow the manufacturer's maintenance and cleaning procedures [48].
Table 1: Troubleshooting Guide for Co-elution and Broad Peaks
| Symptom | Potential Cause | Corrective Action |
|---|---|---|
| Co-elution | Insufficient selectivity (α) | Change organic modifier (MeOH, THF instead of ACN) [45] |
| Adjust mobile phase pH to alter ionization [47] | ||
| Use a different column chemistry (e.g., C8, Phenyl) [45] | ||
| Overloaded column | Reduce sample injection volume or concentration [48] | |
| Broad Peaks | Low column efficiency (N) | Use a column with smaller particle size [45] |
| Increase column length (if pressure allows) [45] | ||
| Suboptimal flow rate | Lower the flow rate to improve efficiency [48] | |
| High system volume | Reduce extra-column volume (check tubing, fittings) | |
| Column degradation | Clean or replace the HPLC column [48] |
Application Protocol: Resolving Co-elution in Cardiovascular Drug Analysis
The following protocol is adapted from a validated method for the simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin in human plasma [6] [29].
Experimental Workflow
The detailed workflow for sample preparation and analysis is outlined below.
Materials and Equipment
- HPLC System: Waters Alliance 2695 system with quaternary pump and auto-sampler [6].
- Detectors:
- Analytical Column: Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 µm) [6].
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in a 40:60 ratio [6].
- Flow Rate: 0.6 mL/min (isocratic elution) [6].
- Column Temperature: Maintained between 25–35°C [6].
Sample Preparation Procedure
- Protein Precipitation: To a 200 µL aliquot of plasma sample (or spiked standard), add 600 µL of absolute ethanol. Vortex the mixture thoroughly and centrifuge for 2 minutes to precipitate proteins [6].
- Liquid-Liquid Extraction (LLE) - Step 1: Transfer the supernatant to a clean tube. Add 1.0 mL of diethyl ether (first extraction solvent). Vortex the mixture for 5 minutes, then centrifuge at 3500 rpm for 5 minutes at 0°C. Carefully collect and transfer the organic (upper) layer to a new test tube [6].
- LLE - Step 2: To the remaining aqueous layer, add 0.5 mL of dichloromethane (second extraction solvent). Vortex for 5 minutes and centrifuge again at 3500 rpm for 5 minutes at 0°C. Collect the organic layer [6].
- Combination and Evaporation: Combine the organic layers from the first and second extractions. Evaporate the combined extract to dryness under a gentle stream of nitrogen gas at 40°C [6].
- Reconstitution: Reconstitute the dry residue in 500 µL of ethanol by vortexing for 2 minutes [6].
- Injection: Inject 20 µL of the prepared solution into the HPLC system [6].
Method Optimization Notes
- Selectivity: The use of a C18 column with a mildly acidic mobile phase (pH 5.2) provides a balanced retention and selectivity for the four cardiovascular drugs, which have varying pKa values and polarities [6].
- Sensitivity: The two-step LLE and dual detection (PDA and FLD) provide high sensitivity and specificity, effectively removing plasma matrix interferences and allowing for precise quantification at nanogram-per-milliliter levels [6] [29].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for HPLC Method Development and Analysis
| Item | Function / Application |
|---|---|
| C18 Analytical Column (e.g., 150 mm x 4.6 mm, 5 µm) | The primary stationary phase for reversed-phase separation of non-polar to moderately polar analytes; a versatile starting point [49]. |
| Acetonitrile & Methanol (HPLC Grade) | Organic modifiers for the mobile phase in reversed-phase HPLC; used to control elution strength and selectivity [45] [47]. |
| Potassium Phosphate Buffer Salts | For preparing aqueous buffer solutions to control mobile phase pH, which is critical for the separation of ionizable compounds [6] [47]. |
| Ion-Pairing Reagents (e.g., Alkyl sulfonates) | Additives used to improve the retention and peak shape of highly ionic or ionizable compounds that are poorly retained in standard RPLC [47]. |
| Solid-Phase Extraction (SPE) Cartridges | For complex sample clean-up and pre-concentration of analytes from biological matrices like plasma, reducing matrix effects [50]. |
| Protein Precipitation Solvents (e.g., Ethanol, Acetonitrile) | Used to denature and remove proteins from biological samples during the initial preparation step [6] [50]. |
| Fluorescence Detector (FLD) | A highly specific and sensitive detection method for analytes possessing native fluorescence or that can be derivatized to become fluorescent [6]. |
Resolving co-elution and broad peaks in HPLC methods for cardiovascular drug analysis requires a systematic approach grounded in the fundamental resolution equation. By sequentially optimizing selectivity (α) through mobile phase and column chemistry, and efficiency (N) through column parameters and instrument conditions, a robust, high-resolution method can be achieved. The provided protocol and troubleshooting guide offer a practical pathway for researchers to enhance their analytical methods, ensuring accurate and reliable simultaneous quantification of drugs in complex plasma matrices.
{title}
Strategies for Enhancing Sensitivity and Lowering Limits of Detection (LOD)
In the development of High-Performance Liquid Chromatography (HPLC) methods for the simultaneous determination of cardiovascular drugs in plasma, achieving superior sensitivity and low Limits of Detection (LOD) is paramount for accurate pharmacokinetic profiling and therapeutic drug monitoring. The LOD is defined as the lowest concentration of an analyte that can be reliably detected, though not necessarily quantified, under the stated conditions of the method, and is globally accepted at a signal-to-noise ratio (S/N) of 3:1 [51] [52] [53]. For researchers analyzing complex biological matrices like plasma, enhancing method sensitivity directly translates to the ability to detect trace-level drug concentrations and their metabolites, thereby providing critical data for clinical decision-making. This document outlines a structured framework of strategies, categorized into signal enhancement and noise reduction, and provides a detailed, applicable protocol from a recent successful bioanalytical study on cardiovascular drugs [6].
Core Enhancement Strategies
Improving the LOD in HPLC is a dual-pronged approach that involves increasing the analyte signal while simultaneously reducing the background noise. The following strategies have been proven effective for methods involving cardiovascular drugs in plasma.
Table 1: Strategies for Enhancing Sensitivity and Lowering LOD
| Strategy Category | Specific Technique | Key Mechanism | Application Note |
|---|---|---|---|
| Signal Enhancement | Reduce Column Internal Diameter (ID) [51] | Increases analyte concentration at detection; halving ID yields ~4x higher concentration. | Ideal for limited sample volumes; requires adjustment of injection volume and flow rate. |
| Increase Column Efficiency [51] [54] | Uses smaller or superficially porous particles (e.g., core-shell) to produce narrower, taller peaks. | Replacing a 3 µm fully porous with a 2.7 µm core-shell particle can nearly double efficiency. | |
| Optimize Detection Wavelength [54] [55] | Operate at the analyte's λmax or a compromise wavelength for multiple compounds. | For low-concentration degradants, a wavelength offering superior sensitivity (e.g., 272 nm) is critical [55]. | |
| Utilize Fluorescence Detection (FLD) [6] | Leverages native fluorescence of analytes for superior specificity and lower LOD vs. UV. | Method for bisoprolol, amlodipine, telmisartan, and atorvastatin used optimized excitation/emission pairs. | |
| Noise Reduction | Purify Mobile Phase & Solvents [51] [53] | Reduces UV-absorbing impurities that contribute to baseline noise, especially at low wavelengths. | Use high-purity HPLC/MS-grade solvents. Acetonitrile is preferred over methanol for low UV wavelengths [54] [53]. |
| Optimize Mobile Phase Additives [54] | Selects volatile additives (e.g., formic acid) that do not contribute to UV absorbance or MS noise. | For amines, 0.1% formic acid can reduce tailing and improve peak shape [54]. | |
| Implement Stringent Sample Cleanup [6] [56] | Removes matrix interferences (e.g., proteins) via Liquid-Liquid Extraction (LLE) or Solid-Phase Extraction (SPE). | LLE with diethyl ether and dichloromethane effectively cleaned up human plasma samples for drug analysis [6]. | |
| Maintain HPLC System & Column [51] [53] | Prevents contamination and column bleeding that increase baseline noise. | Perform regular system cleaning, use guard columns, and replace old separation columns. | |
| Advanced Approaches | On-line Sample Pre-concentration [56] | Automates analyte concentration and cleanup via on-line SPE, reducing manual handling and contamination. | Significantly improves throughput and reproducibility for trace-level analysis. |
| Nano-LC or Micro-LC [56] | Dramatically increases analyte concentration and ionization efficiency via reduced column ID and flow rates. | Highly effective for mass spectrometry detection, though requires specialized instrumentation. |
Detailed Experimental Protocol
This protocol is adapted from a validated, highly sensitive HPLC method for the simultaneous quantification of four cardiovascular drugs—bisoprolol (BIS), amlodipine (AML), telmisartan (TEL), and atorvastatin (ATV)—in human plasma [6].
Materials and Equipment
- HPLC System: Alliance 2695 system (Waters) or equivalent, equipped with a quaternary pump, auto-sampler, and column oven.
- Detector: Dual detection system is employed:
- Photodiode Array Detector (PDA): For monitoring separation, set at 240 nm.
- Fluorescence Detector (FLD): For enhanced sensitivity and specificity. Wavelengths are set as follows [6]:
- BIS: 227 nm ex / 298 nm em
- TEL: 294 nm ex / 365 nm em
- ATV: 274 nm ex / 378 nm em
- AML: 361 nm ex / 442 nm em
- Column: Thermo Hypersil BDS C18 column (150 mm × 4.6 mm, 5.0 μm) or equivalent.
- Mobile Phase: Isocratic elution with a mixture of Ethanol and 0.03 M Potassium Phosphate Buffer (pH 5.2) in a ratio of 40:60 (v/v).
- Chemicals & Reagents: Ethanol, diethyl ether, dichloromethane, potassium dihydrogen phosphate (all HPLC grade or higher). Drug reference standards.
- Sample Preparation: Centrifuge, vortex mixer, nitrogen evaporator.
Step-by-Step Procedure
1. Sample Preparation via Liquid-Liquid Extraction (LLE):
- Pipette 200 µL of human plasma into a microcentrifuge tube.
- Add 50 µL of the working standard solution and 600 µL of absolute ethanol.
- Vortex the mixture for 30 seconds and centrifuge at ≥3500 rpm for 2 minutes to precipitate proteins.
- Transfer the supernatant to a new clean tube.
- Add 1.0 mL of diethyl ether (first extraction solvent), vortex for 5 minutes, and centrifuge at 3500 rpm for 5 minutes at 0°C. Transfer the organic (upper) layer to another tube.
- Add 0.5 mL of dichloromethane (second extraction solvent) to the remaining solution, vortex for 5 minutes, and centrifuge again under the same conditions. Combine this organic layer with the first extract.
- Evaporate the combined organic layers to dryness under a gentle stream of nitrogen at 40°C.
- Reconstitute the dry residue in 500 µL of ethanol, vortex for 2 minutes, and transfer to an HPLC vial [6].
2. Chromatographic Separation:
- Maintain the column temperature between 25–35°C.
- Set the mobile phase flow rate to 0.6 mL/min.
- Set the injection volume to 20 µL.
- Equilibrate the system with the mobile phase until a stable baseline is achieved.
- Inject the prepared sample and run the isocratic method for less than 10 minutes [6].
3. Data Acquisition and LOD Determination:
- Acquire chromatographic data using both PDA and FLD.
- For LOD estimation, prepare and analyze samples with progressively lower analyte concentrations.
- Calculate the LOD based on a signal-to-noise ratio (S/N) of 3:1, measured from the chromatogram of the lowest concentration sample that yields a detectable peak [6] [52] [53]. The peak height (H) of the analyte is measured from the maximum of the peak to the extrapolated baseline, and the noise (h) is the range of the background noise in a blank injection over a distance equivalent to 20 times the peak width at half-height. LOD is the concentration that gives S/N = H/h ≥ 3 [52].
Workflow Diagram
The following diagram illustrates the complete experimental workflow for the simultaneous determination of cardiovascular drugs in plasma.
The Scientist's Toolkit
The following reagents and materials are essential for implementing the described protocol and achieving high sensitivity in plasma analysis.
Table 2: Key Research Reagent Solutions for Sensitive Plasma Analysis
| Item | Function / Rationale |
|---|---|
| C18 Chromatography Column (e.g., 150 mm x 4.6 mm, 5 µm) | Provides the stationary phase for reverse-phase separation of drugs. A column with high efficiency, such as one packed with core-shell particles, is recommended for sharper peaks [51] [6]. |
| Ethanol & Phosphate Buffer (pH 5.2) | Serves as the mobile phase. The specific pH and composition are critical for achieving baseline separation of the target analytes and maintaining column stability [6]. |
| Diethyl Ether & Dichloromethane | Organic solvents used in the sequential LLE process to efficiently extract the target drugs from the complex plasma matrix while leaving interfering proteins and polar compounds behind [6]. |
| Fluorescence Detector (FLD) | Provides highly specific and sensitive detection for analytes with native fluorescence, drastically reducing baseline noise and LOD compared to UV detection in complex matrices [6]. |
| Solid-Phase Extraction (SPE) Cartridges | An alternative or complementary sample clean-up technique that can selectively adsorb analytes and remove interferences, often leading to lower matrix effects and higher recovery rates [56]. |
| LC-MS Grade Solvents & Additives | High-purity solvents are essential to minimize baseline noise, particularly for low-wavelength UV detection and mass spectrometry, where impurities can cause significant interference [56]. |
Managing Matrix Effects and Improving Extraction Recovery from Plasma
In the development of high-performance liquid chromatography (HPLC) methods for the simultaneous determination of cardiovascular drugs in human plasma, two of the most significant analytical challenges are managing matrix effects and ensuring high extraction recovery. Matrix effects, defined as the impact of all sample components other than the analytes of interest, can suppress or enhance the analyte signal, leading to inaccurate quantification [57] [58]. These effects are particularly pronounced in complex biological matrices like plasma, which contains phospholipids, proteins, and other endogenous compounds that can co-elute with target analytes [58].
Simultaneously, achieving consistent and high extraction recovery is crucial for method sensitivity and reproducibility, especially when monitoring multiple cardiovascular drugs with differing physicochemical properties. This application note, framed within broader thesis research on HPLC method development, details standardized protocols and strategies to overcome these challenges, ensuring reliable bioanalysis for therapeutic drug monitoring and pharmacokinetic studies.
Understanding and Mitigating Matrix Effects
Mechanisms and Impact
In liquid chromatography, particularly when coupled with mass spectrometry (LC-MS), matrix effects primarily arise when co-eluting compounds from the biological matrix interfere with the ionization process of the target analytes [58]. This interference can cause ion suppression or enhancement, adversely affecting the accuracy and precision of quantification [57]. The electrospray ionization (ESI) source is notably more vulnerable to these effects compared to other ionization techniques [57].
Critically, matrix effects are not limited to ionization interference. Recent research demonstrates that matrix components can also significantly alter the retention time and shape of LC peaks, challenging the fundamental chromatographic principle that one compound yields one peak with a reliable retention time [57]. This can lead to misidentification and erroneous quantification of analytes in complex samples.
Practical Strategies for Minimization
Several practical strategies can be employed to mitigate matrix effects:
- Sample Cleanup: Utilizing effective sample preparation techniques is the first line of defense. Liquid-liquid extraction (LLE) and solid-phase extraction (SPE) can selectively isolate analytes and remove significant matrix interferents, particularly phospholipids from plasma [58]. An optimized LLE protocol for cardiovascular drugs is detailed in Section 4.1.
- Chromatographic Optimization: Adjusting HPLC conditions to achieve better separation of analytes from co-eluting matrix components is essential. This can involve optimizing the mobile phase composition, gradient profile, and column type [58]. A well-resolved separation confirms method specificity, demonstrating the ability to discriminate between analytes and interfering components [44].
- Internal Standardization: The use of isotopically labeled internal standards (IS) is considered one of the most effective approaches for compensating for matrix effects in quantitative LC-MS. Because the IS is nearly identical to the analyte, it experiences virtually the same degree of ion suppression or enhancement, allowing for accurate correction [58].
Strategies for Optimizing Extraction Recovery
Extraction recovery (ER) refers to the efficiency with which an analyte is extracted from the biological matrix. High and consistent recovery is vital for method sensitivity and reproducibility.
- Extraction Technique Selection: The choice between LLE and SPE depends on the physicochemical properties of the target analytes. For the simultaneous extraction of multiple cardiovascular drugs, a well-optimized LLE can provide excellent recovery for a wide polarity range [6].
- Solvent Optimization: The composition and pH of the extraction solvent are critical parameters. For instance, a two-step LLE using diethyl ether and dichloromethane has been successfully applied to recover drugs like bisoprolol, amlodipine, telmisartan, and atorvastatin from plasma [6].
- Minimizing Adsorption and Degradation: The extraction process should be designed to minimize analyte adsorption to surfaces and prevent degradation. This includes using silanized vials, avoiding excessive temperatures, and potentially adding antioxidant agents where necessary.
Table 1: Optimization of Extraction Recovery and Matrix Effect Mitigation
| Strategy | Key Parameters | Target Outcome | Example from Literature |
|---|---|---|---|
| Liquid-Liquid Extraction (LLE) | Solvent type/ratio, pH, number of extraction steps | High, reproducible recovery for multiple analytes; removal of phospholipids | Two-step LLE with diethyl ether & dichloromethane for 4 cardiovascular drugs [6] |
| Solid-Phase Extraction (SPE) | Sorbent chemistry, wash/elution solvents | Selective cleanup, concentration of analytes, reduced matrix effects | C18 SPE used for ecdysones in plants, demonstrating clean-up principle [59] |
| Chromatographic Optimization | Column chemistry, mobile phase, gradient profile | Separation of analytes from co-eluting matrix interferents | Specificity demonstrated by baseline resolution of API, impurities, and degradants [44] |
| Internal Standardization | Isotopically labeled analogs of analytes | Compensation for variable recovery and ionization suppression/enhancement | Use of 6 deuterated IS for 6 analytes in a multi-analyte CVD method [60] |
Detailed Experimental Protocols
Protocol: Liquid-Liquid Extraction of Cardiovascular Drugs from Plasma
This protocol is adapted from a validated method for the simultaneous extraction of bisoprolol, amlodipine, telmisartan, and atorvastatin from human plasma [6].
Workflow Overview:
Materials and Reagents:
- Human Plasma: Drug-free, typically available from biological suppliers [6].
- Extraction Solvents: HPLC-grade Diethyl Ether and Dichloromethane (DCM).
- Precipitating Solvent: Absolute Ethanol.
- Standard Solutions: Stock solutions (100 µg/mL) of target cardiovascular drugs in ethanol [6].
- Equipment: Microcentrifuge, vortex mixer, nitrogen evaporator, calibrated pipettes.
Step-by-Step Procedure:
- Sample Preparation: Pipette 200 µL of plasma into a microcentrifuge tube. Add 50 µL of the working standard solution [6].
- Protein Precipitation: Add 600 µL of absolute ethanol to the plasma. Vortex the mixture vigorously for 30 seconds, then centrifuge at >10,000 RPM for 2 minutes to pellet the precipitated proteins [6].
- First Extraction: Transfer the supernatant to a clean glass tube. Add 1.0 mL of diethyl ether. Vortex the mixture for 5 minutes, then centrifuge at 3500 RPM for 5 minutes at 0°C. Carefully transfer the upper organic layer to a new tube [6].
- Second Extraction: To the remaining aqueous layer, add 0.5 mL of dichloromethane. Vortex for 5 minutes and centrifuge again at 3500 RPM for 5 minutes at 0°C. Collect the lower organic layer and combine it with the extract from the previous step [6].
- Evaporation and Reconstitution: Evaporate the combined organic extracts to dryness under a gentle stream of nitrogen gas at 40°C. Reconstitute the dry residue in 500 µL of ethanol, vortex for 2 minutes, and transfer to an HPLC vial for analysis [6].
Protocol: Method Validation for Specificity and Matrix Effects
This protocol outlines the key experiments required to validate an HPLC method, with a focus on demonstrating specificity and assessing matrix effects as per ICH guidelines [44] [6].
Workflow Overview:
Procedure:
- Specificity: Demonstrate that the method can unequivocally assess the analyte in the presence of other components.
- Analysis of Blank Matrix: Inject at least six independent sources of blank control plasma. The chromatograms should show no significant interfering peaks at the retention times of the analytes or internal standard [44].
- Analysis of Spiked Samples: Inject blank plasma spiked with the analytes at the lower limit of quantification (LLOQ) and with known interferents (e.g., other commonly co-administered drugs). Confirm that the response for the analytes is unbiased [44].
- Matrix Effect (ME) and Extraction Recovery (ER): These are often assessed simultaneously using a post-extraction spiking technique.
- Prepare three sets of samples:
- Set A (Pure Solution): Analytes in mobile phase or reconstitution solvent (representing 100% response).
- Set B (Post-extraction Spiked): Blank plasma extracted, then the analytes spiked into the extracted residue before reconstitution.
- Set C (Pre-extraction Spiked): Blank plasma spiked with analytes before extraction, then carried through the entire extraction procedure.
- Calculate the Matrix Effect (ME) and Extraction Recovery (ER) using the formulas below, where peak areas are used for the calculations.
Matrix Effect (%) = (Mean Peak Area of Set B / Mean Peak Area of Set A) × 100Extraction Recovery (%) = (Mean Peak Area of Set C / Mean Peak Area of Set B) × 100
- A matrix effect of 100% indicates no suppression or enhancement. The precision of the ME (measured by %RSD) across different plasma lots should be ≤ 15% [60].
- Prepare three sets of samples:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Plasma Analysis of Cardiovascular Drugs
| Item | Function & Importance | Example from Protocol |
|---|---|---|
| HPLC-MS Grade Solvents | Mobile phase and sample preparation; high purity minimizes background noise and ion suppression. | Ethanol, Methanol, Acetonitrile, Water [6] [60] |
| Stable Isotope Internal Standards | Corrects for losses during extraction and variability in ionization efficiency; crucial for LC-MS accuracy. | Deuterated analogs of atorvastatin, bisoprolol, etc. [60] |
| Buffers & Modifiers | Control pH and ionic strength of mobile phase; improve chromatographic peak shape and separation. | 0.03 M Potassium Phosphate Buffer (pH 5.2), Formic Acid [6] [60] |
| SPE Cartridges / LLE Solvents | Selective extraction and cleanup of analytes from the complex plasma matrix. | Diethyl Ether, Dichloromethane (for LLE); C18 Sorbent (for SPE) [6] [59] |
| Authentic Analytical Standards | Used for calibration and quality control; defines the method's quantitative basis. | Bisoprolol, Amlodipine, Telmisartan, Atorvastatin reference standards [6] |
Effectively managing matrix effects and optimizing extraction recovery are non-negotiable for developing robust, sensitive, and reproducible HPLC methods for the simultaneous determination of cardiovascular drugs in plasma. By implementing the detailed protocols and strategies outlined herein—including a standardized LLE procedure, systematic method validation for specificity, and the mandatory use of appropriate internal standards—researchers can significantly enhance the quality and reliability of their bioanalytical data. These practices are foundational to generating meaningful results in therapeutic drug monitoring, pharmacokinetic studies, and clinical research, thereby supporting the broader objective of optimizing cardiovascular pharmacotherapy.
In the development of a high-performance liquid chromatography (HPLC) method for the simultaneous determination of cardiovascular drugs in plasma, demonstrating the method's reliability is as crucial as establishing its sensitivity and selectivity. Robustness testing represents a critical validation parameter that evaluates a method's capacity to remain unaffected by small, deliberate variations in method parameters [61]. For bioanalytical methods quantifying complex drug mixtures in biological matrices such as plasma, establishing robustness ensures reliability during routine use and successful transfer between laboratories [62] [63].
This application note details structured protocols for robustness testing of an HPLC method through intentional variation of three critical parameters: flow rate, temperature, and mobile phase pH. These protocols are framed within the context of an HPLC method for quantifying cardiovascular drugs—bisoprolol, amlodipine, telmisartan, and atorvastatin—in human plasma [6] [29]. The procedures align with International Council for Harmonisation (ICH) guidelines and provide a framework for establishing system suitability criteria, ensuring that the analytical method maintains performance consistency despite expected operational variations in different laboratory environments [61] [63].
Theoretical Foundations of Robustness Testing
Definitions and Regulatory Significance
The robustness of an analytical procedure is formally defined as "a measure of its capacity to remain unaffected by small but deliberate variations in method parameters and provides an indication of its reliability during normal usage" [61]. This characteristic should not be confused with ruggedness, which refers to the reproducibility of results under varying external conditions such as different laboratories, analysts, or instruments [62]. While robustness is often investigated during method development rather than formal validation, its assessment is implicitly expected by regulatory authorities including the FDA and EMA [62] [63].
For HPLC methods quantifying cardiovascular drugs in plasma, robustness testing takes on additional importance due to the complex matrix effects and the critical therapeutic drug monitoring applications. A method that demonstrates robustness ensures that pharmacokinetic studies and therapeutic monitoring produce reliable data, essential for making informed clinical decisions [6].
Critical Parameters in HPLC Robustness
In reversed-phase HPLC, numerous method parameters can influence chromatographic performance. For the simultaneous determination of multiple cardiovascular drugs, the most critical parameters typically include:
- Flow rate: Affects retention times, peak shape, and back pressure [64] [65]
- Temperature: Influences retention, selectivity, and peak efficiency [63]
- Mobile phase pH: Critically impacts ionization, retention, and selectivity of ionizable compounds [61] [64]
Other parameters such as mobile phase composition, wavelength detection, and column type may also be considered, but flow rate, temperature, and pH represent fundamental variables that laboratories must control to ensure method integrity [62] [61] [63].
Experimental Design for Robustness Assessment
Selection of Factor Levels
The cornerstone of effective robustness testing lies in selecting appropriate ranges for parameter variations. These intervals should represent the "worst-case scenario" of variations expected during routine method operation in different laboratories [61] [64]. The following table summarizes recommended ranges for the three target parameters in cardiovascular drug analysis:
Table 1: Recommended Variation Ranges for Robustness Testing
| Parameter | Nominal Value | Recommended Variation | Justification |
|---|---|---|---|
| Flow Rate | Method-specific (e.g., 0.6 mL/min [6]) | ±10% of nominal value [65] | Represents potential pump calibration drift and minor fluctuations |
| Temperature | Method-specific (e.g., 25-35°C [6]) | ±2-5°C from nominal [63] | Accounts for variations in column oven performance |
| Mobile Phase pH | Method-specific (e.g., pH 5.2 [6]) | ±0.1-0.2 pH units [61] | Reflects normal variability in buffer preparation |
For pH variations, it is important to note that asymmetric intervals may be preferable when the nominal pH is near the pKa of the analytes, as this can reveal non-linear responses that symmetric intervals might mask [61].
Experimental Design Approaches
Robustness testing can be efficiently conducted using structured experimental designs that evaluate multiple parameters simultaneously while minimizing experimental runs [62]. For assessing three factors (flow rate, temperature, and pH), a full factorial design is both practical and comprehensive.
Table 2: Full Factorial Design for Three-Factor Robustness Testing
| Experiment | Flow Rate | Temperature | pH |
|---|---|---|---|
| 1 | -10% | -2°C | -0.1 |
| 2 | -10% | -2°C | +0.1 |
| 3 | -10% | +2°C | -0.1 |
| 4 | -10% | +2°C | +0.1 |
| 5 | +10% | -2°C | -0.1 |
| 6 | +10% | -2°C | +0.1 |
| 7 | +10% | +2°C | -0.1 |
| 8 | +10% | +2°C | +0.1 |
| 9 (Center point) | Nominal | Nominal | Nominal |
This full factorial design requires only 9 experiments (including a center point) to systematically evaluate all combinations of the three parameters at two levels each [62]. The center point serves as a reference for comparison and helps identify any non-linear responses.
The following workflow diagram illustrates the complete robustness testing process:
Application Protocol: Robustness Testing for Cardiovascular Drug Analysis
Materials and Reagents
The following research reagent solutions and materials are essential for implementing this robustness testing protocol for cardiovascular drug analysis:
Table 3: Essential Research Reagent Solutions and Materials
| Item | Specification | Function/Application |
|---|---|---|
| HPLC System | Binary or quaternary pump with column oven and DAD/FLD | Method execution with precise parameter control |
| Analytical Column | Thermo Hypersil BDS C18 (150 × 4.6 mm, 5.0 μm) or equivalent [6] | Stationary phase for chromatographic separation |
| Mobile Phase | Ethanol and 0.03 M potassium phosphate buffer (40:60, v/v) [6] | Elution of cardiovascular drugs |
| pH Adjustment | Standard pH meter with calibration buffers | Precise mobile phase pH adjustment |
| Drug Standards | Bisoprolol, amlodipine, telmisartan, atorvastatin [6] | Method evaluation compounds |
| Plasma Samples | Spiked human plasma with target analytes [6] | Bioanalytical matrix for testing |
Step-by-Step Experimental Procedure
Step 1: Mobile Phase Preparation
- Prepare the mobile phase as specified in the method: 0.03 M potassium phosphate buffer and ethanol (40:60, v/v) [6]
- Adjust the buffer to the required pH values (nominal ±0.1-0.2 units) using phosphoric acid or sodium hydroxide as needed
- Filter all mobile phases through 0.45 μm membrane filters and degas prior to use
Step 2: System Setup and Equilibration
- Install the specified C18 column in the column oven
- Set the nominal flow rate (e.g., 0.6 mL/min) and allow the system to equilibrate with the nominal mobile phase
- Verify system stability through baseline monitoring
Step 3: Sample Preparation
- Prepare quality control samples of the cardiovascular drugs in processed human plasma [6]
- Use concentrations within the validated range: 5-100 ng/mL for bisoprolol and amlodipine, 0.1-5 ng/mL for telmisartan, and 10-200 ng/mL for atorvastatin [6]
- Maintain consistent sample preparation across all robustness experiments
Step 4: Experimental Execution
- Follow the experimental design matrix (Table 2), adjusting parameters as specified for each run
- For each experimental condition, inject the quality control sample in triplicate
- Maintain all other method parameters at their nominal values unless specifically being tested
Step 5: Data Collection
- For each chromatographic run, record the following system suitability parameters:
- Retention times of all analytes
- Peak area and symmetry
- Resolution between critical pairs
- Theoretical plates
- Document any observations regarding baseline noise or unusual peak shapes
Data Analysis and Interpretation
Calculation of Factor Effects
The effect of each parameter variation on the chromatographic responses is calculated as the difference between the average results at the high level and the average results at the low level for each factor [61]. For a factor X, the effect (Ex) on response Y is calculated as:
Ex = Ȳ(high) - Ȳ(low)
Where:
- Ȳ(high) is the average of all results when factor X was at its high level
- Ȳ(low) is the average of all results when factor X was at its low level
The following diagram illustrates the decision-making process for interpreting robustness results:
Acceptance Criteria and Method Evaluation
For the cardiovascular drug analysis method, the following acceptance criteria should be applied when evaluating robustness:
Table 4: Acceptance Criteria for Robustness Evaluation of Cardiovascular Drug Analysis
| Response Parameter | Acceptance Criterion | Critical Impact |
|---|---|---|
| Retention Time | RSD ≤ 2% across variations | Ensures consistent identification |
| Peak Area | RSD ≤ 2% across variations | Maintains quantification accuracy |
| Resolution | ≥ 2.0 between critical pairs | Prevents co-elution |
| Theoretical Plates | ≥ 2000 for all analytes | Maintains separation efficiency |
| Tailing Factor | ≤ 2.0 for all analytes | Ensures peak shape integrity |
A method is considered robust when none of the deliberate parameter variations cause the system suitability parameters to fall outside these acceptance criteria [61] [63]. If significant effects are observed, the method protocol should specify tighter control limits for the problematic parameter or include appropriate precautions in the method documentation.
Case Study: Application to Cardiovascular Drug Method
In the development of an HPLC method for simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin in human plasma, robustness testing was implemented using the described protocol [6]. The nominal method conditions employed were:
- Column: Thermo Hypersil BDS C18 (150 × 4.6 mm, 5.0 μm)
- Mobile phase: Ethanol:0.03 M potassium phosphate buffer, pH 5.2 (40:60, v/v)
- Flow rate: 0.6 mL/min
- Temperature: Ambient (25-35°C)
- Detection: Fluorescence with specific λex/λem for each drug
When robustness testing was applied to this method, results demonstrated that the separation remained unaffected by variations of ±0.1 units in pH, ±10% in flow rate, and ±5°C in temperature [6]. This confirmed the method's suitability for transfer to quality control laboratories and for routine therapeutic drug monitoring applications.
The resolution between critical pairs, particularly between bisoprolol and its potential metabolites, was maintained above 2.0 throughout the robustness testing, ensuring accurate quantification of each drug in the complex plasma matrix. The retention times for all four drugs showed minimal variation (RSD < 1%), supporting the method's reliability for peak identification in clinical samples.
Robustness testing through intentional variation of flow rate, temperature, and pH provides essential validation of an HPLC method's reliability for the simultaneous determination of cardiovascular drugs in plasma. The structured experimental design and detailed protocol presented in this application note offer a systematic approach to establishing operational ranges for critical method parameters.
For the specific analysis of cardiovascular drugs in biological matrices, demonstrating robustness ensures that the method will perform consistently across different instruments, operators, and laboratories—a fundamental requirement for generating reliable data in pharmaceutical research and therapeutic drug monitoring. The documented robustness profile further strengthens the method's regulatory submission package and facilitates its successful implementation in routine clinical practice.
The pharmaceutical industry faces increasing pressure to align analytical practices with the principles of green chemistry. Micellar Liquid Chromatography (MLC) has emerged as a powerful, sustainable alternative to conventional Reversed-Phase High-Performance Liquid Chromatography (RP-HPLC), particularly for complex applications like the simultaneous determination of cardiovascular drugs in plasma [66]. This technique utilizes mobile phases containing surfactants at concentrations above the critical micellar concentration (cmc), forming micelles that act as a distinct separation medium [67]. The most significant green advantage of MLC is its drastic reduction in the consumption of toxic organic solvents, such as acetonitrile and methanol, which are used in high volumes in traditional HPLC [68] [66]. Furthermore, the unique properties of micellar solutions enable the direct injection of physiological fluids like plasma, bypassing extensive sample pre-treatment procedures and further minimizing solvent use and waste generation [67]. This application note details the practical implementation of MLC for analyzing cardiovascular drugs in plasma, providing a comprehensive protocol to achieve high-performance, reproducible results while adhering to green chemistry principles.
Micellar Liquid Chromatography Fundamentals
Principles and Green Chemistry Advantages
In MLC, the stationary phase is typically a conventional C18 column, while the mobile phase is an aqueous solution of a surfactant. Above a specific concentration (the cmc), surfactant molecules aggregate to form micelles—spherical structures with a hydrophobic interior and a hydrophilic exterior [66]. These micelles, along with surfactant monomers adsorbed onto the stationary phase, create a biphasic partitioning system for analytes. Separation is achieved based on the differential partitioning of solutes between the bulk aqueous mobile phase, the micellar pseudophase, and the stationary phase [67].
The green chemistry advantages of MLC are substantial:
- Reduced Organic Solvent Consumption: Hybrid micellar mobile phases often require only a small percentage (e.g., 3-10%) of a short-chain alcohol like propanol or butanol, significantly reducing toxicity and waste compared to the high organic solvent content (often 40-90%) in conventional RP-HPLC [66] [67].
- Waste Minimization and Safety: The low volatility of micellar mobile phases reduces inhalation risks and evaporation losses. These mobile phases are stable and can be stored for extended periods without composition changes [67].
- Direct Plasma Injection: Micelles can solubilize proteins and other matrix components, allowing plasma samples to be injected directly after a simple pretreatment like dilution or protein precipitation, eliminating the need for large volumes of solvents used in traditional liquid-liquid extraction [67].
Separation Mechanism and Workflow
The following diagram illustrates the core separation mechanism and experimental workflow of MLC for plasma analysis.
Experimental Protocol: MLC for Cardiovascular Drugs in Plasma
This protocol is adapted from validated methods for the simultaneous analysis of cardiovascular drugs, such as those reported for amlodipine, bisoprolol, and valsartan [7] [6].
Materials and Reagent Solutions
Table 1: Key Research Reagent Solutions for MLC
| Reagent/Solution | Function/Description | Example & Notes |
|---|---|---|
| Surfactant (SDS) | Forms micelles; primary component of the mobile phase. | Sodium Dodecyl Sulfate (SDS), 0.05-0.15 M. Most common anionic surfactant for MLC [67]. |
| Organic Modifier | Fine-tunes retention and efficiency in hybrid mobile phase. | 1-Propanol or 2-Propanol, 3-10% (v/v). Reduces analysis time and improves peak shape [67]. |
| Aqueous Buffer | Maintains pH stability for reproducible separations. | 50 mM Borate (pH ~9) or Phosphate (pH ~3-7). Choice depends on analyte stability and pKa [7] [67]. |
| Protein Precipitant | For simple plasma sample pretreatment prior to direct injection. | Ethanol or Acetonitrile. Used to precipitate plasma proteins; supernatant is injected [6]. |
| Stock Standard Solutions | For preparation of calibration standards in drug-free plasma. | 100 µg/mL of each cardiovascular drug in ethanol or methanol. Stable for weeks at 2-8°C [6]. |
Mobile Phase Preparation
- Background Electrolyte: Dissolve the appropriate mass of surfactant (e.g., SDS) and buffer salts (e.g., sodium phosphate) in approximately 70% of the final volume of deionized water. For a 1 L solution of 0.10 M SDS in 50 mM phosphate buffer, dissolve 28.8 g of SDS and 7.1 g of Na₂HPO₄ in 700 mL water [7] [69].
- pH Adjustment: Adjust the pH to the desired value (e.g., pH 3 for phosphate buffer) using a concentrated acid (e.g., H₃PO₄) or base (e.g., NaOH).
- Organic Modifier Addition: Add the required volume of organic solvent (e.g., 50 mL of 1-propanol for a 5% v/v solution).
- Final Volume and Filtration: Make up to the final volume (1 L) with deionized water. Filter the entire mobile phase through a 0.45 µm cellulose acetate membrane and degas by sonication before use [67].
Column Conditioning and Equilibration
- Initial Solvent Replacement: Flush the C18 column (e.g., ZORBAX Extend-C18, 4.6 × 250 mm, 5 µm) with 100% water at a low flow rate (≤0.5 mL/min) for at least 30 column volumes to remove any storage solvent (e.g., methanol) [67].
- Surfactant Coating: Switch to the prepared micellar mobile phase. Condition the column for at least 1 hour at the operational flow rate (e.g., 1.0 mL/min) to establish a stable layer of adsorbed surfactant monomers on the stationary phase. Monitor the system pressure and baseline until stable [67].
- Use of Saturator Column: To protect the analytical column from silica dissolution at neutral to basic pH, a silica saturator column can be installed between the pump and the injector [67].
Plasma Sample Preparation
- Protein Precipitation: Pipette 200 µL of plasma sample into a microcentrifuge tube. Add 600 µL of a precipitating solvent like ethanol [6].
- Vortex and Centrifuge: Vortex the mixture vigorously for 1 minute, then centrifuge at 10,000 rpm for 5 minutes to pellet the precipitated proteins.
- Supernatant Collection: Carefully collect the clear supernatant. It can be diluted with the mobile phase if necessary and then directly injected into the MLC system [67].
Application in Cardiovascular Drug Analysis
Experimental Design and Method Parameters
The robustness of MLC is demonstrated by its application in the simultaneous analysis of complex mixtures of cardiovascular drugs and a nutraceutical in a single run, as shown in recent studies [7]. The table below summarizes key parameters from a validated method.
Table 2: MLC Method for Simultaneous Determination of Cardiovascular Drugs [7]
| Parameter | Specification | Experimental Details |
|---|---|---|
| Analytes | 8 Cardiovascular Drugs + Nutraceutical | Hydrochlorothiazide, Captopril, Lisinopril, Valsartan, Atorvastatin, Bisoprolol, Amlodipine, Carvedilol, Vincamine. |
| Column | C18 | Fused silica capillary (41.5 cm × 50 µm id) or ZORBAX Extend-C18 (4.6 × 250 mm, 5 µm). |
| Mobile Phase | Micellar Solution | 50 mM borate buffer (pH 9) containing 50 mM SDS and 10% Acetonitrile. |
| Flow Rate | - | Optimized for the column dimensions (e.g., 1.0 mL/min for 4.6 mm ID column). |
| Detection | DAD | UV detection at multiple wavelengths optimized for each drug. |
| Linearity | r ≥ 0.9996 | Demonstrated over the therapeutic range for each drug. |
| Application | Plasma & Dosage Forms | Successfully applied to spiked rat plasma and commercial dosage forms. |
Method Validation and Greenness Assessment
The developed MLC methods for cardiovascular drugs have been rigorously validated according to international guidelines [7] [6]. Key validation parameters include:
- Linearity, LOD, and LOQ: Methods show excellent linearity (correlation coefficients, r ≥ 0.9996) with low limits of detection (LOD) and quantification (LOQ), suitable for quantifying drugs in plasma [7].
- Accuracy and Precision: Recovery rates from spiked plasma samples confirm accuracy, while low relative standard deviation (RSD) values attest to the high precision of the methods [7] [6].
- Green Metrics: The methods were evaluated using green (ecological impact), white (practical efficiency), and blue (safety) metrics. The significant reduction in organic solvent use and waste production directly contributes to a high greenness score [7].
Micellar Liquid Chromatography presents a viable, eco-friendly pathway for the simultaneous determination of cardiovascular drugs in complex matrices like plasma. By significantly reducing the reliance on hazardous organic solvents and simplifying sample preparation through direct injection, MLC aligns analytical practices with the urgent principles of green chemistry without compromising analytical performance. The detailed protocols and case studies provided herein offer researchers a clear framework to adopt this sustainable technology, promoting greener and more cost-effective quality control and bioanalytical processes in drug development.
Ensuring Reliability: Method Validation, Comparison, and Regulatory Compliance
Comprehensive Validation per ICH, FDA, and EMA Guidelines
The development and validation of bioanalytical methods, such as the HPLC analysis of cardiovascular drugs in human plasma, is a critical activity in pharmaceutical research and development. It provides the essential data required for pre-clinical and clinical studies, ensuring that drug concentrations can be accurately and reliably measured. In a regulated environment, this process is not a one-time event but a lifecycle that integrates product and process development, validation of the commercial manufacturing process, and maintenance of the process in a state of control during routine commercial production [70]. Regulatory bodies including the International Council for Harmonisation (ICH), the US Food and Drug Administration (FDA), and the European Medicines Agency (EMA) have converged on a science- and risk-based lifecycle model for validation, underpinned by the principles of Quality Risk Management (QRM) [70]. This application note provides a detailed protocol for the comprehensive validation of an HPLC method for the simultaneous determination of cardiovascular drugs in human plasma, framed within the specific requirements of ICH, FDA, and EMA guidelines.
Experimental Protocol: Method Development and Validation
Chromatographic Conditions and Instrumentation
This protocol is adapted from a validated method for the concurrent determination of bisoprolol (BIS), amlodipine besylate (AML), telmisartan (TEL), and atorvastatin (ATV) in human plasma [6].
- Instrumentation: A Waters Alliance 2695 HPLC system or equivalent, equipped with a quaternary pump, an auto-sampler, a column oven, and a dual-detection system (Photodiode Array Detector and Multi-Wavelength Fluorescence Detector) is used [6].
- Chromatographic Column: Thermo Hypersil BDS C18 column (150 mm × 4.6 mm, 5 μm) or equivalent [6].
- Mobile Phase: Isocratic elution with a mixture of ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in a ratio of 40:60 (v/v) [6].
- Flow Rate: 0.6 mL/min [6].
- Injection Volume: 20 µL [6].
- Column Temperature: Maintained between 25–35 °C [6].
- Detection:
- UV Detection: Used to confirm separation, with monitoring at 240 nm [6].
- Fluorescence Detection: For enhanced sensitivity and specificity [6].
- BIS: Excitation 227 nm / Emission 298 nm
- TEL: Excitation 294 nm / Emission 365 nm
- ATV: Excitation 274 nm / Emission 378 nm
- AML: Excitation 361 nm / Emission 442 nm
Sample Preparation: Liquid-Liquid Extraction
The following liquid-liquid extraction (LLE) procedure shall be followed [6]:
- To a 200 µL aliquot of human plasma, add 50 µL of the working standard solution and 600 µL of absolute ethanol.
- Vortex the mixture and centrifuge for 2 minutes to precipitate proteins.
- Perform the first extraction by adding 1.0 mL of diethyl ether. Vortex for 5 minutes and centrifuge at 3500 rpm for 5 minutes at 0°C.
- Carefully transfer the organic layer to a clean test tube.
- Perform the second extraction on the remaining aqueous layer by adding 0.5 mL of dichloromethane. Vortex for 5 minutes and centrifuge at 3500 rpm for 5 minutes at 0°C.
- Combine the organic layer from this second extraction with the first.
- Evaporate the combined organic extracts to dryness under a gentle stream of nitrogen at 40°C.
- Reconstitute the dry residue with 500 µL of ethanol, vortex for 2 minutes, and inject 20 µL into the HPLC system.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 1: Essential materials and reagents for HPLC method development and validation.
| Item | Function / Role in the Analysis |
|---|---|
| Thermo Hypersil BDS C18 Column | A robust reversed-phase column providing the hydrophobic surface for separation of analytes. |
| Potassium Dihydrogen Phosphate | Used to prepare the aqueous buffer component of the mobile phase, helping to control pH and ionic strength. |
| Ethanol (HPLC Grade) | Serves as the organic modifier in the mobile phase and as the reconstitution solvent. |
| Diethyl Ether & Dichloromethane | Organic solvents used in the liquid-liquid extraction process to isolate analytes from the plasma matrix. |
| Drug Reference Standards | High-purity compounds used for preparing calibration standards and quality control samples. |
Comprehensive Validation Parameters and Acceptance Criteria
The method must be validated according to ICH guidelines [71]. The following parameters and acceptance criteria shall be demonstrated.
Validation Parameters Protocol
1. Selectivity/Specificity
- Protocol: Analyze at least six independent sources of blank human plasma. Compare chromatograms of blank plasma, plasma spiked with the analytes at the Lower Limit of Quantification (LLOQ), and plasma from dosed subjects.
- Acceptance Criteria: There should be no significant interference (response < 20% of the LLOQ for analytes and < 5% for internal standards) at the retention times of the analytes and internal standards from the blank matrix [71].
2. Linearity and Range
- Protocol: Prepare and analyze a minimum of six non-zero calibration standards across the expected range, plus a blank and a zero sample. The calibration curve is constructed using a linear regression model, plotting peak area versus concentration.
- Acceptance Criteria: The coefficient of determination (r²) should be ≥ 0.99 [7]. The back-calculated concentrations of the standards should be within ±15% of the nominal value (±20% at the LLOQ) [71].
3. Accuracy and Precision
- Protocol: Assess using Quality Control (QC) samples at a minimum of four concentration levels (LLOQ, Low, Medium, and High), with at least six replicates at each level. Accuracy is measured as percent recovery. Precision is expressed as the relative standard deviation (%RSD).
- Acceptance Criteria:
- Accuracy: Mean values should be within ±15% of the nominal value (±20% at the LLOQ).
- Precision: The %RSD should not exceed 15% (20% at the LLOQ) [71].
4. Limit of Detection (LOD) and Lower Limit of Quantification (LLOQ)
- Protocol: The LOD and LLOQ can be determined based on the signal-to-noise ratio (S/N).
- Acceptance Criteria:
- LOD: Typically, an S/N of 3:1.
- LLOQ: Typically, an S/N of 10:1, with demonstrated precision and accuracy as defined above [71].
5. Robustness
- Protocol: Deliberately introduce small, deliberate variations in method parameters (e.g., mobile phase pH ±0.2 units, organic composition ±2%, column temperature ±2°C, flow rate ±10%).
- Acceptance Criteria: The method should maintain system suitability criteria (e.g., resolution, tailing factor) and the quantitative results for QC samples should remain within acceptable limits [71].
Table 2: Example validation data and regulatory ranges for cardiovascular drugs in plasma.
| Analyte | Linear Range (ng/mL) | LLOQ (ng/mL) | Accuracy (% Recovery) | Precision (% RSD) |
|---|---|---|---|---|
| Bisoprolol (BIS) | 5 - 100 [6] | 5 [6] | 85-115% [71] | ≤15% [71] |
| Amlodipine (AML) | 5 - 100 [6] | 5 [6] | 85-115% [71] | ≤15% [71] |
| Telmisartan (TEL) | 0.1 - 5 [6] | 0.1 [6] | 85-115% [71] | ≤15% [71] |
| Atorvastatin (ATV) | 10 - 200 [6] | 10 [6] | 85-115% [71] | ≤15% [71] |
The Validation Lifecycle: Alignment with FDA and EMA
The modern validation paradigm is structured around a three-stage lifecycle: Process Design, Process Qualification, and Continued Process Verification [70]. While originally framed for process validation, this lifecycle model is conceptually applicable to the analytical method validation lifecycle.
Stage 1: Method Design This stage corresponds to the activities described in the experimental protocol. The goal is to design a method suitable for routine use that can consistently deliver reliable results. This is achieved through systematic development, leveraging scientific tools and risk analysis to understand the relationship between method parameters (e.g., mobile phase composition, column temperature) and performance outputs (e.g., resolution, peak shape) [70]. The outcome is a formal analytical procedure and a control strategy.
Stage 2: Method Qualification This is the formal validation exercise described in Section 3. It serves as the bridge between method development and routine use, confirming that the method design is capable of reproducible operation [70]. The FDA's framework is highly structured around a robust Process Performance Qualification (PPQ) concept, which in an analytical context translates to the execution of a pre-defined validation protocol [70]. The EMA guideline is more flexible, allowing for different validation approaches (e.g., traditional, continuous verification) based on the level of process understanding and risk [70]. A successful qualification is a prerequisite for using the method to generate data for regulatory submissions.
Stage 3: Continued Method Verification The final stage ensures the method remains in a state of control throughout its operational life. This requires an "ongoing program to collect and analyze product and process data that relate to product quality" [70]. In practice, this means:
- System Suitability Tests (SST): Performed before each analytical run to ensure the system is working adequately.
- Monitoring Control Samples: The analysis of QC samples with each batch of unknowns to verify the continued accuracy and precision of the method.
- Trending Data: Regular review of SST results, QC data, and calibration curve performance to identify any potential drift or loss of control.
This application note provides a structured protocol for the development and comprehensive validation of an HPLC method for the analysis of cardiovascular drugs in human plasma, fully aligned with ICH, FDA, and EMA regulatory expectations. By adopting a science-based, lifecycle approach—from robust method design and formal qualification to ongoing verification—researchers and drug development professionals can ensure the generation of reliable, high-quality data essential for supporting pre-clinical and clinical studies. The detailed experimental protocols and validation parameters outlined herein serve as a practical guide for implementing a globally harmonized validation strategy.
Establishing Linearity, Accuracy, Precision, and Selectivity
In the development of bioanalytical high-performance liquid chromatography (HPLC) methods for the simultaneous determination of cardiovascular drugs in human plasma, the demonstration of method validity is paramount. For researchers and drug development professionals, establishing key validation parameters—linearity, accuracy, precision, and selectivity—provides the foundational assurance that analytical methods will generate reliable and reproducible data for pharmacokinetic studies and therapeutic drug monitoring [6]. This framework is particularly critical for cardiovascular disease management, where polypharmacy is common and therapeutic drug monitoring can optimize treatment outcomes [30].
The International Council for Harmonisation (ICH) guidelines provide the primary framework for method validation, requiring rigorous assessment of these parameters to ensure methods are fit for their intended purpose in regulated environments [6] [72]. This application note delineates detailed protocols and contemporary case studies for establishing these critical validation parameters, with specific application to the simultaneous quantification of cardiovascular drugs in human plasma.
Theoretical Foundations and Regulatory Framework
Definitions and Acceptance Criteria
Linearity refers to the ability of the method to obtain test results that are directly proportional to the concentration of the analyte within a given range [72]. For cardiovascular drug monitoring, linearity must be established across the expected physiological concentration range, including the maximum plasma concentration (Cmax) [30].
Accuracy expresses the closeness of agreement between the value found and the value accepted as a true or reference value. In bioanalytical method validation, accuracy should be within ±15% of the nominal concentration for quality control samples, with ±20% acceptable at the lower limit of quantification [30].
Precision describes the closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample under prescribed conditions. It is typically evaluated at three levels: repeatability (intra-day), intermediate precision (inter-day), and reproducibility [72].
Selectivity is the ability of the method to measure the analyte response in the presence of potential interferents such as metabolites, concomitant medications, and matrix components [6]. For plasma analysis, selectivity must be demonstrated by analyzing blank plasma from at least six different sources [30].
Relevant Guidelines and Frameworks
Analytical methods used in pharmaceutical quality control must be developed using protocols set out in ICH guidelines (Q2(R2)) [72]. For bioanalytical methods specifically, the FDA Guidance for Industry on Bioanalytical Method Validation provides additional requirements for methods used in pharmacokinetic and bioequivalence studies [30]. The United States Pharmacopeia (USP) General Chapter <621> on Chromatography provides specific system suitability requirements that must be met during routine analysis to ensure method validity [73].
Experimental Protocols
Establishing Linearity
Protocol for Calibration Curve Construction:
- Preparation of Standard Solutions: Prepare stock solutions of reference standards at approximately 100 µg/mL in appropriate solvent [6]. For the simultaneous determination of four cardiovascular drugs, prepare individual stock solutions then combine as needed.
- Calibration Standards: Prepare a minimum of six non-zero calibration standards covering the expected concentration range. For example:
- Bisoprolol: 5–100 ng/mL
- Amlodipine: 5–100 ng/mL
- Telmisartan: 0.1–5 ng/mL
- Atorvastatin: 10–200 ng/mL [6]
- Sample Processing: Process calibration standards using the same extraction procedure as unknown samples (detailed in Section 3.4).
- Analysis and Calculation: Analyze calibration standards in triplicate. Plot peak area (or peak area ratio to internal standard) versus nominal concentration. Perform regression analysis using least-squares method. The correlation coefficient (r²) should be ≥0.99 [30].
- Back-Calculation: Calculate concentrations from the calibration curve. The mean accuracy should be within 85-115% for all standards except the LLOQ, which should be within 80-120% [30].
Establishing Accuracy and Precision
Protocol for Quality Control (QC) Sample Analysis:
- QC Sample Preparation: Prepare QC samples at a minimum of three concentrations (low, medium, high) covering the calibration range [30]. For example:
- Low QC: 3x the lower limit of quantification (LLOQ)
- Medium QC: Near the mid-point of the calibration curve
- High QC: 75-85% of the upper limit of quantification
- Intra-Day Precision and Accuracy (Repeatability): Analyze six replicates of each QC concentration within the same analytical run. Calculate mean concentration, standard deviation (SD), and percent relative standard deviation (%RSD). Accuracy should be within ±15% of nominal, precision should not exceed 15% RSD [30].
- Inter-Day Precision and Accuracy (Intermediate Precision): Analyze six replicates of each QC concentration over three different days or with different analysts/instruments. Calculate overall mean, SD, and %RSD. Acceptance criteria are the same as for intra-day evaluation [6].
Table 1: Accuracy and Precision Acceptance Criteria for QC Samples
| Validation Parameter | Acceptance Criterion | Application in Cardiovascular Drug Analysis |
|---|---|---|
| Accuracy | ±15% of nominal value | Applied to bisoprolol, amlodipine, telmisartan, atorvastatin in plasma [6] |
| Precision (RSD) | ≤15% | Demonstrated for felodipine and metoprolol in spiked human plasma [30] |
| LLOQ Accuracy | ±20% of nominal value | Critical for low concentration telmisartan quantification (0.1-5 ng/mL) [6] |
| LLOQ Precision | ≤20% | Essential for sensitivity requirements in pharmacokinetic studies [30] |
Establishing Selectivity
Protocol for Specificity and Selectivity Assessment:
- Blank Matrix Screening: Analyze blank human plasma samples from at least six different sources to demonstrate the absence of interfering peaks at the retention times of the target analytes and internal standard [30].
- Interference Check: Spiked blank samples with commonly co-administered cardiovascular medications to demonstrate no interference with analyte quantification.
- Matrix Effect Evaluation: Prepare post-extraction spiked samples at low and high QC concentrations from six different plasma lots. Compare the peak areas with neat standards at the same concentrations. The matrix factor should be consistent across different lots (RSD <15%) [6].
- Hemolyzed and Lipemic Plasma: Include at least one hemolyzed and one lipemic plasma sample to evaluate potential matrix effects.
Sample Preparation and Chromatography
Liquid-Liquid Extraction Protocol for Cardiovascular Drugs in Plasma:
- Sample Volume: Transfer 200 µL of plasma into a clean test tube.
- Protein Precipitation: Add 600 µL of absolute ethanol and 50 µL of working standard solution. Vortex mix, then centrifuge for 2 minutes to remove proteins [6].
- First Extraction: Add 1.0 mL of diethyl ether (first extraction solvent). Vortex for 5 minutes, then centrifuge at 3500 rpm for 5 minutes at 0°C. Transfer the organic phase to a clean test tube [6].
- Second Extraction: Add 0.5 mL of dichloromethane (second extraction solvent) to the remaining aqueous layer. Vortex for 5 minutes, then centrifuge at 3500 rpm for 5 minutes at 0°C. Combine this organic layer with the first extract [6].
- Evaporation and Reconstitution: Evaporate the combined organic layers under a gentle stream of nitrogen at 40°C. Reconstitute the residue in 500 µL of ethanol, vortex for 2 minutes, and inject 20 µL into the HPLC system [6].
Chromatographic Conditions for Simultaneous Analysis:
- Column: Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 µm) or equivalent [6]
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in ratio of 40:60 [6]
- Flow Rate: 0.6 mL/min in isocratic mode [6]
- Detection: Fluorescence detection with specific wavelengths for each drug:
- Bisoprolol: 227/298 nm (excitation/emission)
- Telmisartan: 294/365 nm
- Atorvastatin: 274/378 nm
- Amlodipine: 361/442 nm [6]
Case Studies and Data Presentation
Case Study: Simultaneous Determination of Four Cardiovascular Drugs
A recent study demonstrated the simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin in human plasma. The method was validated according to ICH guidelines with the following results [6]:
Table 2: Linearity Data for Cardiovascular Drugs in Human Plasma
| Analyte | Linear Range (ng/mL) | Correlation Coefficient (r²) | Lower Limit of Quantification (ng/mL) |
|---|---|---|---|
| Bisoprolol | 5–100 | >0.999 | 5 |
| Amlodipine | 5–100 | >0.999 | 5 |
| Telmisartan | 0.1–5 | >0.999 | 0.1 |
| Atorvastatin | 10–200 | >0.999 | 10 |
The accuracy and precision data demonstrated the method's reliability across the calibration range, with intra-day and inter-day precision ≤2% for all analytes in their pure forms and within acceptable limits in human plasma [6].
Case Study: Eco-Friendly Method for Felodipine and Metoprolol
A 2025 study developed and validated an eco-friendly RP-HPLC method with fluorescence detection for simultaneous determination of felodipine and metoprolol in spiked human plasma. Validation followed ICH Q2(R2) and FDA bioanalytical guidelines [30]:
Table 3: Precision and Accuracy Data for Felodipine and Metoprolol in Human Plasma
| Analyte | Concentration Level | Intra-Day Precision (%RSD) | Inter-Day Precision (%RSD) | Accuracy (% of Nominal) |
|---|---|---|---|---|
| Felodipine | Low (0.03 µg/mL) | ≤2% | ≤2% | Within ±10% |
| Medium (0.50 µg/mL) | ≤2% | ≤2% | Within ±10% | |
| High (0.90 µg/mL) | ≤2% | ≤2% | Within ±10% | |
| Metoprolol | Low (0.003 µg/mL) | ≤2% | ≤2% | Within ±10% |
| Medium (0.50 µg/mL) | ≤2% | ≤2% | Within ±10% | |
| High (0.90 µg/mL) | ≤2% | ≤2% | Within ±10% |
The method demonstrated excellent linearity over 0.01–1.00 µg/mL for felodipine and 0.003–1.00 µg/mL for metoprolol, with correlation coefficients of 0.9998 and 0.9999, respectively [30].
The Scientist's Toolkit
Table 4: Essential Research Reagents and Materials for HPLC Method Validation
| Item | Function/Application | Example from Literature |
|---|---|---|
| HPLC-Grade Solvents | Mobile phase preparation; minimizes UV background noise and system contamination | Ethanol, methanol, acetonitrile, potassium dihydrogen phosphate [6] [30] |
| Reference Standards | Calibration and quantification; certified purity ensures accurate results | USP reference standards; drugs with certified purity (99.24-99.78%) [6] |
| Sample Preparation | Extraction and clean-up; critical for removing matrix interferents from plasma | Diethyl ether, dichloromethane for liquid-liquid extraction [6] |
| Biological Matrix | Method development and validation; should represent study samples | Blank human plasma from multiple donors (≥6) [30] |
| HPLC Column | Stationary phase for chromatographic separation | Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 µm) [6] |
| Internal Standard | Correction for extraction and injection variability | Tadalafil as internal standard for felodipine and metoprolol analysis [30] |
Workflow and Method Validation Diagrams
Diagram 1: Method validation workflow for HPLC analysis of cardiovascular drugs in plasma
Diagram 2: Sample preparation workflow for plasma sample analysis
The establishment of linearity, accuracy, precision, and selectivity forms the cornerstone of any validated HPLC method for the simultaneous determination of cardiovascular drugs in human plasma. The protocols outlined in this application note, supported by contemporary case studies, provide researchers with a robust framework for developing methods that meet regulatory requirements and generate scientifically sound data. As cardiovascular drug therapy increasingly involves complex regimens and fixed-dose combinations, the ability to reliably monitor multiple drugs simultaneously becomes ever more critical for optimizing patient outcomes through therapeutic drug monitoring and pharmacokinetic studies.
Stability assessment is a critical component of bioanalytical method validation in pharmaceutical research, ensuring the reliability of analytical results throughout a method's lifecycle. For the simultaneous determination of cardiovascular drugs in plasma using High-Performance Liquid Chromatography (HPLC), comprehensive stability evaluation under various conditions is mandatory to demonstrate method robustness and data integrity. This protocol outlines standardized procedures for assessing bench-top, freeze-thaw, and long-term stability specifically tailored for cardiovascular drug analysis in biological matrices, framed within the context of developing a robust HPLC method for simultaneous quantification of commonly prescribed cardiovascular medications including bisoprolol, amlodipine, telmisartan, and atorvastatin [6].
The stability of analytes during sample collection, processing, storage, and analysis directly impacts the accuracy and reliability of pharmacokinetic and bioequivalence studies. Factors such as temperature, time, sample handling procedures, and storage conditions can significantly influence analyte stability, potentially leading to degradation that compromises data quality. This document provides detailed methodologies for evaluating stability under conditions that mimic actual sample handling scenarios in clinical and preclinical studies, with particular emphasis on cardiovascular drugs which are frequently co-administered to patients with hypertension and other cardiovascular conditions [6] [74].
Theoretical Foundations of Stability Assessment
Stability testing in bioanalytical method validation is governed by the principles of chemical kinetics and degradation pathways. Understanding the potential degradation mechanisms of cardiovascular drugs is essential for designing appropriate stability assessments. The cardiovascular drugs highlighted in this protocol – bisoprolol (beta-blocker), amlodipine (calcium channel blocker), telmisartan (angiotensin receptor blocker), and atorvastatin (statin) – each possess distinct chemical functionalities that may be susceptible to different degradation pathways including hydrolysis, oxidation, and photodegradation [6].
The International Council for Harmonisation (ICH) guidelines provide the framework for stability testing, requiring demonstration that analyte stability is maintained under specific conditions relevant to sample handling, processing, and storage. The matrix effect – the influence of sample components on the detection of analytes – must also be considered throughout stability evaluation, as degradation of matrix components over time may indirectly affect analyte stability or detection [6].
Freeze-thaw stability is particularly crucial for cardiovascular drug analysis as clinical samples often undergo multiple freezing and thawing cycles during analytical processing. The formation of ice crystals during freezing and the subsequent concentration of solutes in the remaining liquid phase can accelerate degradation reactions. Similarly, long-term stability must demonstrate that samples remain stable throughout their intended storage period, which for clinical trial samples may extend for several years [75] [76].
Materials and Reagents
Research Reagent Solutions
Table 1: Essential Materials and Reagents for Stability Assessment
| Item | Function | Specifications/Notes |
|---|---|---|
| HPLC System with Fluorescence Detector | Separation and detection of analytes | Waters Alliance 2695 system or equivalent; FLD with variable wavelength settings [6] |
| C18 Reverse-Phase Column | Chromatographic separation | Thermo Hypersil BDS C18 (150 × 4.6 mm, 5.0 μm) or equivalent [6] |
| Centrifuge | Sample preparation | Capable of 3500-6000 rpm; temperature control (0-4°C) [6] |
| pH Meter | Buffer preparation | Accurate to ±0.01 pH units [6] |
| Rotary Evaporator or Nitrogen Evaporator | Sample concentration | Temperature control (40°C) [6] |
| Ethanol, HPLC Grade | Protein precipitation and mobile phase | 600 μL used for protein precipitation [6] |
| Diethyl Ether | Liquid-liquid extraction | First extraction solvent (1.0 mL) [6] |
| Dichloromethane | Liquid-liquid extraction | Second extraction solvent (0.5 mL) [6] |
| Potassium Dihydrogen Phosphate | Mobile phase buffer | 0.03 M, pH adjusted to 5.2 [6] |
| Human Plasma | Biological matrix | Typically sourced from approved vendors; should be screened for interference [6] |
Experimental Design and Workflow
The stability assessment follows a systematic workflow from study design through data analysis to ensure comprehensive evaluation of all critical parameters.
Figure 1: Experimental Workflow for Comprehensive Stability Assessment
Quality Control Sample Preparation
For all stability experiments, prepare quality control (QC) samples at three concentrations (low, medium, and high) by spiking blank human plasma with working standard solutions of the cardiovascular drugs of interest. For the cardiovascular drug panel including bisoprolol, amlodipine, telmisartan, and atorvastatin, appropriate concentration ranges would be: 5-100 ng/mL for bisoprolol and amlodipine, 0.1-5 ng/mL for telmisartan, and 10-200 ng/mL for atorvastatin, based on reported therapeutic ranges [6]. Prepare a sufficient volume of QC samples to allow for all planned stability tests and divide into appropriate aliquots to avoid repeated freeze-thaw cycles of the same sample.
Detailed Experimental Protocols
Bench-Top Stability Protocol
5.1.1 Purpose: To evaluate the stability of analytes in plasma under typical laboratory handling conditions at room temperature.
5.1.2 Procedure:
- Prepare six aliquots of each QC concentration (low, medium, high).
- Keep three aliquots of each concentration at room temperature (approximately 25°C) for 4 hours and the other three aliquots for 24 hours.
- Process the samples alongside freshly prepared QC samples (time zero) using the validated sample extraction procedure.
- Analyze all samples in a single batch to minimize analytical variability.
- Calculate the percentage deviation of the stability samples from the fresh QC samples.
5.1.3 Acceptance Criteria: The mean concentration of stability samples should be within ±15% of the nominal concentration, with precision not exceeding 15% relative standard deviation (RSD).
Freeze-Thaw Stability Protocol
5.2.1 Purpose: To assess analyte stability after multiple freeze-thaw cycles that may occur during routine analysis of clinical samples.
5.2.2 Procedure:
- Prepare nine aliquots of each QC concentration (low, medium, high).
- Subject the aliquots to three complete freeze-thaw cycles as follows:
- First freeze: Store at -20°C or -40°C for a minimum of 12 hours.
- First thaw: Thaw completely at room temperature (approximately 2 hours).
- Second freeze: Return to -20°C or -40°C for 12-24 hours.
- Repeat the process for three complete cycles.
- After the third cycle, process the samples alongside freshly thawed QC samples (control).
- Analyze all samples in a single batch.
- Compare the results with control samples to determine the effect of freeze-thaw cycles.
5.2.3 Acceptance Criteria: The mean concentration after three freeze-thaw cycles should be within ±15% of the nominal concentration, with precision not exceeding 15% RSD.
Long-Term Stability Protocol
5.3.1 Purpose: To demonstrate analyte stability in matrix during storage at the intended storage temperature for the entire duration that study samples will be stored.
5.3.2 Procedure:
- Prepare multiple aliquots of each QC concentration (low, medium, high).
- Store the aliquots at the intended storage temperature (typically -20°C or -40°C).
- Remove and analyze three aliquots of each concentration at predetermined time points (e.g., 1, 3, 6, 9, and 12 months).
- At each time point, analyze the stability samples alongside freshly prepared QC samples.
- Record the concentration values and compare with time zero results.
5.3.3 Acceptance Criteria: The mean concentration at each time point should be within ±15% of the nominal concentration, with precision not exceeding 15% RSD.
Sample Processing Procedure
For the extraction of cardiovascular drugs from plasma, employ the following liquid-liquid extraction method [6]:
- Add 600 μL of absolute ethanol to 200 μL of plasma sample and 50 μL of working standard solution.
- Vortex mix thoroughly and centrifuge for 2 minutes to precipitate proteins.
- Add 1.0 mL of diethyl ether (first extraction solvent), vortex for 5 minutes, and centrifuge at 3500 rpm for 5 minutes at 0°C.
- Carefully transfer the organic phase to a clean test tube.
- Add 0.5 mL of dichloromethane (second extraction solvent), vortex for 5 minutes, and centrifuge at 3500 rpm for 5 minutes at 0°C.
- Combine the organic layers from both extractions.
- Evaporate the combined organic layers under a gentle stream of nitrogen at 40°C.
- Reconstitute the residue in 500 μL of ethanol, vortex for 2 minutes.
- Inject 20 μL into the HPLC system.
HPLC Analysis Conditions
For the simultaneous determination of cardiovascular drugs, use the following chromatographic conditions [6]:
- Column: Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 μm)
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in 40:60 ratio
- Flow Rate: 0.6 mL/min
- Injection Volume: 20 μL
- Column Temperature: 25-35°C
- Detection: Dual detection with UV (210-260 nm) and fluorescence with specific excitation/emission wavelengths for each analyte:
- Bisoprolol: 227/298 nm
- Telmisartan: 294/365 nm
- Atorvastatin: 274/378 nm
- Amlodipine: 361/442 nm
Data Analysis and Interpretation
Stability Assessment Criteria
Stability is determined by comparing the measured concentrations of stability samples with freshly prepared quality control samples. The percentage deviation from the nominal concentration is calculated as:
% Deviation = [(Mean Concentration of Stability Samples - Nominal Concentration) / Nominal Concentration] × 100
For all stability tests, the acceptance criterion is typically ±15% deviation from the nominal concentration, except for the lower limit of quantification where ±20% may be acceptable.
Documentation
Maintain comprehensive documentation of all stability experiments including:
- Sample preparation records
- Storage conditions and duration
- Analysis dates and conditions
- Raw data and calculated results
- Deviations from protocol and corrective actions
Results and Data Presentation
The following tables present stability data from research on cardiovascular drugs and related analytes, demonstrating how to document and interpret stability assessment results.
Table 2: Freeze-Thaw Stability Data for Cardiovascular Drugs and Related Analytes
| Analyte | Matrix | Storage Temperature | Freeze-Thaw Cycles | Stability Outcome | Reference |
|---|---|---|---|---|---|
| Bisoprolol, Amlodipine, Telmisartan, Atorvastatin | Human plasma | -20°C or -40°C | 3 cycles | Stable (within ±15% deviation) | [6] |
| 8-iso-PGF2α | Human urine | -40°C | 10 cycles | Significant increase by cycle 6 (151% of baseline at cycle 10) | [76] |
| 11-dehydro-TxB2 | Human urine | -40°C | 10 cycles | Stable (100.4% of baseline at cycle 10) | [76] |
| Creatinine | Human urine | -40°C | 10 cycles | Stable (101% of baseline at cycle 10) | [76] |
| Clinical Chemistry Analytes (AST, ALT, CK, GGT, etc.) | Human serum | -20°C | 10 cycles | Stable (considering clinical acceptability) | [77] |
Table 3: Long-Term Stability Data for Cardiovascular Drugs and Related Analytes
| Analyte | Matrix | Storage Temperature | Storage Duration | Stability Outcome | Reference |
|---|---|---|---|---|---|
| 11-dehydro-TxB2, 8-iso-PGF2α, Creatinine | Human urine | -40°C | 10 years | Highly correlated (all rho = 0.99, P < 0.0001) | [76] |
| Clinical Chemistry Analytes | Human serum | -20°C | 3 months | Most analytes stable; BUN, uric acid, total protein, albumin, total bilirubin, calcium, LD showed significant changes | [77] |
Troubleshooting and Technical Notes
Common Issues and Solutions
Degradation Observed in Bench-Top Stability: If significant degradation occurs within 4 hours at room temperature, implement stricter control of sample processing time and temperature. Consider using ice baths during sample processing.
Variable Freeze-Thaw Stability Results: Ensure consistent thawing procedures across all samples. Use water baths or controlled temperature environments for thawing rather than leaving samples at room temperature for variable time periods.
Decreased Recovery After Long-Term Storage: Adsorption to storage containers may occur over time. Consider adding carrier proteins or changing container materials if decreased recovery is observed.
Factors Influencing Stability
pH Sensitivity: Some cardiovascular drugs, particularly those with ester functionalities or labile protons, may be pH-sensitive. Maintain consistent pH during sample processing and storage.
Light Sensitivity: Amlodipine and other dihydropyridine calcium channel blockers are light-sensitive. Use amber vials or protect samples from light during processing and storage.
Oxidative Degradation: Atorvastatin and other compounds with phenolic groups may be susceptible to oxidation. Consider adding antioxidants to the storage matrix if instability is observed.
Comprehensive stability assessment including bench-top, freeze-thaw, and long-term stability evaluation is essential for validating HPLC methods for simultaneous determination of cardiovascular drugs in plasma. The protocols outlined in this document provide a systematic approach to demonstrate analyte stability under various conditions that mimic real-world sample handling scenarios. Properly conducted stability studies ensure the reliability and reproducibility of bioanalytical data, ultimately supporting the validity of pharmacokinetic and bioequivalence studies for cardiovascular drug formulations.
The data presented from recent studies demonstrates that most cardiovascular drugs maintain stability under appropriate storage conditions, though analyte-specific characteristics must be considered when designing stability assessments. Regular monitoring of stability throughout the method's application is recommended, particularly for long-term studies where samples may be stored for extended periods before analysis.
Within pharmaceutical research, particularly for the sensitive determination of cardiovascular drugs in human plasma, the selection of an analytical technique must balance analytical performance with environmental impact. High-Performance Liquid Chromatography with Fluorescence Detection (HPLC-FLD) and Micellar Electrokinetic Chromatography (MEKC) are two prominent separation techniques. This application note provides a detailed comparative analysis of these methods, framing the discussion within the context of developing a green and efficient HPLC-FLD method for the simultaneous determination of cardiovascular drugs in plasma. The evaluation is based on analytical performance metrics, practical applicability in drug monitoring, and alignment with Green Analytical Chemistry (GAC) principles, providing researchers and drug development professionals with a clear framework for method selection.
Fundamental Principles and Instrumentation
High-Performance Liquid Chromatography with Fluorescence Detection (HPLC-FLD)
HPLC separates compounds based on their differential partitioning between a mobile phase and a stationary phase. The integration of a fluorescence detector (FLD) provides exceptional sensitivity and selectivity for analytes that are inherently fluorescent or can be derivatized to form fluorescent compounds. Detection involves measuring the emitted light after the analyte is excited at a specific wavelength [6] [78]. This technique is a mainstay in bioanalysis, such as for quantifying cardiovascular drugs in plasma, where high sensitivity is required to detect low therapeutic concentrations amidst a complex biological matrix [6].
Micellar Electrokinetic Chromatography (MEKC)
MEKC is a mode of Capillary Electrophoresis (CE) that overcomes CE's primary limitation—the inability to separate neutral molecules. It does so by introducing surfactant micelles into the background electrolyte (BGE) at a concentration above the critical micelle concentration (CMC). These micelles act as a pseudostationary phase, enabling the separation of neutral analytes based on their differential partitioning between the hydrophilic aqueous phase and the hydrophobic micellar core [79]. Charged analytes are separated based on both their electrophoretic mobility and their interaction with the micelles [80] [79]. The fundamental workflow of MEKC is outlined in the diagram below.
Experimental Protocols
Protocol A: HPLC-FLD for Cardiovascular Drugs in Plasma
This protocol is adapted from a validated method for the simultaneous determination of bisoprolol, amlodipine, telmisartan, and atorvastatin in human plasma [6].
3.1.1 Research Reagent Solutions
| Reagent / Solution | Function in the Protocol |
|---|---|
| Thermo Hypersil BDS C18 Column (150 x 4.6 mm, 5.0 µm) | Stationary phase for reverse-phase chromatographic separation. |
| Ethanol & 0.03 M Potassium Phosphate Buffer (pH 5.2) (40:60, v/v) | Isocratic mobile phase; ethanol is a greener alternative to acetonitrile. |
| Liquid-Liquid Extraction (LLE) | Sample preparation technique using diethyl ether and dichloromethane to isolate analytes from plasma proteins and matrix. |
| Fluorescence Detector | Provides highly sensitive and selective detection using optimized excitation/emission wavelengths for each drug. |
| Nitrogen Evaporator | Gently removes organic extraction solvents under a stream of nitrogen to preconcentrate the analytes. |
3.1.2 Detailed Procedure
- Chromatographic Conditions:
- Column: Thermo Hypersil BDS C18 (150 x 4.6 mm, 5.0 µm).
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer, pH 5.2 (40:60, v/v). The use of ethanol aligns with green chemistry principles by replacing more toxic solvents [42] [81].
- Flow Rate: 0.6 mL/min.
- Detection: Fluorescence detection with programmable wavelengths: 227/298 nm for bisoprolol, 294/365 nm for telmisartan, 274/378 nm for atorvastatin, and 361/442 nm for amlodipine [6].
- Injection Volume: 20 µL.
- Run Time: <10 minutes.
- Plasma Sample Preparation (LLE):
- To 200 µL of human plasma, add 50 µL of the working standard solution and 600 µL of absolute ethanol.
- Vortex the mixture and centrifuge for 2 minutes to precipitate proteins.
- Perform a two-step LLE:
- First Extraction: Add 1.0 mL of diethyl ether to the supernatant, vortex for 5 minutes, and centrifuge at 3500 rpm for 5 minutes at 0°C. Transfer the organic layer to a clean tube.
- Second Extraction: Add 0.5 mL of dichloromethane to the remaining aqueous layer, vortex for 5 minutes, and centrifuge as before. Combine this organic layer with the first extract.
- Evaporate the combined organic layers to dryness under a gentle stream of nitrogen at 40°C.
- Reconstitute the dry residue in 500 µL of ethanol, vortex for 2 minutes, and inject 20 µL into the HPLC system [6].
Protocol B: MEKC for Pharmaceutical Analysis
This protocol outlines a general MEKC method, with parameters that can be adapted for the analysis of various drugs, including cardiovascular compounds [7] [79].
3.2.1 Research Reagent Solutions
| Reagent / Solution | Function in the Protocol |
|---|---|
| Fused Silica Capillary (e.g., 50-75 µm i.d., 40-60 cm length) | The separation channel where electrophoresis and partitioning occur. |
| Sodium Dodecyl Sulfate (SDS) | Surfactant forming anionic micelles that act as the pseudostationary phase. |
| Borate or Phosphate Buffer | Constitutes the background electrolyte (BGE), defining pH and ionic strength. |
| Organic Modifier (e.g., Acetonitrile, Methanol) | Added to the BGE to modify selectivity and improve separation efficiency. |
| Sodium Cholate | A bile salt surfactant, an alternative to SDS, offering different selectivity [82]. |
3.2.2 Detailed Procedure
- MEKC Conditions:
- Capillary: Fused silica, 41.5 cm total length (or 50 cm effective length), 50 µm internal diameter.
- Background Electrolyte (BGE): 50 mM borate buffer (pH 9.0) containing 50 mM Sodium Lauryl Sulfate (SLS, synonymous with SDS) and 10% (v/v) acetonitrile [7].
- Voltage: 20-30 kV (optimize to minimize Joule heating).
- Temperature: 20-25°C (controlled by the instrument cartridge).
- Detection: UV or Diode Array Detection (DAD), often at 200-220 nm or analyte-specific wavelengths.
- Injection: Hydrodynamic injection (e.g., 50 mbar for 5 s).
- Capillary Preparation and Operation:
- Conditioning: Before first use and each run, rinse the capillary sequentially with 1 M NaOH (10 min), purified water (10 min), and the BGE (10 min) [80] [7].
- Sample Injection: Hydrodynamically inject the prepared sample.
- Separation: Apply the high voltage to initiate separation. The electroosmotic flow (EOF) and electrophoretic mobility of the micelles drive the separation process.
- Between Runs: A shorter rinsing cycle with BGE (e.g., 2 min) is typically sufficient.
Comparative Data Analysis
The following tables summarize a direct comparison of the two techniques based on key performance and sustainability metrics.
Table 1: Analytical Performance and Practical Application Comparison
| Parameter | HPLC-FLD | MEKC |
|---|---|---|
| Mechanism | Partitioning between mobile & stationary phases | Partitioning + Electrophoresis (micelles as pseudo-phase) |
| Separation Efficiency | High | Very High (theoretical plates often >100,000) [79] |
| Analysis Time | Fast (e.g., <10 min for 4 drugs) [6] | Typically fast, but can be method-dependent |
| Sensitivity (LOD/LOQ) | Excellent (e.g., LOQ: 0.1-10 ng/mL in plasma) [6] | Generally lower than HPLC-FLD; can be improved with stacking [82] [80] |
| Selectivity Tuning | Mobile phase composition, column chemistry, gradient | BGE pH, surfactant type/concentration, organic modifiers [80] [79] |
| Sample Matrix Tolerance | High; robust with biological matrices post-extraction | Lower; requires sample cleanup for complex matrices like plasma [80] |
| Multi-Analyte Capacity | Excellent for simultaneous drug analysis [6] [7] | Excellent for simultaneous drug analysis [7] |
Table 2: Greenness and Operational Cost Comparison
| Parameter | HPLC-FLD | MEKC |
|---|---|---|
| Solvent Consumption | Moderate to High (mL/min) | Very Low (mL/day) [7] [79] |
| Chemical Waste Generation | High (hundreds of mL/day) | Very Low (tens of mL/day) |
| Hazardous Waste | Organic solvents (e.g., ACN, MeOH) | Mostly aqueous buffer with surfactants |
| Energy Consumption | Moderate (pumps, oven) | Low (high voltage power supply) |
| Sample/Solvent Volume | µL to mL sample volume; mL mobile phase | nL sample injection; mL total BGE volume |
| Cost per Analysis | Higher (cost of solvents, columns) | Lower (minimal reagent consumption) |
Greenness and Practical Applicability Assessment
The "whiteness" of an analytical method—a balance of analytical performance (red), ecological impact (green), and practical/economic feasibility (blue)—is a modern paradigm for evaluating its overall sustainability and practicality [42].
- HPLC-FLD excels in analytical performance (Red), particularly for complex tasks like quantifying multiple cardiovascular drugs in plasma, where its superior sensitivity, robustness, and tolerance to sample matrices are paramount [6]. Its ecological score is lower, though it can be improved using ethanol-based mobile phases [81].
- MEKC demonstrates superior ecological impact (Green) and practical feasibility (Blue) due to minimal reagent consumption, reduced waste generation, and lower operational costs [7] [79]. However, its practical application in biological analysis can be hampered by lower sensitivity and susceptibility to matrix effects, placing it lower on the analytical performance axis unless sensitivity-enhancing techniques like stacking are employed [82] [80].
The choice between HPLC-FLD and MEKC is context-dependent. For the specific thesis context of developing a highly sensitive and robust method for the simultaneous determination of cardiovascular drugs in human plasma, HPLC-FLD is the recommended technique. Its proven sensitivity, compatibility with complex biological matrices, and the high selectivity of fluorescence detection make it the more reliable and practical choice for this demanding application, despite its higher environmental footprint.
Conversely, MEKC is the ideal choice for applications where green chemistry principles are the highest priority and for the analysis of less complex matrices, such as pharmaceutical dosage forms. Its minimal consumption of solvents and reagents aligns perfectly with the goals of sustainable laboratory practice.
Future work should focus on bridging this gap by further developing sensitivity-enhancement strategies for MEKC (e.g., advanced stacking, alternative detectors) and continuing to replace hazardous solvents with greener alternatives in HPLC methods to achieve a "whiter" overall analytical process.
High-Performance Liquid Chromatography (HPLC) serves as a cornerstone analytical technique in pharmacokinetic studies, enabling the precise quantification of drug concentrations in biological fluids. Within the context of a broader thesis on HPLC method development for the simultaneous determination of cardiovascular drugs in plasma, this application note details specific protocols for determining fundamental pharmacokinetic parameters—Cmax, Tmax, and bioavailability. These parameters are critical for understanding the absorption and exposure profiles of drugs, which directly informs dosing regimen design and therapeutic efficacy assessments [83] [6]. The methodologies outlined herein are validated for a panel of cardiovascular drugs—bisoprolol, amlodipine, telmisartan, and atorvastatin—facilitating robust bioanalysis in support of drug development and clinical monitoring [6].
Core Pharmacokinetic Parameters and Their Significance
Cmax is the maximum observed drug concentration in the plasma following dose administration. It provides a critical indicator of the drug's absorption rate and extent, helping to assess both therapeutic efficacy and potential toxicity risks. Doses that result in a Cmax exceeding the therapeutic window may lead to adverse effects, while a sub-therapeutic Cmax can indicate inadequate dosing [83].
Tmax is the time taken to reach Cmax after drug administration. It serves as a key pharmacokinetic marker for the rate of absorption, informing formulation development and dosing interval recommendations.
Bioavailability denotes the fraction of an administered drug dose that reaches the systemic circulation unchanged. It is a pivotal parameter for evaluating the efficiency of drug absorption from various formulations. The absolute bioavailability is typically determined by comparing the area under the plasma concentration-time curve (AUC) after extravascular administration (e.g., oral) to that after intravenous administration [83].
The relationship between dosing frequency and drug accumulation is fundamental to pharmacokinetics. Repetitive dosing at intervals shorter than the drug's elimination half-life leads to drug accumulation until a steady-state concentration is achieved. The Accumulation Ratio (AR) quantifies how much higher steady-state concentrations are compared to those after a single dose [83]. Table 1 summarizes the core pharmacokinetic parameters and their roles in drug development.
Table 1: Core Pharmacokinetic Parameters in Drug Development
| Parameter | Definition | Pharmacokinetic Significance | Role in Drug Development |
|---|---|---|---|
| Cmax | Maximum observed plasma concentration | Reflects peak exposure and absorption rate | Critical for safety assessments (therapeutic window) and efficacy |
| Tmax | Time to reach Cmax | Indicates absorption rate | Guides dosing interval and formulation optimization |
| AUC | Area Under the plasma Concentration-time curve | Measures total drug exposure over time | Primary metric for calculating bioavailability (F) and clearance |
| Bioavailability (F) | Fraction of dose reaching systemic circulation | Quantifies absorption efficiency | Key for comparing formulations and routes of administration |
| Accumulation Ratio (AR) | Ratio of steady-state to single-dose exposure | Predicts drug build-up with multiple dosing | Informs dosing regimen design to avoid toxicity [83] |
HPLC Method Development and Validation
Analytical Conditions for Cardiovascular Drug Panel
A simultaneous HPLC method for quantifying bisoprolol (BIS), amlodipine besylate (AML), telmisartan (TEL), and atorvastatin (ATV) in human plasma has been developed and validated. This method employs a dual detection strategy (UV and fluorescence) for enhanced sensitivity and specificity [6] [29].
Chromatographic System:
- Column: Thermo Hypersil BDS C18 (150 mm × 4.6 mm, 5.0 μm)
- Mobile Phase: Ethanol and 0.03 M potassium phosphate buffer (pH 5.2) in a 40:60 ratio
- Flow Rate: 0.6 mL/min
- Elution Mode: Isocratic
- Injection Volume: 20 µL
- Run Time: <10 minutes [6]
Detection Parameters:
Sample Preparation Protocol
The sample preparation utilizes a liquid-liquid extraction (LLE) technique to isolate the analytes from the plasma matrix efficiently [6].
- Protein Precipitation: To 200 µL of plasma sample, add 50 µL of the working standard solution and 600 µL of absolute ethanol. Vortex the mixture thoroughly and centrifuge for 2 minutes to precipitate proteins.
- First Extraction: Add 1.0 mL of diethyl ether (first extraction solvent) to the supernatant. Vortex the mixture for 5 minutes and then centrifuge at 3500 rpm for 5 minutes at 0°C. Carefully transfer the separated organic layer to a clean test tube.
- Second Extraction: Add 0.5 mL of dichloromethane (second extraction solvent) to the remaining aqueous layer. Vortex for 5 minutes and centrifuge again under the same conditions. Combine this organic layer with the one obtained from the first extraction.
- Evaporation and Reconstitution: Evaporate the combined organic extracts to dryness under a gentle stream of nitrogen gas at 40°C. Reconstitute the resulting residue in 500 µL of ethanol, vortex for 2 minutes, and inject 20 µL into the HPLC system [6].
The method was validated per International Council for Harmonisation (ICH) guidelines, demonstrating high sensitivity and reliability for pharmacokinetic application [6]. The key validation parameters are summarized in Table 2 below.
Table 2: HPLC Method Validation Parameters for Cardiovascular Drugs
| Analyte | Linear Range (ng/mL) | LLOQ (ng/mL) | Accuracy & Precision | Detection Type |
|---|---|---|---|---|
| Bisoprolol (BIS) | 5 - 100 | 5 | Meets ICH criteria | Fluorescence |
| Amlodipine (AML) | 5 - 100 | 5 | Meets ICH criteria | Fluorescence |
| Telmisartan (TEL) | 0.1 - 5 | 0.1 | Meets ICH criteria | Fluorescence |
| Atorvastatin (ATV) | 10 - 200 | 10 | Meets ICH criteria | Fluorescence |
Experimental Protocol for PK Study
Subject Dosing and Blood Sampling
- Administration: Administer a single oral dose of the drug formulation (e.g., a fixed-dose combination of the cardiovascular drugs) to study subjects under fasting conditions.
- Blood Collection: Draw serial blood samples (e.g., 2-4 mL) into heparinized tubes at pre-dose (0 h) and at pre-defined time points post-dose (e.g., 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, 8, 12, 16, and 24 hours). The specific time points should be optimized to adequately capture the absorption, distribution, and elimination phases.
- Sample Processing: Centrifuge the blood samples immediately after collection at 3000 rpm for 10 minutes to separate plasma. Transfer the plasma into polypropylene tubes and store at -80°C until analysis.
Bioanalytical Workflow
The following diagram illustrates the complete workflow from sample collection to pharmacokinetic analysis.
Data and Statistical Analysis
- Concentration-Time Profile: Using the measured concentration at each time point, plot the mean plasma concentration-time profile for each analyte.
- PK Parameter Calculation:
- Cmax and Tmax: Directly observed from the concentration-time data.
- AUC0-t: Calculate using the linear trapezoidal rule from time zero to the last measurable time point (t).
- AUC0-∞: Calculate as AUC0-t + Ct/λz, where Ct is the last measurable concentration and λz is the terminal elimination rate constant.
- Bioavailability (F) Calculation: For absolute bioavailability assessment, calculate F using the formula: F (%) = (AUCpo × Doseiv) / (AUCiv × Dosepo) × 100, where the subscripts 'po' and 'iv' refer to oral and intravenous administration, respectively.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of this protocol requires specific, high-quality materials. Table 3 lists the key reagents and their functions in the analytical process.
Table 3: Essential Research Reagents and Materials
| Item | Specification/Example | Function in Protocol |
|---|---|---|
| HPLC System | Waters Alliance 2695 with quaternary pump, auto-sampler, and column oven | Precise solvent delivery, sample injection, and temperature control for separation |
| Detection System | Dual-wavelength UV/PDA Detector and Multi λ Fluorescence Detector | Sensitive and selective detection of separated analytes [6] |
| Analytical Column | Thermo Hypersil BDS C18 (150 x 4.6 mm, 5 µm) | Stationary phase for reverse-phase separation of analytes [6] |
| Mobile Phase | Ethanol and 0.03 M Potassium Phosphate Buffer (pH 5.2) | Liquid phase that carries the sample through the column, achieving separation [6] |
| Extraction Solvents | Absolute Ethanol, Diethyl Ether, Dichloromethane | Protein precipitation and liquid-liquid extraction to isolate analytes from plasma [6] |
| Reference Standards | High-purity Bisoprolol, Amlodipine, Telmisartan, Atorvastatin | Qualification and quantification of analytes; construction of calibration curves |
| Human Plasma | Blank (drug-free) and study samples | Biological matrix for method development and subject sample analysis [6] |
Regulatory and Data Standards
For regulatory submissions, pharmacokinetic data must often be structured according to CDISC standards. The Analysis Dataset for Pharmacokinetic Concentrations (ADPC) is the ADaM dataset used for submitting concentration results, structured with one record per subject, per analyte, per time point. Key variables in ADPC include PARAMCD (analyte code), AVAL (numeric concentration value), ARELTM (relative time from dosing), and ATPT (planned time point). This dataset is used to derive pharmacokinetic parameters, which are subsequently stored in the Analysis Dataset for Pharmacokinetic Parameters (ADPP) dataset, with one record per subject per parameter (e.g., Cmax, AUC) [84]. Standardized datasets ensure traceability and facilitate regulatory review.
Conclusion
The development of sophisticated, validated HPLC methods is paramount for the accurate simultaneous determination of cardiovascular drugs in plasma, directly supporting advancements in therapeutic drug monitoring and personalized medicine. The integration of green chemistry principles, dual detection systems, and robust validation frameworks ensures that these methods are not only scientifically sound but also sustainable and compliant with regulatory standards. Future directions should focus on expanding multi-analyte panels using HPLC-MS/MS for metabolomics, further miniaturizing and automating sample preparation, and applying these robust methods in large-scale clinical studies to establish clear correlations between drug concentrations and therapeutic outcomes, ultimately enhancing drug safety and efficacy for cardiovascular patients worldwide.
References
- 1. Global burden of cardiovascular diseases: projections from ... [https://pubmed.ncbi.nlm.nih.gov/39270739/]
- 2. Polypharmacy and Rising Medication Use in the United ... [https://www.odu.edu/polypharmacy-and-rising-medication-use-the-united-states-25-year-national-trends]
- 3. Polypharmacy's Association With Mortality: Confounding ... [https://pubmed.ncbi.nlm.nih.gov/40614131/]
- 4. Fixed-dose combination therapy for the prevention of ... [https://www.nature.com/articles/s41591-024-02896-w]
- 5. Fixed dose combination drugs for cardiovascular disease in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9884866/]
- 6. Development and validation of a highly sensitive HPLC ... [https://www.nature.com/articles/s41598-025-94907-0]
- 7. Simple simultaneous analysis of various cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11468470/]
- 8. Calcium Channel Blockers - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK482473/]
- 9. Angiotensin II Receptor Blockers (ARB) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK537027/]
- 10. HPLC methods for the determination of simvastatin and ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993608000113]
- 11. Application of UHPLC-QqQ-MS/MS Method for Quantification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11477679/]
- 12. Calcium channel blockers for hypertension: old, but still ... [https://www.e-jcpp.org/journal/view.php?doi=10.36011/cpp.2023.5.e16]
- 13. Angiotensin Receptor Blockers: New Considerations in Their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8109530/]
- 14. Use of Ultra High Performance Liquid Chromatography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2975081/]
- 15. Development and validation of an analytical method using ... [https://www.sciencedirect.com/science/article/pii/S1570023222004573]
- 16. Evaluation of the clinical and quantitative performance of a ... [https://jphcs.biomedcentral.com/articles/10.1186/s40780-023-00298-7]
- 17. A Single-Run HPLC–MS Multiplex Assay for Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10674734/]
- 18. Determination of nine cardiovascular drugs in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10716505/]
- 19. Steps for HPLC Method Validation [https://www.pharmaguideline.com/2017/12/hplc-method-validation.html]
- 20. Design-assisted HPLC-UV method for therapeutic drug ... [https://www.nature.com/articles/s41598-024-78793-6]
- 21. Evaluation of the clinical and quantitative performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10544152/]
- 22. Development and validation of a RP-HPLC method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264094/]
- 23. A validated method using RP-HPLC for the simultaneous ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X2500596X]
- 24. QbD-driven RP-HPLC method for the simultaneous analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574138/]
- 25. New HPLC, MS, and CDS Products from 2024–2025 [https://www.chromatographyonline.com/view/new-hplc-ms-and-cds-products-from-2024-2025-a-brief-review]
- 26. A sustainable multi-task HPLC–UV method for ... [https://www.nature.com/articles/s41598-025-07502-8]
- 27. Development of a sustainable multianalyte MEKC method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10518094/]
- 28. Determination of nine cardiovascular drugs in human ... [https://www.sciencedirect.com/science/article/pii/S2405844023097517]
- 29. Development and validation of a highly sensitive HPLC ... [https://pubmed.ncbi.nlm.nih.gov/40210736/]
- 30. An eco-friendly bioanalytical RP-HPLC method coupled with ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-025-01507-0]
- 31. Green HPLC strategy for quantification of carvedilol and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224793/]
- 32. A Fast and Validated HPLC Method for Simultaneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7936887/]
- 33. (PDF) RP- HPLC Method for the Simultaneous Estimation of Eight... [https://www.academia.edu/11839928/RP_HPLC_Method_for_the_Simultaneous_Estimation_of_Eight_Cardiovascular_Drugs]
- 34. HPLC Column Selection Guide [https://www.auroraprosci.com/HPLC-column-selection-guide?srsltid=AfmBOooKiFXXmt156ks0cAh0xGAbErjsFFjtD3UolvrHnzGZQQH2_29f]
- 35. A rapid method for determination of rosuvastatin in blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12013102/]
- 36. Validation of a sensitive bioanalytical method for ... [https://www.sciencedirect.com/science/article/pii/S2949771X2400001X]
- 37. Simultaneous determination of cardiovascular drugs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9306983/]
- 38. Development and validation of a highly sensitive HPLC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11986036/]
- 39. HPLC method offers value for cardiovascular drug QC ... [https://www.europeanpharmaceuticalreview.com/news/240768/hplc-method-demonstrates-value-for-quality-control-analysis-of-cardiovascular-drug/]
- 40. An eco-friendly bioanalytical RP-HPLC method coupled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12102954/]
- 41. Recent approaches in green liquid chromatography for ... [https://www.sciencedirect.com/science/article/abs/pii/S2950357425000265]
- 42. Green Approaches in High-Performance Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12430196/]
- 43. HPLC Tips & Tricks: Getting Greener in HPLC [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/analytical-chemistry/small-molecule-hplc/getting-greener-in-hplc?srsltid=AfmBOoqtsB3KmHjruD5kmzd2rRwORnTqa-9c3wcrPABISjzRIk12Xwpk]
- 44. Validation of Stability-Indicating HPLC Methods for ... [https://www.chromatographyonline.com/view/validation-of-stability-indicating-hplc-methods-for-pharmaceuticals-overview-methodologies-and-case-studies]
- 45. Methods for Changing Peak Resolution in HPLC [https://www.chromatographyonline.com/view/methods-changing-peak-resolution-hplc-advantages-and-limitations]
- 46. Resolving Co-Eluted Peaks in HPLC: A Derivative-Based ... [https://www.linkedin.com/pulse/resolving-co-eluted-peaks-hplc-derivative-based-approach-hossain-7kgye]
- 47. Mobile Phase Optimization: A Critical Factor in HPLC [https://www.phenomenex.com/knowledge-center/hplc-knowledge-center/mobile-phase-in-chromatography?srsltid=AfmBOop629Md1-QFPfMc6mbhjikN113Wa2rlSS-tebzeIDvjQfdnh2uH]
- 48. Real Solutions to Improve Your HPLC Peak Resolution [https://www.thermofisher.com/blog/analyteguru/real-solutions-to-improve-your-hplc-peak-resolution/]
- 49. Learn HPLC Method Development With Expert Tips, 4 ... [https://pharmaguru.co/hplc-method-development/]
- 50. HPLC Method Development Steps [https://www.thermofisher.com/us/en/home/industrial/chromatography/chromatography-learning-center/liquid-chromatography-information/hplc-method-development-steps.html]
- 51. HPLC Tips & Tricks: Increase Your HPLC/UHPLC Method ... [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/analytical-chemistry/small-molecule-hplc/increase-your-hplc-uhplc-method-sensitivity?srsltid=AfmBOoqYKITeBq8WqOVpi3qbdlDKnNubgfvVhXJUTcvv55Ftuq26d28n]
- 52. The Limit of Detection [https://www.chromatographyonline.com/view/limit-detection]
- 53. Increasing the sensitivity in case of LOD / LOQ ... - Lösungsfabrik [https://mpl.loesungsfabrik.de/en/english-blog/high-performance-liquid-chromatography/increase-of-sensitivity]
- 54. How to improve LOD or detection limits in HPLC [https://www.mtc-usa.com/kb-article/aa-01024]
- 55. Simultaneous Development and Validation of an HPLC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12526389/]
- 56. Advanced Strategies to Improve Detection Limits in ... [https://www.organomation.com/advanced-strategies-to-improve-detection-limits-in-chromatography-mass-spectrometry]
- 57. Matrix effects break the LC behavior rule for analytes in LC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4935370/]
- 58. What are Matrix Effect in Liquid Chromatography Mass ... [https://www.nebiolab.com/what-are-matrix-effect-in-liquid-chromatography-mass-spectrometry/]
- 59. Efficient extraction and sensitive HPLC-MS ... [https://www.sciencedirect.com/science/article/pii/S0889157522001983]
- 60. Development, validation and application of a novel HPLC ... [https://www.sciencedirect.com/science/article/pii/S0731708518313232]
- 61. Robustness Tests [https://www.chromatographyonline.com/view/robustness-tests]
- 62. Method Validation and Robustness [https://www.chromatographyonline.com/view/method-validation-and-robustness]
- 63. What Is HPLC Method Robustness Assessment and Its ... [https://altabrisagroup.com/hplc-method-robustness-assessment/]
- 64. Implementing Robustness Testing for HPLC Methods [https://www.sepscience.com/implementing-robustness-testing-for-hplc-methods-6978]
- 65. how to evaluate robustness in gradient method [http://www.chromforum.org/viewtopic.php?t=18036]
- 66. Micellar systems for sustainable applications in ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25028012]
- 67. Micellar Liquid Chromatography: How to Start [https://www.chromatographyonline.com/view/micellar-liquid-chromatography-how-start-1]
- 68. A new green approach for the reduction of consumed ... [https://pubmed.ncbi.nlm.nih.gov/35733689/]
- 69. Development of Micellar HPLC-UV Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5852859/]
- 70. Process Validation Regulations For Non [https://www.linkedin.com/pulse/comparative-analysis-process-validation-framework-us-fda-uday-shetty-fppqc]
- 71. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 72. HPLC Method Development and Validation for ... [https://www.pharmtech.com/view/hplc-method-development-and-validation-pharmaceutical-analysis]
- 73. Are You Sure You Understand USP <621>? [https://www.chromatographyonline.com/view/are-you-sure-you-understand-usp-621-]
- 74. Simple simultaneous analysis of various cardiovascular drug ... [https://bmcchem.biomedcentral.com/articles/10.1186/s13065-024-01303-2]
- 75. Evaluating Freeze–Thaw Processes in Biopharmaceutical ... [https://www.bioprocessintl.com/fill-finish/evaluating-freeze-thaw-processes-in-biopharmaceutical-development-small-scale-study-designs]
- 76. Effect of very long-term storage and multiple freeze and ... [https://www.nature.com/articles/s41598-024-55720-3]
- 77. The effect of storage time and freeze-thaw cycles on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3900085/]
- 78. HPLC-Fluorescence Detection Method for Concurrent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10140086/]
- 79. Micellar Electrokinetic Chromatography: A Workhorse for ... [https://www.sepscience.com/micellar-electrokinetic-chromatography-a-workhorse-for-complex-separations-12150]
- 80. Method Development for Capillary Electrophoresis [https://www.labx.com/resources/method-development-for-capillary-electrophoresis-optimization-strategies/5638]
- 81. Sustainable and white HPLC method for simultaneous ... [https://www.sciencedirect.com/science/article/pii/S2772577424000120]
- 82. High Performance Liquid Chromatography versus Stacking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8746415/]
- 83. Accumulation: What It Means and How to Calculate It [https://www.certara.com/knowledge-base/accumulation-what-it-means-and-how-to-calculate-it/]
- 84. The Creation of ADaM Datasets for Pharmacokinetic (PK) ... [https://www.quanticate.com/blog/adam-datasets-for-pharmacokinetic-pk-analysis]