Blood Spectroscopy in Modern Medicine: From Fundamentals to Clinical Applications
This article provides a comprehensive overview of the latest advancements and applications of blood spectroscopy in medical diagnostics, tailored for researchers, scientists, and drug development professionals.
Blood Spectroscopy in Modern Medicine: From Fundamentals to Clinical Applications
Abstract
This article provides a comprehensive overview of the latest advancements and applications of blood spectroscopy in medical diagnostics, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of various spectroscopic techniques, including Raman, Surface-Enhanced Raman Spectroscopy (SERS), and infrared spectroscopy. The scope extends to detailed methodologies for detecting diseases and monitoring therapeutics, addresses key challenges in clinical translation, and presents rigorous validation frameworks and comparative analyses of different techniques. By synthesizing recent research and clinical studies, this review aims to serve as a critical resource for understanding the current landscape and future potential of blood-based spectroscopic diagnostics.
Core Principles and Emerging Diagnostic Paradigms in Blood Spectroscopy
Fundamental Light-Matter Interactions in Blood Components
The analysis of fundamental light-matter interactions in blood components provides a critical foundation for advancing medical diagnostics. Blood, a complex biological fluid, exhibits distinct optical behaviors when illuminated by light across various wavelengths. These interactions—including absorption, scattering, and Raman effects—create unique spectroscopic fingerprints that can be quantified to determine blood composition and identify pathological conditions [1] [2]. This Application Note explores the principles underpinning these phenomena and presents standardized protocols for leveraging spectroscopic techniques in blood analysis, framed within the broader context of developing non-invasive, rapid diagnostic platforms for clinical and research settings.
The optical properties of blood are predominantly governed by its cellular components, particularly red blood cells (RBCs), which contain hemoglobin at concentrations of approximately 150 g/L in whole blood [2]. Hemoglobin derivatives—including oxyhemoglobin (HbO₂), deoxyhemoglobin (Hb), and carboxyhemoglobin (HbCO)—each exhibit characteristic absorption spectra due to their molecular structures and the vibrational modes of their atomic bonds [3] [4]. These spectral signatures enable researchers to quantify hematologic parameters critical for diagnosing conditions such as anemia, polycythemia, and hemoglobinopathies.
Fundamental Principles of Light-Matter Interactions in Blood
Key Interaction Mechanisms
When light encounters blood components, several physical interactions occur simultaneously, with the dominant mechanism depending on the wavelength of incident light and the specific molecular structures present:
Absorption: Photons transfer energy to molecules, promoting electrons to higher energy states. In blood, hemoglobin serves as the primary chromophore, with absorption peaks varying significantly based on oxygenation state and molecular conformation [3]. The absorption coefficient (μâ‚) is proportional to hemoglobin concentration and can be described by the Beer-Lambert law, though this requires modification for highly scattering media like whole blood [2] [5].
Elastic Scattering: Photons change direction without energy loss, primarily through interactions with cellular interfaces. Red blood cells dominate scattering in blood due to their high concentration and refractive index mismatch with plasma [2]. The scattering coefficient (μₛ) exhibits a non-linear relationship with hematocrit, saturating at values above 10% due to dependent scattering effects between densely packed cells [2].
Raman Scattering: A small fraction of photons (approximately 1 in 10â·) undergo inelastic scattering, resulting in energy shifts that provide detailed molecular fingerprint information. Raman spectroscopy can probe vibrational modes of hemoglobin, proteins, and other blood constituents without external labels [1]. This technique is particularly valuable for detecting specific molecular bonds and conformational changes.
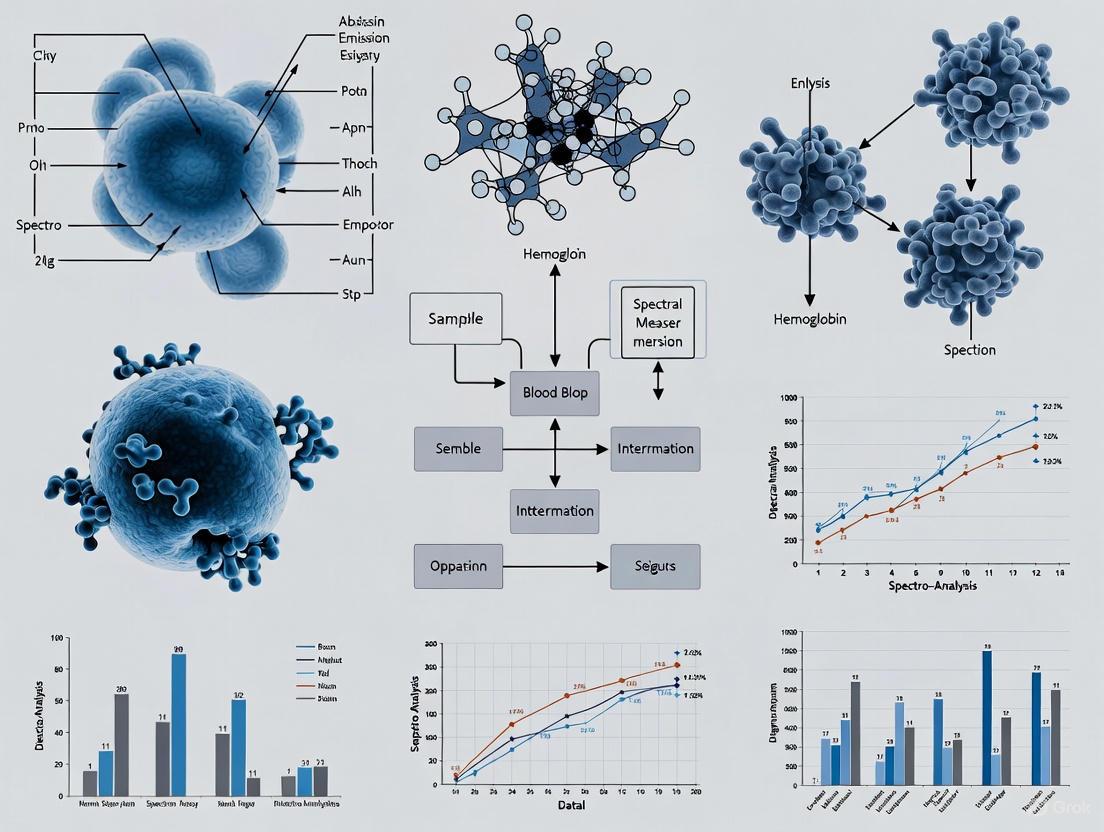
The following diagram illustrates the fundamental light-matter interactions that occur when light encounters key blood components:
Optical Properties of Whole Blood
Whole blood represents a complex, multi-component system with optical properties influenced by hematocrit, oxygen saturation, flow dynamics, and aggregate formation. The effective attenuation coefficient (μeff) combines absorption and scattering effects, representing the total rate of light attenuation in a blood sample [2]. Table 1 summarizes the key optical properties of whole blood and their determining factors.
Table 1: Optical Properties of Whole Blood and Their Determining Factors
| Optical Property | Symbol | Primary Determinants | Typical Values (at 600 nm) | Wavelength Dependence |
|---|---|---|---|---|
| Absorption Coefficient | μ₠| Hemoglobin concentration and type, oxygen saturation | 2-5 mmâ»Â¹ [2] [5] | Strong, with peaks at 415, 540, 575 nm [3] |
| Scattering Coefficient | μₛ | Hematocrit, RBC size and shape, refractive index mismatch | 70-120 mmâ»Â¹ [5] | Decreases with increasing wavelength [2] |
| Reduced Scattering Coefficient | μₛ' | Hematocrit, RBC aggregation | 1-3 mmâ»Â¹ [2] | Power law dependence: λ^(-k) where k~0.7-1.2 [2] |
| Scattering Anisotropy | g | RBC size relative to wavelength, membrane properties | 0.98-0.995 [2] | Increases with wavelength [2] |
| Effective Attenuation Coefficient | μeff | Combination of μ₠and μₛ' | 3-8 mmâ»Â¹ [2] | Varies with wavelength based on dominant mechanism |
Spectroscopic Techniques for Blood Analysis
Multi-Optical Path Length Spectroscopy
Multi-optical path length spectroscopy employs varied path lengths (typically 0-4.0 mm with 0.2 mm intervals) to acquire near-infrared absorption spectra of serum samples [6]. This approach enhances measurement accuracy by capturing spectral data at multiple depths, enabling the construction of robust quantitative models for blood components including glucose (GLU), total cholesterol (TC), total protein (TP), and albumin (ALB) [6]. The technique leverages the non-linear spectral characteristics of blood, with partial least squares (PLS) regression serving as the primary computational method for correlating spectral data with reference biochemical measurements.
Raman Spectroscopy
Raman spectroscopy probes the inelastic scattering of light to provide detailed chemical fingerprint information from blood components [1]. When combined with machine learning algorithms, this technique enables non-invasive, specimen-free diagnostic platforms capable of detecting both metabolites (e.g., glucose) and infections (e.g., COVID-19) through transcutaneous finger measurements [7]. The molecular specificity of Raman spectroscopy arises from its sensitivity to vibrational modes of chemical bonds, with enhancements such as Surface-Enhanced Raman Spectroscopy (SERS) increasing sensitivity by up to 15 orders of magnitude [1].
Visible-Light Spectroscopic Optical Coherence Tomography (vis-sOCT)
Visible-light sOCT combines the depth-resolution of OCT with spectral analysis capabilities to quantify total hemoglobin concentration ([tHb]) by measuring wavelength-dependent attenuation in the visible range [5]. This technique provides controlled optical path lengths, enabling spatially confined measurements of chromophore concentrations within individual blood vessels without cross-talk from surrounding tissues. Advanced implementations incorporate focus tracking and zero-delay acquisition to maintain optimal system sensitivity throughout the imaging depth, significantly improving measurement precision compared to conventional sOCT [5].
Experimental Protocols
Protocol: Multi-Optical Path Length Analysis of Blood Components
Research Reagent Solutions
Table 2: Essential Research Reagents for Multi-Optical Path Length Spectroscopy
| Reagent/Material | Specifications | Function | Handling Considerations |
|---|---|---|---|
| Human Serum Samples | 200 samples minimum, stored at -80°C | Provide biological matrix for analysis | Avoid repeated freeze-thaw cycles |
| Phosphate Buffered Saline (PBS) | 1X, pH 7.4 ± 0.1 | Dilution medium for serum samples | Prepare fresh weekly |
| Cuvette Cleaning Solution | Hellmanex III or equivalent | Ensure optical clarity of measurement chambers | Rinse extensively with deionized water |
| Quality Control Standards | Commercial biochemical standards for GLU, TC, TP, ALB | Validate analytical performance | Prepare according to manufacturer specifications |
Equipment and Instrumentation
- Automated micro-displacement measuring device capable of path length adjustments from 0-4.0 mm with 0.2 mm increments [6]
- Near-infrared spectrometer with wavelength range covering 800-2500 nm
- Temperature-controlled sample chamber maintained at 25°C ± 0.5°C
- Centrifuge for sample preparation (3000-5000 × g capability)
- Analytical balance (0.1 mg precision)
Procedure
Sample Preparation:
- Thaw frozen serum samples at room temperature and mix thoroughly by gentle inversion.
- Centrifuge samples at 3000 × g for 10 minutes to remove any particulate matter.
- Dilute samples 1:1 with PBS if necessary to maintain absorbance values within the instrument's linear range.
Instrument Calibration:
- Power on the NIR spectrometer and allow 30 minutes for lamp stabilization.
- Perform background measurement with PBS-filled cuvette at each path length setting.
- Validate system performance using quality control standards across all path lengths.
Spectral Acquisition:
- Load prepared sample into temperature-controlled cuvette.
- Program the automated micro-displacement device to cycle through path lengths from 0 to 4.0 mm in 0.2 mm increments.
- At each path length, acquire spectra with integration time optimized for signal-to-noise ratio without saturation.
- Triplicate measurements are recommended for each sample to assess reproducibility.
Data Analysis:
- Pre-process spectra using standard normal variate (SNV) or multiplicative scatter correction (MSC).
- Develop quantitative models using partial least squares (PLS) regression with 160 samples for calibration.
- Validate model performance with the remaining 40 samples, comparing predicted values against reference biochemical analyses.
- Evaluate model quality using correlation coefficients (r) between predicted and measured values, with typical performance ranging from r = 0.9320 for glucose to r = 0.9712 for total cholesterol [6].
The following workflow diagram outlines the key steps in the multi-optical path length spectroscopy protocol:
Protocol: Non-Invasive Blood Analysis Using Raman Spectroscopy
Research Reagent Solutions
Table 3: Essential Research Reagents for Non-Invasive Raman Spectroscopy
| Reagent/Material | Specifications | Function | Handling Considerations |
|---|---|---|---|
| Finger Interface Device | Custom pulse oximeter-like design with 830 nm laser | Standardized finger placement and measurement | Clean with alcohol wipes between uses |
| Calibration Standards | Silicon wafer or polystyrene | Verify instrument wavelength and intensity calibration | Store in dust-free container |
| Disinfectant Solution | 70% isopropanol wipes | Maintain hygiene for patient interface | Allow complete evaporation before use |
| Reference Glucose Measurements | Dexcom sensor and Accu-Chek device | Provide ground truth for machine learning training | Follow manufacturer guidelines |
Equipment and Instrumentation
- Raman spectrometer with 830 nm excitation laser [7]
- Custom finger-scanning hardware (US patent #11452454; 11304605) [7]
- Machine learning workstation with GPU acceleration
- Reference instruments for ground truth validation (PCR for infection, Dexcom/Accu-Chek for glucose)
Procedure
Instrument Preparation:
- Power on Raman system and allow laser to stabilize for 15 minutes.
- Perform wavelength calibration using silicon wafer (peak at 520 cmâ»Â¹).
- Verify intensity response using polystyrene standard.
- Clean finger interface with 70% isopropanol and allow to dry completely.
Data Acquisition:
- Position subject's finger comfortably in the scanning interface.
- Acquire Raman spectra with laser power optimized for patient safety and signal quality.
- Typical integration times range from 10-30 seconds per measurement.
- Collect reference measurements concurrently (nasal PCR for infection studies, venous blood glucose for metabolic studies).
Machine Learning Implementation:
- For COVID-19 detection: Frame as a classification problem using Raman spectra as input to distinguish between infected and non-infected individuals.
- For glucose monitoring: Implement regression analysis to predict continuous glucose values from spectral features.
- Employ five-fold cross-validation to assess model performance.
- For COVID-19 detection, expect cross-validation sensitivity of 0.80 with specificity of 0.837 and AUROC of 0.896 [7].
- For glucose detection, target area under precision-recall curve (AUPR) of 0.58 in cross-validation [7].
Model Deployment:
- Deploy trained algorithms to field devices for point-of-care testing.
- Implement continuous learning protocols to adapt to new viral variants or changing patient populations.
Data Analysis and Interpretation
Quantitative Spectral Analysis
The analysis of spectroscopic data from blood components requires specialized approaches to extract meaningful biological information from complex spectral signatures:
Absorption Spectroscopy Quantification: For hemoglobin quantification using vis-sOCT, apply the following relationship between absorption coefficient and hemoglobin concentration:
μâ‚(λ) = (2.303 × ε(λ) × [tHb] × 150 g/L) / (64,500 g/mole) [3]
where ε(λ) is the wavelength-dependent molar extinction coefficient of hemoglobin, [tHb] is the total hemoglobin concentration, and 64,500 g/mole is the molecular weight of hemoglobin.
Multivariate Analysis: Employ partial least squares (PLS) regression for multi-component analysis, which effectively handles collinearity in spectral data. For multi-optical path length measurements, correlation coefficients between predicted and reference values should exceed 0.93 for glucose, 0.97 for total cholesterol, 0.95 for total protein, and 0.95 for albumin [6].
Machine Learning for Raman Spectroscopy: Implement support vector machines (SVM) or deep learning architectures for classification tasks. For COVID-19 detection, optimal performance is achieved with sensitivity of 0.80 and specificity of 0.837 in cross-validation [7]. Note that temporal validation (training on data before July 2022, testing on data after) may show decreased AUROC (0.67) due to domain shift from viral evolution [7].
Technical Considerations and Limitations
Several factors must be considered when interpreting spectroscopic data from blood components:
Hematocrit Effects: Scattering coefficient (μₛ) demonstrates non-linear saturation at hematocrit values above 10% due to dependent scattering effects [2]. Apply appropriate scaling relations when working with diluted blood samples.
Oxygen Saturation Dependence: Both absorption and scattering properties vary with oxygen saturation, particularly in the visible wavelength range [2]. Report saturation levels alongside spectroscopic measurements.
Multiple Scattering: In whole blood, multiple scattering contributes significantly to measured attenuation, violating the assumption of single scattering in traditional models [5]. Implement appropriate correction factors for accurate quantification.
Sample Preparation Artifacts: Replacement of plasma with saline or phosphate buffer alters the refractive index mismatch, increasing measured scattering coefficients by 5.5-9.4% compared to native blood [2].
Vibrational and diffuse optical spectroscopies have emerged as powerful, non-invasive tools for medical diagnostics and biomarker discovery. These techniques provide a unique window into the molecular composition and physiological dynamics of biological samples, particularly blood, enabling rapid disease detection and monitoring. Raman spectroscopy and Surface-Enhanced Raman Spectroscopy (SERS) probe molecular vibrations to generate detailed chemical fingerprints of samples, while Infrared (IR) spectroscopy complements this by measuring molecular absorption characteristics. In contrast, Diffuse Correlation Spectroscopy (DCS) utilizes the dynamic scattering of light to quantify microvascular blood flow, representing a functional rather than molecular measurement modality. Together, these techniques form a comprehensive analytical toolkit for researchers and clinicians investigating hematological conditions, cancer, neurodegenerative disorders, and cardiovascular diseases through blood-based analysis. Their minimal sample preparation requirements, potential for real-time measurement, and compatibility with multivariate analysis and machine learning create unprecedented opportunities for advancing diagnostic medicine and therapeutic development.
Technical Fundamentals and Principles
Raman and Surface-Enhanced Raman Spectroscopy (SERS)
Raman spectroscopy is an optical technique based on the inelastic scattering of photons by molecular bond vibrations and rotations. When light interacts with a molecule, a small fraction of photons (approximately 1 in 10â·) undergoes a shift in energy corresponding to the vibrational modes of the chemical bonds present, creating a unique spectral "fingerprint" for each molecular species. The most informative vibrations for biological molecules typically occur in the 500-1800 cmâ»Â¹ range (fingerprint region), with additional characteristic peaks appearing in the high-wavenumber region (2700-3500 cmâ»Â¹) related to CH stretches in proteins and lipids [8].
Surface-Enhanced Raman Spectroscopy (SERS) significantly amplifies this inherently weak Raman effect by exploiting the plasmon resonance phenomena of metallic nanostructures. When analyte molecules are adsorbed onto or in close proximity to nanostructured noble metal surfaces (typically silver, gold, or copper), the Raman scattering signal can be enhanced by factors of up to 10â¸-10¹¹, enabling the detection of analytes at extremely low concentrations [8]. This dramatic enhancement occurs through two primary mechanisms: (1) electromagnetic enhancement resulting from localized surface plasmon resonance, and (2) chemical enhancement through charge-transfer interactions. SERS has revolutionized biomedical applications by enabling the detection of low-abundance biomarkers in complex biological matrices like blood serum and plasma.
Infrared (IR) Spectroscopy
Infrared spectroscopy measures the absorption of IR radiation by molecular bonds as they undergo vibrational transitions. Unlike Raman spectroscopy, IR spectroscopy requires a change in the dipole moment of the molecule during vibration to be active. IR spectroscopy encompasses several techniques with distinct wavelength ranges and applications [4]:
- Mid-infrared (MIR) spectroscopy (4000-400 cmâ»Â¹) offers high sensitivity to fundamental molecular vibrations and is particularly valuable for detailed molecular characterization of biological samples.
- Fourier Transform Infrared (FTIR) spectroscopy, a type of MIR spectroscopy, provides high-resolution spectra and is frequently used for qualitative analysis of blood components.
- Near-infrared (NIR) spectroscopy (14,000-4000 cmâ»Â¹) excels in quantitative analyses due to its deeper sample penetration capabilities.
- Attenuated Total Reflection (ATR)-FTIR specializes in probing surface properties and requires minimal sample preparation.
In biological applications, major IR absorption bands typically arise from functional groups in proteins, lipids, and nucleic acids, including N-H, C=O, C-H, and P=O bonds [4].
Diffuse Correlation Spectroscopy (DCS)
Diffuse Correlation Spectroscopy (DCS) is an optical technique that measures microvascular blood flow in deep tissues by analyzing the temporal fluctuations of near-infrared light scattered by moving red blood cells [9] [10]. When coherent light diffuses through biological tissue, it undergoes scattering events from both static tissue structures and dynamic scatterers (primarily red blood cells). The motion of these red blood cells causes speckle fluctuations in the detected light intensity [11].
DCS quantifies these fluctuations by measuring the temporal autocorrelation function of the scattered light intensity, which decays more rapidly with increased blood flow. The correlation diffusion equation models this light transport phenomenon, enabling the extraction of a blood flow index (BFI) that is proportional to tissue blood flow [11] [9]. DCS typically employs near-infrared light (650-850 nm) due to its relatively deep tissue penetration (up to ~1 cm) and sensitivity to hemodynamic changes.
Table 1: Comparison of Fundamental Principles of Spectroscopic Techniques
| Technique | Physical Principle | Measurable Parameters | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| Raman | Inelastic scattering of light by molecular vibrations | Molecular composition, chemical structure, crystal phases | Minimal sample preparation, works with aqueous samples, fingerprinting capability | Weak inherent signal, fluorescence interference |
| SERS | Plasmon-enhanced Raman scattering | Low-concentration analytes, biomarkers, molecular interactions | Extreme sensitivity (single molecule detection), signal amplification, quenching of fluorescence | Substrate dependency, potential inconsistency, complex optimization |
| IR Spectroscopy | Absorption of IR radiation by molecular bonds | Functional groups, molecular conformations, quantitative analysis | High sensitivity to polar bonds, well-established libraries, rapid analysis | Strong water absorption, limited penetration depth, sample thickness effects |
| DCS | Temporal fluctuations of scattered NIR light | Blood flow index (BFI), microvascular dynamics | Non-invasive deep tissue monitoring, continuous measurement, quantitative flow metrics | Limited spatial resolution, sensitivity to movement artifacts, complex modeling |
Experimental Protocols and Methodologies
SERS Analysis of Blood Serum for Cancer Detection
Protocol Objective: Detection of disease-specific biomarkers in blood serum using SERS for diagnostic applications such as multiple myeloma [12] or multiple sclerosis [13].
Materials and Reagents:
- Blood collection tubes (serum separator tubes)
- Silver nitrate (AgNO₃) and sodium citrate for nanoparticle synthesis [12] [13]
- Aluminum foil or appropriate substrate for SERS analysis
- Purified water (HPLC grade or higher)
- Sodium nitrate crystals (0.02% volume concentration) [12]
- Raman spectrometer system with 785 nm laser excitation [12]
Procedure:
- Sample Collection and Preparation:
- Collect venous blood samples (e.g., 9 ml) using standard phlebotomy techniques with appropriate aseptic procedures [13].
- Allow blood to clot at room temperature for 30 minutes, then centrifuge at 1000-2000 × g for 10 minutes to separate serum.
- Aliquot serum samples and store at -80°C if not analyzing immediately.
SERS Substrate Preparation:
Sample Loading:
- Apply 1.5 µl of serum sample onto the prepared SERS substrate on aluminum foil [13].
- Allow the sample to dry for 30 minutes at room temperature before analysis.
SERS Measurements:
- Use a Raman spectrometric system with a 785 nm laser excitation source [12] [13].
- Set laser power to 10 mW at the sample to avoid degradation [13].
- For each sample, acquire three spectra, with each spectrum representing an average of four measurements with 4-second integration times [13].
- Record background signal immediately before sample analysis and subtract automatically using instrument software.
Data Analysis:
- Pre-process spectra (background subtraction, smoothing, normalization).
- Apply multivariate analysis techniques such as Principal Component Analysis (PCA) or Partial Least Squares Discriminant Analysis (PLS-DA) for classification.
- Utilize machine learning algorithms (e.g., convolutional neural networks) for pattern recognition and disease classification [13].
IR Spectroscopy of Blood Plasma for Disease Detection
Protocol Objective: Analysis of blood plasma using IR spectroscopy for detection of endometrial cancer [14] or hematological disorders [4].
Materials and Reagents:
- EDTA or heparin blood collection tubes
- IR-transparent substrates (e.g., barium fluoride or calcium fluoride windows)
- Phosphate-buffered saline (PBS) for dilution if required
- Purified water for cleaning substrates
- ATR-FTIR accessory if using ATR mode
Procedure:
- Sample Preparation:
- Collect blood samples in anticoagulant-containing tubes and centrifuge at 1500-2000 × g for 15 minutes to separate plasma.
- For "wet" plasma analysis, use freshly separated plasma immediately [14].
- For dry film analysis, deposit 2-5 µl of plasma onto IR-transparent substrates and allow to dry under mild desiccation.
Instrument Setup:
- For FTIR spectroscopy in ATR mode, clean the ATR crystal thoroughly with purified water and obtain background spectrum.
- Set spectral resolution to 4 cmâ»Â¹ and accumulate 64-128 scans per spectrum to ensure adequate signal-to-noise ratio [14].
- For transmission mode, optimize sample thickness and pathlength to avoid signal saturation.
Spectral Acquisition:
Data Processing:
- Apply vector normalization or standard normal variate (SNV) normalization to correct for baseline variations.
- Use second derivatives to resolve overlapping bands (e.g., Savitzky-Golay derivative with 9-13 point smoothing).
- Employ multivariate statistical analysis for classification and biomarker identification.
DCS for Cerebral Blood Flow Monitoring
Protocol Objective: Non-invasive measurement of cerebral blood flow (CBF) using DCS [9] [10].
Materials and Equipment:
- DCS instrument with long-coherence-length laser source (e.g., 785 nm or 850 nm)
- Single-photon counting detectors (SPADs or APDs)
- Source and detector fiber optic probes
- Probe holder or headgear for stable positioning
- Calibration phantom with known optical properties
Procedure:
- Instrument Calibration:
- Verify instrument performance using tissue-simulating phantoms with known flow characteristics.
- Measure instrument noise baseline and correlation curve parameters.
Subject Preparation:
- Position subject comfortably in a reclined chair or bed.
- Clean skin surface at probe placement sites.
- Arrange source and detector optodes on the scalp with a separation distance of 2.5-3.0 cm to ensure sufficient penetration depth into cerebral cortex [9].
Data Acquisition:
- Acquire continuous intensity fluctuations at a sampling rate sufficient to capture blood flow dynamics (typically >10 Hz).
- Record measurements for a minimum of 2-3 minutes under baseline conditions to establish stable flow indices.
- During functional activation studies, synchronize DCS measurements with stimulus presentation.
- For clinical monitoring, acquire data continuously or at regular intervals as required by the protocol.
Data Processing and Analysis:
- Compute intensity autocorrelation functions from the detected signals.
- Fit correlation curves to solutions of the correlation diffusion equation to extract blood flow index (BFI) [11] [9].
- Normalize BFI to baseline values for relative flow changes or convert to absolute units using calibration procedures.
- Integrate with concurrent NIRS measurements to compute cerebral metabolic rate of oxygen (CMROâ‚‚) when applicable.
Data Analysis and Interpretation
Spectral Data Processing and Multivariate Analysis
The analysis of spectroscopic data from Raman, SERS, and IR techniques requires sophisticated processing pipelines to extract meaningful biological information. Preprocessing is essential to remove instrumental artifacts and enhance spectral features, typically including: noise reduction (Savitzky-Golay smoothing, wavelet denoising), background subtraction (especially for fluorescence in Raman spectra), normalization (vector normalization, standard normal variate), and scaling (mean-centering, Pareto scaling) [8].
Multivariate analysis techniques are then applied to identify patterns and classify samples based on their spectral signatures. Principal Component Analysis (PCA) reduces dimensionality while preserving variance, allowing visualization of natural clustering between sample groups. Projection to Latent Structures Discriminant Analysis (PLS-DA) builds predictive models that maximize separation between predefined classes, making it particularly valuable for diagnostic applications [15]. For complex spectral datasets, machine learning approaches such as support vector machines (SVM) and convolutional neural networks (CNN) have demonstrated remarkable classification performance, achieving accuracies exceeding 90% for diseases like multiple myeloma and multiple sclerosis [12] [13].
Table 2: Characteristic Spectral Markers for Disease Detection in Blood
| Disease | Technique | Informative Spectral Bands (cmâ»Â¹) | Associated Biomarkers/Molecular Changes | Diagnostic Performance |
|---|---|---|---|---|
| Multiple Myeloma [12] | SERS | 635, 723, 1052 | Not specified | Accuracy >96% |
| Multiple Sclerosis [13] | SERS with CNN | Pattern-based rather than specific bands | Metabolic changes in serum | Specificity: 0.9, Sensitivity: 1.0 |
| Atherosclerosis [15] | SERS | 670-680, 718, 1004, 1073, 1146, 1439 | Metabolic profile associated with atherosclerosis | Accuracy: 0.93-1.00 |
| Endometrial Cancer [14] | Raman ('wet' plasma) | Pattern-based | Molecular bio-fingerprint | Accuracy: 82% |
| Endometrial Cancer [14] | ATR-FTIR ('wet' plasma) | Pattern-based | Molecular bio-fingerprint | Accuracy: 78% |
| Heart Failure with Atherosclerosis [15] | SERS | 672, 728, 1077, 1123, 1214, 1284, 1402 | Metabolic profile associated with CHF | High discriminative power |
DCS Data Interpretation and Physiological Correlations
DCS data analysis focuses on extracting clinically relevant parameters related to tissue hemodynamics. The primary measured parameter is the blood flow index (BFI), which is proportional to the product of the fraction of scattering events from moving red blood cells (α) and their effective diffusion coefficient (D₆) [11]. Relative changes in blood flow (rBF) are calculated as the ratio of BFI during a perturbation to baseline BFI. In neurological applications, DCS can detect characteristic flow pulsatility correlated with the cardiac cycle and has been validated against established modalities including arterial spin-labeled MRI, transcranial Doppler ultrasound, and Xenon-CT [9].
When combined with concurrent near-infrared spectroscopy (NIRS), DCS enables calculation of the cerebral metabolic rate of oxygen consumption (CMROâ‚‚) through Fick's principle, providing a more comprehensive assessment of cerebral oxygen delivery and utilization [9]. This hybrid approach has proven valuable in monitoring patients with brain injuries, assessing cerebral autoregulation, and evaluating functional activation responses in both clinical and research settings.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents and Materials for Spectroscopic Blood Analysis
| Category | Specific Items | Function/Purpose | Application Examples |
|---|---|---|---|
| Nanoparticle Substrates | Silver colloid from AgNO₃ reduction | SERS signal amplification through plasmon resonance | Multiple myeloma detection [12] |
| Gold nanoparticles | Alternative SERS substrate with different enhancement properties | General SERS applications [8] | |
| Sample Collection & Processing | Serum separator tubes | Clean serum collection for SERS/Raman analysis | Multiple sclerosis studies [13] |
| EDTA/heparin blood collection tubes | Plasma separation for IR spectroscopy | Endometrial cancer detection [14] | |
| IR-transparent substrates (BaFâ‚‚, CaFâ‚‚) | Sample presentation for transmission IR spectroscopy | Dry plasma analysis [14] | |
| Spectral Calibration | Polystyrene standards | Wavelength calibration for Raman systems | Instrument validation |
| Acetaminophen standards | Intensity calibration for Raman systems | Quantitative comparison | |
| Data Analysis | MATLAB, Python with scikit-learn | Multivariate analysis and machine learning implementation | Spectral classification [13] [15] |
| Commercial chemometrics software | User-friendly spectral analysis | PLS-DA modeling [15] |
Workflow Visualization and Signaling Pathways
The integration of Raman, SERS, IR, and DCS techniques represents a transformative approach to blood-based medical diagnostics, offering complementary capabilities for comprehensive disease characterization. SERS excels in detecting low-concentration molecular biomarkers with exceptional sensitivity, while IR spectroscopy provides robust metabolic profiling. Conventional Raman spectroscopy offers label-free molecular fingerprinting, and DCS adds functional hemodynamic assessment to the diagnostic arsenal. The convergence of these spectroscopic modalities with advanced machine learning algorithms creates unprecedented opportunities for precision medicine, enabling early disease detection, stratification of patient subgroups, and monitoring of therapeutic responses.
Future developments in this field will likely focus on several key areas: (1) standardization of protocols and substrates to improve reproducibility across laboratories and clinical settings; (2) miniaturization of instrumentation for point-of-care applications; (3) multi-modal integration that combines the strengths of each technique while mitigating their individual limitations; and (4) implementation of artificial intelligence for real-time analysis and interpretation of complex spectral data. As these technologies mature and validation studies expand, spectroscopic blood analysis is poised to become an indispensable tool in clinical diagnostics and therapeutic development, potentially revolutionizing how we detect, monitor, and treat a wide spectrum of human diseases.
Blood is a quintessential biofluid that provides a rich source of information for medical diagnostics. Its complex composition—comprising cellular components suspended in a liquid matrix—can reveal critical insights into physiological and pathological states. Spectroscopic analysis of blood offers a powerful, often non-invasive or minimally invasive, window into this complexity, enabling researchers to probe molecular-level changes associated with disease. This application note details the fundamental differences between key blood derivatives—plasma and serum—and provides validated protocols for their spectroscopic analysis, supporting their use in therapeutic development and clinical diagnostics.
Blood Components: Plasma vs. Serum
Whole blood consists of cellular components (red blood cells, white blood cells, and platelets) suspended in a liquid fraction. When separated, this liquid fraction can be processed into either plasma or serum, which are the primary matrices for most spectroscopic analyses.
Plasma is the liquid component of blood in which formative elements are removed via centrifugation, but it retains all proteins and clotting factors. It is obtained by collecting blood in anti-coagulant tubes [16] [17].
Serum is blood plasma without the clotting factors; it is obtained by allowing a blood sample to clot (coagulate) before centrifuging [16] [17]. Serum is often preferred for spectroscopic analysis as it typically removes red blood cells more effectively than other preparation methods [16].
Table 1: Key Differences Between Plasma and Serum
| Characteristic | Plasma | Serum |
|---|---|---|
| Preparation Method | Centrifugation of blood collected with an anticoagulant [16] | Centrifugation of clotted blood [16] |
| Clotting Factors | Present | Absent |
| Fibrinogen Content | Present (typically 2-4 g/L) | Absent (consumed in clot formation) |
| Relative Volume Yield | Higher (~55% of blood volume) | Slightly lower |
| Spectral Influence | May contain spectral features of anticoagulants (e.g., EDTA) [17] | Lacks anticoagulant signals |
Despite these preparation differences, a recent 2025 quantitative metabolomics study found that plasma and serum samples from various collection methods (venous, microblade, fingerstick) exhibited minimal metabolic differences. When identical biofluid types were compared, only two metabolites—sarcosine and pyruvic acid—consistently showed significant differences between plasma and serum across all collection methods [18]. This finding proves that inexpensive blood microsampling systems can yield data comparable to those from traditional venous collection.
Spectroscopic Techniques for Blood Analysis
Various spectroscopic methods are employed to analyze blood components, each with unique advantages and applications.
Table 2: Spectroscopic Techniques for Blood Analysis
| Technique | Principle | Key Applications | Sample Form |
|---|---|---|---|
| ATR-FTIR [16] | Measures molecular bond vibrations in the mid-IR range (4000-400 cmâ»Â¹) | Disease discrimination (cancer, endometriosis, viral infections) [16]; Health monitoring via Infrared Molecular Fingerprints (IMFs) [17] | Liquid or dried serum/plasma |
| SERS [19] | Enhances Raman signal using nanostructured metal surfaces | Label-free, diagnostic screening for cancer; Rapid, non-invasive mass screening [19] | Biofluids (blood, urine, saliva) |
| UV-Vis Spectrophotometry [20] [21] | Measures absorption of light in UV and visible regions | Quantification of drugs (e.g., antiplatelets/anticoagulants) in spiked plasma [20]; Haemoglobin analysis [21] | Liquid plasma/serum |
| Diffuse Reflectance Spectroscopy [22] | Measures light reflected from a turbid medium | Non-invasive estimation of haemoglobin, bilirubin, and oxygen saturation [22] | In vivo measurement (e.g., conjunctiva, nail bed) |
Experimental Protocols
Protocol: ATR-FTIR Analysis of Blood Serum/Plasma
Principle: Attenuated Total Reflection Fourier-Transform Infrared (ATR-FTIR) spectroscopy probes the fundamental vibrations of functional groups in biological samples, such as proteins, lipids, and amino acids, providing a "biological fingerprint" [16].
The Scientist's Toolkit:
- FTIR Spectrometer: Equipped with a heated ATR accessory (e.g., Edinburgh Analytical IA30). The internal reflective element is typically diamond for its durability and thermal conductivity [16].
- Micro-pipette: For accurate dispensing of low microliter volumes.
- Centrifuge: For separating serum or plasma from whole blood.
- Anti-coagulant Tubes: (e.g., EDTA) for plasma collection.
Procedure:
- Sample Preparation: Collect venous blood. For serum, allow blood to clot for 30 minutes at room temperature. For plasma, collect blood in anti-coagulant tubes. Centrifuge both at 1500-2000 RCF for 10 minutes to separate the liquid fraction [16].
- Loading: Pipette 3 µL of the serum or plasma sample directly onto the ATR crystal [16].
- Drying: Engage the heated ATR accessory and maintain at 50°C for approximately 2 minutes to accelerate water evaporation. Note: Water has a strong IR response that can obscure biological information if the sample is analyzed in the liquid phase [16].
- Acquisition: Acquire IR spectra with a resolution of 4 cmâ»Â¹, accumulating 10 scans, resulting in an acquisition time of about 35 seconds [16].
- Data Processing: Normalize spectra to mitigate variations due to the total amount of biomolecules, which reveals differences in molecular composition [17].
Protocol: Quantitative Spectrophotometric Analysis of Drugs in Spiked Plasma
Principle: Ratio spectra and derivative ratio spectra are signal-processing techniques in UV-Vis spectrophotometry used to resolve overlapping peaks in multicomponent analysis without prior separation [20].
Procedure for Antiplatelet/Anticoagulant Assay (e.g., Apixaban, Aspirin, Clopidogrel):
- Plasma Preparation: Obtain drug-free human plasma from healthy volunteers. Centrifuge at 3000 rpm for 10 minutes to separate clear plasma [20].
- Spiking: Prepare stock solutions of each drug. Spike the plasma with known concentrations of the drugs (Apixaban, Aspirin, Clopidogrel) to create calibration standards [20].
- Sample Pre-treatment: Mix the spiked plasma sample with a precipitating solvent (e.g., methanol) to precipitate proteins. Vortex mix, then centrifuge [20].
- Spectrum Acquisition: Scan the supernatant in the UV-Vis range (e.g., 200-400 nm) using a double-beam spectrophotometer (e.g., Shimadzu UV-1601 PC) with 1 cm pathlength quartz cells [20].
- Data Processing (Ratio Spectra Method):
- Obtain the absorption spectrum of the mixture.
- Divide (ratio) this spectrum by a carefully selected divisor spectrum (a standard spectrum of one component) to suppress interfering signals [20].
- Apply derivative transformations to the ratio spectrum to further enhance resolution and allow for selective quantification of each analyte [20].
Data Interpretation and Applications
Infrared Molecular Fingerprints (IMFs) for Health Monitoring
Fourier-transform infrared (FTIR) spectroscopy of liquid serum and plasma produces IMFs that are highly stable over clinically relevant timescales for a given individual [17]. These IMFs cover characteristic absorption bands for proteins (amide I/II at ~1654 cmâ»Â¹ and ~1548 cmâ»Â¹), carbohydrates (1000-1200 cmâ»Â¹), and lipids (~1741 cmâ»Â¹, ~2854 cmâ»Â¹, ~2929 cmâ»Â¹) [17]. The high temporal stability of person-specific IMFs enables the detection of deviations from an individual's healthy baseline, forming a basis for non-invasive health monitoring and early disease detection [17].
Non-Invasive Monitoring of Blood Constituents
The optical properties of blood, primarily dictated by hemoglobin in the visible and near-infrared range, underpin several non-invasive technologies [21]. Diffuse reflectance spectroscopy can be deployed via portable, fiber-less probes to measure hemoglobin (for anemia), bilirubin (for jaundice), and oxygen saturation at points of care, such as the neonatal nail bed or the bulbar conjunctiva [22]. Advanced analytical frameworks like the improved Concentration Independent Calibration (iCONIC) approach further enable the tracking of dynamic analyte concentrations, such as glucose, using vibrational spectroscopy with minimal reliance on invasive calibration [23].
Molecular fingerprinting is emerging as a revolutionary paradigm for clinical disease diagnostics, shifting the focus from the detection of single, specific biomarkers to the identification of unique, multi-analyte spectral patterns associated with physiological and pathological states [24]. This approach leverages advanced spectroscopic techniques to capture a holistic snapshot of the molecular composition of biofluids, such as blood plasma. When combined with machine learning, it allows for the robust detection of diseases like cancer and metabolic disorders based on characteristic pattern changes [7] [24]. This Application Note details the underlying principles, key experimental protocols, and performance data for two prominent molecular fingerprinting techniques—Electric-Field Molecular Fingerprinting (EMF) and Raman Spectroscopy—framed within the context of blood-based diagnostic research.
Technical Basis and Diagnostic Specificity
The diagnostic specificity of molecular fingerprinting stems from its ability to measure a vast array of molecular vibrations simultaneously, creating a unique "fingerprint" that is sensitive to the subtle biochemical alterations caused by disease.
- Electric-Field Molecular Fingerprinting (EMF): EMF is a laser-based spectroscopic technique that employs an ultrashort pulse of broadband infrared light to impulsively excite molecular bonds in a sample [24]. The key differentiator from conventional spectroscopy is that it directly measures the infrared electric field emitted by the excited molecules over time, temporally separating the resonant molecular response from the excitation source. This process results in a background-free measurement with enhanced sensitivity, capturing a coherent sum of the infrared responses from diverse molecular classes (e.g., proteins, lipids, carbohydrates) to form a cross-molecular infrared fingerprint of the biofluid [24].
- Raman Spectroscopy: This technique relies on the inelastic scattering of monochromatic light, typically from a laser. When light interacts with a molecule, the scattered light can shift in energy, corresponding to the vibrational modes of the molecular bonds present. The resulting Raman spectrum serves as a physicochemical fingerprint of the molecules in the sample [7]. A significant advantage in a clinical setting is that water produces a very weak Raman scattering, making it particularly suitable for analyzing aqueous biological samples [7].
The "specificity" for a particular disease is not pre-programmed but is learned computationally. Machine learning models, trained on spectral fingerprints from confirmed patient and control cohorts, identify the complex, multi-feature patterns that reliably distinguish a target disease state from a non-disease state.
Quantitative Performance Data
The following tables summarize key quantitative findings from recent proof-of-concept clinical studies utilizing these fingerprinting technologies.
Table 1: Performance of EMF in Cancer Detection in a Clinical Study (N=2533) [24]
| Cancer Type | Sample Size (Training Set) | Cross-Validation ROC AUC | Held-Out Test Set ROC AUC |
|---|---|---|---|
| Lung Cancer | 2104 (across all cancers) | 0.88 | 0.81 |
| Prostate Cancer | 2104 (across all cancers) | 0.68 - 0.69 | Not Specified |
| Breast Cancer | 2104 (across all cancers) | 0.68 - 0.69 | Not Specified |
| Bladder Cancer | 2104 (across all cancers) | 0.68 - 0.69 | Not Specified |
Table 2: Performance of Raman Spectroscopy for Disease Detection [7]
| Diagnostic Target | Study Design | Reference Method | Key Performance Metric | Result |
|---|---|---|---|---|
| COVID-19 | 455 patients | Nasal PCR | Sensitivity/Specificity | 0.80 / 0.837 |
| COVID-19 | 455 patients | Nasal PCR | AUROC (Cross-Validation) | 0.896 |
| Blood Glucose | 205 observations | Dexcom Sensor & Accu-Chek | AUPR (Cross-Validation) | 0.58 |
Detailed Experimental Protocols
Protocol: Electric-Field Molecular Fingerprinting of Blood Plasma for Cancer Detection
This protocol is adapted from the Lasers4Life clinical study involving the detection of lung, prostate, breast, and bladder cancer [24].
1. Sample Collection and Preparation: - Collect venous blood from participants into EDTA or heparin tubes. - Centrifuge the blood at 2,000 x g for 10 minutes at 4°C to separate plasma. - Aliquot the plasma and store at -80°C until analysis. Avoid repeated freeze-thaw cycles.
2. EMF Measurement Setup: - Instrumentation: Utilize an EMF instrument equipped with a femtosecond-pulse laser source, a semiautomated sample delivery system, and a flow-through cuvette [24]. - Laser Stabilization: Allow the laser source a 2-hour stabilization period before commencing measurements [24].
3. Measurement Procedure: - Blank Measurement: Inject pure water into the cuvette and acquire a 40-second blank EMF measurement. This averages 112,000 individual traces and is used for subsequent signal standardization [24]. - Sample Measurement: Inject the plasma sample into the cuvette. Acquire a 40-second EMF measurement, again averaging 112,000 individual traces [24]. - Cuvette Cleaning: Implement a rigorous 2-minute cleaning step between samples to prevent carryover contamination [24]. - Randomization: Measure all samples in a fully randomized order to minimize batch effects. - Quality Control: Periodically measure aliquots of a commercially obtained pooled human serum sample to monitor instrument stability and experimental variability over the entire measurement campaign [24].
4. Data Preprocessing and Standardization: - Apply a time-domain filter to the raw infrared fingerprints to separate the resonant molecular signal from the impulsive excitation [24]. - Standardize the sample measurements using the blank measurement to suppress fluctuations originating from the laser source [24].
5. Data Analysis and Machine Learning: - Split the standardized infrared fingerprint data into training and independent test sets. - Train a machine learning classifier (e.g., based on pattern recognition) on the training set using the EMF data as input and the clinical diagnosis as the ground truth. - Evaluate the model's performance on the held-out test set using metrics such as the Area Under the Receiver Operating Characteristic Curve (ROC AUC).
Protocol: No-Specimen Raman Spectroscopy for COVID-19 and Glucose Detection
This protocol outlines a non-invasive approach using a finger-scanning device, as demonstrated in proof-of-concept studies for COVID-19 and glucose monitoring [7].
1. Patient Interface and Hardware: - Device: Use a custom-built, pulse-oximeter-like device equipped with an 830 nm Raman laser system designed to scan a patient's finger transcutaneously without collecting any specimen [7].
2. Measurement Procedure: - Position the patient's finger comfortably on the scanner. - Acquire the Raman spectrum from the finger. The specific acquisition time may vary per device setup.
3. Data Analysis and Machine Learning: - For COVID-19 Detection (Classification): - Use a machine learning classifier (e.g., Support Vector Machine or similar) trained on Raman spectra from patients with PCR-confirmed COVID-19 status. - Perform model validation using k-fold cross-validation (e.g., five-fold) and report sensitivity, specificity, and AUROC [7]. - For Blood Glucose Monitoring (Regression): - Use a machine learning regression algorithm trained on Raman spectra paired with reference blood glucose measurements (e.g., from a Dexcom sensor or Accu-Chek device). - Validate the model using cross-validation and report metrics such as the Area Under the Precision-Recall Curve (AUPR) [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Molecular Fingerprinting Experiments
| Item | Function / Application | Specific Examples & Notes |
|---|---|---|
| Blood Collection Tubes | Collection and preservation of whole blood samples. | EDTA or heparin tubes for plasma separation. |
| Quality Control Serum | Monitoring instrument performance and measurement reproducibility over time. | Commercially obtained pooled human serum [24]. |
| Cuvette Cleaning Solution | Preventing carryover contamination between sample measurements in liquid analysis. | Specific solution depends on the biofluid and instrument manufacturer. |
| Raman Laser | Light source for exciting molecular vibrations in Raman spectroscopy. | 830 nm laser used in finger-scanning device [7]. |
| Enzymatic Detection Reagents | Chromogenic detection in immunoassays; can be used for validation. Enzyme: Horseradish Peroxidase (HRP). Substrate: TMB (3,3',5,5'-tetramethylbenzidine), yields soluble blue product measurable at 650nm (or yellow at 450nm when stopped); DAB (3,3'-diaminobenzidine), yields insoluble brown precipitate [25] [26]. | |
| Enzymatic Detection Reagents | Chromogenic detection in immunoassays; can be used for validation. Enzyme: Alkaline Phosphatase (AP). Substrate: p-NPP (p-nitrophenylphosphate), yields soluble yellow product measurable at 405-410nm; BCIP/NBT, yields insoluble blue/purple precipitate [25] [26]. | |
| Reference Glucose Meter | Providing ground-truth data for training and validating Raman glucose models. | Dexcom sensor, Accu-Chek device [7]. |
| PCR Test Kits | Providing ground-truth data for training and validating Raman or EMF infection models. | Nasal PCR tests for COVID-19 [7]. |
| C15H22ClNS | C15H22ClNS Research Chemical | High-purity C15H22ClNS for laboratory research. This product is for Research Use Only (RUO), not for human or veterinary diagnostics. |
| C16H19N3O6S3 | C16H19N3O6S3, MF:C16H19N3O6S3, MW:445.5 g/mol | Chemical Reagent |
Recent breakthroughs and exploratory research directions (2024-2025)
Blood spectroscopy continues to revolutionize medical diagnostics by providing non-invasive, rapid, and reagent-free analytical capabilities. The period of 2024-2025 has witnessed significant technological breakthroughs across multiple spectroscopic domains, particularly through integration with artificial intelligence and nanotechnology. This application note details the most recent advances in vibrational spectroscopy, diffuse correlation spectroscopy, and related techniques for blood-based analysis, providing structured quantitative data and detailed experimental protocols for research implementation. These developments highlight a clear trend toward point-of-care diagnostics and personalized medicine, enabling unprecedented capabilities in therapeutic drug monitoring, cerebral blood flow measurement, and bloodstain forensics.
Recent Breakthroughs in Blood Spectroscopy Technologies
AI-Enhanced Surface-Enhanced Raman Spectroscopy for Drug Monitoring
Breakthrough Summary: Researchers from Harbin Medical University and the University of Oulu have developed a novel SERS platform integrating "molecular hook" technology with AI-driven spectral analysis for ultrasensitive detection of cardiovascular drugs in blood [27]. This approach achieves detection limits as low as 10 pg/mL for dobutamine hydrochloride and 10 ng/mL for milrinone, significantly below therapeutic thresholds, enabling real-time therapeutic drug monitoring previously impossible with conventional techniques.
Key Advantages Over Traditional Methods:
- Eliminates complex sample preparation required by LC-MS/MS
- Provides results in minutes rather than hours
- Enables selective binding of small drug molecules while excluding larger serum biomolecules
- Maintains SERS activity for at least five days, ensuring clinical reliability
Table 1: Performance Metrics of AI-SERS Drug Detection Platform
| Parameter | Dobutamine Hydrochloride | Milrinone | Traditional Methods |
|---|---|---|---|
| Detection Limit | 10 pg/mL | 10 ng/mL | ~1 ng/mL |
| Analysis Time | Minutes | Minutes | Hours |
| Sample Prep | Minimal | Minimal | Extensive |
| Selectivity | High (via molecular hooks) | High (via molecular hooks) | Moderate |
Deep Learning-Enhanced Diffuse Correlation Spectroscopy for Cerebral Blood Flow
Breakthrough Summary: A groundbreaking deep learning architecture called DCS-NET has been developed to transform the analysis of blood flow index (BFi) in diffuse correlation spectroscopy [28]. This approach demonstrates a 17,000-fold acceleration in processing speed compared to traditional three-layer fitting models while maintaining superior accuracy, particularly at larger source-detector distances (up to 30 mm) corresponding to deeper tissue measurements.
Technical Significance:
- Enables continuous real-time blood flow monitoring
- Exhibits enhanced anti-noise characteristics and reduced sensitivity to optical property variations
- Achieves only 8.35% error in relative BFi extraction compared to 43.76% with semi-infinite models
- Provides higher intrinsic sensitivity to deep tissues compared to fitting methods
ATR-FTIR Spectroscopy with Chemometrics for Bloodstain Age Estimation
Breakthrough Summary: Research published in July 2024 demonstrates a reliable, non-destructive approach for estimating time-since-deposition of bloodstains on various surfaces using ATR-FTIR spectroscopy combined with chemometric analysis [29]. The technique achieves exceptional predictive accuracy across multiple substrates, with the metal surface model showing minimal prediction error (RMSE: 1.1-1.43, R²: 0.84-0.89).
Forensic Applications:
- Strong performance across cement, metal, and wooden surfaces
- Majority of age-related transformations occur in 2800 cmâ»Â¹ to 3500 cmâ»Â¹ spectral range
- Enables crime scene reconstruction with unprecedented temporal accuracy
- Non-destructive preservation of evidence integrity
Quantitative Data Comparison of Spectroscopic Techniques
Table 2: Comprehensive Comparison of Recent Blood Spectroscopy Advancements
| Technique | Primary Application | Key Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|
| AI-Enhanced SERS [27] | Therapeutic drug monitoring | Detection limits: 10 pg/mL-10 ng/mL; Analysis time: Minutes | Ultra-sensitive, minimal sample prep, real-time capability | Requires nanoparticle functionalization |
| DCS-NET [28] | Cerebral blood flow monitoring | 17,000x speed increase; 8.35% rBFi error | Deep tissue penetration, noise-resistant, real-time | Computational resource requirements |
| ATR-FTIR/Chemometrics [29] | Bloodstain age estimation | RMSE: 1.1-1.43; R²: 0.84-0.89 | Non-destructive, substrate versatility, quantitative | Substrate-dependent accuracy |
| UV-Vis Spectroscopy [30] | Whole blood analysis | Spectral range: 215-2500 nm; Integration: 3.8 ms | Rapid screening, portable options, cost-effective | Limited molecular specificity |
| Diffuse Reflectance Spectroscopy [31] | Tissue oxygenation monitoring | Sensitivity: 64-92%; Specificity: 72-92% | Non-invasive, real-time tissue analysis | Pressure-dependent variability |
Detailed Experimental Protocols
Protocol: AI-SERS for Cardiovascular Drug Detection
Sample Preparation:
- Blood Collection & Processing: Collect whole blood via venipuncture using EDTA vacuum tubes. Centrifuge at 1500 × g for 10 minutes to separate plasma.
- Nanoparticle Functionalization: Prepare silver nanoparticle solution (50 nm diameter) and functionalize with A13 "molecular hook" molecules at 0.1 mM concentration for 2 hours at room temperature with gentle agitation.
- Sample-Nanoparticle Incubation: Mix 10 μL of plasma with 90 μL of functionalized nanoparticle solution. Incubate for 5 minutes to allow drug molecule capture.
- Calcium Ion-Induced Aggregation: Add 10 μL of 10 mM CaCl₂ solution to enhance "hotspot" formation, amplifying Raman signals.
Instrumentation Parameters:
- Spectrometer: Raman system with 785 nm excitation laser
- Laser Power: 10 mW at sample
- Integration Time: 10 seconds
- Spectral Range: 500-1800 cmâ»Â¹
- Resolution: 4 cmâ»Â¹
AI Analysis Workflow:
- Spectral Preprocessing: Apply vector normalization, baseline correction, and cosmic ray removal.
- Feature Extraction: Utilize principal component analysis to reduce dimensionality.
- Concentration Prediction: Implement trained neural network model (architecture: 3 hidden layers, ReLU activation, Adam optimizer) to convert spectral features to drug concentrations.
AI-SERS Drug Detection Workflow
Protocol: DCS-NET for Cerebral Blood Flow Monitoring
Instrument Setup:
- Source-Detector Configuration: Arrange multiple source-detector separations (5, 10, 15, 20, 25, and 30 mm) to enable depth-sensitive measurements.
- Laser Source: Utilize long-coherence-length laser at 785 nm or 850 nm wavelength.
- Detector System: Implement single-photon counting avalanche photodiodes (APDs) or superconducting nanowire single-photon detectors (SNSPDs).
- Correlator: Use digital correlator for computing intensity autocorrelation functions in real-time.
Data Acquisition Parameters:
- Measurement Duration: 1-5 seconds per time point
- Source-Detector Distances: 5-30 mm (multiple distances simultaneously)
- Sampling Rate: 10 Hz for dynamic flow monitoring
- Laser Power: <50 mW (within safety limits)
DCS-NET Implementation:
- Data Preprocessing: Normalize autocorrelation functions and arrange as input vectors.
- Network Architecture: Implement 1D convolutional neural networks with 5 convolutional layers, followed by 3 fully connected layers.
- Training Parameters: Use Adam optimizer with learning rate of 0.001, batch size of 64, and mean squared error loss function.
- BFi Extraction: Process measured intensity autocorrelation functions through trained DCS-NET to obtain blood flow index values.
DCS-NET Deep Learning Architecture
Protocol: ATR-FTIR Bloodstain Age Estimation
Sample Preparation:
- Substrate Preparation: Clean cement, metal, and wooden surfaces with ethanol and allow to dry completely.
- Blood Application: Apply 10 μL fresh human blood samples to each substrate type using micropipette.
- Controlled Aging: Store samples under controlled conditions (25°C, 50% RH) for time series analysis (0-11 days).
- Spectral Collection: Analyze triplicate samples from each time point.
ATR-FTIR Parameters:
- Instrument: FTIR spectrometer with ATR accessory (diamond crystal)
- Spectral Range: 4000-500 cmâ»Â¹
- Resolution: 4 cmâ»Â¹
- Scans per Spectrum: 32
- Background Correction: Collect background spectrum before each sample
Chemometric Analysis:
- Spectral Preprocessing: Apply vector normalization and second derivative transformation (Savitzky-Golay, 13-point window).
- Principal Component Analysis: Reduce dimensionality while retaining 95% of spectral variance.
- Regression Modeling: Develop Orthogonal Signal Correction Partial Least Square Regression (OSC-PLSR) models for age prediction.
- Validation: Use leave-one-out cross-validation and external validation sets.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Advanced Blood Spectroscopy
| Reagent/Material | Application | Function | Specifications |
|---|---|---|---|
| A13 Functionalized Silver Nanoparticles [27] | AI-SERS Drug Detection | Molecular hooks for selective drug capture | 50 nm diameter, 0.1 mM in aqueous solution |
| SPINREACT Control Sera [32] | FTIR Serum Modeling | Certified reference material for method validation | Lyophilized, ~38 certified parameters |
| Zinc Selenide (ZnSe) Substrates [32] | ATR-FTIR Spectroscopy | IR-transparent substrate for serum analysis | 50 mm diameter, 3 mm thickness |
| QP450-XSR Optical Fibers [30] | UV-Vis/DCS Systems | Solarization-resistant light transmission | 450 μm core, stainless steel jacketing |
| Diamond ATR Crystal [29] | Bloodstain Analysis | Internal reflection element for solid samples | Single bounce, 2 mm diameter |
| Deep-UV Deuterium-Tungsten Source [30] | UV-Vis Blood Analysis | Broadband illumination for absorbance | 215-2500 nm range, 30 min warm-up |
| C29H25Cl2NO4 | C29H25Cl2NO4|High-Purity Reference Standard | Bench Chemicals | |
| C21H15BrN2O5S2 | C21H15BrN2O5S2, MF:C21H15BrN2O5S2, MW:519.4 g/mol | Chemical Reagent | Bench Chemicals |
Implementation Considerations & Future Directions
The integration of artificial intelligence with spectroscopic techniques represents a paradigm shift in blood analysis, moving from purely analytical instruments to intelligent diagnostic systems. Future research directions should focus on:
- Multi-modal Integration: Combining SERS with DCS and FTIR approaches for comprehensive blood characterization
- Miniaturization: Developing handheld spectroscopic devices for true point-of-care applications
- Expanded Biomarker Panels: Validating these techniques for simultaneous monitoring of multiple disease biomarkers
- Regulatory Pathway: Establishing standardized protocols for clinical adoption and regulatory approval
These recent breakthroughs demonstrate that spectroscopic blood analysis is transitioning from research laboratories to clinical implementation, offering unprecedented capabilities for personalized medicine, therapeutic monitoring, and non-invasive diagnostics.
Advanced Methodologies and Translational Clinical Applications
Therapeutic Drug Monitoring (TDM) is a critical clinical process for measuring drug concentrations in patient blood to optimize dosage regimens, particularly for drugs with a narrow therapeutic index [33]. Conventional TDM methods like liquid chromatography-mass spectrometry (LC-MS/MS) and immunoassays present limitations including complex sample preparation, lengthy analysis times, and high costs [34] [35]. Surface-Enhanced Raman Spectroscopy (SERS) has emerged as a powerful analytical technique that overcomes these limitations by providing rapid, sensitive, and specific detection of drugs in complex biological matrices like blood, serum, and plasma [33]. This Application Note details experimental protocols and recent advancements in SERS-based TDM for cardiovascular and antibiotic drugs, supporting their integration into clinical diagnostics and personalized medicine.
SERS-Based TDM for Cardiovascular Drugs
Protocol: Determination of Dobutamine and Milrinone in Blood
Principle: This protocol utilizes functionalized silver nanoparticles as "molecular hooks" to selectively capture drug molecules while excluding larger serum biomolecules, combined with artificial intelligence for automated spectral analysis [27].
Materials and Reagents:
- Self-assembled silver nanoparticles (AgNPs)
- A13 functionalization molecule (acts as molecular hook)
- Dobutamine hydrochloride standard
- Milrinone standard
- Calcium ions (for nanoparticle aggregation)
- Ethylenediaminetetraacetic acid (EDTA) or heparin blood collection tubes
Instrumentation:
- Raman spectrometer with 785 nm laser excitation
- Transmission Electron Microscopy (TEM) for nanoparticle characterization
- Scanning Electron Microscopy (SEM)
- UV-Vis spectrophotometer
Procedure:
- Nanoparticle Functionalization: Functionalize AgNPs with A13 "molecular hook" molecules to create selective binding sites for drug molecules [27].
- Sample Preparation: Mix 15 μL of functionalized AgNPs with 15 μL of blood sample. Drop the mixture onto a Raman-compatible slide and allow to dry at room temperature in the dark [36].
- Signal Enhancement: Introduce calcium ions to induce controlled nanoparticle aggregation, generating electromagnetic "hotspots" that amplify drug-specific Raman signals [27].
- SERS Measurement: Acquire spectra using 785 nm laser excitation, 5 mW laser power, 50x objective, and 40 s exposure time across the 500-1600 cmâ»Â¹ fingerprint region [36].
- Data Analysis: Process spectra using AI algorithms for automated drug quantification, eliminating human error and accelerating detection [27].
Performance Characteristics: Table 1: Analytical Performance of SERS-Based Detection for Cardiovascular Drugs
| Drug | Limit of Detection | Therapeutic Range | Key Raman Bands (cmâ»Â¹) |
|---|---|---|---|
| Dobutamine hydrochloride | 10 pg/mL | Not specified | Not specified |
| Milrinone | 10 ng/mL | Not specified | Not specified |
Research Reagent Solutions
Table 2: Essential Reagents for SERS-Based Cardiovascular Drug Monitoring
| Reagent | Function | Specifications |
|---|---|---|
| Silver Nanoparticles (AgNPs) | SERS substrate providing electromagnetic enhancement | Functionalized with A13 "molecular hooks," characterized by UV-Vis and SEM |
| A13 Molecule | Molecular hook for selective drug capture | Selective for small drug molecules, excludes larger biomolecules |
| Calcium Ions | Nanoparticle aggregant | Generates dense electromagnetic "hotspot" regions |
SERS-Based TDM for Antibiotics
Protocol: Determination of Ceftriaxone, Ampicillin, and Vancomycin in Serum
Principle: This protocol employs tungsten disulfide/gold and silver core-shell (WSâ‚‚/Au@Ag) nanocomposites as SERS substrates with enhanced uniformity and sensitivity, combined with a two-dimensional convolutional neural network (2D-CNN) for quantitative analysis of antibiotic mixtures in serum [34].
Materials and Reagents:
- WSâ‚‚/Au@Ag nanocomposites
- Ceftriaxone, ampicillin, and vancomycin standards
- Fetal bovine serum (FBS) or human serum
- Chloroauric acid tetrahydrate (HAuCl₄·4H₂O)
- Sodium citrate dihydrate (C₆H₅Na₃O₇·2H₂O)
- Silver nitrate (AgNO₃)
- WSâ‚‚ dispersion
Instrumentation:
- Raman spectrometer
- UV-Vis spectroscopy
- Dynamic light scattering (DLS) instrument
- Transmission Electron Microscopy (TEM)
Procedure:
- Substrate Synthesis: Prepare WSâ‚‚/Au@Ag nanocomposites by conjugating WSâ‚‚ onto Au@Ag core-shell nanoparticles. Characterize using UV-Vis, DLS, and TEM [34].
- Sample Preparation: Mix serum samples with WSâ‚‚/Au@Ag nanocomposites. For qualitative identification, use characteristic Raman bands: 1353 cmâ»Â¹ for ceftriaxone, 1000 cmâ»Â¹ for ampicillin, and 1594 cmâ»Â¹ for vancomycin [34].
- SERS Measurement: Acquire spectra using 785 nm laser excitation. For quantitative analysis, collect multiple spectra from each sample to generate sufficient data for 2D-CNN processing [34].
- Data Analysis: Convert spectral data into 2D arrays and process with a 2D-CNN regression model to predict concentrations of individual antibiotics in mixture samples [34].
Performance Characteristics: Table 3: Analytical Performance of SERS-Based Detection for Antibiotics
| Antibiotic | Linear Range (μg/mL) | Limit of Detection | Therapeutic Range |
|---|---|---|---|
| Ceftriaxone | 0.5-1000 | Not specified | Not specified |
| Ampicillin | 0.5-1000 | Not specified | Not specified |
| Vancomycin | 0.5-1000 | Not specified | 10.0–15.0 μg/mL |
The WSâ‚‚/Au@Ag substrate demonstrates superior enhancement effect, with detection limit for R6G as low as 10â»Â¹â´ M [34].
Research Reagent Solutions
Table 4: Essential Reagents for SERS-Based Antibiotic Monitoring
| Reagent | Function | Specifications |
|---|---|---|
| WSâ‚‚/Au@Ag Nanocomposites | SERS substrate with enhanced uniformity and sensitivity | Core-shell structure, provides adsorption properties and biocompatibility |
| Transition Metal Dichalcogenides (WSâ‚‚) | Composite component | Allows uniform analyte distribution, enhances Raman effect |
| 2D-CNN Algorithm | Data processing model | Converts spectral data to 2D arrays for concentration prediction |
Workflow Visualization
SERS-TDM Experimental Workflow: This diagram illustrates the integrated process for SERS-based therapeutic drug monitoring, from sample collection to result interpretation, highlighting key substrate technologies and data analysis methods.
Technological Advancements and Clinical Implementation
Integrated Automated Systems
The ACU-SERS project exemplifies the clinical translation of SERS-TDM technology, developing a fully automated system that integrates centrifugal microfluidics with SERS chip technology [37]. This system performs biological sample pre-treatment, analyte separation, and analysis in a single benchtop device, providing quantitative antibiotic drug levels within approximately 15 minutes [37]. This represents a significant improvement over conventional methods that require hours or days, particularly crucial for sepsis management in intensive care units where rapid dose adjustment can be life-saving.
Advanced Substrate Design
Recent innovations in SERS substrates have substantially improved the sensitivity and reliability of TDM applications:
- Bimetallic nanoparticles: Core-shell structures such as Au@Ag NPs offer tunable plasmonic properties and enhanced electromagnetic fields [33].
- Composite substrates: Materials like WSâ‚‚/Au@Ag nanocomposites combine the advantages of plasmonic metals and semiconductors, providing more uniform analyte distribution and addressing limitations of traditional substrates including cost, uniformity, and stability [34].
- Molecular hooks: Functionalized nanoparticles with specific capture molecules enable selective binding of target drug molecules while excluding interfering biomolecules [27].
Artificial Intelligence Integration
The combination of SERS with machine learning algorithms represents a paradigm shift in spectral analysis:
- 2D-CNN models: Effectively process spectral data for quantitative prediction of drug concentrations in complex mixtures, outperforming traditional linear regression methods [34].
- Automated analysis: AI-driven spectral processing eliminates human error and accelerates detection, enabling real-time clinical applications [27].
- Multivariate analysis: Techniques including Principal Component Analysis (PCA) and Partial Least Squares Discriminant Analysis (PLS-DA) enable classification and quantification of drugs even at low concentrations in complex body fluids [36].
Challenges and Future Perspectives
Despite significant advancements, several challenges remain in the widespread clinical implementation of SERS for TDM. Substrate reproducibility and standardization continue to be hurdles, though recent developments in ordered nanostructures like AgNP/AAO substrates show promise for quantitative SERS measurements with variations below 10% [38]. Matrix effects from complex biological samples can interfere with detection, addressed through strategies such as sample filtration [39], "molecular hook" technology [27], and composite substrates with improved selectivity [34].
Future development will focus on creating multiplexed detection platforms for simultaneous monitoring of multiple drugs, expanding the technique to broader classes of therapeutics including antiepileptics and immunosuppressants [37], and developing point-of-care devices for decentralized testing. As SERS technology continues to mature with improvements in substrate design, AI integration, and automated systems, it holds tremendous potential to revolutionize therapeutic drug monitoring and usher in an era of personalized precision medicine.
Endometrial Cancer Detection with IR and Raman Spectroscopy
Endometrial cancer (EC) is the sixth most common cancer among women globally, and the development of rapid, non-invasive screening methods remains a critical unmet clinical need [40]. Current diagnostic pathways rely on invasive tissue collection and histopathological evaluation, which are time-consuming and subjective [41]. Blood spectroscopy research offers a paradigm shift, leveraging the molecular "fingerprint" of biofluids for diagnostic purposes. Vibrational spectroscopy techniques, specifically Infrared (IR) and Raman spectroscopy, probe the biochemical composition of blood plasma or serum by detecting changes in proteins, nucleic acids, and lipids associated with carcinogenesis [40] [41] [8]. This Application Note details the experimental protocols and summarizes the quantitative performance of these emerging techniques for the rapid detection of endometrial cancer, providing a framework for their implementation in research and clinical development settings.
Research studies have demonstrated the high diagnostic potential of both Raman and IR spectroscopy when applied to blood-derived samples. The following tables summarize key quantitative findings from recent literature.
Table 1: Overall Diagnostic Performance of Spectroscopy Techniques for Endometrial Cancer Detection
| Analytical Technique | Sample Type | Key Differentiation | Accuracy | Sensitivity | Specificity | Reference |
|---|---|---|---|---|---|---|
| Raman Spectroscopy | 'Wet' Blood Plasma | EC vs. Healthy Controls | 82% | - | - | [40] |
| ATR-FTIR Spectroscopy | 'Wet' Blood Plasma | EC vs. Healthy Controls | 78% | - | - | [40] |
| Combined Raman & ATR-FTIR | 'Wet' Blood Plasma | EC vs. Healthy Controls | 86% | - | - | [40] |
| ATR-FTIR Spectroscopy | Dry Blood Plasma | EC vs. Healthy Controls | 83% | - | - | [40] |
| Surface-Enhanced Raman Spectroscopy (SERS) | Dry Blood Plasma | Adenocarcinoma vs. Control & Hyperplasia | 85% | 66% | 92% | [42] [43] |
| SERS | Dry Blood Plasma | Adenocarcinoma vs. Hyperplasia (incl. Polyps) | 91% | 93% | 88% | [42] |
Table 2: Spectral Biomarkers Associated with Endometrial Carcinogenesis
| Spectroscopic Technique | Molecular Assignments (Wavenumber cmâ»Â¹) | Associated Biochemical Changes in Endometrial Cancer | Reference |
|---|---|---|---|
| Raman Spectroscopy | 812, 1065, 1293 (Nucleic Acids); 890 (Proline/Hydroxyproline); 1447 (Proteins/Lipids); 1695 (Amide I) | Changes in nucleic acids, alterations in collagen (proline/hydroxyproline), shifts in protein structure (amide I), and lipid composition. | [41] |
| FTIR Spectroscopy | ~1168, 1245 (C-O, Amide III); ~1560 (Amide II); ~1650 (Amide I); ~2842 (Lipids) | Vibrational changes in carbohydrates, proteins (amides I, II, and III), and lipids. | [41] |
| SERS | Peaks consistent with proteins, lipids, and nucleic acids in the fingerprint region (500-1800 cmâ»Â¹). | Specific spectral patterns enabling differential diagnosis of adenocarcinoma, hyperplasia, and polyps. | [42] [43] |
Detailed Experimental Protocols
Protocol: Blood Plasma Analysis via ATR-FTIR and Raman Spectroscopy
This protocol is adapted from a study comparing 'wet' and dry plasma analysis for EC detection [40].
Sample Collection and Preparation
- Blood Collection: Collect peripheral blood using EDTA or heparin tubes from consented patients (EC group) and healthy controls.
- Plasma Separation: Centrifuge blood samples at 1,500-2,000 × g for 10 minutes. Carefully aspirate the supernatant plasma layer.
- Sample Preparation (Two Methods):
- 'Wet' Plasma Analysis: Use freshly prepared plasma immediately after separation with minimal preprocessing.
- Dry Plasma Analysis: Spot 2-10 µL of plasma onto a suitable substrate (e.g., quartz for Raman, metal-coated slide for SERS, or an ATR crystal). Allow the sample to air-dry completely at room temperature in a desiccator.
Instrumentation and Data Acquisition
- ATR-FTIR Spectroscopy:
- Instrument: Use a Fourier Transform Infrared spectrometer equipped with an Attenuated Total Reflection (ATR) accessory (e.g., diamond crystal).
- Acquisition Parameters: Acquire spectra over the range of 4000–400 cmâ»Â¹. Co-add 64-128 scans at a resolution of 4 cmâ»Â¹. Collect a background spectrum (ambient air) before each sample or set of samples.
- Raman Spectroscopy:
- Instrument: Use a Raman spectrometric system with a 785 nm laser excitation source to minimize fluorescence and a CCD detector.
- Acquisition Parameters: For 'wet' plasma, use a low-power laser (<100 mW) with short integration times (seconds). For dry plasma or SERS, optimize power and integration time (e.g., 10-30 seconds). Acquire multiple spectra (e.g., 3-10) from different spots per sample to account for heterogeneity.
Data Preprocessing and Analysis
- Preprocessing: Apply vector normalization (e.g., Euclidean norm) to all spectra [40] [44]. Perform baseline correction to remove fluorescence background (e.g., asymmetric least squares smoothing) [42].
- Multivariate Analysis & Machine Learning:
- Use Principal Component Analysis (PCA) for unsupervised exploration of spectral variance and dimensionality reduction [40] [45].
- Employ machine learning algorithms such as k-Nearest Neighbors (kNN), Support Vector Machines (SVM), or Partial Least Squares-Discriminant Analysis (PLS-DA) to build classification models [40] [45] [43].
- Validate models using k-fold cross-validation (e.g., 5- or 10-fold) and/or an independent test set of spectra not used in model training.
Protocol: Surface-Enhanced Raman Spectroscopy (SERS) for Differential Diagnosis
This protocol is adapted from studies using SERS to distinguish EC from benign conditions [42] [43].
SERS Substrate Preparation
- Silver Nanoparticle Substrate: Utilize a substrate composed of dried silver colloid to achieve the surface enhancement effect. This can be prepared by reducing silver salts (e.g., Lee & Meisel method) and depositing the colloid onto a solid support [42].
- Characterization: Validate substrate uniformity and enhancement factor using techniques like Transmission Electron Microscopy (TEM) and by measuring the SERS signal of a standard analyte [27].
Sample Preparation and Measurement
- Plasma Application: Spot 1-2 µL of the prepared blood plasma onto the SERS-active silver substrate and allow it to dry.
- SERS Measurement: Place the substrate on the microscope stage of the Raman system. Focus the laser on the sample surface. Acquire multiple spectra (e.g., 3 per sample) from random locations to ensure representative sampling.
Data Analysis
- Follow the preprocessing and analysis steps outlined in section 3.1.3. PLS-DA has been successfully applied to SERS data for discriminating adenocarcinoma, hyperplasia, polyps, and healthy controls with high accuracy [43].
Diagram Title: SERS-Based Diagnostic Workflow
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Blood-Based Spectroscopy
| Item | Function/Benefit | Example/Notes |
|---|---|---|
| Anticoagulant Blood Tubes | Prevents coagulation for plasma separation. | EDTA or heparin tubes are standard. |
| SERS-Active Substrates | Amplifies Raman signal by orders of magnitude for high-sensitivity detection. | Colloidal silver nanoparticles [42] or functionalized nanoparticles with "molecular hooks" [27]. |
| ATR-FTIR Crystals | Enables direct, non-destructive analysis of liquid and solid samples. | Diamond is durable and chemically inert; suitable for blood plasma. |
| Chemometrics Software | For preprocessing spectra, multivariate analysis, and building classification models. | PLS Toolbox, SIMCA, or custom scripts in Python/R/MATLAB. |
| Machine Learning Libraries | Training and validation of diagnostic algorithms. | Scikit-learn (Python), Caret (R); used for kNN, SVM, etc. [40] [45]. |
| Reference Standards | Validates instrument performance and SERS substrate activity. | Polystyrene, 4-mercaptobenzoic acid, or other compounds with known Raman peaks. |
| C20H25BrN2O7 | C20H25BrN2O7|High-Purity Reference Standard | |
| Cadmium isooctanoate | Cadmium isooctanoate, CAS:30304-32-6, MF:C16H30CdO4, MW:398.82 g/mol | Chemical Reagent |
IR and Raman spectroscopy represent a revolutionary approach for the rapid, non-invasive detection of endometrial cancer directly from blood plasma. The methodologies outlined herein provide researchers with a robust framework to explore these techniques further. Achieving diagnostic accuracies exceeding 85%, particularly when techniques are combined or enhanced with SERS and machine learning, underscores their significant potential [40] [42]. Future work should focus on standardizing protocols, validating findings in large-scale, multi-center cohorts, and further elucidating the specific biomolecular signatures underpinning the spectral changes to translate this promising technology from the research bench to the clinical laboratory.
The management of metabolic disorders like diabetes relies on frequent monitoring of key biomarkers, primarily blood glucose. Traditional invasive methods, which require blood extraction via finger-pricking, cause patient discomfort and carry infection risks, leading to poor adherence [46] [47]. Non-invasive optical techniques present a promising alternative by using light to probe blood analytes through the skin. These methods are painless, reduce infection risk, and enable continuous monitoring, thereby facilitating better disease management and personalized treatment strategies [48] [47].
This application note details the experimental protocols and key methodologies for three leading optical techniques—Near-Infrared (NIR) Spectroscopy, Mid-Infrared Optoacoustic Sensing, and Raman Spectroscopy. We frame these within the broader context of medical diagnostic applications of blood spectroscopy research, providing structured quantitative data, detailed workflows, and essential reagent information to support researchers and drug development professionals in implementing these approaches.
Comparative Analysis of Non-Invasive Optical Techniques
The following table summarizes the core operational principles, performance metrics, and comparative advantages of the three primary non-invasive optical monitoring techniques.
Table 1: Comparison of Key Non-Invasive Glucose Monitoring Techniques
| Technique | Principle | Reported Accuracy (MAECV/MSEP) | Key Advantages | Primary Challenges |
|---|---|---|---|---|
| Near-Infrared (NIR) Spectroscopy | Measures absorption of NIR light by glucose in tissue [48] | RMSEP: 0.835 mmol/L (specific setup) [48] | Deep tissue penetration; Can use inexpensive LEDs [48] [49] | Strong interference from water & hemoglobin; Scattering effects [48] [49] |
| Depth-Gated Mid-IR Optoacoustic (DIROS) | Pulse of mid-IR light generates ultrasound via optoacoustic effect; time-gating selects depth [47] | MAECV: 11 mg/dL (with time-gating) [47] | High spectral specificity of mid-IR; Depth-selective measurement targets vasculature [47] | Complex instrumentation; Sensitivity to superficial skin heterogeneity [47] |
| Raman Spectroscopy | Analyzes inelastically scattered (Raman) light providing a molecular "fingerprint" [50] | Clinical agreement vs. blood tests (Study with 50 type 2 diabetics) [50] | High specificity; Minimal water interference; Pre-trained models reduce calibration [50] | Inherently weak signal; Requires long acquisition times (~50 sec) [50] [49] |
Detailed Experimental Protocols
Protocol for NIR Spectroscopy with Machine Learning
This protocol outlines a method for non-invasive blood glucose estimation using NIR spectroscopy and a stacked auto-encoder (SAE) deep neural network, suitable for data from human palms or blood samples [48] [49].
Experimental Workflow:
The logical flow of the experiment, from sample preparation to final prediction, is outlined below.
Key Materials & Equipment:
- Light Source: Super Luminescent Emitting Diodes (SLDs) at wavelengths such as 1050 nm, 1150 nm, and 1600 nm, which correspond to glucose absorption peaks [48].
- Optical Setup: A fiber optic bundle and probe for delivering light to the measurement site (e.g., palm) and collecting diffuse reflectance spectra [48].
- Detector: A spectrometer, such as an AS7341 11-channel spectrometer IC, for capturing spectral data [49].
- Reference Glucose Measurement: A portable blood glucose meter (e.g., GT-1820) or continuous glucose monitor (CGM) for obtaining reference values during an Oral Glucose Tolerance Test (OGTT) [48] [47].
Procedure:
- Subject Preparation & OGTT: Participants should fast before the experiment. Conduct an OGTT by administering a glucose solution and collecting spectral data alongside reference blood glucose measurements at regular intervals to capture a wide range of glucose concentrations [48].
- Spectral Data Acquisition: Position the optical probe firmly on the measurement site (e.g., the palm). Acquire diffuse reflectance spectra in the 1050-1700 nm range throughout the OGTT. Each spectral recording should be associated with a timestamped reference glucose value [48].
- Data Preprocessing: Process raw spectral data to reduce noise and correct for baseline effects. Techniques include vector normalization using the Euclidean (L2) norm [44].
- Modeling and Prediction:
- Initial PLSR Modeling: First, use a Partial Least Squares Regression (PLSR) model on the preprocessed spectra. This linear model helps eliminate poorly correlated samples and provides initial features [48].
- SAE Deep Neural Network Processing: Use the output from the PLSR model as the input to a Stacked Auto-Encoder (SAE) deep neural network. The SAE model, with its multiple hidden layers, learns complex, non-linear relationships between the spectral features and blood glucose levels, ultimately providing the final prediction [48].
Protocol for Depth-Gated Mid-IR Optoacoustic Spectroscopy (DIROS)
This protocol describes a method for depth-resolved, non-invasive glucose sensing in humans using the DIROS technology, which combines mid-infrared spectroscopy with ultrasound detection for depth selection [47].
Experimental Workflow:
The following diagram illustrates the core principle and steps of the DIROS measurement process.
Key Materials & Equipment:
- DIROS Sensor: A confocal setup comprising a pulsed mid-infrared light source (tunable across 925–1250 cmâ»Â¹), a focused broadband piezoelectric ultrasound transducer (UST), and a zinc sulfide (ZnS) window [47].
- Reference Glucose Monitor: A continuous glucose monitor (CGM) is used for obtaining reference interstitial glucose measurements [47].
- Data Acquisition System: A system for synchronizing wavelength scanning with ultrasound time-of-flight detection and recording optoacoustic spectra.
Procedure:
- Sensor Placement: Position the subject's hand such that the skin flap of the first interdigital space is placed against the ZnS window of the DIROS sensor [47].
- Signal Acquisition & Time-Gating: Illuminate the skin with pulsed MIR light. The absorption of light by glucose and other components generates broadband ultrasound waves via the optoacoustic effect. Record the signals detected by the UST. Crucially, apply time-gating to the received signals, selecting time windows that correspond to ultrasound waves originating from specific skin depths (e.g., deeper layers rich in microvasculature) based on their time-of-flight [47].
- Spectral Reconstruction: Reconstruct an optoacoustic spectrum for the selected depth by scanning the MIR light wavelength.
- Multivariate Model Fitting: Train a multivariate regression model (e.g., using Partial Least Squares regression) on the time-gated optoacoustic spectra. Use leave-one-out cross-validation (LOOCV) to assess the model's accuracy in predicting glucose concentrations against the CGM reference values [47].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of non-invasive monitoring protocols requires specific reagents and materials. The following table details key solutions and their functions in a research context.
Table 2: Key Research Reagent Solutions for Non-Invasive Sensing Development
| Item Name | Function/Application in Research |
|---|---|
| Intralipid Solutions | Used as tissue-simulating phantoms for initial validation of NIR and other optical systems due to their controlled scattering properties [48]. |
| A13 "Molecular Hook" Functionalized Nanoparticles | Surface-enhanced Raman spectroscopy (SERS) substrates designed to selectively capture small drug molecules (e.g., cardiovascular drugs) while excluding larger biomolecules, minimizing interference in complex biofluids [27]. |
| 5% Dextrose Injection Solution & Sterile Water | Used in in vitro studies with blood samples (e.g., canine blood) to create a series of diluted and concentrated blood samples, generating a range of glucose concentrations for method calibration and validation [49]. |
| Silver Nanoparticles | Serve as the plasmonic substrate in SERS applications. Aggregation of these nanoparticles, induced by calcium ions, creates electromagnetic "hotspots" that dramatically amplify the weak Raman signals of target analytes [27]. |
| Folin Wu Colouring Reagent | A component of the older, reference Modified Folin Wu method for blood glucose estimation. Used in comparative studies to validate the accuracy of new, non-invasive methods against established (though invasive) laboratory techniques [46]. |
| Vanadium(4+) tetraformate | Vanadium(4+) Tetraformate - CAS 60676-73-5 |
| Isodecyl nonyl phthalate | Isodecyl Nonyl Phthalate|High-Purity Phthalate |
Non-invasive monitoring of blood glucose and other metabolic indicators via optical spectroscopy is a rapidly advancing field with significant potential to transform clinical diagnostics and personalized medicine. The protocols and data presented here for NIR, DIROS, and Raman spectroscopy provide a foundational toolkit for researchers and drug development professionals. While challenges related to accuracy, miniaturization, and individual variability remain, the integration of advanced data processing techniques like deep learning and the development of novel sensing strategies are steadily overcoming these hurdles. Future work will focus on the refinement of these technologies for robust, long-term, and continuous monitoring applications, ultimately enabling better management of metabolic disorders.
Red blood cell (RBC) membrane disorders constitute a heterogeneous group of hemolytic anemias whose accurate diagnosis is essential for appropriate clinical management [51]. The integration of advanced spectroscopic techniques with conventional clinical haematology provides a powerful toolkit for dissecting the structural and functional integrity of the erythrocyte membrane. These methodologies enable researchers and clinicians to probe molecular-level alterations in membrane composition, fluidity, and cytoskeletal organization that underlie pathological states, offering insights that complement standard diagnostic parameters [4] [52] [53]. This document details standardized protocols and applications for key spectroscopic and biophysical techniques in the analysis of RBC membrane disorders, framed within the broader context of medical diagnostic applications of blood spectroscopy research.
Spectroscopic Techniques for RBC Membrane Analysis
Quasi-Elastic Light Scattering (QELS) Spectroscopy
Principle: QELS measures intensity fluctuations of laser light scattered from a sample, analyzed via power spectra and the intensity autocorrelation function to probe membrane dynamics [54]. The correlation time (Tcorr) serves as a key parameter for comparing results, reflecting the physical properties of the membrane-cytoskeleton complex.
Protocol:
- Sample Preparation: Isolate RBCs from fresh whole blood via centrifugation and washing in isotonic buffer (e.g., phosphate-buffered saline). Adjust hematocrit to approximately 0.5% for optimal scattering intensity.
- Instrument Setup: Utilize a QELS microscope spectrometer with a laser source (e.g., He-Ne laser). Align optical components to ensure the laser is focused on the cell membrane.
- Data Acquisition: Record scattered light intensity fluctuations from individual RBCs for a minimum of 60 seconds per measurement. Maintain temperature control at 37°C using a stage heater.
- Data Analysis: Calculate the intensity autocorrelation function g(²)(τ). Fit the decay with a single exponential to extract the correlation time Tcorr. Compare Tcorr values under different physiological or pharmacological perturbations.
- Quality Control: Include control samples from healthy donors in each experiment. Verify instrument performance using standard latex bead suspensions.
Applications: QELS detects biochemically induced changes in membrane deformability. Increased cytoplasmic viscosity (via osmotic manipulation), elevated membrane cholesterol content, or higher intracellular calcium all significantly increase Tcorr, indicating reduced membrane flexibility [54]. The technique can also distinguish age-separated RBC populations, with older, less deformable cells exhibiting longer correlation times.
Fluorescence Anisotropy for Membrane Microviscosity
Principle: This technique measures the rotational diffusion of a lipophilic fluorescent probe (e.g., PKH26) incorporated into the lipid bilayer. Time-resolved fluorescence anisotropy decay provides a direct assessment of membrane microviscosity, a key parameter of membrane fluidity and order [55].
Protocol:
- Staining Procedure: Incubate washed RBCs with PKH26 dye at a final concentration of 2 μM for 5 minutes. Terminate staining by adding an equal volume of serum or protein solution.
- Purification: Remove unincorporated dye by centrifugation through a density gradient or multiple washing steps.
- Time-Resolved Fluorescence Measurement: Place labeled RBCs in a quartz cuvette. Use a time-correlated single photon counting fluorometer with polarizers to record anisotropy decay curves. Excitate at 551 nm and collect emission at 567 nm.
- Data Analysis: Fit the anisotropy decay curve using a biphasic model to extract two correlation times corresponding to the rotational diffusion of free and membrane-bound probe molecules. Calculate membrane microviscosity (ηₘ) using the Stokes-Einstein relationship.
- Temperature Control: Perform measurements at multiple temperatures (e.g., 25°C, 37°C) to characterize thermal dependence of membrane fluidity.
Applications: Membrane microviscosity values typically range from 100–500 cP, varying with temperature [55]. This parameter serves as a sensitive indicator of membrane structural integrity, with alterations observed in diabetes, cardiovascular diseases, and COVID-19-related hemorheological abnormalities.
Infrared (IR) Spectroscopy of Hemoglobin and Membrane Components
Principle: IR spectroscopy detects molecular vibrational energies, providing a "fingerprint" of biochemical composition. It is particularly sensitive to hemoglobin ligand binding states and conformational changes relevant to hematological pathologies [4] [56].
Protocol:
- Sample Preparation: For RBC membrane studies, prepare hemoglobin-free white ghosts via hypotonic lysis and repeated centrifugation. Alternatively, use whole RBCs dried on IR-transparent substrates (e.g., zinc selenide).
- Spectral Acquisition: Employ Fourier Transform Infrared (FTIR) spectroscopy with a resolution of 4 cmâ»Â¹. Accumulate 32–64 scans per spectrum across the 4000–500 cmâ»Â¹ range.
- Data Processing: Perform vector normalization and linear baseline correction. Remove contributions from water vapor and COâ‚‚.
- Band Assignment: Identify key absorption bands: amide I (1650 cmâ»Â¹, protein secondary structure), lipid esters (1740 cmâ»Â¹), and heme-ligand vibrations (e.g., CO stretch at 1951 cmâ»Â¹ for HbACO).
- Quantitative Analysis: Use absorbance values or integrated band areas for multivariate statistical analysis or construction of regression models for component quantification.
Applications: IR spectroscopy identifies hemoglobin variants and ligand binding states through characteristic spectral shifts. For example, the CO stretching band shifts from 1951 cmâ»Â¹ in normal hemoglobin to 1970 cmâ»Â¹ in Hb Zurich and Hb Boston mutants [4]. It can also detect molecular alterations in membrane disorders through changes in protein secondary structure and lipid composition.
Eosin-5-Maleimide (EMA) Fluorescence Test for Band 3 Content
Principle: The EMA test uses flow cytometry to quantify band 3 protein content on RBC membranes. EMA covalently binds to lysine-430 on the first extracellular loop of band 3, with fluorescence intensity directly proportional to band 3 content [53].
Protocol:
- Labeling Reaction: Incubate 5 μL of washed RBCs with 25 μL of EMA working solution (0.5 mg/mL in PBS) for 60 minutes at room temperature in the dark.
- Termination and Washing: Stop the reaction by adding 1 mL of PBS containing 0.5% bovine serum albumin. Wash cells three times with PBS.
- Flow Cytometry Analysis: Resuspend labeled RBCs in 500 μL PBS. Analyze using a flow cytometer with a 488 nm excitation laser and fluorescence detection through a 530/30 nm bandpass filter.
- Data Interpretation: Record mean channel fluorescence (MCF) for at least 10,000 events. Express results as a ratio of patient MCF to control MCF. Analyze histogram patterns for abnormal cell populations.
- Controls: Include normal control samples with each assay run. Consider internal controls such as residual leukocytes.
Applications: The EMA test is a primary screening tool for hereditary spherocytosis (HS), where MCF ratios are typically reduced to 0.80–0.90 of normal controls due to membrane vesiculation and band 3 loss [53]. It can also detect other membranopathies with abnormal band 3 content or distribution.
Comparative Analysis of Techniques
Table 1: Quantitative Parameters for RBC Membrane Disorder Diagnostics
| Technique | Measured Parameters | Normal Range / Reference Values | Pathological Alterations |
|---|---|---|---|
| QELS [54] | Correlation time (Tcorr) | Baseline established from healthy controls | Increased in dehydrated cells, cholesterol-loaded membranes, and aged RBCs |
| Fluorescence Anisotropy [55] | Membrane microviscosity (ηₘ) | 100–500 cP (temperature-dependent) | Increased in oxidative stress and metabolic disorders |
| EMA Binding Test [53] | Mean Channel Fluorescence (MCF) ratio | 1.0 (normal control) | Reduced to 0.80–0.90 in hereditary spherocytosis |
| Osmotic Gradient Ektacytometry [53] | DImax (maximal deformability index), Omin (osmolality at minimum deformability) | DImax: 0.4–0.6; Omin: 150–160 mOsm/kg | Reduced DImax in spherocytosis; Increased Omin in hydrocytosis |
| IR Spectroscopy [4] | CO stretching vibration, Amide I/II ratio | 1951 cmâ»Â¹ for HbACO | Shifts to 1970 cmâ»Â¹ in Hb Zurich and Hb Boston mutants |
Table 2: Research Reagent Solutions for RBC Membrane Studies
| Reagent / Material | Function / Application | Specifications / Notes |
|---|---|---|
| PKH26 lipophilic dye [55] | Membrane labeling for fluorescence anisotropy | Long-chain carbocyanine; Excitation/emission: 551/567 nm |
| Eosin-5-Maleimide (EMA) [53] | Band 3 protein quantification | Covalently binds to lysine-430 of band 3; Use at 0.5 mg/mL |
| FTIR Substrate (Zinc Selenide) [57] | Sample substrate for IR measurements | IR-transparent; suitable for dried serum or membrane films |
| Dextran 70 kDa [55] | Inducer of RBC aggregation for microrheological studies | Used in "bridging model" of RBC aggregation |
| Control Sera (SPINREACT) [57] | Reference material for serum spectroscopy | Certified for 38 parameters; based on bovine blood serum |
Integrated Diagnostic Workflow
For a comprehensive assessment of RBC membrane disorders, we propose the following integrated workflow:
- Initial Screening: Perform EMA binding test and peripheral blood smear evaluation.
- Functional Characterization: Conduct osmotic gradient ektacytometry to assess deformability profile.
- Molecular Analysis: Apply IR spectroscopy to detect hemoglobin variants and membrane composition alterations.
- Biophysical Assessment: Utilize QELS and fluorescence anisotropy to evaluate membrane dynamics and microviscosity.
- Data Integration: Correlate findings from all techniques with genetic testing when indicated.
Experimental Pathway and Workflow Diagrams
Diagram 1: RBC Membrane Analysis Workflow. This diagram illustrates the integrated experimental pathway from sample collection to diagnosis, incorporating multiple spectroscopic techniques.
Diagram 2: Membrane Defects and Detection Methods. This diagram maps specific membrane abnormalities to appropriate spectroscopic detection techniques and their resulting diagnostic parameters.
The application of advanced spectroscopic techniques provides unprecedented insights into the molecular basis of RBC membrane disorders. The protocols outlined herein enable comprehensive characterization of membrane structure, dynamics, and function, facilitating both basic research and clinical diagnostics. Integration of these methodologies offers a multidimensional assessment approach that enhances diagnostic precision and provides a platform for evaluating therapeutic interventions targeting membrane properties.
Integration of AI and machine learning for spectral analysis and automation
The integration of Artificial Intelligence (AI) and machine learning (ML) with spectral analysis is fundamentally transforming the landscape of biomedical research and clinical diagnostics. In the specific context of blood analysis, these technologies are enabling the extraction of unprecedented levels of information from complex spectral data, facilitating faster, more accurate, and automated diagnostic processes. Spectral techniques, including fluorescence spectroscopy and hyperspectral imaging, generate rich, multidimensional datasets that are ideally suited for analysis by sophisticated AI algorithms [58] [52]. This synergy is particularly powerful for hematological diagnostics, where it allows researchers and clinicians to identify subtle, pathologically significant alterations in blood components that traditional methods might overlook [52].
The core value proposition of AI in this domain lies in its ability to learn complex, non-linear patterns from vast amounts of spectral data. Machine learning models, including convolutional neural networks (CNNs) and support vector machines (SVMs), can be trained to recognize the spectral fingerprints associated with specific diseases, metabolic states, or cellular abnormalities. This capability moves analysis beyond simple quantification to intelligent interpretation, paving the way for automated, high-throughput diagnostic systems [59]. The transition towards real-time data processing and cloud-based analysis solutions further amplifies this potential, making advanced spectral diagnostics more accessible and actionable in both research and clinical settings [58] [59].
The performance of various AI-integrated spectral methods can be quantitatively assessed based on their accuracy, sensitivity, and specificity in classifying blood-related samples. The following table summarizes key quantitative findings from recent research applications, highlighting the efficacy of these approaches.
Table 1: Performance Metrics of AI-Based Spectral Analysis in Blood Research
| Application Focus | Spectral Technique | AI/ML Model Used | Reported Accuracy | Key Performance Metrics | Source/Reference |
|---|---|---|---|---|---|
| Bloodstain Identification | Hyperspectral Imaging (HSI) | Support Vector Machine (SVM) | Outperformed state-of-the-art methods | High specificity against 8 non-blood substances | [60] |
| Bloodstain Identification | Hyperspectral Imaging (HSI) | Artificial Neural Network (ANN) | Outperformed state-of-the-art methods | Effective on multiple substrates (fabric, tile, PVC) | [60] |
| Erythrocyte Analysis | 3D Fluorescence Spectroscopy | Pattern Recognition & Classification | Improved precision for hematological diagnostics | Detection of biochemical and metabolic alterations | [52] |
| Metabolite Quantitation | NMR Spectroscopy | N/A (Data for AI training) | Identification of 67 blood metabolites | High reproducibility and quantitative accuracy | [61] |
Beyond accuracy, the integration of AI and ML is driving significant improvements in analytical speed and efficiency. Trends for 2025 indicate a strong movement towards real-time data processing, which is critical for clinical decision-making [59]. Furthermore, cloud-based analysis solutions are enhancing scalability and collaboration, allowing research teams to manage and process large spectral datasets more effectively than ever before [59]. The adoption of these technologies is not merely incremental; it represents a paradigm shift in how spectral data is utilized for diagnostic purposes.
Detailed Experimental Protocols
Protocol for AI-Enhanced Fluorescence Spectroscopy of Erythrocytes
This protocol details the methodology for employing fluorescence spectroscopy combined with AI-based analysis to diagnose pathological changes in erythrocytes. The procedure is adapted from current research practices aimed at enhancing the precision of hematological diagnostics [52].
I. Sample Preparation
- Blood Collection: Collect whole blood samples via venipuncture into anticoagulant tubes (e.g., EDTA).
- Sample Dilution: Dilute the whole blood in a buffered saline solution (e.g., phosphate-buffered saline) to achieve an appropriate concentration for spectroscopic analysis, typically a 1:100 to 1:1000 dilution.
- Sample Loading: Place a small volume (e.g., 50-100 µL) of the diluted sample into a quartz cuvette with a 1 cm path length. Ensure the cuvette is clean and free of contaminants.
II. Instrumentation and Data Acquisition
- Spectrometer Setup: Utilize a fluorescence spectrometer (e.g., StellarNet BlackComet) equipped with deuterium, halogen, and UV excitation sources [52].
- System Calibration: Perform a calibration of the spectrometer using known emission line standards to ensure wavelength accuracy and intensity response.
- 3D Fluorescence Scanning: Acquire fluorescence excitation-emission matrices (EEMs). Scan excitation wavelengths from 250 nm to 600 nm and record emission spectra across a range that captures the key fluorescence peaks of erythrocyte components (e.g., 300 nm to 750 nm).
- Data Export: Export the raw 3D spectral data (intensity as a function of excitation and emission wavelength) for pre-processing.
III. AI/ML Data Processing and Analysis
- Data Pre-processing:
- Savitzky-Golay Filtering: Apply Savitzky-Golay smoothing to the raw spectra to reduce high-frequency noise while preserving the spectral line shapes [60].
- Scaling: Normalize the spectral data to a unit vector or standard normal variate (SNV) to minimize the effects of scattering and path length differences.
- Feature Engineering:
- Stokes Shift Calculation: Compute the Stokes shift (Δλ = λemission - λabsorption) for key peaks, which provides information on the molecular environment [52].
- Integrated Intensity: Calculate the total integrated fluorescence intensity (I_total = ∫I(λ)dλ) across specific spectral regions of interest [52].
- Peak Identification: Extract parameters such as peak wavelengths, intensities, and ratios between peaks.
- Model Training and Classification:
- Dataset Construction: Assemble a labeled dataset where each sample's spectral features are linked to a clinical diagnosis (e.g., healthy, anemic, sickle cell).
- Algorithm Selection: Train a machine learning classifier, such as a Support Vector Machine (SVM) or an Artificial Neural Network (ANN), on the extracted features [60] [59].
- Model Validation: Validate the model's performance using a separate, blinded test set, reporting metrics such as accuracy, sensitivity, and specificity.
Protocol for Hyperspectral Imaging (HSI) of Blood Stains for Forensic Diagnostics
This protocol describes a non-destructive method for identifying blood stains against confounding substances using HSI and AI, a method with transferable value to clinical sample handling [60].
I. Sample Preparation on Substrates
- Substrate Selection: Prepare samples on relevant substrates such as white cotton fabric, white tile, and PVC wall sheets to simulate diverse surfaces.
- Sample Deposition: Deposit blood samples (from different donors) and control non-blood substances (e.g., ketchup, acrylic paint, nail polish, fake blood, red ink) onto the substrates.
- Aging: Image the samples over a period of up to three days to include spectral data from dehydrated (aged) samples.
II. HSI System Setup and Image Acquisition
- Imaging System: Use a line-scanning HSI system (e.g., Specim FX-10 camera) covering the visible and near-infrared range (397–1000 nm) [60].
- Reference Capture: Acquire dark reference images (by closing the shutter) and white reference images (using a standard white tile) for radiometric correction.
- Hypercube Acquisition: Scan each sample to capture a hypercube, a data cube with two spatial dimensions (x, y) and one spectral dimension (λ). Each hypercube in the cited study had dimensions of 1000 × 512 × 224 (spatial x, spatial y, spectral bands) [60].
III. Data Processing and AI-Driven Identification
- Pre-processing:
- Radiometric Correction: Convert raw digital numbers to reflectance values using the dark and white reference images.
- Savitzky-Golay Derivative: Apply a Savitzky-Golay derivative filter to the reflectance spectra to enhance subtle spectral features, particularly the weak absorption bands of heme components in the 500-700 nm range [60].
- Feature Selection: Identify the most important wavelengths (spectral bands) that contribute to differentiating blood from non-blood substances based on the derivative spectra.
- Model Training for Classification:
- Pixel-Level Classification: Use the selected spectral bands to train a classifier, such as a Support Vector Machine (SVM) or Artificial Neural Network (ANN), to classify each pixel in the hypercube as "blood" or "non-blood" [60].
- Validation: Perform a blind validation test using samples from a new donor and new non-blood substances to evaluate the generalizability and accuracy of the model.
Workflow and Signaling Pathway Diagrams
AI-Enhanced Spectral Analysis Workflow
The following diagram illustrates the end-to-end workflow for an AI-enhanced spectral analysis pipeline, from sample preparation to diagnostic insight.
AI Spectral Analysis Workflow
Data Processing and Model Training Logic
This diagram outlines the logical flow of data through the AI model training and validation phase, which is critical for developing a robust diagnostic tool.
AI Model Training Logic
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of AI-driven spectral analysis relies on a foundation of precise experimental techniques and high-quality materials. The following table catalogs key reagents, instruments, and software solutions essential for research in this field.
Table 2: Essential Research Reagents and Solutions for Blood Spectroscopy
| Item Name | Function/Application | Specific Example / Note |
|---|---|---|
| StellarNet BlackComet Spectrometer | Fluorescence spectra acquisition in the UV-Vis range. Ideal for examining erythrocyte samples in liquid media [52]. | Equipped with CCD detector; uses deuterium, halogen, and UV light sources. |
| Specim FX-10 Hyperspectral Camera | Capturing HSI hypercubes in the 397-1000 nm range for non-destructive bloodstain identification [60]. | Line scanner; requires dark and white reference for calibration. |
| High-Field NMR Spectrometer | Quantitative identification and validation of blood metabolites in serum/plasma [61]. | e.g., Bruker Avance III 800 MHz with cryogenically cooled probe. |
| Methanol (Precipitation Grade) | Protein precipitation from serum/plasma to reduce macromolecular interference for clearer metabolite detection in NMR [61]. | Superior performance for metabolite recovery compared to acetonitrile. |
| Deuterium Oxide (Dâ‚‚O) | Solvent for NMR spectroscopy to provide a stable lock signal and avoid overwhelming the Hâ‚‚O signal [61]. | Used in preparing phosphate buffer for NMR samples. |
| Phosphate Buffer | Provides a stable pH environment for spectral analysis, crucial for reproducible results in both fluorescence and NMR spectroscopy [52] [61]. | Often prepared in Dâ‚‚O for NMR applications. |
| AI/ML Analysis Software (Python/R) | Provides open-source libraries (e.g., Scikit-learn, TensorFlow) for developing custom spectral classification and analysis models [59]. | Offers flexibility and customization for specialized analytical needs. |
| Cloud Computing Platform (AWS, Azure) | Provides scalable computational resources for processing large hyperspectral cubes and training complex AI models [59]. | Enables high-performance computing and collaboration. |
| 3'-Deoxycytidine sulphate | 3'-Deoxycytidine sulphate, CAS:75489-87-1, MF:C9H13N3O7S, MW:307.28 g/mol | Chemical Reagent |
| Barium disalicylate | Barium Disalicylate|(C7H5O3)2Ba|5908-78-1 |
Overcoming Technical Hurdles and Enhancing Analytical Performance
Addressing Signal Reproducibility and Substrate Standardization in SERS
Surface-enhanced Raman scattering (SERS) possesses exceptional attributes for medical diagnostics, including single-molecule sensitivity, molecular specificity, and the ability to function in complex biological matrices like blood [62] [63]. However, its transition from a research technique to a reliable clinical tool is critically dependent on overcoming longstanding challenges in signal reproducibility and substrate standardization [64] [65]. The inherent variability of SERS signals, influenced by subtle differences in substrate morphology, analyte-substrate interaction, and measurement conditions, has severely hindered the inter-laboratory comparability of results and the technique's adoption in routine analysis [64] [66]. For diagnostic applications based on blood spectroscopy, where detecting low-abundance biomarkers with high precision is paramount, addressing these issues is not merely an optimization step but a fundamental requirement [62]. This Application Note details standardized protocols and analytical practices designed to achieve reproducible and quantitative SERS measurements, specifically framed within the context of biomedical diagnostics.
Key Factors Influencing SERS Reproducibility
The reproducibility of a SERS measurement is governed by a complex interplay of factors related to the substrate, the analyte, and the instrumental setup. Understanding and controlling these variables is the first step toward standardization.
- Substrate Homogeneity: The spatial distribution of electromagnetic "hot spots" – nanoscale gaps and sharp features where field enhancement is maximal – must be uniform across the substrate and from batch to batch [65] [67]. Inconsistent "hot spot" density is a primary source of signal variance [67].
- Analyte-Substrate Interaction: The affinity of the target molecule for the metal surface and its orientation upon adsorption directly influence the observed SERS intensity. Molecules that do not reliably reach the enhancing surface will yield weak and variable signals [64] [66].
- Instrumental Stability: Variations in laser power, focus, and alignment can introduce significant measurement error, necessitating robust instrument calibration and standardized measurement protocols [64] [65].
The following workflow diagram illustrates the logical relationship between these key challenges and the corresponding strategies to mitigate them, leading toward reliable diagnostics.
SERS Standardization Strategy Flowchart
Standardized Substrate Platforms
The choice and fabrication of the SERS-active substrate are the most critical determinants of reproducibility. The following substrates have demonstrated high performance and can be synthesized with good batch-to-batch consistency.
Core-Shell Nanostructures (SiOâ‚‚@Ag NPs)
Silver-embedded silica nanoparticles represent a class of substrates where a dielectric core (SiOâ‚‚) is used as a template to create a dense, uniform shell of metal nanoparticles (Ag). This configuration generates numerous interparticle gaps ("hot spots") in a highly controlled manner [68].
Synthesis Protocol for SiOâ‚‚@Ag NPs (Adapted from [68]):
Synthesis of Silica Cores (~145 nm):
- Add 1.6 mL of Tetraethyl orthosilicate (TEOS) and 3 mL of aqueous ammonium hydroxide (NH₄OH, 25–28%) to 40 mL of absolute ethanol.
- Stir the mixture vigorously for 20 hours at 25°C.
- Centrifuge the resulting SiOâ‚‚ nanoparticle suspension at 8500 rpm for 15 minutes. Wash the pellet with ethanol and re-disperse in ethanol to a final concentration of 50 mg/mL.
Surface Functionalization (Thiolation):
- Add 200 µL of (3-mercaptopropyl)trimethoxysilane (MPTS) and 40 µL of NH₄OH to 200 mg of the SiO₂ nanoparticle suspension.
- Stir vigorously for 12 hours at 25°C to form thiolated SiO₂ NPs (SiO₂-SH).
- Centrifuge and wash several times with ethanol to remove excess reagents.
Deposition of Silver Nanoparticles (~17 nm):
- Completely dissolve 5 mg of polyvinylpyrrolidone (PVP, Mw ~40,000) and 26 mg of silver nitrate (AgNO₃) in separate 25 mL volumes of ethylene glycol (EG).
- To the PVP/EG solution, add 30 mg of SiO₂-SH NPs, the AgNO₃/EG solution, and 41.4 µL of octylamine.
- Stir the suspension for 30 minutes.
- Centrifuge and wash thoroughly with ethanol to remove unattached Ag NPs. The final SiO₂@Ag NPs are dispersed in ethanol and stored at 25°C.
Metallic Glassy Nanowire Arrays (MGNWAs)
For solid substrates, metallic glassy nanowire arrays fabricated by die nanoimprinting offer exceptional uniformity and air stability [67].
Fabrication Protocol for Pd-based MGNWAs [67]:
- Template Preparation: Use a commercially available anodic aluminum oxide (AAO) template with defined pore dimensions (e.g., 55 nm diameter, 100 nm pitch).
- Thermoplastic Forming:
- Assemble a polished Pdâ‚„â‚€.â‚…Niâ‚„â‚€.â‚…Pâ‚₉ metallic glass specimen against the AAO template in a steel die mould.
- Heat the mould to 633 K (within the supercooled liquid region of the alloy) and hold for 1 minute.
- Apply a pressure of 354 MPa for 3-5 minutes to force the metallic glass into the nanopores.
- Release: Dissolve the AAO template in a KOH solution to release the freestanding metallic glassy nanowire array.
Quantitative Comparison of Substrate Performance
The following table summarizes key performance metrics for the described substrates, providing a basis for selection based on analytical requirements.
Table 1: Performance Comparison of Reproducible SERS Substrates
| Substrate Type | Enhancement Factor (EF) | Reproducibility (RSD of Signal) | Key Advantages | Ideal Diagnostic Use Case |
|---|---|---|---|---|
| SiOâ‚‚@Ag NPs [68] | Not specified | 2.33% - 5.95% | High uniformity, solution-based, good for bio-functionalization | Detection of small molecules (e.g., toxins, drugs) in serum |
| Metallic Glassy Nanowire Array [67] | 1.1 × 10ⵠ| 9.60% (across 121 points) | Excellent spatial reproducibility, air-stable, robust | Solid-phase immunoassay for protein biomarkers |
| Aggregated Ag/Au Colloids [66] | Varies | Requires internal standard | Easily accessible, robust performance | Exploratory research, proof-of-concept studies |
Experimental Protocol: Quantitative SERS Immunoassay for Biomarker Detection
This protocol outlines a sandwich immunoassay for the detection of a low-abundance protein biomarker (e.g., Hepatitis B surface antigen) in human blood plasma, utilizing a SERS-based microfluidic platform for high sensitivity [62].
Materials and Reagent Setup
Table 2: Research Reagent Solutions for SERS Immunoassay
| Reagent / Material | Function / Description | Supplier Example / Notes |
|---|---|---|
| Capture Antibody | Binds target antigen to solid support | Monoclonal antibody specific to target biomarker |
| SERS Tag | Detection probe; Au/Ag NP functionalized with Raman reporter and detection antibody | Au Nanostars labeled with 4,4'-thiobisbenzenethiol (TBBT) |
| Blocking Buffer | Prevents non-specific binding | 1-3% Bovine Serum Albumin (BSA) in PBS |
| Washing Buffer | Removes unbound reagents | Phosphate Buffered Saline (PBS) with 0.05% Tween-20 |
| Microfluidic Chip | Platform for automated, controlled assay execution | Glass or PDMS chip with immobilized capture antibodies |
Step-by-Step Workflow
The following diagram visualizes the key steps of the SERS immunoassay protocol.
SERS Immunoassay Workflow
Procedure:
- Substrate Preparation: Functionalize the surface of a microfluidic channel (e.g., GaN substrate) with the capture antibody using EDC/NHS coupling chemistry [62].
- Blocking: Introduce a blocking buffer (e.g., 1% BSA) into the channel and incubate for 1 hour at 25°C to passivate the surface against non-specific adsorption. Rinse with washing buffer.
- Sample Incubation: Inject the processed human blood plasma sample (potentially containing the target antigen) into the microfluidic channel. Allow it to incubate for 1 hour to facilitate the formation of the antigen-capture antibody complex. Rinse thoroughly.
- SERS Tag Incubation: Introduce the SERS tags (e.g., Raman reporter-labeled gold nanoflowers conjugated with the detection antibody) into the channel. Incubate for 1 hour to form the complete "sandwich" immuno-complex. Perform a final rigorous wash to eliminate any unbound SERS tags.
- SERS Measurement & Quantification:
- Focus the laser of a Raman spectrometer (e.g., 532 nm excitation) onto the microfluidic channel.
- Acquire SERS spectra using standardized parameters: 8.0 mW laser power, 16 s exposure time [68].
- Plot the intensity of the characteristic Raman peak (e.g., 1178 cmâ»Â¹ for basic fuchsin [62]) against the antigen concentration to generate a calibration curve. The limit of detection (LOD) for this method can be as low as 0.01 IU/mL for HBsAg [62].
Data Analysis and Quantitation Practices
Reliable quantitation requires strategies to mitigate the inherent variance in SERS measurements.
- Internal Standardization: The most effective method for achieving precise quantification is to use an internal standard (IS) [66]. This involves adding a known quantity of a stable, Raman-active molecule (e.g., deuterated benzoic acid, 4-mercaptobenzoic acid) that co-adsorbs with the analyte. The SERS signal of the analyte is then normalized to the signal of the IS, canceling out variations due to laser power fluctuations, substrate density, and focusing differences.
- Calibration Curve Model: SERS calibration curves are typically non-linear due to the finite number of adsorption sites on the substrate, following a Langmuir-type isotherm [66]. For quantitation, a limited, approximately linear range of the curve should be used as the working quantitation range.
- Analytical Figures of Merit:
- Precision: Report as the Relative Standard Deviation (RSD) of the recovered concentration, not just the signal intensity [66].
- Limit of Detection (LOD): LOD can be calculated as 3σ/slope, where σ is the standard deviation of the blank measurement.
- Enhancement Factor (EF): Calculate EF using established formulas [64]: EF = (ISERS / NSERS) / (IRS / NRS), where I is signal intensity and N is the number of molecules probed. Use probe molecules with high surface affinity (e.g., aromatic thiols) for consistent EF estimation [64].
The path to mainstream adoption of SERS in clinical diagnostics is contingent on resolving the challenges of reproducibility and standardization. By employing engineered substrates like SiOâ‚‚@Ag core-shell nanoparticles or metallic glassy nanowire arrays, adhering to rigorous experimental protocols such as the SERS immunoassay, and implementing robust data analysis practices centered on internal standardization, researchers can generate reliable, quantitative, and clinically actionable data. These protocols provide a foundational framework for advancing SERS-based blood spectroscopy research toward fulfilling its promise as a rapid, sensitive, and multiplexed diagnostic technology.
Mitigating Complex Matrix Effects and Biomolecular Interference
Matrix effects and biomolecular interference represent significant challenges in the analytical sciences, particularly in the field of medical diagnostics based on blood spectroscopy. These effects occur when components within a complex biological sample, such as blood, alter the analytical signal of the target analyte, leading to suppressed or enhanced signals that compromise quantitative accuracy [69] [70]. In liquid chromatography-mass spectrometry (LC-MS), for instance, matrix effects can cause ion suppression or enhancement when co-eluting compounds interfere with the ionization process [70] [71]. Similar challenges manifest in spectroscopic techniques like Raman spectroscopy, where fluorescence from biological molecules or interference from substrates can obscure the target signal [72] [73]. The multifaceted nature of matrix effects, influenced by factors including target analyte characteristics, sample composition, preparation protocols, and instrumental parameters, necessitates a pragmatic and integrated approach to mitigation [69]. This document outlines standardized protocols and application notes for detecting, quantifying, and mitigating these effects, with a specific focus on blood-based diagnostic applications.
The table below summarizes the primary challenges posed by matrix effects and the corresponding mitigation strategies explored in this document.
Table 1: Matrix Effect Challenges and Corresponding Mitigation Strategies
| Challenge | Impact on Analysis | Mitigation Strategy | Key References |
|---|---|---|---|
| Ion Suppression/Enhancement (LC-MS) | Reduced accuracy, sensitivity, and reproducibility in quantitative analysis. | Use of stable isotope-labeled internal standards (SIL-IS); optimized chromatographic separation; advanced sample preparation (e.g., SPE). | [70] [71] |
| Fluorescence Interference (Raman Spectroscopy) | Obscures weak Raman scattering signals, compromising molecular fingerprinting. | Dual-wavelength Raman methods; mathematical modeling; physical suppression techniques. | [73] |
| Substrate Interference | Strong background signal from substrates masks the signal from target biological fluids. | Computational spectral analysis (MCRAD, RSC); use of minimally interacting substrates (e.g., aluminum foil). | [72] |
| Sample Complexity | Co-elution of interfering compounds from biological matrices like blood plasma. | Cleaner sample preparation (QuEChERS, Solid Phase Extraction); dilution methods where sensitivity allows. | [69] [74] [71] |
Protocol 1: Mitigating Ion Suppression in LC-MS for Blood Drug Monitoring
Background and Principle
Liquid chromatography-mass spectrometry is a cornerstone technique for drug monitoring in blood. A primary challenge is ion suppression caused by co-eluting matrix components, such as phospholipids, which can impair detection sensitivity and quantitative accuracy [70] [71]. This protocol utilizes a stable isotope-labeled internal standard (SIL-IS), which is the most well-recognized technique for correcting matrix effects, as the SIL-IS experiences nearly identical suppression as the target analyte, allowing for accurate correction [70] [71].
Materials and Reagents
Table 2: Research Reagent Solutions for LC-MS Drug Monitoring
| Item | Function | Specification / Notes |
|---|---|---|
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Corrects for variability in sample preparation and ionization efficiency; compensates for matrix effects. | Isotopically labeled version of the target analyte (e.g., Deuterium, Carbon-13). |
| Formic Acid | Mobile-phase additive to improve chromatographic separation and ionization efficiency. | LC-MS grade, purity ≥99%. |
| Acetonitrile & Methanol | Organic solvents for protein precipitation and mobile-phase composition. | LC-MS grade. |
| Solid Phase Extraction (SPE) Cartridges | Selectively retains target analytes and removes phospholipids and other interfering matrix components. | Various phases (e.g., C18) depending on analyte chemistry. |
Step-by-Step Procedure
Sample Preparation (Protein Precipitation & SPE):
- Add a known amount of SIL-IS to 100 µL of blood plasma or serum at the beginning of the sample preparation process.
- Precipitate proteins by adding 300 µL of ice-cold acetonitrile, vortex for 1 minute, and centrifuge at 14,000 × g for 10 minutes.
- For further cleanup, load the supernatant onto a pre-conditioned SPE cartridge. Wash with an appropriate solvent to remove impurities, and elute the analyte and SIL-IS with a strong elution solvent.
- Evaporate the eluent to dryness under a gentle stream of nitrogen and reconstitute in the initial mobile phase for LC-MS analysis [70] [71].
Chromatographic Separation:
- Utilize a UPLC or HPLC system with a suitable reverse-phase column (e.g., C18, 2.1 x 100 mm, 1.7 µm).
- Optimize the gradient elution program to achieve baseline separation of the target analyte from known interfering compounds and the solvent front. A typical gradient might run from 10% to 90% organic solvent over 5-10 minutes.
- Maintain a column temperature of 40°C and a flow rate of 0.3 mL/min [70].
Mass Spectrometric Detection & Data Analysis:
- Use an electrospray ionization (ESI) source in positive or negative mode, as appropriate for the analyte.
- Optimize source parameters (temperature, gas flows, voltages) for maximum signal stability.
- Operate the mass spectrometer in Multiple Reaction Monitoring (MRM) mode for high specificity.
- Construct a calibration curve by plotting the peak area ratio (analyte / SIL-IS) against the nominal concentration of the calibrators. The response of the SIL-IS will correct for any ion suppression, enabling accurate quantification of the target drug [70].
Protocol 2: Overcoming Fluorescence in Raman Spectroscopy for Blood-Based Diagnostics
Background and Principle
Raman spectroscopy provides a molecular "fingerprint" ideal for identifying pathological changes in blood and tissues. However, its application in biomedicine is often limited by strong fluorescence background from biological molecules, which can swamp the inherently weak Raman signal [73]. This protocol details a dual-wavelength Raman method that computationally eliminates fluorescence interference, enabling high-quality spectral acquisition for cancer diagnosis [73].
Materials and Reagents
Table 3: Research Reagent Solutions for Dual-Wavelength Raman Spectroscopy
| Item | Function | Specification / Notes |
|---|---|---|
| Dual-Wavelength Raman Spectrometer | Excites the sample with two different laser wavelengths to enable fluorescence subtraction. | Equipped with 532 nm and 633 nm lasers. |
| Aluminum Foil Substrate | A minimally interfering substrate for mounting blood stains or tissue samples. | Provides a low, consistent background signal. |
| Reference Standards | For instrument calibration and validation of spectral accuracy. | e.g., Silicon wafer for peak calibration. |
Step-by-Step Procedure
Sample Mounting:
- For blood stain analysis, deposit a small volume (e.g., 10 µL) of whole blood on an aluminum foil substrate and allow it to dry under ambient conditions [72].
- For tissue analysis, mount thin sections of esophageal or other relevant tissue on a low-fluorescence glass slide or aluminum foil.
Spectral Acquisition:
- Focus the Raman spectrometer on the region of interest.
- Acquire the first Raman spectrum (Sâ‚) using the 532 nm laser. Record the integration time and laser power.
- Without moving the sample, acquire the second Raman spectrum (Sâ‚‚) from the identical spatial spot using the 633 nm laser. Maintain identical integration times for both measurements [73].
Computational Fluorescence Elimination:
- Perform a two-step normalization calibration on the two spectra.
- Subtract the normalized Sâ‚‚ spectrum from the normalized Sâ‚ spectrum. This process effectively cancels out the fluorescence component, which is dependent on the excitation wavelength, while preserving the Raman signal, which is relative to the laser wavelength [73].
- The resulting differential spectrum is a high-fidelity Raman profile, free from fluorescence background, suitable for detailed molecular analysis.
Protocol 3: Computational Subtraction of Substrate Interference in Blood Trace Detection
Background and Principle
Detecting trace amounts of blood on forensically relevant substrates (e.g., fabrics) using Raman spectroscopy is complicated by the substrate's strong Raman scattering. This protocol employs two computational approaches—Multivariate Curve Resolution combined with the Additions Method (MCRAD) and Reducing Spectrum Complexity (RSC)—to extract the blood signal without prior knowledge of the substrate's spectral properties [72].
Materials and Reagents
- Raman Spectrometer with mapping stage.
- Common Substrates: White cotton, polyester fabric, denim.
- Reference Blood Spectrum: Acquired from a blood stain on a non-interfering substrate like aluminum foil [72].
Step-by-Step Procedure
Reference and Sample Acquisition:
- Prepare a standard blood stain on aluminum foil and acquire its reference Raman spectrum (S_ref).
- Acquire multiple Raman spectra from different spots on the blood stain deposited on the interfering substrate (e.g., denim). This set of experimental spectra is labeled S_org [72].
Method A: Reducing Spectrum Complexity (RSC):
- This method is based on the principle that subtracting the true blood spectrum from the mixed spectrum will minimize the spectral complexity (i.e., smoothness) of the residual.
- The algorithm varies the concentration coefficient (C) in the equation: Sblank = Sorg - C × S_ref.
- It calculates the functional δf(C) = ∫ |d(S_blank)/dk| dk, which represents the total "complexity" of the residual spectrum.
- The value of C that minimizes δf(C) is taken as the correct concentration, effectively identifying the blood contribution in the mixed signal [72].
Method B: Multivariate Curve Resolution with Additions Method (MCRAD):
- This method numerically "titrates" the experimental spectrum by adding a known amount of the reference blood spectrum.
- The known spectrum of the target component (blood) is added to the experimental data set, and a bilinear model (MCR) is applied to resolve the mixture.
- The known concentration change allows the model to uniquely separate the blood signal from the unknown substrate signal, even without a pure spectrum of the substrate [72].
The mitigation of matrix effects and biomolecular interference is not a one-size-fits-all endeavor but requires a strategic, integrated approach that spans sample preparation, instrumental analysis, and computational data processing. As demonstrated, techniques such as the use of SIL-IS in LC-MS, dual-wavelength excitation in Raman spectroscopy, and advanced chemometric algorithms are powerful tools for safeguarding analytical integrity. The continued advancement of these protocols, particularly through the integration of artificial intelligence and machine learning for spectral analysis [7] [27], promises to further enhance the accuracy, sensitivity, and reliability of blood-based diagnostic methods, ultimately paving the way for more precise and personalized medical interventions.
Blood plasma analysis represents a cornerstone of modern clinical diagnostics and therapeutic monitoring. The sample preparation methodology, specifically the choice between analyzing plasma in its native liquid state ('wet') or as a dried residue ('dry'), fundamentally influences the analytical outcome and diagnostic validity. Within the context of medical diagnostic applications of blood spectroscopy research, this decision carries significant implications for assay sensitivity, reproducibility, and translational potential. The spectral profiles obtained via vibrational spectroscopy techniques, including Raman and Fourier Transform Infrared (FTIR) spectroscopy, are highly susceptible to variations in sample preparation protocols. As research increasingly focuses on detecting subtle spectral changes associated with pathological states, optimizing sample processing becomes paramount. This application note provides a detailed comparison of wet and dry plasma analysis methodologies, supported by experimental data and standardized protocols, to guide researchers in selecting and implementing the most appropriate approach for their specific diagnostic applications.
Technical Comparison: Wet vs. Dry Plasma Analysis
The choice between wet and dry plasma analysis involves fundamental trade-offs between analytical simplicity and spectral information content. Dry plasma analysis, typically involving the deposition of a small volume of plasma onto a suitable substrate followed by evaporation, concentrates analytes and eliminates the strong water background that can dominate infrared spectra. This concentration effect enhances signals from low-abundance constituents and has made dried plasma the traditional choice for Attenuated Total Reflection (ATR)-FTIR spectroscopy [75] [40]. Conversely, wet plasma analysis examines plasma in its native state, preserving the natural physiological environment of biomolecules and enabling potentially more accurate quantification of metabolites and proteins without crystallization artifacts that can affect dried samples. Recent research indicates that Raman spectroscopy demonstrates superior performance for wet plasma analysis due to its relative insensitivity to water interference compared to infrared techniques [75].
Table 1: Analytical Performance Comparison Between Wet and Dry Plasma Analysis
| Parameter | Wet Plasma Analysis | Dry Plasma Analysis |
|---|---|---|
| Sample Volume | Typically 50-200 µL [76] | As little as 5-10 µL (dried blood spots) [77] |
| Water Interference | Significant in FTIR, minimal in Raman [75] | Eliminated through evaporation |
| Diagnostic Accuracy (Example) | 82% (Raman) for endometrial cancer [40] | 83% (ATR-FTIR) for endometrial cancer [40] |
| Combined Diagnostic Power | 86% accuracy when combined with dry analysis [40] | Complementary to wet analysis approaches [40] |
| Throughput Potential | Faster results possible with minimal preparation [40] | Requires drying time (hours) [40] |
| Molecular Environment | Native aqueous state [75] | Concentrated, potentially crystallized |
Experimental Protocols
Plasma Collection and Preparation
Proper plasma collection is fundamental to both analytical approaches and requires strict adherence to standardized protocols to ensure sample integrity.
Collection Tube Selection: Draw whole blood into commercially available anticoagulant-treated tubes. For most applications, EDTA-treated tubes (lavender tops) are recommended. Citrate-treated (light blue tops) or heparinized tubes (green tops) are alternatives, though heparin can be contaminated with endotoxin, which may stimulate white blood cells to release cytokines [78].
Plasma Separation: Centrifuge collected blood at 1,000-2,000 × g for 10 minutes in a refrigerated centrifuge. For platelet-poor plasma, extend centrifugation to 15 minutes at 2,000 × g. Immediately following centrifugation, carefully transfer the supernatant (plasma) into a clean polypropylene tube using a Pasteur pipette, maintaining samples at 2-8°C throughout handling [79] [78].
Aliquoting and Storage: If analysis is not immediate, aliquot plasma into 0.5 mL portions in cryogenic vials. Store and transport aliquots at -20°C or lower. Minimize freeze-thaw cycles as they are detrimental to many plasma components. Visually inspect samples and note any that are hemolyzed, icteric, or lipemic, as these can invalidate certain tests [78].
Wet Plasma Analysis Protocol
This protocol is optimized for Raman spectroscopic analysis of liquid plasma, capitalizing on its advantages for aqueous samples [75] [40].
Sample Thawing: Thaw frozen plasma aliquots slowly on ice or in a refrigerator at 4°C. Once thawed, gently mix by inverting the tube 3-5 times. Avoid vortex mixing to prevent protein denaturation.
Debris Removal: Transfer 100-150 µL of plasma to a microcentrifuge tube. Centrifuge at 14,000 × g for 10 minutes at 4°C to remove any remaining particulate matter.
Spectroscopic Analysis:
- Transfer the clarified supernatant to a quartz cuvette with an appropriate path length (typically 1 mm).
- Acquire Raman spectra using a 785 nm laser to minimize fluorescence background.
- Employ an integration time of 30-60 seconds with 3-5 accumulations to ensure adequate signal-to-noise ratio.
- Maintain sample temperature at 25°C using a temperature-controlled stage throughout measurement.
Data Processing:
- Subtract water spectrum and correct for background fluorescence using polynomial fitting.
- Apply vector normalization to account for minor concentration variations.
Dry Plasma Analysis Protocol
This protocol details the preparation of dried plasma films for ATR-FTIR spectroscopy, the preferred technique for solid samples [40].
Sample Preparation: Follow the same thawing and clarification steps as in the wet plasma protocol (steps 1-2 above).
Film Deposition:
- Pipette a precise volume (typically 5-10 µL) of clarified plasma onto the ATR crystal (diamond or zinc selenide) or an optically inert substrate (e.g., glass slide) for transmission measurements.
- Allow the sample to dry at room temperature in a desiccator to prevent water absorption. Drying typically requires 2-3 hours.
- For highly reproducible films, control ambient temperature (20±1°C) and humidity (<30% RH) during drying.
Spectroscopic Analysis:
- Acquire FTIR spectra in ATR mode with a resolution of 4 cmâ»Â¹.
- Collect 64-128 co-scans to ensure adequate signal-to-noise.
- Apply consistent pressure to the sample using the ATR pressure arm to ensure reproducible contact with the crystal.
Data Processing:
- Apply atmospheric correction to remove COâ‚‚ and water vapor contributions.
- Perform vector normalization on the Amide I region (1700-1600 cmâ»Â¹) or entire spectrum (1800-900 cmâ»Â¹).
- Employ second derivative spectroscopy to enhance spectral resolution for overlapping bands.
Diagram 1: Plasma analysis workflow: wet vs. dry methods
Method Selection Guidelines
Choosing between wet and dry plasma analysis depends on multiple factors related to analytical goals and practical constraints.
Analytical Technique: For Raman spectroscopy, wet plasma analysis is generally preferred as it preserves the native biochemical environment and avoids crystallization artifacts [75]. For FTIR spectroscopy, dry plasma analysis typically provides superior results due to the elimination of strong water absorption [40].
Sample Availability: When sample volume is limited (pediatric studies, small animal models), dry plasma analysis offers advantages as it requires smaller volumes (5-10 µL) and enables analysis from dried blood spots [77].
Throughput Requirements: Wet plasma analysis provides faster results with minimal preparation time, making it suitable for high-throughput clinical settings where rapid analysis is prioritized [40].
Diagnostic Performance: For maximum diagnostic accuracy, consider a combined approach utilizing both methods. Recent research on endometrial cancer detection demonstrated that combining wet (Raman) and dry (ATR-FTIR) analyses achieved 86% accuracy, outperforming either method alone (82% and 83%, respectively) [40].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of plasma analysis protocols requires specific laboratory materials and reagents. The following table details essential components for both wet and dry plasma analysis workflows.
Table 2: Essential Research Reagents and Materials for Plasma Analysis
| Item | Function/Application | Specifications/Notes |
|---|---|---|
| EDTA Blood Collection Tubes (Lavender Top) | Anticoagulant for plasma preparation | Preferred over heparin for minimizing cytokine release [78] |
| Refrigerated Centrifuge | Plasma separation | Maintains 2-8°C during processing; capable of 1,000-2,000 × g [79] |
| Quartz Cuvettes | Wet plasma analysis for Raman spectroscopy | Low fluorescence; path length 1 mm [75] |
| ATR Crystals (Diamond/ZnSe) | Dry plasma analysis for FTIR spectroscopy | Diamond preferred for durability; ZnSe for broader spectral range [40] |
| Protein Precipitation Reagents | Sample cleanup for metabolomics | Acetonitrile (2:1 v/v with plasma) provides optimal feature extraction [76] |
| Cryogenic Vials | Sample storage | Polypropylene; maintains integrity at -80°C [78] |
| Solid Phase Extraction Cartridges | Sample cleanup and fractionation | HybridSPE-Phospholipid effective for phospholipid removal [77] [76] |
The optimization of sample processing methodologies represents a critical component in the advancement of blood-based diagnostic applications. Both wet and dry plasma analysis approaches offer distinct advantages that can be strategically leveraged based on specific research objectives, analytical techniques, and practical constraints. Wet plasma analysis using Raman spectroscopy provides superior performance for quantitative analysis in the native aqueous environment, while dry plasma analysis with ATR-FTIR spectroscopy offers enhanced sensitivity for specific diagnostic applications. The emerging evidence that these approaches provide complementary diagnostic information suggests that a combined methodology may offer the most powerful approach for complex diagnostic challenges. As spectroscopic techniques continue to evolve toward clinical implementation, standardized protocols for both wet and dry plasma analysis will be essential for ensuring reproducibility and translational success across research laboratories and clinical settings.
Advanced Computational Models for Data Processing and Noise Reduction
The medical diagnostic applications of blood spectroscopy are rapidly evolving, driven by advanced computational models for data processing and noise reduction. These models are crucial for transforming raw, complex spectral data into reliable, clinically actionable information. The integration of machine learning (ML) and deep learning (DL) techniques has enabled researchers to overcome traditional limitations associated with physiological noise, instrument artifacts, and environmental variability, thereby enhancing the accuracy of non-invasive blood-based diagnostics [28] [80] [7]. This document outlines specific computational protocols and applications, providing researchers and drug development professionals with practical tools for implementing these advanced methods.
The following table summarizes the prominent computational models recently applied to blood spectroscopy data, highlighting their specific functions and performance metrics.
Table 1: Key Computational Models for Blood Spectroscopy Data
| Computational Model | Primary Function | Spectroscopy Type | Reported Performance / Advantage |
|---|---|---|---|
| DCS-NET (Deep Learning) [28] | Blood Flow Index (BFi) estimation | Diffuse Correlation Spectroscopy (DCS) | ~17,000x faster analysis speed; 8.35% error in relative BFi; robust to noise. |
| Independent Component Analysis (ICA) [81] | Noise reduction in hemodynamic response | Functional Near-Infrared Spectroscopy (fNIRS) | Improved t-value of hemodynamic response from 20 to 40 on average. |
| Adaptive Pulse-Coupled Neural Network (AD-PCNN) [82] | Noise and speckle reduction in spectrograms | Doppler Ultrasound Blood Flow | Reduced RRMS error of maximum frequency by 25.2% on average. |
| Support Vector Machine (SVM) & Principal Component Analysis (PCA) [80] | Classification of pathological vs. healthy blood cells | FTIR Spectroscopy | Most common methods for distinction and dimensionality reduction. |
| Gradient Boosting Multi-Output Regression [83] | Estimation of blood biomarkers (HDL, LDL, HGB) | Near-Infrared (NIR) Absorbance Spectra | Achieved R² scores: HDL: 0.827, LDL: 0.795, HGB: 0.873. |
| Raman Spectroscopy with ML Classifier [7] | Non-invasive detection of infection (COVID-19) | Raman Spectroscopy | Achieved specificity of 0.837 at a sensitivity of 0.80 (AUROC: 0.896). |
Detailed Experimental Protocols
Protocol 1: Rapid Blood Flow Estimation Using DCS-NET
This protocol details the use of a deep learning model to replace traditional fitting algorithms for quantifying the Blood Flow Index (BFi) in Diffuse Correlation Spectroscopy [28].
1. Hardware and Data Acquisition:
- Utilize a DCS instrument with a laser source and single-photon detectors.
- Collect measured intensity autocorrelation functions (ACFs) at multiple source-detector distances (e.g., 5, 10, 15, 20, 25, and 30 mm).
- Note: The multi-distance approach increases sensitivity to deeper tissues and improves model robustness.
2. Data Preprocessing and Simulation for Training:
- Training Data Generation: Simulate a large dataset of ACFs and corresponding ground-truth BFi values using a three-layer computational brain model (representing scalp, skull, and brain tissues).
- Parameter Variation: Incorporate physiologically relevant variations in optical properties (absorption coefficient μa and reduced scattering coefficient μs') and layer thicknesses during simulation to ensure model generalizability.
- Noise Introduction: Add realistic noise levels to the simulated ACFs to train a model with excellent anti-noise capabilities.
3. Model Implementation and Training:
- Architecture: Implement a one-dimensional convolutional neural network (1D-CNN) architecture, termed DCS-NET, designed to process the temporal ACF data.
- Input: Simulated ACFs.
- Output: Estimated BFi and coherent factor (β).
- Training: Train the network using the simulated dataset with a standard supervised learning approach, such as minimizing the mean squared error between predicted and true BFi.
4. Validation and Deployment:
- Validate the trained DCS-NET model on a hold-out set of experimental or simulated data.
- Deploy the model for real-time analysis. The input is the measured ACF, and the output is the directly estimated BFi, bypassing the need for computationally intensive nonlinear fitting.
Figure 1: DCS-NET Workflow for Blood Flow Analysis.
Protocol 2: Noise Reduction in fNIRS Signals Using Independent Component Analysis
This protocol describes a method for denoising functional Near-Infrared Spectroscopy (fNIRS) signals to isolate the hemodynamic response related to neuronal activity [81].
1. Signal Acquisition:
- Conduct fNIRS measurements while administering a controlled block-based or event-related paradigm (e.g., arithmetic tasks) to volunteer subjects.
- Record the raw intensity data and convert it to concentration changes of oxy-hemoglobin (HbO) and deoxy-hemoglobin (HbR) using the modified Beer-Lambert law.
2. Data Preprocessing:
- Apply a low-pass filter to the HbO and HbR signals to remove high-frequency noise (e.g., instrument noise).
- Optional: Down-sample the data to a uniform sampling rate if necessary.
3. Independent Component Analysis (ICA):
- Concatenate the preprocessed HbO and HbR signals from all channels and subjects to form a single input matrix for ICA.
- Perform ICA decomposition on this matrix to separate it into statistically independent components (ICs). Each IC represents a source signal that contributed to the measured data.
4. Component Identification and Signal Reconstruction:
- Identify Noise Components: Visually inspect the time-course and spatial map of each IC to identify components corresponding to physiological noise (e.g., cardiac pulsation, respiration), motion artifacts, or other interferences.
- Reconstruct Hemodynamic Response: Create a denoised signal by reconstructing the data using only the ICs that represent the task-related hemodynamic response. This is typically done by setting the weighting coefficients of noise-related ICs to zero and projecting the remaining components back to the sensor space.
- Validation: Compare the t-value or signal-to-noise ratio (SNR) of the reconstructed hemodynamic response with the original, low-pass filtered signal to quantify improvement.
Protocol 3: Non-Invasive Blood Biomarker Estimation via NIR Spectroscopy and Machine Learning
This protocol outlines a multi-output regression pipeline for estimating key blood biomarkers from NIR absorbance spectra, offering a non-invasive alternative to traditional blood tests [83].
1. Data Collection and Preprocessing:
- Collect NIR absorbance spectra from blood samples or non-invasively via a transcutaneous probe.
- Obtain ground-truth values for target biomarkers (e.g., HDL, LDL, Hemoglobin) using standard laboratory assays (e.g., enzymatic methods for cholesterol, complete blood count for HGB).
- Preprocess the spectral data: perform smoothing, correct for baseline drift, and normalize the spectra to account for path-length and scattering effects.
2. Dimensionality Reduction:
- Apply Principal Component Analysis (PCA) to the preprocessed spectral data.
- Use the principal components (PCs) that capture the majority of the variance in the data as new features for the regression model. This step reduces multicollinearity and computational cost.
3. Model Training and Validation:
- Algorithm: Employ a multi-output gradient boosting regression model (e.g., XGBoost).
- Training: Train the model using the PCs as input features and the multiple biomarker levels as simultaneous regression targets.
- Validation: Use k-fold cross-validation (e.g., 5-fold) to assess model performance.
- Metrics: Calculate R² score, Mean Absolute Error (MAE), and Root Mean Square Error (RMSE) independently for each target biomarker.
Table 2: Key Research Reagent Solutions for Spectroscopy Protocols
| Item / Solution | Function in Protocol | Application Context |
|---|---|---|
| Greiner VACUETTE Blood Collection Tubes (with EDTA) [84] | Anticoagulant preservation of whole blood samples. | Securing stable human and non-human blood samples for spectral analysis. |
| Simulated Three-Layer Phantom (Scalp, Skull, Brain) [28] | Generating ground-truth data for training computational models. | Training and validating deep learning models for DCS data analysis. |
| Dexcom Sensor / Accu-Chek Device [7] | Providing reference ground-truth measurements for biomarkers. | Validating non-invasive glucose and metabolite estimations. |
| Standardized Enzyme Assays & CBC Analysis [83] | Providing reference ground-truth measurements for biomarkers (HDL, LDL, HGB). | Training and validating multi-output regression models for NIR spectra. |
Figure 2: Machine Learning Pipeline for Biomarker Estimation.
Navigating Regulatory Pathways and Clinical Implementation Barriers
Table 1: Performance Metrics of Spectroscopic Blood Diagnostics
| Disease Target | Technology Platform | Key Performance Metrics | Reference Standard |
|---|---|---|---|
| Multiple Cancers (8 types) | FTIR Spectroscopy | Pooled Sensitivity: 57% (Stage I, 99% specificity); Up to 99% (Stage I, 59% specificity) | Histopathology [85] |
| COVID-19 | Raman Spectroscopy & ML | Sensitivity: 0.80; Specificity: 0.837 (Cross-validation) | Nasal PCR [7] |
| Blood Glucose | Raman Spectroscopy & ML | Area Under Precision-Recall Curve (AUPR): 0.58 (Cross-validation) | Dexcom Sensor & Accu-Chek [7] |
| Cardiovascular Drugs | SERS & AI (Molecular Hook) | Detection Limit: 10 pg/mL (Dobutamine); 10 ng/mL (Milrinone) | Liquid Chromatography/Mass Spectrometry [27] |
The integration of vibrational spectroscopy and machine learning represents a paradigm shift in clinical diagnostics, offering a rapid, non-invasive, and often reagent-free platform for disease detection [7] [85]. These technologies analyze the full molecular signature of a blood sample, capturing a pan-omic profile inclusive of tumor, immune, and metabolic-derived markers [85]. However, the path from a promising proof-of-concept study to widespread clinical adoption is fraught with challenges, including evolving regulatory requirements, the need for demonstrable clinical utility, and overcoming implementation barriers in complex healthcare settings [86]. This application note provides a detailed overview of the experimental protocols, performance data, and strategic considerations for navigating the translational pathway for spectroscopic blood diagnostics.
Experimental Protocols for Spectroscopic Liquid Biopsies
Protocol: Serum-Based Cancer Detection via ATR-FTIR Spectroscopy
This protocol outlines the procedure for using Attenuated Total Reflectance Fourier Transform Infrared (ATR-FTIR) spectroscopy to detect multiple cancer types from blood serum, as demonstrated in a large-scale study of 2092 patients [85].
Sample Preparation
- Collection: Collect whole blood samples from patients using standard venipuncture techniques into serum separator tubes.
- Processing: Allow blood to clot for 30 minutes at room temperature, then centrifuge at 1500-2000 RCF for 10 minutes. Carefully aliquot the supernatant serum.
- Storage: Store serum samples at -80°C until analysis. Avoid multiple freeze-thaw cycles.
- Analysis: Thaw samples slowly on ice. For spectroscopic measurement, deposit 2-3 µL of serum directly onto the ATR crystal [85].
Instrumentation and Data Acquisition
- Instrument: Use an FTIR spectrometer equipped with an ATR accessory (e.g., diamond crystal).
- Acquisition Parameters:
- Spectral Range: 4000 - 400 cmâ»Â¹
- Resolution: 4 cmâ»Â¹
- Number of Scans: 64 scans per spectrum (to achieve a high signal-to-noise ratio)
- Replicates: Acquire nine technical replicates per patient sample to account for instrumental and sample heterogeneity [85].
- Background: Collect a background spectrum of the clean ATR crystal before each sample measurement.
Data Pre-processing and Machine Learning
- Pre-processing: Apply standard spectroscopic pre-processing to the raw spectra:
- Atmospheric correction (for water vapor and COâ‚‚)
- Vector normalization
- Derivative spectroscopy (e.g., Savitzky-Golay second derivative) to enhance spectral features and remove baseline effects [85].
- Model Training: Employ a nested cross-validation (CV) strategy to prevent data leakage and overfitting.
- Outer CV: Split patient data randomly into 70% training and 30% test sets, repeated 51 times.
- Inner CV: Use 5-fold CV on the training set to tune model hyperparameters.
- Classification: The final diagnosis for a patient is determined by a consensus prediction (maximum vote) from all nine spectra [85].
- Pre-processing: Apply standard spectroscopic pre-processing to the raw spectra:
Protocol: Non-Specimen COVID-19 Detection via Transcutaneous Raman Spectroscopy
This protocol describes a novel, no-specimen approach for detecting COVID-19 by scanning a patient's finger with Raman spectroscopy, mimicking a pulse oximeter's interface [7].
Patient Interface and Data Acquisition
- Hardware: A custom-built finger scanner using an 830 nm laser as the excitation source.
- Procedure: The patient places their finger into the pulse oximeter-like device. The laser is directed onto the fingertip skin, and the resulting Raman-scattered light is collected by a spectrograph and detected with a CCD camera [7].
- Safety: Laser power must comply with safe exposure limits for human skin.
Spectral Processing and Machine Learning Classification
- Data Input: The raw Raman spectra from the finger scan serve as the input for the machine learning model.
- Modeling Approach: Frame the problem as a binary classification task (COVID-19 positive vs. negative).
- Validation: In a study of 455 patients, a five-fold cross-validation analysis was performed. The model was also tested with a temporally split dataset (training on data before July 2022, testing on data after) to evaluate performance against viral variants, which revealed a domain shift challenge (AUROC dropped to 0.67) [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Spectroscopic Blood Diagnostics
| Item | Function / Rationale |
|---|---|
| Serum Separator Tubes | Standard for clinical blood collection; enables clean serum harvest for FTIR and other serum-based assays [85]. |
| ATR-FTIR Spectrometer | Core instrumentation for serum analysis; requires minimal sample prep and provides rapid, reproducible results [85]. |
| Raman Spectrometer (830 nm) | Enables transcutaneous, no-specimen measurements; near-IR laser minimizes fluorescence and is safe for in-vivo use [7]. |
| Silver Nanoparticles (Functionalized) | Critical for Surface-Enhanced Raman Spectroscopy (SERS); functionalized with 'molecular hooks' (e.g., A13) to selectively capture and enhance signal from target analytes like drugs [27]. |
| Machine Learning Algorithms | Software tools for spectral analysis and diagnostic classification; allows test to be adapted by re-training algorithm for new diseases [7] [85]. |
Navigating Regulatory and Implementation Hurdles
Successfully translating a diagnostic platform requires a strategic approach to regulatory approval and a proactive plan to overcome barriers to clinical adoption.
Strategic Regulatory Pathways
Engaging with regulatory bodies early is critical. Several designations can expedite development and review:
- Breakthrough Device Designation (FDA): For devices that provide more effective treatment or diagnosis of life-threatening diseases.
- Regenerative Medicine Advanced Therapy (RMAT) Designation (FDA): As demonstrated by Nanoscope's MCO-010, this designation can be applicable for novel platforms, offering intensive FDA guidance and potential accelerated approval [87].
- Orphan Drug/Device Designation (FDA & EMA): For diagnostics targeting rare conditions, this provides incentives like protocol assistance and market exclusivity [87].
Overcoming Implementation Barriers
The Consolidated Framework for Implementation Research (CFIR) provides a useful taxonomy for identifying barriers. Key barriers and mitigation strategies, aligned with the Expert Recommendations for Implementing Change (ERIC), include [86]:
Barrier: Access to Knowledge and Information
- Strategy: Develop comprehensive educational materials for clinicians and staff. Identify and prepare champions within the clinical setting to promote the technology [86].
Barrier: Knowledge and Beliefs about the Intervention
- Strategy: Conduct local consensus processes to engage stakeholders and address skepticism. Share local data and outcomes from early pilots to build credibility [86].
Barrier: Tension for Change (Lack of Perceived Need)
- Strategy: Organize implementation clinician teams to take ownership. Use audit and feedback to demonstrate the new test's impact on clinical outcomes and efficiency [86].
Clinical Validation, Performance Metrics, and Technique Comparison
Clinical Trial Outcomes and Performance Validation Frameworks
The validation of clinical trial outcomes is a cornerstone in the translation of biomedical research into clinically actionable diagnostic tools. This is particularly true in the field of blood-based diagnostics, where robust validation frameworks ensure that new tests are reliable, accurate, and fit for purpose. With the recent advent of disease-modifying therapies for conditions like Alzheimer's disease, the imperative for validated diagnostic tests to identify eligible patients has never been greater [88]. This document details application notes and experimental protocols for validating clinical trial outcomes, with a specific focus on the analytical and clinical validation of blood spectroscopy and mass spectrometry-based assays within medical diagnostic applications. The frameworks described herein are designed to meet stringent regulatory standards and provide researchers, scientists, and drug development professionals with a clear roadmap for test development and validation.
Experimental Protocols
Protocol 1: Mass Spectrometry-Based Blood Biomarker Assay for Brain Amyloidosis
This protocol describes the methodology for developing and clinically validating a blood test to identify the presence of brain amyloid, a key pathological feature of Alzheimer's disease, as exemplified by the PrecivityAD2 test [88].
1. Principle: High-throughput mass spectrometry (MS) is used to measure specific protein biomarkers in blood. An algorithm then combines these biomarker values to produce a score that predicts the presence of a pathological feature, such as brain amyloidosis, as determined by an established reference standard like amyloid positron emission tomography (PET).
2. Specimen Collection and Processing:
- Specimen Type: Blood collected in EDTA tubes.
- Processing: Centrifuge blood samples to isolate plasma. Aliquot plasma and store at -80°C until analysis. Avoid multiple freeze-thaw cycles.
3. Reagents and Materials:
- Internal Standards: Stable isotope-labeled peptides for amyloid-beta (Aβ) 40, Aβ42, and tau peptide (e.g., p-tau217).
- Immunoaffinity Enrichment: Anti-Aβ and anti-tau antibodies coupled to magnetic beads.
- Digestion Enzymes: Sequencing-grade trypsin.
- Mass Spectrometry: Liquid chromatography (LC) system coupled to a high-resolution tandem mass spectrometer (e.g., LC-MS/MS).
- Calibrators and Quality Controls: Purified Aβ40, Aβ42, and p-tau217 peptides in a matrix that mimics plasma.
4. Experimental Procedure: a. Immunoaffinity Enrichment: Thaw plasma samples. Add internal standards. Incubate with antibody-coupled magnetic beads to capture target analytes (Aβ40, Aβ42, and p-tau217). Wash beads to remove non-specifically bound proteins. b. Digestion: Elute captured proteins from beads. Add trypsin to digest proteins into peptides. Desalt peptides. c. Mass Spectrometric Analysis: Inject digested peptides onto the LC-MS/MS system. Separate peptides using a reverse-phase C18 column. Analyze eluting peptides using a scheduled multiple reaction monitoring (MRM) or parallel reaction monitoring (PRM) method. d. Data Analysis: Integrate chromatographic peaks for the target peptides and their corresponding internal standards. Calculate the ratio of the analyte peak area to the internal standard peak area for quantification.
5. Algorithm Development and Scoring:
- Key Biomarkers: The primary analytes are the Aβ42/40 ratio and the percentage of p-tau217 (%p-tau217) relative to the total tau peptide.
- Model Training: Use a training cohort of samples with paired amyloid PET status to develop a classification algorithm (e.g., logistic regression, machine learning). The algorithm outputs an Amyloid Probability Score (APS2).
- Performance Metrics: The model's performance is evaluated using the area under the receiver operating characteristic curve (AUC-ROC). For the PrecivityAD2 test, the APS2 achieved an AUC-ROC of 0.94 [88].
Protocol 2: NMR-Based Metabolomic Analysis of Blood Specimens
This protocol outlines the use of nuclear magnetic resonance (NMR) spectroscopy for the quantitative analysis of metabolites in blood serum, plasma, and whole blood, suitable for metabolomic profiling in clinical trials [89].
1. Principle: Proton NMR (1H NMR) spectroscopy detects hydrogen atoms in molecular structures, providing a highly reproducible and quantitative fingerprint of the metabolome in a biofluid. The protocol involves protein removal to improve spectral quality.
2. Specimen Preparation:
- Protein Precipitation: Add a cold mixture of methanol and chloroform to the blood sample (serum, plasma, or whole blood). Vortex mix and centrifuge to pellet proteins.
- Recovery of Supernatant: Carefully collect the supernatant containing the metabolites.
- Drying and Reconstitution: Evaporate the solvent under a stream of nitrogen gas and reconstitute the metabolite pellet in a deuterated buffer (e.g., D2O) containing a known concentration of a chemical shift reference (e.g., TSP, trimethylsilylpropanoic acid).
3. Reagents and Materials:
- Solvents: HPLC-grade methanol and chloroform.
- NMR Buffer: Deuterium oxide (D2O) with phosphate buffer and TSP (for chemical shift referencing and quantification).
- NMR Tubes: High-quality, matched NMR tubes.
- Instrumentation: High-field NMR spectrometer (e.g., 600 MHz or higher).
4. Experimental Procedure:
a. Data Acquisition: Insert the prepared sample into the NMR spectrometer. Maintain the sample temperature at a constant level (e.g., 298 K).
b. 1D 1H NMR Experiment: Acquire a one-dimensional proton NMR spectrum using a standard pulse sequence with water suppression (e.g., NOESYPRESAT or CPMG to suppress broad protein signals).
c. Spectral Processing: Process the raw data: apply Fourier transformation, phase correction, baseline correction, and calibrate the chemical shift scale to TSP at 0.0 ppm.
5. Data Analysis and Quantification:
- Spectral Deconvolution: Use software tools to identify and quantify metabolites by fitting spectral profiles to a database of reference compound spectra.
- Absolute Quantification: Calculate the concentration of metabolites by comparing the integral of a target metabolite's peak to the integral of the known concentration of the reference compound (TSP). This method can enable the absolute quantitation of nearly 70 metabolites in serum/plasma and nearly 80 in whole blood [89].
Validation Framework and Data Presentation
A rigorous, multi-level validation framework is essential to demonstrate that a diagnostic test is analytically sound and clinically useful.
Analytical and Clinical Performance Metrics
The following table summarizes key quantitative outcomes from the clinical validation of the PrecivityAD2 test, providing a benchmark for performance [88].
Table 1: Clinical Validation Performance of a Blood-Based Biomarker Test for Brain Amyloidosis
| Performance Metric | Value | Interpretation and Context |
|---|---|---|
| Area Under the Curve (AUC-ROC) | 0.94 | The overall ability of the test to discriminate between amyloid PET positive and negative individuals is excellent. |
| Agreement with Amyloid PET | 88% | The percentage of cases where the blood test result matched the amyloid PET status. |
| Cohort Size (n) | 583 | Number of individuals with suspected Alzheimer's disease in the validation study. |
| Amyloid PET Positivity Prevalence | 53% | The proportion of the study cohort that was positive for brain amyloid by PET (Centiloid > 25). |
Regulatory and Reporting Guidelines
Adherence to established reporting guidelines is a critical component of the validation framework, ensuring transparency and reproducibility.
- FDA Guidelines on Data Visualization: Recent FDA guidelines emphasize standardized formats for tables and figures in clinical trial submissions to enhance clarity, consistency, and the interpretation of safety and efficacy data by regulators [90].
- EQUATOR Network: Serves as a central repository for research reporting guidelines, such as STARD for diagnostic accuracy studies and CONSORT for randomized trials, which should be followed where applicable [91].
- Principles for Effective Figures: Figures should notably improve the reader's understanding, give an immediate visual impression, and be aesthetically clean and uncluttered. Key numerical estimates should not be reported solely in figures but also in the text or accompanying tables [92].
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and their functions for the methodologies described in this document.
Table 2: Essential Research Reagents and Materials for Blood-Based Assay Development
| Item | Function / Application |
|---|---|
| Stable Isotope-Labeled Peptides | Serve as internal standards in mass spectrometry for precise and accurate quantification of target proteins/peptides, correcting for sample preparation losses and ion suppression [88]. |
| Immunoaffinity Magnetic Beads | Used for the selective enrichment of low-abundance protein biomarkers (e.g., Aβ, tau) from complex biological fluids like plasma or serum prior to MS analysis, greatly improving assay sensitivity [88]. |
| Deuterated NMR Solvents (e.g., D2O) | Used in NMR spectroscopy to provide a signal lock for the spectrometer and to avoid a large interfering signal from water protons in the spectral region of interest [89]. |
| Chemical Shift Reference (e.g., TSP) | Provides a known reference peak (0.0 ppm) for calibrating the chemical shift axis in NMR spectra and can serve as a quantitative internal standard for metabolite concentration determination [89]. |
| Methanol-Chloroform Mixture | A standard solvent system for precipitating proteins from blood samples (serum, plasma, whole blood) for metabolomic analysis, leading to highly resolved NMR spectra [89]. |
Workflow and Pathway Visualizations
Blood Biomarker Validation Workflow
The following diagram outlines the logical workflow for the development and validation of a blood-based biomarker test, from specimen collection to clinical application.
Clinical Validation Analysis Pathway
This diagram illustrates the key analytical steps and decision points in the clinical validation phase of a diagnostic test.
In the field of medical diagnostics, particularly in blood-based research, the selection of analytical methodology profoundly impacts the quality, reliability, and applicability of generated data. This application note provides a detailed comparative analysis of three cornerstone analytical families: spectroscopy techniques (including fluorescence and Raman), liquid chromatography-tandem mass spectrometry (LC-MS/MS), and traditional clinical assays. Framed within the context of a broader thesis on medical diagnostic applications of blood spectroscopy research, this document provides structured quantitative data, detailed experimental protocols, and visual workflows to guide researchers, scientists, and drug development professionals in selecting and implementing the most appropriate analytical strategy for their specific needs. The comparison focuses on key parameters including sensitivity, specificity, analytical throughput, and applicability in blood-based biomarker discovery and validation.
The following table summarizes the core characteristics, advantages, and limitations of each analytical approach for blood-based diagnostic applications.
Table 1: Comparative Analysis of Diagnostic Techniques for Blood-Based Applications
| Parameter | Spectroscopy (Fluorescence/Raman) | LC-MS/MS | Traditional Assays (e.g., ELISA, Clinical Chemistry) |
|---|---|---|---|
| Principle | Measurement of light interaction with matter (emission, scattering) [52] [93] | Physical separation (LC) coupled with mass analysis and fragmentation (MS/MS) [94] [95] | Biochemical reactions (e.g., antibody-antigen binding, enzyme activity) |
| Primary Applications in Blood Diagnostics | Erythrocyte analysis, hemoglobin oxygenation status, metabolic alterations [52]; Detection of biochemical changes in serum/plasma [93] | Targeted and untargeted metabolomics, lipidomics, proteomics; pharmacokinetic studies [95] [96] | Measurement of specific proteins (e.g., cytokines), hormones, clinical chemistry panels (e.g., liver enzymes) |
| Sensitivity | High for fluorescent compounds; can detect subtle physiological variations [52] | Extremely high (detection at picogram-femtogram levels) [95] | High for immunoassays (e.g., pg/mL for ELISA); moderate for clinical chemistry |
| Specificity | Moderate (based on spectral fingerprints) [52] [93] | Very High (separation by retention time, mass, and fragmentation pattern) [94] [97] | High for immunoassays; variable for other assays |
| Sample Throughput | Rapid (minutes per sample for direct measurements) [52] | Moderate (analysis time longer due to chromatography) [95] | High (amenable to full automation and 96/384-well formats) |
| Multiplexing Capability | Intrinsic for multiple analytes with overlapping spectra (requires deconvolution) | High in targeted (MRM) and untargeted (HRMS) modes [95] [96] | Low per assay (typically single-analyte); multiplex ELISA panels available |
| Sample Volume & Preparation | Low volume; minimal preparation (often direct measurement of blood/erythrocytes) [52] | Low volume; requires extensive preparation (e.g., protein precipitation, extraction) [98] | Variable; can be low for automated immunoassays |
| Key Advantage | Non-invasive, rapid, provides information on biochemical environment and cell status [52] | Unparalleled specificity and ability to analyze a vast range of molecules without prior knowledge [95] [96] | Rugged, standardized, widely available in clinical settings |
| Primary Limitation | Limited molecular identification capability without reference standards | High cost, complex operation, requires skilled personnel [97] | Targeted nature limits discovery potential; antibody cross-reactivity |
Detailed Experimental Protocols
Protocol A: 3D Fluorescence Spectroscopy for Erythrocyte Analysis
This protocol is designed to analyze the biochemical and metabolic status of erythrocytes in whole blood or purified samples, based on methodologies detailed in fluorescence spectroscopy research [52].
1. Sample Preparation:
- Blood Collection: Collect venous blood into anticoagulant tubes (e.g., EDTA or heparin).
- Erythrocyte Isolation: Centrifuge blood at 1,500 x g for 10 minutes. Carefully remove plasma and buffy coat. Wash the erythrocyte pellet three times with isotonic phosphate-buffered saline (PBS), pH 7.4.
- Suspension: Resuspend the purified erythrocytes in PBS to a final hematocrit of approximately 5%.
2. Instrumentation and Setup:
- Spectrometer: Utilize a fluorescence spectrometer equipped with a deuterium, halogen, and ultraviolet excitation sources, such as the StellarNet BlackComet [52].
- Cuvette: Place the sample in a quartz cuvette with a 1 cm path length.
- Temperature Control: Maintain the sample holder at 37°C using a thermostatted cuvette holder.
- Calibration: Perform standard calibration procedures using known emission lines prior to analysis [52].
3. Data Acquisition (3D Fluorescence Mapping):
- Set the emission wavelength range from 250 nm to 700 nm.
- Set the excitation wavelength range from 240 nm to 550 nm, with increments of 5-10 nm.
- For each excitation wavelength, collect the full emission spectrum.
- The instrument software will compile the data into a 3D matrix (Excitation-Emission Matrix, EEM), plotting fluorescence intensity as a function of both excitation and emission wavelengths.
4. Data Analysis:
- Identify distinct spectral peaks corresponding to key biomarkers such as hemoglobin (e.g., excitation ~410 nm, emission ~630 nm), deoxyhemoglobin, and plasma components [52].
- Calculate quantitative characteristics:
- Fluorescence Intensity (
I):I = Φ · I₀ · C · ϵ, whereΦis quantum yield,I₀is excitation intensity,Cis concentration, andϵis absorption coefficient [52]. - Stokes Shift:
Δλ = λ_emission - λ_absorption[52]. - Total Integrated Fluorescence Intensity:
I_total = ∫ I(λ) dλacross the emission spectrum [52].
- Fluorescence Intensity (
Protocol B: LC-MS/MS for Targeted Metabolite Quantification in Plasma
This protocol describes a validated method for quantifying specific metabolites or small molecule biomarkers in human plasma, reflecting standard practices in clinical and pharmaceutical research [95] [96] [98].
1. Sample Preparation (Protein Precipitation):
- Aliquot: Transfer 50 µL of plasma into a microcentrifuge tube.
- Precipitate: Add 150 µL of ice-cold acetonitrile containing internal standards (e.g., isotope-labeled analogs of the target analytes).
- Vortex and Centrifuge: Vortex mix vigorously for 1 minute and centrifuge at 14,000 x g for 10 minutes at 4°C.
- Collect Supernatant: Carefully transfer the supernatant to a clean LC-MS vial for analysis.
2. Liquid Chromatography (LC) Conditions:
- Column: UHPLC C18 column (e.g., 2.1 x 100 mm, 1.7 µm particle size).
- Mobile Phase A: Water with 0.1% formic acid.
- Mobile Phase B: Acetonitrile with 0.1% formic acid.
- Gradient:
- 0-1 min: 2% B
- 1-8 min: 2% B to 95% B
- 8-10 min: Hold at 95% B
- 10-11 min: 95% B to 2% B
- 11-15 min: Re-equilibrate at 2% B
- Flow Rate: 0.4 mL/min.
- Column Oven: 40°C.
- Injection Volume: 5 µL.
3. Mass Spectrometry (MS) Conditions:
- Ionization: Electrospray Ionization (ESI), positive/negative mode switching based on analyte [97].
- Source Parameters: Capillary voltage, source temperature, and desolvation gas flow are optimized for the specific instrument (e.g., Thermo Scientific TSQ Endura or similar) [99].
- Data Acquisition: Multiple Reaction Monitoring (MRM).
- For each analyte and internal standard, define the precursor ion (Q1) and the most abundant product ion (Q3).
- Optimize collision energy for each transition.
4. Data Analysis:
- Integrate peak areas for each analyte and its corresponding internal standard.
- Generate a calibration curve using spiked matrix standards and calculate the analyte concentration in unknown samples using the ratio of analyte-to-internal standard peak area.
Essential Research Reagent Solutions
Successful implementation of the described protocols requires specific, high-quality materials. The following table lists key reagent solutions and their functions.
Table 2: Essential Research Reagents and Materials
| Item | Function / Application | Example / Specification |
|---|---|---|
| Anticoagulant Blood Collection Tubes | Prevents coagulation for plasma and erythrocyte analysis [52]. | Kâ‚‚EDTA or Lithium Heparin tubes. |
| Isotonic Phosphate-Buffered Saline (PBS) | Washing and resuspending erythrocytes without inducing osmotic stress [52]. | 1X, pH 7.4, sterile filtered. |
| Stable Isotope-Labeled Internal Standards | Normalizes for variability in sample preparation and ionization efficiency in LC-MS/MS, enabling accurate quantification [96]. | ¹³C or ²H-labeled analogs of target analytes. |
| LC-MS Grade Solvents | Minimizes background noise and ion suppression, ensuring high sensitivity and reproducible chromatography [97] [98]. | Acetonitrile and Methanol (≥99.9% purity), Water (18.2 MΩ·cm). |
| Volatile Buffers & Additives | Enables efficient droplet formation and solvent evaporation in ESI; non-volatile buffers can cause instrument contamination [97]. | Formic Acid, Ammonium Formate, Ammonium Acetate (0.01-0.1%). |
| UHPLC Chromatography Columns | High-efficiency separation of complex biological samples prior to MS detection [95] [98]. | C18, 50-100 mm length, sub-2 µm particle size. |
| Fluorescence Reference Standards | Calibration of spectrometer wavelength and response [52]. | Solutions of known fluorescent compounds (e.g., Quinine sulfate). |
The choice between spectroscopy, LC-MS/MS, and traditional assays is not a matter of superiority but of strategic alignment with research objectives. Fluorescence spectroscopy offers a rapid, non-invasive window into cellular and metabolic status, ideal for initial diagnostic screening and monitoring physiological changes. In contrast, LC-MS/MS provides an unparalleled tool for definitive identification and precise quantification of specific biomarkers, making it indispensable for hypothesis-driven research in metabolomics and pharmacokinetics. Traditional assays remain the workhorse for high-throughput, routine clinical measurements. An integrated approach, leveraging the strengths of each technology, will provide the most comprehensive and robust framework for advancing blood-based medical diagnostics, ultimately contributing to more personalized and effective therapeutic strategies.
Vibrational spectroscopy, encompassing both Raman and Infrared (IR) techniques, has emerged as a powerful tool in the field of medical diagnostics, particularly for cancer detection. These label-free, rapid, and minimally invasive methods probe the molecular vibrations within a sample, providing a comprehensive "biochemical fingerprint" of its composition [100]. For researchers and drug development professionals, understanding the comparative advantages, limitations, and performance of these techniques is crucial for selecting the appropriate methodology for specific cancer diagnostic applications. This application note provides a detailed benchmark of Raman and IR spectroscopy, focusing on their application in cancer detection via blood-based liquid biopsies, and includes standardized protocols to facilitate implementation in research settings.
Technical Comparison: Raman vs. IR Spectroscopy
The fundamental principles of Raman and IR spectroscopy are distinct, leading to different technical considerations for biological sampling.
Fundamental Principles and Selection Rules
- IR Spectroscopy: IR spectroscopy is based on the absorption of infrared light by molecules. A molecular vibration is IR-active if it results in a change in the dipole moment of the molecule. Fourier-transform infrared (FTIR) spectroscopy, particularly when coupled with an attenuated total reflection (ATR) module, is commonly used for analyzing biofluids [101] [100].
- Raman Spectroscopy: Raman spectroscopy relies on the inelastic scattering of monochromatic light, usually from a laser. A vibration is Raman-active if it induces a change in the polarizability of the electron cloud around a molecule [102] [103].
Table 1: Fundamental Comparison of Raman and IR Spectroscopy.
| Parameter | Raman Spectroscopy | IR (ATR-FTIR) Spectroscopy |
|---|---|---|
| Physical Principle | Inelastic Light Scattering | Light Absorption |
| Selection Rule | Change in Polarizability | Change in Dipole Moment |
| Water Compatibility | High (Weak Scatterer) | Low (Strong Absorber) |
| Fluorescence Interference | High (Can obscure signal) | Low (IR does not induce fluorescence) |
| Typical Sample Throughput | Moderate to High | High |
| Sensitivity to Functional Groups | Homonuclear bonds (C-C, C=C, S-S) | Polar bonds (C=O, O-H, N-H) |
Practical Advantages and Limitations for Biofluid Analysis
The different physical principles lead to direct practical implications for analyzing blood plasma or serum:
- Aqueous Samples: Raman spectroscopy holds a significant advantage for analyzing hydrated samples or aqueous solutions because water is a very weak Raman scatterer. In contrast, water absorbs IR radiation strongly, which can obscure the signal from analytes of interest. This can be partially mitigated in IR by using short path lengths or ATR crystals, which limit the penetration depth of the evanescent wave [103] [100].
- Fluorescence: Fluorescence, which can be orders of magnitude stronger than the Raman signal, is a major interference in Raman spectroscopy and can overwhelm the desired spectral data. IR spectroscopy is not susceptible to this issue, as IR radiation does not cause electronic excitation [103].
- Sensitivity and Specificity: The techniques are often considered complementary. IR is generally more sensitive for studying polar bonds and reaction intermediates. Raman is particularly sensitive to non-polar bonds and is excellent for studying crystal lattice vibrations and polymorphisms [103].
Performance Benchmarking in Cancer Detection
Recent clinical studies demonstrate the powerful application of both techniques in detecting various cancers from blood derivatives.
Quantitative Performance Metrics
The following table summarizes key performance metrics from recent studies utilizing Raman and IR spectroscopy for cancer detection.
Table 2: Benchmarking Performance in Cancer Detection from Blood Plasma/Serum.
| Cancer Type | Technique | Sample Type | Accuracy | Sensitivity/ Specificity | AUC | Citation |
|---|---|---|---|---|---|---|
| Endometrial | Raman ('wet' plasma) | Blood Plasma | 82% | - | - | [40] |
| Endometrial | ATR-FTIR ('wet' plasma) | Blood Plasma | 78% | - | - | [40] |
| Endometrial | Combined Raman & FTIR | Blood Plasma | 86% | - | - | [40] |
| Endometrial | ATR-FTIR (dry plasma) | Blood Plasma | 83% | - | - | [40] |
| Lung | FTIR (Serum) | Blood Serum | - | - | - | [104] |
| Multi-Cancer | FTIR (Serum) | Blood Serum | - | 57% Sens / 99% Spec (Stage I) | 0.76-0.91* | [85] |
| Multi-Cancer | FTIR (Serum) | Blood Serum | - | 99% Sens / 59% Spec (Stage I) | 0.76-0.91* | [85] |
Note: AUC (Area Under the receiver operating characteristic Curve) values are organ-specific, with the range given for brain, breast, colorectal, kidney, lung, ovarian, pancreatic, and prostate cancers [85]. Sensitivity (Sens) and Specificity (Spec) are reported for pooled cancer analysis. AUC values provide a aggregate measure of diagnostic performance across all classification thresholds.
Analysis of Key Findings
- Synergistic Effect: The study on endometrial cancer (EC) highlights that combining Raman and IR spectroscopy can yield higher diagnostic accuracy (86%) than either technique alone, as they provide complementary molecular information [40].
- Early-Stage Detection: A large-scale multi-cancer study demonstrated that a spectroscopic liquid biopsy (FTIR) could detect 64% of Stage I cancers at a high specificity of 99%. By tuning the algorithm, the test could identify 99% of Stage I cancers, albeit at a lower specificity (59%), showcasing the flexibility for triage or screening applications [85].
- Prognostic Potential: Research on lung cancer has established a strong correlation between infrared molecular fingerprints (IMFs) and disease progression, including tumor stage. Furthermore, IMFs provided insights into patient survival comparable to established prognostic factors like tumor stage [104].
Detailed Experimental Protocols
Protocol: ATR-FTIR Spectroscopy of Blood Plasma for Cancer Detection
This protocol is adapted from studies on endometrial and multi-cancer detection [40] [85].
1. Sample Collection and Preparation: - Collect whole blood using EDTA or heparin tubes. Centrifuge at 2,000-3,000 x g for 10-15 minutes to separate plasma. - For dry film analysis: Spot 5-10 µL of plasma onto a suitable substrate (e.g., glass slide, ATR crystal) and allow it to air-dry or under a gentle stream of nitrogen. - For 'wet' plasma analysis: Use a liquid ATR cell. Load 2-5 µL of plasma directly onto the crystal.
2. Instrumentation and Data Acquisition: - Instrument: FTIR Spectrometer with an ATR accessory (e.g., diamond crystal). - Spectral Range: 4000 - 400 cmâ»Â¹. - Resolution: 4 or 8 cmâ»Â¹. - Number of Scans: 64-128 scans per spectrum to achieve a good signal-to-noise ratio. - Environmental Control: Perform measurements in a controlled atmosphere to minimize spectral contributions from water vapor and COâ‚‚. - Replication: Acquire multiple spectra (e.g., 9 technical replicates) per patient sample from different spots.
3. Data Pre-processing: - Subtract the background spectrum. - Perform atmospheric suppression (water vapor, COâ‚‚). - Apply vector normalization or Standard Normal Variate (SNV) to minimize scattering effects. - For dry films, a baseline correction may be necessary.
4. Data Analysis and Machine Learning: - Use multivariate statistical analysis or machine learning algorithms (e.g., Principal Component Analysis (PCA), Linear Discriminant Analysis (LDA), Support Vector Machines (SVM)). - Employ a nested cross-validation strategy to train models and prevent overfitting. - Validate model performance on a held-out test set not used during training.
Diagram 1: ATR-FTIR spectroscopy experimental workflow for blood plasma analysis.
Protocol: Raman Spectroscopy of Blood Plasma for Cancer Detection
This protocol is adapted from studies on endometrial cancer and point-of-care applications [40] [7].
1. Sample Collection and Preparation: - Prepare plasma as described in Section 4.1. - For 'wet' plasma analysis: Use a quartz capillary tube or a welled slide. Load 5-20 µL of plasma. - For non-invasive detection: A finger-probe device can be used to acquire spectra transcutaneously, requiring no sample preparation [7].
2. Instrumentation and Data Acquisition: - Instrument: Raman Spectrometer (portable or benchtop). - Laser Excitation Wavelength: 785 nm or 830 nm are common to minimize fluorescence. - Laser Power: Optimize to avoid sample degradation (e.g., 50-300 mW). - Exposure Time: 1-10 seconds per accumulation. - Number of Accumulations: 10-60 to build up a spectrum with acceptable signal-to-noise. - Spectral Range: Typically, 500 - 2000 cmâ»Â¹ (fingerprint region).
3. Data Pre-processing: - Subtract background and remove cosmic rays. - Apply a filter to smooth noise (e.g., Savitzky-Golay). - Perform fluorescence background subtraction (e.g., using polynomial fitting). - Apply vector normalization.
4. Data Analysis and Machine Learning: - Similar to the IR protocol, employ machine learning algorithms (SVM, PCA-LDA) for classification. - For SERS-based assays, the analysis may focus on specific biomarker peaks and their intensities.
Diagram 2: Raman spectroscopy experimental workflow showing both plasma and non-invasive approaches.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Spectroscopy-Based Cancer Detection.
| Item | Function / Application | Example / Specification |
|---|---|---|
| EDTA/Heparin Blood Tubes | Anticoagulant for plasma separation from whole blood. | Standard venous blood collection tubes. |
| ATR Crystal | Substrate for FTIR measurement; enables minimal sample preparation. | Diamond, Zinc Selenide (ZnSe). |
| Quartz Capillaries/Cuvettes | Hold liquid samples for Raman spectroscopy with low background signal. | Suitable for UV-Vis-NIR transmission. |
| Portable Raman Spectrometer | For point-of-care or intra-operative measurements. | e.g., MIRA XTR (Metrohm) with 785 nm laser [105]. |
| FTIR Spectrometer | Core instrument for acquiring infrared absorption spectra. | Must be equipped with an ATR accessory. |
| Machine Learning Software | For development of classification models from spectral data. | Python (scikit-learn), R, MATLAB, proprietary software. |
| Surface-Enhanced Raman Scattering (SERS) Substrates | Gold or silver nanoparticles to dramatically enhance Raman signal for low-abundance biomarkers. | Colloidal nanoparticles or nanostructured chips [105]. |
Within the advancing field of medical diagnostics, blood-based biomarkers are revolutionizing disease detection and monitoring. The analytical validation of these diagnostic tools is paramount, ensuring that test results are reliable, accurate, and reproducible across different laboratories and instrumentation platforms. This document outlines the core metrics of analytical validation—sensitivity, specificity, and reproducibility—within the context of developing blood spectroscopy-based assays for clinical application. Adherence to these rigorous validation standards provides the foundation for robust diagnostic tests that can reliably inform patient management and drug development.
Core Analytical Performance Metrics
The fundamental parameters for evaluating the performance of a diagnostic assay are sensitivity and specificity. These metrics are determined through a comparison of the test results against a reference or "gold standard" method, typically summarized in a 2x2 contingency table [106].
Table 1: Core Definitions for Diagnostic Test Accuracy
| Metric | Definition | Formula |
|---|---|---|
| Sensitivity | The ability of a test to correctly identify individuals who have the disease. | True Positives / (True Positives + False Negatives) |
| Specificity | The ability of a test to correctly identify individuals who do not have the disease. | True Negatives / (True Negatives + False Positives) |
| Positive Predictive Value (PPV) | The probability that a subject with a positive test result truly has the disease. | True Positives / (True Positives + False Positives) |
| Negative Predictive Value (NPV) | The probability that a subject with a negative test result truly does not have the disease. | True Negatives / (True Negatives + False Negatives) |
A critical concept in setting a diagnostic cut-off is the inherent trade-off between sensitivity and specificity. Increasing sensitivity to avoid missing true cases (false negatives) often results in a decrease in specificity, leading to more false positives, and vice versa [106]. This relationship is analyzed using a Receiver Operating Characteristic (ROC) curve, where the Area Under the Curve (AUC) provides a measure of the test's overall discriminative power, with a value closer to 1.0 indicating higher accuracy [106].
It is crucial to distinguish between different types of "sensitivity". Analytical sensitivity refers to the lowest concentration of an analyte that an assay can reliably detect, often described by the limit of detection (LOD) [107]. In contrast, diagnostic sensitivity is a clinical performance metric that describes the test's ability to correctly identify diseased patients [107]. Functional sensitivity is the lowest analyte concentration that can be measured with a specified precision, typically defined as a coefficient of variation (CV) ≤20% [107].
Assessing Reproducibility and Real-World Performance
Reproducibility ensures that an assay delivers consistent results across anticipated variations in testing conditions, a critical factor for clinical deployment.
Table 2: Key Reproducibility Parameters and Tolerances
| Parameter | Description | Typical Acceptance Criterion |
|---|---|---|
| Precision | The closeness of agreement between independent measurement results obtained under stipulated conditions. Often measured as intra-assay and inter-assay CV. | CV ≤ 20% for biomarker assays [108] [109]. |
| Inter-laboratory Variability | The consistency of results when the same method is applied to the same samples in different laboratories. | Assessed through proficiency testing and external quality assurance programs [110] [109]. |
| Sample Stability | The robustness of the analyte under various storage conditions (e.g., freeze-thaw cycles, room temperature storage). | Established through stability studies (e.g., stability at 7 freeze/thaw cycles, 72 hours at room temperature) [108]. |
Factors affecting reproducibility include equipment calibration, reagent quality and consistency, environmental conditions (temperature, humidity), and operator training [110]. Standardization of protocols, rigorous training, and participation in external quality assurance programs are essential to mitigate this variability [110] [109].
Application Note: Validation of a Blood-Based P-tau217 Immunoassay for Alzheimer's Disease
Background and Clinical Utility
Alzheimer's disease (AD) diagnosis has been transformed by the development of blood-based biomarkers. Phosphorylated tau 217 (P-tau217) in plasma has emerged as a highly specific marker for AD pathology. This application note summarizes the analytical and clinical validation of a novel P-tau217 chemiluminescent immunoassay, demonstrating its utility as a diagnostic tool [108].
Experimental Protocol
1. Assay Principle: A sandwich chemiluminescent immunoassay was developed using the antibodies 4G10E2 and IBA493. A synthetic tau peptide was used as a calibrator, and detection was performed on the Quanterix SP-X imager [108].
2. Analytical Validation Procedures:
- Precision: 80 independent runs were performed using 23 patient-derived plasma samples with P-tau217 concentrations ranging from 0.09 U/mL to 3.35 U/mL. The coefficient of variation (CV) was calculated for each sample.
- Linearity & Analytical Measurement Range (AMR): Samples were serially diluted to verify the assay's linearity. The functional analytical sensitivity, or Lower Limit of Quantitation (LLOQ), was established at 0.08 U/mL. The final AMR was confirmed from 0.08 to 2.81 U/mL.
- Interference Testing: The assay was challenged with potential interferents, including purified tau protein (2N4R) and lipemic samples. Hemolyzed samples (>2+) were also evaluated.
- Sample Stability: Stability was assessed under various conditions, including multiple freeze-thaw cycles (up to 7 cycles) and storage at room temperature and refrigerated conditions for up to 72 hours.
- Lot-to-Lot Variation: Multiple lots of reagents were compared to ensure consistency.
3. Clinical Validation: The validated assay was applied to plasma samples from 1091 individuals screened in the TRAILBLAZER-ALZ 2 study. Florbetapir positron emission tomography (PET) was used as the reference standard to quantify brain amyloid burden [108].
Key Results and Performance
The analytical validation demonstrated robust performance:
- Precision: The assay achieved a CV of ≤20% across all 80 runs and all tested samples [108].
- Sensitivity and Specificity: When compared to amyloid PET status, the assay showed an Area Under the Curve (AUC) of 91.6% (95% CI: 0.90-0.94). The positive and negative predictive values were both >90% and >85%, respectively [108].
- Robustness: No significant interference was observed from purified tau or lipemia, and the assay demonstrated excellent sample stability and lot-to-lot consistency [108].
Figure 1: P-tau217 Immunoassay Analytical Validation Workflow
Advanced Topic: Normalization for Enhanced Assay Reproducibility
Advanced statistical normalization methods are critical for improving the reproducibility of complex assays, such as the Luminex platform. Traditional normalization techniques can oversimplify data corrections, introducing errors. A novel method has been developed that employs:
- Orthogonal Regression: Uses measured fluorescence of negative control and blank beads to correct for background fluorescence, preventing overcorrection from cross-reactivity [111].
- Generalized Additive Models (GAM): Applies GAM to standard curves to calculate a plate correction factor, effectively accounting for machine drift and reducing error [111].
- Clustering Analysis: For binary classification, clustering is used to accurately determine the cut-point between positive and negative populations based on the true data distribution, rather than arbitrary thresholds [111].
This comprehensive approach enhances the sensitivity, specificity, and reproducibility of assay data analysis by addressing key limitations of conventional normalization techniques [111].
Figure 2: Advanced Luminex Data Normalization and Classification
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Diagnostic Assay Development
| Item | Function / Application |
|---|---|
| High-Sensitivity Spectrometers (e.g., Avantes AvaSpec) | Enables precise absorbance and fluorescence measurements for protein detection and identification in biomedical spectroscopy [112]. |
| Validated Antibody Pairs | Form the basis of specific sandwich immunoassays (e.g., 4G10E2 & IBA493 for P-tau217) [108]. |
| Stable Isotope-Labeled Internal Standards | Critical for LC-MS/MS assay validation; used for normalization to correct for sample preparation variability and matrix effects [109]. |
| Synthetic Peptide Calibrators | Provide a defined and consistent standard for generating calibration curves in protein immunoassays [108]. |
| Reference Standards (Tetraspanins) | Common exosomal markers (CD9, CD63, CD81) used as quality controls in extracellular vesicle (exosome) isolation and analysis [109]. |
| Standardized Negative Control and Blank Beads | Essential for advanced background fluorescence correction in bead-based assays like Luminex [111]. |
Multi-modal Approaches and Data Fusion for Enhanced Diagnostic Accuracy
Multi-modal data fusion represents a transformative paradigm in medical diagnostics, leveraging complementary information from multiple spectroscopic and imaging techniques to achieve a comprehensive understanding of complex diseases. This approach is particularly valuable in blood-based diagnostics, where different spectroscopic modalities capture distinct molecular signatures that, when integrated, provide a more robust and accurate diagnostic picture than any single modality alone. The core principle involves combining data from various sources—such as Raman spectroscopy, Fourier-Transform Infrared (FTIR) spectroscopy, and other analytical techniques—to create enriched feature representations that enhance diagnostic precision for conditions including thyroid cancer, breast cancer, and other malignancies [113] [114]. This protocol outlines standardized methodologies for implementing these approaches in blood spectroscopy research, providing researchers with practical frameworks for experimental design, data acquisition, and computational analysis to advance precision medicine initiatives.
Quantitative Performance Comparison of Diagnostic Modalities
Table 1: Diagnostic Performance of Single vs. Multi-modal Spectroscopic Approaches
| Diagnostic Modality | Application Context | Accuracy (%) | AUC | Sensitivity/Specificity | Reference |
|---|---|---|---|---|---|
| Raman Spectroscopy (Single) | Thyroid Cancer Cervical Lymph Node Metastasis | 63.63 | 63.78 | Not Reported | [113] |
| FTIR Spectroscopy (Single) | Thyroid Cancer Cervical Lymph Node Metastasis | 95.84 | 96.00 | Not Reported | [113] |
| Raman + FTIR (Fused) | Thyroid Cancer Cervical Lymph Node Metastasis | 97.95 | 98.00 | Not Reported | [113] |
| Multi-modal Deep Learning | Breast Cancer Diagnosis & Prognosis | Varies by study | >0.85 typically | Varies by study | [114] |
| Multi-modal AI Models (Llama 3.2-90B) | Abdominal CT Diagnosis | 85.27% preference over human diagnosis | Not Reported | Not Reported | [115] |
The quantitative comparison clearly demonstrates the diagnostic advantage of multi-modal approaches over single-modality methods. In the context of thyroid cancer lymph node metastasis detection, the fusion of Raman and FTIR spectroscopic data increased diagnostic accuracy by approximately 34% compared to Raman spectroscopy alone, and by 2% compared to the better-performing FTIR single modality [113]. This performance enhancement is attributed to the complementary nature of the information captured by different spectroscopic techniques, which when properly integrated, provides a more comprehensive molecular profile of the pathological state.
Experimental Protocols for Multi-modal Blood Spectroscopy
Sample Preparation Protocol
Objective: To prepare human blood serum samples for multi-modal spectroscopic analysis while preserving molecular integrity and ensuring analytical reproducibility.
Materials Required:
- Blood collection tubes (serum separator tubes recommended)
- Centrifuge capable of 1,500-2,000 × g
- Low-protein-binding microcentrifuge tubes
- Zinc selenide (ZnSe) substrate slides for FTIR
- Aluminum-coated glass slides for Raman spectroscopy
- Freeze-dried control sera for quality control (e.g., SPINREACT normal/pathologic)
- Bidistilled water for dilution series
Procedure:
- Blood Collection and Processing: Collect venous blood using standard phlebotomy techniques. Allow samples to clot at room temperature for 30 minutes, then centrifuge at 1,500-2,000 × g for 15 minutes to separate serum.
- Aliquoting and Storage: Transfer clarified serum to low-protein-binding microcentrifuge tubes in 50-100 μL aliquots. Store at -80°C if not analyzed immediately to prevent degradation.
- Sample Dilution Series: Prepare dilutions of model serum solutions with bidistilled water at 2x, 3x, 5x, 7x, and 10x dilution factors in triplicate to create calibration curves [57].
- Substrate Preparation: Apply 50 μL of each sample to appropriate substrates:
- For FTIR: Zinc selenide substrates
- For Raman: Aluminum-coated glass slides
- Sample Drying: Dry samples in an oven at 37°C for 60 minutes to create uniform films for spectroscopic analysis [57].
- Quality Control: Include freeze-dried control sera certified for multiple parameters (e.g., SPINREACT with ~38 certified components) in each batch to validate analytical performance [57].
Spectroscopic Data Acquisition
Objective: To acquire high-quality vibrational spectroscopic data from prepared serum samples using both Raman and FTIR spectroscopy.
FTIR Spectroscopy Protocol:
- Instrument Setup: Use an FTIR spectrometer (e.g., FT-801 Fourier IR spectrometer) with the following parameters:
- Spectral range: 500-4000 cmâ»Â¹
- Resolution: 4 cmâ»Â¹
- Scan number: 32 scans per spectrum
- Background measurement: Air reference before each sample [57]
Data Collection:
- Position prepared ZnSe substrate in sample holder
- Collect triplicate spectra for each sample to assess technical variability
- Include background subtraction using air reference for each sample
Spectral Preprocessing:
- Remove COâ‚‚ vibration peaks using "straight line generation" option in instrument software
- Apply baseline correction using a simple two-point linear subtraction method
- Perform vector normalization to standardize spectral intensity [57]
Raman Spectroscopy Protocol:
- Instrument Setup: Configure Raman spectrometer with appropriate laser wavelength (typically 785 nm or 532 nm for biological samples) and the following parameters:
- Spectral resolution: 2-4 cmâ»Â¹
- Laser power: Optimize to avoid sample degradation (typically 10-100 mW)
- Integration time: 1-10 seconds per accumulation
- Accumulations: 10-30 per spectrum
Data Collection:
- Focus laser beam on sample area with uniform coverage
- Collect multiple spectra from different spots on each sample to account for heterogeneity
- Include calibration standards (e.g., silicon wafer) for frequency verification
Spectral Preprocessing:
- Remove cosmic ray spikes
- Apply fluorescence background subtraction (e.g., using polynomial fitting)
- Perform vector normalization for intensity standardization
Multi-modal Data Fusion and Analysis Protocol
Objective: To integrate spectroscopic data from multiple modalities using computational fusion strategies for enhanced diagnostic classification.
Multi-modal Separation and Cross-Fusion Network (MSCNet) Workflow
Implementation Steps:
Feature Extraction with Fully Connected Neural Network (FCNN) Encoder:
- Input: Preprocessed Raman and FTIR spectra
- Architecture: Design a FCNN with 3-5 hidden layers to extract relevant features
- Output: Unified dimension feature space (e.g., 256-512 features per modality)
- Implementation: Use ReLU activation functions and batch normalization between layers [113]
Multimodal Feature Separation Module:
- Objective: Separate and interact differences between spectral modalities to capture complementary molecular information
- Method: Implement cross-modal attention mechanisms to highlight modality-specific and shared features
- Output: Enhanced feature representations emphasizing complementary information [113]
Feature Cross-Fusion Network Module:
- Architecture: Design a dual-path network with cross-connections between modalities
- Dynamic Modeling: Implement gating mechanisms to weight contributions from different modalities adaptively
- Integration: Fuse intra-modal and inter-modal features through concatenation or weighted summation [113]
Prediction with Bidirectional Long Short-Term Memory (BiLSTM):
- Input: Fused multi-modal features
- Architecture: Implement BiLSTM network to capture sequential dependencies in spectral features
- Output Layer: Use softmax activation for classification tasks (e.g., malignant vs. benign)
- Training: Employ sequential decision reconstruction to enhance decision information [113]
Validation Framework:
- Data Partitioning: Implement k-fold cross-validation (typically k=5 or 10) to ensure robust performance estimation
- Performance Metrics: Calculate accuracy, AUC, sensitivity, specificity, and F1-score
- Statistical Testing: Perform significance testing (e.g., paired t-tests) to verify performance improvements from multi-modal fusion
- Ablation Studies: Systematically remove individual components to quantify their contribution to overall performance
Research Reagent Solutions and Essential Materials
Table 2: Essential Research Reagents and Materials for Multi-modal Blood Spectroscopy
| Category | Specific Item | Function/Application | Key Specifications |
|---|---|---|---|
| Reference Materials | Freeze-dried Control Sera (e.g., SPINREACT) | Quality control and method validation | Certified for ~38 parameters, normal and pathological variants available [57] |
| Sample Preparation | Zinc Selenide (ZnSe) Substrates | FTIR spectroscopy substrate | IR-transparent, suitable for liquid sample deposition [57] |
| Aluminum-coated Glass Slides | Raman spectroscopy substrate | Low fluorescence background, enhanced signal for weak Raman scatterers | |
| Low-Protein-Binding Microtubes | Sample storage and aliquoting | Prevents analyte adhesion to tube walls | |
| Solvents & Reagents | Bidistilled Water | Sample dilution series preparation | Minimal impurity interference in spectroscopic analysis [57] |
| Phosphate Buffered Saline (PBS) | Sample dilution and buffer preparation | Maintains physiological pH for native state analysis | |
| Calibration Standards | Silicon Wafer | Raman frequency calibration | Provides characteristic peak at 520.7 cmâ»Â¹ for instrument calibration |
| Polystyrene Films | FTIR wavelength calibration | Provides characteristic peaks for instrument validation | |
| Software & Analysis | Spectral Processing Software (e.g., ZaIR, MATLAB) | Spectral preprocessing and analysis | Baseline correction, normalization, peak identification capabilities [57] |
| Deep Learning Frameworks (e.g., PyTorch, TensorFlow) | Implementation of fusion algorithms | Support for custom neural network architectures [113] |
Analytical Considerations and Technical Notes
Data Quality Assessment
Prior to multi-modal fusion, assess data quality for each modality independently. For FTIR spectra, inspect amide I (1650 cmâ»Â¹) and amide II (1536 cmâ»Â¹) bands for protein integrity. For Raman spectra, evaluate signal-to-noise ratio and presence of characteristic biomolecule bands. Exclude samples with poor spectral quality or evidence of degradation from analysis.
Optimization of Fusion Parameters
The performance of multi-modal fusion approaches depends critically on proper parameter optimization. Key parameters include:
- Feature dimension in the FCNN encoder: Typically 256-512 features provides optimal balance between information retention and computational efficiency
- Fusion weights in cross-fusion network: Can be fixed or learned adaptively during training
- Network depth in separation and fusion modules: 3-5 layers typically sufficient for spectroscopic data
Validation with Orthogonal Methods
Where possible, validate multi-modal spectroscopic findings with orthogonal clinical methods such as histopathology, immunohistochemistry, or established clinical assays. This confirms that spectroscopic signatures correlate with biologically meaningful endpoints.
Addressing Technical Variability
Incorporate randomization and blocking in experimental design to account for potential technical variability from sample processing order, reagent batches, and instrument drift. Include quality control samples in each analytical batch to monitor performance over time.
The protocols outlined herein provide a comprehensive framework for implementing multi-modal approaches in blood-based diagnostic research. The integration of complementary spectroscopic techniques, particularly through advanced computational fusion strategies like MSCNet, demonstrates significant improvements in diagnostic accuracy compared to single-modality approaches. These methods enable researchers to leverage the full potential of blood spectroscopy for precise disease detection and characterization, advancing the field toward clinical implementation of these powerful analytical techniques.
Conclusion
Blood spectroscopy represents a rapidly advancing frontier in medical diagnostics, with demonstrated success in therapeutic drug monitoring, cancer detection, and non-invasive disease screening. The integration of AI with techniques like SERS and the development of robust, standardized protocols are overcoming traditional limitations, bringing these tools closer to routine clinical use. Future directions include expanding multi-analyte panels for comprehensive disease profiling, developing point-of-care devices for decentralized testing, and establishing large-scale validation studies to secure regulatory approval. For researchers and drug development professionals, these technologies offer powerful tools for precision medicine, enabling more personalized treatment strategies and fundamentally transforming how we diagnose and monitor disease through minimal blood analysis.
References
- 1. (PDF) Raman Spectroscopy of Blood and Blood Components [https://www.academia.edu/35584415/Raman_Spectroscopy_of_Blood_and_Blood_Components]
- 2. A literature review and novel theoretical approach on the optical properties of whole blood - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3953607/]
- 3. Optical Absorption of Hemoglobin [https://omlc.org/spectra/hemoglobin/]
- 4. Infrared Spectroscopy: A New Frontier in Hematological Disease Diagnosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10707114/]
- 5. Quantification of total haemoglobin concentrations in human whole... [https://www.nature.com/articles/s41598-019-51721-9?error=cookies_not_supported&code=957783a2-6222-4237-9931-72da26923602]
- 6. [Research on the blood detecting by multi-optical path...] components [https://pubmed.ncbi.nlm.nih.gov/21105400/]
- 7. Point-of-Care No-Specimen Diagnostic Platform Using Machine Learning and Raman Spectroscopy: Proof-of-Concept Studies for Both COVID-19 and Blood Glucose [https://www.mdpi.com/2813-446X/3/1/6]
- 8. -Based Techniques in Raman for Medical ... Applications Diagnostic [https://pmc.ncbi.nlm.nih.gov/articles/PMC10647591/]
- 9. Diffuse correlation spectroscopy for non-invasive, micro-vascular cerebral blood flow measurement - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3991554/]
- 10. Diffuse Optics for Tissue Monitoring and Tomography - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4482362/]
- 11. Comparison of diffuse correlation spectroscopy, interferometric diffusing wave spectroscopy, and speckle contrast optical spectroscopy for blood flow monitoring - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12340614/]
- 12. -based technique for accessible and rapid SERS of multiple... diagnosis [https://www.light-am.com/article/doi/10.37188/lam.2025.035]
- 13. Deep learning of surface-enhanced Raman data for... spectroscopy [https://link.springer.com/article/10.1140/epjs/s11734-024-01449-z]
- 14. Infrared and Raman spectroscopy of blood plasma for rapid endometrial cancer detection | British Journal of Cancer [https://www.nature.com/articles/s41416-025-03050-0]
- 15. Surface-enhanced Raman Spectroscopy of Blood Serum for... [https://romj.org/2025-0306]
- 16. Analyzing Biofluids with ATR-FTIR Spectroscopy [https://www.azom.com/article.aspx?ArticleID=22517]
- 17. Stability of person-specific blood -based... | Nature Communications [https://www.nature.com/articles/s41467-021-21668-5?error=cookies_not_supported&code=1dc3c9a4-58ce-494a-bbef-f14a0ef0a2ed]
- 18. Quantitative comparison of whole blood, plasma and serum ... [https://link.springer.com/article/10.1007/s11306-025-02345-w]
- 19. Label-free surface-enhanced Raman spectroscopy of biofluids ... [https://pubmed.ncbi.nlm.nih.gov/25935674/]
- 20. Harmonizing drug analysis and sustainability: Spectroscopic quantification of antiplatelet-anticoagulant regimens - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1386142525010765]
- 21. Frontiers | Absorption, scattering, and refractive index of blood and its... [https://www.frontiersin.org/journals/photonics/articles/10.3389/fphot.2025.1636398/full]
- 22. Frontiers | Challenges in “probing spectroscopic probes†for noninvasive simultaneous disease diagnosis [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2024.1463273/full]
- 23. Spectroscopic approach for dynamic bioanalyte tracking with minimal concentration information - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4894421/]
- 24. Electric-Field Molecular to Probe Cancer - PMC Fingerprinting [https://pmc.ncbi.nlm.nih.gov/articles/PMC12022918/]
- 25. Chromogenic Detection for Western Blot, IHC, and ELISA [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/chromogenic-detection-for-western-blot-ihc-and-elisa/]
- 26. Chromogenic Assay - ELISA [http://www.elisa-antibody.com/ELISA-Introduction/elisa-detection-strategies/elisa-chromogenic-assay.html]
- 27. New AI-Powered Raman Spectroscopy Method Enables Rapid Drug... [https://www.spectroscopyonline.com/view/new-ai-powered-raman-spectroscopy-method-enables-rapid-drug-detection-in-blood]
- 28. Quantification of blood flow index in diffuse correlation spectroscopy ... [https://pubmed.ncbi.nlm.nih.gov/38283935/]
- 29. Estimation of Time-Since-Deposition of bloodstains on different... [https://link.springer.com/article/10.1007/s12024-024-00849-w]
- 30. Whole Blood Analysis using UV-Vis Spectroscopy | Ocean Optics [https://www.oceanoptics.com/blog/whole-blood-analysis/]
- 31. Applications of Diffuse Reflectance Spectroscopy in Medicine [https://www.azooptics.com/Article.aspx?ArticleID=2710]
- 32. Application of FTIR Spectroscopy for Quantitative Analysis of Blood Serum: A Preliminary Study - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8700755/]
- 33. Advances in Surface-Enhanced Raman Spectroscopy for Therapeutic... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11721930/]
- 34. SERS based determination of ceftriaxone, ampicillin, and vancomycin in serum using WS2/Au@Ag nanocomposites and a 2D-CNN regression model - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1386142525001568]
- 35. A new perspective on antimicrobial therapeutic drug monitoring: Surface-enhanced Raman spectroscopy - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0039914025005077]
- 36. Illicit Drug Analysis in Blood Samples with Multivariate Analysis Using Surface-Enhanced Raman Spectroscopy | Spectroscopy Online [https://www.spectroscopyonline.com/view/illicit-drug-analysis-in-blood-samples-with-multivariate-analysis-using-surface-enhanced-raman-spectroscopy]
- 37. Automated clinical platform for personalized... [https://cordis.europa.eu/project/id/101158666]
- 38. -based rapid susceptibility testing of commonly administered... SERS [https://link.springer.com/article/10.1007/s11274-023-03717-x]
- 39. Surface-enhanced Raman spectroscopy of blood plasma and serum using Ag and Au nanoparticles: a systematic study - PubMed [https://pubmed.ncbi.nlm.nih.gov/24493335/]
- 40. and Infrared of blood plasma for rapid... Raman spectroscopy [https://pubmed.ncbi.nlm.nih.gov/40383740/]
- 41. evaluation of carcinogenesis in Spectroscopic endometrial cancer [https://www.nature.com/articles/s41598-021-88640-7?error=cookies_not_supported]
- 42. Surface-enhanced Raman in women with benign and... spectroscopy [https://journals.rcsi.science/2313-8726/article/view/219533]
- 43. Differential Rapid Diagnosis of Endometrial and Its Benign... Cancer [https://jbpe.ssau.ru/index.php/JBPE/article/view/9041]
- 44. Toward Informative Representations of Bloodâ€Based Infrared Spectra via Unsupervised Deep Learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318647/]
- 45. as a non-invasive diagnostic technique for... Raman spectroscopy [https://www.nature.com/articles/s41598-019-56308-y?error=cookies_not_supported&code=17102a5f-4f44-43ab-b3ce-dcd2d1090d9f]
- 46. METHODS FOR ESTIMATION OF BLOOD GLUCOSE : A COMPARATIVE EVALUATION - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5531325/]
- 47. - Non glucose measurements in humans with... | medRxiv invasive [https://www.medrxiv.org/content/10.1101/2025.03.12.25323511v1.full]
- 48. Noninvasive blood glucose sensing by near-infrared spectroscopy based on PLSR combines SAE deep neural network approach - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S135044952030668X]
- 49. A Feasibility Study on Noninvasive Blood Glucose Estimation Using Machine Learning Analysis of Near-Infrared Spectroscopy Data [https://www.mdpi.com/2079-6374/15/11/711]
- 50. Wearables May Have A Bright Future, Study Says Blood Glucose [https://www.forbes.com/sites/andrewwilliams/2025/03/25/blood-glucose-wearables-may-have-a-bright-future-says-study/]
- 51. : structure meets function Red cell membrane disorders [https://pubmed.ncbi.nlm.nih.gov/32702754/]
- 52. Fluorescence spectroscopy as a novel tool in hematological diagnostics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11964476/]
- 53. Frontiers | Clinical Diagnosis of Red ... Cell Membrane Disorders [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.00636/full]
- 54. A study of the dynamic properties of the human red blood cell membrane using quasi-elastic light-scattering spectroscopy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1226000/]
- 55. Probing Red Blood Cell Membrane Microviscosity Using Fluorescence Anisotropy Decay Curves of the Lipophilic Dye PKH26 [https://www.mdpi.com/1422-0067/23/24/15767]
- 56. Infrared Spectroscopy: A New Frontier in Hematological Disease Diagnosis - PubMed [https://pubmed.ncbi.nlm.nih.gov/38069330/]
- 57. of FTIR Application for Quantitative Analysis of Spectroscopy ... Blood [https://pmc.ncbi.nlm.nih.gov/articles/PMC8700755/]
- 58. What is Spectral Software? Uses, How It Works & Top Companies... [https://www.linkedin.com/pulse/what-spectral-software-uses-how-works-top-companies-2025-y9gie]
- 59. 5 Surprising Spectral Trends Transforming Data Science Analysis [https://www.numberanalytics.com/blog/5-surprising-spectral-analysis-trends]
- 60. Hyperspectral Imaging for Bloodstain Identification - PMC [https://ncbi.nlm.nih.gov/pmc/articles/PMC8123592]
- 61. Expanding the Limits of Human Blood Metabolite Quantitation Using NMR Spectroscopy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4287831/]
- 62. Current Trends in In Vitro Diagnostics Using Surface-Enhanced Raman Scattering in Translational Biomedical Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109636/]
- 63. Development and Application of Surface - Enhanced ... Raman [https://www.preprints.org/manuscript/202407.1632]
- 64. Towards Reliable and Quantitative Surfaceâ€Enhanced Raman Scattering (SERS): From Key Parameters to Good Analytical Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7154527/]
- 65. in Reproducibility - surface spectroscopy enhanced Raman [https://link.springer.com/article/10.1007/s12204-014-1566-7]
- 66. A practical approach to quantitative analytical surface - enhanced ... [https://pubs.rsc.org/en/content/articlehtml/2025/cs/d4cs00861h]
- 67. Highly Uniform and Reproducible ... Surface Enhanced Raman [https://www.nature.com/articles/srep05835?error=cookies_not_supported&code=fe6637dd-151f-45a6-8421-53b1c54c8173]
- 68. Highly Reproducible - Surface ... Enhanced Raman Scattering [https://pmc.ncbi.nlm.nih.gov/articles/PMC7349361/]
- 69. demystified: Strategies for resolving challenges in... Matrix effects [https://pubmed.ncbi.nlm.nih.gov/37897324/]
- 70. Strategies for the Detection and Elimination of Matrix in... Effects [https://www.chromatographyonline.com/view/strategies-detection-and-elimination-matrix-effects-quantitative-lc-ms-analysis]
- 71. What are Matrix in Liquid Chromatography Mass Effect ? Spectrometry [https://www.nebiolab.com/what-are-matrix-effect-in-liquid-chromatography-mass-spectrometry/]
- 72. A novel Raman spectroscopic for detecting traces of method ... blood [https://www.nature.com/articles/s41598-023-31918-9?error=cookies_not_supported]
- 73. Cancer Diagnosis: New Raman Spectroscopy Eliminates... Method [https://www.spectroscopyonline.com/view/cancer-diagnosis-new-raman-spectroscopy-method-eliminates-fluorescence-interference]
- 74. Advanced Strategies for Matrix Effect Mitigation [https://www.numberanalytics.com/blog/advanced-strategies-for-matrix-effect-mitigation]
- 75. Quantitative analysis of human blood serum using vibrational spectroscopy - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2666054720300041]
- 76. Evaluation of human plasma sample preparation protocols for untargeted metabolic profiles analyzed by UHPLC-ESI-TOF-MS - PubMed [https://pubmed.ncbi.nlm.nih.gov/25308499/]
- 77. and Sample in metabolite identification | PPTX preparation protocols [https://www.slideshare.net/slideshow/sample-preparation-and-protocols-in-metabolite-identification/251023384]
- 78. and Serum Plasma | Thermo Fisher Scientific - AM Preparation [https://www.thermofisher.com/am/en/home/references/protocols/cell-and-tissue-analysis/elisa-protocol/elisa-sample-preparation-protocols/plasma-and-serum-preparation.html]
- 79. Serum and Plasma Preparation | Quansys Biosciences [https://www.quansysbio.com/support/serum-and-plasma-preparation/]
- 80. A Review of Machine Learning Methods Recently Applied to FTIR Spectroscopy Data for the Analysis of Human Blood Cells [https://www.mdpi.com/2072-666X/14/6/1145]
- 81. Noise reduction in functional near-infrared spectroscopy signals by independent component analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/23902043/]
- 82. Noise and Speckle Reduction in Doppler Blood Flow Spectrograms Using an Adaptive Pulse-Coupled Neural Network | EURASIP Journal on Advances in Signal Processing | Full Text [https://asp-eurasipjournals.springeropen.com/articles/10.1155/2010/918015]
- 83. GitHub... [https://github.com/sirisaacnewton540/Blood-Spectroscopy-Based-Biomarker-Estimation-using-Machine-Learning]
- 84. Spectra-based blood species discrimination by machine learning: Between human and non-human - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1350449522000433]
- 85. A spectroscopic liquid biopsy for the earlier detection of multiple... [https://www.nature.com/articles/s41416-023-02423-7?error=cookies_not_supported&code=e08d990e-7f41-4b82-bbfd-4bd2365bfb05]
- 86. Overcoming barriers to evidence-based patient blood management... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-020-0965-4]
- 87. Nanoscope Strengthens Global Regulatory for MCO-010... Pathways [https://nanostherapeutics.com/2025/09/02/nanoscope-strengthens-global-regulatory-pathways-for-mco-010-with-fda-rmat-and-five-ema-orphan-designations/]
- 88. of the PrecivityAD2 Clinical test: A mass... validation blood [https://pubmed.ncbi.nlm.nih.gov/38491912/]
- 89. Analysis of Plasma, Serum, and Whole Blood Metabolites Using... [https://pubmed.ncbi.nlm.nih.gov/31463837/]
- 90. Clinical Trial Data Visualization: The New FDA Guideline on Standard Formats [https://beaconcure.com/resources/clinical-trial-data-visualization/]
- 91. Research Reporting Guidelines and Initiatives: By Organization [https://www.nlm.nih.gov/services/research_report_guide.html]
- 92. Guidelines for Reporting of Figures and Tables for Clinical Research in Urology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7387170/]
- 93. Spectroscopic methods for COVID-19 detection and early diagnosis | Virology Journal | Full Text [https://virologyj.biomedcentral.com/articles/10.1186/s12985-022-01867-2]
- 94. Liquid chromatography–mass spectrometry - Wikipedia [https://en.wikipedia.org/wiki/Liquid_chromatography%E2%80%93mass_spectrometry]
- 95. Recent Advances in Liquid Chromatography–Mass Spectrometry (LC–MS) Applications in Biological and Applied Sciences - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204688/]
- 96. Quantification for non-targeted LC/MS screening without standard substances | Scientific Reports [https://www.nature.com/articles/s41598-020-62573-z]
- 97. Positive and Negative Mode in Mass Spectroscopy : LC - MS / MS Method [https://www.nebiolab.com/positive-and-negative-mode-in-mass-spectroscopy/]
- 98. LC-MS Sample Preparation | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/industrial/mass-spectrometry/mass-spectrometry-learning-center/liquid-chromatography-mass-spectrometry-lc-ms-information/lc-ms-sample-preparation.html]
- 99. Mass Spectrometry Explained: How LC/MS/MS Works | PerkinElmer Blog [https://blog.perkinelmer.com/posts/mass-spectrometry-explained-how-lc-ms-ms-works/]
- 100. Introduction to Infrared and Raman-Based Biomedical Molecular Imaging and Comparison with Other Modalities - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7731440/]
- 101. The Promise of Infrared in Liquid Biopsies for Solid... Spectroscopy [https://pubmed.ncbi.nlm.nih.gov/39941298/]
- 102. Raman spectroscopy - Wikipedia [https://en.wikipedia.org/wiki/Raman_spectroscopy]
- 103. Infrared or Raman Spectroscopy? - Edinburgh Instruments [https://www.edinst.com/resource/infrared-or-raman-spectroscopy/]
- 104. Assessing lung cancer progression and survival with infrared ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03924-3]
- 105. for Raman spectroscopy cancer detection [https://www.news-medical.net/whitepaper/20240520/Raman-spectroscopy-for-cancer-detection.aspx]
- 106. for Evaluating the Accuracy of Diagnostic Tests Methods [https://www.e-jcpp.org/journal/view.php?doi=10.36011/cpp.2021.3.e2]
- 107. Lots of sensitivities , or: How do analytical , diagnostical, and... [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/sensitivities]
- 108. and Performance of a Analytical -Based P-tau217... Validation Blood [https://pubmed.ncbi.nlm.nih.gov/39836199/]
- 109. of Exosome Analytical for Clinical Applications Validation Diagnostics [https://www.sepscience.com/analytical-validation-of-exosome-diagnostics-for-clinical-applications-12159]
- 110. Assessing the reproducibility of diagnostic tests across different... [https://editverse.com/assessing-the-reproducibility-of-diagnostic-tests-across-different-laboratories-and-settings/]
- 111. Comprehensive normalization and binary classification methods for... [https://pubmed.ncbi.nlm.nih.gov/39929347/]
- 112. Biomedical Applications for Spectroscopy - Avantes [https://www.avantes.com/applications/cases/biomedical-applications-for-spectroscopy/]
- 113. Multimodal separation and cross fusion network based on Raman... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11586440/]
- 114. Deep learning in multi - modal breast cancer data : a literature... fusion [https://qims.amegroups.org/article/view/143128/html]
- 115. Comprehensive Evaluation of Multimodal AI Models in Medical Imaging Diagnosis: From Data Augmentation to Preference-Based Comparison [https://arxiv.org/html/2412.05536v1]