Analytical Sensitivity vs. Functional Sensitivity: A Comprehensive Guide for Biomarker and Diagnostic Assay Development
This article provides a critical examination of analytical and functional sensitivity, two pivotal performance metrics in the development and validation of diagnostic assays and biomarkers.
Analytical Sensitivity vs. Functional Sensitivity: A Comprehensive Guide for Biomarker and Diagnostic Assay Development
Abstract
This article provides a critical examination of analytical and functional sensitivity, two pivotal performance metrics in the development and validation of diagnostic assays and biomarkers. Tailored for researchers, scientists, and drug development professionals, it explores the foundational definitions, distinctions, and regulatory frameworks governing these parameters. The scope extends to methodological approaches for their assessment across various technology platforms—including immunoassays, molecular diagnostics, and novel biosensors—addressed through intent-focused sections on troubleshooting, optimization, and rigorous validation. By synthesizing current standards with emerging trends such as AI-driven optimization and dual-modality biosensors, this guide aims to equip professionals with the knowledge to enhance assay robustness, ensure regulatory compliance, and successfully translate biomarkers from research to clinical application.
Demystifying Sensitivity: Core Concepts and Regulatory Foundations for Robust Assay Design
In the field of bioanalysis, accurately measuring substances at very low concentrations is crucial for drug development, clinical diagnostics, and regulatory decision-making. The terms Limit of Blank (LoB), Limit of Detection (LoD), and Limit of Quantitation (LoQ) are used to describe the smallest concentration of an analyte that can be reliably measured by an analytical procedure [1]. These parameters form a critical foundation for characterizing the analytical sensitivity of an assay and are essential for understanding its capabilities and limitations to ensure it is "fit for purpose" [1]. Within the broader context of analytical versus functional sensitivity performance research, clearly distinguishing between these related but distinct concepts enables researchers to properly validate methods, compare assay performance, and make informed decisions based on reliable data, particularly at the lower limits of detection.
Core Definitions and Statistical Foundations
LoB, LoD, and LoQ represent progressively higher concentration levels that define an assay's detection capabilities, each with specific statistical definitions and practical implications [1].
| Parameter | Definition | Sample Characteristics | Statistical Calculation |
|---|---|---|---|
| Limit of Blank (LoB) | The highest apparent analyte concentration expected when replicates of a blank sample (containing no analyte) are tested [1]. | Sample containing no analyte (e.g., zero-level calibrator), commutable with patient specimens [1]. | LoB = mean~blank~ + 1.645(SD~blank~) [1] |
| Limit of Detection (LoD) | The lowest analyte concentration likely to be reliably distinguished from the LoB and at which detection is feasible [1]. | Low concentration sample, commutable with patient specimens [1]. | LoD = LoB + 1.645(SD~low concentration sample~) [1] |
| Limit of Quantitation (LoQ) | The lowest concentration at which the analyte can be reliably detected and measured with predefined goals for bias and imprecision [1]. | Low concentration sample at or above the LoD [1]. | LoQ ≥ LoD; concentration where predefined bias/imprecision goals are met [1] |
The relationships and progression from LoB to LoD and LoQ can be visualized as a continuum of detectability and reliability.
The diagram above illustrates the hierarchical relationship where each limit builds upon the previous one. The LoB establishes the baseline noise level of the assay. The LoD represents a concentration that produces a signal strong enough to be distinguished from this noise with high statistical confidence (typically 95% that the signal is not from a blank) [1]. The LoQ is the level at which not only can the analyte be detected, but it can also be measured with specified accuracy and precision, often defined by a target coefficient of variation (CV%), such as 10% or 20% [2] [3].
Methodological Approaches and Experimental Protocols
Standardized Protocols for Determination
The Clinical and Laboratory Standards Institute (CLSI) guideline EP17 provides a standardized method for determining LoB, LoD, and LoQ [1]. The experimental process involves specific sample types and replication strategies to ensure statistical reliability.
Recommended Experimental Replication:
- Manufacturer Establishment: 60 replicates for both LoB and LoD [1]
- Laboratory Verification: 20 replicates for LoB and LoD verification [1]
LoB Determination Protocol:
- Sample Preparation: Multiple replicates of a blank sample containing no analyte are tested [1].
- Data Analysis: The mean and standard deviation (SD) of the blank sample results are calculated [1].
- Calculation: LoB = mean~blank~ + 1.645(SD~blank~) (assuming a Gaussian distribution) [1]. This formula ensures that only 5% of blank sample measurements would exceed the LoB due to random variation, representing a false positive rate (Type I error) of 5% [1].
LoD Determination Protocol:
- Sample Preparation: Test replicates of a sample containing a low concentration of analyte [1].
- Data Analysis: Calculate the mean and SD of the low concentration sample [1].
- Calculation: LoD = LoB + 1.645(SD~low concentration sample~) [1]. This ensures that 95% of measurements at the LoD concentration will exceed the LoB, with only 5% falling below (Type II error) [1].
LoQ Determination Protocol:
- Sample Preparation: Test samples containing low concentrations of analyte at or above the LoD [1].
- Data Analysis: Determine the concentration at which predefined goals for bias and imprecision (e.g., CV ≤ 20% or ≤ 10%) are met [1] [3].
- Validation: The LoQ is confirmed when the measurement uncertainty at that concentration falls within acceptable limits [2].
Comparison of Calculation Approaches
Researchers have developed multiple approaches for calculating these limits, which can yield different results and require careful interpretation.
Statistical vs. Empirical Approaches:
- Statistical Approach: Based on measuring replicate blank and low-concentration samples per CLSI guidelines [1]. A traditional approach calculates LoD as the mean of blank samples + 2 SD, though this may underestimate the true LoD [1] [4].
- Empirical Approach: Involves measuring progressively more dilute concentrations of analyte [4]. This method often provides more realistic LoD values, with studies showing empirical LoDs can be 0.5-0.03 times the magnitude of statistically determined LoDs [4].
Graphical Validation Approaches:
- Uncertainty Profile: A modern graphical tool that combines uncertainty intervals with acceptability limits, based on β-content tolerance intervals [2]. A method is considered valid when uncertainty limits are fully included within acceptability limits [2].
- Accuracy Profile: Another graphical method using tolerance intervals for method validation [2].
Comparative studies have shown that while the classical statistical strategy often provides underestimated values of LoD and LoQ, graphical tools like uncertainty and accuracy profiles offer more relevant and realistic assessments [2].
Comparative Performance Data in Analytical Applications
Case Study: High-Sensitivity Cardiac Troponin T (hs-cTnT) Assays
A 2025 study evaluating the analytical performance of the new Sysmex HISCL hs-cTnT assay provides illustrative data on how these parameters are determined and compared in practice [3].
| Assay Parameter | Sysmex HISCL hs-cTnT | Roche Elecsys hs-cTnT |
|---|---|---|
| Limit of Blank (LoB) | 1.3 ng/L | Not specified in study |
| Limit of Detection (LoD) | 1.9 ng/L | Established reference method |
| Functional Sensitivity (CV 20%) | 1.8 ng/L | Not specified in study |
| Functional Sensitivity (CV 10%) | 3.3 ng/L | Not specified in study |
| Assay Precision | 2.2% at 3253 ng/L, 2.5% at 106 ng/L | Not specified in study |
| Method Comparison | r = 0.95 with Roche hs-cTnT | Reference method |
This verification followed CLSI EP17-A2 guidelines for LoB and LoD determination [3]. The functional sensitivity (a term often used interchangeably with LoQ) was determined by testing serial dilutions and identifying concentrations corresponding to CVs of 20% and 10% [3]. The study concluded that the Sysmex HISCL hs-cTnT fulfills the criteria for a high-sensitivity assay, demonstrating the practical application of these performance metrics in assay validation [3].
Ultrasensitive vs. Highly Sensitive Thyroglobulin Assays
A 2025 comparison of thyroglobulin (Tg) assays for monitoring differentiated thyroid cancer patients demonstrates how different generations of assays vary in their detection capabilities [5].
| Assay Generation | Representative Assay | Limit of Detection | Functional Sensitivity |
|---|---|---|---|
| First-Generation | Initial Tg tests | 0.2 ng/mL | 0.9 ng/mL |
| Second-Generation (Highly Sensitive) | BRAHMS Dynotest Tg-plus | 0.035-0.1 ng/mL | 0.15-0.2 ng/mL |
| Third-Generation (Ultrasensitive) | RIAKEY Tg IRMA | 0.01 ng/mL | 0.06 ng/mL |
This study found that the ultrasensitive Tg assay demonstrated higher sensitivity in predicting positive stimulated Tg levels and potential recurrence compared with the highly sensitive assay, though with lower specificity [5]. The clinical performance differences between these assay generations highlight the importance of understanding LoD and LoQ characteristics when selecting analytical methods for specific clinical applications.
Advanced Considerations and Research Reagents
Research Reagent Solutions for Sensitivity Analysis
| Reagent/Material | Function in Sensitivity Determination |
|---|---|
| Blank Matrix | Sample containing all matrix constituents except the analyte of interest; essential for LoB determination [6]. |
| Zero-Level Calibrator | Calibrator with no analyte; used for LoB studies and establishing baseline signals [1]. |
| Low-Concentration Quality Controls | Samples with analyte concentrations near the expected LoD; used for LoD and LoQ determination [1]. |
| Calibration Curve Standards | Series of standards spanning from blank to above expected LoQ; essential for linearity assessment and LoQ confirmation [2]. |
| Tolerance Interval Calculators | Statistical tools for computing β-content tolerance intervals used in uncertainty profile validation [2]. |
Critical Methodological Considerations
Matrix Effects: The sample matrix significantly impacts LoB, LoD, and LoQ determinations. For complex matrices, generating a proper blank can be challenging, particularly for endogenous analytes that are constituent parts of the matrix [6].
Signal-to-Noise Ratio: Some approaches use signal-to-noise ratio (S/N) for estimating detection limits, typically requiring a ratio of 3:1 for LoD and 10:1 for LoQ [6] [7]. This method allows for initial estimation of the concentration range to be tested.
Uncertainty Profile Validation: This approach involves calculating β-content tolerance intervals and comparing them to acceptance limits [2]. The LoQ is determined by finding the intersection point of the uncertainty profile with the acceptability limit, providing a statistically robust method validation approach [2].
The precise determination and distinction of LoB, LoD, and LoQ are fundamental to characterizing analytical sensitivity and ensuring the reliability of bioanalytical methods. While standardized protocols like CLSI EP17 provide statistical frameworks for these determinations, comparative studies show that empirical and graphical approaches may offer more realistic assessments of assay capabilities, particularly for complex matrices. As assay technology advances toward increasingly sensitive detection, exemplified by the evolution from highly sensitive to ultrasensitive thyroglobulin and cardiac troponin assays, understanding these fundamental performance parameters becomes increasingly critical for researchers, method developers, and clinicians relying on accurate low-end measurement capabilities. The appropriate application of these concepts enables meaningful comparison of analytical methods and ensures that data generated at the limits of detection can be interpreted with appropriate scientific confidence.
In the realm of bioanalytical science, accurately quantifying the lowest concentration of an analyte is paramount for reliable data in drug development and clinical diagnostics. While terms like analytical sensitivity and Limit of Detection (LOD) describe an assay's ability to detect an analyte, they do not guarantee that the measurement is quantitatively precise. Functional Sensitivity, or the Lower Limit of Quantitation (LLOQ), addresses this critical distinction by defining the lowest analyte concentration that can be measured with stated acceptable precision and accuracy, making it the true benchmark for practical, clinically useful results. This guide objectively compares these performance characteristics, providing researchers with the experimental protocols and data needed to evaluate and implement functional sensitivity in their analytical workflows.
Understanding the Key Performance Parameters
Before comparing performance, it is essential to define the distinct parameters that describe an assay's capabilities at low analyte concentrations.
Limit of Blank (LoB) is the highest apparent analyte concentration expected to be found when replicates of a blank sample containing no analyte are tested. It describes the background noise of the assay. Statistically, it is calculated as
Mean_blank + 1.645(SD_blank), assuming a Gaussian distribution where 95% of blank measurements will fall below this value [1] [8].Limit of Detection (LOD), sometimes referred to as Analytical Sensitivity, is the lowest analyte concentration that can be reliably distinguished from the LoB. It is a measure of detection, not quantification, and does not guarantee accurate concentration measurement. Its calculation incorporates the LoB:
LOD = LoB + 1.645(SD_low concentration sample), ensuring that 95% of measurements at the LOD exceed the LoB [1] [9] [10].Limit of Quantitation (LoQ) or Lower Limit of Quantitation (LLOQ), also known as Functional Sensitivity, is the lowest concentration at which the analyte can not only be reliably detected but also measured with acceptable precision and accuracy. The LLOQ is the practical lower limit for reporting quantitative results [1] [11]. It is defined by meeting predefined performance goals for bias and imprecision, most commonly a coefficient of variation (CV) of 20% [9] [10].
Table 1: Core Definitions and Distinctions
| Parameter | Core Question | Definition | Key Characteristic |
|---|---|---|---|
| Limit of Blank (LoB) | What is the background noise? | Highest concentration expected from a blank sample [1]. | Describes assay background; not for sample measurement. |
| Analytical Sensitivity (LOD) | Can the analyte be detected? | Lowest concentration distinguished from the LoB [1] [10]. | Confers presence/absence; results are not quantitatively reliable. |
| Functional Sensitivity (LLOQ) | Can the analyte be measured reliably? | Lowest concentration measured with acceptable precision and accuracy [1] [10]. | Defines the practical reporting limit; results are quantitatively valid. |
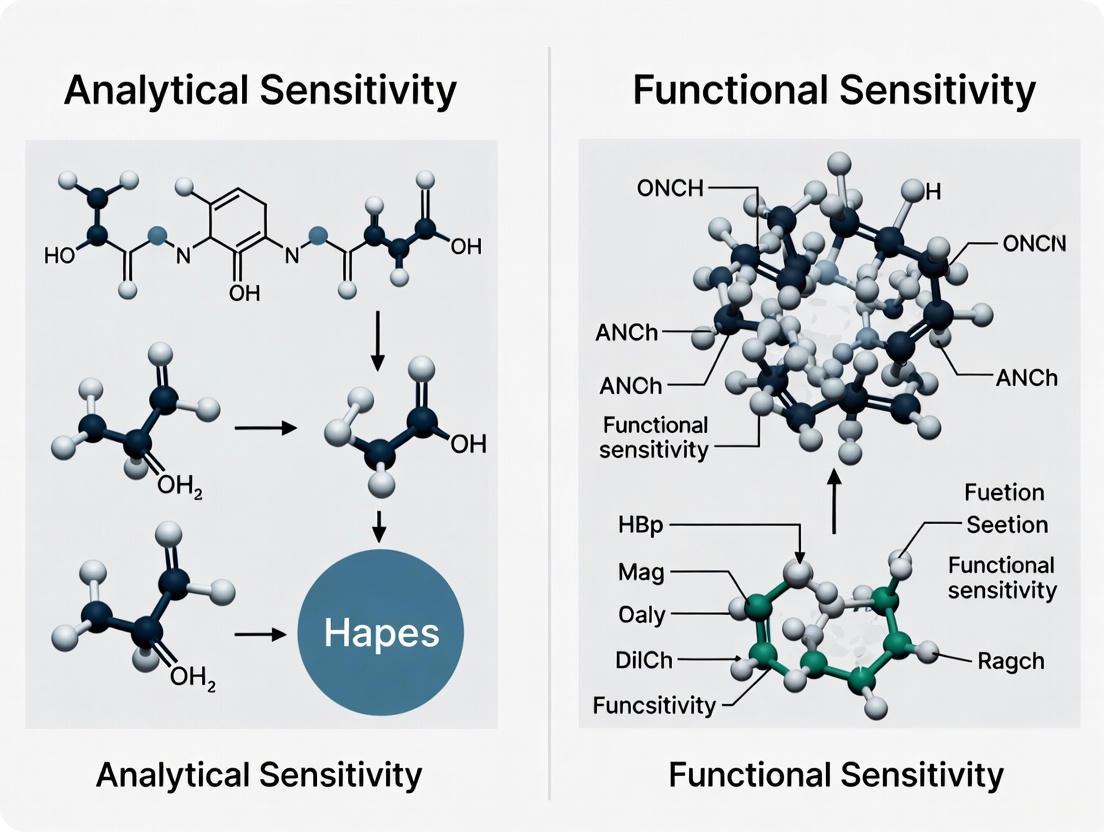
Analytical Sensitivity vs. Functional Sensitivity: A Performance Comparison
The conflation of analytical sensitivity (LOD) and functional sensitivity (LLOQ) is a common source of confusion. The critical difference lies in their clinical utility and reliability.
Analytical sensitivity, or LOD, has limited practical value because imprecision increases rapidly as analyte concentration decreases. At the LOD, the imprecision (CV) is so great that results are not reproducible enough for clinical decision-making [10]. Consequently, the LOD does not represent the lowest measurable concentration that is clinically useful.
Functional sensitivity was developed to address this limitation. Originally defined for Thyroid-Stimulating Hormone (TSH) assays, it is "the lowest concentration at which an assay can report clinically useful results," with "useful results" defined by good accuracy and a maximum CV of 20% [10]. This concept ensures that reported results are sufficiently precise to be actionable.
Table 2: Performance Characteristic Comparison
| Feature | Analytical Sensitivity (LOD) | Functional Sensitivity (LLOQ) |
|---|---|---|
| Primary Focus | Detection | Quantification |
| Defining Criterion | Distinguishes signal from LoB [1] | Meets predefined precision/accuracy goals (e.g., ≤20% CV) [10] |
| Clinical Utility | Low | High |
| Result Reliability | Qualitative (detected/not detected) | Quantitative (precise concentration) |
| Typical Position | Below the LLOQ | At or above the LOD [1] |
| Impact on Reporting | Results at or near LOD should not be reported as numerical values [10] | Defines the lowest concentration that can be reported as a precise numerical value |
The relationship between these parameters can be visualized as a continuum of confidence at low concentrations.
Experimental Protocols for Determining Functional Sensitivity
Determining the functional sensitivity (LLOQ) of an assay is an empirical process that requires testing samples with low concentrations of the analyte and evaluating their precision and accuracy.
- Define Performance Goals: Establish the precision goal (e.g., CV ≤ 20%) that represents the limit of clinical usefulness for the specific assay and its intended application.
- Source Low-Concentration Samples: Ideally, use several undiluted patient samples or pools of patient samples with concentrations spanning the target range (bracketing the expected LLOQ). If such samples are unavailable, reasonable alternatives include:
- Patient samples diluted to concentrations in the target range.
- Control materials with concentrations in or near the target range.
- Note: Use an appropriate diluent to avoid biasing the results.
- Execute Longitudinal Testing: Analyze the selected samples repeatedly over multiple independent runs (e.g., across different days or weeks, using different reagent lots) to capture day-to-day (inter-assay) precision.
- Calculate Imprecision and Determine LLOQ: For each sample, calculate the mean concentration and the CV. The functional sensitivity is the lowest concentration at which the CV meets the predefined goal (e.g., 20%). This can be determined directly if a tested sample meets the criterion or by interpolation between the CVs of two samples that bracket the goal.
- Source Blank Sample: Use a true zero-concentration sample with an appropriate sample matrix (e.g., a zero calibrator or processed matrix without the analyte).
- Replicate Testing: Assay a minimum of 20 replicates of the blank sample.
- Calculate Mean and Standard Deviation (SD): Determine the mean and SD of the analytical signals (e.g., counts, absorbance) from the blank replicates.
- Compute LOD: The LOD is the concentration equivalent to the mean of the blank plus 2 or 3 times the SD. For immunometric assays, it is typically
Mean_blank + 2(SD_blank)[10] [8].
Data Presentation: Comparative Experimental Results
The following table summarizes hypothetical experimental data from a validation study for a cardiac biomarker assay, illustrating how LOD and LLOQ are determined and why the LLOQ is the critical parameter for reporting.
Table 3: Hypothetical Experimental Data from a Cardiac Biomarker Assay Validation
| Sample Type | Nominal Concentration (pg/mL) | Mean Measured Concentration (pg/mL) | Standard Deviation (SD) | Coefficient of Variation (CV%) | Meets 20% CV Goal? |
|---|---|---|---|---|---|
| Blank | 0 | 0.5 | 0.2 | N/A | No |
| LoB (Calculated) | 0.8 | - | - | - | - |
| Low Sample A | 2.0 | 2.1 | 0.5 | 23.8% | No |
| Low Sample B | 3.0 | 3.2 | 0.6 | 18.8% | Yes |
| Low Sample C | 5.0 | 5.1 | 0.8 | 15.7% | Yes |
| Resulting Metrics | |||||
| LOD (Calculated) | ~1.6 pg/mL | ||||
| LLOQ (Functional Sensitivity) | 3.0 pg/mL |
Interpretation: While the assay can detect the analyte at concentrations as low as 1.6 pg/mL (LOD), the CV at this level is unacceptably high. The data shows that 3.0 pg/mL is the lowest concentration (LLOQ) where the CV falls below the 20% threshold, making it the lowest reportable and clinically usable value.
The Scientist's Toolkit: Essential Reagents and Materials
Successful determination of functional sensitivity requires careful selection of critical materials.
Table 4: Essential Research Reagent Solutions
| Item | Function in Validation | Critical Considerations |
|---|---|---|
| Blank Matrix | Used to determine LoB and background signal. | Must be commutable with patient specimens and truly analyte-free [1]. |
| Low-Level QC Materials / Patient Pools | Used to determine LOD and LLOQ by testing precision at low concentrations. | Pools of actual patient samples are ideal. If using spiked samples, the matrix should match the blank [1] [10]. |
| Appropriate Diluent | For preparing sample dilutions for the LLOQ study. | The diluent must not contain the analyte or interfere with the assay; routine sample diluents may bias results [10]. |
| Calibrators | Establish the standard curve for converting signal to concentration. | The lowest calibrator should be near the expected LLOQ. The curve should not be extrapolated below the LLOQ [11]. |
For researchers and drug development professionals, understanding the distinction between analytical sensitivity (LOD) and functional sensitivity (LLOQ) is critical for generating reliable and actionable data. While the LOD indicates the theoretical detection capability of an assay, the LLOQ defines its practical, quantitative utility. By adopting the experimental protocols outlined here and focusing validation efforts on establishing a robust LLOQ, scientists can ensure their analytical methods are truly "fit-for-purpose," providing the precision and accuracy necessary to drive confident decision-making in both drug development and clinical diagnostics.
In the development of diagnostic tests and therapeutic agents, a fundamental gap often exists between a technology's theoretical capability and its practical, clinical utility. Theoretical capability, often represented by metrics like analytical sensitivity, describes the optimum performance of a technology under ideal, controlled conditions. Clinical utility, in contrast, is measured by a test's or intervention's ability to positively influence real-world health outcomes by informing clinical decision-making, streamlining workflows, and ultimately improving patient care [12]. This guide objectively compares these concepts, focusing on the specific context of analytical sensitivity versus functional sensitivity, to provide researchers and drug development professionals with a framework for evaluating performance in biologically relevant matrices.
Defining the Concepts: Analytical vs. Functional Sensitivity
The distinction between analytical and functional sensitivity provides a foundational model for understanding the broader divide between theoretical capability and clinical utility in diagnostic testing.
Analytical Sensitivity, often termed the "detection limit," is a measure of theoretical capability. It describes the lowest concentration of an analyte that an assay can reliably distinguish from a blank sample with no analyte [10] [9]. It answers the question, "How low can you detect?" This metric is typically determined by measuring replicates of a zero-concentration sample and calculating the concentration equivalent to the mean signal plus a specific multiple (e.g., 2 or 3) of the standard deviation [10]. While crucial for understanding an assay's fundamental detection strength, its primary limitation is that it does not account for the precision or reproducibility of the measurement at these low levels. Consequently, a result at or near the analytical sensitivity may be detectable but not reproducible enough for clinical interpretation [10].
Functional Sensitivity is a key indicator of clinical utility. It is defined as the lowest analyte concentration that can be measured with a specific, clinically acceptable level of precision, often expressed as a coefficient of variation (CV) of 10% or 20% [10] [3] [9]. This concept was developed specifically to address the limitations of analytical sensitivity by answering the question, "How low can you report a clinically useful result?" [10]. It is determined by repeatedly testing patient samples or pools over multiple days and identifying the concentration at which the inter-assay CV meets the predefined precision goal [10] [3]. This metric ensures that results at the low end of the measuring range are not only detectable but also sufficiently reproducible to support reliable clinical decision-making.
Table 1: Core Conceptual Distinctions Between Analytical and Functional Sensitivity
| Feature | Analytical Sensitivity (Theoretical Capability) | Functional Sensitivity (Clinical Utility) |
|---|---|---|
| Definition | Lowest concentration distinguishable from background noise [10] [9] | Lowest concentration measurable with a defined, clinically acceptable precision [10] [3] |
| Primary Question | "Can the analyte be detected?" | "Is the result reproducible enough for clinical use?" |
| Key Determining Factor | Signal-to-noise ratio | Assay imprecision (CV%) |
| Typical Metric | Meanblank + 2SD [10] | Concentration at a CV of 10% or 20% [3] |
| Clinical Relevance | Limited; indicates detectability only | High; defines the lower limit of clinically reportable range [10] |
Performance Data and Experimental Comparison
The performance gap between theoretical and functional limits is consistently demonstrated in assay validation studies. The following data, drawn from recent research, quantifies this disparity.
A recent evaluation of the Sysmex HISCL hs-cTnT assay provides clear quantitative data on these performance characteristics [3]. The study followed rigorous protocols to establish the assay's limits and its functional performance at the 99th-percentile upper reference limit (URL), a critical clinical decision point for diagnosing myocardial infarction.
Table 2: Performance Data for the Sysmex HISCL hs-cTnT Assay [3]
| Performance Characteristic | Value | Protocol Summary |
|---|---|---|
| Limit of Blank (LOB) | 1.3 ng/L | Determined according to CLSI EP17-A2 guidelines using assay diluent [3]. |
| Limit of Detection (Analytical Sensitivity) | 1.9 ng/L | Determined according to CLSI EP17-A2 guidelines. Distinguishable from LOB with high probability [3]. |
| Functional Sensitivity (at 20% CV) | 1.8 ng/L | Determined by serial dilution of control reagents; 20 replicates tested to establish mean and CV%; value found by curve-fitting [3]. |
| Functional Sensitivity (at 10% CV) | 3.3 ng/L | Protocol as above, with a more stringent precision requirement [3]. |
| 99th Percentile URL (Overall) | 14.4 ng/L | Established using 1004 cardio-renal healthy individuals. Assay CV was below 10% at this level, confirming high-sensitivity status [3]. |
The data shows that while the assay can theoretically detect concentrations as low as 1.9 ng/L, its precision at that level is poor. For clinical use where a 10% CV is required, the reliably reportable limit is nearly 74% higher (3.3 ng/L). Furthermore, the clinical decision point (14.4 ng/L) is significantly higher, situated well within the assay's precise measurement range. This demonstrates that the clinically useful range is substantially narrower than the theoretically detectable range.
Experimental Protocol for Determination
The following workflow details the standard methodology for establishing these key metrics, as applied in the Sysmex study and other validation workflows [10] [3].
The Researcher's Toolkit: Essential Reagents and Materials
Successful validation of assay sensitivity requires specific, high-quality materials. The table below details key reagents and their functions based on the cited experimental protocols.
Table 3: Key Research Reagent Solutions for Sensitivity Validation
| Reagent / Material | Function in Validation | Example from Search Results |
|---|---|---|
| Blank Matrix / Diluent | Serves as the analyte-free sample for determining the Limit of Blank (LOB) and background signal [10]. | HISCL diluent used in determining LOB and for serial dilution in LoQ studies [3]. |
| Control Materials | Characterized samples with known, low analyte concentrations used for precision profiling and determining functional sensitivity [10]. | HISCL control reagents serially diluted to establish the precision profile and functional sensitivity [3]. |
| Calibrators | Solutions with precisely defined analyte concentrations used to establish the instrument's calibration curve [3]. | Sysmex HISCL uses a 6-point calibration curve (C0-C5) with human serum, stable for 30 days [3]. |
| Patient-Derived Samples/Pools | Undiluted or pooled serum from patients provides a biologically relevant matrix for assessing real-world performance and establishing reference limits [10]. | Used in the Sysmex study to establish the 99th percentile URL in a cohort of 1004 healthy individuals [3]. |
Implications for Drug Development and Clinical Research
The analytical/functional sensitivity paradigm extends to broader concepts in pharmaceutical development. Clinical Utility Assessments and Multi-Attribute Utility (MAU) analysis are formal frameworks used to weigh multiple factors—including efficacy, safety, biomarker data, and patient quality of life—into a single quantitative metric for decision-making on compound selection and dose/regimen optimization [13]. This moves beyond the theoretical "can it work?" to the practical "should it be advanced?" based on a holistic view of risk and benefit.
Similarly, the growing use of Real-World Evidence (RWE) underscores the importance of performance in real-world matrices. While Randomized Controlled Trials (RCTs) establish efficacy under ideal conditions (theoretical capability), RWE studies how interventions perform in routine clinical practice with heterogeneous patients, comorbidities, and variable adherence—directly assessing clinical utility [14] [15]. For diagnostic tests, a result must not only be accurate (clinical validity) but must also lead to an intervention that improves patient outcomes to possess true clinical utility [12].
The distinction between theoretical capability and clinical utility is critical for effective research and development. As demonstrated by the comparison between analytical and functional sensitivity, an assay's pure detection power is a poor predictor of its real-world value. True utility is defined by reproducible, reliable performance at clinically relevant decision thresholds within complex biological matrices. For researchers and drug developers, prioritizing functional performance and clinical utility from the early stages of design and validation is essential for creating diagnostic tests and therapies that deliver meaningful improvements to patient care.
In Vitro Diagnostics (IVDs) are critical medical devices used to perform tests on samples derived from the human body, providing essential information for disease diagnosis, monitoring, and treatment decisions [16]. The global regulatory landscape for IVDs is primarily governed by three distinct frameworks: the U.S. Food and Drug Administration (FDA) regulations, the European Union's In Vitro Diagnostic Regulation (IVDR), and the Clinical Laboratory Improvement Amendments (CLIA) in the United States. Each framework approaches performance evaluation with different requirements, oversight mechanisms, and philosophical underpinnings, creating a complex environment for manufacturers and researchers.
Performance evaluation serves as the cornerstone of all three regulatory systems, ensuring that IVD devices are safe, effective, and clinically valid. However, the specific requirements, terminology, and evidentiary standards vary significantly between these frameworks. Understanding these differences is particularly crucial when conducting research on performance metrics such as analytical sensitivity and functional sensitivity, as regulatory expectations directly influence study design, data collection, and validation methodologies. This guide provides a detailed comparison of how FDA, IVDR, and CLIA approaches performance evaluation, with special emphasis on sensitivity requirements to inform researchers, scientists, and drug development professionals.
Comparative Analysis of Regulatory Frameworks
The FDA, IVDR, and CLIA represent fundamentally different approaches to ensuring IVD quality and performance. The FDA employs a comprehensive premarket review process, the IVDR establishes a risk-based classification system with ongoing surveillance, and CLIA focuses primarily on laboratory operations and quality control rather than device-specific approval.
Table 1: Key Characteristics of IVD Regulatory Frameworks
| Characteristic | FDA (U.S.) | IVDR (EU) | CLIA (U.S.) |
|---|---|---|---|
| Regulatory Focus | Device safety and effectiveness [16] | Device performance and clinical benefit [17] [18] | Laboratory testing quality and accuracy [16] [19] |
| Primary Authority | U.S. Food and Drug Administration | Notified Bodies (designated by EU member states) | Centers for Medicare & Medicaid Services (CMS) [20] |
| Applicable Products | Commercially distributed IVD kits [19] | Commercially distributed IVDs and laboratory-developed tests [17] | Laboratory-developed tests (LDTs) and laboratory testing procedures [20] |
| Basis for Oversight | Risk-based classification (Class I, II, III) [16] | Risk-based classification (Class A, B, C, D) [21] | Test complexity (waived, moderate, high) [16] |
| Premarket Review | Required (510(k), PMA, or De Novo) [22] [16] | Required for most devices (Technical Documentation review) [21] | Not required for LDTs; laboratory accreditation required [20] |
| Clinical Evidence Requirements | Required for all IVDs; extent varies by classification [22] [21] | Performance Evaluation Report required for all classes [17] [18] | Not required for LDTs; analytical validation required [20] |
Table 2: Performance Evaluation Requirements Across Frameworks
| Requirement | FDA | IVDR | CLIA |
|---|---|---|---|
| Analytical Performance Studies | Comprehensive testing required [22] | Comprehensive testing required [18] | Internal validation required [19] |
| Clinical Performance Studies | Required; comparative studies with predicate device [22] | Required; clinical performance report mandatory [17] | Not formally required; clinical validity often not assessed [20] |
| Scientific Validity | Implicit in substantial equivalence determination [22] | Explicitly required and documented [18] | Not assessed [20] |
| Post-Market Surveillance | Adverse event reporting required [19] | Formal Post-Market Performance Follow-up (PMPF) required [17] [21] | Proficiency testing and quality control required [16] |
| Key Documentation | 510(k), PMA submission [16] | Performance Evaluation Plan, Performance Evaluation Report, Clinical Performance Report [17] | Validation records, quality control data, proficiency testing results [20] |
Regulatory Pathways for IVD Devices: This diagram illustrates the distinct classification and regulatory pathways under FDA, IVDR, and CLIA frameworks, highlighting their different risk-based approaches.
Performance Evaluation: Core Concepts and Methodologies
Analytical vs. Functional Sensitivity in Performance Evaluation
Understanding the distinction between analytical and functional sensitivity is fundamental to designing appropriate performance evaluation studies across regulatory frameworks. These related but distinct metrics serve different purposes in assessing device performance and clinical utility.
Analytical Sensitivity, often referred to as the limit of detection (LOD), represents the lowest concentration of an analyte that can be distinguished from background noise [10] [9]. This parameter establishes the fundamental detection capability of an assay under controlled conditions. The standard methodology for determining analytical sensitivity involves testing multiple replicates of a blank sample (containing no analyte) to establish the mean background signal and standard deviation. The analytical sensitivity is typically calculated as the concentration equivalent to the mean blank value plus two standard deviations for immunometric assays [10].
Functional Sensitivity represents the lowest concentration at which an assay can report clinically useful results with acceptable precision [10] [9]. Unlike analytical sensitivity, functional sensitivity incorporates precision requirements, typically defined as the concentration at which the assay achieves a coefficient of variation (CV) of ≤20% [10]. This metric better reflects real-world performance where precision limitations may render results clinically unreliable even at concentrations above the theoretical detection limit.
Table 3: Comparative Analysis of Sensitivity Metrics
| Characteristic | Analytical Sensitivity | Functional Sensitivity |
|---|---|---|
| Definition | Lowest concentration distinguishable from background [10] [9] | Lowest concentration measurable with ≤20% CV [10] |
| Primary Focus | Detection capability | Clinical utility and precision |
| Typical Methodology | Measurement of blank replicates to establish mean + 2SD [10] | Testing patient samples at multiple concentrations over time to establish precision profile [10] |
| Regulatory Emphasis | FDA and IVDR require demonstration [22] [18] | Often required for assays where low-end precision impacts clinical decisions [10] |
| Clinical Relevance | Limited - indicates detection potential but not necessarily reliable measurement [10] | High - indicates concentration range for clinically reportable results [10] |
| Common Applications | All quantitative IVDs [22] | Hormone assays, tumor markers, cardiac markers [10] |
Experimental Protocols for Sensitivity Determination
Protocol for Determining Analytical Sensitivity
Purpose: To establish the lowest concentration of an analyte that can be reliably distinguished from a blank sample with no analyte [10].
Materials and Reagents:
- Matrix-appropriate blank sample (true zero concentration)
- Calibrators with known analyte concentrations
- Assay reagents and controls
- Appropriate instrumentation
Procedure:
- Prepare a minimum of 20 replicates of the blank sample [10]
- Analyze all replicates in the same run under identical conditions
- Record measurement signals for each replicate (e.g., counts, optical density)
- Calculate mean signal and standard deviation of the blank measurements
- Compute analytical sensitivity as mean blank signal + 2 standard deviations [10]
- Convert signal to concentration using the assay calibration curve
Acceptance Criteria: The determined analytical sensitivity should meet or exceed manufacturer claims and be comparable to predicate devices for FDA submissions [22].
Protocol for Determining Functional Sensitivity
Purpose: To establish the lowest analyte concentration that can be measured with acceptable precision (typically ≤20% CV) for clinical use [10].
Materials and Reagents:
- Patient samples or pools with concentrations near expected functional sensitivity
- Matrix-appropriate diluent if sample dilution is required
- Assay reagents, calibrators, and controls
- Appropriate instrumentation
Procedure:
- Identify target concentration range based on preliminary data or package insert
- Obtain 3-5 patient samples or pools spanning the target concentration range [10]
- Analyze each sample in duplicate or triplicate over multiple runs (minimum 10-20 runs)
- Space analyses over different days (minimum 5-10 days) to capture inter-assay precision [10]
- Calculate mean, standard deviation, and coefficient of variation for each concentration level
- Plot CV versus concentration and determine the concentration where CV crosses 20%
- Verify with additional testing if necessary
Acceptance Criteria: Functional sensitivity should demonstrate ≤20% CV or a pre-specified precision goal appropriate for the assay's clinical application [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful performance evaluation requires carefully selected reagents and materials that meet regulatory standards and ensure experimental integrity.
Table 4: Essential Research Reagents for Performance Evaluation Studies
| Reagent/Material | Function | Key Considerations |
|---|---|---|
| Clinical Samples | Validation with real-world matrices | Must reflect intended use population; fresh specimens preferred over stored samples [22] |
| Interferent Panels | Specificity testing | Should include structurally similar compounds, common medications, endogenous substances [22] |
| Calibrators | Establishing measurement scale | Traceable to reference materials; matrix-matched to patient samples [10] |
| Quality Controls | Monitoring assay performance | Multiple concentration levels (low, medium, high); stable and well-characterized [10] |
| Matrix Components | Equivalence studies | Critical when comparing different sample types (serum vs. plasma); demonstrate minimal matrix effects [22] |
| Stability Materials | Establishing shelf life | Used in real-time and accelerated stability studies; support expiration dating claims [22] |
Regulatory Pathways and Their Impact on Performance Evaluation
FDA 510(k) Substantial Equivalence Pathway
The FDA 510(k) pathway requires manufacturers to demonstrate substantial equivalence to a legally marketed predicate device [22] [16]. This comparative approach heavily influences performance evaluation design, requiring head-to-head studies against the predicate device across multiple performance characteristics.
Performance Evaluation Emphasis:
- Analytical Performance: Comprehensive testing including precision, accuracy, sensitivity, specificity, and interference [22]
- Clinical Performance: Focus on positive percent agreement (PPA) and negative percent agreement (NPA) compared to predicate [22]
- Statistical Requirements: Adequate sample sizes to demonstrate non-inferiority with pre-specified confidence intervals [22]
Common Pitfalls: Underpowered studies, inadequate statistical justification, and unrepresentative clinical populations are frequent causes of FDA requests for additional information [22].
IVDR Performance Evaluation Process
The IVDR introduces a systematic, ongoing performance evaluation process consisting of three key elements: scientific validity, analytical performance, and clinical performance [18]. Unlike the FDA's predicate-based approach, IVDR requires direct demonstration of performance relative to the device's intended purpose.
Performance Evaluation Structure:
- Performance Evaluation Plan (PEP): Prospective plan outlining the approach to generating necessary evidence [17]
- Performance Evaluation Report (PER): Comprehensive report integrating all performance data [17]
- Clinical Performance Report (CPR): Detailed documentation of clinical performance evidence [17]
Ongoing Requirements: IVDR mandates continuous performance evaluation through Post-Market Performance Follow-up (PMPF), requiring regular updates to performance documentation [17].
CLIA Laboratory Validation Approach
CLIA takes a fundamentally different approach by regulating laboratory testing quality rather than device performance [16] [20]. Laboratories developing LDTs must establish assay performance characteristics but without the comprehensive premarket review required by FDA or IVDR.
Validation Requirements:
- Analytical Validation: Demonstration of precision, accuracy, reportable range, reference range, and sensitivity [19]
- Verification of FDA-Cleared Tests: Establishment of performance specifications for modified FDA-cleared assays [20]
- Quality Control: Ongoing monitoring through internal quality control and external proficiency testing [16]
Regulatory Developments: Recent FDA initiatives aim to increase oversight of LDTs, potentially aligning CLIA requirements more closely with traditional IVD regulations [20].
Sensitivity Concepts and Methodologies: This diagram illustrates the relationship between analytical and functional sensitivity, their distinct methodologies, and different regulatory applications.
The regulatory frameworks governing IVD performance evaluation continue to evolve, with increasing convergence on the need for robust clinical evidence while maintaining distinct philosophical approaches. Researchers and manufacturers should consider several strategic implications:
For Global Market Access:
- FDA submissions require rigorous comparative studies against predicate devices [22]
- IVDR mandates direct demonstration of clinical performance and scientific validity [18]
- CLIA focuses on laboratory process quality rather than device-specific claims [20]
For Sensitivity Studies:
- Analytical sensitivity establishes fundamental detection capability required by all frameworks [22] [18]
- Functional sensitivity demonstrates clinical utility, particularly important for assays with critical low-end performance requirements [10]
- Study designs must accommodate framework-specific statistical and methodological requirements
For Future Development: The increasing regulatory scrutiny of LDTs [20] and the emphasis on real-world evidence across all frameworks suggest continued evolution toward more standardized, evidence-based approaches to performance evaluation. Researchers should design studies with sufficient rigor to satisfy multiple regulatory requirements while generating scientifically valid data on device performance.
The Critical Role in Diagnostic Accuracy and Early Biomarker Detection
The accurate detection of protein biomarkers is a cornerstone of modern in vitro diagnostics (IVD), providing dynamic readouts of physiological states that are critical for monitoring diseases ranging from cancer to neurological disorders [23]. In clinical practice, the sensitivity of an immunoassay—its ability to detect minute quantities of an analyte—directly influences diagnostic accuracy and the potential for early disease detection. Substantial advancements in assay technology have led to the development of increasingly sensitive tests, broadly categorized into generations based on their detection capabilities [24]. First-generation assays provided initial testing capabilities but with limited sensitivity. Second-generation, or highly sensitive (hs) assays, offered improved sensitivity with functional sensitivity values between 0.15 and 0.2 ng/mL, making them the current most widely used tests in clinical practice. The latest development, third-generation ultrasensitive (ultra) assays, can detect proteins at extremely low levels, with a functional sensitivity of 0.06 ng/mL [24]. This evolution is particularly impactful in monitoring differentiated thyroid cancer (DTC), where thyroglobulin (Tg) measurement serves as the gold standard for detecting residual or recurrent disease [24]. This guide provides an objective comparison of these assay generations, focusing on their performance characteristics and clinical implications to inform researchers, scientists, and drug development professionals.
Analytical Comparison: Ultrasensitive vs. Highly Sensitive Assays
Performance Characteristics and Metrics
The critical difference between highly sensitive (hs) and ultrasensitive (ultra) assays lies in their detection limits. Functional sensitivity, defined as the lowest concentration measurable with acceptable precision (typically with a coefficient of variation <20%), represents the assay's clinical reliability in real-world settings [24]. In contrast, analytical sensitivity denotes the minimum detectable concentration under optimal conditions, reflecting the assay's technical detection limits [24].
Table 1: Direct Comparison of Highly Sensitive vs. Ultrasensitive Tg Assays
| Performance Parameter | Highly Sensitive (hsTg) Assay | Ultrasensitive (ultraTg) Assay |
|---|---|---|
| Representative Platform | BRAHMS Dynotest Tg-plus IRMA | RIAKEY Tg Immunoradiometric Assay |
| Analytical Sensitivity | 0.1 ng/mL | 0.01 ng/mL |
| Functional Sensitivity | 0.2 ng/mL | 0.06 ng/mL |
| Correlation with Stimulated Tg (R value) | 0.79 (overall) | 0.79 (overall) |
| Correlation in TgAb-Positive Patients (R value) | 0.52 | 0.52 |
| Optimal Cut-off for Predicting Stimulated Tg ≥1 ng/mL | 0.105 ng/mL | 0.12 ng/mL |
| Sensitivity at Optimal Cut-off | 39.8% | 72.0% |
| Specificity at Optimal Cut-off | 91.5% | 67.2% |
| Key Clinical Advantage | Higher specificity reduces false positives | Higher sensitivity enables earlier recurrence detection |
Clinical Performance Data
A 2025 study directly comparing these technologies demonstrated that while both assays show a strong correlation (R=0.79, P<0.01) with stimulated Tg levels, their clinical performance differs significantly [24]. The correlation was notably weaker in Tg antibody-positive patients (R=0.52) for both platforms, highlighting a shared limitation in the presence of interfering antibodies [24]. The ultrasensitive Tg assay demonstrated superior sensitivity (72.0% vs. 39.8%) in predicting stimulated Tg levels ≥1 ng/mL, but this came at the cost of reduced specificity (67.2% vs. 91.5%) compared to the highly sensitive assay [24]. This trade-off has direct clinical implications: the higher sensitivity of ultraTg may lead to earlier detection of potential recurrence, while its lower specificity may result in more frequent classifications of biochemical incomplete response [24].
Table 2: Clinical Outcomes Comparison Based on Assay Type
| Clinical Scenario | Highly Sensitive (hsTg) Assay Interpretation | Ultrasensitive (ultraTg) Assay Interpretation | Clinical Implications |
|---|---|---|---|
| 8 Discordant Cases (hsTg <0.2 ng/mL but ultraTg >0.23 ng/mL) | Suggests negative/low risk | Suggests elevated risk | 3 patients developed structural recurrence within 3.4-5.8 years |
| Response Classification in 2 Patients | Excellent response | Indeterminate or biochemical incomplete response | Altered follow-up strategy and patient management |
Technological Foundations and Methodologies
Experimental Protocols for Tg Assay Comparison
The comparative data presented in this guide primarily derives from a rigorous 2025 study conducted at Seoul National University Hospital [24]. The experimental methodology is outlined below:
Subject Population: The study included 268 individuals who underwent total thyroidectomy for differentiated thyroid cancer (DTC) and either radioiodine treatment or I-123 diagnostic scanning. Patients were enrolled when planning to undergo radioiodine treatment or an I-123 diagnostic scan between November 2013 and December 2018 [24].
Sample Collection: After patients provided informed consent, blood samples were collected for measurement of TSH, Tg, and TgAb levels using two different immunoradiometric assay (IRMA) kits. Unstimulated serum samples were collected after total thyroidectomy. Stimulated samples were obtained after TSH stimulation, performed either through levothyroxine withdrawal or intramuscular injection of recombinant human TSH (rhTSH) [24].
Assay Methods: For Tg measurement, two IRMA kits representing different generations of Tg assays were utilized:
- Second-generation Tg IRMA (hsTg): Dynotest Tg-plus kit (BRAHMS Diagnostic GmbH) with functional sensitivity of 0.2 ng/mL and analytical sensitivity of 0.1 ng/mL
- Third-generation Tg IRMA (ultraTg): RIAKEY Tg IRMA kit (Shinjin Medics) with functional sensitivity of 0.06 ng/mL and analytical sensitivity of 0.01 ng/mL [24]
Statistical Analysis: Reliability between hsTg and ultraTg assays was assessed using Pearson correlation coefficient. The diagnostic performance of unstimulated Tg levels in predicting positive stimulated Tg values was evaluated using functional and analytical sensitivities as cut-off thresholds. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated. Optimal cut-off values were determined using receiver operating characteristic (ROC) curve analysis [24].
Sensitivity Enhancement Techniques in Immunoassays
Efforts to enhance ELISA sensitivity have primarily focused on two key areas: optimizing capture antibody immobilization to improve biomarker retention and developing efficient signal amplification strategies to boost detection sensitivity [23]. Unlike nucleic acids, which can be amplified using PCR or isothermal amplification techniques, proteins lack an intrinsic amplification mechanism, making these optimization strategies crucial [23].
Surface Modification Strategies: Traditional passive adsorption of capture antibodies onto polystyrene microplates often results in random antibody orientation and partial denaturation, reducing the number of functionally active capture antibodies. To address this, several advanced strategies have been developed:
- Nonfouling surface modifications using synthetic polymers like polyethylene glycol (PEG) or polysaccharides such as dextran, chitosan, and hyaluronic acid can prevent non-specific protein adsorption [23].
- Antibody orientation strategies using Protein A, Protein G, or the biotin-streptavidin system ensure proper orientation of capture antibodies, significantly enhancing antigen accessibility and assay sensitivity [23].
- Covalent crosslinking provides permanent and stable attachment of antibodies to solid surfaces, preventing antibody loss during wash steps [23].
Signal Amplification Approaches: Digital ELISA represents a revolutionary advancement in ultrasensitive immunoassays, detecting proteins at ultra-low concentrations in the femtomolar range (fM; 10⁻¹⁵M) compared to nanomolar (nM; 10⁻⁹M) to picomolar (pM; 10⁻¹²M) levels in conventional ELISA [25]. This technology uses beads to isolate and detect single enzyme molecules in femtoliter-sized wells, allowing for orders of magnitude greater sensitivity than standard sandwich-based immunoassay techniques [25].
Figure 1: Enhanced Immunoassay Workflow with Sensitivity Optimization Strategies. This diagram illustrates the sequential steps in a sensitive immunoassay workflow, highlighting key technological enhancement strategies (red boxes) that improve detection capabilities at each stage.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Ultrasensitive Immunoassays
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Paramagnetic Beads | Solid support for antibody immobilization | Enable digital counting in single molecule arrays; higher surface area-to-volume ratio than traditional plates [25] |
| Protein A/Protein G | Antibody orientation | Binds Fc region of antibodies, ensuring uniform orientation and enhanced antigen accessibility [23] |
| Biotin-Streptavidin System | Antibody immobilization | Strong interaction ensures uniform, functional antibody state; requires biotinylation of capture antibody [23] |
| Polyethylene Glycol (PEG) | Nonfouling surface modification | Prevents non-specific protein adsorption; improves signal-to-noise ratio [23] |
| Polymer-Based Detection Systems | Signal amplification | Multiple peroxidase molecules and secondary antibodies attached to dextran polymer backbone increase sensitivity [23] |
| Chromogenic Substrates (DAB, NovaRed) | Signal generation | Produce colored product after incubation with enzyme labels; compatible with light microscopy [26] |
| Antigen Retrieval Buffers (e.g., citrate buffer) | Epitope unmasking | Breaks protein cross-links caused by fixation; essential for FFPE tissue analysis [26] |
| Blocking Reagents (BSA, casein, skim milk) | Reduce nonspecific binding | Occupies uncoated surface areas to minimize false-positive signals [23] |
Clinical Decision Pathway and Research Implications
Figure 2: Clinical Decision Pathway for Thyroid Cancer Monitoring. This diagram outlines the decision-making process for selecting and interpreting thyroglobulin assays in differentiated thyroid cancer (DTC) monitoring, highlighting the different performance characteristics and clinical implications of highly sensitive versus ultrasensitive testing approaches.
The choice between highly sensitive and ultrasensitive assays should be guided by specific clinical and research objectives. For routine monitoring of differentiated thyroid cancer patients with low to intermediate risk, highly sensitive assays provide sufficient sensitivity with excellent specificity, reducing the likelihood of false positives and unnecessary additional testing [24]. For high-risk patients or those with clinically suspicious cases where highly sensitive Tg falls below the cut-off but clinical suspicion remains, ultrasensitive assays may provide additional diagnostic value by detecting minimal residual disease earlier [24]. In research settings focused on biomarker discovery or early detection, ultrasensitive technologies offer the potential to identify novel low-abundance biomarkers and establish earlier disease detection windows [23] [25].
The emerging field of cell-free synthetic biology promises to further bridge the sensitivity gap between protein and nucleic acid detection. Recent developments such as expression immunoassays, CRISPR-linked immunoassays (CLISA), and T7 RNA polymerase-linked immunosensing assays (TLISA) demonstrate how programmable nucleic acid and protein synthesis systems can be integrated into ELISA workflows to surpass current sensitivity limitations [23]. By combining synthetic biology-driven amplification with traditional immunoassay formats, researchers are developing increasingly modular and adaptable diagnostic platforms capable of detecting protein biomarkers at concentrations previously undetectable in peripheral biofluids [25].
The evolution from highly sensitive to ultrasensitive immunoassays represents a significant advancement in diagnostic accuracy and early biomarker detection. While highly sensitive assays remain the standard in many clinical applications due to their robust performance and higher specificity, ultrasensitive technologies offer unprecedented detection capabilities that are reshaping diagnostic paradigms, particularly in neurology, oncology, and endocrinology. The trade-off between sensitivity and specificity must be carefully considered in both clinical practice and research applications. As synthetic biology and digital detection technologies continue to mature, the next generation of immunoassays promises to further dissolve the sensitivity barriers between protein and nucleic acid detection, potentially enabling earlier diagnosis and more precise monitoring across a spectrum of diseases.
From Theory to Practice: Methodologies for Assessing Sensitivity Across Assay Platforms
Standardized Protocols for Establishing LoD and LLOQ
In analytical science, the Limit of Detection (LoD) and Lower Limit of Quantitation (LLOQ or LoQ) are fundamental performance characteristics that define the capabilities of an analytical procedure. The LoD represents the lowest concentration of an analyte that can be reliably distinguished from zero, while the LLOQ is the lowest concentration that can be measured with acceptable precision and accuracy [1]. These parameters are essential for method validation across diverse fields including clinical diagnostics, pharmaceutical development, and environmental testing, providing critical information about the dynamic range and sensitivity of analytical methods [27].
Understanding the distinction between these parameters is crucial for proper method characterization. The LoD represents a detection capability, whereas the LLOQ represents a quantitation capability where predefined goals for bias and imprecision are met [1]. The LLOQ may be equivalent to the LoD or exist at a much higher concentration, but it can never be lower than the LoD [1]. This relationship becomes particularly important when establishing the reportable range of an assay, as results below the LLOQ but above the LoD may be detected but not quantified with sufficient reliability for analytical purposes [10].
Standardized Frameworks and Guidelines
Key Regulatory Guidelines
Two primary standardized frameworks govern the establishment of LoD and LLOQ: the Clinical and Laboratory Standards Institute (CLSI) EP17 guideline and the International Council for Harmonisation (ICH) Q2(R2) guideline [1] [28]. The CLSI EP17 guideline, titled "Evaluation of Detection Capability for Clinical Laboratory Measurement Procedures," provides a comprehensive approach specifically tailored for clinical laboratory measurements [28]. This protocol defines three critical parameters: Limit of Blank (LoB), LoD, and LLOQ, each with distinct definitions and statistical approaches for determination [1].
The ICH Q2(R2) guideline, "Validation of Analytical Procedures," offers a broader framework applicable to various analytical methods, particularly in pharmaceutical quality control [27] [28]. This guideline describes multiple approaches for determining detection and quantitation limits, including methods based on visual evaluation, signal-to-noise ratio, standard deviation of the blank, and standard deviation of the response relative to the slope of the calibration curve [27]. The choice between these frameworks depends on the intended application of the analytical method and regulatory requirements.
Table 1: Comparison of CLSI EP17 and ICH Q2(R2) Approaches for LoD and LLOQ Determination
| Characteristic | CLSI EP17 Protocol | ICH Q2(R2) Approaches |
|---|---|---|
| Primary Application | Clinical laboratory measurements | Pharmaceutical analysis |
| Key Parameters | LoB, LoD, LLOQ | LoD, LLOQ |
| Statistical Basis | Defined formulas based on blank and low-concentration sample distributions | Multiple approaches: visual evaluation, signal-to-noise, standard deviation of blank/response |
| Sample Requirements | 60 replicates for establishment, 20 for verification [1] | Varies by approach; typically 5-7 concentrations with 6+ replicates [27] |
| LoD Definition | Lowest concentration reliably distinguished from LoB [1] | Lowest amount detectable but not necessarily quantifiable as exact value [27] |
| LLOQ Definition | Lowest concentration meeting predefined bias and imprecision goals [1] | Lowest concentration quantifiable with acceptable precision and accuracy [27] |
Detailed Experimental Protocols
CLSI EP17 Protocol
The CLSI EP17 protocol employs a three-tiered approach involving the determination of LoB, LoD, and finally LLOQ [1]. This method requires testing blank samples (containing no analyte) and low-concentration samples (containing known low concentrations of analyte) in sufficient replication to capture expected performance variability.
Limit of Blank (LoB) Determination: The LoB is defined as the highest apparent analyte concentration expected to be found when replicates of a blank sample are tested [1]. The experimental protocol involves:
- Testing approximately 60 replicates of a blank sample using at least two different instruments and reagent lots
- Calculating the mean and standard deviation (SD) of the blank measurements
- Applying the formula: LoB = meanblank + 1.645(SDblank) [1]
- This establishes a one-sided 95% confidence limit, assuming a Gaussian distribution where 95% of blank measurements fall below this value
Limit of Detection (LoD) Determination: The LoD represents the lowest analyte concentration likely to be reliably distinguished from the LoB [1]. The experimental approach includes:
- Testing approximately 60 replicates of a sample with low analyte concentration
- Calculating the mean and standard deviation of these low-concentration measurements
- Applying the formula: LoD = LoB + 1.645(SD_low concentration sample) [1]
- This ensures that 95% of measurements at the LoD concentration exceed the previously established LoB
Limit of Quantitation (LLOQ) Determination: The LLOQ is established as the lowest concentration at which the analyte can be quantified with predefined levels of bias and imprecision [1]. Unlike LoD, LLOQ requires meeting specific performance goals for total error. If these goals are met at the LoD concentration, then LLOQ equals LoD; if not, higher concentrations must be tested until the goals are achieved [1].
The following diagram illustrates the complete CLSI EP17 workflow for establishing these fundamental parameters:
ICH Q2(R2) Approaches
The ICH Q2(R2) guideline provides four distinct approaches for determining LoD and LLOQ, offering flexibility based on methodological characteristics [27].
Visual Evaluation Approach: This subjective method involves analyzing samples with known concentrations of analyte and determining the minimum level at which the analyte can be reliably detected [27]. The experimental protocol typically employs:
- Five to seven concentration levels prepared from a known reference material
- Six to ten replicate determinations at each concentration level
- Binary scoring (detected/not detected) by analysts or instruments
- Statistical analysis using logistic regression to determine the concentration corresponding to 99% detection probability for LoD
Signal-to-Noise Ratio Approach: This method is applicable only when the analytical method exhibits measurable background noise [27]. The experimental design includes:
- Five to seven concentration levels with six or more replicates each
- Calculation of signal-to-noise ratio at each concentration (signal = measurement, noise = blank control)
- Establishment of LoD at a signal-to-noise ratio of 2:1 or 3:1
- Establishment of LLOQ at a signal-to-noise ratio of 10:1 or based on precision profiles
- Nonlinear modeling using four-parameter logistic curves for interpolation
Standard Deviation of the Blank Approach: This method utilizes the mean and standard deviation of blank samples to establish limits [27]. The protocol involves:
- Minimum of ten blank sample determinations in appropriate matrix
- Calculation of LoD and LLOQ using defined formulas:
- LoD = meanblank + 3.3(SDblank)
- LLOQ = meanblank + 10(SDblank)
Standard Deviation of Response and Slope Approach: This approach is particularly suitable for methods with calibration curves and minimal background noise [27]. The methodology includes:
- Analysis of samples at five concentrations in the expected LoD/LLOQ range
- Minimum of six determinations at each concentration level
- Calculation of LoD and LLOQ using the formulas:
- LoD = 3.3σ/slope
- LLOQ = 10σ/slope
- Where σ represents the standard deviation of the response and slope is the slope of the calibration curve
Table 2: Comparative Experimental Requirements for Different ICH Q2(R2) Approaches
| ICH Q2(R2) Approach | Minimum Sample Types | Replicates per Level | Statistical Method | Primary Applications |
|---|---|---|---|---|
| Visual Evaluation | 5-7 concentration levels | 6-10 | Logistic regression | Qualitative and semi-quantitative methods |
| Signal-to-Noise | 5-7 concentration levels + blanks | 6+ | Nonlinear modeling (4PL) | Methods with measurable background noise |
| SD of Blank | Blank samples | 10+ | Direct calculation | Methods with clean background |
| SD of Response/Slope | 5 concentration levels in low range | 6+ | Linear regression | Methods with calibration curves |
Comparative Experimental Data
Application in Molecular Diagnostics
In molecular diagnostics, particularly for pathogen detection, the empirical determination of LoD using probit analysis represents a robust approach [29]. This method involves testing multiple replicates across a dilution series of the target analyte and applying statistical analysis to determine the concentration at which 95% of samples test positive.
A recent study on human cytomegalovirus (hCMV) DNA detection using loop-mediated isothermal amplification (LAMP) technology demonstrated this approach [29]:
- Eight different hCMV DNA concentrations were tested with at least 24 replicates per concentration
- Results were scored as detected or not detected for each replicate
- Probit analysis was applied to determine the LoD as the concentration yielding 95% detection (C95)
- This empirical approach provides a statistically robust LoD estimate that accounts for methodological variability
Similar approaches have been applied to compare the analytical sensitivity of seven commercial SARS-CoV-2 automated molecular assays, highlighting how LoD values can vary significantly between different methodological platforms [30].
Case Study: Ultrasensitive PCR Assay
Research on JC virus (JCV) DNA detection in cerebrospinal fluid for diagnosing progressive multifocal leukoencephalopathy (PML) demonstrates the application of these principles in clinical validation [31]. An ultrasensitive multiplex quantitative PCR assay was developed with both LoD and LLOQ established at 10 copies per milliliter [31]. This validation included:
- Comprehensive determination of both LoD and LLOQ at the same concentration level
- Implementation as a reference method for clinical sample testing
- Application in longitudinal monitoring of virological burden in clinical trials
- Demonstration that meeting precision requirements at the detection limit allows LoD and LLOQ to coincide
Essential Research Reagent Solutions
The experimental protocols for establishing LoD and LLOQ require specific research reagents and materials tailored to the analytical method. The following table outlines essential solutions across different methodological approaches:
Table 3: Key Research Reagent Solutions for LoD/LLOQ Determination
| Reagent/Material | Function in LoD/LLOQ Studies | Application Context |
|---|---|---|
| Blank Matrix | Provides analyte-free background for LoB determination and background noise assessment | All methods; must be commutable with patient specimens [1] |
| Low-Concentration Calibrators | Used for testing samples near the expected LoD and LLOQ | CLSI EP17 protocol; should mimic actual sample matrix [1] |
| Reference Standards | Provide known analyte concentrations for preparing dilution series | All quantitative approaches; certified reference materials preferred |
| Quality Control Materials | Monitor assay performance during validation studies | All protocols; should span critical concentrations including LoD/LLOQ |
| Sample Diluents | Prepare dilution series for empirical determination | Critical selection; inappropriate diluents may bias results [10] |
Critical Considerations in Protocol Implementation
Method Selection and Fit-for-Purpose Validation
Selecting the appropriate protocol for establishing LoD and LLOQ requires careful consideration of the analytical method's characteristics and intended application [27]. The "fit-for-purpose" principle dictates that the validation approach should match the eventual use of the method, with more rigorous requirements for clinical decision-making compared to research applications [1].
Key considerations include:
- Matrix effects: Blank and low-concentration samples should be commutable with actual patient specimens to ensure realistic performance assessment [1]
- Instrumentation variability: LoD and LLOQ determination should incorporate multiple instruments and reagent lots when establishing performance characteristics [1]
- Total error requirements: LLOQ establishment must consider the total allowable error (bias + imprecision) required for clinical or regulatory purposes [10]
- Practical limitations: While CLSI EP17 recommends 60 replicates for establishment, practical constraints may require verification with fewer replicates (e.g., 20) [1]
Troubleshooting Common Challenges
Several common challenges arise during LoD and LLOQ determination that require methodological adjustments:
- High background noise: When blank samples produce significant signal, the signal-to-noise approach may be most appropriate [27]
- Non-Gaussian distributions: For methods where blank results don't follow normal distribution, non-parametric statistical methods should be employed [1]
- Limited sample availability: For methods with scarce matrices, creative approaches using diluted samples may be necessary while recognizing potential limitations [10]
- Discrepancies between approaches: When different methodologies yield substantially different LoD/LLOQ values, empirical testing with clinical samples may be needed to determine the clinically relevant limit
The relationship between different performance characteristics and their application to real-world analytical challenges can be visualized as follows:
Standardized protocols for establishing LoD and LLOQ provide essential frameworks for characterizing analytical method performance. The CLSI EP17 and ICH Q2(R2) guidelines offer complementary approaches with varying levels of rigor and applicability to different methodological challenges. Proper selection and implementation of these protocols require understanding both statistical principles and practical experimental considerations to ensure methods are fit for their intended purpose. As analytical technologies continue to evolve with increasing sensitivity demands, these standardized approaches provide the foundation for reliable method validation across diverse scientific disciplines.
In biomedical research and drug development, the accurate detection and quantification of biomarkers are paramount. The core challenge lies in measuring increasingly low-abundance targets—from rare genetic variants to single protein molecules—within complex biological matrices. This comprehensive guide objectively compares three foundational technology classes: Immunoassays, including ultra-sensitive platforms like Single Molecule Array (Simoa); the Polymerase Chain Reaction (PCR) and its digital derivatives; and Next-Generation Sequencing (NGS). The analysis is framed within the critical context of analytical sensitivity (the lowest concentration an assay can reliably detect) versus functional sensitivity (the lowest concentration an assay can measure with acceptable precision, often defined as ≤20% coefficient of variation) [32]. Understanding this distinction and the performance boundaries of each technology is essential for selecting the optimal tool for diagnosing diseases, monitoring treatment efficacy, and advancing precision medicine.
Immunoassays: Antibody-Based Protein Detection
Immunoassays are designed for the detection of proteins and other antigens. Their fundamental principle relies on the specific binding of an antibody to a target antigen. The most common format, the sandwich ELISA (Enzyme-Linked Immunosorbent Assay), immobilizes a capture antibody on a solid substrate, which binds the target protein from a sample. A detection antibody, conjugated to an enzyme like Horseradish Peroxidase (HRP), then binds to the captured protein. The enzyme catalyzes a colorimetric, fluorescent, or chemiluminescent reaction, generating a signal proportional to the target concentration [33]. The sensitivity of standard immunoassays typically ranges from 1 pg/mL to 10 ng/mL [33].
Recent advancements have pushed these limits. Single Molecule Array (Simoa) technology represents a revolutionary ultra-sensitive immunoassay. It uses antibody-coated beads to capture single protein molecules, which are then labeled with an enzymatic detection antibody. The beads are isolated in femtoliter-sized wells, creating a confined space where the enzyme converts a substrate into a highly concentrated fluorescent product that is easily imaged. This single-molecule counting enables detection in the femtomolar (fg/mL) range, offering a sensitivity up to 1,000 times greater than conventional ELISA [33] [32].
PCR and Digital PCR: Nucleic Acid Amplification
The Polymerase Chain Reaction (PCR) is a cornerstone of molecular biology for detecting nucleic acids (DNA and RNA). It enables the in vitro enzymatic amplification of a specific DNA sequence, exponentially copying it through repeated heating and cooling cycles. Quantitative PCR (qPCR) allows for the real-time monitoring of this amplification using fluorescent probes, providing quantitative data on the initial amount of the target sequence [34] [35].
Digital PCR (dPCR) is a refined approach that partitions a single PCR reaction into tens of thousands of nanoscale reactions (e.g., in droplets or microwells). This partitioning follows a Poisson distribution, so that some partitions contain one or more target molecules while others contain none. After endpoint PCR amplification, the fraction of positive partitions is counted, allowing for absolute quantification of the target nucleic acid without a standard curve. This makes dPCR exceptionally robust and sensitive, capable of detecting rare mutations with a variant allele frequency as low as 0.1% and enabling true single-molecule detection [34].
Next-Generation Sequencing (NGS): Comprehensive Genomic Interrogation
Next-Generation Sequencing (NGS) represents a paradigm shift from targeted analysis to hypothesis-free, massive parallel sequencing. NGS technologies simultaneously determine the nucleotide sequence of millions to billions of DNA fragments, providing comprehensive genomic, transcriptomic, and epigenomic profiles [36].
A key advantage of NGS is its unparalleled discovery power. While qPCR and dPCR are limited to detecting known, pre-defined sequences, NGS can identify novel genes, transcripts, splice variants, and complex structural rearrangements without prior knowledge [35]. It offers single-base resolution, allowing it to detect single nucleotide polymorphisms (SNPs), insertions/deletions (indels), copy number variations (CNVs), and chromosomal rearrangements in a single assay. Compared to Sanger sequencing, the previous gold standard, NGS provides massively higher throughput, greater sensitivity for low-frequency variants (down to ~1%), and is more cost-effective for analyzing large numbers of genes or samples [36] [37].
Comparative Performance Data
The following tables synthesize key performance metrics and characteristics for the three technologies, based on current literature and commercial platform data.
Table 1: Quantitative Comparison of Key Performance Metrics
| Technology | Typical Sensitivity (Lower Limit of Detection) | Sample Volume per Replicate | Multiplexing Capacity | Key Instrument |
|---|---|---|---|---|
| Standard ELISA | 1 - 100 pg/mL [33] | 50 - 100 µL [33] | Low (single-plex) | Microplate Reader |
| Simoa | 10 fg/mL - 1 pg/mL [33] (465x more sensitive than ELISA) [33] | ~125 µL [33] | Medium (~6 targets without sensitivity loss) [33] | Dedicated Simoa HD-X Analyzer [33] [32] |
| qPCR | Varies by target; less sensitive than dPCR [34] | 10 - 25 µL (for immuno-qPCR) [33] | Low to Medium | Real-time PCR Thermocycler |
| Digital PCR (dPCR) | Can detect single molecules; Rare mutation detection down to 0.1% VAF [34] | Varies by platform | Limited (challenging for high-plex) [34] | Droplet or Chip-based dPCR System |
| Targeted NGS | Down to 1% Variant Allele Frequency [35] | Varies by library prep | High (100s-1000s of targets in a single run) [35] [36] | Illumina, PacBio, Oxford Nanopore Sequencers [36] |
Table 2: Functional and Application-Based Comparison
| Aspect | Immunoassays (e.g., Simoa) | PCR/dPCR | NGS |
|---|---|---|---|
| Primary Target | Proteins, Antigens [33] | Specific Nucleic Acid Sequences [34] [35] | Entire Genomes, Exomes, Transcriptomes [36] |
| Throughput | Medium to High (plate-based) [33] | High for targeted analysis | Highest (massively parallel) [36] |
| Discovery Power | Low (requires specific antibodies) | Low (requires known sequence for primers) | Highest (hypothesis-free; detects novel variants) [35] [36] |
| Quantification | Relative or absolute (with standard curve) | Absolute (dPCR), Relative (qPCR) | Absolute (count-based) [35] |
| Best Applications | Protein biomarkers, cytokine signaling, pharmacokinetics [33] [38] | Viral load, gene expression, rare mutation detection [34] | Comprehensive genomic profiling, liquid biopsy, novel biomarker discovery [36] [39] |
Experimental Protocols and Validation
Simoa Assay Protocol for Plasma Protein Detection
The following workflow details a method used to measure SARS-CoV-2 Nucleoprotein (N) in plasma, demonstrating the platform's application for low-abundance protein detection in complex fluids [32].
- Reagent Preparation: The Simoa SARS-CoV-2 N Protein Advantage Kit reagents are brought to room temperature. The assay uses antibody-coated magnetic beads and a biotinylated detection antibody specific to the target.
- Sample and Reagent Incubation: 125 µL of plasma sample is mixed with the capture beads and detection antibody. This mixture is incubated to allow the formation of the antibody-antigen "sandwich" complex [33] [32].
- Washing and Labeling: The beads are magnetically captured and washed to remove unbound material. An enzyme label (Streptavidin-β-galactosidase, SβG) is added, which binds to the biotinylated detection antibody.
- Single-Molecule Array Loading: The labeled beads are resuspended and loaded into a consumable disc containing ~240,000 femtoliter-sized wells. The wells are designed to hold only one bead each. An oil layer is added to seal the wells and isolate them from each other [33].
- Signal Detection and Imaging: A fluorescent substrate (resorufin β-D-galactopyranoside) is added. If a bead in a well has captured a target protein, the associated SβG enzyme converts the substrate into a concentrated fluorescent signal. A built-in fluorescence microscope images the entire array to count the number of "on" wells (containing a bead with a protein molecule) versus "off" wells (containing a bead without a protein molecule) [33] [32].
- Data Analysis: The average enzymes per bead (AEB) is calculated, and the protein concentration is determined by interpolating from a standard curve run in parallel [32].
Key Validation Data: In a study comparing Simoa to other immunoassays for SARS-CoV-2 N protein, Simoa demonstrated a functional sensitivity (limit of detection, LOD) of 0.15 ng/L in plasma, significantly lower than a standard ELISA (LOD of 10 ng/L) and an electrochemiluminescence immunoassay (ECLIA, LOD >0.40 COI) [32].
Digital PCR Workflow for Rare Mutation Detection
This protocol, often referred to as BEAMing (Bead, Emulsion, Amplification, and Magnetics), highlights the extreme sensitivity of dPCR for detecting rare genetic variants like circulating tumor DNA (ctDNA) [34].
- Sample Preparation: Genomic DNA, including the wild-type and suspected mutant sequences, is extracted.
- Emulsion PCR: The DNA sample is mixed with PCR reagents and magnetic beads coated with primer sequences. This mixture is emulsified into millions of individual water-in-oil droplets, each acting as a separate microreactor. The dilution is designed so that most droplets contain either zero or one DNA molecule [34].
- Amplification: The emulsion is subjected to PCR thermocycling. If a droplet contains a DNA molecule, it is amplified, and the copies bind to the bead within that same droplet.
- Bead Recovery and Hybridization: After amplification, the emulsion is broken, and the beads are purified. The beads, now covered with amplified DNA, are hybridized with fluorescent probes specific to the wild-type sequence and the mutant sequence.
- Flow Cytometry: The beads are analyzed by flow cytometry. Beads with wild-type DNA fluoresce in one color, beads with mutant DNA fluoresce in another, and beads with no DNA show no fluorescence [34].
- Quantification by Poisson Statistics: The number of mutant and wild-type beads is counted. The concentration of the original mutant DNA is calculated using a Poisson model to account for partitions with zero, one, or multiple molecules, achieving a limit of detection for rare mutations as low as 0.01% [34].
Targeted NGS Panel for Comprehensive Genomic Profiling
Targeted NGS focuses on sequencing specific regions of interest (e.g., a panel of cancer-related genes), providing deep coverage and high sensitivity across multiple targets simultaneously [36] [37].
- Library Preparation: Fragmented genomic DNA is used as input. Adapters containing sequencing motifs and sample-specific barcodes (indices) are ligated to the fragments, creating a "library." For targeted sequencing, the library is hybridized with biotinylated probes designed to capture the genes of interest. The captured fragments are purified and amplified [37].
- Cluster Amplification: The library is loaded onto a flow cell. For Illumina platforms, each fragment binds to a complementary adapter on the flow cell surface and is amplified in situ through bridge amplification to form clusters, each containing thousands of identical copies of the original fragment [36].
- Sequencing by Synthesis: The flow cell is placed in the sequencer. Fluorescently labeled, reversible-terminator nucleotides are added. As each nucleotide is incorporated into the growing DNA chain, its fluorescent signal is imaged, determining the base identity for each cluster across millions of clusters in parallel [36].
- Data Analysis and Variant Calling: The generated short reads are aligned to a reference human genome. Bioinformatics pipelines then identify and filter variants (SNPs, indels, etc.) based on sequencing quality, depth of coverage, and other parameters. This process can detect variants with a variant allele frequency down to 1-5% [36] [37].
Validation Data: A study assessing the clinical utility of NGS demonstrated 100% concordance with Sanger sequencing in detecting 119 known mutations across 20 disease genes, confirming its high analytical sensitivity and specificity for clinical application [37].
Technology Selection Workflow
The following diagram illustrates the decision-making process for selecting the most appropriate technology based on the research question and target type.
Research Reagent Solutions
This table outlines essential materials and reagents required for implementing the discussed technologies.
Table 3: Key Research Reagents and Their Functions
| Technology | Essential Reagent | Function | Example from Literature |
|---|---|---|---|
| Simoa | Capture Antibody-Coated Beads | Solid-phase for immobilizing target protein | Simoa SARS-CoV-2 N Protein Advantage Kit [32] |
| Biotinylated Detection Antibody | Binds captured protein for enzymatic labeling | Simoa SARS-CoV-2 N Protein Advantage Kit [32] | |
| Streptavidin-β-Galactosidase (SβG) | Enzyme label for signal amplification | Simoa HD-1 Assay Kit [33] | |
| dPCR | TaqMan Probes | Fluorescently labeled probes for target-specific detection during amplification | BEAMing RT-PCR [34] |
| Microfluidic Droplet Generator Oil | Creates partitions for individual reactions | Droplet Digital PCR [34] | |
| Targeted NGS | Hybridization Capture Probes | Biotinylated oligonucleotides to enrich specific genomic regions | SOLiD Fragment Library Oligo Kit [37] |
| Library Adapters with Barcodes | Enable sequencing and multiplexing of samples | ABI SOLiD Library [37] |
The choice between advanced immunoassays, PCR/dPCR, and NGS is not a matter of which technology is superior, but which is most appropriate for the specific biological question and analytical requirement. Immunoassays like Simoa are unparalleled for ultra-sensitive, single-molecule protein detection. PCR and dPCR offer robust, absolute quantification of nucleic acids, with dPCR providing the highest sensitivity for rare variant detection in targeted applications. NGS stands alone in its ability to perform unbiased discovery and comprehensively profile hundreds to thousands of genomic targets simultaneously.
The trend in biomedical research is toward multi-omics integration. The most powerful diagnostic and research strategies will likely combine these technologies, such as using NGS for novel biomarker discovery and Simoa or dPCR for ultrasensitive, longitudinal monitoring of validated targets. By understanding the distinct sensitivity profiles, strengths, and limitations of each toolkit, researchers and drug developers can make informed decisions that accelerate scientific discovery and the development of new therapeutics.
Surface Plasmon Resonance (SPR) biosensors have established themselves as powerful analytical tools for real-time, label-free detection of molecular interactions. Their utility spans critical applications from disease diagnosis to drug development. The performance of these biosensors is fundamentally governed by two distinct yet complementary concepts: analytical sensitivity and functional sensitivity. Analytical sensitivity, often described as the lowest concentration that can be distinguished from background noise, represents the theoretical detection limit of an assay [10] [9]. In contrast, functional sensitivity is a more practical metric, defined as the lowest analyte concentration that can be measured with a specified level of precision, typically a coefficient of variation (CV) ≤ 20%, ensuring clinically useful results [10] [9]. This distinction is paramount for researchers and drug development professionals who must select appropriate sensing platforms for their specific needs, balancing ultimate detection limits with the reproducibility required for reliable decision-making.
The integration of artificial intelligence (AI) with SPR biosensing is pushing these performance boundaries further. AI-enhanced assays are now enabling more sophisticated data analysis, predictive modeling, and automated optimization of sensing parameters. This review provides a comparative analysis of emerging SPR platforms, evaluates their performance against traditional alternatives, and examines how AI is transforming biosensor capabilities from mere detection to intelligent analysis.
Performance Comparison of Advanced SPR Biosensor Configurations
Recent research has focused on enhancing SPR biosensor performance through novel material combinations and structural innovations. The performance of a biosensor is quantified through several key parameters: sensitivity (the change in sensor output per unit change in refractive index, often expressed in °/RIU), detection accuracy (DA), figure of merit (FOM), and limit of detection (LOD) [40] [41]. The choice of prism material, plasmonic metal, and two-dimensional (2D) transition metal dichalcogenides (TMDCs) significantly influences these outcomes.
Table 1: Performance Comparison of Heterostructure SPR Biosensors for SARS-CoV-2 Detection
| Sensor Configuration | Sensitivity (°/RIU) | Detection Accuracy | Figure of Merit (FOM) | Quality Factor (/RIU) |
|---|---|---|---|---|
| CaF₂/TiO₂/Ag/BP/Graphene/Sensing-layer | 390° | 0.464 | 87.95 | 92.86 |
| BK7/ZnO/Ag/Si₃N₄/WS₂/Sensing-layer [41] | 342.14° (Blood cancer) | - | 124.86 [41] | - |
| BK7/Ag/MoS₂/WS₂/WSe₂ [40] | 142° | - | - | - |
| BK7/Ag/PtSe₂/WS₂ [40] | 194° | - | - | - |
| Prism/Ag/Au/WS₂/Graphene [40] | 182.5° | - | - | - |
| BK7/MoS₂/h-BN/Graphene [40] | 194.12° | - | - | - |
The data reveal that configurations utilizing combinations of 2D materials like Black Phosphorus (BP) and Graphene with silver (Ag) as the plasmonic metal achieve superior performance [40]. The highest sensitivity was reported for a CaF₂ prism with TiO₂ adhesion layer, Ag, BP, and Graphene, showcasing the benefit of optimized heterostructures [40].
Table 2: SPR Biosensor Performance for Cancer Cell Detection
| Cancer Cell Type | Sensor Configuration | Sensitivity (°/RIU) | FOM (RIU⁻¹) |
|---|---|---|---|
| Blood Cancer (Jurkat) | BK7/ZnO/Ag/Si₃N₄/WS₂ | 342.14° | 124.86 |
| Cervical Cancer (HeLa) | BK7/ZnO/Ag/Si₃N₄/WS₂ | 222.01° | 80.66 |
| Skin Cancer (Basal) | BK7/ZnO/Ag/Si₃N₄/WS₂ | 212.85° | 77.51 |
For cancer detection, the incorporation of TMDCs such as WS₂ demonstrates high sensitivity in distinguishing cancerous from healthy cells [41]. The variability in sensitivity for different cell types underscores the importance of tailoring the biosensor design to the specific target analyte and its refractive index properties.
Experimental Protocols for High-Performance SPR
The superior performance of these advanced SPR sensors is validated through rigorous experimental protocols. Numerical analysis is primarily performed using the Transfer Matrix Method (TMM) for modeling the reflectance curves and determining resonance angles and minimum reflectance intensities [40]. To analyze the electric field intensity at the sensor interface, the Finite-Difference Time-Domain (FDTD) approach is utilized [40]. The performance parameters are then calculated as follows:
- Sensitivity: The shift in resonance angle per unit change in the refractive index of the sensing medium (Δθ/ΔRIU) [40] [41].
- Detection Accuracy (DA): Calculated as the ratio of the resonance angle shift to the full width at half maximum (FWHM) of the resonance curve.
- Figure of Merit (FOM): Often defined as the sensitivity divided by the full width at half maximum (FWHM) of the resonance dip [41].
- Quality Factor: Another metric that relates sensitivity to the resonance width.
For biomolecular interaction studies, such as the binding of SARS-CoV-2 spike protein to its receptor, varying concentrations (0–1000 nM) of ligands and analytes are introduced to the sensing surface to observe binding kinetics and determine the limit of detection [40].
The Analytical vs. Functional Sensitivity Framework in Biosensor Validation
Understanding the distinction between analytical and functional sensitivity is critical for interpreting biosensor performance data and aligning platform selection with application requirements.
This conceptual framework highlights a critical reality: a biosensor's functional sensitivity often lies at a significantly higher concentration than its analytical sensitivity [10]. For instance, an assay might have an analytical sensitivity of 0.3 µg/dL but a functional sensitivity of 1.0 µg/dL, establishing the latter as the lower limit for clinically reportable results [10]. This ensures that results at the reporting limit are sufficiently reproducible for meaningful clinical or research interpretation, preventing the potential misreading of noise-based fluctuations as significant concentration differences.
AI-Enhanced Assays: Transforming Data into Insight
The integration of Artificial Intelligence (AI) into biosensing represents a paradigm shift from data collection to intelligent analysis. AI and machine learning algorithms are being deployed to enhance nearly every aspect of biosensor operation. According to the 2025 AI Index Report, AI is increasingly embedded in everyday life and business, with 78% of organizations reporting AI use in 2024, a significant increase from 55% the year before [42]. In biosensing, this translates to several key advancements:
- Predictive Modeling and Optimization: AI algorithms can predict optimal sensor configurations and material combinations, reducing the need for extensive trial-and-error experimentation. This is crucial for designing sensors for novel biomarkers or complex sample matrices.
- Data Analysis and Noise Reduction: Machine learning models excel at identifying subtle patterns in complex sensorgram data, enabling them to differentiate specific binding signals from non-specific background noise, effectively improving the signal-to-noise ratio and functional sensitivity [42].
- Multi-analyte Sensing and Deconvolution: In complex biological samples, AI can deconvolute signals from multiple simultaneous interactions, allowing for multiplexed detection without physical separation of analytes.
- Workflow Integration and Automation: AI agents are being scaled in business functions, including IT and knowledge management, which can streamline the data management and analytical workflows associated with running biosensor assays [43]. High-performing organizations are nearly three times as likely to have fundamentally redesigned individual workflows to incorporate AI [43].
The impact of AI is not just incremental; it enables a fundamental redesign of how biosensing data is generated, interpreted, and acted upon, moving the field toward more predictive, personalized, and automated diagnostic platforms.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and operation of high-performance SPR biosensors rely on a carefully selected set of materials and reagents. The choice of each component is deliberate, aimed at maximizing sensitivity, specificity, and stability.
Table 3: Key Research Reagent Solutions for SPR Biosensor Development
| Material/Reagent | Function in SPR Biosensor | Example Application |
|---|---|---|
| Plasmonic Metals (Ag, Au) | Generate surface plasmon waves; Ag offers higher sensitivity, Au provides better stability and biocompatibility [40]. | Metal film in Kretschmann configuration. |
| 2D TMDCs (WS₂, MoS₂, WSe₂, MoSe₂) | Enhance light-matter interaction due to high absorption; increase binding surface area; improve detection stability [40] [41]. | Coating on metal film to boost sensitivity and FOM. |
| Graphene | Protects metal layer from oxidation; provides large surface area with π–π stacking for biomolecule adsorption [40]. | Top layer in heterostructure for probe immobilization. |
| Black Phosphorus (BP) | High carrier mobility and tunable direct bandgap; significantly enhances sensor sensitivity [40]. | Sensitizing layer in high-performance heterostructures. |
| Metal Oxides (ZnO, TiO₂, Si₃N₄) | Act as adhesion layers; modify the dielectric environment; can enhance the electric field and protect the metal layer [40] [41]. | Interface layer between prism and metal. |
| Capture Probes (Antibodies, Aptamers) | Provide specificity by binding to the target analyte (e.g., viral protein, cancer biomarker). | Immobilized on sensor surface for selective detection. |
| Microfluidic Components | Enable precise control and delivery of sample and reagents over the sensor surface for real-time, label-free analysis [44]. | Integrated chips for automated fluid handling. |
The landscape of SPR biosensing is being reshaped by two powerful, converging trends: sophisticated nanomaterial engineering and the integration of artificial intelligence. The comparative data presented in this guide clearly demonstrates that heterostructures incorporating 2D materials like BP, Graphene, and WS₂ consistently outperform conventional metal-only sensors in terms of sensitivity and figure of merit. However, raw sensitivity is only part of the story. A rigorous evaluation of biosensor performance must consider the crucial distinction between analytical sensitivity (detection limit) and functional sensitivity (practical utility), with the latter defining the true lower limit of reportable results.
Looking forward, AI-enhanced assays are set to amplify these advancements further. By optimizing sensor design, interpreting complex data, and automating workflows, AI is transforming SPR from a powerful detection tool into an intelligent analytical system. For researchers and drug development professionals, this means that emerging SPR platforms offer unprecedented capabilities for sensitive, specific, and reliable detection of biomarkers, accelerating diagnostics and therapeutic development. The future of biosensing lies not just in sharper signals, but in smarter systems.
The diagnosis of cancers within the central nervous system (CNS), including primary brain tumors, brain metastases (BM), and leptomeningeal metastases (LM), presents a unique set of clinical challenges. The blood-brain barrier (BBB) significantly limits the release of tumor-derived biomarkers into the peripheral circulation, rendering plasma-based liquid biopsies less sensitive for CNS malignancies [45]. Consequently, diagnosis has often relied on invasive neurosurgical procedures to obtain tumor tissue or cerebrospinal fluid (CSF) for cytological analysis. However, CSF cytology, while the traditional gold standard for conditions like LM, is notoriously insensitive, with a single test yielding a diagnostic sensitivity of only approximately 55-71% [46] [47]. This clinical need has driven the development of molecular liquid biopsy assays using CSF, which offer a minimally invasive method to detect tumor-derived genetic material with the potential for greater sensitivity and objective genomic profiling.
This case study focuses on the analytical and clinical validation of the "Belay Summit" assay, a novel CSF liquid biopsy test designed for the genomic profiling of CNS tumors. We will objectively compare its performance against established and emerging diagnostic alternatives, delving into the critical distinction between its analytical sensitivity (the assay's inherent ability to detect a biomarker at low concentrations) and its functional sensitivity (its performance in a real-world clinical setting with unselected patient samples). The data and methodologies presented herein are intended to inform researchers, scientists, and drug development professionals about the evolving landscape of CNS tumor diagnostics.
The Belay Summit Assay: Methodology and Analytical Performance
The Belay Summit assay is a tumor-derived DNA–based genomic profiling test that utilizes CSF to inform the diagnosis of both primary and metastatic CNS tumors [45]. Its development was motivated by the need for a less invasive and more accurate alternative to surgical biopsies and cytology.
Core Experimental Protocol and Workflow
The analytical validation of the Belay Summit assay followed a rigorous methodology to establish its performance characteristics. The general workflow is summarized in the diagram below.
Sample Acquisition and Processing: CSF samples are obtained via lumbar puncture, intraoperative extraction, or from an Ommaya reservoir [48]. A typical sample volume is 2-5 mL, though the assay can function on lower volumes [49]. Cell-free DNA (cfDNA) is extracted from the CSF using commercial kits, such as the MagMAX Cell-Free DNA Isolation Kit, which involves a multi-step process of lysis, binding to magnetic beads, washing, and elution [47].
Genomic Analysis: The isolated cfDNA undergoes targeted next-generation sequencing (NGS). The analytical validation established key performance metrics using this protocol across a range of genomic alterations, including single-nucleotide variants (SNVs), multi-nucleotide variants (MNVs), insertions/deletions (indels), and chromosomal arm-level aneuploidy [45].
Key Research Reagent Solutions
Table 1: Essential Research Materials for CSF Liquid Biopsy Protocols.
| Research Reagent | Function in the Workflow | Specific Example / Kit |
|---|---|---|
| cfDNA Isolation Kit | Isolation and purification of cell-free DNA from CSF samples. | MagMAX Cell-Free DNA Isolation Kit [47] |
| DNA Quantitation Assay | Accurate measurement of cfDNA concentration post-extraction. | Quant-iT PicoGreen dsDNA assay [47] |
| Targeted NGS Panel | Library preparation and sequencing of target genomic regions. | Custom 131-gene panel (e.g., Belay Summit assay) [45] [48] |
| PCR Reagents | Detection and quantification of specific mutations (used in ddPCR protocols). | Droplet Digital PCR (ddPCR) assays [50] |
Establishing Analytical Sensitivity
Analytical sensitivity refers to the lowest level at which an assay can reliably detect a specific analyte. For the Belay Summit assay, this was defined for different variant types [45]:
- For SNVs, MNVs, and indels, the analytical sensitivity was demonstrated to be 96%.
- This level of sensitivity was achieved at a 95% limit of detection (LOD) of 0.30% variant allele fraction (VAF). The LOD is the lowest VAF at which a variant can be detected with 95% confidence.
- For chromosomal arm-level aneuploidy, the analytical sensitivity was 91%, with an LOD defined by a absolute log2 ratio [abs(log2r)] of 0.09.
These metrics demonstrate the assay's robust capability to detect low-abundance tumor-derived DNA in a controlled analytical setting, a prerequisite for clinical application.
Comparative Performance: Belay Summit vs. Other Diagnostic Modalities
A critical step in validating a new diagnostic is comparing its performance to existing standards and other emerging technologies.
Functional Sensitivity in a Clinical Cohort
While analytical sensitivity is measured in controlled samples, functional (or clinical) sensitivity is assessed in real patient populations. In a cohort of 124 specimens from patients with primary and metastatic CNS tumors, the Belay Summit assay demonstrated a clinical sensitivity of 90% and a specificity of 95% [45]. This high specificity is particularly notable, as it indicates a low rate of false positives, which is crucial for avoiding misdiagnosis.
Head-to-Head Diagnostic Performance
Table 2: Comparison of Diagnostic Modalities for Leptomeningeal Metastases (LM) [46] [47] [50].
| Diagnostic Method | Pooled Sensitivity (%) | Pooled Specificity (%) | Key Advantages | Key Limitations |
|---|---|---|---|---|
| CSF Cytology (Gold Standard) | 54.7 - 71.9 | ~100 | High specificity; well-established. | Low and variable sensitivity; requires expert pathologist. |
| CSF Circulating Tumor Cells (CTC) | 87.0 | 93.8 | High sensitivity for LM. | Isolation of intact cells can be technically challenging. |
| CSF Cell-free Tumor DNA (ctDNA) | 97.9 (range: 85-100) | 89.0 - 93.5 | High sensitivity; enables genomic profiling. | Requires sufficient tumor DNA shedding; bioinformatic complexity. |
| MRI | 59.4 - 76.9 | 97.6 | Non-invasive; excellent anatomic detail. | Lower sensitivity, especially for early LM. |
| Belay Summit Assay | 90.0 (Clinical) | 95.0 (Clinical) | Balanced high sensitivity/specificity; provides genomic data. | Requires CSF sampling; performance in very early-stage disease not fully defined. |
The relationship between the high analytical sensitivity of the Belay assay and its resulting clinical performance is foundational to its utility. This logical progression is illustrated below.
Furthermore, a 2024 study on intramedullary spinal cord tumors highlighted the clinical impact of this approach. It found that H3K27M mutations in CSF exhibited a sensitivity of 85.7% and a specificity of 100% (AUC=0.929) for diagnosing diffuse midline glioma, H3K27-altered, significantly outperforming traditional methods for this specific tumor type [48].
Discussion: Analytical vs. Functional Sensitivity in Context
The data presented above clearly delineates the difference between a test's inherent technical capabilities and its real-world clinical performance. The Belay Summit assay's high analytical sensitivity (96% for SNVs/MNVs/indels) is the engine that drives its superior functional sensitivity (90% in a mixed CNS tumor cohort) compared to cytology (71.9% sensitivity) [45] [46].
This performance must be framed within the broader thesis of CSF liquid biopsy development. The field is moving toward multi-analyte approaches. For instance, while the Belay assay focuses on ctDNA, other biomarkers like CTCs have shown exceptional sensitivity for LM (87.0%) [46]. The choice of biomarker and technology platform directly influences the diagnostic profile. ctDNA analysis excels at providing comprehensive genomic information for targeted therapy selection (e.g., detecting EGFR mutations in non-small cell lung cancer metastases), while CTC analysis may provide living cells for functional studies [50] [51] [52].
Challenges remain, including the standardization of pre-analytical variables (CSF collection volume, processing time), bioinformatic analysis of often low-concentration samples, and determining the clinical utility of these assays for early detection and monitoring minimal residual disease. Future research directions will likely involve the validation of these assays in larger, prospective trials and their integration into standard clinical decision-making pathways for neuro-oncology.
With the recent approval of disease-modifying therapies for Alzheimer's disease (AD), the need for accurate, scalable, and minimally invasive biomarkers to detect underlying pathology has become increasingly urgent [53]. Blood-based biomarkers, particularly phosphorylated tau 217 (p-tau217), have emerged as leading candidates to facilitate diagnosis and identify candidates for therapy [54]. This case study provides a comprehensive analytical validation of a plasma p-tau217 immunoassay, examining its performance characteristics against other technological platforms and assessing its suitability for clinical implementation within the context of analytical versus functional sensitivity performance research.
Assay Principle and Platform Specifications
The validated p-tau217 immunoassay utilizes single molecule array (Simoa) technology on the HD-X analyzer, a fully automated digital immunoassay platform that provides attomolar sensitivity through digitized bead-based ELISA technology [53]. The assay employs a three-step sandwich immunoassay format with the following key reagent components:
Research Reagent Solutions
Table 1: Key Research Reagents for p-Tau217 Immunoassay
| Component | Specifications | Function |
|---|---|---|
| Capture Beads | Monoclonal anti-p-Tau217 antibody (Janssen PT3) specific for epitope spanning residues 210-220 with phosphorylation sites at 212 and 217, coupled to 2.7 μm carboxy paramagnetic microbeads | Isolation and immobilization of target analyte |
| Detector Antibody | Biotinylated monoclonal anti-tau antibody (Janssen HT43) specific for N-terminal residues 7-20 | Recognition and binding for signal generation |
| Conjugate | Streptavidin-β-galactosidase (SβG) | Enzyme conjugation for signal amplification |
| Calibrator | Purified peptide construct (MW 4929) composed of N-terminal epitope (tau residues 7-20) and phosphorylated mid-region epitope (tau residues 210-220) connected by PEG linker | Quantification standard for calibration curve |
| Sample Diluent | PBS with heterophilic blockers, EDTA, and surfactant | Matrix for sample preparation and interference reduction |
The assay protocol involves initial incubation of plasma samples with capture beads, followed by sequential addition of biotinylated detector antibody and SβG conjugate, with signal generation achieved through resorufin β-D-galactopyranoside (RGP) substrate hydrolysis [53]. The concentration of p-tau217 is interpolated from a logistic 4-parameter standard curve with a time to assay completion of approximately one hour.
Figure 1: Experimental workflow for the Simoa p-Tau217 immunoassay, illustrating the sequential steps from sample introduction to signal detection.
Analytical Validation Experimental Protocols
Precision Studies
Precision was evaluated according to Clinical and Laboratory Standards Institute (CLSI) protocols across multiple instruments, operators, and reagent lots [53]. The experimental design involved:
- 80 independent runs using 23 patient-derived samples with p-tau217 concentrations ranging from 0.09 U/mL to 3.35 U/mL
- Testing across multiple kit lots and different operators to assess inter-assay and inter-operator variability
- Evaluation of total coefficient of variation (CV) across the analytical measurement range
Sensitivity and Linearity Assessment
Analytical sensitivity was determined through:
- Functional analytical sensitivity (lower limit of quantitation - LLOQ) established at 0.08 U/mL using standard protocols [55]
- Linearity studies performed according to CLSI Document EP06 Ed2 to validate assay response across the measurement range [53]
- Determination of minimum required dilution (MRD) for plasma samples
Interference and Stability Testing
Interference studies evaluated the effect of:
- Hemolysis with tolerance up to 2+ level [55]
- Lipemic interference using purified lipids added to samples
- Specificity against purified tau (2N4R) to assess cross-reactivity Stability testing assessed:
- Freeze-thaw stability through 7 complete cycles
- Short-term stability at room temperature and refrigerated conditions for up to 72 hours
- Long-term stability at recommended storage conditions
Performance Comparison Across Platforms
Analytical Performance Metrics
Table 2: Comparative Analytical Performance of p-Tau217 Assay Platforms
| Performance Parameter | Simoa Immunoassay (This Validation) | Lumipulse Immunoassay | Mass Spectrometry (%p-tau217) |
|---|---|---|---|
| Lower Limit of Quantitation | 0.08 U/mL [55] | 0.27 pg/mL [54] | Not specified |
| Precision (Total CV) | ≤20% across analytical range [55] | Not specified | Not specified |
| Analytical Measurement Range | 0.08 to 2.81 U/mL [55] | Not specified | Not specified |
| Sample Volume | 33.3 μL [56] | Not specified | Not specified |
| Interference Tolerance | Hemolysis (>2+ not acceptable), no lipemia interference [55] | Affected by CKD, age [54] | Not specified |
| Stability | 7 freeze-thaw cycles, 72h room temperature [55] | Not specified | Not specified |
Clinical Performance Comparison
Table 3: Clinical Performance Across p-Tau217 Detection Platforms
| Platform/Assay | AUC for Aβ-PET+ | Accuracy | Sensitivity | Specificity | Reference |
|---|---|---|---|---|---|
| Simoa p-Tau217 (LucentAD) | 0.91-0.96 | 89-91% (secondary care) 85% (primary care) | 95% (at 95% specificity) | 95% (at 95% sensitivity) | [53] [54] |
| Lumipulse p-Tau217 | 0.93-0.96 | 89-91% (secondary care) 85% (primary care) | 95% | 95% | [54] |
| Mass Spectrometry (%p-tau217) | 0.91-0.96 | 93% (Aβ-PET detection) | 91% | 94% | [57] [54] |
| p-Tau217/Aβ42 Ratio | 0.88-0.91 | Comparable to p-tau217 alone | High (race-independent) | High (race-independent) | [58] [54] |
| ALZpath p-Tau217 | Comparable to other immunoassays | 0.83-0.88 (Aβ-PET detection) | 84-87% | 85-89% | [57] |
Discussion: Analytical vs. Functional Sensitivity
Diagnostic Performance in Diverse Populations
The clinical validation across 1,767 participants from primary and secondary care settings demonstrated robust performance with area under the curve (AUC) values of 0.93-0.96 for detecting abnormal cerebrospinal fluid Aβ42:p-tau181 ratios [54]. The implementation of a two-cutoff approach significantly improved diagnostic certainty, increasing accuracy to 92-94% across settings while identifying 12-17% of cases with intermediate results requiring further testing [53] [54].
Figure 2: Two-cutoff diagnostic approach for p-Tau217 interpretation, showing the classification of patients into definitive positive, definitive negative, and intermediate zones requiring confirmatory testing.
Comparative Platform Performance
When compared to other technologies, mass spectrometry-based %p-tau217 demonstrated the highest overall performance with accuracy of 93%, sensitivity of 91%, and specificity of 94% for detecting Aβ-PET status, significantly outperforming immunoassays (P<0.007) [57]. Among immunoassays, the p-tau217Lilly and p-tau217ALZpath assays showed higher AUC values than p-tau217Janssen for Aβ-PET status detection [57].
The p-tau217/Aβ42 ratio demonstrated particular utility in diverse populations, showing comparable performance across racial groups (AUC 0.88 for Black individuals, 0.91 for White individuals) with the lowest proportion of intermediate classifications (≤16%) [58]. This suggests that ratio measurements may enhance diagnostic consistency across demographically varied populations.
Impact of Comorbidities and Age
Analytical performance remained consistent across cognitive stages (subjective cognitive decline, mild cognitive impairment, and dementia) with accuracies of 86-89% using a single cutoff [54]. However, chronic kidney disease and advanced age (≥80 years) affected absolute p-tau217 concentrations, though implementing the two-cutoff approach mitigated these effects on diagnostic accuracy [54].
This comprehensive validation demonstrates that the plasma p-tau217 immunoassay meets recommended performance criteria for clinical implementation, with analytical characteristics supporting its use as a rule-out test for Alzheimer's disease pathology. The two-cutoff approach optimizes diagnostic certainty while appropriately identifying cases requiring confirmatory testing. When considering analytical versus functional sensitivity, mass spectrometry-based %p-tau217 maintains superior performance, but fully automated immunoassays provide the scalability and practicality necessary for widespread clinical adoption across diverse healthcare settings.
Optimizing Performance: Strategies to Overcome Sensitivity Challenges and Assay Noise
In the field of clinical diagnostics and drug development, the performance of an immunoassay is critically dependent on its sensitivity and precision. Two key metrics—analytical sensitivity (the lowest detectable concentration of an analyte) and functional sensitivity (the lowest concentration at which an assay can measure with a specified precision)—are paramount for reliable clinical decision-making [3]. High-sensitivity cardiac troponin (hs-cTn) assays, essential for diagnosing acute coronary syndromes, must satisfy strict criteria: a coefficient of variation (CV) of ≤10% at the 99th percentile upper reference limit (URL) and measurable values below the 99th percentile URL in >50% of healthy individuals [3]. This guide objectively compares the performance of the new Sysmex HISCL hs-cTnT assay against the established Roche Elecsys hs-cTnT assay, focusing on their analytical and functional sensitivity characteristics. By examining experimental data on limits of detection, precision profiles, and the impact of biological variables, this analysis provides researchers and scientists with a framework for evaluating assay performance and identifying strategies to mitigate inherent noise and imprecision.
Assay Performance Comparison: Sysmex HISCL vs. Roche Elecsys
A direct method comparison study involving 2,151 samples demonstrated strong correlation (r=0.95) between the Sysmex HISCL and Roche Elecsys hs-cTnT assays [3]. The quantitative performance data, essential for understanding their operational boundaries, are summarized in the table below.
Table 1: Analytical Performance Metrics of Sysmex HISCL and Roche hs-cTnT Assays
| Performance Metric | Sysmex HISCL hs-cTnT Assay | Roche Elecsys hs-cTnT Assay |
|---|---|---|
| Limit of Blank (LoB) | 1.3 ng/L | Not specified in study |
| Limit of Detection (LoD) | 1.9 ng/L | Not specified in study |
| Functional Sensitivity (CV ≤20%) | 1.8 ng/L | Not specified in study |
| Functional Sensitivity (CV ≤10%) | 3.3 ng/L | Not specified in study |
| Measurement Range | 2 – 10,000 ng/L | Not specified in study |
| Assay Time | 17 minutes | 9 minutes |
| Precision (Control Level 1, 106 ng/L) | 2.5% CV | Not specified in study |
| Precision (Control Level 2, 3253 ng/L) | 2.2% CV | Not specified in study |
| 99th Percentile URL (Overall) | 14.4 ng/L | Derivation population provided |
| 99th Percentile URL (Male) | 17.0 ng/L | Derivation population provided |
| 99th Percentile URL (Female) | 13.9 ng/L | Derivation population provided |
The data show that the Sysmex HISCL assay meets the criteria for a high-sensitivity assay. Its functional sensitivity of 3.3 ng/L (CV ≤10%) is below its derived 99th percentile URLs, ensuring precise measurement at clinically decision-relevant concentrations [3]. The Bland-Altman analysis revealed a mean absolute difference of 3.5 ng/L for samples with hs-cTnT ≤52 ng/L, indicating good agreement in the low concentration range most critical for rule-out algorithms [3].
Experimental Protocols for Assay Evaluation
The following section details the key methodologies employed in the evaluation of the Sysmex HISCL hs-cTnT assay, providing a reproducible framework for assay validation.
Protocol for Determining Limits of Blank, Detection, and Quantitation
This protocol follows CLSI EP17-A2 guidelines [3].
- Limit of Blank (LoB): The LoB was determined by repeatedly testing a sample with no analyte (the HISCL diluent) to establish the highest apparent analyte concentration expected to be found in a blank sample.
- Limit of Detection (LoD): The LoD was derived from the LoB and the variability of low-level analyte samples, representing the lowest concentration at which the analyte can be reliably distinguished from the blank.
- Functional Sensitivity: HISCL control reagents were serially diluted with diluent to create low-concentration samples. Each dilution was tested 20 times to determine the mean concentration and associated CV%. The functional sensitivity was defined as the concentration corresponding to a CV of 20% and 10%, respectively, identified through curve-fitting of the results [3].
Protocol for Precision Assessment
This protocol adheres to CLSI EP05-A3 guidelines [3].
- Materials: Two levels of HISCL control material (at 106 ng/L and 3253 ng/L) were used.
- Procedure: Each control level was analyzed five times per day over five separate days.
- Analysis: The within-run, between-run, and total precision were calculated and expressed as the coefficient of variation (CV%).
Protocol for 99th Percentile Upper Reference Limit (URL) Derivation
- Cohort Definition: A cardio-renal healthy population (n=1,004) over 18 years of age was recruited. Subjects with a history of hypertension, diabetes, known cardiac, muscle, liver, renal, or pulmonary diseases, or an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m² were excluded [3].
- Sample Analysis: Serum samples from this cohort were analyzed using the Sysmex HISCL-5000 analyzer.
- Statistical Calculation: The 99th percentile URLs were calculated separately for the overall population, males, and females.
Visualizing Assay Evaluation and Performance
The following diagrams, created using Graphviz and the specified color palette, illustrate the key workflows and relationships in assay evaluation.
High-Sensitivity Troponin Assay Evaluation Workflow
Factors Influencing Troponin Baseline Levels
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation and validation of high-sensitivity immunoassays require specific, high-quality materials. The following table details key reagents and their functions based on the Sysmex HISCL hs-cTnT evaluation.
Table 2: Key Research Reagent Solutions for hs-cTnT Immunoassay Development
| Reagent / Material | Function in the Assay | Specification / Notes |
|---|---|---|
| Mouse Anti-TnT Coated Magnetic Particles | Solid phase for capturing hs-cTnT antigen from the sample; enables separation of bound and unbound material. | Forms the foundation of the sandwich immunoassay. Specific clone not disclosed. |
| Alkaline-Phosphatase-Labeled Monoclonal Mouse Anti-TnT | Detection antibody that binds to the captured TnT; generates a chemiluminescent signal proportional to TnT concentration. | The enzyme label catalyzes the chemiluminescent reaction. |
| Chemiluminescent Substrate | Substance (chloro-dioxetane phenyl phosphate) that produces light upon reaction with the alkaline phosphatase enzyme. | The intensity of the emitted light is directly measured to quantify TnT. |
| HISCL hs-cTnT Calibrators (C0-C5) | Set of solutions with known TnT concentrations used to generate the standard curve for interpolating sample concentrations. | Calibrators C1-C5 contain human serum. Calibration curve is valid for 30 days [3]. |
| HISCL Control Materials | Quality control samples at defined concentrations (e.g., 106 ng/L and 3253 ng/L) used to monitor assay precision and day-to-day performance. | Included in the assay kit; essential for verifying assay validity per CLSI guidelines [3]. |
| HISCL Diluent | A matrix used for serial dilution of controls for functional sensitivity studies and for sample dilution if required. | Serves as the blank matrix for determining the Limit of Blank [3]. |
Discussion: Mitigation of Noise and Imprecision
The comparative data reveal that the Sysmex HISCL hs-cTnT assay successfully mitigates key sources of noise and imprecision to meet high-sensitivity criteria. Its low functional sensitivity (3.3 ng/L at CV≤10%) ensures that measurements at the clinically critical 99th percentile URL (14.4 ng/L) are analytically precise [3]. This performance is achieved through a robust immunoassay design employing magnetic particle separation and chemiluminescent detection.
However, biological and physiological variables remain significant sources of potential "noise" in clinical interpretation. The data confirm that hs-cTnT concentrations are influenced by age, sex, and renal function. For instance, hs-cTnT baselines increase with decreasing eGFR, a phenomenon well-documented for the Roche assay, which was also observed with the Sysmex assay [3]. Furthermore, unlike troponin I, hs-cTnT can be elevated in patients with skeletal muscle disorders without cardiac disease, posing a risk of false-positive interpretation if not considered [3]. Mitigation strategies therefore must extend beyond the analytical phase to include clinical correlation and the use of gender-specific 99th percentile URLs, as provided for the Sysmex assay (17.0 ng/L for males and 13.9 ng/L for females) [3]. Understanding these factors is crucial for drug development professionals and researchers to accurately design studies and interpret troponin data in both clinical and preclinical settings.
The performance of modern biosensors is critically evaluated using two distinct but complementary metrics: analytical sensitivity and functional sensitivity. Analytical sensitivity, often referred to as the calibration sensitivity, is formally defined as the slope of a method's calibration function, indicating how strongly the measurement signal changes with analyte concentration [9]. In practical terms, it describes the detection strength of the laboratory method itself. In contrast, functional sensitivity represents "the lowest concentration at which an assay can report clinically useful results," with usefulness defined by an acceptable level of precision, typically a maximum coefficient of variation (CV) of 20% [10]. This crucial distinction separates the theoretical detection capability of a sensor from its practical, clinically applicable performance.
The drive to enhance both metrics has catalyzed the development of advanced signal amplification strategies. These innovations are particularly vital for detecting low-abundance disease biomarkers, such as microRNAs (miRNAs) in cancer diagnostics, which are present at ultralow concentrations in complex biological matrices [59]. This guide provides a comparative analysis of two dominant amplification paradigms: nanomaterial-based enhancement and dual-modality sensing, evaluating their performance data, experimental protocols, and implementation requirements to inform researcher selection for specific diagnostic applications.
Nanomaterial-Based Signal Amplification Strategies
Nanomaterial-based amplification represents a foundational approach for enhancing biosensor signals by dramatically increasing the electroactive surface area, improving electron transfer kinetics, and facilitating higher bioreceptor loading densities [60] [61].
Key Nanomaterial Classes and Amplification Mechanisms
- Carbon Nanomaterials: Graphene, carbon nanotubes (CNTs), and reduced graphene oxide (rGO) provide exceptional electrical conductivity and large surface areas. For instance, Muniandy et al. developed a Salmonella sensor using a reduced graphene oxide/titanium dioxide (rGO-TiO2) nanocomposite, which produced a significantly improved signal response compared to single-component platforms [61].
- Gold Nanoparticles (AuNPs): prized for their high surface-to-volume ratio, excellent biocompatibility, and ease of functionalization. Wang et al. exploited raspberry-shaped gold (RC-Au) nanoprisms with exposed high-index crystal faces to create an aptasensor for flufenpyr detection, achieving enhanced catalytic activity and signal amplification [61].
- Hybrid Nanocomposites: Combining multiple nanomaterials often yields synergistic effects. Akbarzadi et al. developed a sensor for oxytetracycline using a nanocomposite of multi-walled carbon nanotubes (MWCNTs), gold nanoparticles (AuNPs), reduced graphene oxide (rGO), and chitosan (CS), resulting in greatly enhanced conductivity and an impressive detection limit of 30.0 pM [61].
Table 1: Performance Comparison of Nanomaterial-Based Biosensors
| Target Analyte | Nanomaterial Platform | Amplification Strategy | Detection Limit | Functional Sensitivity (CV ≤20%) | Reference |
|---|---|---|---|---|---|
| Salmonella | rGO-TiO2 Nanocomposite | Increased surface area & electron transfer | 10 cfu·mL⁻¹ | Not specified | [61] |
| Oxytetracycline | MWCNTs-AuNPs/CS-AuNPs/rGO | Layer-by-layer electrode modification | 30.0 pM | Not specified | [61] |
| microRNA | Laser-induced N-doped graphene | Nanostructured electrode surface | Femtomolar | Not specified | [59] |
| E. coli O157:H7 | AuNPs/rGO–PVA Composite | Increased surface area & signal output | 9.34 CFU mL⁻¹ | Not specified | [61] |
Experimental Protocol: Nanomaterial-Enhanced Electrochemical Detection
A typical protocol for constructing a nanomaterial-based electrochemical biosensor involves several critical stages [61]:
- Electrode Modification: A glassy carbon electrode (GCE) is first polished and cleaned. The nanomaterial (e.g., MWCNTs, rGO) is dispersed in a solvent like dimethylformamide and drop-cast onto the GCE surface.
- Bioreceptor Immobilization: Bioreceptors (aptamers, antibodies) are immobilized onto the modified electrode. This can be achieved via covalent coupling (using EDC/NHS chemistry to form amide bonds with carboxylated nanomaterials) or non-covalent physical adsorption.
- Signal Amplification & Detection: The binding event is transduced into a measurable electrochemical signal (e.g., change in current in DPV or impedance in EIS). The nanomaterial matrix amplifies this signal, enabling detection of low-abundance targets.
Dual-Modality and Microfluidic Signal Amplification
Dual-modality biosensors represent an emerging paradigm that integrates two independent sensing mechanisms within a single device, overcoming the limitations inherent in single-mode detection and providing cross-verified, highly reliable data [62].
Operational Principles and Performance Advantages
A prime example is a flexible physiological mechano-sensor that leverages microfluidic deformation to simultaneously induce liquid-solid interfacial capacitance and triboelectric effects [62]. In this configuration:
- The liquid droplet acts as a deformable electrode, forming a parallel-plate capacitor with a bottom electrode for high-precision static force detection.
- The same droplet functions as a triboelectric component, interacting with a PDMS tribo-layer to capture dynamic force signals in a self-powered mode.
- This dual-mode operation enables the sensor to achieve both high sensitivity (4.078 kPa⁻¹) and a rapid dynamic response (21 ms), allowing for stable, long-term monitoring of physiological signals such as pulse waves [62].
Beyond mechanical sensing, microfluidic confinement itself is a powerful strategy for amplifying assay performance. By drastically reducing channel height, convective mass transport of analytes to the sensor surface is significantly enhanced [63]. This effect, governed by the Levich equation, can lead to a 2000% acceleration in target recruitment kinetics, a 600% improvement in target response magnitude, and a 300% enhancement in assay selectivity, even without catalytic amplification or specialized nanomaterials [63].
Experimental Protocol: Dual-Modality Microfluidic Sensor Fabrication
The construction of a dual-mode microfluidic sensor involves precision engineering and integration [62]:
- Bottom Structure Fabrication: A flexible polyethylene terephthalate (PET) substrate is prepared. Indium tin oxide (ITO) electrodes are deposited via mask-assisted sputtering, followed by spin-coating a thin PDMS layer to act as the dielectric and tribo-layer.
- Microfluidic Mold Creation: A silicon wafer undergoes a two-step photolithography process to sequentially define differentiated height structures—first for the sensing channel (100 μm), then for the injection port and sensing cavity (200 μm).
- Device Integration: The demolded PDMS structural layer is bonded to the PET substrate using oxygen plasma treatment, forming a sealed microfluidic network. The system is then filled with water via the injection port.
Table 2: Performance Comparison of Dual-Modality and Microfluidic-Enhanced Biosensors
| Sensor Type | Amplification Mechanism | Key Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|
| Dual-Mode Microfluidic Mechano-sensor [62] | Liquid-solid interfacial capacitance & triboelectricity | Sensitivity: 4.078 kPa⁻¹Response: 21 msStable operation: 168 hours | Self-powered dynamic mode; multi-parameter sensing; customizable range/sensitivity | Complex fabrication; requires microfluidic expertise |
| Microfluidic-Enhanced Flux Biosensor [63] | Confinement-enhanced mass transport | 2000% faster kinetics600% higher signal300% better selectivity | Reagentless; no nanomaterials needed; works with untreated surfaces | Requires precise flow control; limited to analyzed volumes |
| MS-based HCR Detection [64] | Hybridization Chain Reaction (HCR) with photocleavable mass tags | Detection Limit: 415 amol (HBV)Dynamic Range: 1 fmol-100 pmol | Enzyme-free; highly multiplexed; quantitative reliability with internal standard | Specialized MS equipment required; complex probe design |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of advanced biosensing strategies requires specific functional materials and reagents.
Table 3: Essential Research Reagents and Materials for Advanced Biosensing
| Material/Reagent | Function in Biosensing | Example Application |
|---|---|---|
| Gold Nanoparticles (AuNPs) | Signal amplification carriers; enhance electron transfer; biocompatible probe immobilization | Flufenpyr detection using raspberry-shaped Au nanoprisms [61] |
| Reduced Graphene Oxide (rGO) | High surface area matrix; improves electrical conductivity; facilitates bioreceptor loading | rGO-TiO2 nanocomposite for Salmonella sensing [61] |
| Chitosan (CS) | Biocompatible polymer for electrode modification; improves stability and binding capacity | Component of MWCNTs-AuNPs/CS-AuNPs/rGO nanocomposite [61] |
| Photocleavable Mass Tags (PMTs) | MS-detectable labels for multiplexed analysis; generate ions via laser cleavage | Target-triggered HCR with LDI-TOF MS detection of viral genes [64] |
| Polydimethylsiloxane (PDMS) | Flexible, transparent elastomer for microfluidic channels; triboelectric layer | Dual-mode microfluidic mechano-sensor fabrication [62] |
| Hairpin DNA (HP) Probes | Nucleic acid amplification elements; form concatemers upon target recognition | HCR-based signal amplification for miRNA and viral DNA detection [59] [64] |
| Screen-Printed Electrodes (SPE) | Disposable, portable electrochemical platforms; ideal for point-of-care testing | Miniaturized biosensor systems for clinical and environmental monitoring [65] |
The comparative analysis of amplification strategies reveals a clear trade-off between performance, complexity, and application scope. Nanomaterial-based approaches offer a robust, well-established pathway for significantly lowering detection limits, with carbon nanomaterials and gold nanoparticles providing substantial signal enhancement. However, they often face challenges related to reproducibility, nanomaterial batch variability, and potential complex modification procedures [61].
In contrast, dual-modality and microfluidic confinement strategies address different aspects of sensor performance. Dual-modality sensors enhance data reliability and enable multi-parameter sensing from a single platform [62], while microfluidic confinement provides a transformative, yet underutilized, method to boost both analytical and functional sensitivity by fundamentally improving mass transport to the sensor surface, often in a reagentless format [63].
For researchers and drug development professionals, the strategic choice depends on the specific diagnostic challenge. For maximum signal amplification in complex samples, nanomaterial composites remain a powerful choice. When seeking highly reliable, multi-parameter data or operation in resource-limited settings, dual-modality and microfluidic approaches offer compelling advantages. The emerging integration of artificial intelligence with these platforms is poised to further accelerate the rational design of interfacial layers and predictive optimization of surface architectures, marking the next frontier in high-performance biosensing [60].
Leveraging AI and Machine Learning for Parameter Optimization
The pursuit of optimal parameters lies at the heart of scientific research and drug development. Traditionally, this process relied on labor-intensive, sequential experimentation often constrained by cost, time, and human bandwidth. The emergence of Artificial Intelligence (AI) and Machine Learning (ML) has fundamentally transformed this landscape, introducing a paradigm shift towards data-driven, intelligent optimization. In the specific context of assay development and diagnostic testing, optimizing for parameters like analytical sensitivity (the ability to distinguish a signal from background noise) and functional sensitivity (the lowest concentration measurable with a defined precision, often a CV of 20%) is critical for clinical utility [9] [10]. AI and ML algorithms excel at navigating complex, high-dimensional parameter spaces—such as those found in Model-Informed Drug Development (MIDD) and quantitative assay validation—to identify configurations that enhance performance, reduce resource consumption, and accelerate timelines [66] [67]. This guide provides a comparative analysis of leading AI/ML platforms and techniques, evaluating their efficacy in optimizing parameters to bridge the gap between analytical detection and clinically functional performance.
Comparative Analysis of AI/ML Optimization Platforms
The following section provides a comparative analysis of prominent AI/ML platforms, focusing on their application in parameter optimization for drug discovery and assay development. The table below summarizes their core technologies, primary applications, and documented performance metrics.
Table 1: Comparison of Leading AI-Driven Platforms for Parameter Optimization
| Platform/ Company | Core AI/ML Technology | Primary Optimization Application | Reported Performance & Metrics |
|---|---|---|---|
| Exscientia | Generative AI, Centaur Chemist approach, Automated Design-Make-Test-Learn cycles [68] | Small-molecule drug design, lead optimization, target selection [68] | Achieved clinical candidate for a CDK7 inhibitor after synthesizing only 136 compounds (vs. thousands traditionally); compressed discovery timeline to 18 months for an IPF drug [68] |
| Insilico Medicine | Generative AI, Deep neural networks for target and molecule design [68] | Target identification, de novo drug candidate generation [68] | Advanced an idiopathic pulmonary fibrosis drug from target discovery to Phase I trials in 18 months [68] |
| Recursion | Phenotypic screening, AI-powered image analysis of cell cultures [68] | Target discovery, lead optimization using high-content biological data [68] | Platform generates massive, proprietary biological datasets to train its AI models for identifying novel drug candidates [68] |
| BenevolentAI | Knowledge graphs mining scientific literature and clinical data [68] | Target identification and prioritization, uncovering novel disease biology [68] | Uses AI to generate and validate novel hypotheses from vast amounts of structured and unstructured biomedical data [68] |
| Schrödinger | Physics-based computational models (e.g., free energy perturbation), ML [68] | Prediction of molecular properties, binding affinity, and optimization of drug candidates [68] | Integrates first-principles physics with machine learning for high-accuracy in-silico candidate screening [68] |
| Nested Learning (Google Research) | Self-modifying architecture (Hope), Continuum Memory Systems, Nested optimization problems [69] | Mitigating catastrophic forgetting in continual learning, long-context memory management [69] | Demonstrated lower perplexity and higher accuracy on language modeling and reasoning tasks compared to standard transformers [69] |
Core AI/ML Optimization Techniques and Experimental Protocols
Beyond integrated platforms, specific AI/ML techniques form the toolkit for parameter optimization. These methods can be applied to a wide range of problems, from tuning assay conditions to optimizing pharmacokinetic models.
Key Optimization Techniques
- Hyperparameter Tuning: This process involves optimizing the configuration settings that govern the ML training process itself. Modern methods have moved beyond inefficient grid searches [70].
- Bayesian Optimization: A sample-efficient technique that builds a probabilistic model of the objective function to intelligently select the most promising hyperparameters to evaluate next. It balances exploration of unknown regions with exploitation of known good regions [66] [70]. Tools like Optuna automate this process and can slash search time by 50-90% through features like aggressive pruning, which halts underperforming trials early [70].
- Random Search: Involves sampling hyperparameter combinations randomly from a defined search space. It is often more efficient than grid search, as it better explores the importance of different parameters without an exhaustive combinatorial search [70].
- Model Pruning: This technique systematically removes unnecessary weights or neurons from a neural network after training. The goal is to create a smaller, faster model for inference (deployment) that maintains accuracy. Magnitude pruning targets weights with values closest to zero, while structured pruning removes entire channels or layers, often leading to better hardware acceleration [66].
- Quantization: This method reduces the numerical precision of the model's parameters, for example, from 32-bit floating-point (FP32) to 8-bit integers (INT8). The benefits are substantial: a ~75% reduction in model size and corresponding speedups in inference, making deployment on mobile or edge devices feasible. This can be done post-training or more effectively as quantization-aware training [66] [71].
- Knowledge Distillation: A process where a large, accurate, but computationally heavy "teacher" model is used to train a smaller, more efficient "student" model. The student learns to mimic the teacher's outputs, often achieving comparable accuracy with a fraction of the size and cost, making it ideal for production environments [71].
Experimental Protocol for AI-Assayed Functional Sensitivity Determination
Determining the functional sensitivity of an assay is a key application of parameter optimization. The following protocol outlines how AI can streamline this process.
- Objective: To determine the functional sensitivity of a diagnostic assay—defined as the lowest analyte concentration that can be measured with an inter-assay coefficient of variation (CV) ≤ 20% [9] [10] [1]—using AI-powered experimental design and data analysis.
- Materials & Reagents:
- Automated immunoassay analyzer (e.g., IMMULITE series) [10].
- Patient-derived serum samples or appropriate control materials at low analyte concentrations [10].
- Appropriate sample diluent (matrix-matched to avoid bias) [10].
- AI/Statistical analysis software (e.g., Python with Scikit-learn, Optuna, or custom MIDD tools).
- Methodology:
- Sample Preparation: Prepare a series of 5-10 low-concentration samples, spanning from just above the Limit of Blank (LoB) to a level where precision is expected to be acceptable. Using patient sample pools is ideal, but carefully diluted samples are a valid alternative [10] [1].
- AI-Optimized Run Scheduling: Use an algorithm to design a non-sequential, randomized run order for analyzing sample replicates. This helps to de-confound instrument drift or time-based effects from the precision measurements.
- Data Collection: Analyze each low-concentration sample in replicates (n=20 recommended for verification) across multiple separate runs, ideally over several days or weeks, to capture true day-to-day imprecision [10].
- Precision Analysis: For each sample concentration, calculate the mean measured concentration and the inter-assay CV.
- Model Fitting & Optimization: Input the (concentration, CV) data pairs into a curve-fitting model (e.g., a power law or exponential decay model). The AI's role is to optimize the model parameters to best fit the data and precisely identify the concentration where the fitted curve crosses the CV=20% threshold.
- Validation: The estimated functional sensitivity should be validated by testing a new set of samples at that concentration across multiple runs to confirm the CV meets the ≤20% goal.
Table 2: Research Reagent Solutions Toolkit for Sensitivity Optimization
| Reagent / Material | Function in Experiment |
|---|---|
| Blank (Zero) Sample | A sample containing no analyte, used to establish the baseline signal (Limit of Blank - LoB) and assess background noise [10] [1]. |
| Low Concentration Calibrators | Samples with known, low analyte concentrations used to characterize the assay's performance near its detection and quantitation limits [1]. |
| Matrix-Matched Diluent | A solution with a protein and chemical composition similar to the patient sample (e.g., serum). Critical for diluting high-concentration samples without altering the assay's measurement characteristics [10]. |
| Patient Serum Pools | Pools of actual patient samples that provide a commutable matrix, ensuring that performance validation reflects real-world conditions [10] [1]. |
| Precision Profile Analysis Software | AI/ML tools that automate the calculation of CVs, fit curves to the precision data, and accurately interpolate the functional sensitivity [66] [71]. |
The workflow for this AI-optimized determination of functional sensitivity is illustrated below.
The Interplay of AI Optimization and Sensitivity Metrics in Drug Development
In Model-Informed Drug Development (MIDD), AI-driven parameter optimization is not an isolated step but an integral part of a continuous cycle. It bridges the gap between model prediction and real-world performance, concepts that are directly analogous to analytical and functional sensitivity. A model might have high analytical sensitivity—the ability to detect a small effect—but without optimization for robustness and generalizability, its functional sensitivity—the ability to provide reliable, useful predictions in a clinical context—may be poor [9] [67]. Techniques like hyperparameter tuning and pruning ensure that a Quantitative Systems Pharmacology (QSP) or population PK/PD model is not just finely tuned to its training data but is also efficient and reliable for simulating new clinical scenarios [66] [67]. This "fit-for-purpose" philosophy, championed by regulatory agencies, emphasizes that a model's complexity and parameters must be justified by its context of use, ensuring that its outputs are clinically actionable, much like a diagnostic assay must be functionally sensitive to guide medical decisions [67]. The following diagram illustrates this continuous optimization cycle within MIDD.
The integration of AI and ML into parameter optimization represents a fundamental advancement for research and drug development. As the comparative analysis shows, platforms like Exscientia and Insilico Medicine can dramatically compress discovery timelines, while underlying techniques like Bayesian optimization and quantization deliver the efficiency and speed required for modern applications. The critical insight for scientists and researchers is that true performance is not defined by a model's or assay's best possible performance (analytical sensitivity) but by its reliable, reproducible utility in a real-world context (functional sensitivity). By leveraging the AI/ML tools and protocols outlined in this guide, professionals can systematically navigate this complex landscape, optimizing parameters to build robust, "fit-for-purpose" models and assays that ultimately enhance decision-making and accelerate the delivery of new therapies.
Surface Functionalization and Interface Engineering to Improve Signal-to-Noise
In the realm of analytical science and biosensing, the signal-to-noise ratio (SNR) serves as a fundamental determinant of performance, directly impacting key metrics such as detection sensitivity, limit of detection (LOD), and analytical reliability. Surface functionalization and interface engineering have emerged as pivotal strategies for enhancing SNR by systematically controlling interactions at the molecular level. These approaches optimize the binding, orientation, and stability of recognition elements while minimizing non-specific interactions that contribute to background noise [60]. The strategic design of interfaces is particularly crucial for distinguishing between analytical sensitivity (the lowest detectable concentration under ideal conditions) and functional sensitivity (the lowest concentration measurable with acceptable precision in real-world settings) [24]. This distinction is not merely academic; it represents the bridge between technical capability and clinical utility, especially in applications such as drug development, diagnostic testing, and therapeutic monitoring where reliable low-abundance biomarker detection is paramount.
The following sections provide a comprehensive comparison of surface engineering strategies, their quantitative impact on analytical performance, and detailed experimental methodologies. By examining specific technologies across multiple domains—from electrochemical biosensing to quantum applications—this guide offers researchers a structured framework for selecting and implementing interface optimization techniques to advance their analytical capabilities.
Key Concepts: Analytical vs. Functional Sensitivity
Understanding the distinction between analytical and functional sensitivity is essential for evaluating biosensor performance and diagnostic assay reliability. These related but distinct parameters define different aspects of detection capability:
- Analytical Sensitivity (also known as limit of detection - LOD): Represents the lowest detectable concentration of an analyte that can be reliably distinguished from zero, typically determined under optimal and controlled conditions. It reflects the technical detection limits of an assay or instrument [24].
- Functional Sensitivity: Defined as the lowest analyte concentration that can be measured with acceptable precision (typically a coefficient of variation <20%) in real-world operational environments. This parameter indicates clinical reliability and represents the practical quantification limit for routine applications [24].
The transition from analytical to functional sensitivity represents a critical pathway from technical feasibility to practical implementation. Surface functionalization plays a decisive role in bridging this gap by improving binding efficiency, reducing interference, and enhancing signal stability. For example, in thyroglobulin (Tg) monitoring for thyroid cancer patients, ultrasensitive assays (ultraTg) with an analytical sensitivity of 0.01 ng/mL demonstrate superior predictive capability for disease recurrence compared to highly sensitive assays (hsTg) with 0.1 ng/mL analytical sensitivity, despite both targeting the same clinical application [24].
Table 1: Performance Comparison of Highly Sensitive vs. Ultrasensitive Thyroglobulin Assays
| Parameter | Highly Sensitive (hsTg) | Ultrasensitive (ultraTg) |
|---|---|---|
| Analytical Sensitivity | 0.1 ng/mL | 0.01 ng/mL |
| Functional Sensitivity | 0.2 ng/mL | 0.06 ng/mL |
| Correlation with Stimulated Tg | R=0.79 (weaker in TgAb-positive patients: R=0.52) | Stronger correlation across patient populations |
| Clinical Sensitivity | 39.8% | 72.0% |
| Clinical Specificity | 91.5% | 67.2% |
| Optimal Cut-off | 0.105 ng/mL | 0.12 ng/mL |
Surface Engineering Approaches and Performance Comparison
Various surface engineering strategies have been developed to enhance SNR across different technological platforms. The following comparison highlights the most effective approaches and their quantitative impact on performance metrics.
Biosensor Surface Functionalization
In biosensing applications, surface functionalization strategies focus on optimizing the interface between transducers and biological recognition elements. These approaches enhance SNR by improving bioreceptor orientation, density, and stability while reducing non-specific binding [60].
Table 2: Surface Functionalization Strategies for Improved SNR in Biosensors
| Functionalization Approach | Key Materials/Techniques | Impact on SNR | Applications |
|---|---|---|---|
| Covalent Modification | Silanization (APTES), SAMs (alkanethiols) | Enhanced bioreceptor stability and orientation | Electrochemical biosensors, optical biosensors |
| Polymer Coatings | PEG, polydopamine, chitosan | Reduced non-specific binding and biofouling | Implantable sensors, wearable devices |
| Nanomaterial Integration | Graphene, CNTs, AuNPs | Increased surface area and signal amplification | Signal-enhanced biosensors |
| Zwitterionic Coatings | Carboxybetaine, sulfobetaine | Ultra-low fouling surfaces | Complex biological samples |
| AI-Optimized Interfaces | ML-predicted surface architectures | Optimal bioreceptor configuration | Next-generation intelligent sensors |
Advanced functionalization approaches have demonstrated remarkable improvements in detection capabilities. For instance, laser-induced graphene (LIG) electrodes create porous, interconnected 3D structures that provide high conductivity and extensive electroactive surface area, significantly enhancing electron transfer efficiency and signal amplification in electrochemical biosensors [72]. Similarly, the integration of gold nanoparticles (AuNPs) and carbon nanotubes (CNTs) leverages their unique optoelectronic properties and high surface-to-volume ratios to enhance signal transduction while maintaining compact sensor footprints [60].
Interface Engineering in Quantum Sensing
Beyond conventional biosensing, interface engineering principles yield significant benefits in quantum applications. For shallow nitrogen-vacancy (NV) centers in diamond—promising quantum sensors—surface electron spins create noise that drastically reduces coherence times. Interface engineering through oxygen termination combined with graphene patching has demonstrated remarkable noise suppression, extending coherence times from approximately 70-170 μs to over 1 ms, approaching the fundamental T1 limit [73] [74].
This approach utilizes the gapless energy band structure of graphene as an electron source to pair with unpaired electrons on the oxygen-terminated diamond surface. Double electron-electron resonance (DEER) spectroscopy confirmed at least an order of magnitude reduction in unpaired electron spin concentration (to ~10¹¹ cm⁻²) following interface engineering [73]. The resulting coherence enhancement enables detection of single weakly coupled ¹³C nuclear spins and external ¹¹B spins from hexagonal boron nitride (h-BN) layers, achieving unprecedented sensitivity for nanoscale nuclear magnetic resonance applications [74].
Microfluidic Surface Engineering
In microfluidic systems designed for fluorescent detection, surface properties dramatically impact optical performance. Conventional silicon microfluidic channels with uneven surfaces cause light scattering and angle variations that compromise interference filter performance, leading to significant background noise [75].
Transitioning to silicon-on-insulator (SOI) substrates with precisely defined channel depths created by halting etching at the buried SiO₂ layer produces exceptionally flat surfaces. This simple substrate modification reduces fluorescent background signal by approximately 5 times, lowering the limit of detection from 0.05 mM to 50 nM for fluorescein [75]. Furthermore, this approach improves the signal-to-noise ratio more than 18-fold compared to conventional silicon wafers, enabling high-sensitivity techniques like total internal reflection fluorescence (TIRF) microscopy for single-molecule detection within microfluidic environments [75].
Experimental Protocols and Methodologies
AI-Enhanced Surface Optimization Protocol
The integration of artificial intelligence (AI) and machine learning (ML) has transformed surface optimization from empirical trial-and-error to predictive design. The following protocol outlines a representative approach for AI-enhanced surface functionalization:
Data Collection and Feature Engineering: Compile comprehensive datasets of surface properties (hydrophobicity, charge distribution, functional groups, topography) and corresponding performance metrics (LOD, sensitivity, specificity, stability) from literature and experimental results [60].
Model Selection and Training: Implement neural networks, genetic algorithms, or other ML approaches to establish complex relationships between surface characteristics and sensor performance. For instance, generative adversarial networks (GANs) can design novel nanomaterials with tailored plasmonic or catalytic properties for signal amplification [60].
Molecular Dynamics Simulations: Employ AI-guided simulations to provide atomic-level understanding of bioreceptor-substrate interactions, enabling the design of high-affinity binding surfaces or antifouling coatings [60].
Experimental Validation and Iteration: Fabricate predicted optimal surfaces and characterize performance. Feed experimental results back into the model for continuous refinement.
This approach has demonstrated remarkable efficiency, accelerating optimization cycles and unlocking unprecedented precision in tailoring biosensors for emerging applications such as wearable health monitors and single-molecule detection systems [60].
Nanoparticle Functionalization for Drug Delivery
Surface functionalization of nanoparticles for enhanced electrostatic adsorption in drug delivery applications follows a systematic methodology:
Surface Charge Modification: Employ direct chemical functionalization using organosilanes (e.g., APTES for positive charge) or carboxylic acid-functionalized silanes (for negative charge) to create targeted surface potentials [76].
Polymer Coating Application: Implement polymer wrapping with charged polymers such as polyethyleneimine (PEI) or chitosan (cationic) or poly(acrylic acid) (anionic) to modify surface potential and provide multivalent interaction sites [76].
Layer-by-Layer Assembly: Construct multilayer thin films via alternating deposition of oppositely charged polyelectrolytes to precisely control surface properties and functional group density [76].
Irradiation-Based Modification: Apply emerging irradiation techniques (e.g., plasma treatment, gamma irradiation) for direct modulation of surface charge without chemical additives [76].
Characterization and Validation: Utilize spectroscopic methods (FTIR, XPS), microscopic techniques (SEM, TEM), and electrokinetic measurements (zeta potential) to verify surface properties and evaluate biomolecule adsorption efficiency [76].
This protocol emphasizes the critical relationship between functionalization strategy and characterization methodology, both essential for developing effective nanoparticle-based delivery systems with optimized electrostatic interactions.
Experimental Workflow Visualization
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of surface functionalization strategies requires specific materials and reagents tailored to the target application. The following table catalogues essential components for constructing optimized interfaces with enhanced signal-to-noise characteristics.
Table 3: Essential Research Reagents for Surface Functionalization and Interface Engineering
| Category | Specific Materials | Function and Application |
|---|---|---|
| Substrates | Silicon wafers, SOI substrates, Glass, Diamond, Gold electrodes | Base materials providing structural foundation for functionalization |
| Chemical Modifiers | APTES, Alkanethiols, VTES, Carboxyethylsilanetriol | Covalent surface modification and functional group introduction |
| Polymers | PEG, Polydopamine, Chitosan, PEI, PAA, PSS | Non-fouling coatings, charge modification, and steric stabilization |
| Nanomaterials | Graphene, CNTs, AuNPs, SiO₂ nanoparticles | Signal amplification, increased surface area, enhanced conductivity |
| Characterization Reagents | Fluorescein, Rhodamine 6G, Standard analyte solutions | Performance validation and calibration standards |
| Biological Elements | Antibodies, Enzymes, Aptamers, DNA/RNA probes | Target recognition and binding for biosensing applications |
Surface functionalization and interface engineering represent powerful paradigms for enhancing signal-to-noise ratios across diverse technological platforms. The comparative analysis presented in this guide demonstrates that strategic interface optimization consistently improves key performance metrics, including detection sensitivity, specificity, and reliability. The distinction between analytical sensitivity (technical detection limits) and functional sensitivity (practical quantification limits) provides a crucial framework for evaluating true analytical capability in real-world applications.
As evidenced by the experimental data and methodologies presented, the most successful approaches often combine multiple functionalization strategies—such as covalent modification with nanomaterial enhancement or polymer coatings with AI-guided optimization. These integrated methods address both signal amplification and noise reduction simultaneously, delivering synergistic improvements in overall performance. Furthermore, the workflow visualizations and reagent toolkit provide practical resources for researchers implementing these strategies in their own laboratories.
The continuing evolution of surface engineering—particularly through AI-driven design and novel nanomaterial integration—promises further advances in analytical capability. By systematically applying these principles and learning from cross-disciplinary successes, researchers can develop increasingly sophisticated interfaces that push the boundaries of detection sensitivity and operational reliability in chemical and biological sensing applications.
The Interplay of Specificity, Precision, and Sensitivity in Assay Optimization
In the rigorous field of bioanalytical science, the optimization of diagnostic and research assays hinges on the precise balancing of three cornerstone metrics: sensitivity, specificity, and precision. Sensitivity, defined as the proportion of actual positive cases that are correctly identified, is crucial for minimizing false negatives and is often expressed as True Positive Rate (TPR) [77]. Its counterpart, specificity, measures the proportion of actual negative cases correctly identified, thus controlling for false positives and is known as the True Negative Rate (TNR) [77] [78]. In contrast, precision—or Positive Predictive Value (PPV)—answers a different but equally critical question: of all the positive results the assay produces, what proportion are truly positive? This metric becomes paramount when the cost of a false positive is high [77] [78].
The interplay between these metrics is not merely theoretical; it has direct implications for assay utility in drug discovery and clinical diagnostics. A foundational understanding of their definitions and calculations, derived from the confusion matrix of true positives (TP), false positives (FP), true negatives (TN), and false negatives (FN), is essential [77] [78]. The ongoing evolution from manual to robotic high-throughput screening (HTS) has made statistically designed experiment-based assay optimization a critical step to overcome development bottlenecks, ensuring that these key metrics are robustly balanced for real-world application [79].
Defining Analytical and Functional Sensitivity
Beyond the basic metrics of sensitivity and specificity, assay performance is further characterized by two tiers of detection capability: analytical sensitivity and functional sensitivity. Analytical sensitivity, often reported as the Limit of Detection (LOD), refers to the lowest concentration of an analyte that an assay can reliably distinguish from a blank sample [3]. It represents the fundamental detection threshold of the assay technology. Functional sensitivity, more relevant to clinical and research practice, is defined as the lowest analyte concentration that can be measured with a specified level of precision, typically expressed as an inter-assay coefficient of variation (CV), such as 10% or 20% [3] [5]. This metric, sometimes called the Limit of Quantitation (LOQ), ensures that measurements at the low end of the range are not merely detectable but quantitatively reliable.
The distinction between these sensitivities is clearly demonstrated in cardiac troponin T (hs-cTnT) and thyroglobulin (Tg) assays. For the Sysmex HISCL hs-cTnT assay, the limit of blank (LOB) was 1.3 ng/L, the LOD was 1.9 ng/L, and the functional sensitivity (concentration at 10% CV) was 3.3 ng/L [3]. Similarly, the evolution of Tg assays spans three generations: first-generation with a functional sensitivity of 0.9 ng/mL, second-generation (highly sensitive, hsTg) with functional sensitivity between 0.15-0.2 ng/mL, and third-generation (ultrasensitive, ultraTg) with a functional sensitivity of 0.06 ng/mL [5]. This progression towards lower functional sensitivity enables earlier disease detection and more precise monitoring of residual disease, directly impacting patient management strategies in conditions like differentiated thyroid cancer.
Experimental Protocols for Sensitivity and Specificity Assessment
Protocol 1: Verification of Analytical Performance Characteristics
The verification of a high-sensitivity assay requires a rigorous, step-wise protocol to establish its analytical performance characteristics, as exemplified by the evaluation of the Sysmex HISCL hs-cTnT assay [3].
- Step 1: Determine Limit of Blank (LOB) and Limit of Detection (LOD). These are established according to Clinical and Laboratory Standards Institute (CLSI) EP17-A2 guidelines. The LOB is measured by repeatedly testing blank samples, while the LOD is determined from the analysis of low-level analyte samples, often calculated as LOB + 1.645(SD of low-level sample) [3].
- Step 2: Establish Functional Sensitivity (Limit of Quantitation). Serially dilute control reagents to obtain several low concentration testing points. Test each concentration repeatedly (e.g., 20 times) to determine the mean value and associated CV%. The functional sensitivity is the lowest concentration at which the CV% meets the desired threshold (e.g., 10% or 20%) [3].
- Step 3: Assess Assay Precision. Evaluate precision using multiple levels of control material run repeatedly over several days (e.g., 5 times daily for 5 days) as per CLSI EP05-A3 guidelines. This determines inter-assay and intra-assay CV% [3].
- Step 4: Conduct Method Comparison. Analyze a large set of patient samples (e.g., n=2151) using both the new assay and a reference standard. Use statistical methods like Passing-Bablok regression to assess agreement and Bland-Altman analysis to evaluate bias [3].
- Step 5: Define Population-specific 99th Percentile Upper Reference Limits (URLs). Establish gender-specific 99th percentile URLs by testing a large cohort of healthy individuals (e.g., n=1004) with no known history of relevant diseases. This confirms the assay meets criteria for clinical classification, such as in myocardial infarction diagnosis [3].
Protocol 2: Clinical Utility and Comparison of Assay Generations
To evaluate the real-world impact of improved sensitivity, a clinical comparison protocol between different assay generations is employed, as seen in thyroglobulin testing [5].
- Step 1: Cohort Selection. Enroll a well-defined patient cohort (e.g., 268 patients with differentiated thyroid cancer who have undergone total thyroidectomy and radioiodine treatment or diagnostic scanning).
- Step 2: Paired Sample Collection. Collect both unstimulated and TSH-stimulated blood serum samples from each patient. Stimulation can be achieved via thyroid hormone withdrawal or recombinant human TSH (rhTSH) injection.
- Step 3: Parallel Testing. Measure Tg levels in all samples using both the current standard (e.g., second-generation hsTg) and the new ultrasensitive (third-generation ultraTg) assays.
- Step 4: Statistical Correlation and Performance Analysis. Calculate the correlation (e.g., Pearson coefficient) between the two assays across the entire dataset and in subgroups (e.g., Tg antibody-positive vs. negative patients).
- Step 5: Predictive Value and Outcome Analysis. Perform Receiver Operating Characteristic (ROC) analysis to determine the optimal cut-off value for the unstimulated ultraTg that best predicts a positive stimulated Tg result (e.g., ≥1 ng/mL). Compare the sensitivity, specificity, and predictive values of the two assays. Finally, conduct long-term follow-up to correlate assay results with clinical outcomes like disease recurrence [5].
Comparative Performance Data: Ultrasensitive vs. Highly Sensitive Assays
The theoretical advantages of ultrasensitive assays are borne out in direct comparative studies. The following tables synthesize performance data from recent evaluations of troponin and thyroglobulin assays, highlighting the trade-offs between sensitivity and specificity.
Table 1: Analytical Sensitivity Performance Comparison
| Assay / Characteristic | Analyte | Limit of Detection (LOD) | Functional Sensitivity (CV=10%) | 99th Percentile URL (Overall) | 99th Percentile URL (Male) | 99th Percentile URL (Female) |
|---|---|---|---|---|---|---|
| Sysmex HISCL hs-cTnT [3] | Cardiac Troponin T | 1.9 ng/L | 3.3 ng/L | 14.4 ng/L | 17.0 ng/L | 13.9 ng/L |
| Roche Elecsys hs-cTnT [3] | Cardiac Troponin T | (Reference) | (Reference) | (Reference) | (Reference) | (Reference) |
| Highly Sensitive Tg (hsTg) [5] | Thyroglobulin | 0.1 ng/mL | 0.2 ng/mL | Not Applicable | Not Applicable | Not Applicable |
| Ultrasensitive Tg (ultraTg) [5] | Thyroglobulin | 0.01 ng/mL | 0.06 ng/mL | Not Applicable | Not Applicable | Not Applicable |
Table 2: Clinical Performance in Predicting Positive Stimulated Thyroglobulin (≥1 ng/mL)
| Assay / Performance Metric | Optimal Cut-off Value | Sensitivity | Specificity | Clinical Outcome Notes |
|---|---|---|---|---|
| Ultrasensitive Tg (ultraTg) [5] | 0.12 ng/mL | 72.0% | 67.2% | Higher detection of potential recurrence; lower specificity may increase "biochemical incomplete response" classifications. |
| Highly Sensitive Tg (hsTg) [5] | 0.105 ng/mL | 39.8% | 91.5% | Missed several recurrences; higher specificity provides more definitive "excellent response" classification. |
The data reveals a clear pattern: third-generation ultrasensitive assays push the boundaries of detection and functional sensitivity to remarkable lows. The ultraTg assay demonstrated superior sensitivity (72.0% vs. 39.8%) in predicting a positive stimulated Tg, which translated into earlier identification of patients who later developed structural recurrence [5]. However, this enhanced sensitivity comes at the cost of reduced specificity (67.2% vs. 91.5%), meaning a higher rate of false positives and potential for over-classifying patients as having a biochemical incomplete response, which could lead to unnecessary anxiety and additional testing [5]. Similarly, for cardiac troponin, the Sysmex HISCL assay demonstrated that over 50% of healthy individuals had measurable levels above the LOD, a key requirement for a true high-sensitivity assay, and established specific gender-based 99th percentile URLs [3].
The Scientist's Toolkit: Key Research Reagent Solutions
Assay optimization and performance are dependent on the quality and characteristics of the reagents employed. The following table outlines key solutions that underpin robust and sensitive assay systems.
Table 3: Essential Research Reagent Solutions for Assay Optimization
| Reagent / Solution | Primary Function | Application Example |
|---|---|---|
| Universal Activity Assays (e.g., Transcreener) [80] | Detects universal enzymatic products (e.g., ADP, SAH); enables broad target screening within an enzyme family without redeveloping core chemistry. | Kinase activity measurement (via ADP detection) across multiple kinase targets using a single, mix-and-read format. |
| High-Sensitivity Immunoassay Kits (e.g., HISCL, Elecsys) [3] | Provides all necessary pre-optimized calibrators, controls, and detection reagents (e.g., monoclonal antibodies, chemiluminescent substrates) for specific analyte quantification. | High-sensitivity cardiac troponin T (hs-cTnT) measurement on automated immunoassay analyzers. |
| Automated Liquid Handlers (e.g., I.DOT) [81] | Enables precise, non-contact dispensing of picoliter to microliter volumes; minimizes human error, variability, and reagent waste in optimization. | Miniaturizing PCR or ELISA setups, ensuring consistent well-to-well volumes for high-throughput screening. |
| Statistically Designed Experiments (DoE) [79] | A statistical (not reagent) solution that systematically optimizes multiple assay factors (e.g., concentrations, pH, time) and their interactions efficiently. | Rapidly identifying significant factors and optimal conditions for buffer composition, substrate, and enzyme levels. |
Signaling Pathways and Logical Workflows
The journey from assay design to optimized implementation involves a critical sequence of steps and decision points. The diagram below outlines the core logical workflow for assay development and optimization.
Diagram 1: Assay Development Workflow
A fundamental challenge in assay optimization is the inherent trade-off between sensitivity and specificity, or between precision and recall. This relationship is visually captured in threshold optimization curves.
Diagram 2: The Sensitivity-Specificity Trade-off
The pursuit of superior assay performance is a balancing act centered on the dynamic interplay between sensitivity, specificity, and precision. The evidence from contemporary studies indicates a clear trend: advancements in assay technology are relentlessly pushing the limits of analytical and functional sensitivity, as demonstrated by third-generation ultrasensitive assays [3] [5]. This enhanced sensitivity provides a critical tool for early detection of disease recurrence and minimal residual disease. However, this gain is frequently accompanied by a statistically significant decrease in specificity, which can complicate clinical interpretation by increasing rates of biochemical false positives [5].
Therefore, the choice between a highly sensitive and a highly specific assay is not a matter of selecting the objectively "better" tool, but rather the context-appropriate one. The optimal assay configuration depends heavily on the clinical or research question. For screening a population for a rare disease or ruling out a serious condition, maximum sensitivity is paramount. Conversely, for confirming a diagnosis before initiating an invasive or costly treatment, high specificity is essential [77]. Ultimately, successful assay optimization requires a holistic view that integrates robust experimental protocols, advanced reagent systems, and a clear understanding of the inherent trade-offs between these foundational metrics to ensure data quality and translational utility.
Benchmarking and Validation: Ensuring Analytical Rigor and Clinical Readiness
Designing a Comprehensive Analytical Validation Plan
In the development of bioanalytical methods, establishing a comprehensive validation plan is a critical prerequisite for generating reliable, reproducible, and clinically meaningful data. Such a plan provides the framework for assessing whether an analytical method is fit for its intended purpose, from basic research to supporting regulatory submissions for drug development. A cornerstone of this validation is the thorough evaluation of an assay's sensitivity, which encompasses both its analytical sensitivity (the lowest detectable amount of the analyte) and its functional sensitivity (the lowest concentration measurable with acceptable precision in a real-world setting) [24]. The distinction between these two parameters is not merely academic; it has direct implications for clinical decision-making, patient monitoring, and the interpretation of research data.
This guide objectively compares the performance of different generations of assays and analytical techniques, focusing on their sensitivity characteristics. It provides a structured approach for validating these key parameters, complete with experimental protocols and data presentation frameworks, to support researchers, scientists, and drug development professionals in their method development and evaluation processes.
Analytical vs. Functional Sensitivity: Core Concepts and Definitions
Understanding the hierarchical relationship between different types of sensitivity and the experiments required to establish them is fundamental. The following workflow outlines the key stages in characterizing assay sensitivity.
Analytical sensitivity, often termed the Limit of Detection (LOD), represents the fundamental technical capability of an assay. It is the smallest concentration of an analyte that the assay can distinguish from a blank sample with a high degree of confidence [24] [3]. It is typically determined by repeatedly measuring a zero-concentration sample (or a sample very close to zero) and calculating the mean signal plus 2 or 3 standard deviations. This parameter answers the question, "Can the assay detect the presence of the analyte at all?"
Functional sensitivity, or the Lower Limit of Quantitation (LLOQ or LOQ), is a more stringent and clinically relevant metric. It is defined as the lowest analyte concentration that can be quantitatively measured with acceptable precision (typically a coefficient of variation, CV, of ≤20%) in a routine operating environment [24]. While the LOD tells you if the analyte is present, the LOQ tells you how much is there with sufficient reliability for making interpretations. For high-sensitivity cardiac troponin T (hs-cTnT) assays, this is reflected by a precision of <10% CV at the 99th percentile upper reference limit (URL) [3] [82].
The relationship between these concepts is hierarchical: the LOQ is always greater than or equal to the LOD. A robust validation plan must characterize both to fully understand an assay's capabilities and limitations.
Comparative Performance of Assay Generations
The evolution of assay technologies has led to significant improvements in sensitivity, which can be broadly categorized into generations. A prime example is found in Thyroglobulin (Tg) testing for monitoring differentiated thyroid cancer (DTC).
Case Study: Thyroglobulin Assays
Table 1: Performance Comparison of Tg Assay Generations [24]
| Assay Generation | Representative Assay | Analytical Sensitivity (LOD) | Functional Sensitivity (LOQ) | Clinical Decision Threshold |
|---|---|---|---|---|
| First-Generation | Early Tg Assays | ~0.2 ng/mL | ~0.9 ng/mL | Stimulated Tg < 1 ng/mL |
| Second-Generation (Highly Sensitive, hsTg) | BRAHMS Dynotest Tg-plus | 0.1 ng/mL | 0.2 ng/mL | Unstimulated Tg < 0.2 ng/mL |
| Third-Generation (Ultrasensitive, ultraTg) | RIAKEY Tg IRMA | 0.01 ng/mL | 0.06 ng/mL | Proposed: < 0.1 ng/mL |
A 2025 study directly compared second-generation (hsTg) and third-generation (ultraTg) assays in 268 DTC patients. The key findings from this comparative analysis were [24]:
- Correlation: The hsTg and ultraTg assays showed a strong correlation (R=0.79) in TgAb-negative patients, which weakened in TgAb-positive patients (R=0.52), highlighting the impact of interferents.
- Predictive Performance: The ultraTg assay demonstrated higher sensitivity (72.0% vs. 39.8%) in predicting a stimulated Tg level ≥1 ng/mL, but lower specificity (67.2% vs. 91.5%) compared to the hsTg assay.
- Clinical Impact: The use of the ultraTg assay led to the reclassification of patient response categories. In some cases, patients classified as having an "excellent response" by hsTg criteria were reclassified as having an "indeterminate" or "biochemical incomplete" response by ultraTg criteria. Furthermore, discordant cases with low hsTg but elevated ultraTg were identified, and some of these patients developed structural recurrence within several years [24].
This data illustrates the trade-off between sensitivity and specificity when adopting more advanced assays and underscores the need to redefine clinical decision thresholds when changing assay methodologies.
High-Sensitivity Troponin T Assays
The principles of validation are universally applied, as seen in the evaluation of cardiac biomarkers. A 2025 study of the new Sysmex HISCL hs-cTnT assay provides a template for a comprehensive validation plan.
Table 2: Analytical Performance of the Sysmex HISCL hs-cTnT Assay [3] [82]
| Performance Parameter | Result | Experimental Protocol Summary |
|---|---|---|
| Limit of Blank (LoB) | 1.3 ng/L | Per CLSI EP17-A2, using HISCL diluent. |
| Limit of Detection (LoD) | 1.9 ng/L | Per CLSI EP17-A2. |
| Functional Sensitivity (CV=20%) | 1.8 ng/L | Serially diluted control reagents, tested 20 times. |
| Functional Sensitivity (CV=10%) | 3.3 ng/L | Serially diluted control reagents, tested 20 times. |
| Precision (at 106 ng/L) | 2.5% CV | 2 levels of control material run 5x/day over 5 days (CLSI EP05-A3). |
| 99th Percentile URL (Overall) | 14.4 ng/L | Measured in 1004 healthy individuals with eGFR ≥60 mL/min/1.73 m². |
| 99th Percentile URL (Male) | 17.0 ng/L | - |
| 99th Percentile URL (Female) | 13.9 ng/L | - |
| Correlation with Roche Elecsys | r = 0.95 | Passing-Bablok regression & Bland-Altman analysis (n=2,151 samples). |
The Sysmex HISCL hs-cTnT assay meets the criteria for a high-sensitivity test, as it demonstrated a CV <10% at the 99th percentile URL and could measure troponin levels above the LoD in more than 50% of the healthy reference population [3] [82]. The study also highlighted the importance of considering biological variables, noting that hs-cTnT levels increased with age and decreasing estimated glomerular filtration rate (eGFR).
Experimental Protocols for Sensitivity Validation
A robust validation plan is built on standardized experimental protocols. The following section details key methodologies cited in the performance comparisons.
Protocol for Establishing Functional Sensitivity (Precision Profile)
This protocol is used to determine the Lowest Limit of Quantitation (LLOQ) and is adapted from CLSI guideline EP05-A3 and applications in the cited studies [24] [3].
- Objective: To determine the lowest concentration of an analyte that can be measured with an inter-assay CV ≤20%.
- Materials:
- Samples: Prepare a series of low-concentration pooled patient samples or quality control materials spanning the expected low-end range of the assay. The matrix should mimic the clinical sample type (e.g., human serum).
- Instrumentation: The analytical platform under validation.
- Procedure:
- Sample Preparation: Create a dilution series of the low-concentration pool. A minimum of 5 different concentration levels is recommended.
- Data Collection: Analyze each concentration level in duplicate, in at least two separate runs per day, over 5 to 10 days. This provides a minimum of 20 data points per concentration.
- Statistical Analysis:
- For each concentration level, calculate the mean, standard deviation (SD), and coefficient of variation (CV%).
- Plot the CV% against the analyte concentration to generate a precision profile.
- The functional sensitivity (LLOQ) is defined as the lowest concentration at which the CV is ≤20%.
- Application Note: In the Tg study, the functional sensitivities for the hsTg and ultraTg assays were defined as 0.2 ng/mL and 0.06 ng/mL, respectively, following this general principle [24].
Protocol for Method Comparison
This protocol is essential when validating a new assay against an established comparator, as demonstrated in the Sysmex hs-cTnT evaluation [3] [82].
- Objective: To evaluate the agreement and potential bias between two measurement procedures.
- Materials:
- Samples: A minimum of 100-200 patient samples covering the measuring interval of the assay. The sample size can be larger for a more comprehensive evaluation (e.g., n=2,151 in the Sysmex study).
- Procedure:
- Sample Analysis: Measure all samples using both the new test method and the comparator method within a time frame that ensures sample stability.
- Statistical Analysis:
- Passing-Bablok Regression: A non-parametric method used to calculate the regression equation (slope and intercept) between the two methods. It is robust to outliers and does not assume a normal distribution of errors.
- Bland-Altman Analysis: A plot of the differences between the two methods against their averages. This visualization helps identify systematic bias and checks if the bias is consistent across the concentration range.
- Interpretation: The correlation coefficient (r), the slope of the regression line (ideally close to 1), and the mean difference in the Bland-Altman plot (ideally close to zero) are key indicators of agreement.
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key reagents and materials critical for executing the experimental protocols described in this validation plan.
Table 3: Key Research Reagent Solutions for Analytical Validation
| Item | Function / Purpose | Example from Search Context |
|---|---|---|
| Calibrators | Substances used to adjust an instrument's response and create a calibration curve for converting signal into concentration. | HISCL hs-cTnT assay uses 6 levels of calibrators (C0 to C5) [3]. |
| Control Materials | Stable materials with known concentration ranges used to monitor the precision and stability of the assay over time. | Two levels of HISCL control material were used for precision testing [3]. |
| Reference Panel (Patient Samples) | A set of well-characterized clinical samples used for method comparison and correlation studies. | 2,151 samples were used for Sysmex/Roche method comparison [82]. |
| Healthy Cohort Samples | Samples from carefully screened healthy individuals used to establish reference intervals and the 99th percentile URL. | 1,004 cardio-renal healthy individuals defined the 99th percentile for hs-cTnT [3]. |
| Troponin T / Thyroglobulin Assay Kits | Commercial kits containing all necessary antibodies, reagents, and buffers for specific analyte detection. | BRAHMS Dynotest Tg-plus (hsTg) and RIAKEY Tg IRMA (ultraTg) kits [24]. |
| CLSI Guidelines (EP05, EP17, etc.) | Standardized protocols published by the Clinical and Laboratory Standards Institute ensuring consistent and rigorous experimental design. | Referenced for LoB/LoD (EP17) and precision (EP05) testing [3]. |
Setting Analytical Performance Specifications (APS)
Beyond establishing an assay's performance, a validation plan must define the acceptable limits for that performance. The Milan consensus outlines models for setting Analytical Performance Specifications (APS). A 2025 study illustrated an approach using statistical simulation to set APS for bias based on clinical outcomes (Model 1b) [83].
- Model 1 (Clinical Outcomes): Sets APS based on the impact of analytical performance on clinical decisions. This can be direct (Model 1a) or indirect, by assessing the effect on classification of patients (Model 1b).
- Model 2 (Biological Variation): Sets APS based on the known within-subject and between-subject biological variation of an analyte.
- Model 3 (State of the Art): Sets APS based on the highest level of performance currently achievable by the majority of available methods.
The simulation study used data from the National Health and Nutrition Examination Survey (NHANES) and defined a tolerable "reclassification rate" of 1.9% (the increase in flagging rate due to analytical bias) as a clinical performance criterion. It then simulated analytical bias to determine the maximum bias that would not exceed this reclassification rate for common clinical chemistry measurands [83]. This approach aligns APS directly with the test's intended clinical use, ensuring it is "fit-for-purpose."
A comprehensive analytical validation plan is a multi-faceted endeavor that moves from basic technical characterization to establishing clinical utility. The comparison between assay generations reveals a clear trend towards ever-increasing sensitivity, which offers the potential for earlier disease detection and more nuanced patient monitoring. However, this advancement comes with the responsibility to rigorously validate these new tools against clinically relevant endpoints, such as functional sensitivity and predictive value for patient outcomes, as demonstrated in the Tg and hs-cTnT studies.
The adoption of ultrasensitive assays necessitates a re-evaluation of established clinical decision thresholds and a clear understanding of the potential trade-offs, such as reduced specificity leading to more classifications of "biochemical" disease. By employing standardized experimental protocols, such as precision profiles and method comparison studies, and by setting Analytical Performance Specifications grounded in clinical outcomes, researchers and drug developers can ensure that the analytical methods they rely on are not only technically sophisticated but also robust, reliable, and ultimately capable of generating data that improves patient care.
Comparative Analysis of Sensitivity Metrics Across Commercial Platforms
The performance of diagnostic assays is fundamentally governed by two critical metrics: analytical sensitivity and functional sensitivity. Analytical sensitivity, often defined by the limit of detection (LoD), represents the lowest concentration of an analyte that an assay can reliably distinguish from zero. Functional sensitivity, typically characterized by the limit of quantitation (LoQ) at a specified coefficient of variation (CV), reflects the lowest concentration at which an assay can precisely measure the analyte with reproducible accuracy. For researchers, clinicians, and drug development professionals, understanding the nuanced differences in how commercial platforms implement and report these sensitivities is paramount for selecting appropriate assays, interpreting low-level results, and ensuring data reliability across clinical and research settings. This guide provides a structured, data-driven comparison of sensitivity performances across several commercial diagnostic platforms, focusing on real-world applications in areas such as cardiology, endocrinology, and virology.
Comparative Performance Data Tables
The following tables consolidate key sensitivity metrics from recent evaluations of commercial assays, allowing for direct cross-platform comparison.
Cardiac and Thyroid Assay Performance
Table 1: Comparative Sensitivity Metrics for Cardiac and Thyroid Assays
| Analyte (Platform) | Analytical Sensitivity (LoD) | Functional Sensitivity (LoQ) | 99th Percentile URL (Healthy Cohort) | Key Correlation (vs. Comparator) |
|---|---|---|---|---|
| hs-cTnT (Sysmex HISCL) [3] | 1.9 ng/L | 3.3 ng/L (CV 10%) | 14.4 ng/L (Overall) | r = 0.95 vs. Roche Elecsys [3] |
| hs-cTnT (Roche Elecsys) [3] | Not explicitly stated | Established benchmark | Established benchmark | Benchmark for comparison |
| UltraSensitive Tg (RIAKEY IRMA) [5] | 0.01 ng/mL | 0.06 ng/mL | Not Applicable | R = 0.79 vs. hsTg [5] |
| Highly Sensitive Tg (BRAHMS Dynotest) [5] | 0.1 ng/mL | 0.2 ng/mL | Not Applicable | R = 0.79 vs. ultraTg [5] |
SARS-CoV-2 RT-qPCR Pooling Efficiency
Table 2: Impact of Sample Pooling on Assay Sensitivity and Efficiency [84]
| Pool Size | Estimated Ct Value Shift | Pooling Efficiency | Resulting Analytical Sensitivity |
|---|---|---|---|
| 4-Sample Pool | Moderate | Maximized | 87.18% - 92.52% |
| 8-Sample Pool | Significant | Moderate / Low | Significantly Dropped |
| 12-Sample Pool | Very Significant | No considerable savings | 77.09% - 80.87% |
Detailed Experimental Protocols
To ensure the reproducibility of the comparative data, this section outlines the core methodologies employed in the cited studies.
Protocol for High-Sensitivity Cardiac Troponin T (hs-cTnT) Assay Evaluation
The performance verification of the Sysmex HISCL hs-cTnT assay followed established clinical and laboratory standards to ensure robustness and reliability [3].
- Limit of Blank (LoB) and Limit of Detection (LoD) Determination: These were conducted in accordance with the Clinical and Laboratory Standards Institute (CLSI) EP17-A2 guidelines. The LoB was established at 1.3 ng/L, and the LoD at 1.9 ng/L [3].
- Functional Sensitivity (LoQ) Assessment: The limit of quantitation was determined by serially diluting control reagents and testing each dilution repeatedly (20 times). The functional sensitivity was defined as the concentration at which the assay achieved a CV of 10%, which was found to be 3.3 ng/L. The concentration corresponding to a 20% CV was 1.8 ng/L [3].
- Precision Testing: Assay precision was evaluated according to CLSI EP05-A3 guidelines. Two levels of control materials were run five times daily over five days. The demonstrated precision was 2.2% CV at 3,253 ng/L and 2.5% CV at 106 ng/L [3].
- Method Comparison: A total of 2,151 samples were analyzed in parallel on the Sysmex HISCL-5000 and the Roche Elecsys analyzers. Agreement between the two methods was assessed using Passing-Bablok regression analysis and Bland-Altman plots [3].
- 99th Percentile URL Derivation: The 99th percentile upper reference limits (URLs) were derived from a cardio-renal healthy population of 1,004 individuals with no known history of hypertension, diabetes, and an estimated glomerular filtration rate (eGFR) ≥ 60 mL/min/1.73 m² [3].
Protocol for Ultrasensitive vs. Highly Sensitive Thyroglobulin Assay Comparison
This study directly compared the clinical performance of second-generation (highly sensitive) and third-generation (ultrasensitive) thyroglobulin assays in monitoring differentiated thyroid cancer (DTC) patients [5].
- Patient Cohort: The study included 268 DTC patients who had undergone total thyroidectomy and either radioiodine treatment or I-123 diagnostic scanning. Blood samples were collected for both unstimulated and TSH-stimulated conditions [5].
- Assay Methods: Each serum sample was measured using two immunoradiometric assay (IRMA) kits:
- Highly Sensitive Tg (hsTg): BRAHMS Dynotest Tg-plus assay (functional sensitivity: 0.2 ng/mL; analytical sensitivity: 0.1 ng/mL).
- Ultrasensitive Tg (ultraTg): RIAKEY Tg IRMA assay (functional sensitivity: 0.06 ng/mL; analytical sensitivity: 0.01 ng/mL). Tg antibody (TgAb) levels were also determined to identify and account for potential interference [5].
- Statistical Analysis: The correlation between the two assays was assessed using Pearson correlation. The predictive performance of unstimulated Tg levels (from both assays) for stimulated Tg levels ≥1 ng/mL was analyzed, including receiver operating characteristic (ROC) curve analysis to determine optimal clinical cut-offs [5].
Protocol for SARS-CoV-2 Sample Pooling Model
This study developed a mathematical model to optimize sample pooling strategies for SARS-CoV-2 testing, balancing reagent efficiency with analytical sensitivity [84].
- Experimental Design: Thirty samples were tested both individually and in pools ranging from 2 to 12 samples. The Ct (cycle threshold) value shift for each pool size was estimated using Passing-Bablok regressions [84].
- Sensitivity Estimation: The impact of Ct value shifts on overall test sensitivity was estimated in the context of the distribution of 1,030 individually evaluated positive samples. This allowed researchers to model how pooling diluted positive samples and affected the probability of detection [84].
- Efficiency Calculation: Reagent efficiency gains were calculated based on the reduction in the number of individual tests required. The "sweet spot" for pooling was identified as the point that maximized reagent savings without an unacceptable drop in sensitivity [84].
Visualizing the Comparative Analysis Workflow
The following diagram illustrates the logical workflow for conducting a comparative analysis of sensitivity metrics, as applied in the studies discussed.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials critical for conducting rigorous sensitivity analyses in a laboratory setting.
Table 3: Key Reagent Solutions for Sensitivity Analysis
| Reagent / Material | Function in Sensitivity Analysis | Example from Cited Research |
|---|---|---|
| Calibrators | A series of standards with known analyte concentrations used to construct the assay's calibration curve, defining the relationship between signal and concentration. | Sysmex HISCL hs-cTnT assay utilizes 6 levels of calibrators (C0 to C5) [3]. |
| Control Materials | Stable samples with predetermined analyte concentrations used to monitor the precision and stability of the assay over time (within-run and between-day). | Two levels of HISCL control material were used for precision testing over 5 days [3]. |
| Immunoassay Kits | Integrated kits containing all necessary antibodies (e.g., monoclonal mouse anti-TnT), magnetic particles, and enzyme labels for performing specific sandwich immunoassays. | Sysmex HISCL hs-cTnT and BRAHMS/RIAKEY Tg IRMA kits were used in the comparisons [3] [5]. |
| Chemiluminescent Substrate | A reagent that produces light upon reaction with an enzyme label (e.g., alkaline phosphatase). The light signal is measured and is proportional to the analyte concentration. | The HISCL assay uses a chloro-dioxetane phenyl phosphate substrate [3]. |
| Specimen Diluent | A solution used to dilute samples that exceed the analytical measurement range of the assay or, in some cases, to prepare serial dilutions for LoQ studies. | HISCL diluent was used to serially dilute control reagents for the functional sensitivity study [3]. |
| Pooling Matrix | A sterile, neutral medium used to combine multiple patient samples (e.g., nasopharyngeal swabs) into a single pool for efficient high-throughput screening. | Implied but not specified in the SARS-CoV-2 pooling study [84]. |
The comparative data unequivocally demonstrates a clear trade-off in the performance of diagnostic assays, often between ultimate sensitivity and clinical specificity. For instance, in thyroid cancer monitoring, the ultrasensitive Tg assay showed superior sensitivity (72.0%) in predicting stimulated Tg levels ≥1 ng/mL, correctly identifying more patients with potential recurrence. However, this came at the cost of lower specificity (67.2%) compared to the highly sensitive Tg assay (sensitivity 39.8%, specificity 91.5%) [5]. This means the ultraTg assay may correctly flag more true recurrences but also generates more false positives, potentially leading to more frequent classifications of "biochemical incomplete response" and unnecessary patient anxiety and follow-up testing.
Furthermore, the concept of functional sensitivity is critical for real-world application. An assay might detect an analyte at a very low level (good LoD) but cannot be trusted for precise clinical decision-making at that level if its precision is poor. The Sysmex HISCL hs-cTnT assay demonstrates this by achieving a 10% CV at 3.3 ng/L, a level well below its derived 99th percentile URL of 14.4 ng/L, ensuring reliable measurement at clinically relevant thresholds [3]. Finally, strategies like sample pooling highlight that sensitivity is not an isolated metric but is intrinsically linked to operational efficiency. Maximizing testing capacity, as during a pandemic, may require a deliberate and calculated trade-off in analytical sensitivity, as evidenced by the optimal 4-sample pool strategy [84].
In conclusion, the selection of a commercial diagnostic platform should not be based on a single sensitivity metric in isolation. Researchers and clinicians must adopt a holistic view, considering the analytical goals (e.g., earliest possible detection vs. precise quantification at a clinical cut-off), the clinical consequences of false positives and false negatives, and the operational context. The most sensitive assay is not always the best; the most appropriate assay is the one whose performance characteristics are strategically aligned with the intended clinical or research question.
The rigorous evaluation of diagnostic assays is fundamental to biomedical research and development, particularly for tests that inform critical clinical decisions. Statistical tools such as precision profiles, Receiver Operating Characteristic (ROC) curves, and confidence intervals provide the quantitative framework needed to objectively compare assay performance. These methodologies allow researchers to characterize key parameters including analytical sensitivity, which represents the lowest detectable concentration of an analyte, and functional sensitivity, defined as the lowest concentration measurable with a specified precision, typically expressed as a coefficient of variation (CV) of 20% or 10% [3]. In drug development and clinical diagnostics, understanding the distinction and relationship between these sensitivity measures is crucial for determining whether an assay is suitable for its intended purpose, especially when monitoring disease recurrence or low-level biomarkers.
This guide provides a structured comparison of these statistical evaluation methods, framed within the context of analytical versus functional sensitivity performance research. We present experimental data and protocols that enable direct comparison between diagnostic assays, with a focus on applications relevant to researchers, scientists, and drug development professionals. The content emphasizes practical implementation, data interpretation, and the essential materials required for conducting robust assay evaluations.
Experimental Data Comparison of Diagnostic Assays
High-Sensitivity Cardiac Troponin T (hs-cTnT) Assay Comparison
The analytical performance of the new Sysmex HISCL hs-cTnT assay was systematically compared against the established Roche Elecsys hs-cTnT assay in a comprehensive method comparison study [3]. The evaluation followed standardized clinical laboratory protocols to characterize key performance parameters.
Table 1: Analytical Performance Comparison of Sysmex HISCL vs. Roche Elecsys hs-cTnT Assays
| Performance Parameter | Sysmex HISCL hs-cTnT | Roche Elecsys hs-cTnT |
|---|---|---|
| Limit of Blank (LoB) | 1.3 ng/L | Not specified in study |
| Limit of Detection (LoD) | 1.9 ng/L | Not specified in study |
| Functional Sensitivity (20% CV) | 1.8 ng/L | Not specified in study |
| Functional Sensitivity (10% CV) | 3.3 ng/L | Not specified in study |
| Assay Precision at 106 ng/L | 2.5% CV | Not specified in study |
| Assay Precision at 3253 ng/L | 2.2% CV | Not specified in study |
| Measurement Range | 2-10,000 ng/L | Not specified in study |
| 99th Percentile URL (Overall) | 14.4 ng/L | Established values used |
| 99th Percentile URL (Male) | 17.0 ng/L | Established values used |
| 99th Percentile URL (Female) | 13.9 ng/L | Established values used |
| Correlation with Roche Assay | r = 0.95 (n=2151) | Reference method |
The correlation between the Sysmex HISCL and Roche Elecsys assays was evaluated using Passing-Bablok regression analysis, demonstrating excellent agreement (r = 0.95) across 2,151 samples [3]. Bland-Altman analysis revealed a mean absolute difference of 3.5 ng/L for samples with hs-cTnT ≤ 52 ng/L, while for higher concentrations (>52 ng/L) the mean difference was 2.8%. These results confirmed that the Sysmex HISCL hs-cTnT assay meets the criteria for a high-sensitivity assay based on international guidelines, with a CV below 10% at the 99th percentile upper reference limit (URL) and measurable levels above the limit of detection in more than 50% of healthy individuals [3].
Ultrasensitive vs. Highly Sensitive Thyroglobulin Assay Comparison
A comparative study evaluated the performance of ultrasensitive thyroglobulin (ultraTg) and highly sensitive thyroglobulin (hsTg) assays in monitoring differentiated thyroid cancer (DTC) patients [5]. The study aimed to determine whether unstimulated Tg levels could predict stimulated Tg values ≥1 ng/mL without thyroid-stimulating hormone (TSH) stimulation.
Table 2: Performance Comparison of Ultrasensitive vs. Highly Sensitive Thyroglobulin Assays
| Performance Parameter | Ultrasensitive Tg (RIAKEY) | Highly Sensitive Tg (BRAHMS) |
|---|---|---|
| Analytical Sensitivity | 0.01 ng/mL | 0.1 ng/mL |
| Functional Sensitivity | 0.06 ng/mL | 0.2 ng/mL |
| Correlation Between Assays | R=0.79 (P<0.01) | R=0.79 (P<0.01) |
| Correlation in TgAb-Positive Patients | R=0.52 | R=0.52 |
| Optimal Cut-off for Predicting Stimulated Tg ≥1 ng/mL | 0.12 ng/mL | 0.105 ng/mL |
| Sensitivity at Optimal Cut-off | 72.0% | 39.8% |
| Specificity at Optimal Cut-off | 67.2% | 91.5% |
| Clinical Cases Identified | 8 discordant cases with low hsTg but elevated ultraTg | Missed 3 recurrences identified by ultraTg |
The ultraTg assay demonstrated significantly higher sensitivity (72.0% vs. 39.8%) in predicting stimulated Tg levels ≥1 ng/mL, potentially allowing for earlier detection of recurrence [5]. However, this increased sensitivity came at the cost of reduced specificity (67.2% vs. 91.5%), which may lead to more frequent classifications of biochemical incomplete response. The study identified eight discordant cases where ultraTg was elevated while hsTg remained low; three of these patients developed structural recurrence within 3.4 to 5.8 years, suggesting the potential clinical value of ultraTg in specific cases where clinical suspicion remains high despite low hsTg levels [5].
Experimental Protocols and Methodologies
Assay Evaluation Protocol for High-Sensitivity Assays
The experimental protocol for evaluating the Sysmex HISCL hs-cTnT assay followed established clinical laboratory guidelines [3]:
Sample Preparation and Storage: The study utilized anonymized, de-identified leftover sera stored at -70°C if not immediately analyzed. This preservation method maintains analyte stability and prevents degradation during storage.
Determination of Analytical Sensitivity Parameters:
- Limit of Blank (LoB) and Limit of Detection (LoD): These were determined according to Clinical and Laboratory Standards Institute (CLSI) EP17-A2 guidelines. The LoB represents the highest apparent analyte concentration expected to be found when replicates of a blank sample containing no analyte are tested, while the LoD is the lowest analyte concentration likely to be reliably distinguished from the LoB.
- Limit of Quantitation (Functional Sensitivity): The functional sensitivity was determined using serial dilutions of control reagents to obtain multiple testing points. Each point was tested 20 times to establish the CV% at different concentrations. The functional sensitivity was defined as the concentration corresponding to CVs of 20% and 10% through curve-fitting of the results [3].
Precision Evaluation: Assay precision was assessed using two levels of control material run five times daily over five days according to CLSI EP05-A3 guidelines. This protocol evaluates both within-run and between-day precision to characterize total assay variability [3].
Method Comparison: Samples were analyzed on both the Sysmex HISCL and Roche Elecsys analyzers. Statistical comparison included Passing-Bablok regression to assess agreement and Bland-Altman analysis to evaluate bias across the measurement range. Values below the claimed limit of quantitation (1.5 ng/L) were reported as 1.5 ng/L for analysis purposes [3].
Establishment of Reference Intervals: The 99th percentile upper reference limits (URLs) were derived from a cardio-renal healthy population (n=1004) with no known history of hypertension, diabetes, and an estimated glomerular filtration rate (eGFR) ≥60 mL/min/1.73 m². Creatinine was measured using the Roche Elecsys assay, and eGFR was calculated using the CKD-EPI equation [3].
Diagram 1: High-Sensitivity Assay Evaluation Workflow (76 characters)
Protocol for Comparing Ultrasensitive and Highly Sensitive Assays
The comparative study of thyroglobulin assays implemented the following methodology [5]:
Subject Selection and Inclusion Criteria: The study included 268 patients with differentiated thyroid cancer (DTC) who had undergone total thyroidectomy and either radioiodine treatment or I-123 diagnostic scanning. Patients were enrolled when planning to undergo radioiodine treatment or an I-123 diagnostic scan, with written informed consent obtained from all participants.
Sample Collection and Stimulation Protocols:
- Unstimulated Samples: Serum samples were collected after total thyroidectomy without TSH stimulation.
- Stimulated Samples: Stimulated samples were obtained after TSH stimulation, performed either through levothyroxine withdrawal or intramuscular injection of recombinant human TSH (rhTSH). rhTSH stimulation involved a 2-day course of intramuscular injections of 0.9 mg rhTSH administered 2 days prior to radioiodine intake.
Assay Methodology: Two immunoradiometric assay (IRMA) kits representing different generations of Tg assays were utilized:
- Second-generation (hsTg): BRAHMS Dynotest Tg-plus assay with functional sensitivity of 0.2 ng/mL and analytical sensitivity of 0.1 ng/mL.
- Third-generation (ultraTg): RIAKEY Tg IRMA kit with functional sensitivity of 0.06 ng/mL and analytical sensitivity of 0.01 ng/mL.
Interference Management: Tg antibody (TgAb) levels were determined using the Dynotest Anti-Tg kit. A TgAb titer below 60 U/mL was considered negative, and interference in serum Tg measurement due to serum autoantibodies was adjusted accordingly.
Statistical Analysis: Analyses were performed using R version 4.3.2. For continuous variables, the analytical sensitivity value was substituted for Tg values below the analytical sensitivity threshold within each Tg assay. The Pearson correlation coefficient was calculated using the merged dataset to assess reliability between hsTg and ultraTg assays.
Statistical Analysis Methods
ROC Curve Analysis and Precision-Recall Curves
ROC analysis is a fundamental statistical tool for evaluating the diagnostic accuracy of medical tests, quantifying how effectively a test can discriminate between two patient states (typically "diseased" and "non-diseased") [85]. The ROC curve illustrates the relationship between the true positive rate (sensitivity) and the false positive rate (1-specificity) across all possible threshold values [85].
Key ROC Analysis Concepts:
- Area Under the Curve (AUC): The AUC provides a single measure of overall diagnostic performance, with values ranging from 0.5 (no discrimination) to 1.0 (perfect discrimination). The AUC represents the probability that a randomly selected diseased subject will have a higher test result than a randomly selected non-diseased subject [85].
- Optimal Cut-off Determination: The point on the ROC curve closest to the upper left corner (0,1) typically represents the optimal cut-off value, maximizing both sensitivity and specificity. Alternatively, cost-benefit analysis or predefined clinical requirements can guide cut-off selection.
Precision-Recall Curves: As an alternative to ROC curves, precision-recall curves plot precision (positive predictive value) against recall (sensitivity) for different thresholds [86]. These curves are particularly informative when evaluating binary classifiers on imbalanced datasets, where one class significantly outnumbers the other [86].
Statistical Comparison of Curves: MedCalc and other statistical software packages enable comparison of ROC or precision-recall curves from two diagnostic tests. The analysis calculates the difference between the areas under the curves (AUC or AUPRC) together with the 95% BCa bootstrap confidence interval for this difference. If the confidence interval does not include zero, the two areas are considered significantly different (p<0.05) [86].
Diagram 2: Statistical Evaluation Relationships (76 characters)
Calculation of Confidence Intervals
Confidence intervals provide essential information about the precision of estimated performance metrics and are particularly important when comparing diagnostic assays.
Confidence Intervals for AUPRC: The 95% confidence interval for the Area Under the Precision-Recall Curve (AUPRC) can be calculated using the logit method [86]:
$$ CI(AUPRC) = \left[ \frac{e^{\mu\eta - 1.96 \tau}}{1+ e^{\mu\eta - 1.96 \tau}} \; ; \; \frac{e^{\mu\eta + 1.96 \tau}}{1+ e^{\mu\eta + 1.96 \tau}} \right] $$
where $$ \mu_\eta = logit(AUPRC) = \ln \left ( \frac {AUPRC} {1-AUPRC} \right ) $$ and $$ \tau = \frac{1}{\sqrt{nAUPRC(1-AUPRC)}} $$
Bootstrap Confidence Intervals: Modern statistical software often employs bootstrap techniques to compute confidence intervals for AUC or AUPRC differences. The BCa (Bias-Corrected and Accelerated) bootstrap method is commonly used, which adjusts for bias and skewness in the distribution of estimated parameters [86]. When comparing two precision-recall curves, MedCalc reports the difference between the two AUPRCs with the 95% BCa bootstrap confidence interval for this difference. If this interval does not include zero, the two areas are considered statistically significantly different (p<0.05) [86].
Implementation in Statistical Software: Tools such as MATLAB's rocmetrics object enable computation of performance metrics for ROC curves, including pointwise confidence intervals when using bootstrap methods or cross-validated data [87]. Similarly, MedCalc Statistical Software provides comprehensive tools for comparing ROC curves or precision-recall curves with appropriate confidence interval estimation [86].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Diagnostic Assay Evaluation
| Reagent/Material | Function/Application | Example from Literature |
|---|---|---|
| Immunoassay Calibrators | Establish standard curve for quantitative measurements | HISCL troponin T hs calibrators (C0-C5) with 90-day post-reconstitution shelf life [3] |
| Control Materials | Monitor assay precision and accuracy over time | Two-level HISCL control materials for precision verification [3] |
| Diluent Solutions | Matrix for sample dilution and preparation | HISCL diluent for serial dilution in functional sensitivity studies [3] |
| Stable Reference Samples | Method comparison and longitudinal performance monitoring | Archived serum samples stored at -70°C [3] |
| Antibody Reagents | Analyte detection and quantification | Mouse anti-TnT-coated magnetic particles and alkaline-phosphatase-labeled monoclonal mouse anti-TnT [3] |
| Signal Generation Reagents | Produce detectable signal proportional to analyte | Chemiluminescent substrate (chloro-dioxetane phenyl phosphate) [3] |
| Interference Testing Materials | Evaluate assay specificity | Samples with known interfering substances (e.g., TgAb-positive samples) [5] |
| Matrix-matched Materials | Address matrix effects in sample preparation | Human serum-based calibrators [3] |
The statistical evaluation of diagnostic assays through precision profiles, ROC curves, and confidence intervals provides a rigorous framework for comparing analytical performance, particularly in the context of analytical versus functional sensitivity. The experimental data presented demonstrates that while higher sensitivity assays can improve early detection of disease recurrence (as shown in the thyroglobulin comparison), this often comes with a trade-off in specificity that must be carefully considered in clinical contexts [5]. Similarly, the comparison between the Sysmex HISCL and Roche Elecsys hs-cTnT assays illustrates the comprehensive approach needed to validate that new assays meet established performance criteria for high-sensitivity applications [3].
The experimental protocols and statistical methods outlined in this guide provide researchers with standardized approaches for conducting robust assay evaluations. As diagnostic technologies continue to evolve toward increasingly sensitive assays, these statistical evaluation methods will remain essential for objectively characterizing performance and ensuring that new diagnostic tools provide clinically meaningful information for patient management.
Linking Analytical Performance to Clinical Sensitivity and Specificity
In the critical field of diagnostic medicine and preclinical drug development, understanding the distinction and relationship between analytical performance and clinical diagnostic performance is paramount. While analytical sensitivity and functional sensitivity describe an assay's technical capability to detect minute quantities of an analyte, clinical sensitivity and specificity determine how effectively a test identifies truly diseased and non-diseased individuals in a population. This guide objectively compares these performance characteristics, provides detailed experimental protocols for their determination, and explores how advanced models like organ-chips are bridging the translational gap between analytical capabilities and clinical utility. Through structured data presentation and methodological breakdowns, we equip researchers and drug development professionals with the framework to evaluate diagnostic tools and preclinical models comprehensively.
Defining the Performance Spectrum
Analytical Sensitivity vs. Functional Sensitivity
Analytical sensitivity represents the fundamental detection capability of an assay, formally defined as the smallest amount of a substance in a sample that can be accurately measured by an assay [88] [89]. It is determined through statistical analysis of blank samples, calculating the concentration equivalent to the mean measurement of the blank plus 2 standard deviations (for immunometric assays) [10]. This parameter is often referred to as the "detection limit" [10].
In contrast, functional sensitivity describes the lowest analyte concentration that can be measured with a defined precision level, typically expressed as a coefficient of variation (CV) ≤ 20% [9] [10]. This concept was developed in response to the limited clinical utility of analytical sensitivity, as it accounts for the practical reality that assay imprecision increases rapidly at very low concentrations [10]. Functional sensitivity thus represents "the lowest concentration at which an assay can report clinically useful results" [9], incorporating both precision and accuracy considerations that align more closely with clinical requirements.
Clinical Sensitivity vs. Specificity
Clinical (diagnostic) sensitivity measures a test's ability to correctly identify individuals who have the disease, calculated as the proportion of true positives out of all individuals with the disease [90] [91]. Mathematically, this is expressed as:
Clinical (diagnostic) specificity measures a test's ability to correctly identify individuals without the disease, calculated as the proportion of true negatives out of all disease-free individuals [90] [91]:
These clinical performance metrics are fundamentally different from analytical performance characteristics, as they evaluate how effectively a test classifies patients in real-world scenarios rather than its technical detection capabilities [9] [88].
Table 1: Comparison of Key Performance Metrics
| Performance Metric | Definition | Primary Focus | Typical Determination Method |
|---|---|---|---|
| Analytical Sensitivity | Smallest amount of analyte that can be detected | Technical detection capability | Mean blank + 2SD (zero concentration sample) [10] |
| Functional Sensitivity | Lowest concentration measurable with defined precision (CV ≤ 20%) | Clinically usable detection | Patient samples at different concentrations analyzed over multiple runs [9] [10] |
| Clinical Sensitivity | Ability to correctly identify diseased individuals | Patient classification - true positives | Comparison to gold standard in known positive population [90] [91] |
| Clinical Specificity | Ability to correctly identify non-diseased individuals | Patient classification - true negatives | Comparison to gold standard in known negative population [90] [91] |
Experimental Protocols for Performance Characterization
Determining Analytical and Functional Sensitivity
- Sample Preparation: Obtain a true zero concentration sample with an appropriate matrix (analyte-free)
- Replication: Assay 20 replicates of the zero sample
- Calculation: Determine mean and standard deviation (SD) of measured counts (CPS)
- Result Interpretation: For immunometric assays, analytical sensitivity = concentration equivalent to mean counts + 2SD
- Sample Selection: Obtain multiple patient samples or pools with concentrations spanning the target low range
- Dilution Series: Prepare samples at different dilution levels if necessary
- Extended Testing: Analyze samples repeatedly over multiple different runs (days/weeks)
- Precision Calculation: Calculate CV for each concentration level
- Threshold Determination: Identify the concentration at which CV reaches ≤20% through interpolation if needed
Establishing Clinical Sensitivity and Specificity
- Study Population: Recruit subjects with and without the target condition (using gold standard diagnosis)
- Blinded Testing: Perform index test on all subjects without knowledge of true disease status
- 2x2 Table Construction: Cross-tabulate index test results against true disease status
- Calculation:
- Clinical Sensitivity = True Positives / (True Positives + False Negatives)
- Clinical Specificity = True Negatives / (True Negatives + False Positives)
- Additional Metrics:
- Positive Predictive Value = True Positives / (True Positives + False Positives)
- Negative Predictive Value = True Negatives / (True Negatives + False Negatives)
The Relationship Between Analytical and Clinical Performance
The relationship between analytical performance and clinical performance is complex and non-linear. While high analytical sensitivity is often necessary for achieving high clinical sensitivity, it does not guarantee it [89]. Other factors including disease prevalence, patient population characteristics, and pre-analytical variables significantly influence the translation of technical capability to clinical utility.
The following diagram illustrates the conceptual relationship and workflow connecting these performance characteristics:
Figure 1: Relationship between technical and diagnostic performance metrics. While analytical and functional sensitivity establish technical capabilities, their translation to clinical sensitivity and specificity is influenced by multiple biological and operational factors.
Comparative Performance Data: Case Examples
Preclinical Drug Development Models
In preclinical drug development, sensitivity and specificity take on slightly different meanings while retaining their fundamental principles. Model sensitivity describes how successfully a model identifies toxic drug candidates, while model specificity reflects accuracy in identifying non-toxic candidates [92]. Advanced models like the Emulate Liver-Chip demonstrate how optimizing both parameters simultaneously can significantly improve drug development efficiency.
Table 2: Performance Comparison of Preclinical Toxicology Models
| Model System | Reported Sensitivity | Reported Specificity | Key Advantages | Translational Limitations |
|---|---|---|---|---|
| Traditional Animal Models | Varies by species and endpoint | Varies by species and endpoint | Regulatory acceptance, holistic physiology | Species differences, limited human predictability [92] |
| Hepatic Spheroids | Not specified | Threshold set at 50 for specific output | Human cells, moderate throughput | Limited tissue complexity, variable reproducibility |
| Emulate Liver-Chip | 87% | 100% (in cited study) | Human cells, physiological fluid flow, high specificity prevents good drug rejection [92] | Higher complexity, cost, and technical requirements |
Tissue Specificity in Drug Sensitivity
A meta-analysis of pharmacogenomic datasets revealed significant tissue-specific drug sensitivities in vitro, with 63% of tested drugs showing tissue specificity and 8% of total drug-tissue interactions deemed statistically significant [93]. However, the concordance between these preclinical tissue-specific sensitivity patterns and actual clinical indications was remarkably weak (Matthew correlation coefficient = 0.0003, P > .10) [93], highlighting the substantial translational gap between in vitro findings and clinical utility.
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Performance Studies
| Reagent/Material | Function in Performance Characterization | Critical Specifications |
|---|---|---|
| Zero Standard/Blank Matrix | Determines baseline signal for analytical sensitivity | Authentic matrix without analyte; appropriate for assay type [10] |
| Patient-Derived Samples | Evaluation of functional sensitivity and clinical performance | Known disease status; appropriate preservation; ethical sourcing [10] |
| Reference Standards | Calibration and accuracy determination | Traceable purity; stability documentation; matrix-matched when possible |
| Quality Control Materials | Precision assessment across reportable range | Multiple concentration levels; commutability with patient samples |
| Cross-Reactivity Panels | Analytical specificity evaluation | Structurally similar compounds; common concomitant medications |
The journey from exceptional analytical performance to meaningful clinical utility requires careful consideration of the distinct yet interconnected metrics discussed in this guide. While analytical sensitivity establishes the fundamental detection limit and functional sensitivity defines the clinically usable threshold, these technical capabilities only translate to effective clinical sensitivity and specificity when biological variability, disease prevalence, and real-world operating conditions are adequately addressed. Advanced models that maintain high specificity while achieving strong sensitivity, such as organ-chips with their demonstrated 100% specificity and 87% sensitivity in toxicology assessment [92], represent promising approaches for bridging this translational gap. For researchers and drug development professionals, a comprehensive understanding of these performance characteristics—and the methodologies for their proper determination—remains essential for developing diagnostic tools and therapeutic interventions that truly benefit patient care.
In the field of in vitro diagnostics (IVD), the performance of an assay is fundamentally governed by two critical parameters: analytical sensitivity and functional sensitivity. Analytical sensitivity, often referred to as the Limit of Detection (LoD), is the lowest concentration of an analyte that an assay can reliably distinguish from zero. It represents a fundamental characteristic of the assay's ability to detect minute quantities of a substance. Functional sensitivity, in contrast, is a more practical measure. It is typically defined as the lowest analyte concentration that an assay can measure with a specified level of precision, usually expressed as a coefficient of variation (CV), such as 10% or 20% [3]. Understanding the distinction and relationship between these two parameters is essential for researchers and drug development professionals when selecting and validating diagnostic assays for clinical use and regulatory approval.
This guide provides an objective comparison of performance data from leading diagnostic assays, detailing the experimental protocols used to derive key sensitivity metrics. The focus is on empowering professionals to make informed decisions by interpreting sensitivity data within the context of robust methodological frameworks.
Comparative Performance Data of Diagnostic Assays
The following tables summarize key performance metrics from recent studies and product evaluations for various diagnostic technologies, focusing on analytical and functional sensitivity.
Table 1: Performance Metrics of High-Sensitivity Cardiac Troponin T (hs-cTnT) Assays
| Assay / Parameter | Roche Elecsys hs-cTnT | Sysmex HISCL hs-cTnT |
|---|---|---|
| Limit of Blank (LoB) | Information not provided in search results | 1.3 ng/L [3] |
| Limit of Detection (LoD) | Information not provided in search results | 1.9 ng/L [3] |
| Functional Sensitivity (at 10% CV) | Established benchmark | 3.3 ng/L [3] |
| 99th Percentile URL (Overall) | Established benchmark | 14.4 ng/L [3] |
| Assay Time | 9 minutes [3] | 17 minutes [3] |
Table 2: Performance Metrics of Other Diagnostic Technologies
| Assay / Technology | CRISPR-Cas13 | RT-qPCR Pooling (4-sample pool) |
|---|---|---|
| Primary Application | Nucleic acid detection (e.g., SARS-CoV-2, mutations) [94] | SARS-CoV-2 detection [84] |
| Analytical Sensitivity (LoD) | attomolar (aM) level after PCR amplification [94] | Defined by Ct value shift [84] |
| Reported Diagnostic Sensitivity | >95% [94] | 87.18% - 92.52% [84] |
| Reported Diagnostic Specificity | >99% [94] | Information not provided in search results |
| Key Feature | Portable, rapid (<2 hr), low cost (~$0.05/test) [94] | Maximizes reagent efficiency and testing capacity [84] |
Experimental Protocols for Sensitivity Determination
Protocol for Determining LoB and LoD for hs-cTnT Assays
The determination of LoB and LoD for assays like the Sysmex HISCL hs-cTnT follows established clinical laboratory guidelines to ensure reliability [3].
- Objective: To empirically determine the lowest concentration of troponin T that the instrument can reliably distinguish from a blank sample (LoD) and the concentration at which the assay's precision meets a defined threshold (Functional Sensitivity).
- Materials: Diluent matrix (e.g., Sysmex HISCL diluent), control reagents, the automated immunoassay analyzer (e.g., HISCL-5000).
- Procedure (for LoB/LoD):
- The diluent matrix (a sample containing no analyte) is measured multiple times (e.g., as per CLSI EP17-A2 guidelines) [3].
- The mean and standard deviation (SD) of the results from the blank samples are calculated.
- The LoB is derived from these replicate measurements of the blank [3].
- Low-concentration samples are then measured repeatedly. The LoD is determined as the lowest concentration at which the analyte is reliably detected, typically defined as LoB + a multiple of the SD of low-level samples [3].
- Procedure (for Functional Sensitivity):
- Control reagents are serially diluted to create samples with concentrations near the expected detection limit.
- Each dilution is tested repeatedly (e.g., 20 times) to obtain a mean concentration and the associated CV% for each level [3].
- The results are curve-fitted, and the concentration corresponding to a CV% of 10% is identified as the functional sensitivity [3].
Protocol for Comparative Method Validation
When comparing a new assay to an existing market leader, a rigorous method comparison study is essential, as demonstrated in the validation of the Sysmex HISCL hs-cTnT assay against the Roche Elecsys benchmark [3].
- Objective: To evaluate the agreement between two different assay platforms for measuring the same analyte across a clinically relevant range.
- Materials: A large set of patient samples (e.g., n=2151), covering a wide range of analyte concentrations from low to high; both analyzer platforms (e.g., Sysmex HISCL and Roche Elecsys) [3].
- Procedure:
- Each patient sample is split and tested on both analyzer platforms within a timeframe that ensures sample stability.
- The results from the two methods are compared using statistical regression analysis, such as Passing-Bablok regression, which is non-parametric and robust against outliers and specific error distributions [3].
- The degree of agreement is further quantified using Bland-Altman analysis, which plots the differences between the two methods against their averages, highlighting any systematic bias [3].
- For hs-cTnT assays, performance is also validated against international criteria, which require that at the 99th percentile URL, the assay CV is <10%, and that measurable results are obtained in >50% of healthy individuals [3].
Visualizing Assay Validation and Comparison Workflow
The following diagram illustrates the logical workflow and key decision points in the process of validating and comparing diagnostic assays, from initial setup to final interpretation.
The Scientist's Toolkit: Key Research Reagent Solutions
A successful assay validation relies on a suite of essential materials and reagents. The table below details key components and their critical functions in the experimental process.
Table 3: Essential Materials for Diagnostic Assay Validation
| Item | Function in Validation |
|---|---|
| Automated Immunoassay Analyzer | Platform for performing the assay, ensuring standardized and reproducible measurement of samples (e.g., HISCL-5000, Roche Elecsys analyzer) [3]. |
| Calibrators | A set of samples with known, predefined analyte concentrations used to establish the assay's calibration curve, which is essential for converting signal into a quantitative result [3]. |
| Control Materials | Stable samples with known high and low analyte concentrations, used to monitor the precision and stability of the assay over time and across multiple runs [3]. |
| Matrix-Matched Diluent | A solution that mimics the sample matrix (e.g., human serum) without containing the analyte. It is used for preparing dilutions for LoB/LoD studies and for reconstituting controls and calibrators [3]. |
| Reference Panel of Patient Samples | A well-characterized collection of clinical samples that represents the biological variability of the target population. This is crucial for method comparison studies and for establishing clinical reference ranges [3] [95]. |
Conclusion
A thorough grasp of both analytical and functional sensitivity is non-negotiable for developing clinically viable diagnostic assays. As this article has detailed, moving from foundational concepts through rigorous methodology, optimization, and validation creates a clear pathway from theoretical sensitivity to reliable clinical performance. The future of sensitivity enhancement lies in the strategic integration of advanced materials like nanomaterials for signal amplification [citation:1], computational approaches like AI for intelligent design optimization [citation:3][citation:5], and innovative formats such as dual-modality biosensors for self-validating accuracy [citation:1]. For researchers and drug developers, prioritizing these interconnected metrics is paramount for accelerating the translation of novel biomarkers, meeting stringent regulatory standards, and ultimately delivering precise and actionable diagnostic tools to the clinic.
References
- 1. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 2. Comparison of approaches for assessing detection and ... [https://www.nature.com/articles/s41598-024-83474-5]
- 3. Analytical Performance of the New Sysmex High-Sensitivity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346695/]
- 4. Limit of detection (LQD)/limit of quantitation (LOQ) [https://pubmed.ncbi.nlm.nih.gov/8013092/]
- 5. Comparison of Ultrasensitive and Highly Sensitive Assay to ... [https://www.e-enm.org/journal/view.php?doi=10.3803/EnM.2025.2302]
- 6. Binding the gap between experiments, statistics, and ... [https://www.sciencedirect.com/science/article/pii/S0003267021011685]
- 7. An Explanation of Sensitivity and the LLD, LLOQ, and ... [https://www.quansysbio.com/support/explanation-of-sensitivity-lld-lloq-and-uloq/]
- 8. the limit of detection (LOD) is defined ... [https://www.cytometry.org/web/q_view.php?id=258&searchterm=sensitiv]
- 9. How do analytical, diagnostical, and functional sensitivity differ? [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/sensitivities]
- 10. Analytical Sensitivity, Functional Sensitivity [https://www.dpcweb.com/documents/news&views/spring01/performancemeasures.html]
- 11. Limit of Quantitation - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/limit-of-quantitation]
- 12. The concept of clinical utility for diagnostic tests [https://www.thermofisher.com/blog/clinical-conversations/the-concept-of-clinical-utility-for-diagnostic-tests/]
- 13. The Use of Clinical Utility Assessments in Early Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2664875/]
- 14. Introduction to real-world evidence studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8323556/]
- 15. The relevance of the real-world evidence in research, ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1512429/full]
- 16. Overview of IVD Regulation [https://www.fda.gov/medical-devices/ivd-regulatory-assistance/overview-ivd-regulation]
- 17. Clinical Performance Report under IVDR | A Complete Guide [https://morulaa.com/ivd-eu-ivdr-746-in-vitro-diagnostic-regulation-clinical-performance-report-cpr/]
- 18. In vitro diagnostic medical device performance evaluation [https://blog.johner-institute.com/regulatory-affairs/performance-evaluation-of-in-vitro-diagnostics/]
- 19. US FDA IVD Kit and Non IVD Kit Device - Key Understanding [https://www.i3cglobal.com/us-fda-ivd-kit-and-ivd-non-kit/]
- 20. Laboratory developed tests [https://www.pathologyoutlines.com/topic/managementlabdevelopedtests.html]
- 21. A Comparison of IVDR to FDA IVD Regulatory Submission ... [https://www.rqmplus.com/blog/a-comparison-of-ivdr-to-fda-ivd-regulatory-submission-requirements/]
- 22. Performance Evaluation for FDA 510(k): Building Your ... [https://www.abingdonhealth.com/substantial-equivalence-ivd-fda-510k/]
- 23. Enhancing ELISA Sensitivity: From Surface Engineering to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293621/]
- 24. Comparison of Ultrasensitive and Highly Sensitive Assay to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12602004/]
- 25. Utilizing Digital ELISA for Precise Measurement of Brain ... [https://www.quanterix.com/utilizing-digital-elisa-for-precise-measurement-of-brain-biomarkers-in-blood/]
- 26. An Introduction to the Performance of Immunohistochemistry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6749998/]
- 27. Method Validation Essentials, Limit of Blank ... [https://www.biopharminternational.com/view/method-validation-essentials-limit-blank-limit-detection-and-limit-quantitation]
- 28. Approaches to Assay Characterization and Validation: Part 1 [https://www.quanterix.com/approaches-to-assay-characterization-and-validation-part-1-limit-of-detection-and-lower-limit-of-quantitation/]
- 29. Determination of limit of detection (LOD) for loop-mediated ... [https://www.sciencedirect.com/science/article/abs/pii/S0732889324003924]
- 30. Comparison of the analytical sensitivity of seven commonly ... [https://www.sciencedirect.com/science/article/abs/pii/S1386653220303206]
- 31. emerging data supporting use of JC virus DNA copy number ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12489873/]
- 32. Sensitivity and performance of three novel quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9937528/]
- 33. ELISA vs. Immuno-PCR vs. SIMOA: Comparison of Protein ... [https://www.raybiotech.com/elisa-immunopcr-simoa]
- 34. Analytical techniques for nucleic acid and protein detection ... [https://www.nature.com/articles/s12276-025-01453-w]
- 35. NGS vs qPCR [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-qpcr.html]
- 36. Next-Generation Sequencing: A Review of Its Transformative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523276/]
- 37. Assessment of clinical analytical sensitivity and specificity of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3599218/]
- 38. Multi-analyte proteomic analysis identifies blood-based ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-024-00753-5]
- 39. NGS Testing More Cost-Effective Than SGT in Oncology [https://www.jons-online.com/web-exclusives/ngs-testing-more-cost-effective-than-sgt-in-oncology]
- 40. A performance comparison of heterostructure surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10039361/]
- 41. On the sensing performance improvement in SPR ... [https://www.nature.com/articles/s41598-025-14131-8]
- 42. The 2025 AI Index Report | Stanford HAI [https://hai.stanford.edu/ai-index/2025-ai-index-report]
- 43. The State of AI: Global Survey 2025 [https://www.mckinsey.com/capabilities/quantumblack/our-insights/the-state-of-ai]
- 44. Advancements in surface plasmon resonance sensors for real ... [https://pubs.rsc.org/en/content/articlehtml/2025/tc/d4tc04890c]
- 45. Analytical Validation and Clinical Sensitivity of the Belay ... [https://www.sciencedirect.com/science/article/pii/S1525157825000923]
- 46. Diagnostic accuracy of cerebrospinal fluid liquid biopsy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034915/]
- 47. High Cell-Free DNA Levels in Cerebrospinal Fluid Predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7541998/]
- 48. Sequencing of cerebrospinal fluid cell-free DNA facilitated ... [https://www.nature.com/articles/s41698-024-00541-w]
- 49. Metabolic Profiling and Quantitative Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8231178/]
- 50. Comparison of the diagnostic value of liquid biopsy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9806138/]
- 51. Cerebrospinal fluid Circulating Tumor DNA (ctDNA) as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12312583/]
- 52. Liquid biopsy: a step closer to transform diagnosis, prognosis ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-022-01543-7]
- 53. Analytical and clinical validation of a high accuracy fully ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1568971/full]
- 54. Plasma phospho-tau217 for Alzheimer's disease diagnosis ... [https://www.nature.com/articles/s41591-025-03622-w]
- 55. Analytical Validation and Performance of a Blood-Based P ... [https://pubmed.ncbi.nlm.nih.gov/39836199/]
- 56. Validation of an Ultra-Sensitive Method for Quantitation ... [https://www.sciencedirect.com/science/article/pii/S2274580724006496]
- 57. A Comprehensive Head-to-Head Comparison of Key Plasma ... [https://pubmed.ncbi.nlm.nih.gov/39006421/]
- 58. Comparison of plasma p‐tau217/Aβ42, p‐tau217, and ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344574/]
- 59. Integrating amplification strategies and functional ... [https://www.sciencedirect.com/science/article/abs/pii/S1567539425002737]
- 60. AI-Enhanced Surface Functionalization in Biosensors [https://www.sciencedirect.com/science/article/abs/pii/S0165993625003887]
- 61. Research Progress on Aptamer Electrochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300297/]
- 62. Dual-mode flexible physiological mechano-sensor ... [https://www.nature.com/articles/s41528-025-00487-4]
- 63. Leveraging microfluidic confinement to boost assay sensitivity ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc00199d]
- 64. Ultrasensitive and Multiplexed Target Detection Strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12348162/]
- 65. Revolutionary advances in nanomaterials-based ... [https://www.sciencedirect.com/science/article/pii/S2666831925001110]
- 66. AI Model Optimization Techniques for Enhanced ... [https://www.netguru.com/blog/ai-model-optimization]
- 67. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 68. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]
- 69. Introducing Nested Learning: A new ML paradigm for ... [https://research.google/blog/introducing-nested-learning-a-new-ml-paradigm-for-continual-learning/]
- 70. Hyperparameter Tuning: Complete 2025 Guide To ML ... [https://www.futureskillguides.com/hyperparameter-tuning-guide-2025/]
- 71. ML Model Optimization in 2025 [https://signiance.com/ml-model-optimization-in-2025/]
- 72. Engineering signal interfaces for enhanced ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993625001785]
- 73. Enhancement of quantum coherence in solid-state qubits ... [https://www.nature.com/articles/s41467-025-61026-3]
- 74. Enhancement of quantum coherence in solid-state qubits ... [https://arxiv.org/abs/2507.02312]
- 75. Improvement of the signal to noise ratio for fluorescent ... [https://www.nature.com/articles/s41598-022-23426-z]
- 76. Surface Functionalization of Nanoparticles for Enhanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12348736/]
- 77. Benchmarking performance with sensitivity, specificity, ... [https://epi2me.nanoporetech.com/benchmarking-performance/]
- 78. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 79. Assay Optimization: A Statistical Design of Experiments ... [https://www.sciencedirect.com/science/article/pii/S1535553505004077]
- 80. Biochemical Assay Development: Strategies to Speed Up ... [https://bellbrooklabs.com/accelerate-biochemical-assay-development/?srsltid=AfmBOoolmEXW04KZIWxKTN0D0L9Ud2BhufpNLCc5SAEYos_KQBNdBFnN]
- 81. Assay Optimization 101: Enhancing Sensitivity, Specificity, ... [https://dispendix.com/blog/assay-optimization-101-enhancing-sensitivity-specificity-and-reproducibility]
- 82. Analytical Performance of the New Sysmex High-Sensitivity ... [https://www.mdpi.com/2075-4418/15/15/1838]
- 83. Setting analytical performance specification by simulatio... [https://www.degruyterbrill.com/document/doi/10.1515/cclm-2025-0121/html?lang=en&srsltid=AfmBOoref-jb8yLnEvj8hlKt0sl4co6p0crWHJBayicY8oN9dhvvFfsG]
- 84. Reagent efficiency and analytical sensitivity optimization ... [https://www.sciencedirect.com/science/article/pii/S2405844025000027]
- 85. Receiver Operating Characteristic (ROC) Curve Analysis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3755824/]
- 86. Comparison of precision-recall curves - MedCalc Manual [https://www.medcalc.org/en/manual/precision-recall-comparison.php]
- 87. rocmetrics - Receiver operating characteristic (ROC) curve ... [https://www.mathworks.com/help/stats/rocmetrics.html]
- 88. Analytical vs Diagnostic Sensitivity and Specificity [https://www.immqas.org.uk/news/analytical-vs-clinical-sensitivity-and-specificity/]
- 89. the meaning of these terms in analytical and diagnostic settings [https://pubmed.ncbi.nlm.nih.gov/8992938/]
- 90. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 91. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 92. Specificity in Preclinical Drug Development Models [https://emulatebio.com/specificity-in-preclinical-drug-development-models-organ-chips/]
- 93. Tissue specificity of in vitro drug sensitivity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6381764/]
- 94. Development and application of sensitive, specific, and rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8014745/]
- 95. How to compare sensitivity and specificity in in vitro diagnostic ... [https://operondx.com/how-to-compare-sensitivity-and-specificity-in-in-vitro-diagnostic-tests/]