Development and Validation of HPLC-UV Methods for Antiretroviral Drug Analysis: A Comprehensive Guide for Researchers
This article provides a comprehensive overview of the development, validation, and application of High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) for the analysis of antiretroviral drugs.
Development and Validation of HPLC-UV Methods for Antiretroviral Drug Analysis: A Comprehensive Guide for Researchers
Abstract
This article provides a comprehensive overview of the development, validation, and application of High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) for the analysis of antiretroviral drugs. Tailored for researchers, scientists, and drug development professionals, it covers foundational principles from the role of therapeutic drug monitoring in managing HIV treatment to advanced methodological applications for simultaneous multi-drug quantification in various matrices. The content explores robust troubleshooting strategies for common chromatographic challenges and delivers a rigorous framework for method validation according to International Conference on Harmonization (ICH) guidelines, including comparative analysis with alternative techniques like spectrophotometry. By synthesizing current research and practical methodologies, this resource aims to support advancements in pharmaceutical quality control, clinical trial analysis, and personalized HIV therapy.
The Critical Role of HPLC-UV in Modern Antiretroviral Therapy and Research
Antiretroviral therapy (ART) involves the use of a combination of medications to treat HIV infection. The primary goals of ART are to suppress HIV replication, restore and preserve immune function, reduce HIV-associated morbidity and mortality, and prevent HIV transmission [1] [2]. Modern combination ART typically consists of three drugs from at least two different classes, which effectively suppresses the virus to undetectable levels, allowing people with HIV to live long, healthy lives and preventing sexual transmission of the virus [3] [4].
The following table outlines the major classes of antiretroviral drugs and their primary mechanisms of action:
| Drug Class | Mechanism of Action | Key Drug Examples |
|---|---|---|
| Nucleoside Reverse Transcriptase Inhibitors (NRTIs) | Incorporate into viral DNA, causing chain termination during reverse transcription [3] [1] | Abacavir, Emtricitabine, Lamivudine, Tenofovir [3] |
| Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) | Directly bind to and inhibit reverse transcriptase enzyme [3] [1] | Efavirenz, Nevirapine, Rilpivirine [3] [5] |
| Protease Inhibitors (PIs) | Inhibit HIV protease, preventing viral maturation [3] [1] | Atazanavir, Darunavir, Lopinavir [3] [6] |
| Integrase Strand Transfer Inhibitors (INSTIs) | Block integration of viral DNA into host genome [3] [1] [7] | Dolutegravir, Raltegravir, Bictegravir [3] [5] |
| Entry Inhibitors | Prevent HIV from entering host CD4 cells [1] [7] | Fostemsavir, Ibalizumab, Maraviroc, Enfuvirtide [1] [7] |
| Capsid Inhibitors | Disrupt HIV capsid function, interfering with viral lifecycle [1] [8] | Lenacapavir [8] |
| Pharmacokinetic Enhancers | Inhibit drug metabolism to increase ART drug levels [3] [1] | Cobicistat, Ritonavir [3] [1] |
The HIV Lifecycle and ART Drug Targets
Understanding the HIV lifecycle is fundamental to comprehending the mechanism of action of ART. The diagram below illustrates the key stages of the HIV replication cycle and the specific steps where different classes of antiretroviral drugs exert their inhibitory effects.
The Critical Need for Therapeutic Drug Monitoring (TDM) in ART
Therapeutic Drug Monitoring (TDM) is a critical practice for optimizing ART, defined as the measurement of drug concentrations in biological fluids to guide dosing for individual patients [5]. Several factors create variability in drug exposure, which can lead to treatment failure or drug toxicity if unaddressed [6] [5] [2].
Key justifications for TDM in ART include:
- Polypharmacy and Drug-Drug Interactions: Patients with HIV, particularly the aging population and those with co-infections like tuberculosis, often take multiple medications. This polypharmacy increases the risk of drug-drug interactions that can significantly alter ART plasma concentrations [6] [5] [2].
- Pharmacogenetic Variability: Inter-individual genetic differences in drug-metabolizing enzymes and transporters can lead to significant variations in drug pharmacokinetics [5].
- Prevention of Resistance and Toxicity: Subtherapeutic drug concentrations can lead to incomplete viral suppression and the emergence of drug-resistant HIV strains [8] [2]. Conversely, supratherapeutic concentrations increase the risk of dose-related adverse effects [8].
- Special Patient Populations: Patients with hepatic or renal impairment require careful dose adjustment, as many ART drugs are metabolized by the liver or can be nephrotoxic (e.g., tenofovir) [3].
HPLC-UV as a Core Analytical Tool for ARV Quantification
High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) is a well-established and accessible analytical technique for the simultaneous quantification of multiple antiretroviral drugs in human plasma. It offers a cost-effective and technically feasible alternative to more complex methods like LC-MS/MS, making it suitable for clinical laboratories in various settings [6].
Application Note: Simultaneous Quantification of Nine ARVs
A validated HPLC-UV method demonstrates the capability to simultaneously analyze nine frequently administered antiretroviral drugs in human plasma, providing a robust framework for TDM [6].
Table: Optimized Chromatographic Parameters for ARV Analysis [6]
| Parameter | Specification |
|---|---|
| Analytical Column | XBridge C18 (4.6 mm × 150 mm, 3.5 µm) |
| Guard Column | Sentry (4.6 mm × 10 mm) |
| Mobile Phase | Solvent A: Acetonitrile; Solvent B: 50 mM Acetate Buffer (pH 4.5) |
| Flow Rate | 1.0 mL/min |
| Gradient Elution | 40% A for 9 min, then linear increase over 7 min |
| Detection Wavelengths | 260 nm (ATV, DRV, DTG, EFV, LPV, RGV, TPV); 305 nm (ETV, RPV) |
| Column Temperature | 35 °C |
| Injection Volume | Not Specified |
| Internal Standard | Quinoxaline |
| Sample Volume | 500 µL of human plasma |
| Sample Preparation | Solid Phase Extraction (SPE) |
Table: Analytical Performance Data for the Validated HPLC-UV Method [6]
| Analyte | Retention Time (min) | Calibration Range (ng/mL) | Intra-day & Inter-day Precision (RSD, %) | Accuracy (% Deviation) |
|---|---|---|---|---|
| Atazanavir (ATV) | 15.3 | 60 - 12,000 | < 15.0 | < 15.0 |
| Dolutegravir (DTG) | 5.4 | 20 - 8,000 | < 15.0 | < 15.0 |
| Darunavir (DRV) | 9.6 | 150 - 15,000 | < 15.0 | < 15.0 |
| Efavirenz (EFV) | 17.1 | 150 - 15,000 | < 15.0 | < 15.0 |
| Etravirine (ETV) | 17.4 | 50 - 4,000 | < 15.0 | < 15.0 |
| Lopinavir (LPV) | 17.4 | 150 - 15,000 | < 15.0 | < 15.0 |
| Raltegravir (RGV) | 5.6 | 40 - 9,600 | < 15.0 | < 15.0 |
| Rilpivirine (RPV) | 13.8 | 20 - 2,000 | < 15.0 | < 15.0 |
| Tipranavir (TPV) | 18.7 | 500 - 40,000 | < 15.0 | < 15.0 |
Detailed Experimental Protocol: HPLC-UV Analysis of ARVs
Materials and Reagents
- Analytical Standards: Certified reference standards for all analytes (e.g., from Spectra 2000, Janssen Cilag) [6].
- Internal Standard (IS): Quinoxaline (e.g., from Sigma-Aldrich) [6].
- Solvents: HPLC-grade methanol, acetonitrile, and dimethylsulfoxide (DMSO) [6].
- Water: Deionized water purified through a Milli-Q system [6].
- Buffers: Sodium acetate for preparing 50 mM acetate buffer, pH 4.5 [6].
- Biological Matrix: Drug-free human plasma from healthy volunteers [6].
Sample Preparation: Solid Phase Extraction
This protocol is designed for a 500 µL plasma sample [6].
- Spiking: Add appropriate volumes of analyte working solutions and internal standard (Quinoxaline) to 500 µL of plasma.
- Extraction: Process the plasma sample using a solid-phase extraction (SPE) procedure.
- Reconstitution: After extraction, evaporate the eluent to dryness under a gentle stream of nitrogen. Reconstitute the dry residue with a suitable volume of mobile phase initial conditions prior to HPLC injection.
Instrumental Analysis and Quantification
- System Setup: Configure the HPLC-UV system as per parameters in Table 2.
- Calibration: Prepare two separate calibration curves (Curve A and Curve B) due to co-elution of DTG/RGV and EFV/LPV. Analyze calibrators in duplicate [6].
- Quality Control (QC): Analyze QC samples at low, medium, and high concentrations in each batch to ensure accuracy and precision.
- Chromatographic Run: Inject the processed sample and perform gradient elution.
- Data Analysis: Measure peak areas. Calculate the analyte/IS peak area ratio. Construct a calibration curve for each analyte using a weighted (1/x or 1/x²) least-squares regression model. Determine the concentration of analytes in unknown samples by interpolation from the calibration curve [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table: Key Reagent Solutions for HPLC-UV based ARV Analysis
| Research Reagent / Material | Function / Application |
|---|---|
| C18 Reverse-Phase Analytical Column | Core component for chromatographic separation of analytes based on hydrophobicity [6]. |
| Certified Drug Reference Standards | Essential for preparing calibration standards and QC samples to ensure method accuracy and identity confirmation [6] [5]. |
| Stable Isotope-Labeled Internal Standards | Correct for variability in sample preparation and injection; improve quantitative accuracy (e.g., Dolutegravir-d4) [5]. |
| Solid Phase Extraction (SPE) Cartridges | Clean-up and concentrate analytes from complex plasma matrix, improving sensitivity and reducing interferences [6]. |
| HPLC-Grade Solvents & Buffers | Constitute the mobile phase; high purity is critical for low background noise and reproducible retention times [6] [5]. |
| Mass Spectrometer (LC-MS/MS Alternative) | Provides superior specificity and sensitivity for complex TDM applications, though at a higher cost [8] [5]. |
| (3-(Cyclopentylcarbamoyl)phenyl)boronic acid | (3-(Cyclopentylcarbamoyl)phenyl)boronic acid, CAS:850567-24-7, MF:C12H16BNO3, MW:233.07 g/mol |
| 2,2,2-Trichloro-N-(pyridin-3-YL)acetamide | 2,2,2-Trichloro-N-(pyridin-3-YL)acetamide, CAS:82202-41-3, MF:C7H5Cl3N2O, MW:239.5 g/mol |
Advanced and Emerging Analytical Techniques
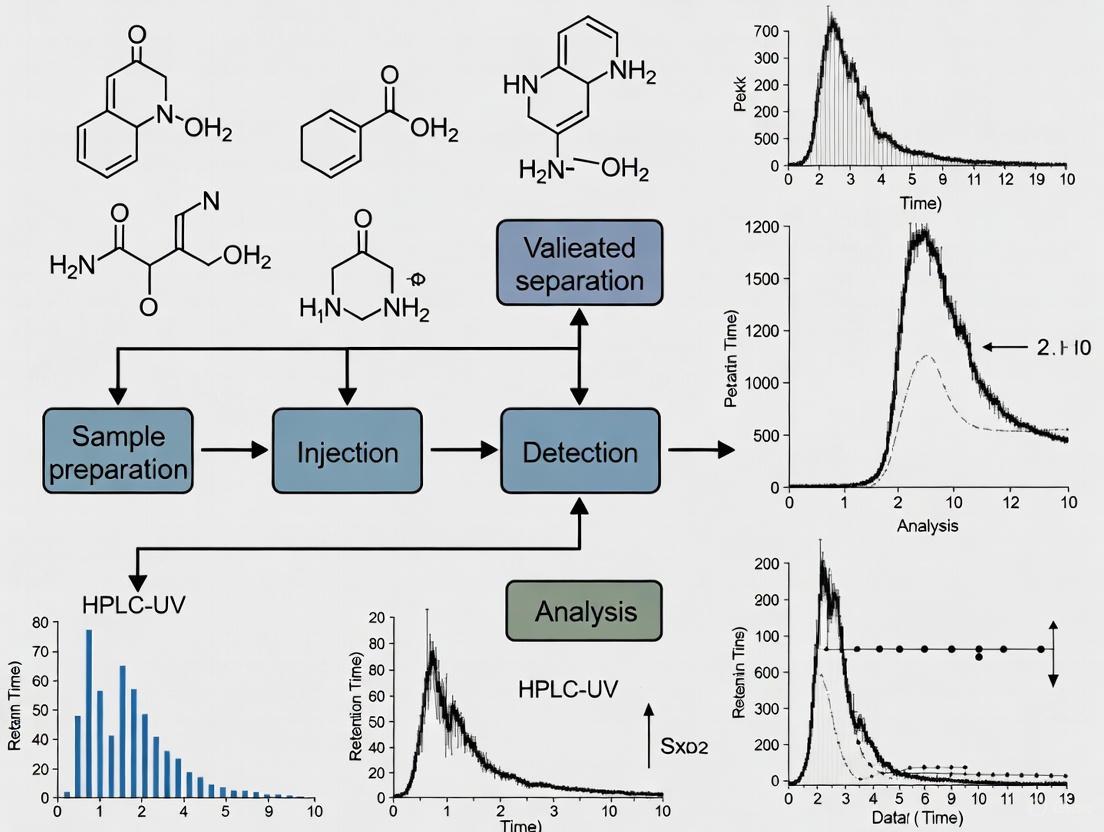
While HPLC-UV is a robust workhorse, advanced methodologies are continuously developed. The experimental workflow for developing and validating a bioanalytical method for ART monitoring is outlined below.
- LC-MS/MS Methods: Liquid chromatography coupled with tandem mass spectrometry offers superior sensitivity and specificity. A recent study developed an LC-MS method for simultaneous determination of dolutegravir, nevirapine, efavirenz, rifampicin, and rifapentine in human plasma, which is crucial for managing HIV-TB co-infections [5]. This method demonstrated a linear range of 0.25 µg/mL to 10.00 µg/mL and used protein precipitation with 100% acetonitrile for sample preparation [5].
- Novel Fluorometric Methods: Emerging techniques utilize carbon dots (C-dots) as fluorescent nanoprobes. One novel method for monitoring lenacapavir, a capsid inhibitor, uses orange-emitting carbon dots (O-CDs) and operates via an inner filter effect mechanism [8]. This approach offers a simpler, more cost-effective, and environmentally friendly alternative for TDM, though it is not yet as widely established as chromatographic methods [8].
High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) represents a cornerstone analytical technique in the field of antiretroviral (ARV) drug research and therapeutic drug monitoring (TDM). The complexity of highly active antiretroviral therapy (HAART), which typically involves combinations of multiple drugs from different classes, creates a significant analytical challenge that HPLC-UV is uniquely positioned to address [6] [9]. This technique enables the simultaneous quantification of numerous ARV agents in various matrices, including human plasma, providing crucial data for optimizing dosing regimens, assessing compliance, and investigating drug-drug interactions [6]. For researchers and clinical laboratories, HPLC-UV offers an optimal balance of analytical performance, accessibility, and cost-effectiveness compared to more sophisticated techniques like LC-MS/MS, making it particularly suitable for routine monitoring in hospital settings [6] [9].
Fundamental Principles of HPLC-UV
Chromatographic Separation Mechanism
The separation of antiretroviral compounds in HPLC-UV relies on differential partitioning between mobile and stationary phases. Most ARV methods utilize reversed-phase chromatography with C18 bonded silica columns, where analytes interact with the hydrophobic stationary phase through van der Waals forces and hydrophobic interactions [6] [10] [9]. The degree of retention depends on the compound's chemical structure, with more hydrophobic molecules exhibiting stronger retention. Gradient elution, typically employing increasing concentrations of organic modifier (acetonitrile or methanol) in an aqueous buffer, enables the resolution of complex ARV mixtures with diverse physicochemical properties within a single analytical run [6] [11]. Efficient separation is critical for resolving co-administered drugs and their metabolites from endogenous plasma components.
Ultraviolet Detection Principles
UV detection capitalizes on the inherent chromophoric properties of most antiretroviral compounds, which contain aromatic rings or conjugated systems that absorb light in the UV range [6] [10]. When photons of specific energy interact with these molecules, electrons transition to higher energy states, resulting in measurable absorption according to the Beer-Lambert law. Most ARVs exhibit strong absorbance between 240-270 nm, though some require detection at higher wavelengths (e.g., 305 nm for etravirine and rilpivirine) for optimal selectivity [6]. The photodiode array detector enhances method specificity by providing full spectral information for peak purity assessment and identity confirmation [6].
Advantages for Antiretroviral Drug Analysis
HPLC-UV offers several distinct advantages that make it particularly suitable for ARV analysis:
Cost-Effectiveness and Accessibility: Unlike LC-MS/MS systems that require significant capital investment and specialized operational expertise, HPLC-UV instruments are more affordable and widely available in clinical laboratories, facilitating broader implementation of therapeutic drug monitoring programs [6].
Robustness and Reliability: HPLC-UV systems demonstrate exceptional stability and performance in high-throughput clinical environments, with minimal downtime compared to more complex mass spectrometry-based platforms [9].
Adequate Sensitivity for TDM: The sensitivity of modern HPLC-UV systems (typically in the ng/mL range) is sufficient for monitoring ARV concentrations within their therapeutic windows, which generally range from 0.1 to 10 μg/mL in plasma [9].
Straightforward Method Development and Validation: The well-understood principles of HPLC-UV facilitate method development and validation according to regulatory guidelines, making it accessible to laboratories with varying levels of analytical expertise [10] [12].
Compatibility with Diverse Sample Matrices: HPLC-UV methods can be adapted for various biological matrices, including plasma, serum, and cellular extracts, following appropriate sample preparation [6] [9].
Applications in Antiretroviral Research and Monitoring
Simultaneous Multi-Drug Analysis
The capability to simultaneously quantify multiple ARV agents represents one of the most significant applications of HPLC-UV in clinical practice. Advanced methods have been developed for the concurrent analysis of up to nine antiretroviral compounds, including atazanavir, dolutegravir, darunavir, efavirenz, etravirine, lopinavir, raltegravir, rilpivirine, and tipranavir, in a single 25-minute analytical run [6]. This comprehensive profiling is essential for patients on complex regimens, enabling complete pharmacokinetic assessment without requiring multiple analytical methods.
Therapeutic Drug Monitoring (TDM)
HPLC-UV serves as the workhorse for TDM programs aimed at optimizing ARV therapy by maintaining drug concentrations within the therapeutic window while minimizing toxicity [9]. The interindividual variability in ARV pharmacokinetics necessitates personalized dosing approaches, particularly for drugs with narrow therapeutic indices like efavirenz [10]. Regular monitoring of plasma concentrations using robust HPLC-UV methods allows clinicians to make informed dosage adjustments, especially in special populations such as elderly patients with age-related physiological changes or those experiencing polypharmacy [6].
Pharmacokinetic and Bioequivalence Studies
Well-validated HPLC-UV methods provide the necessary precision, accuracy, and sensitivity to support pharmacokinetic studies and bioequivalence assessments of generic ARV formulations [13]. The ability to generate reliable concentration-time data is fundamental to establishing bioavailability, half-life, clearance, and other critical pharmacokinetic parameters that inform dosing recommendations and regulatory decisions.
Table 1: Representative HPLC-UV Methods for Antiretroviral Drug Analysis
| Antiretroviral Drugs Analyzed | Sample Preparation | Chromatographic Conditions | Linear Range | Key Applications | Reference |
|---|---|---|---|---|---|
| ATV, DTG, DRV, EFV, ETV, LPV, RAL, RPV, TPV | Solid-phase extraction | C18 column; gradient of acetonitrile and sodium acetate buffer (pH 4.5) | Varies by drug: e.g., DTG: 20-8000 ng/mL; EFV: 150-15,000 ng/mL | Simultaneous TDM of 9 ARVs | [6] |
| Efavirenz | Liquid-liquid extraction (ethyl acetate) | C18 column (50 × 4.6 mm, 3.5 μm); phosphate buffer pH 3.5 and acetonitrile gradient | 1-300 μg/mL | EFV pharmacokinetic studies | [10] |
| Emtricitabine, Tenofovir, Efavirenz | Protein precipitation | CN column (250 × 4.6 mm, 5 μm); methanol and ammonium acetate buffer (pH 4.5) gradient | FTC: 40-120 μg/mL; TFV: 80-160 μg/mL; EFV: 200-280 μg/mL | Pharmaceutical formulation analysis | [11] |
| Darunavir, Raltegravir | Not specified | C18 column (150 × 4.6 mm); 0.037 M NaH₂PO₄ buffer:ACN:MeOH (40:50:10 v/v/v) | 5-100 mg/L | Dosage form analysis | [14] |
Pharmaceutical Formulation Analysis
HPLC-UV methods play a crucial role in quality control of ARV pharmaceutical products, ensuring accurate dosage, stability, and batch-to-batch consistency [12] [11]. These methods can simultaneously quantify multiple active ingredients in fixed-dose combinations, which have become increasingly common in HIV treatment to improve adherence. The application of HPLC-UV extends to stability-indicating methods that monitor degradation products under various stress conditions, supporting shelf-life determination and proper storage recommendations.
Table 2: Analytical Performance Characteristics of Representative HPLC-UV Methods
| Method Parameter | Performance Characteristics | Validation Guidelines |
|---|---|---|
| Linearity | Correlation coefficient (r²) > 0.99 for all analytes [6] [10] | ICH Q2(R1) [10] [12] |
| Precision | Intra-day and inter-day RSD < 15% for plasma methods [6]; RSD < 5% for formulation analysis [12] | ICH Q2(R1) [10] [12] |
| Accuracy | Recovery rates typically 85-115% for plasma methods [6]; 97-103% for formulation analysis [12] | ICH Q2(R1) [10] [12] |
| Sensitivity | LOD: 0.03 μg/mL for efavirenz; LOQ: 0.1 μg/mL for efavirenz [10] | Signal-to-noise ratio approach [10] |
| Specificity | Baseline separation of analytes from internal standard and matrix components [6] [10] | Peak purity assessment [10] |
Detailed Experimental Protocols
Sample Preparation: Solid-Phase Extraction
Proper sample preparation is critical for reliable ARV quantification in biological matrices. Solid-phase extraction (SPE) provides excellent cleanup and pre-concentration for plasma samples [6] [9]:
- Aliquot 500 μL of plasma sample into a clean tube and add appropriate internal standard (e.g., quinoxaline) [6].
- Condition SPE cartridge (typically C18 or mixed-mode sorbents) with 1 mL methanol followed by 1 mL water or buffer.
- Load samples onto conditioned cartridges using positive pressure or vacuum manifold.
- Wash with aqueous solution (e.g., 5% methanol in water or dilute acid) to remove interfering compounds.
- Elute analytes with organic solvent (e.g., pure methanol or acetonitrile, or mixtures with acid/base).
- Evaporate eluent to dryness under gentle nitrogen stream at 30-40°C.
- Reconstitute residue in 100-200 μL mobile phase and vortex mix thoroughly.
- Transfer to autosampler vials for HPLC-UV analysis.
This procedure typically yields recovery rates between 80-120% for most ARV drugs, effectively removes matrix interferences, and provides a pre-concentration factor of 2.5-5x [6] [9].
Chromatographic Method Development
Developing a robust HPLC-UV method for ARV analysis requires systematic optimization of multiple parameters:
- Column Selection: Choose appropriate stationary phase chemistry (typically C8 or C18), dimensions (150 mm length recommended), and particle size (3-5 μm) [6] [10].
- Mobile Phase Optimization: Test different buffer systems (acetate, phosphate), pH values (typically 3.5-4.5), and organic modifiers (acetonitrile, methanol) to achieve optimal selectivity [6] [10] [11].
- Gradient Elution Programming: Develop gradient profile to resolve all analytes within reasonable run time (20-30 minutes), incorporating equilibration time for reproducibility [6] [11].
- Detection Wavelength Selection: Utilize PDA detection to identify optimal wavelengths for each analyte, typically 260 nm for most ARVs and 305 nm for etravirine and rilpivirine [6].
- Temperature and Flow Rate Optimization: Evaluate effects of column temperature (30-40°C) and flow rate (1.0-1.5 mL/min) on separation efficiency and analysis time [6] [10].
Method Validation Protocol
Comprehensive validation establishes method reliability for its intended application [10] [12]:
- Linearity: Prepare and analyze minimum of six calibration standards across the expected concentration range, including lower and upper limits of quantification. Accept correlation coefficient (r²) > 0.99 [6] [10].
- Precision: Assess intra-day precision (repeatability) through six replicates at three concentration levels within same day; determine inter-day precision over three consecutive days. Accept RSD < 15% for biological samples [6].
- Accuracy: Perform recovery studies using spiked samples at three concentration levels (low, medium, high) with minimum of three replicates each. Accept recovery of 85-115% [6].
- Specificity: Demonstrate baseline separation of analytes from potentially interfering substances, including matrix components, metabolites, and co-administered drugs [6] [10].
- Sensitivity: Determine limit of detection (LOD) and quantification (LOQ) using signal-to-noise ratios of 3:1 and 10:1, respectively [10].
- Robustness: Evaluate method resilience to deliberate variations in critical parameters (flow rate ±0.1 mL/min, temperature ±2°C, mobile phase pH ±0.2 units) [10].
- Stability: Conduct short-term (bench-top), long-term (freezer storage), and freeze-thaw stability studies for all analytes [10].
HPLC-UV Method Development Workflow
Essential Research Reagents and Materials
Table 3: Essential Research Reagent Solutions for Antiretroviral HPLC-UV Analysis
| Reagent/Material | Specification | Function in Analysis |
|---|---|---|
| HPLC-UV System | Alliance e2695 Separation Module with 2998 PDA detector or equivalent [6] | Liquid handling, separation, and detection |
| Analytical Column | XBridge C18 (4.6×150 mm, 3.5 µm) or equivalent [6] | Stationary phase for chromatographic separation |
| Mobile Phase A | 50 mM sodium acetate buffer, pH 4.5 [6] | Aqueous component for reversed-phase separation |
| Mobile Phase B | HPLC-grade acetonitrile [6] | Organic modifier for gradient elution |
| Solid-Phase Extraction Cartridges | C18 or mixed-mode sorbents (e.g., Oasis HLB) [6] [9] | Sample clean-up and analyte pre-concentration |
| ARV Reference Standards | Certified purity (>98%) from reputable suppliers [6] [10] | Method development, calibration, and quality control |
| Internal Standard | Quinoxaline, nevirapine, or tenofovir disoproxil fumarate [6] [10] [14] | Normalization of analytical variability |
Method Optimization Strategies
Successful HPLC-UV method development for ARV analysis requires strategic optimization of critical parameters:
- pH Optimization: Maintaining mobile phase pH between 3.5-4.5 enhances peak shape for ionizable ARVs by suppressing silanol interactions and controlling ionization state [6] [10] [11].
- Gradient Profile Design: Implement multi-segment gradients with appropriate equilibration times to resolve complex ARV mixtures while maintaining baseline stability [6] [11].
- Column Temperature Control: Operating at 35°C improves retention time reproducibility and separation efficiency while reducing backpressure [6] [14].
- Flow Rate Selection: Balancing analysis time and resolution through flow rates typically between 1.0-2.0 mL/min, considering column dimensions and pressure limitations [6] [10] [14].
ARV Analysis Workflow
HPLC-UV remains an indispensable analytical technique for antiretroviral drug analysis, offering an optimal combination of performance, accessibility, and cost-effectiveness for both research and clinical applications. The principles of reversed-phase chromatography coupled with ultraviolet detection align exceptionally well with the physicochemical properties of most ARV drugs, enabling reliable quantification in complex biological matrices. Well-designed HPLC-UV methods support critical aspects of HIV management, including therapeutic drug monitoring, pharmacokinetic studies, and quality control of pharmaceutical formulations. While mass spectrometry offers superior sensitivity for some applications, HPLC-UV continues to provide a robust, practical solution for laboratories worldwide engaged in the ongoing effort to optimize antiretroviral therapy and improve patient outcomes.
Key Antiretroviral Drug Classes and Their Analytical Challenges
The management of Human Immunodeficiency Virus (HIV) infection relies on combination antiretroviral therapy (cART), which typically involves administering three HIV medications from a minimum of two drug classes [3]. This approach has transformed HIV from a fatal illness to a manageable chronic condition, significantly improving patient survival rates [6] [15]. The life expectancy of HIV-infected patients aged 20 years has increased from 36.1 years to 49.4 years, according to multinational cohort studies [6]. The success of cART hinges on maintaining therapeutic drug concentrations to ensure efficacy while minimizing toxicity, making reliable analytical methods for drug quantification essential for both clinical management and pharmaceutical quality control.
Therapeutic Drug Monitoring (TDM) has emerged as a critical strategy for optimizing dosing regimens of antiretroviral drugs [16]. TDM primarily involves determining plasma drug concentrations in patients to establish relationships with activity and toxicity, requiring accurate, precise, and robust analytical methods. For antiretroviral drugs, TDM has been primarily focused on non-nucleoside reverse transcriptase inhibitors (NNRTIs) and protease inhibitors (PIs), as their plasma concentrations show better correlation with therapeutic outcomes compared to nucleoside reverse transcriptase inhibitors (NRTIs), which are prodrugs requiring intracellular metabolic activation [16].
Antiretroviral Drug Classes: Mechanisms and Properties
Classification and Mechanisms of Action
Table 1: Key Antiretroviral Drug Classes and Their Mechanisms of Action
| Drug Class | Mechanism of Action | Representative Drugs |
|---|---|---|
| Nucleoside Reverse Transcriptase Inhibitors (NRTIs) | Compete with natural deoxynucleotides for incorporation into growing viral DNA chain, causing chain termination [3]. | Zidovudine, Lamivudine, Stavudine, Abacavir, Emtricitabine, Tenofovir [3] [17] |
| Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) | Directly bind to and inhibit reverse transcriptase enzyme by disrupting the movement of protein domains essential for DNA synthesis [3]. | Nevirapine, Efavirenz, Etravirine, Rilpivirine [3] [15] |
| Protease Inhibitors (PIs) | Inhibit HIV-1 protease, preventing proteolytic cleavage of protein precursors necessary for producing infectious viral particles [3]. | Atazanavir, Darunavir, Lopinavir, Tipranavir, Ritonavir (often as pharmacokinetic enhancer) [3] [16] |
| Integrase Strand Transfer Inhibitors (INSTIs) | Block the action of integrase enzyme, preventing the viral genome from inserting into host cell DNA [3]. | Dolutegravir, Raltegravir, Elvitegravir, Bictegravir [3] |
| Pharmacokinetic Enhancers | Inhibit human CYP3A enzymes, increasing plasma concentrations of co-administered drugs [3]. | Cobicistat, Ritonavir [3] |
Fixed-Dose Combinations and Analytical Implications
The development of fixed-dose combinations (FDCs) represents a significant advancement in HIV treatment, enhancing patient adherence through reduced pill burden [18]. These combinations integrate drugs from multiple classes into single formulations, creating complex analytical challenges for quality control and drug quantification. Common FDCs include dolutegravir/lamivudine, abacavir/lamivudine/zidovudine, and emtricitabine/rilpivirine/tenofovir alafenamide [3]. The complexity of these formulations necessitates robust analytical methods capable of simultaneously quantifying multiple active pharmaceutical ingredients with differing physicochemical properties while maintaining specificity, accuracy, and precision [18].
Analytical Challenges in Antiretroviral Drug Analysis
Chromatographic Separation Challenges
The simultaneous analysis of multiple antiretroviral drugs presents significant chromatographic challenges due to their diverse chemical structures and properties. Method development must account for co-elution issues, as demonstrated by the need for two separate calibration curves in a validated method for nine antiretroviral compounds due to co-elution of dolutegravir with raltegravir and efavirenz with lopinavir [6]. The structural diversity of antiretroviral drugs demands careful optimization of chromatographic conditions: NRTIs are small, polar molecules requiring acidic mobile phases for improved peak shape; INSTIs are more lipophilic, necessitating higher organic content or gradient elution; NNRTIs are highly hydrophobic, often requiring elevated acetonitrile concentrations; and PIs are bulky molecules demanding robust gradient methods to ensure resolution [18].
Sensitivity and Detection Considerations
The selection of detection parameters must accommodate the varied spectroscopic properties of antiretroviral drugs. Most NRTIs and NNRTIs contain highly absorbent molecular moieties that enable satisfactory UV detection, with limits of detection typically around 10 ng/mL [16]. In contrast, protease inhibitors generally exhibit lower molar absorptivities, resulting in poorer UV sensitivity [16]. Wavelength selection must be optimized for multi-drug assays, with common detection settings including 260 nm for drugs like atazanavir, dolutegravir, darunavir, efavirenz, lopinavir, raltegravir, and tipranavir, while 305 nm may be preferred for etravirine and rilpivirine [6].
Sample Preparation and Matrix Effects
Biological sample analysis introduces additional complexities, particularly with plasma proteins and other matrix components that can interfere with analysis. Solid-phase extraction (SPE) procedures have been successfully applied to plasma samples, with recovery rates ranging between 80% and 120% for antiretroviral drugs [6]. The choice of sample preparation method must consider the specific biological matrix (plasma, peripheral blood mononuclear cells, etc.) and the stability of analytes during processing and storage [16]. For intracellular drug level determination, which is particularly relevant for NRTIs as they require metabolic activation, more specialized extraction techniques are necessary to access the phosphorylated active metabolites [16].
Table 2: Key Analytical Challenges in Antiretroviral Drug Analysis
| Analytical Challenge | Impact on Method Development | Potential Solutions |
|---|---|---|
| Structural Diversity | Wide variability in polarity, solubility, and spectroscopic properties among drug classes [18]. | Gradient elution, multiple detection wavelengths, specialized sample preparation [6] [18] |
| Co-elution Issues | Simultaneous analysis of multiple drugs may result in peak overlap and quantification inaccuracies [6]. | Two-dimensional chromatography, sophisticated mobile phase optimization, staggered calibration curves [6] |
| Matrix Effects | Complex biological matrices (plasma, cells) interfere with detection and quantification [16]. | Solid-phase extraction, protein precipitation, matrix-matched calibration standards [6] [16] |
| Sensitivity Requirements | Therapeutic concentrations vary significantly between drugs (ng/mL to μg/mL) [6] [16]. | Optimized detection wavelengths, sample concentration techniques, pathlength consideration for UV detection [16] |
| Stability Concerns | Degradation during sample storage, preparation, and analysis [16]. | Controlled temperature conditions, stability-indicating methods, appropriate pH manipulation [16] |
Experimental Protocols for HPLC-UV Analysis of Antiretrovirals
Comprehensive Method for Simultaneous Analysis of Nine Antiretroviral Drugs
Materials and Reagents:
- Drug Standards: Atazanavir, dolutegravir, darunavir, efavirenz, etravirine, lopinavir, raltegravir, rilpivirine, tipranavir reference standards
- Internal Standard: Quinoxaline
- Solvents: HPLC-grade acetonitrile, methanol, dimethyl sulfoxide
- Water: Deionized water purified through Milli-Q system
- Buffer Components: Sodium acetate for 50 mM acetate buffer, pH 4.5
Chromatographic Conditions:
- Apparatus: Alliance e2695 Separation Module with 2998 photodiode array detector
- Column: XBridge C18 (4.6 mm × 150 mm, 3.5 μm) with Sentry guard column
- Column Temperature: 35°C
- Mobile Phase: Gradient of acetonitrile (A) and 50 mM acetate buffer, pH 4.5 (B)
- Flow Rate: 1 mL/min
- Detection Wavelengths: 260 nm for most analytes; 305 nm for etravirine and rilpivirine
- Injection Volume: 10 μL
- Run Time: 25 minutes
Gradient Program:
- 0-9 min: 40% A (isocratic)
- 9-16 min: Linear increase to 80% A
- 16-20 min: 80% A (isocratic)
- 20-21 min: Return to 40% A
- 21-25 min: 40% A (re-equilibration)
Sample Preparation Protocol:
- Aliquot 500 μL of plasma sample into a clean tube
- Add appropriate volume of internal standard working solution (quinoxaline, 7.5 mg/mL in methanol)
- Vortex mix for 30 seconds
- Condition SPE cartridge (C18) with 1 mL methanol followed by 1 mL water
- Apply sample to cartridge and wash with 1 mL water
- Elute analytes with 1 mL methanol
- Evaporate eluent to dryness under gentle nitrogen stream at 40°C
- Reconstitute residue in 200 μL mobile phase initial conditions
- Vortex mix for 60 seconds and transfer to HPLC vial
Calibration Standards: Prepare six-point calibration curves in drug-free plasma with concentrations optimized according to therapeutic ranges:
- Atazanavir: 60-12,000 ng/mL
- Dolutegravir: 20-8,000 ng/mL
- Darunavir: 150-15,000 ng/mL
- Efavirenz: 150-15,000 ng/mL
- Etravirine: 50-4,000 ng/mL
- Lopinavir: 150-15,000 ng/mL
- Raltegravir: 40-9,600 ng/mL
- Rilpivirine: 20-2,000 ng/mL
- Tipranavir: 500-40,000 ng/mL
Validation Parameters:
- Linearity: Coefficient of determination (r²) > 0.99 for all analytes
- Precision: Intraday and interday relative standard deviation (RSD) < 15%
- Accuracy: Mean deviation from nominal concentration < 15%
- Recovery: 80-120% for all analytes
- Specificity: No interference from endogenous plasma components
Quality Control Procedures
Quality control samples at three concentration levels (low, medium, high) should be analyzed with each batch of experimental samples. The method should demonstrate consistent performance with precision and accuracy within acceptable limits (±15%) for reliable quantification [6].
Diagram 1: HPLC-UV Analysis Workflow for Antiretroviral Drugs. This flowchart illustrates the comprehensive analytical procedure from sample preparation through method validation for the simultaneous quantification of multiple antiretroviral drugs in biological matrices.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Antiretroviral Drug Analysis
| Reagent/Material | Function in Analysis | Application Notes |
|---|---|---|
| C18 Reverse-Phase Columns (e.g., XBridge C18, 4.6 × 150 mm, 3.5 μm) | Primary separation mechanism for analytes based on hydrophobicity [6] | Compatible with wide polarity range of antiretrovirals; withstands pH variations (2-8) |
| Acetonitrile (HPLC Grade) | Organic mobile phase component for gradient elution [6] | Provides optimal separation efficiency; lower viscosity compared to methanol alternatives |
| Buffer Systems (e.g., Acetate, Phosphate) | Aqueous mobile phase component; controls ionization state of analytes [6] | Acetate buffer (pH 4.5) commonly used to suppress silanol interactions and improve peak shape |
| Solid-Phase Extraction Cartridges (C18 based) | Sample clean-up and concentration from biological matrices [6] [16] | Removes interfering plasma proteins; achieves 80-120% recovery for most antiretrovirals |
| Photodiode Array Detector | Multi-wavelength UV detection for simultaneous monitoring [6] | Enables specific wavelength selection (260 nm, 305 nm) for different drug classes |
| Internal Standards (e.g., Quinoxaline) | Normalization of extraction and injection variability [6] | Should exhibit similar extraction characteristics to analytes without co-elution |
| 3,5-Diiodopyridine | 3,5-Diiodopyridine|CAS 53710-18-2|Research Chemical | 3,5-Diiodopyridine is a versatile diiodinated pyridine building block for organic synthesis and cross-coupling. For Research Use Only. Not for human or veterinary use. |
| 2-Chloro-5-nitropyridin-4-amine | 2-Chloro-5-nitropyridin-4-amine, CAS:2604-39-9, MF:C5H4ClN3O2, MW:173.56 g/mol | Chemical Reagent |
The analysis of antiretroviral drugs presents significant challenges stemming from their structural diversity, varying physicochemical properties, and the complexity of biological matrices. HPLC-UV methods have proven to be reliable, cost-effective solutions for therapeutic drug monitoring and quality control of these essential medications. The development of robust analytical methods requires careful optimization of chromatographic conditions, sample preparation techniques, and detection parameters to address the specific challenges associated with each drug class. As fixed-dose combinations continue to evolve with newer drug entities, analytical methods must similarly advance to ensure accurate quantification and appropriate therapeutic management for HIV-infected patients. The methodologies outlined in this application note provide a foundation for reliable antiretroviral drug analysis that balances analytical performance with practical implementation considerations suitable for clinical and research laboratories.
The accurate quantification of antiretroviral drugs (ARVs) is a cornerstone of pharmaceutical research, therapeutic drug monitoring, and quality control for fixed-dose combinations. Within this analytical landscape, High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) remains a widely adopted technique due to its robustness, cost-effectiveness, and accessibility, especially in resource-limited settings [6] [18]. This review synthesizes the current state of HPLC-UV methods for ARV analysis, providing a detailed examination of developed protocols, their performance characteristics, and practical guidance for implementation. The focus on HPLC-UV is particularly relevant where advanced techniques like LC-MS/MS are not financially or technically feasible, underscoring the need for reliable, validated methods that can be deployed in diverse laboratory environments to support the global HIV treatment effort [6].
Method Development Strategies for ARV Analysis
Successful development of an HPLC-UV method for ARVs requires systematic optimization of chromatographic conditions to achieve separation, sensitivity, and efficiency.
Column Chemistry and Mobile Phase Optimization: The majority of reported methods utilize reversed-phase C18 columns [18]. Mobile phase composition is critical; most methods employ a buffer-acetonitrile gradient. A common and effective system uses acetonitrile and a 50 mM acetate buffer (e.g., at pH 4.5) to sharpen peaks and control ionization of analytes [6]. The trend towards sustainable analysis is exemplified by the development of Micellar Liquid Chromatography (MLC), which uses surfactants like sodium lauryl sulfate (SLS) to replace a significant portion of organic solvents, offering a greener alternative without compromising performance for drugs like lamivudine, dolutegravir, and tenofovir [19].
Detection Wavelength Selection: Wavelength selection is guided by the UV absorption maxima of the target analytes. Many ARVs are effectively detected at 260 nm, while others, such as etravirine and rilpivirine, require higher wavelengths (e.g., 305 nm) for optimal sensitivity [6]. For complex, multi-drug assays, the use of a photodiode array (PDA) detector is advantageous as it allows for simultaneous monitoring at multiple wavelengths and peak purity assessment [20].
Sample Preparation Techniques: For bioanalytical applications involving plasma, a solid-phase extraction (SPE) procedure is commonly implemented. This technique effectively cleans up the sample, reduces matrix interference, and improves overall method sensitivity and reliability [6].
The following diagram illustrates the logical workflow for developing and validating an HPLC-UV method for ARVs.
Quantitative Comparison of Existing HPLC-UV Methods
The performance of published HPLC-UV methods demonstrates the technique's capability for precise and accurate ARV analysis. The tables below summarize key parameters for simultaneous quantification of multiple ARVs and for specific dual/triple therapy combinations.
Table 1: HPLC-UV Method for Simultaneous Quantification of Nine ARVs in Human Plasma [6]
| Analyte | Retention Time (min) | Wavelength (nm) | Calibration Range (ng/mL) | Key Validation Results |
|---|---|---|---|---|
| Atazanavir (ATV) | 15.3 | 260 | 60 - 12,000 | R² > 0.99; Accuracy & Precision < 15% |
| Dolutegravir (DTG) | 5.4 | 260 | 20 - 8,000 | R² > 0.99; Accuracy & Precision < 15% |
| Darunavir (DRV) | 9.6 | 260 | 150 - 15,000 | R² > 0.99; Accuracy & Precision < 15% |
| Efavirenz (EFV) | 17.1 | 260 | 150 - 15,000 | R² > 0.99; Accuracy & Precision < 15% |
| Etravirine (ETV) | 17.4 | 305 | 50 - 4,000 | R² > 0.99; Accuracy & Precision < 15% |
| Lopinavir (LPV) | 17.4 | 260 | 150 - 15,000 | R² > 0.99; Accuracy & Precision < 15% |
| Raltegravir (RGV) | 5.6 | 260 | 40 - 9,600 | R² > 0.99; Accuracy & Precision < 15% |
| Rilpivirine (RPV) | 13.8 | 305 | 20 - 2,000 | R² > 0.99; Accuracy & Precision < 15% |
| Tipranavir (TPV) | 18.7 | 260 | 500 - 40,000 | R² > 0.99; Accuracy & Precision < 15% |
Table 2: Methods for Specific ARV Combinations in Pharmaceutical Formulations
| ARV Combination | Chromatographic Conditions | Performance Metrics | Reference Application |
|---|---|---|---|
| Lamivudine, Dolutegravir, Tenofovir | Column: C18 (100 x 4.6 mm, 3.5 µm)Mobile Phase: Micellar (SLS)Run Time: < 8 min | Linear (optimized range);Accuracy: ~100%;Complies with green chemistry principles | Quality control of FDC tablets [19] |
| Lamivudine, Stavudine, Nevirapine | Column: C18 (isocratic)Detection: Multi-wavelength (270, 265, 313 nm) | R² > 0.999;Accuracy: 97-103%;RSD < 5% | API content in commercial formulations [12] |
Detailed Experimental Protocols
Protocol 1: Simultaneous Assay of Nine ARVs in Plasma
This protocol is adapted from a validated method for the quantification of nine ARVs, which is particularly useful for therapeutic drug monitoring [6].
Instrumentation and Materials:
- HPLC System: Alliance e2695 Separation Module with a 2998 PDA detector or equivalent.
- Software: Empower or equivalent for data processing.
- Column: XBridge C18 (4.6 mm × 150 mm, 3.5 µm) guarded by a Sentry C18 guard column.
- Chemicals: HPLC-grade acetonitrile, methanol, and sodium acetate. Water from a Milli-Q system. Drug standards and Internal Standard (Quinoxaline).
Chromatographic Conditions:
- Mobile Phase: Solvent A: Acetonitrile. Solvent B: 50 mM Sodium Acetate Buffer, pH 4.5.
- Gradient Program:
- 0-9 min: 40% A
- 9-16 min: Ramp from 40% to 70% A
- 16-20 min: 70% A
- 20-21 min: Return to 40% A
- 21-25 min: Re-equilibrate at 40% A
- Flow Rate: 1.0 mL/min
- Column Temperature: 35 °C
- Detection: PDA, with channels at 260 nm and 305 nm.
- Injection Volume: As optimized (typically 10-100 µL).
Sample Preparation (Solid-Phase Extraction):
- Spike 500 µL of plasma sample with the internal standard solution.
- Condition and equilibrate a suitable SPE cartridge (e.g., C18) with methanol and water.
- Load the plasma sample onto the cartridge.
- Wash with water or a mild buffer to remove interfering compounds.
- Elute the analytes with a strong solvent like pure methanol or acetonitrile.
- Evaporate the eluent to dryness under a gentle stream of nitrogen.
- Reconstitute the dry residue in a suitable volume of mobile phase or a compatible solvent.
- Vortex-mix and inject into the HPLC system.
Validation Parameters:
- Linearity: Construct six-point calibration curves for each analyte. The coefficient of determination (r²) should be greater than 0.99.
- Precision and Accuracy: Assess using QC samples at low, medium, and high concentrations. Both intra-day and inter-day precision (RSD) and accuracy (% deviation) should be within ±15%.
- Recovery: Determine by comparing extracted samples with post-extraction spiked samples. Recovery should be consistent and high (e.g., 80-120%).
- Specificity: Verify that there is no interference from blank plasma at the retention times of the analytes and IS.
Protocol 2: Green Micellar LC for FDC Tablets
This protocol outlines a sustainable approach for analyzing a common triple FDC tablet, reducing the environmental impact of analysis [19].
Instrumentation and Materials:
- HPLC System: Standard HPLC system with PDA detector.
- Column: Symmetry C18 (100 × 4.6 mm, 3.5 µm).
- Chemicals: Lamivudine, Dolutegravir, and Tenofovir disoproxil fumarate standards. Sodium lauryl sulfate (SLS), orthophosphoric acid.
Chromatographic Conditions:
- Mobile Phase: 0.15 M SLS solution adjusted to pH 7 with orthophosphoric acid.
- Mode: Isocratic.
- Flow Rate: 1.0 mL/min.
- Detection: PDA, at optimized wavelengths for the three drugs (e.g., 260-270 nm).
- Injection Volume: 20 µL.
- Column Temperature: Ambient.
Sample Preparation (Tablet):
- Accurately weigh and powder not less than 20 tablets.
- Transfer an amount of powder equivalent to one tablet dose into a volumetric flask.
- Add a suitable solvent (e.g., methanol) to dissolve the active ingredients.
- Sonicate for 15-20 minutes to ensure complete dissolution.
- Dilute to volume with the same solvent and mix well.
- Filter the solution through a 0.45 µm membrane filter, discarding the first few mL of the filtrate.
- Further dilute the filtrate with mobile phase to reach the desired concentration within the linear range of the calibration curve.
Column Maintenance for MLC:
- After analysis, wash the column sequentially with water and a 50:50 mixture of methanol and water for at least 15 minutes each to prevent surfactant precipitation and preserve column life [19].
Essential Research Reagent Solutions
The following table catalogues critical reagents and materials required for developing and implementing HPLC-UV methods for ARV analysis, as derived from the cited protocols.
Table 3: Research Reagent Solutions for ARV HPLC-UV Analysis
| Reagent/Material | Function in Analysis | Specific Examples & Notes |
|---|---|---|
| C18 Analytical Columns | Reversed-phase separation of ARVs based on hydrophobicity. | XBridge C18 (150 mm, 3.5 µm) [6]; Symmetry C18 (100 mm, 3.5 µm) [19]. |
| Acetate & Ammonium Acetate Buffers | Mobile phase component to control pH, improving peak shape and retention. | 50 mM Sodium Acetate, pH 4.5 [6]; 0.01 M Ammonium Acetate, pH 4.5 [21]. |
| Solid-Phase Extraction (SPE) Cartridges | Clean-up and preconcentration of ARVs from biological matrices like plasma. | C18-based cartridges used for plasma sample preparation prior to injection [6]. |
| Micellar Agents (e.g., SLS) | Green mobile phase component; replaces organic solvents, enabling direct injection. | 0.15 M Sodium Lauryl Sulfate (SLS) at pH 7 for isocratic elution [19]. |
| Internal Standards | Correction for variability in sample preparation and injection. | Quinoxaline used for multi-ARV plasma assay [6]. |
Emerging Trends and Future Perspectives
The field of HPLC-UV analysis for ARVs continues to evolve, with several key trends emerging. There is a growing emphasis on green analytical chemistry, with methods like micellar liquid chromatography (MLC) gaining traction as sustainable alternatives that reduce hazardous solvent waste [19]. Another significant trend is the development of methods for complex drug combinations, including those used to treat co-infections such as HIV/HCV, pushing the limits of traditional HPLC-UV to ensure specificity [18] [21]. Furthermore, the application of advanced detection strategies, such as programmed fluorescence detection, offers enhanced sensitivity and selectivity for specific ARVs in complex biological matrices like urine, overcoming some limitations of UV detection [21]. These advancements ensure that HPLC-UV will remain a vital, adaptable tool in the pharmaceutical analyst's arsenal for supporting the quality and efficacy of antiretroviral therapies worldwide.
Applications in Clinical Monitoring, Pharmacokinetics, and Pharmaceutical Quality Control
The accurate and reliable quantification of antiretroviral (ARV) drugs is a critical component of pharmaceutical development, clinical pharmacology, and quality control in manufacturing. Within the broader context of research on validated HPLC-UV methods for antiretroviral drug analysis, this application note provides detailed protocols for determining drug concentrations in various matrices. The methods outlined herein are designed to support therapeutic drug monitoring, pharmacokinetic studies, and the quality assessment of pharmaceutical dosage forms, ensuring that these vital medications meet stringent standards for safety, efficacy, and quality.
Application in Pharmaceutical Quality Control
Analysis of Active Pharmaceutical Ingredients (API) in Dosage Forms
A fundamental application of HPLC-UV in the antiretroviral field is the quantification of the active pharmaceutical ingredient in finished dosage forms. A validated method for the simultaneous analysis of Lamivudine, Stavudine, and Nevirapine—a first-line antiretroviral regimen—demonstrates this application effectively.
Experimental Protocol:
- Chromatographic Column: Reversed-phase C-18 SYMMETRY column.
- Mobile Phase: Optimized based on the polarity of the molecules; delivered via isocratic elution.
- Detection Wavelengths: 270 nm for Lamivudine, 265 nm for Stavudine, and 313 nm for Nevirapine.
- Validation Parameters: The method was validated as per International Conference on Harmonization (ICH) Q2B guidelines, assessing linearity, precision, accuracy, specificity, limit of detection (LOD), and limit of quantification (LOQ) [12].
The method demonstrated excellent linearity (r² > 0.999) for all three drugs, with accuracy (recovery between 97-103%) and precision (Relative Standard Deviation, R.S.D. < 5%) [12]. This protocol ensures that commercial formulations contain the correct amount of API, a cornerstone of quality control.
Cleaning Validation in Manufacturing
Verifying the removal of drug residues from manufacturing equipment surfaces is a mandatory Good Manufacturing Practice (GMP) requirement. A validated HPLC-UV method for determining ceftriaxone sodium residues on stainless steel surfaces provides a template for similar applications in antiretroviral drug production.
Experimental Protocol:
- Sample Collection: Cotton swabs moistened with an extraction solution (50% water, 50% mobile phase) are used to swab a defined surface area.
- Chromatographic Conditions:
- Column: Hypersil ODS 5 μm (250 × 4.6 mm).
- Temperature: 50 °C.
- Mobile Phase: Acetonitrile:water:pH 7 buffer:pH 5 buffer (39:55:5.5:0.5 v/v).
- Flow Rate: 1.5 ml/min.
- Detection: 254 nm.
- Validation: The method was linear from 1.15-6.92 μg mLâ»Â¹, with swab recoveries exceeding 91% and RSD < 1.5%, proving its suitability for detecting trace-level contaminants [22].
Table 1: Validation Parameters for Quality Control HPLC-UV Methods
| Parameter | API Content Analysis [12] | Cleaning Validation [22] |
|---|---|---|
| Analytes | Lamivudine, Stavudine, Nevirapine | Ceftriaxone Sodium |
| Linearity Range | Not Specified | 1.15 - 6.92 μg mLâ»Â¹ |
| Accuracy (% Recovery) | 97 - 103% | 91.12 - 98.7% |
| Precision (RSD) | < 5% | < 1.5% |
| Key Performance Metric | Quantification of API in formulation | Detection of residue on surfaces |
Application in Clinical and Pharmacokinetic Monitoring
Advancing Therapeutic Drug Monitoring (TDM) with LC-MS/MS
While HPLC-UV is a mainstay for quality control, liquid chromatography-tandem mass spectrometry (LC-MS/MS) has become the gold standard for the bioanalysis of ARV drugs in biological fluids due to its superior sensitivity and specificity [23]. Therapeutic Drug Monitoring (TDM) is particularly valuable in managing HIV patients, especially those on complex combination therapies [23].
Experimental Protocol: UPLC-MS/MS for 16 ARV Drugs in Plasma
- Sample Preparation: Protein precipitation of 100 μL human plasma using acetonitrile containing stable isotope-labeled internal standards.
- Chromatography: Acquity UPLC system with an Acclaim TM RSLC 120 C18 column (2.1 × 100 mm, 2.2 μm).
- Mass Spectrometry: Tandem mass spectrometer operated in selected-reaction monitoring (SRM) mode, monitoring specific transitions from protonated [M+H]⺠molecules to characteristic product ions.
- Method Performance: The method was fully validated, with lower limits of quantification (LLOQ) between 2.5 and 10 ng/mL, and intra-/inter-day precision below 8.9% [24]. This high sensitivity allows for precise pharmacokinetic profiling and TDM.
Table 2: Key Classes of Antiretroviral Drugs for Bioanalysis [23]
| Drug Class | Abbreviation | Role in HIV Therapy | Example Drugs |
|---|---|---|---|
| Nucleoside Reverse Transcriptase Inhibitors | NRTI | Block the reverse transcriptase enzyme | Lamivudine, Stavudine |
| Non-Nucleoside Reverse Transcriptase Inhibitors | nNRTI | Bind to and disable reverse transcriptase | Nevirapine, Efavirenz |
| Protease Inhibitors | PI | Prevent viral maturation by inhibiting protease | Ritonavir, Lopinavir |
| Integrase Inhibitors | INI | Block the integrase enzyme | Bictegravir, Dolutegravir |
| CCR5 Inhibitors | npPI | Prevent viral entry by blocking CCR5 co-receptor | Maraviroc |
Comprehensive Experimental Protocol: Simultaneous Analysis of Antiretrovirals
The following is a detailed protocol for the simultaneous quantification of five antiviral drugs, adaptable for ARV analysis, based on a recently developed and green chemistry-analytical method.
Method Title: RP-HPLC-UV for Simultaneous Determination of Five Antiviral Drugs in Pharmaceutical Formulations.
1. Scope and Application: This method is suitable for the quantitative analysis of Favipiravir, Molnupiravir, Nirmatrelvir, Remdesivir, and Ritonavir in bulk and finished pharmaceutical dosage forms [25].
2. Materials and Equipment:
- HPLC System: With quaternary pump, auto-sampler, column thermostat, and UV-Vis/DAD detector.
- Software: For data acquisition and processing.
- Analytical Balance: For weighing reference standards and samples.
- Sonicator, pH Meter, Volumetric Glassware.
3. Chromatographic Conditions:
- Column: Hypersil BDS C18 (150 mm × 4.5 mm, 5 μm).
- Mobile Phase: Water:Methanol (30:70, v/v). Adjust pH to 3.0 with 0.1% ortho-phosphoric acid.
- Elution Mode: Isocratic.
- Flow Rate: 1.0 mL/min.
- Detection Wavelength: 230 nm.
- Injection Volume: 10 μL.
- Column Temperature: Ambient (~25 °C).
- Run Time: ~10 minutes.
4. Standard and Sample Preparation:
- Standard Stock Solutions (1 mg/mL): Accurately weigh 10 mg of each reference standard into a 10 mL volumetric flask. Dissolve and make up to volume with methanol.
- Working Standard Solutions: Dilute the stock solutions with the mobile phase or a suitable diluent to obtain concentrations within the linearity range (e.g., 10-50 μg/mL).
- Sample Preparation: For tablets/capsules, powder an equivalent of 10 mg of the API, transfer to a volumetric flask, and extract with methanol using sonication. Filter and dilute as needed.
5. System Suitability Test: Before analysis, perform a system suitability test by injecting six replicates of a standard solution. The method should meet the following pre-defined criteria:
- RSD of Peak Areas and Retention Times: ≤ 2.0%.
- Theoretical Plates: > 2000 for each peak.
- Tailing Factor: ≤ 2.0 for each peak.
- Resolution: Baseline resolution (R > 1.5) between all analyte peaks.
6. Validation Parameters (as per ICH Q2(R1)): The following parameters must be assessed and meet acceptance criteria [25] [26]:
- Specificity: No interference from blank or placebo at the retention times of the analytes.
- Linearity and Range: Minimum of 5 concentrations, with r² ≥ 0.999.
- Accuracy (% Recovery): 98-102% for assay level.
- Precision:
- Repeatability (System): RSD ≤ 2.0% for multiple injections of standard.
- Repeatability (Method): RSD ≤ 2.0% for multiple preparations of the same sample.
- Intermediate Precision: RSD ≤ 3.0% (performed on a different day, with different analyst/instrument).
- LOD and LOQ: Typically, Signal-to-Noise ratios of 3:1 and 10:1, respectively.
Diagram 1: HPLC Method Validation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for HPLC-UV Analysis of ARVs
| Item | Function / Purpose | Example / Specification |
|---|---|---|
| Chromatographic Column | Stationary phase for analyte separation. | Reversed-phase C18 (e.g., Symmetry, Hypersil BDS) [12] [25]. |
| Mobile Phase Solvents | Liquid carrier that transports the sample. | HPLC-grade Water, Acetonitrile, Methanol; often buffered to control pH [22] [25]. |
| Reference Standards | Provides known quantity of analyte for calibration and identification. | Certified Active Pharmaceutical Ingredient (API) standards [12]. |
| Placebo Formulation | Mock drug product without API. | Critical for validating specificity and accuracy in drug product methods [26]. |
| Forced Degradation Samples | Stressed samples (acid, base, oxidant, heat) of the drug product. | Used to demonstrate the stability-indicating property and specificity of the method [26]. |
| 4-(4-Methoxyphenyl)-2-methyl-4-oxobutanoic acid | 4-(4-Methoxyphenyl)-2-methyl-4-oxobutanoic acid|CAS 5717-16-8 | Buy 4-(4-Methoxyphenyl)-2-methyl-4-oxobutanoic acid (CAS 5717-16-8), a key building block for organic synthesis. For Research Use Only. Not for human or veterinary use. |
| 2-Methyl-4-(1,1,1,2,3,3,3-heptafluoro-2-propyl)aniline | 2-Methyl-4-(1,1,1,2,3,3,3-heptafluoro-2-propyl)aniline, CAS:238098-26-5, MF:C10H8F7N, MW:275.17 g/mol | Chemical Reagent |
The protocols and applications detailed in this document underscore the vital role of robust and validated analytical methods, particularly HPLC-UV, in the lifecycle management of antiretroviral drugs. From ensuring the quality of manufactured products through API and cleaning validation to enabling critical clinical and pharmacokinetic studies, these methods form the backbone of pharmaceutical analysis. The provided experimental protocols, developed and validated in accordance with international guidelines, offer researchers and drug development professionals a reliable framework for the quantitative analysis of these essential medicines, thereby supporting the global effort to combat HIV/AIDS.
A Step-by-Step Guide to Developing Robust HPLC-UV Methods for Antiretrovirals
Solid-Phase vs. Liquid-Liquid Extraction for Plasma and Formulations
The accurate quantification of pharmaceutical compounds, particularly antiretroviral drugs (ARVs), in biological fluids and formulations is crucial for therapeutic drug monitoring, pharmacokinetic studies, and quality control. Sample preparation represents a critical step in analytical methodology, with extraction efficiency and sample cleanliness directly impacting method sensitivity, accuracy, and reproducibility [27]. This application note provides a detailed comparison of two principal extraction techniques—Solid-Phase Extraction (SPE) and Liquid-Liquid Extraction (LLE)—within the context of developing a validated HPLC-UV method for antiretroviral drug analysis. We focus on practical protocols, performance data, and implementation guidelines tailored for researchers and drug development professionals.
Fundamental Principles
Solid-Phase Extraction (SPE) utilizes a cartridge containing a solid sorbent to isolate, pre-concentrate, and clean up analytes from liquid samples. The process involves four key stages: conditioning to prepare the sorbent, sample loading where analytes are retained on the sorbent, washing to remove undesired matrix components, and elution of the purified analytes with a strong solvent [27] [28]. SPE can be optimized for specific compound classes by selecting appropriate sorbent chemistry (e.g., C18 for reversed-phase applications).
Liquid-Liquid Extraction (LLE) separates compounds based on their differential solubility in two immiscible liquids, typically an aqueous sample and a water-immiscible organic solvent. The partition coefficient governs this distribution, which can be manipulated by pH adjustment (for ionizable compounds) or salt addition to enhance recovery [29] [30]. Salting-out assisted LLE utilizes high salt concentrations to separate water-miscible organic solvents (e.g., acetonitrile) from aqueous phases, creating a two-phase system that improves extraction of polar compounds [30].
Comparative Analysis of Technique Characteristics
Table 1: Comparative characteristics of SPE and LLE for antiretroviral drug analysis
| Characteristic | Solid-Phase Extraction (SPE) | Liquid-Liquid Extraction (LLE) |
|---|---|---|
| Basic Principle | Partitioning between liquid sample and solid sorbent | Partitioning between two immiscible liquids |
| Typical Solvent Consumption | Lower (e.g., 1-10 mL) [27] | Higher (e.g., 5-20 mL) [27] |
| Automation Potential | High (compatible with robotic systems) [31] | Moderate to low |
| Sample Clean-up | Excellent (multiple washing steps) [27] | Moderate (limited clean-up) |
| Hands-on Time | Moderate | Low to moderate |
| Cost per Sample | Higher (cartridge cost) | Lower (solvent cost only) |
| Suitability for Complex Matrices | Excellent (e.g., plasma, wastewater) [27] [32] | Good for less complex matrices |
| Risk of Emulsion Formation | None | Possible with certain samples [29] |
| Recovery Range | 80-120% for validated ARV methods [33] [6] [28] | Variable; can be optimized via salting-out [30] |
| Preconcentration Factor | High (e.g., 4-fold concentration) [28] | Moderate |
Experimental Protocols
Protocol 1: Solid-Phase Extraction for Antiretroviral Drugs in Plasma
This protocol is adapted from methods successfully validated for the simultaneous extraction of nine antiretroviral agents (including atazanavir, dolutegravir, darunavir, efavirenz, etravirine, lopinavir, raltegravir, rilpivirine, and tipranavir) from human plasma [33] [6] [34].
Research Reagent Solutions:
- Sorbent: C18 reversed-phase SPE cartridges (100 mg, 1 mL capacity)
- Conditioning Solvent: HPLC-grade methanol (1 mL)
- Equilibration Buffer: 150 mM ammonium acetate buffer, pH 5.0 (1 mL) [28]
- Wash Solution: 5% (v/v) methanol in 50 mM ammonium acetate buffer, pH 7.0 (1 mL) [28]
- Elution Solvent: 1.5% glacial acetic acid in methanol (400 μL) [28] or neat acetonitrile [33] [6]
- Internal Standard Solution: Quinoxaline or diazepam in methanol [33] [28]
- Mobile Phase Buffers: 50 mM sodium acetate buffer (pH 4.5) and HPLC-grade acetonitrile [6]
Step-by-Step Procedure:
- Sample Preparation: Thaw plasma samples at room temperature. For viral inactivation, heat plasma at 58°C for 60 minutes [28]. Centrifuge at 2800 rpm for 15 minutes to remove particulates.
- Internal Standard Addition: Transfer 500 μL of plasma to a clean tube. Add 100 μL of internal standard working solution and vortex mix briefly [33] [6].
- SPE Cartridge Preparation: Condition the C18 cartridge with 1 mL methanol, then equilibrate with 1 mL of 150 mM ammonium acetate buffer (pH 5.0). Do not allow the sorbent bed to dry out.
- Sample Loading: Apply the entire spiked plasma sample (600 μL) to the cartridge. Allow it to pass through the sorbent using minimal suction or gravity flow.
- Washing: Wash the cartridge with 1 mL of 5% methanol in 50 mM ammonium acetate buffer (pH 7.0) to remove interfering matrix components. Dry the sorbent bed under vacuum for ≥1 minute.
- Elution: Elute the analytes into a clean collection tube with 400 μL of 1.5% glacial acetic acid in methanol [28]. Alternatively, acetonitrile can be used as eluent [33] [6].
- Reconstitution: Evaporate the eluate to dryness under a gentle nitrogen stream at 35°C. Reconstitute the residue with 50 μL of HPLC mobile phase, vortex for 30 seconds, and centrifuge at 12,000 rpm for 3 minutes. Transfer the supernatant to an HPLC vial for analysis [28].
Protocol 2: Liquid-Liquid Extraction for Ribavirin in Plasma
This protocol validates an LLE method coupled with HPLC-UV for measuring ribavirin plasma levels in HCV-positive patients, providing a cost-effective alternative to SPE [29].
Research Reagent Solutions:
- Extraction Solvent: HPLC-grade ethyl acetate (5 mL) [29]
- Aqueous Buffer: 50 mM potassium dihydrogen phosphate buffer, pH 6.0 [29]
- Analytical Standards: Ribavirin reference standard
- Mobile Phase: 100% aqueous 50 mM potassium dihydrogen phosphate buffer, pH 6.0 [29]
Step-by-Step Procedure:
- Sample Preparation: Thaw plasma samples and centrifuge to remove any precipitates.
- Internal Standard Addition: Transfer 500 μL of plasma to a glass tube. Add internal standard if applicable.
- Extraction: Add 5 mL of ethyl acetate to the plasma sample. Vortex mix vigorously for 1-2 minutes to ensure thorough contact between phases.
- Phase Separation: Centrifuge the mixture at 3000 rpm for 5 minutes to complete phase separation.
- Organic Layer Collection: Transfer the upper organic layer to a clean glass tube using a Pasteur pipette.
- Evaporation: Evaporate the organic extract to dryness under a gentle nitrogen stream at room temperature.
- Reconstitution: Reconstitute the dry residue in 100 μL of 50 mM potassium dihydrogen phosphate buffer (pH 6.0). Vortex mix thoroughly and transfer to an HPLC vial for analysis.
Salting-Out Assisted LLE (SALLE) Technique
Salting-out assisted LLE represents a hybrid approach that enhances traditional LLE for polar compounds [30].
Procedure:
- Sample Preparation: Transfer 100 μL of plasma to a microcentrifuge tube.
- Protein Precipitation: Add 200 μL of acetonitrile, vortex vigorously for 30 seconds, and centrifuge to pellet proteins.
- Salting-Out: Transfer the supernatant to a new tube containing 50 μL of 2 M magnesium sulfate (or ammonium acetate). Vortex briefly.
- Phase Separation: Centrifuge to achieve phase separation (the acetonitrile layer will form the upper phase).
- Analysis: Collect the upper organic layer for direct analysis or further processing [30].
Application Data and Performance Comparison
Quantitative Performance in Antiretroviral Drug Analysis
Table 2: Performance data of extraction techniques for antiretroviral drugs in biological samples
| Analyte Class | Extraction Technique | Recovery (%) | Precision (RSD%) | Linearity (r²) | Limit of Quantification | Reference |
|---|---|---|---|---|---|---|
| 9 ARVs (e.g., ATV, DTG, DRV) | SPE (C18) | 80-120% | <15% | >0.99 | Varies by drug (e.g., 20 ng/mL for DTG) | [33] [6] |
| Raltegravir | SPE (C18) | ~90% | 1.4-7.9% | >0.99 | 20 ng/mL | [28] |
| NVP, EFV, NFV | SPE-DLLME | High (method specific) | Not specified | Satisfactory | Trace levels | [27] |
| Ribavirin | LLE (Ethyl Acetate) | Not specified | <15% | >0.99 | 500 ng/mL | [29] |
| Lopinavir/Ritonavir | SALLE (ACN/MgSOâ‚„) | 62-84% | 2.7-6.5% | Not specified | Not specified | [30] |
Optimization Strategies
SPE Optimization:
- Ionic Strength and pH: Adjust loading buffer conditions to maximize analyte retention. For raltegravir, 150 mM ammonium acetate (pH 5.0) was optimal [28].
- Selective Washing: Implement a wash step with 5% methanol to remove interfering compounds without eluting targets [28].
- Efficient Elution: Use 1.5% glacial acetic acid in methanol for complete elution of basic compounds [28].
LLE Optimization:
- Solvent Selection: Choose solvents with appropriate polarity for target compounds. Ethyl acetate works well for medium-polarity drugs like ribavirin [29].
- Salting-Out Effect: Add salts (e.g., MgSOâ‚„, NaCl) to decrease analyte solubility in the aqueous phase and improve partitioning into the organic phase [30].
- pH Adjustment: Modify pH to suppress ionization of acidic or basic compounds, enhancing their extraction into organic solvents.
Workflow Integration and Analytical Considerations
HPLC-UV Analysis of Extracted Samples
Following extraction, samples are typically analyzed using reversed-phase HPLC with UV detection. The method developed for nine ARVs employs the following conditions [33] [6]:
- Column: XBridge C18 (150 mm × 4.6 mm, 3.5 μm)
- Mobile Phase: Gradient of acetonitrile and 50 mM acetate buffer (pH 4.5)
- Flow Rate: 1 mL/min
- Detection: Dual wavelengths: 260 nm (most ARVs) and 305 nm (etravirine, rilpivirine)
- Run Time: 25 minutes
Technique Selection Guidelines
The choice between SPE and LLE depends on multiple factors:
- Choose SPE when: Analyzing complex matrices, high sensitivity is required, sample clean-up is crucial, and automation is desired [27] [28].
- Choose LLE when: Processing limited sample numbers, budget constraints exist, methods require rapid implementation, and adequate sensitivity can be achieved with simpler methodology [29].
- Consider SALLE when: Extracting polar compounds that partition poorly into traditional water-immiscible organic solvents [30].
Visualized Workflows
Solid-Phase Extraction Workflow
Liquid-Liquid Extraction Workflow
Both SPE and LLE offer effective sample preparation solutions for the analysis of antiretroviral drugs in plasma and formulations. SPE provides superior clean-up, higher preconcentration factors, and better automation capability, making it ideal for complex matrices and multi-analyte methods [27] [33] [28]. LLE offers simplicity, lower cost, and avoids cartridge variability, making it suitable for single-analyte methods with less complex matrices [29] [30]. The choice between these techniques should be guided by specific analytical requirements, available resources, and the required sensitivity and precision for the intended application.
The selection of an appropriate chromatographic column is a pivotal step in developing a robust and selective High-Performance Liquid Chromatography (HPLC) method for the analysis of antiretroviral drugs (ARVs). Within the context of a broader thesis on validated HPLC-UV methods for ARV analysis, this document provides detailed application notes and protocols to guide researchers, scientists, and drug development professionals. The stationary phase dictates the selectivity, efficiency, and resolution of the separation by engaging in specific chemical interactions with analyte molecules. A fundamental understanding of these interactions is essential for effective method development, particularly for complex matrices and combination therapies common in HIV treatment. This guide synthesizes practical strategies with theoretical principles to facilitate optimal column selection for ARV analysis.
Theoretical Foundations of Stationary Phase Selectivity
The Hydrophobic-Subtraction Model
The Hydrophobic-Subtraction (H-S) Model provides a quantitative framework for understanding and comparing the selectivity of reversed-phase (RP) columns. According to this model, five primary interactions govern solute retention and column selectivity [35].
- Hydrophobic Interaction (H-term): This is the dominant retention mechanism, involving the van der Waals dispersion forces between the non-polar regions of the solute molecule and the alkyl chains (e.g., C18, C8) of the stationary phase.
- Steric Resistance (S*-term): Also known as "shape selectivity," this interaction describes the resistance to penetration of bulky solute molecules into the bonded phase, which is influenced by the ligand density and structure of the stationary phase.
- Hydrogen-Bonding Acidity (A-term): This represents the interaction of basic solutes with acidic, un-derivatized silanol groups on the silica surface.
- Hydrogen-Bonding Basicity (B-term): This represents the interaction of acidic solutes with basic (ionized) silanol groups or other basic groups in the stationary phase.
- Cation Exchange (C-term): This occurs at low pH, where ionized basic solutes interact with ionized silanol groups.
The H-S model allows for the quantitative comparison of columns. Two columns with similar H, S*, A, B, and C parameters are considered equivalent and can be substituted for one another. Conversely, columns with significantly different parameters are orthogonal and can be exploited during method development to resolve challenging peak pairs [35].
Visualization of the Hydrophobic-Subtraction Model
The following diagram illustrates the five key solute-column interactions described by the H-S model.
Application Notes: Column Selection for Antiretroviral Drug Analysis
Antiretroviral drugs encompass a range of chemical classes with diverse physicochemical properties, necessitating a strategic approach to column selection. The following section outlines practical protocols and considerations.
Protocol: A Systematic Approach to Column Screening
Objective: To establish a baseline separation for a mixture of antiretroviral drugs using a systematic column screening strategy.
Workflow Overview: The following diagram outlines the key decision points in the column selection and method development process.
Materials and Reagents:
- Columns for Screening: C18, C8, Phenyl, Cyano (CN)
- Mobile Phase Solvents: HPLC-grade water, acetonitrile, methanol, ethanol, buffer salts (e.g., potassium phosphate, ammonium acetate, sodium acetate).
- ARV Standards: Certified reference standards of the target analytes (e.g., Lamivudine, Dolutegravir, Tenofovir alafenamide, Efavirenz, etc.).
- Equipment: HPLC system equipped with a UV-Vis/DAD detector, vacuum degasser, and auto-sampler.
Procedure:
- Primary Screening on C18: Begin method development on a high-purity, silica-based C18 column (e.g., 150-250 mm x 4.6 mm, 5 µm). This is the most versatile and widely used stationary phase. Use a generic gradient from 5% to 95% organic modifier (acetonitrile or methanol) over 20-30 minutes with a neutral phosphate buffer.
- Evaluation: Assess the chromatogram for resolution (Rs > 1.5), peak shape, and run time.
- Optimization on C18: If separation is inadequate, optimize the method by:
- Adjusting the mobile phase pH to suppress the ionization of acidic/basic analytes.
- Fine-tuning the gradient profile.
- Changing the organic modifier (acetonitrile often provides different selectivity than methanol).
- Increasing the column temperature.
- Secondary Screening with Orthogonal Phases: If optimization on C18 does not yield the desired separation, screen columns with different selectivity. Consult the H-S model to select an orthogonal phase [35]. For example:
- C8: For moderately hydrophobic ARVs or to reduce retention time while maintaining similar selectivity to C18.
- Phenyl: Can provide enhanced selectivity for analytes with aromatic rings or conjugated systems through π-π interactions.
- Cyano (CN): A versatile phase with mixed-mode properties (reversed-phase and weak normal-phase). Useful for polar ARVs and can offer highly orthogonal selectivity [36].
Comparative Performance of Stationary Phases for ARV Analysis
The table below summarizes the typical application and performance of various stationary phases in the analysis of antiretroviral drugs, based on published methods.
Table 1: Comparison of Stationary Phases for Antiretroviral Drug Analysis
| Stationary Phase | Key Interactions | Recommended Application for ARVs | Example ARVs Analyzed | Performance Notes |
|---|---|---|---|---|
| C18 (Octadecyl) | Hydrophobic | Broad-spectrum; first choice for most ARVs; analysis of combination tablets and plasma samples. | Lamivudine, Stavudine, Nevirapine [12], Atazanavir, Darunavir, Lopinavir, Ritonavir [6] [37] | Provides strong retention for hydrophobic drugs. Robust and reproducible. |
| C8 (Octyl) | Hydrophobic (weaker than C18) | Analysis of moderately hydrophobic ARVs; when shorter run times are desired. | Similar profile to C18, but with shorter retention. | Good alternative to C18 if retention is too strong. |
| Phenyl | Hydrophobic, π-π | Separation of ARVs with aromatic rings; often orthogonal to C18. | Efavirenz, Etravirine, Rilpivirine | Can resolve co-eluting peaks from C18 methods. |
| Cyano (CN) | Hydrophobic, Dipole-Dipole, H-Bonding | Polar ARVs; green chromatography with aqueous micellar mobile phases; highly orthogonal selectivity. | Lamivudine, Dolutegravir, Tenofovir alafenamide [36] | Useful for mixed-mode separations. Less retentive than C18/C8. |
Case Study: Development of a Green HPLC-UV Method for Nine ARVs
Background: The development of a single HPLC-UV method for the simultaneous quantification of nine ARVs (Atazanavir, Dolutegravir, Darunavir, Efavirenz, Etravirine, Lopinavir, Raltegravir, Rilpivirine, Tipranavir) in human plasma for therapeutic drug monitoring [6].
Validated Protocol:
- Column: XBridge C18 (150 mm x 4.6 mm, 3.5 µm).
- Mobile Phase: Gradient elution with Solvent A: 50 mM acetate buffer (pH 4.5) and Solvent B: acetonitrile.
- Gradient Program: Initial 40% B for 9 min, then linearly increased to 70% B over 7 min.
- Detection: Dual-wavelength UV: 260 nm for most drugs; 305 nm for Etravirine and Rilpivirine.
- Sample Preparation: Solid-phase extraction (SPE) of 500 µL plasma aliquots.
- Validation: The method was validated over wide calibration ranges (e.g., 20-8000 ng/mL for Dolutegravir) with accuracy and precision (RSD) within ±15%, demonstrating its suitability for clinical TDM [6].
Key Insight: This protocol highlights the capability of a carefully optimized C18 method to resolve a complex mixture of ARVs with diverse structures. The use of a pH-controlled buffer and a multi-step gradient was critical to achieving baseline separation for all nine analytes.
Case Study: Computational-Assisted Green Method for COVID-19 Antiviral
Background: While not an ARV, the development of a green HPLC-UV method for the COVID-19 drug combination Nirmatrelvir/Ritonavir provides a valuable example of computational-assisted column selection [37].
Validated Protocol:
- Computational Screening: Density functional theory (DFT) calculations were used to predict the binding energy of the drugs with C8, C18, and Cyano stationary phases. The C18 column showed the strongest interaction and was selected for the method [37].
- Column: BDS Hypersil C18 (250 mm x 4.6 mm, 5 µm).
- Mobile Phase: Ethanol:Water (80:20, v/v). Ethanol was chosen as a less toxic, green alternative to acetonitrile or methanol.
- Detection: UV at 215 nm.
- Chromatographic Performance: The method achieved baseline separation with retention times of 4.9 min for Nirmatrelvir and 6.8 min for Ritonavir, demonstrating that green solvents can be effectively employed without compromising performance [37].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials required for the development and validation of HPLC-UV methods for antiretroviral drug analysis.
Table 2: Essential Research Reagents and Materials for ARV HPLC-UV Analysis
| Item | Function/Application | Specific Examples / Notes |
|---|---|---|
| C18 Column | Workhorse stationary phase for reversed-phase separation of most ARVs. | High-purity silica, end-capped (e.g., XBridge C18, Symmetry C18) [12] [6]. |
| Orthogonal Columns (C8, Phenyl, Cyano) | Secondary screening to resolve co-eluting peaks; method development. | Zorbax Bonus RP (differing selectivity) [35], Cyano columns for green micellar LC [36]. |
| HPLC-Grade Solvents | Mobile phase constituents; sample and standard preparation. | Acetonitrile, Methanol, Ethanol (green alternative) [37], Water. |
| Buffer Salts | Control of mobile phase pH and ionic strength to modulate selectivity and peak shape. | Sodium/Potassium Phosphate, Ammonium Acetate, Sodium Acetate. Use HPLC-grade. |
| Drug Reference Standards | Qualitative and quantitative analysis; method calibration. | Certified standards from pharmaceutical manufacturers or suppliers (e.g., Pfizer, Janssen Cilag) [6] [37]. |
| Internal Standard | Correction for injection volume and sample preparation variability. | Quinoxaline [6], or a structurally similar analog not present in the sample. |
| Solid-Phase Extraction (SPE) Cartridges | Sample clean-up and pre-concentration for biological matrices (e.g., plasma). | Reverse-phase C18 SPE cartridges are commonly used [6]. |
| 5,5,8,8-Tetramethyl-5,6,7,8-tetrahydronaphthalen-2-amine | 5,5,8,8-Tetramethyl-5,6,7,8-tetrahydronaphthalen-2-amine, CAS:92050-16-3, MF:C14H21N, MW:203.32 g/mol | Chemical Reagent |
| 3-Chloro-2-methylphenyl methyl sulfide | 3-Chloro-2-methylphenyl methyl sulfide, CAS:82961-52-2, MF:C8H9ClS, MW:172.68 g/mol | Chemical Reagent |
The strategic selection of a chromatographic column is fundamental to the success of an HPLC-UV method for antiretroviral drug analysis. A systematic approach, beginning with a standard C18 column and progressing to orthogonal phases like phenyl or cyano when necessary, is highly effective. The Hydrophobic-Subtraction Model provides a powerful theoretical foundation for understanding and comparing column selectivity. Furthermore, the integration of modern strategies—such as computational pre-screening and the adoption of greener solvents like ethanol—can enhance both the efficiency and environmental friendliness of analytical methods. The protocols and application notes detailed herein provide a validated roadmap for developing robust, reliable, and selective methods suitable for pharmaceutical quality control and therapeutic drug monitoring of antiretroviral agents.
In the development of a validated High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) method for antiretroviral drug analysis, mobile phase optimization represents the most critical parameter controlling retention, selectivity, and peak shape. The mobile phase in reversed-phase chromatography serves not merely as a carrier but as an active participant in the separation mechanism, influencing hydrophobic, ionic, and secondary interactions between analytes and the stationary phase. For pharmaceutical analysts developing stability-indicating methods for complex drug matrices, strategic manipulation of the aqueous buffer composition, pH, and organic modifier selection enables resolution of co-eluted peaks, enhances detection sensitivity, and ensures method robustness for quality control applications [38]. This application note provides a systematic framework for mobile phase optimization, contextualized within antiretroviral drug analysis and supported by experimental protocols and validation data.
Theoretical Foundations of Mobile Phase Design
Role of Buffer Composition and pH
The aqueous component (Mobile Phase A) in reversed-phase HPLC typically contains buffers or pH modifiers to control the ionization state of analytes. For ionizable compounds, which constitute most pharmaceutical substances, the pH of the mobile phase determines whether molecules exist in ionized or non-ionized forms, dramatically impacting retention. The ionized species consistently elute earlier than their non-ionized counterparts in reversed-phase systems due to reduced hydrophobicity [39]. Effective buffering is essential within ±1 pH unit of the buffer's pKa to resist pH changes during method execution, thereby ensuring retention time reproducibility [39] [38].
The buffer capacity, a function of buffer concentration, must be sufficient to withstand deliberate pH changes; generally, concentrations between 5-100 mM are employed, with lower limits (≥5 mM) ensuring adequate buffering capability and upper limits (<100 mM) avoiding pump seal wear and precipitation risks [39]. For analytes with ionizable functional groups, selecting a mobile phase pH at least 2 units away from the analyte pKa prevents peak splitting or shouldering caused by the simultaneous presence of both ionic species [39]. When separating multiple ionizable analytes, the optimal pH value is one where all analytes exist predominantly in the same form, either ionized or non-ionized, to achieve predictable retention behavior.
Organic Modifier Selection and Selectivity
The organic solvent (Mobile Phase B) primarily governs retention strength and selectivity through solvophobic interactions. Acetonitrile, methanol, and tetrahydrofuran constitute the three most common modifiers, each possessing distinct chromatographic properties due to differences in their proton acceptor/donor capabilities and dipole interactions [38]. Acetonitrile exhibits stronger elution strength than methanol and produces lower system backpressure due to its lower viscosity (0.37 cP for acetonitrile versus 0.55 cP for methanol), often resulting in higher column efficiency [40] [38]. However, methanol frequently provides superior selectivity for specific analyte classes, particularly those containing acidic functional groups, as demonstrated in cannabinoid separations where acidic compounds showed disproportionately increased retention with methanol compared to acetonitrile, even at matched elution strengths [40].
Table 1: Properties of Common Organic Modifiers in Reversed-Phase HPLC
| Organic Modifier | Elution Strength | Viscosity (cP) | UV Cutoff (nm) | Protic/Aprotic | Selectivity Characteristics |
|---|---|---|---|---|---|
| Acetonitrile | High | 0.37 | 190 | Aprotic | Differentiates based on hydrophobicity and π-π interactions |
| Methanol | Medium | 0.55 | 210 | Protic | Differentiates based on hydrogen bonding capability |
| Tetrahydrofuran | Very High | 0.51 | 220 | Aprotic | Strong solubilizing power, alternative selectivity |
MS-Compatible versus UV-Optimized Mobile Phases
Detector compatibility fundamentally dictates mobile phase selection. Mass spectrometric detection requires volatile additives such as ammonium formate, ammonium acetate, formic acid, or acetic acid [39] [38]. Conversely, UV detection allows non-volatile buffers like phosphate, which offer superior UV transparency down to 200 nm, enabling low-wavelength detection for compounds with weak chromophores [41]. The recent trend toward simplified mobile phases using binary solvents with linear gradients enhances method robustness and facilitates transfer between laboratories [38].
Experimental Protocols for Systematic Optimization
Protocol 1: Buffer pH Scouting Gradient
Purpose: To identify the optimal aqueous pH for separation of ionizable antiretroviral compounds.
Materials:
- HPLC system with UV detector and column oven
- C18 or similar reversed-phase column (e.g., 150 mm × 4.6 mm, 5 µm)
- Stock solutions of all analytes (e.g., 1 mg/mL in methanol)
- Buffer components: phosphoric acid, formic acid, acetic acid, ammonium hydroxide
- pH meter with aqueous buffer calibration
Procedure:
- Prepare 1 L each of aqueous mobile phases at pH 2.2, 3.0, 4.5, 7.0, and 10.0 using appropriate buffers:
- pH 2.2: 50 mM potassium dihydrogen phosphate, adjust with ortho-phosphoric acid [42]
- pH 3.0: 0.1% ortho-phosphoric acid in water [25]
- pH 4.5-5.0: 10 mM ammonium acetate, adjust with acetic acid [43]
- pH 7.0: 10 mM potassium phosphate buffer
- pH 10.0: 10 mM ammonium carbonate, adjust with ammonium hydroxide [41]
Filter all mobile phases through 0.45 µm membrane and degas.
Set organic modifier to acetonitrile for initial scouting.
Program a linear gradient from 5% to 95% organic phase over 20 minutes at 1.0 mL/min flow rate.
Maintain column temperature at 30-40°C and detection wavelength at 230-260 nm for antiretroviral drugs [25] [44].
Inject analyte mixture and record chromatograms at each pH.
Evaluate results based on retention factor (k > 2), resolution (Rs > 1.5), and peak symmetry.
Analysis: Plot retention time versus pH for each analyte. Identify the pH region providing optimal resolution and acceptable peak shape for all components.
Protocol 2: Organic Modifier Selectivity Evaluation
Purpose: To assess selectivity differences between acetonitrile and methanol for resolving critical pairs.
Materials:
- HPLC system with programmable gradient and auto-sampler
- C18 column (150 mm × 4.6 mm, 5 µm)
- Stock solutions of analytes in methanol or acetonitrile
- Mobile phase additives: formic acid, ammonium formate, phosphoric acid
Procedure:
- Prepare mobile phase A with optimized pH from Protocol 1.
- Prepare mobile phase B variants:
- Acetonitrile with same additive as Mobile Phase A
- Methanol with same additive as Mobile Phase A
- For isocratic screening, estimate starting organic percentage based on elution strength equivalency: 44% methanol ≈ 35% acetonitrile ≈ 28% tetrahydrofuran [38].
- Perform initial isocratic runs with acetonitrile and methanol at equivalent elution strengths.
- If critical pairs remain unresolved, implement a shallow gradient around the isocratic point (e.g., ±15% organic over 10 minutes).
- For challenging separations, evaluate ternary mixtures (e.g., acetonitrile-methanol-water) [45].
- Record retention times, resolution values, and peak asymmetries for all analytes.
Analysis: Compare selectivity factors (α) between organic modifiers for critical peak pairs. Note any elution order changes indicating significant selectivity differences.
Protocol 3: Buffer Ionic Strength and Additive Concentration Optimization
Purpose: To fine-tune peak shape and efficiency through buffer concentration adjustment.
Materials:
- HPLC system with column oven
- Selected column chemistry from previous protocols
- Concentrated buffer stock solutions
- Organic modifier selected from Protocol 2
Procedure:
- Prepare mobile phases with buffer concentrations of 5, 10, 25, and 50 mM while maintaining constant pH.
- For ionizable basic compounds, include higher concentrations (up to 100 mM) to suppress silanol interactions [38].
- Employ isocratic conditions determined from previous optimization at a k value of approximately 5 for the mid-retained analyte.
- Inject analyte mixture and measure peak symmetry, efficiency (theoretical plates), and retention time reproducibility.
- Assess buffer solubility in organic-water mixtures by visual inspection for precipitation after preparation.
- For MS-compatible methods, ensure buffer concentration ≤50 mM to prevent source contamination [39].
Analysis: Plot theoretical plates and peak asymmetry factor versus buffer concentration. Select the lowest concentration providing acceptable peak shape and reproducibility.
Application Case Study: Simultaneous Analysis of COVID-19 Antiviral Drugs
Optimized Method Parameters
A recent study demonstrated simultaneous determination of five COVID-19 antiviral drugs (favipiravir, molnupiravir, nirmatrelvir, remdesivir, and ritonavir) using an optimized RP-HPLC method [25]. The final conditions exemplify evidence-based mobile phase optimization:
- Column: Hypersil BDS C18 (150 mm × 4.5 mm, 5 µm)
- Mobile Phase: Water:methanol (30:70 v/v), pH 3.0 adjusted with 0.1% ortho-phosphoric acid
- Flow Rate: 1.0 mL/min
- Detection: UV at 230 nm
- Temperature: Ambient
- Injection Volume: 10 µL
This method achieved baseline resolution of all five compounds with retention times of 1.23, 1.79, 2.47, 2.86, and 4.34 min for favipiravir, molnupiravir, nirmatrelvir, remdesivir, and ritonavir, respectively [25]. The selection of methanol over acetonitrile as organic modifier provided the necessary selectivity for these structurally diverse antiretroviral compounds, while the acidic pH (3.0) ensured protonation of basic functional groups and suppression of silanol interactions.
Method Validation Data
Table 2: Validation Parameters for Simultaneous Antiviral Drug Analysis [25]
| Parameter | Favipiravir | Molnupiravir | Nirmatrelvir | Remdesivir | Ritonavir |
|---|---|---|---|---|---|
| Linearity Range (µg/mL) | 10-50 | 10-50 | 10-50 | 10-50 | 10-50 |
| Correlation Coefficient (r²) | ≥0.9997 | ≥0.9997 | ≥0.9997 | ≥0.9997 | ≥0.9997 |
| LOD (µg/mL) | 0.415 | 0.502 | 0.946 | 0.723 | 0.685 |
| LOQ (µg/mL) | 1.260 | 1.523 | 2.868 | 2.190 | 2.077 |
| Trueness (%) | 99.59-100.08 | 99.59-100.08 | 99.59-100.08 | 99.59-100.08 | 99.59-100.08 |
| Precision (RSD%) | <1.1 | <1.1 | <1.1 | <1.1 | <1.1 |
| Recovery from Formulations (%) | 99.98-100.7 | 99.98-100.7 | 99.98-100.7 | 99.98-100.7 | 99.98-100.7 |
The method demonstrated excellent greenness metrics with AGREE score of 0.70 and practicality assessments confirming environmental friendliness and practical applicability for routine pharmaceutical quality control [25].
Mobile Phase Optimization Workflow
The following diagram illustrates the systematic approach to mobile phase optimization for HPLC-UV method development:
Systematic Mobile Phase Optimization Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for HPLC Mobile Phase Optimization
| Reagent Category | Specific Examples | Function in Mobile Phase | Application Notes |
|---|---|---|---|
| Organic Modifiers | Acetonitrile, Methanol, Ethanol | Control retention and selectivity through solvophobic interactions | Acetonitrile for efficiency, methanol for alternative selectivity, ethanol for green alternatives [45] |
| Acidic Additives | Trifluoroacetic Acid (0.05-0.1%), Formic Acid (0.1%), Phosphoric Acid (0.1%) | Suppress silanol interactions, control ionization of basic analytes | TFA provides excellent peak shape for basics; Formic acid is MS-compatible; Phosphoric acid offers low UV cutoff [38] |
| Volatile Buffers | Ammonium Acetate (5-50 mM), Ammonium Formate (5-50 mM), Ammonium Carbonate (5-50 mM) | Provide pH control and ionic strength for MS-compatible methods | Ammonium acetate pH 3-7; Ammonium carbonate pH 8-11; Formate may absorb at low UV [41] |
| UV-Transparent Buffers | Potassium Phosphate (5-50 mM), Sodium Phosphate (5-50 mM) | Enable low-wavelength detection (200-210 nm) for weak chromophores | Non-volatile, not MS-compatible; Excellent buffer capacity at pH 2.1, 7.2, 12.3 [41] |
| pH Adjustment | Ortho-Phosphoric Acid, Ammonium Hydroxide, Sodium Hydroxide | Fine-tuning of mobile phase pH to optimize ionization state | Always measure pH before organic addition; Use high-purity reagents to minimize UV background [39] |
| (3-Chloro-2-methylphenyl)methanol | (3-Chloro-2-methylphenyl)methanol, CAS:90369-75-8, MF:C8H9ClO, MW:156.61 g/mol | Chemical Reagent | Bench Chemicals |
| 6-Methoxy-1H-indole-3-carboxylic acid | 6-Methoxy-1H-indole-3-carboxylic acid, CAS:90924-43-9, MF:C10H9NO3, MW:191.18 g/mol | Chemical Reagent | Bench Chemicals |
Advanced Considerations and Troubleshooting
Managing Baseline Drift and Detection Artifacts
UV-absorbing buffers cause significant baseline drift during gradient elution, particularly at low wavelengths. For example, 25 mM ammonium formate (pH 3.2) exhibits strong absorbance below 230 nm, while phosphate buffers remain transparent to 200 nm [41]. To minimize drift with UV-absorbing additives: (1) use the lowest effective buffer concentration, (2) employ matching additive concentrations in both mobile phases A and B, and (3) select detection wavelengths above the buffer's UV cutoff when feasible.
Solvent Strength Matching for Method Transfer
When converting methods between acetonitrile and methanol, equivalent elution strength compositions can be estimated using established tables (44% methanol ≈ 35% acetonitrile) [38]. However, selectivity differences may persist even at matched elution strengths, particularly for compounds with hydrogen bonding capabilities [40]. Always verify resolution of critical pairs after solvent substitution.
Green Chemistry Considerations
The pharmaceutical industry's increasing emphasis on environmental responsibility encourages substitution of acetonitrile with less toxic alternatives like ethanol or methanol [45]. While these substitutes may increase backpressure due to higher viscosity, they often provide complementary selectivity and reduce environmental impact. Method greenness can be evaluated using standardized metrics like AGREE and GAPI, as demonstrated in the antiviral drug analysis which scored 0.70 on the AGREE scale [25].
Systematic optimization of mobile phase composition represents a fundamental requirement for developing robust, reproducible HPLC-UV methods for antiretroviral drug analysis. Through strategic manipulation of buffer pH, organic modifier selection, and additive concentration, method developers can achieve optimal resolution of complex drug mixtures while ensuring method reliability for quality control applications. The experimental protocols and case studies presented herein provide a structured framework for method development that balances separation efficiency, detection sensitivity, and practical implementation in pharmaceutical analysis laboratories.
Developing Gradient vs. Isocratic Elution Methods for Multi-Drug Analysis
The analysis of multiple antiretroviral drugs in a single run is a cornerstone of modern therapeutic drug monitoring (TDM) and clinical research for human immunodeficiency virus (HIV) infection. High-performance liquid chromatography with ultraviolet detection (HPLC-UV) remains a widely accessible and cost-effective technique for this purpose, particularly in clinical laboratory settings [6] [9]. A critical decision in developing such multi-analyte methods is the choice of elution mode—isocratic, which uses a constant mobile phase composition, or gradient, which systematically changes the mobile phase strength during the analysis [46] [47]. The complexity of antiretroviral drug regimens, often involving compounds with a wide range of polarities and chemical properties, makes this choice paramount for achieving efficient separation, accurate quantification, and timely analysis [6] [33]. This application note provides a detailed comparison of these two elution strategies, framed within the context of developing a validated HPLC-UV method for the simultaneous quantification of antiretroviral agents, to guide researchers and drug development professionals in selecting and optimizing the appropriate chromatographic approach.
Theoretical Background: Elution Modes in HPLC
Isocratic Elution
Isocratic elution is characterized by a constant mobile phase composition throughout the entire chromatographic run. This mode employs a single solvent or a consistent mixture of solvents, maintaining a uniform elution strength from injection to detection [46] [48].
- Mechanism and Advantages: The primary strength of isocratic elution lies in its simplicity. It is easier to set up and requires less sophisticated instrumentation. The constant conditions typically lead to a stable baseline, which facilitates peak integration and quantification. Furthermore, because the mobile phase does not change, the column does not require a lengthy re-equilibration time between runs, potentially increasing throughput. Its operational costs are generally lower due to reduced solvent consumption and simpler pump requirements [48] [47].
- Limitations and Challenges: The major drawback of isocratic elution becomes apparent when analyzing complex mixtures with components of widely differing polarities. Under constant conditions, highly retained compounds may exhibit excessively long retention times, broad peaks, and poor detection sensitivity. This often results in the "general elution problem," where early-eluting peaks may be co-eluted and poorly resolved, while late-eluting peaks are broad and dilute [46] [49].
Gradient Elution
Gradient elution involves a programmed change in the mobile phase composition during the analytical separation. This is typically achieved by progressively increasing the percentage of a stronger, less polar solvent (e.g., acetonitrile or methanol) in a mixture with a weaker, more polar solvent (e.g., aqueous buffer) [46] [47].
- Mechanism and Advantages: By starting with a weaker solvent, the gradient method ensures that all analytes are well-retained at the head of the column. As the solvent strength increases, it accelerates the elution of more strongly retained compounds. This process compresses the analyte bands, leading to sharper peaks, improved signal-to-noise ratios, and better resolution across a wide range of compound polarities. It is exceptionally well-suited for complex samples and can significantly reduce total run time compared to an isocratic method struggling to elute all components [46] [49] [47].
- Limitations and Challenges: The primary disadvantages of gradient elution are its higher complexity and cost. It requires more sophisticated instrumentation, including high-pressure mixing pumps, and the method development process is more intricate. A mandatory column re-equilibration step to the initial mobile phase conditions is required between runs, which adds to the total cycle time. There is also a potential for baseline drift due to changing UV absorption of the solvents, and it generally consumes a larger volume of solvents [48] [47].
Decision Workflow: Choosing the Appropriate Elution Mode
The following diagram outlines a systematic approach for selecting between isocratic and gradient elution based on sample and analytical requirements.
Application in Antiretroviral Drug Analysis
A Case Study: Simultaneous Analysis of Nine Antiretroviral Drugs
The development of an HPLC-UV method for the simultaneous quantification of nine antiretroviral drugs—atazanavir (ATV), dolutegravir (DTG), darunavir (DRV), efavirenz (EFV), etravirine (ETV), lopinavir (LPV), raltegravir (RGV), rilpivirine (RPV), and tipranavir (TPV)—serves as a prime example of the necessity of gradient elution for complex multi-drug analysis [6] [33].
- Chromatographic Challenge: These drugs exhibit a wide range of chemical properties and polarities, making isocratic separation impractical. Specifically, the method faced issues of co-elution, such as DTG with RGV and EFV with LPV, which could only be resolved by implementing two separate, optimized gradient programs [6].
- Implemented Gradient Method: The successful separation was achieved on a C18 reverse-phase column using a gradient of acetonitrile and sodium acetate buffer (pH 4.5) delivered at a flow rate of 1 mL/min over a 25-minute total run time. The gradient started at 40% acetonitrile, maintained for 9 minutes, and was then increased to a higher percentage over the next 7 minutes to elute the more retained compounds [6].
- Performance and Validation: The method was rigorously validated, demonstrating a coefficient of determination (r²) greater than 0.99 for all analytes across their respective therapeutic ranges. Both intra-day and inter-day precision (RSD) were less than 15.0%, and accuracy was also within ±15.0% of the nominal concentrations. The extraction recovery ranged between 80% and 120% for all drugs, confirming the method's reliability for clinical trials and TDM [6] [33].
Quantitative Data from Validated Method
Table 1: Retention times, detection wavelengths, and calibration ranges for nine antiretroviral drugs analyzed by HPLC-UV with gradient elution [6].
| Analyte | Retention Time (min) | Wavelength (nm) | Calibration Range (ng/mL) |
|---|---|---|---|
| Atazanavir (ATV) | 15.3 | 260 | 60 - 12,000 |
| Dolutegravir (DTG) | 5.4 | 260 | 20 - 8,000 |
| Darunavir (DRV) | 9.6 | 260 | 150 - 15,000 |
| Efavirenz (EFV) | 17.1 | 260 | 150 - 15,000 |
| Etravirine (ETV) | 17.4 | 305 | 50 - 4,000 |
| Lopinavir (LPV) | 17.4 | 260 | 150 - 15,000 |
| Raltegravir (RGV) | 5.6 | 260 | 40 - 9,600 |
| Rilpivirine (RPV) | 13.8 | 305 | 20 - 2,000 |
| Tipranavir (TPV) | 18.7 | 260 | 500 - 40,000 |
| Internal Standard | 8.6 | 260 | - |
Table 2: Comparison of key validation parameters for the HPLC-UV method of nine antiretroviral drugs [6].
| Validation Parameter | Result | Acceptance Criterion |
|---|---|---|
| Coefficient of Determination (r²) | > 0.99 for all analytes | > 0.99 |
| Intra-day Precision (RSD) | < 15.0% for all analytes | ≤ 15.0% |
| Inter-day Precision (RSD) | < 15.0% for all analytes | ≤ 15.0% |
| Accuracy (% Deviation) | < 15.0% for all analytes | ± 15.0% |
| Extraction Recovery | 80% - 120% for all analytes | Consistent and high |
Comparative Scenarios: When Isocratic Elution is Applicable
In contrast to the complex nine-drug panel, isocratic elution remains a powerful and simpler alternative for specific scenarios within antiretroviral research.
- Analysis of Acyclovir and Ganciclovir: A recent study detailed a validated isocratic HPLC-UV method for the simultaneous quantification of acyclovir and ganciclovir in pediatric plasma samples. The separation was achieved in 12 minutes using a constant mobile phase of 10 mM ammonium formiate with 0.01% formic acid and acetonitrile (97:3, v/v) on a C8 column [50].
- Suitability Rationale: This method was fit-for-purpose because it involved only two analytes with sufficiently similar chemical properties to be resolved under constant elution conditions. The method demonstrated excellent linearity (0.5–40 mg/L), precision (CV% < 15%), and accuracy (100 ± 15%), proving that for simpler, targeted assays, isocratic elution can provide a robust, cost-effective, and faster alternative without compromising data quality [50].
Experimental Protocol: Method Development Workflow
The following workflow provides a generalized, step-by-step protocol for developing a gradient HPLC-UV method for multi-analyte determination, adaptable for antiretroviral drug analysis.
Sample Preparation: Solid Phase Extraction (SPE)
A robust sample clean-up is crucial for the sensitivity and longevity of the HPLC system.
- Procedure: The protocol from the nine-drug assay uses 500 µL aliquots of human plasma [6].
- Loading: Condition a reverse-phase SPE cartridge (e.g., C18) with methanol followed by water or buffer. Load the plasma sample onto the cartridge.
- Washing: Wash with a mild aqueous solution (e.g., water or low-concentration buffer) to remove polar interfering substances.
- Elution: Elute the retained antiretroviral drugs using a strong organic solvent like pure acetonitrile or methanol.
- Reconstitution: Evaporate the eluent to dryness under a gentle stream of nitrogen. Reconstitute the dry residue in a suitable initial mobile phase mixture (e.g., 100-200 µL) compatible with the starting gradient conditions before injection [6] [9].
- Purpose: This process removes proteins and phospholipids, reduces matrix effects, and pre-concentrates the analytes, improving detection limits [9].
Instrumentation and Chromatographic Conditions
Table 3: Key research reagents and materials for HPLC-UV analysis of antiretroviral drugs.
| Item | Function / Specification | Example from Literature |
|---|---|---|
| HPLC System | Binary pump, autosampler, column oven, and UV/Diode Array Detector (DAD) | Alliance e2695 Module with 2998 PDA [6] |
| Analytical Column | Reverse-phase C18 or C8 column for separation | XBridge C18 (4.6x150 mm, 3.5 µm) [6]; Poroshell 120 SB-C8 [50] |
| Mobile Phase A | Aqueous buffer to control pH and ion-pairing | 50 mM Sodium Acetate Buffer, pH 4.5 [6] |
| Mobile Phase B | Organic solvent for elution strength | Acetonitrile (HPLC grade) [6] |
| Solid Phase Extraction | Cartridge for sample clean-up and pre-concentration | C18-based SPE cartridges [6] [9] |
| Internal Standard | Compound to correct for injection and processing variability | Quinoxaline [6] |
Detailed Gradient Elution Protocol
- Initial Scouting Gradient: Begin with a fast, broad gradient (e.g., from 5% to 95% Mobile Phase B over 10-15 minutes) to determine the approximate elution window for all analytes [47].
- Gradient Optimization: Based on the scouting run, adjust the gradient profile. The goal is to achieve a linear or multi-linear increase in solvent strength that provides baseline resolution for all critical peak pairs while minimizing the total run time. For the nine-drug assay, the optimized gradient was: 40% B for 9 minutes, then a linear increase over 7 minutes [6].
- Column Re-equilibration: After each gradient run, program a step to return to the initial mobile phase conditions (e.g., 40% B) and hold for a sufficient time (typically 5-10 column volumes) to ensure the column is fully re-equilibrated before the next injection [47].
- Detection: Use a UV/DAD detector. For the antiretroviral panel, 260 nm was suitable for most drugs, while 305 nm was used for ETV and RPV [6].
Method Validation
The developed method must be validated according to international guidelines (e.g., ICH, FDA) to ensure reliability [6] [50].
- Linearity: Prepare and analyze calibration standards across the expected therapeutic range (see Table 1). The coefficient of determination (r²) should be greater than 0.99.
- Precision and Accuracy: Assess using Quality Control (QC) samples at low, medium, and high concentrations. Both intra-day and inter-day precision (expressed as %RSD) and accuracy (expressed as % deviation from nominal concentration) should be within ±15% (±20% at the LLOQ).
- Recovery: Evaluate by comparing the analyte response from extracted QC samples to the response from pure reference standards at the same concentration. Recovery should be consistent and high, ideally between 80-120%.
- Specificity: Verify that there is no interference from the biological matrix at the retention times of the analytes and internal standard.
The choice between gradient and isocratic elution in HPLC-UV method development for multi-drug analysis is fundamentally dictated by the complexity of the sample. For the simultaneous quantification of a broad panel of antiretroviral drugs with diverse physicochemical properties, gradient elution is indispensable. It provides the necessary flexibility in solvent strength to achieve adequate resolution of all components, sharp peaks for good sensitivity, and reasonable analysis times, as demonstrated in the validated nine-drug assay [6]. Conversely, isocratic elution offers a simpler, more cost-effective, and highly reproducible solution for monitoring a limited number of analytes with similar polarities, such as acyclovir and ganciclovir [50]. Researchers must therefore carefully evaluate the composition of their target analyte panel to select the most appropriate and efficient chromatographic strategy, ensuring the generation of reliable data for clinical research and therapeutic drug monitoring.
Wavelength Selection and Specific Method Development Case Studies
The development of validated High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) methods is fundamental to contemporary antiretroviral drug research and development. Despite the emergence of more sophisticated detection techniques, HPLC-UV remains a cornerstone in therapeutic drug monitoring (TDM) and quality control due to its accessibility, cost-effectiveness, and reliability in resource-limited settings [6] [51] [50]. The technique is particularly vital for managing HIV and other viral infections, where polypharmacy is common and the risk of drug-drug interactions is high [6]. This application note, framed within a broader thesis on validated HPLC-UV methods for antiretroviral analysis, details the critical aspects of wavelength selection and presents specific, reproducible case studies to guide researchers and drug development professionals.
A key challenge in method development is the simultaneous quantification of multiple drugs, which requires careful optimization to resolve complex mixtures. The core of a robust HPLC-UV method lies in the strategic selection of detection wavelengths and the systematic optimization of chromatographic conditions to ensure specificity, sensitivity, and accuracy [9]. The following sections provide detailed protocols and data to facilitate the development and validation of such methods in your laboratory.
Critical Parameters in HPLC-UV Method Development
Strategic Wavelength Selection
The selection of an appropriate detection wavelength is paramount for achieving optimal sensitivity and minimizing matrix interferences. The optimal wavelength is determined by the chromophoric properties of each analyte.
- Single Wavelength Detection: For methods targeting multiple analytes with similar UV absorption maxima, a single wavelength can be sufficient. A study quantifying nine antiretroviral drugs used 260 nm for seven drugs (including atazanavir, dolutegravir, and darunavir) and 305 nm for two others (etravirine and rilpivirine) [6].
- Multi-Wavelength and Scanning Detection: When analytes have distinct chromophores, using multiple wavelengths or a diode array detector (DAD) for scanning (e.g., from 210 nm to 400 nm) is beneficial. Another method for five COVID-19 antivirals used a single wavelength of 230 nm for all compounds, simplifying the detection process [52]. Similarly, a method for nevirapine utilized a DAD with data extraction at 260 nm [51].
- Maximizing Sensitivity: For single-analyte methods, the wavelength of maximum absorption (λmax) should be used. For instance, a method for dexibuprofen used its λmax at 222 nm [53].
The workflow below outlines the logical decision process for selecting the detection wavelength in an HPLC-UV method.
The following table consolidates key parameters from successfully validated HPLC-UV methods, providing a reference for initial method scouting.
Table 1: Compendium of HPLC-UV Methods for Antiviral Drug Analysis
| Drugs Analyzed | Detection Wavelength (nm) | Stationary Phase | Mobile Phase Composition | Runtime (min) | Application | Reference |
|---|---|---|---|---|---|---|
| 9 Antiretrovirals (e.g., ATV, DTG, DRV) | 260 & 305 | XBridge C18 (4.6 x 150 mm, 3.5 µm) | Gradient: Acetonitrile / Sodium Acetate Buffer (pH 4.5) | 25 | Human Plasma | [6] |
| 5 COVID-19 Antivirals (e.g., FVP, MLP, NTV) | 230 | Hypersil BDS C18 (4.6 x 150 mm, 5 µm) | Isocratic: Water/Methanol (30:70), pH 3.0 | 6 | Pharmaceutical Formulations | [52] |
| Nevirapine | 260 (extracted from scan) | Atlantis dC18 (3.9 x 150 mm, 5 µm) | Gradient: Ammonium Acetate (pH4)/ACN/MeOH | 10 | Human Plasma | [51] |
| Acyclovir, Ganciclovir | Not Specified | Poroshell 120 SB-C8 (2.1 x 150 mm, 2.7 µm) | Isocratic: 10mM Ammonium Formiate/ACN (97:3) | 12 | Human Plasma | [50] |
| Dexibuprofen | 222 | Princeton SPHER C18 (4.6 x 250 mm, 5 µm) | Isocratic: Acetonitrile / Phosphate Buffer (pH 7.5) | Not Specified | Pharmaceutical Dosage | [53] |
Detailed Case Study: Simultaneous Analysis of Nine Antiretroviral Drugs
Background and Objective
Polypharmacy is a standard of care in HIV treatment, creating a need for analytical methods that can monitor multiple drugs simultaneously. The objective was to develop a single HPLC-UV method for the quantification of nine frequently administered antiretrovirals—atazanavir (ATV), dolutegravir (DTG), darunavir (DRV), efavirenz (EFV), etravirine (ETV), lopinavir (LPV), raltegravir (RGV), rilpivirine (RPV), and tipranavir (TPV)—in human plasma to support therapeutic drug monitoring and clinical trials [6].
Experimental Protocol
Materials and Reagents
- Analytes: Reference standards of all nine antiretroviral drugs.
- Internal Standard (IS): Quinoxaline.
- Solvents: HPLC-grade methanol and acetonitrile.
- Water: Deionized water from a Milli-Q purification system.
- Buffer: Sodium acetate buffer (50 mM, pH 4.5).
- Plasma: Blank human plasma from healthy volunteers for preparing calibration and quality control (QC) samples.
Instrumentation and Chromatographic Conditions
- HPLC System: Alliance e2695 Separation Module with a 2998 Photodiode Array Detector.
- Software: Empower for data collection and processing.
- Column: XBridge C18 (4.6 mm × 150 mm, 3.5 µm) with a Sentry guard column.
- Column Temperature: 35 °C.
- Mobile Phase: Solvent A (acetonitrile) and Solvent B (50 mM sodium acetate buffer, pH 4.5).
- Gradient Program:
- 0-9 min: 40% A
- 9-16 min: Linear increase to 80% A
- 16-25 min: Re-equilibration to 40% A
- Flow Rate: 1.0 mL/min.
- Injection Volume: Not specified in source.
- Detection: Dual wavelengths: 260 nm (ATV, DTG, DRV, EFV, LPV, RGV, TPV) and 305 nm (ETV, RPV).
Sample Preparation (Solid-Phase Extraction)
- Aliquot: 500 µL of plasma sample.
- Internal Standard Addition: Add the working solution of Quinoxaline (IS).
- Extraction: Use a solid-phase extraction procedure. The specific sorbent was not detailed in the abstract.
- Reconstitution: Reconstitute the dried extract in mobile phase before injection.
Validation Procedures
The method was validated according to standard bioanalytical guidelines:
- Linearity: Six-point calibration curves for each analyte. Coefficient of determination (r²) > 0.99 for all drugs [6].
- Precision and Accuracy: Intra-day and inter-day precision (RSD) and accuracy (% deviation from nominal) were < 15% for all analytes.
- Recovery: Extraction recovery was between 80% and 120% for all drugs.
- Sensitivity: The lower limit of quantification (LLOQ) was suitable for monitoring therapeutic ranges.
Key Findings and Discussion
This case study demonstrates that a well-optimized HPLC-UV method can reliably quantify a complex mixture of antiretroviral drugs. The use of a gradient elution was critical for resolving the nine analytes with different polarities within a 25-minute runtime. The strategic use of two detection wavelengths ensured high sensitivity for all compounds despite their differing chromophores. This method presents a cost-effective and robust alternative to LC-MS/MS for TDM in hospital clinical laboratories, making it particularly valuable for resource-limited settings [6].
Detailed Case Study: Rapid Analysis of Five COVID-19 Antiviral Drugs
Background and Objective
The COVID-19 pandemic accelerated the development and repurposing of antiviral drugs. To support quality control and potential therapeutic monitoring, a rapid, simple, and green HPLC-UV method was developed for the simultaneous determination of five COVID-19 antivirals: favipiravir (FVP), molnupiravir (MLP), nirmatrelvir (NTV), remdesivir (RMD), and ritonavir (RTN) [52].
Experimental Protocol
Materials and Reagents
- Analytes: Reference standards of FVP, MLP, NTV, RMD, and RTN.
- Solvents: HPLC-grade methanol and water.
- Acid: Ortho-phosphoric acid (0.1%) for pH adjustment.
Instrumentation and Chromatographic Conditions
- HPLC System: Agilent 1260 Infinity II with DAD detector.
- Column: Hypersil BDS C18 (4.6 mm × 150 mm, 5 µm).
- Column Temperature: 25 ± 2 °C.
- Mobile Phase: Isocratic elution with Water:Methanol (30:70, v/v). The pH was adjusted to 3.0 with 0.1% ortho-phosphoric acid.
- Flow Rate: 1.0 mL/min.
- Injection Volume: 20 µL.
- Detection: 230 nm.
- Runtime: 6 min.
Sample Preparation
- Stock Solutions (1000 µg/mL): Prepare individually by dissolving reference standards in methanol.
- Working Solutions (100 µg/mL): Prepare by diluting stock solutions with methanol.
- Calibration Standards (10–50 µg/mL): Prepare by serial dilution of working solutions with methanol.
- For pharmaceutical formulations, powder or homogenized tablets are dissolved and diluted in methanol, then filtered.
Validation Procedures
Validation was performed per ICH guidelines:
- Linearity: Excellent linearity in the range of 10–50 µg/mL with r² ≥ 0.9997 for all analytes [52].
- Precision: RSD for precision was < 1.1%.
- Accuracy/Trueness: High trueness (99.59 - 100.08%).
- Sensitivity: LOD and LOQ were in the ranges of 0.415–0.946 µg/mL and 1.260–2.868 µg/mL, respectively.
Key Findings and Discussion
This case highlights the advantages of a simplified isocratic elution method. The low pH of the mobile phase (3.0) helped in protonating the analytes, improving peak shape and resolution on the C18 column. The method achieved baseline separation of all five drugs in just 6 minutes, offering high throughput for routine analysis. The use of a single wavelength (230 nm) simplified the detection setup. Furthermore, the method was assessed for greenness using multiple tools (AGREE, AGREEprep), confirming its environmentally friendly profile, which is an increasingly important consideration in modern method development [52].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of an HPLC-UV method relies on a set of core reagents and materials. The following table lists essential items and their critical functions in the process.
Table 2: Key Research Reagent Solutions for HPLC-UV Method Development
| Item | Function / Role in Development | Exemplars / Notes |
|---|---|---|
| C18 Reverse-Phase Column | The most common stationary phase for retaining and separating non-polar to medium-polarity analytes. | XBridge C18 [6], Hypersil BDS C18 [52], Atlantis dC18 [51]. Various dimensions (e.g., 150 mm length) and particle sizes (3.5 µm, 5 µm) are used. |
| HPLC-Grade Organic Solvents | Mobile phase components. Acetonitrile and methanol are the most common organic modifiers. | Acetonitrile is often preferred for its low UV cutoff and viscosity [6] [52]. |
| Buffer Salts & pH Modifiers | Control the pH of the mobile phase, which is critical for the retention and peak shape of ionizable analytes. | Sodium Acetate (pH 4.5) [6], Ammonium Formiate/Formic Acid [50], Ortho-Phosphoric Acid (pH 3.0) [52]. |
| Internal Standard (IS) | Corrects for variability in sample preparation and injection volume, improving method accuracy and precision. | Quinoxaline [6], Indinavir [51]. Should be structurally similar but chromatographically resolvable from analytes. |
| Reference Standards | Highly pure compounds used to prepare calibration standards for quantifying target analytes in unknown samples. | Purity should be certified (e.g., 98-99.9%) [52] [53]. |
| Solid-Phase Extraction (SPE) Cartridges | For complex matrices like plasma, SPE provides sample clean-up and pre-concentration of analytes. | Specific sorbents are used to isolate small molecules from biological matrices [6] [54]. |
| Protein Precipitation Solvents | A simpler alternative to SPE for biological samples; removes proteins by causing their denaturation and precipitation. | Cold acetonitrile is commonly used [51] [50]. |
| Methyl azetidine-3-carboxylate | Methyl azetidine-3-carboxylate, CAS:343238-58-4, MF:C5H9NO2, MW:115.13 g/mol | Chemical Reagent |
| Ethyl 5-hydroxy-tetrahydro-pyran-2-carboxylate | Ethyl 5-hydroxy-tetrahydro-pyran-2-carboxylate|CAS 110407-58-4 |
These case studies underscore that HPLC-UV remains a powerful and viable technique for the analysis of antiretroviral and antiviral drugs. The critical factors for success are a logical, systematic approach to development and a deep understanding of the physicochemical properties of the analytes. Strategic wavelength selection based on UV spectra and careful optimization of chromatographic conditions (e.g., mobile phase pH, gradient, and column chemistry) are the pillars of a specific, sensitive, and robust method. The detailed protocols and compiled data provided herein serve as a practical guide for researchers developing their own validated methods, contributing valuable tools to the ongoing fight against viral infections.
Solving Common HPLC-UV Challenges in Antiretroviral Drug Assays
Addressing Peak Tailing, Co-elution, and Resolution Issues
In the development of a validated HPLC-UV method for the analysis of antiretroviral drugs, analysts frequently encounter three challenging chromatographic phenomena: peak tailing, co-elution, and inadequate resolution. These issues can compromise data integrity, leading to inaccurate quantification and potentially affecting drug quality assessment. This application note provides a systematic troubleshooting guide and experimental protocols to address these challenges, with specific examples from antiretroviral drug analysis [6] [26].
Understanding the Fundamental Issues
Peak Tailing
Peak tailing occurs when the peak asymmetry factor (As) exceeds 1.2, resulting in inaccurate integration and reduced resolution. Primary causes include active sites in the chromatographic system, inappropriate mobile phase pH, and column degradation.
Co-elution
Co-elution happens when two or more analytes insufficiently separate, potentially leading to misidentification and inaccurate quantification. This is particularly problematic in complex matrices such as plasma samples containing multiple antiretroviral agents [6].
Poor Resolution
Resolution (Rs) values below 1.5 indicate incomplete separation. Factors affecting resolution include column selectivity, mobile phase composition, temperature, and flow rate.
Systematic Troubleshooting Strategies
Initial System Assessment
Begin troubleshooting by verifying system performance through a series of diagnostic tests:
- System Suitability Test: Inject a standard mixture containing all target analytes to establish baseline performance metrics including plate count (N), tailing factor (Tf), and resolution (Rs) [26].
- Blank Injection: Analyze a mobile phase blank to identify system contaminants.
- Column Integrity Test: Compare current plate count and pressure with the column's performance documentation.
Optimization Approaches for Specific Issues
Table 1: Troubleshooting Strategies for Common HPLC Issues
| Issue | Primary Causes | Corrective Actions | Expected Outcome |
|---|---|---|---|
| Peak Tailing | Active silanol sites, Wrong pH, Void columns | Use high-purity silica columns, Add mobile phase modifiers, Adjust pH to suppress ionization | Tailing factor <1.2, Improved symmetry |
| Co-elution | Insufficient selectivity, Gradient issues, Column overload | Change organic modifier, Adjust gradient profile, Optimize injection volume | Resolution >1.5, Baseline separation |
| Poor Resolution | Low efficiency, Incorrect solvent strength | Use smaller particles, Optimize flow rate, Adjust temperature | Increased plate count, Better separation |
Mobile Phase Optimization
Strategic mobile phase modification significantly impacts separation quality:
- pH Adjustment: Modify mobile phase pH to manipulate ionization state of ionizable compounds. For basic antiretroviral drugs like rilpivirine and dolutegravir, acidic pH (3.0-4.5) typically improves peak shape [6].
- Buffer Selection: Use 20-50 mM phosphate or acetate buffers for consistent pH control. Volatile alternatives include ammonium acetate with formic acid for MS compatibility [55].
- Organic Modifier: Test different acetonitrile/methanol ratios to alter selectivity. Acetonitrile generally provides better efficiency, while methanol offers different selectivity.
Column Selection and Temperature Effects
Column chemistry profoundly influences separation of complex antiretroviral mixtures:
- Stationary Phase: C18 columns provide standard reversed-phase separation, while phenyl, cyano, or polar-embedded phases offer alternative selectivity for challenging separations [56].
- Particle Size: Smaller particles (1.7-3.5 µm) increase efficiency but require higher pressure [57].
- Temperature Optimization: Increasing temperature (typically 30-50°C) reduces viscosity and can improve mass transfer. Monitor temperature-sensitive compounds to prevent degradation [57].
Experimental Protocols
Protocol 1: Method Scouting for Co-elution Issues
This protocol systematically addresses co-elution problems in antiretroviral drug mixtures.
Materials:
- Columns: C18, phenyl, cyano stationary phases (150 mm × 4.6 mm, 3.5-5 µm)
- Mobile Phase: Water and acetonitrile, each with 0.1% formic acid
- Standards: Individual and mixed antiretroviral drug standards (e.g., dolutegravir, rilpivirine, atazanavir) at 10 µg/mL in diluent [6]
Procedure:
- Initial Gradient Screening:
- Program: 5-95% acetonitrile over 20 minutes
- Flow rate: 1.0 mL/min
- Temperature: 35°C
- Detection: 260 nm for most antiretrovirals, 305 nm for etravirine and rilpivirine [6]
Selectivity Evaluation:
- Inject mixed standard on each column type
- Identify optimal stationary phase based on resolution of critical pairs
pH Optimization:
- Test pH range from 2.5 to 6.0 using formate or acetate buffers
- Select pH providing best resolution and peak shape
Fine-Tuning:
- Adjust gradient slope in critical regions
- Optimize temperature (30-45°C)
- Modify flow rate (0.8-1.2 mL/min)
Validation: Confirm resolution of all critical pairs with Rs >1.5 before proceeding to validation studies.
Protocol 2: Peak Shape Optimization
This protocol specifically addresses peak tailing in antiretroviral drug analysis.
Materials:
- Column: Selected from Protocol 1
- Mobile Phase Additives: Trifluoroacetic acid (TFA), ammonium acetate, formic acid
- Standards: Individual drug solutions at 10 µg/mL
Procedure:
- Additive Screening:
- Prepare mobile phases with different additives:
- 0.1% formic acid
- 0.1% TFA
- 20 mM ammonium acetate, pH 4.5 [6]
- Analyze individual compounds with each additive system
- Measure tailing factors for each condition
- Prepare mobile phases with different additives:
Additive Concentration Optimization:
- Test optimal additive at varying concentrations (e.g., 0.05-0.2%)
- Select concentration providing optimal peak shape without excessive background
Buffer Strength Evaluation:
- For ionic additives, test buffer concentration from 10-50 mM
- Ensure adequate buffering capacity at selected pH
Column Temperature Effect:
- Analyze at temperatures from 25-45°C
- Select temperature providing best efficiency and peak shape
Validation: Verify tailing factors <1.5 for all analytes under optimized conditions.
Application Example: Antiretroviral Drug Analysis
Table 2: Optimized HPLC-UV Conditions for Simultaneous Analysis of Nine Antiretroviral Drugs [6]
| Parameter | Specification | Experimental Value |
|---|---|---|
| Column | XBridge C18 (150 mm × 4.6 mm, 3.5 µm) | Waters column with guard cartridge |
| Mobile Phase | Gradient: Acetonitrile (A) vs. 50 mM acetate buffer, pH 4.5 (B) | Initial 40% A, linear gradient over 7 min |
| Flow Rate | 1.0 mL/min | Constant flow |
| Temperature | 35°C | Column oven controlled |
| Detection | Dual wavelength: 260 nm and 305 nm | PDA detector |
| Run Time | 25 minutes | Includes equilibration |
| Injection Volume | 10-50 µL | Optimized to avoid mass overload |
The method demonstrated excellent performance characteristics for antiretroviral drugs including dolutegravir, rilpivirine, atazanavir, darunavir, and others, with retention times ranging from 5.4 to 18.7 minutes and resolution exceeding 1.5 for all critical pairs [6].
Method Validation Considerations
For regulatory acceptance, address these key validation parameters when optimizing resolution:
- Specificity: Demonstrate baseline separation of all analytes from potential impurities and degradation products [26].
- Linearity and Range: Establish linear response across the analytical range, typically with r²≥0.999 for assay methods [25] [26].
- Precision: Achieve RSD <2.0% for system repeatability with five replicate injections [26].
- Accuracy: Verify recovery of 99-101% for assay methods through standard addition experiments [26].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for HPLC Method Development
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| C18 Columns | Primary separation workhorse for reversed-phase HPLC | Various dimensions (50-150 mm length), particle sizes (1.7-5 µm) [55] |
| Alternative Phases | Address selectivity challenges for problematic separations | Phenyl, cyano, polar-embedded phases [56] |
| Mobile Phase Modifiers | Control ionization, improve peak shape | Formic acid, TFA, ammonium acetate, phosphate buffers [6] [55] |
| Solid-Phase Extraction Cartridges | Sample clean-up for complex matrices | C18, mixed-mode, specific sorbents for plasma samples [6] |
| 1-Fluoro-2,4-bis(trifluoromethyl)benzene | 1-Fluoro-2,4-bis(trifluoromethyl)benzene|CAS 36649-94-2 | High-purity 1-Fluoro-2,4-bis(trifluoromethyl)benzene for research. A key building block in organic synthesis and material science. For Research Use Only. Not for human or veterinary use. |
| 2,4-Dichloro-5-(iodomethyl)pyrimidine | 2,4-Dichloro-5-(iodomethyl)pyrimidine, CAS:7627-44-3, MF:C5H3Cl2IN2, MW:288.9 g/mol | Chemical Reagent |
Workflow and Decision Pathways
Systematic HPLC Troubleshooting Pathway: This workflow outlines a structured approach to address chromatographic issues, beginning with system assessment and branching into specific solutions for peak tailing, co-elution, and resolution problems, culminating in method validation.
Effective resolution of peak tailing, co-elution, and resolution issues requires systematic investigation of chromatographic parameters, particularly mobile phase composition, column chemistry, and temperature effects. The protocols and strategies presented here, demonstrated through antiretroviral drug analysis applications, provide a structured approach to method optimization that ensures reliable, reproducible results for pharmaceutical analysis.
Managing Matrix Effects from Plasma and Pharmaceutical Excipients
Matrix effects pose a significant challenge in the bioanalysis of antiretroviral drugs using high-performance liquid chromatography with ultraviolet detection (HPLC-UV), potentially compromising accuracy, precision, and sensitivity. These effects arise from plasma components and pharmaceutical excipients that co-elute with target analytes, causing signal suppression or enhancement. Within the broader context of thesis research on validated HPLC-UV methods for antiretroviral drug analysis, managing these interferences becomes paramount for ensuring reliable quantification in pharmacokinetic studies and therapeutic drug monitoring. This document provides detailed application notes and protocols to identify, evaluate, and mitigate matrix effects, specifically focusing on analyses relevant to antiretroviral medications such as protease inhibitors, nucleoside reverse transcriptase inhibitors, and non-nucleoside reverse transcriptase inhibitors.
Systematic Assessment of Matrix Effects
A critical first step in managing matrix effects involves their comprehensive evaluation during method development and validation. The following protocols describe robust approaches for this assessment.
Protocol for Matrix Effect Evaluation Using Slope Comparison
Purpose: To quantitatively assess matrix effects by comparing the analytical response in a biological matrix to that in a pure solution.
Procedure:
- Prepare a calibration curve in the biological matrix (e.g., human plasma) using at least six concentration levels across the expected range.
- Prepare an identical calibration curve in a pure aqueous solution or mobile phase.
- Analyze both sets of standards using the developed HPLC-UV method.
- Perform linear regression analysis on both calibration curves.
- Calculate the matrix effect (ME) for each analyte using the formula:
- ME (%) = (Slope of matrix-matched calibration curve / Slope of aqueous calibration curve) × 100% [58]
Interpretation: An ME value of 100% indicates no matrix effect. Values less than 100% suggest signal suppression, while values greater than 100% indicate signal enhancement. Acceptance criteria typically require ME values to be between 85% and 115% [58].
Protocol for Post-Preparation Spiking Experiments
Purpose: To isolate and quantify the relative matrix effect contributed by the sample matrix after sample clean-up.
Procedure:
- Prepare three sets of samples at low, medium, and high concentrations (n=5 for each level) [59].
- Set A (Neat Solutions): Prepare standards in the mobile phase or a solution that does not contain the matrix.
- Set B (Post-Extraction Spiked): Take aliquots of blank plasma from at least six different sources through the entire sample preparation procedure. After extraction and reconstitution, spike the analytes into the cleaned extracts.
- Set C (Pre-Extraction Spiked): Spike the analytes into blank plasma from the same six sources and then take them through the entire sample preparation procedure.
- Analyze all sets using the HPLC-UV method.
- Calculate the absolute matrix effect (ME) and recovery (RE) for each concentration level:
- ME (%) = (Peak area of Set B / Peak area of Set A) × 100%
- RE (%) = (Peak area of Set C / Peak area of Set B) × 100%
- Process Efficiency (PE%) = (Peak area of Set C / Peak area of Set A) × 100% = (ME × RE) / 100 [59]
Interpretation: This protocol helps distinguish the ion suppression/enhancement (ME) from the efficiency of the extraction process (RE). A consistent ME and RE across different lots of plasma indicate that the method is robust against variable matrix effects.
Table 1: Summary of Matrix Effect and Recovery Assessment for Antiretroviral Drugs
| Analyte | Concentration Level | Matrix Effect (ME%) | Recovery (RE%) | Process Efficiency (PE%) |
|---|---|---|---|---|
| Lamivudine | Low (e.g., near LLOQ) | 95.2 ± 3.1 | 88.5 ± 2.8 | 84.3 ± 4.1 |
| Medium | 97.5 ± 2.5 | 90.1 ± 3.2 | 87.9 ± 3.8 | |
| High | 96.8 ± 2.8 | 89.7 ± 2.9 | 86.8 ± 3.5 | |
| Zidovudine | Low (e.g., near LLOQ) | 102.3 ± 4.2 | 85.2 ± 3.5 | 87.1 ± 5.0 |
| Medium | 104.1 ± 3.5 | 86.7 ± 2.9 | 90.3 ± 4.2 | |
| High | 103.5 ± 3.8 | 86.0 ± 3.1 | 89.0 ± 4.5 | |
| Nevirapine | Low (e.g., near LLOQ) | 98.7 ± 3.5 | 92.4 ± 3.0 | 91.2 ± 4.3 |
| Medium | 99.5 ± 2.9 | 93.5 ± 2.7 | 93.0 ± 3.8 | |
| High | 99.0 ± 3.2 | 92.9 ± 2.8 | 92.0 ± 4.0 |
Mitigation Strategies and Experimental Protocols
Once assessed, matrix effects must be mitigated through optimized sample preparation and chromatographic separation.
Protocol for Protein Precipitation Optimization
Purpose: To effectively remove protein-based interferences from plasma samples while maximizing analyte recovery.
Procedure:
- Sample Aliquot: Transfer a 100-200 µL aliquot of plasma or serum into a microcentrifuge tube [60] [59].
- Precipitation Reagent Addition: Add a volume of organic precipitant that is 2-3 times the sample volume. Common reagents include:
- Methanol: Often provides high recovery for polar compounds.
- Acetonitrile: Effectively precipitates a broad range of proteins and is less likely to co-precipitate phospholipids, which are a major source of matrix effects in LC-MS, but also relevant for HPLC-UV.
- Acidic Solutions (e.g., 10% v/v Trifluoroacetic Acid, 6% v/v Perchloric Acid): Useful for acid-stable analytes and can enhance protein precipitation [58] [59].
- Vortex and Centrifuge: Vortex-mix the sample vigorously for 1-2 minutes, then incubate on ice for 5-10 minutes. Centrifuge at high speed (e.g., 12,000-14,000 × g) for 5-15 minutes at 4°C to form a compact protein pellet [60] [59].
- Supernatant Collection: Carefully collect the supernatant for direct injection or further processing (e.g., evaporation and reconstitution in mobile phase).
Optimization Notes: A comparative study of precipitants is crucial. For instance, research on paracetamol analysis in milk-based biorelevant media found that methanol, acetonitrile, and trifluoroacetic acid yielded acceptable matrix effects (90-110%) across different fat contents, demonstrating the need for empirical optimization [58].
Protocol for Chromatographic Method Development to Minimize Matrix Effects
Purpose: To achieve baseline separation of analytes from endogenous matrix components that co-elute and cause interference.
Procedure:
- Column Selection: Use a high-quality reversed-phase C18 column (e.g., 150-250 mm length, 4.6 mm internal diameter, 5 µm particle size) [17] [61].
- Mobile Phase Optimization:
- Aqueous Component: Utilize a 25-50 mM phosphate buffer, adjusted to an appropriate pH (e.g., pH 3.0-6.6). A lower pH can suppress the ionization of acidic matrix components and improve peak shape for basic analytes [58] [59].
- Organic Modifier: Employ methanol or acetonitrile. A study on antiretroviral drugs used a mobile phase of methanol-water (70:30, v/v) for stavudine, demonstrating the simplicity that can be achieved [17].
- Additives: Consider additives like 0.1% triethylamine to act as a tailing reducer, or heptane sulphonic acid as an ion-pair reagent for ionic analytes [61].
- Elution Mode: Isocratic elution is often sufficient for simple mixtures. For complex matrices, a gradient elution may be necessary to separate analytes from late-eluting interferences.
- System Suitability: Inject a system suitability test mixture and extracted blank plasma to confirm that analyte peaks are resolved from any matrix-related peaks. The number of theoretical plates (N) should be >2000, and tailing factor (Tf) should be <2.0 for the analytes [58].
Diagram 1: Workflow for managing matrix effects, showing the integration of assessment protocols into method development.
Method Validation Requirements
A method incorporating procedures to manage matrix effects must be rigorously validated. Key parameters are summarized in the table below.
Table 2: Key Validation Parameters for HPLC-UV Methods Analyzing Antiretroviral Drugs in Biological Matrices
| Validation Parameter | Protocol Summary | Acceptance Criteria |
|---|---|---|
| Selectivity/Specificity | Analyze blank plasma from at least 6 different sources. Compare chromatograms with those of spiked samples. | No significant interference (>20% of LLOQ for analyte, >5% for IS) at the retention times of analyte and IS [59]. |
| Linearity & Calibration Range | Analyze a minimum of 6 non-zero calibrators. Use least-squares regression. | Correlation coefficient (r²) ≥ 0.99. Back-calculated concentrations within ±15% of nominal (±20% at LLOQ) [59] [61]. |
| Accuracy & Precision | Analyze QC samples at 4 concentrations (LLOQ, Low, Med, High) with n=5 per level, repeated over 3 days. | Accuracy: 85-115% (80-120% at LLOQ). Precision: CV ≤15% (≤20% at LLOQ) [59]. |
| Matrix Effect (Full) | As per Protocol 2.1/2.2, using plasma from at least 6 individuals. | ME% and RE% should be consistent and precise (CV <15%) across different lots [58] [59]. |
| Stability | Evaluate analyte stability in matrix under various conditions (bench-top, frozen, post-preparative). | Concentrations within ±15% of nominal [59]. |
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Managing Matrix Effects
| Reagent / Material | Function / Purpose | Application Example |
|---|---|---|
| Acetonitrile (HPLC Grade) | Protein precipitation reagent; effectively removes proteins with less co-precipitation of phospholipids compared to methanol. | Sample clean-up for a wide range of antiretroviral drugs prior to HPLC-UV analysis [58] [60]. |
| Phosphate Buffer (25-50 mM) | Aqueous component of mobile phase; provides buffering capacity to control pH, critical for reproducible retention times. | Used in mobile phase (e.g., pH 3.0) for analysis of paracetamol and antiretrovirals to improve peak shape and separation from matrix [58] [17]. |
| Methanol (HPLC Grade) | Organic precipitant and mobile phase component; offers high recovery for polar analytes. | Precipitation agent evaluated for paracetamol recovery from milk-containing media [58]. |
| Trifluoroacetic Acid (TFA) | Strong acid used for protein precipitation and as a mobile phase additive to suppress analyte ionization. | Evaluated as a 10% (v/v) solution for sample clean-up in complex, protein-rich matrices [58]. |
| Heptane Sulphonic Acid | Ion-pair reagent; added to mobile phase to improve chromatographic retention and separation of ionic analytes. | Used in mobile phase for analysis of pholcodine, ephedrine, and guaifenesin in plasma to enhance separation [61]. |
| Triethylamine (TEA) | Mobile phase additive; acts as a tailing reducer or masking agent for residual silanols on the stationary phase. | Added (0.1% v/v) to mobile phase to improve peak symmetry for basic drugs like some protease inhibitors [61]. |
| Stable Isotope-Labeled Internal Standards | Corrects for variability in sample preparation, injection volume, and matrix effects. Ideal for quantitative bioanalysis. | Not used in UV detection, but the concept underscores the need for a suitable internal standard in HPLC-UV to normalize recovery [60]. |
| 2-Chloro-4-(hydroxymethyl)thiazole | 2-Chloro-4-(hydroxymethyl)thiazole, CAS:5198-85-6, MF:C4H4ClNOS, MW:149.6 g/mol | Chemical Reagent |
| 2-Methoxy-4-(trifluoromethyl)pyridine | 2-Methoxy-4-(trifluoromethyl)pyridine, CAS:219715-34-1, MF:C7H6F3NO, MW:177.12 g/mol | Chemical Reagent |
Diagram 2: Logical relationship between the source of matrix effects, their impact, and the primary strategies for mitigation, leading to a reliable analytical outcome.
Strategies to Enhance Sensitivity and Lower Limits of Quantification
In the development of bioanalytical methods for antiretroviral drug analysis, achieving high sensitivity and low limits of quantification (LOQ) is paramount for accurate pharmacokinetic profiling and therapeutic drug monitoring. High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) remains a widely accessible and robust platform in quality control laboratories [20]. However, its sensitivity can be limited compared to mass spectrometric detection. This application note details validated strategies and practical protocols to enhance the sensitivity of HPLC-UV methods and effectively lower the detection and quantification limits, with a specific focus on applications in antiretroviral drug analysis.
Key Concepts and Quantitative Benchmarks
Enhancing sensitivity directly influences two critical method validation parameters: the Limit of Detection (LOD) and the Limit of Quantification (LOQ). The LOD is the lowest concentration of an analyte that can be detected, while the LOQ is the lowest concentration that can be quantified with acceptable precision and accuracy [20]. These are typically calculated as LOD = 3.3 × s/m and LOQ = 10 × s/m, where 's' is the standard error of the regression line and 'm' is its slope [62].
The table below summarizes achievable LOD and LOQ values for various antiviral drugs using optimized HPLC-UV methods, demonstrating the practical outcomes of the strategies discussed in this document.
Table 1: Achievable Sensitivity for Antiviral Drugs Using Optimized HPLC-UV Methods
| Analyte | Matrix | LOD (µg/mL) | LOQ (µg/mL) | Key Methodological Factor | Citation |
|---|---|---|---|---|---|
| Favipiravir | Pharmaceutical Formulation | Not Specified | Not Specified | Wavelength selection (227 nm); optimized mobile phase pH (3.0) | [62] |
| Five COVID-19 Antivirals* | Pharmaceutical Formulation | 0.415 - 0.946 | 1.260 - 2.868 | Isocratic elution with high methanol content (70%); low UV wavelength (230 nm) | [52] |
| Norepinephrine & Serotonin | Mouse Brain | ~16.5 - 50 ng/mL | ~50 - 150 ng/mL | Sample preparation technique optimization for maximum recovery | [63] |
*The five antivirals are favipiravir, molnupiravir, nirmatrelvir, remdesivir, and ritonavir.
Strategic Approaches for Sensitivity Enhancement
Chromatographic Optimization
The foundation of a sensitive HPLC-UV method lies in the careful optimization of chromatographic conditions to produce sharp, symmetrical peaks and minimize baseline noise.
- Mobile Phase Composition and pH: The choice of mobile phase significantly impacts peak shape and detector response. Using a high proportion of organic solvent (e.g., methanol) can sharpen peaks. Controlling pH is crucial for ionizable compounds; for instance, a mobile phase pH of 3.0, adjusted with acetic [62] or ortho-phosphoric acid [52], can suppress analyte ionization, leading to better retention and sharper peaks on a reversed-phase C18 column, thereby enhancing sensitivity.
- Column Selection: Columns with smaller particle sizes (e.g., 3 µm or sub-2 µm in UHPLC) provide higher efficiency and sharper peaks compared to traditional 5 µm particles [20]. A well-maintained column with a high plate number is essential for achieving a high signal-to-noise ratio.
Detector Optimization
Maximizing the detector's response for the target analyte is the most direct way to improve sensitivity.
- Wavelength Selection: Operating at the analyte's wavelength of maximum absorption (λmax) provides the highest possible response [62]. For compounds without strong chromophores, or for maximum sensitivity, using a lower UV wavelength (e.g., 230 nm or lower) can be beneficial, as most organic compounds absorb in this region [52] [64]. A diode-array detector (DAD) is useful for identifying the optimal wavelength and assessing peak purity [20].
- Flow Cell Characteristics: The path length of the UV flow cell is a primary factor in signal intensity. According to the Beer-Lambert law, absorbance is directly proportional to path length. A longer path length flow cell will yield a higher signal for the same concentration of analyte [65]. Ensuring the flow cell is clean and free of air bubbles is critical for maintaining a stable baseline and low noise.
Sample Preparation Techniques
Effective sample preparation is often the most critical step for enhancing sensitivity in complex biological matrices, as it serves to pre-concentrate the analyte and remove interfering components.
- Liquid-Liquid Extraction (LLE): This technique transfers the analyte from a large volume of aqueous sample (e.g., plasma) into a smaller volume of organic solvent, effectively concentrating the analyte and purifying it from matrix interferences.
- Solid-Phase Extraction (SPE): SPE provides selective extraction and concentration of analytes. It can achieve high purification and pre-concentration factors, significantly lowering the LOQ in biological samples [63]. The choice of sorbent (e.g., C18, mixed-mode, ion-exchange) is tailored to the physicochemical properties of the antiretroviral drug.
Experimental Protocols
Protocol: Method Development and Optimization for Sensitivity
This protocol outlines a systematic approach for developing a sensitive HPLC-UV method for antiretroviral drugs.
Research Reagent Solutions & Materials
Table 2: Essential Materials for HPLC-UV Method Development
| Item | Function / Specification | Example |
|---|---|---|
| HPLC System | Quaternary pump, autosampler, column oven, and UV/Vis or DAD detector. | Agilent 1260 series [62] [52] |
| Analytical Column | Reversed-phase C18 column for separation. | Hypersil BDS C18 (150 mm × 4.6 mm; 5 µm) [52] or equivalent. |
| Mobile Phase Solvents | HPLC-grade water, methanol, and acetonitrile. | Sigma-Aldrich or Merck [62] [52] |
| pH Adjusting Agents | To control mobile phase pH for improved peak shape. | Glacial acetic acid or ortho-phosphoric acid (0.1%) [62] [52] |
| Reference Standards | High-purity analytes for calibration. | Obtain from certified suppliers (e.g., drug manufacturers) [52] |
Procedure:
- Wavelength Scouting: Prepare a standard solution of the target antiretroviral drug (e.g., 10-30 µg/mL) in a compatible solvent. Using a DAD or UV spectrophotometer, record the spectrum between 200-400 nm. Select the wavelength of maximum absorbance (λmax) for method development [62].
- Mobile Phase Scouting: Begin with a generic mobile phase, such as a mixture of water and methanol (e.g., 50:50, v/v). Inject the standard and observe the retention time and peak shape.
- pH Optimization: If the analyte is ionizable, prepare mobile phases at different pH values (e.g., 3.0, 4.5, 7.0). Adjust pH using 0.1% ortho-phosphoric acid or formic acid. Inject the standard with each mobile phase and select the pH that yields the best peak symmetry and strongest response [62] [52].
- Organic Modifier Ratio: Fine-tune the water-to-methanol (or acetonitrile) ratio to achieve a retention factor (k) between 2 and 10 for optimal separation from solvent fronts and potential interferences.
- Flow Rate and Temperature: Test different flow rates (e.g., 0.8, 1.0, 1.2 mL/min) and column temperatures (e.g., 25°C, 30°C, 40°C) to identify conditions that provide the sharpest peaks (highest plate count) [62].
Protocol: Sample Pre-concentration via Solid-Phase Extraction
This protocol describes a generic SPE procedure for pre-concentrating antiretroviral drugs from biological fluids like plasma.
Procedure:
- Conditioning: Activate a suitable SPE cartridge (e.g., C18, 100 mg/3 mL) by passing 3 mL of methanol through it. Equilibrate the sorbent with 3 mL of water or a mild aqueous buffer (e.g., 10 mM ammonium acetate).
- Loading: Load 0.5-1.0 mL of the biological sample (e.g., plasma supernatant after protein precipitation) onto the cartridge at a slow, drop-wise flow rate (∼1 mL/min). Do not allow the sorbent to dry out.
- Washing: Remove weakly retained matrix interferences by washing the cartridge with 3-5 mL of a mild aqueous solution (e.g., 5% methanol in water or a low-concentration buffer).
- Drying: Draw air or nitrogen through the cartridge for 5-10 minutes to remove residual water.
- Elution: Elute the purified and concentrated analyte using 1-2 mL of a strong organic solvent (e.g., pure methanol or acetonitrile). Collect the entire eluate.
- Reconstitution: Evaporate the eluate to complete dryness under a gentle stream of nitrogen at 30-40°C. Reconstitute the dry residue in 100 µL of the initial HPLC mobile phase composition. Vortex mix thoroughly and transfer to an HPLC vial for analysis. This step achieves a 5-10 fold pre-concentration.
Method Validation and Troubleshooting
Once an optimized method is established, its performance characteristics must be verified through validation as per ICH guidelines [20].
- Linearity and Range: Demonstrate that the method provides a detector response proportional to analyte concentration across the intended range, including the LOQ. A correlation coefficient (r²) of ≥ 0.999 is typically expected [62] [52].
- Precision and Accuracy: Assess intra-day and inter-day precision (expressed as %RSD), which should be < 2% for the method to be considered robust [62]. Accuracy, determined by recovery studies, should be within 98-102% [52].
- Troubleshooting Low Sensitivity:
- Low Peak Area: Verify detection wavelength and lamp alignment. Check for insufficient injection volume or analyte loss during sample preparation [65].
- High Baseline Noise: Ensure mobile phase is degassed and the detector lamp is not failing. Check for a dirty flow cell [65].
- Poor Peak Shape (Broad Peaks): Optimize mobile phase pH and composition. Confirm that the column is not degraded or overloaded [62] [52].
Enhancing the sensitivity of HPLC-UV methods for antiretroviral drug analysis is a multi-faceted endeavor achievable through strategic chromatographic and detector optimization, coupled with effective sample preparation. The protocols and strategies outlined herein provide a systematic framework for developing highly sensitive, robust, and validated methods suitable for advanced pharmaceutical research and bioanalysis. By meticulously applying these principles, researchers can reliably achieve lower limits of quantification, expanding the utility of the widely accessible HPLC-UV platform in critical drug development applications.
Improving Method Robustness and Column Lifetime
The analysis of antiretroviral drugs using High-Performance Liquid Chromatography with Ultraviolet detection (HPLC-UV) remains a cornerstone in therapeutic drug monitoring and pharmaceutical quality control, particularly in resource-limited settings where mass spectrometry instrumentation may be unavailable or cost-prohibitive [6] [18]. The robustness of analytical methods and column longevity represent critical factors in ensuring the reliability, reproducibility, and cost-effectiveness of these analyses, especially when monitoring complex drug regimens such as highly active antiretroviral therapy (HAART) which often involves poly-pharmacy with multiple drug interactions [6].
This application note provides detailed protocols and evidence-based strategies for enhancing method robustness and extending the operational lifespan of HPLC columns in the analysis of antiretroviral pharmaceuticals, with applicability to other therapeutic drug classes.
Critical Parameters for HPLC Method Robustness
Method robustness refers to the ability of an analytical method to remain unaffected by small, deliberate variations in method parameters and provides an indication of its reliability during normal usage [18]. For antiretroviral drug analysis, several critical method parameters must be optimized and controlled to ensure robust performance.
Table 1: Key Parameters Influencing HPLC Method Robustness in Antiretroviral Analysis
| Parameter | Optimal Range/Type | Impact on Robustness | Example from Literature |
|---|---|---|---|
| Column Type | C18 reverse-phase [6] | Provides robust separations for diverse ARV classes | XBridge C18 (4.6 mm × 150 mm, 3.5 µm) for 9 ARVs [6] |
| Mobile Phase pH | 2.0-5.5 (acidic) [18] | Suppresses ionization; improves peak shape | Acetate buffer pH 4.5 for ATV, DTG, DRV, etc. [6] |
| Buffer Concentration | 25-50 mM [6] [66] | Maintains pH stability; prevents silanol interactions | 50 mM acetate buffer [6]; 25 mM phosphate buffer [66] |
| Organic Modifier | Acetonitrile or Methanol [6] [67] | Affects selectivity and retention | Acetonitrile with gradient elution [6] |
| Temperature Control | 25-35°C [6] [67] | Improves retention time reproducibility | Column maintained at 35°C [6] |
| Flow Rate | 1.0 mL/min (conventional) [6] [67] | Impacts backpressure and separation efficiency | 1.0 mL/min for ARV separation [6] |
Column Selection and Mobile Phase Optimization
The selection of appropriate stationary phase chemistry and mobile phase composition forms the foundation for robust HPLC methods. For the simultaneous analysis of multiple antiretrovirals with diverse physicochemical properties, C18 reversed-phase columns have demonstrated excellent performance due to their robustness and reproducibility [6] [18]. The use of acidic mobile phases (pH 3-4.5) has been widely adopted to suppress ionization of basic and acidic functional groups on antiretroviral molecules, thereby improving peak symmetry and retention consistency [6] [67]. Adequate buffer capacity (typically 25-50 mM) is essential to maintain pH stability throughout the analysis, particularly for methods employing gradient elution [6] [66].
Systematic Approach to Method Optimization
A structured optimization strategy is crucial for developing robust methods. The Quality-by-Design (QbD) approach, utilizing Design of Experiments (DoE), represents a systematic methodology for identifying optimal method conditions while understanding parameter interactions [66]. This approach contrasts with traditional One-Factor-at-a-Time (OFAT) optimization by simultaneously evaluating multiple factors and their interactions, leading to more robust operational spaces [66].
Experimental Protocols for Enhanced Method Robustness
Protocol 1: Method Robustness Testing
Purpose: To evaluate the influence of small, deliberate variations in method parameters on analytical performance.
Materials:
- HPLC system with UV detection capability
- Validated method for antiretroviral analysis
- Reference standards of target analytes
- Mobile phase components (HPLC grade)
Procedure:
- Prepare standard solutions of target antiretrovirals at quality control concentration levels (low, medium, high) [6]
- Systematically vary critical method parameters one at a time while keeping others constant:
- Mobile phase pH (±0.2 units)
- Organic modifier composition (±2-3%)
- Column temperature (±2°C)
- Flow rate (±0.1 mL/min) [18]
- Inject six replicates at each varied condition
- Monitor key performance indicators:
- Retention time stability (%RSD)
- Peak area precision (%RSD)
- Resolution between critical peak pairs
- Tailing factors
- Establish acceptance criteria: %RSD < 2% for retention times, resolution > 1.5 between all critical pairs [6]
Expected Outcomes: Identification of critical parameters requiring strict control and establishment of system suitability criteria.
Protocol 2: Forced Degradation Studies for Specificity Assessment
Purpose: To demonstrate method specificity in the presence of potential degradants and impurities.
Materials:
- Drug substance or product
- Acid (0.1N HCl)
- Base (0.1N NaOH)
- Oxidizing agent (3% Hâ‚‚Oâ‚‚)
- Thermal stability oven
- Photostability chamber
Procedure:
- Subject antiretroviral standards to various stress conditions:
- Acidic hydrolysis: 0.1N HCl at room temperature for 2-4 hours
- Basic hydrolysis: 0.1N NaOH at room temperature for 2-4 hours
- Oxidative degradation: 3% Hâ‚‚Oâ‚‚ at room temperature for 2-4 hours
- Thermal degradation: 60°C for 24 hours
- Photodegradation: Exposure to UV light for 24 hours [66]
- Neutralize or quench reactions as appropriate
- Analyze stressed samples alongside unstressed controls
- Confirm baseline separation of parent drugs from degradation products
- Assess peak purity using diode array detection
Expected Outcomes: Verification of method specificity and stability-indicating capabilities, essential for reliable quantification in stability studies.
Column Protection and Lifetime Extension Strategies
HPLC column longevity is critical for maintaining method reproducibility and reducing analytical costs. Multiple protection strategies can significantly extend column lifetime while maintaining separation performance.
Table 2: Comprehensive Column Protection Strategy
| Protection Component | Specifications | Function | Implementation Example |
|---|---|---|---|
| Guard Columns | Same stationary phase as analytical column [6] | Traps particulate matter and strongly retained compounds | Sentry Guard Column (4.6 mm × 10 mm) [6] |
| In-line Filters | 0.5-2 µm porosity | Removes particulate matter from mobile phase and samples | 0.45 µm membrane filters [67] |
| Sample Pretreatment | Solid-phase extraction [6] or protein precipitation [50] | Removes proteins and interfering matrix components | Solid-phase extraction for human plasma samples [6] |
| Mobile Phase Filtration | 0.45 µm membrane filter | Removes particulates and microbial contaminants | 0.45 µm membrane filtration [67] |
| Column Temperature Control | 25-35°C [6] | Maintains consistent retention and efficiency | Column compartment at 35°C [6] |
Protocol 3: Systematic Column Care and Maintenance
Purpose: To maximize column lifetime and maintain chromatographic performance through proper maintenance practices.
Materials:
- Guard column or cartridge
- In-line filter (0.5 µm)
- Column cleaning solvents (water, acetonitrile, isopropanol)
- Storage caps
Procedure: Daily Maintenance:
- Flush column with 10-20 column volumes of water/organic solvent mixture (e.g., 50:50 water:acetonitrile) at the end of each analytical run
- Store column in appropriate organic solvent (typically 80% acetonitrile in water)
- Record column performance metrics (pressure, plate count, tailing factor) in column logbook
Preventive Maintenance:
- Replace guard cartridge after 100-200 injections or when pressure increase exceeds 10%
- Clean column with strong solvent (e.g., isopropanol) every 200-300 injections for methods involving biological matrices [6]
- Periodically reverse column flow direction (if recommended by manufacturer) to redistribute contamination
Performance Monitoring:
- Regularly analyze system suitability test mixture
- Track retention time stability and peak symmetry
- Monitor backpressure trends for sudden changes
Expected Outcomes: Extended column lifetime (typically 1000+ injections for biological samples), consistent chromatographic performance, and reduced analytical costs.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Robust HPLC-UV Analysis of Antiretrovirals
| Reagent/Material | Specifications | Function | Application Example |
|---|---|---|---|
| C18 Columns | 4.6 × 150 mm, 3.5-5 µm particle size [6] [67] | Stationary phase for reverse-phase separation | XBridge C18 (150 mm, 3.5 µm) for 9 ARVs [6] |
| Guard Columns | Matching chemistry, 10-20 mm length [6] | Pre-column contamination protection | Sentry Guard Column (10 mm) [6] |
| Acetonitrile (HPLC Grade) | ≥99.9% purity, low UV absorbance | Organic mobile phase modifier | Gradient elution with acetate buffer [6] |
| Buffer Salts | Sodium acetate, ammonium formate, phosphate buffers (HPLC grade) | Aqueous mobile phase component | 50 mM acetate buffer, pH 4.5 [6] |
| Solid Phase Extraction Cartridges | Reverse-phase C18 or mixed-mode | Sample clean-up and concentration | SPE for plasma samples prior to HPLC analysis [6] |
| Membrane Filters | 0.45 µm for mobile phases; 0.2 µm for samples | Particulate removal | 0.45 µm membrane filtration of mobile phase [67] |
| 6-Chloro-2,3-dihydro-1H-indole hydrochloride | 6-Chloro-2,3-dihydro-1H-indole hydrochloride, CAS:89978-84-7, MF:C8H9Cl2N, MW:190.07 g/mol | Chemical Reagent | Bench Chemicals |
| 5,6,7,8-Tetrahydronaphthalen-2-ylboronic acid | 5,6,7,8-Tetrahydronaphthalen-2-ylboronic Acid|CAS 405888-56-4 | High-purity 5,6,7,8-Tetrahydronaphthalen-2-ylboronic acid for research. A key building block in medicinal chemistry. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Implementing a comprehensive strategy for enhancing method robustness and extending column lifetime is essential for reliable, cost-effective HPLC-UV analysis of antiretroviral drugs. Through systematic method optimization, rigorous robustness testing, and proactive column maintenance protocols, laboratories can ensure consistent analytical performance while maximizing resource utilization. The protocols and strategies outlined in this application note provide a practical framework for maintaining analytical integrity in both pharmaceutical quality control and therapeutic drug monitoring applications.
Forced degradation studies, also known as stress testing, are an essential component of pharmaceutical development. These studies involve intentionally exposing a drug substance or product to harsh environmental conditions to elucidate its inherent stability characteristics and identify potential degradation products [68]. When conducted within the context of antiretroviral drug analysis, these studies become crucial for ensuring the safety and efficacy of HIV treatments, as degradation products may not only reduce therapeutic effectiveness but also lead to harmful side-effects [69]. The primary goal of forced degradation is to develop and validate stability-indicating analytical methods – particularly HPLC-UV – that can reliably separate, identify, and quantify the active pharmaceutical ingredient from its degradation products in various matrices, including human plasma and pharmaceutical formulations [6] [69].
For antiretroviral drugs, which often involve complex combination therapies and special population administration (e.g., pediatric dispersible tablets), understanding degradation behavior is paramount for developing appropriate formulations and establishing proper storage conditions [70]. This application note provides detailed protocols and data interpretation frameworks for conducting forced degradation studies specifically tailored to antiretroviral drugs, with emphasis on establishing validated stability-indicating HPLC-UV methods that meet regulatory standards for quality control and therapeutic drug monitoring in resource-limited settings [6] [51].
Experimental Design and Stress Conditions
Objective-Based Study Design
The design of forced degradation studies should be tailored to the specific antiretroviral drug's chemical properties and intended formulation. For protease inhibitors like darunavir and lopinavir, which possess complex molecular structures, extensive stress testing across multiple conditions is essential [6]. Similarly, non-nucleoside reverse transcriptase inhibitors such as nevirapine and rilpivirine require careful evaluation under photolytic conditions due to potential photosensitivity [51] [6].
A well-designed forced degradation study for antiretroviral drugs should aim to generate approximately 5-20% degradation of the active ingredient, as this range provides sufficient degradation products for method validation without causing excessive decomposition that could lead to secondary degradation pathways [69]. The studies should be conducted on both the drug substance and the drug product, as excipients in formulations can influence degradation patterns, particularly in solid dispersions used to enhance bioavailability of poorly soluble drugs like velpatasvir [68].
Comprehensive Stress Conditions
The following table outlines the standard stress conditions recommended for antiretroviral drugs, along with typical degradation outcomes observed for this class of compounds:
Table 1: Standard Stress Conditions for Antiretroviral Drug Forced Degradation Studies
| Stress Condition | Recommended Parameters | Typical Observations for Antiretrovirals | Relevant Drug Examples |
|---|---|---|---|
| Acidic Hydrolysis | 0.1-5 M HCl at room temperature to 70°C for 4-8 hours [68] [69] | Significant degradation observed; dolutegravir shows degradation under acidic conditions [70] | Bictegravir, dolutegravir [71] [70] |
| Basic Hydrolysis | 0.1-1 M NaOH at room temperature to 70°C for 4-8 hours [68] [69] | Variable susceptibility; tadalafil in combination products shows extensive degradation (85%) [69] | Tadalafil combination therapies [69] |
| Oxidative Stress | 3-30% Hâ‚‚Oâ‚‚ at room temperature for several hours to days [68] [69] | Moderate degradation; ambrisentan shows ~40% degradation after 3 days [69] | Ambrisentan, velpatasvir [69] [68] |
| Photolytic Stress | According to ICH Q1B; UV (320-400 nm) and visible light (400-800 nm) [68] | Velpatasvir identified as photolabile; requires protection from light [68] | Velpatasvir, nevirapine [68] [51] |
| Thermal Stress | Dry heat at 105°C for drug substance; 40-80°C for drug product [68] | Generally stable when protected from light; solid dispersions may show different behavior [68] | Velpatasvir copovidone solid dispersion [68] |
Experimental Protocols
Sample Preparation for Stress Studies
Materials and Reagents:
- Drug substance (reference standard with known purity)
- Appropriate solvents (methanol, acetonitrile, water of HPLC grade)
- Stress reagents: HCl, NaOH, Hâ‚‚Oâ‚‚ (analytical grade)
- Internal standard (e.g., quinoxaline for antiretroviral assays) [6]
Procedure:
- Prepare stock solution of the antiretroviral drug at approximately 1 mg/mL in appropriate solvent based on solubility (methanol is commonly used for drugs like dapivirine and nevirapine) [72] [51].
- For acid and base hydrolysis, add 1 mL of stock solution to 9 mL of the appropriate stressor solution (e.g., 0.1-1 N HCl or NaOH) in sealed containers to prevent evaporation.
- For oxidative stress, add 1 mL of stock solution to 9 mL of hydrogen peroxide solution (typically 3-30% v/v).
- Heat the samples at elevated temperatures (e.g., 60-70°C) if necessary to accelerate degradation, monitoring at appropriate time intervals (e.g., 4, 8, 24 hours) to achieve target degradation of 5-20%.
- For thermal degradation, expose solid drug substance to dry heat (e.g., 105°C) in stability chambers.
- For photolytic degradation, expose solid drug substance and drug product to appropriate light sources as per ICH Q1B guidelines [68].
- Neutralize the stressed samples at appropriate time intervals (particularly important for acid and base hydrolysis) to stop the degradation process.
- Prepare diluted samples for HPLC analysis at concentrations within the validated range of the analytical method.
HPLC-UV Method Development and Optimization
Chromatographic Conditions for Antiretroviral Drugs: The development of a stability-indicating HPLC-UV method for antiretroviral drugs requires careful optimization of parameters to separate multiple degradation products while maintaining sensitivity for quantification.
Table 2: Optimized HPLC-UV Conditions for Antiretroviral Drug Analysis
| Parameter | Recommended Conditions | Alternative Options |
|---|---|---|
| Column | C18 reverse-phase (150-250 mm × 4.6 mm, 3-5 μm) [6] [67] | Phenyl-hexyl for improved selectivity [70] |
| Mobile Phase | Gradient of buffer (e.g., acetate, phosphate) and organic modifier (acetonitrile/methanol) [6] [71] | Isocratic for simpler separations [67] |
| Flow Rate | 0.8-1.2 mL/min [6] [70] | Lower flow rates (0.5 mL/min) for improved separation [69] |
| Detection Wavelength | 260 nm for most antiretrovirals [6] | 230-305 nm depending on drug chromophore [6] [68] |
| Column Temperature | 30-40°C [6] [70] | Ambient temperature for stability-limited separations |
| Injection Volume | 20-65 μL [51] [67] | Lower volumes for high sensitivity detection |
Method Optimization Strategy:
- Begin with a scouting gradient (e.g., 5-95% organic phase over 20-30 minutes) to evaluate retention characteristics of the drug and potential degradation products.
- Adjust pH of the aqueous component (typically pH 2.5-4.5 using phosphate or acetate buffers) to improve peak shape and separation [71] [70].
- Modify organic solvent composition (acetonitrile vs. methanol ratios) to achieve optimal selectivity for separating the drug from its degradation products.
- For complex mixtures of antiretroviral drugs, consider using a dual calibration curve approach when co-elution occurs, as demonstrated for simultaneous analysis of nine antiretroviral agents where dolutegravir co-eluted with raltegravir and efavirenz with lopinavir [6].
- Validate the optimized method according to ICH guidelines for specificity, linearity, accuracy, precision, and robustness [69] [70].
The following workflow diagram illustrates the complete forced degradation study process from sample preparation to method validation:
Data Interpretation and Analytical Validation
Interpreting Degradation Profiles
The analysis of forced degradation samples should focus on both the extent of degradation and the formation of specific degradation products. For bictegravir, an anti-HIV drug, forced degradation studies revealed significant degradation under acid and base hydrolysis conditions, with Impurity-A being the most common degradation product in both cases [71]. Similarly, for ambrisentan and tadalafil combination (relevant for pulmonary hypertension in HIV patients), acidic conditions caused extensive degradation of ambrisentan (54.25%) but only mild degradation of tadalafil (9.30%), while basic conditions severely degraded tadalafil (85%) with minimal effect on ambrisentan (5.30%) [69].
The peak purity of the main drug component should be assessed using photodiode array detection to confirm that the drug peak is free from co-eluting impurities. This is particularly important for antiretroviral drugs like dolutegravir in dispersible tablets, where method specificity must be demonstrated for all potential impurities and degradation products [70].
Validation of Stability-Indicating Methods
For a method to be considered truly stability-indicating, it must be validated to demonstrate specificity, linearity, accuracy, precision, and robustness according to ICH guidelines [69] [70]. The following table outlines key validation parameters and acceptance criteria for HPLC-UV methods of antiretroviral drugs:
Table 3: Method Validation Parameters and Acceptance Criteria for Stability-Indicating HPLC-UV Methods
| Validation Parameter | Recommended Procedure | Acceptance Criteria |
|---|---|---|
| Specificity | Resolution of drug peak from all degradation products | Resolution ≥ 2.0 between drug and nearest degradation peak [69] |
| Linearity | Calibration curves across therapeutic range | Correlation coefficient (r²) > 0.99 [6] [67] |
| Accuracy | Recovery of drug from spiked samples | 97-103% for drug substance; 98-102% for drug product [12] |
| Precision | Repeatability (multiple injections) and intermediate precision (different days/analysts) | RSD ≤ 2.0% for assay of drug product [70] |
| LOD/LOQ | Signal-to-noise ratio of 3:1 for LOD and 10:1 for LOQ | LOQ should be sufficiently low to detect relevant impurities (e.g., <0.05% for related substances) [71] |
| Robustness | Deliberate variations in method parameters (pH, temperature, flow rate) | Method remains unaffected by small variations [69] |
Application in Antiretroviral Drug Development
Case Studies
Dolutegravir Dispersible Tablets: Forced degradation studies of dolutegravir dispersible tablets led to the development of a stability-indicating RP-HPLC method that separated the drug from its degradation products, including Impurity B (a key degradation impurity). The method was validated according to USP guidelines and demonstrated specificity, precision, linearity, and accuracy with a correlation coefficient of at least 0.997 and percentage recovery of impurities between 80-120% [70].
Multi-Antiretroviral Drug Assay: A comprehensive HPLC-UV method was developed for simultaneous quantification of nine antiretroviral drugs (including atazanavir, dolutegravir, darunavir, efavirenz, etravirine, lopinavir, raltegravir, rilpivirine, and tipranavir) in human plasma. The method demonstrated linearity across therapeutic ranges with correlation coefficients >0.99, intraday and interday precision RSD <15%, and extraction recovery between 80-120% for all analytes. This method is particularly valuable for therapeutic drug monitoring in resource-limited settings where LC-MS/MS is unavailable [6].
Velpatasvir Copovidone Solid Dispersion: Forced degradation studies of velpatasvir solid dispersion revealed degradation under alkaline, acidic, and oxidative conditions, as well as photodegradation. A stability-indicating HPLC-UV method was developed that separated velpatasvir from eight degradation products using gradient elution, enabling analysis of process impurities and degradation products in this complex formulation [68].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Forced Degradation Studies
| Reagent/Chemical | Function in Study | Application Notes |
|---|---|---|
| HCl (0.1-5 M) | Acidic hydrolysis stressor | Use sealed containers to prevent evaporation at elevated temperatures [69] [68] |
| NaOH (0.1-1 M) | Basic hydrolysis stressor | Neutralize immediately after stress period to stop degradation [69] |
| Hâ‚‚Oâ‚‚ (3-30%) | Oxidative stressor | Lower concentrations (3%) for solution studies, higher for solid state [69] [68] |
| Acetonitrile (HPLC grade) | Mobile phase component | Preferred organic modifier for reverse-phase HPLC of antiretrovirals [6] [67] |
| Methanol (HPLC grade) | Solvent for stock solutions | Alternative mobile phase component; better solubility for some antiretrovirals [51] |
| Ammonium Acetate/Phosphate Buffers | Aqueous mobile phase component | Buffer pH critical for separation; typically pH 2.5-4.5 for antiretrovirals [71] [51] |
| Quinoxaline/Diphenylamine | Internal standard | Improves quantification precision in bioanalytical methods [6] [72] |
| N-Cyclopropyl-3-nitropyridin-4-amine | N-Cyclopropyl-3-nitropyridin-4-amine|CAS 380605-28-7 | |
| 3,4-Difluoro-2-methoxybenzoic acid | 3,4-Difluoro-2-methoxybenzoic acid, CAS:875664-52-1, MF:C8H6F2O3, MW:188.13 g/mol | Chemical Reagent |
Forced degradation studies represent a critical component in the development of stability-indicating HPLC-UV methods for antiretroviral drugs. Through the systematic application of stress conditions including hydrolysis, oxidation, thermal, and photolytic degradation, researchers can develop and validate robust analytical methods that reliably separate drugs from their degradation products. The protocols outlined in this application note provide a framework for conducting these studies in compliance with regulatory guidelines, with special consideration for the unique challenges presented by antiretroviral drugs, including combination therapies and specialized formulations like solid dispersions. When properly executed, these studies ensure that analytical methods can monitor stability throughout the drug product's shelf life, ultimately contributing to the quality, safety, and efficacy of antiretroviral therapies for HIV treatment.
Ensuring Reliability: Method Validation and Comparative Analysis with Other Techniques
The reliability of analytical data in pharmaceutical development is paramount, a goal ensured through rigorous method validation. The International Council for Harmonisation (ICH) Q2(R2) guideline provides the foundational framework for this process, establishing the criteria to demonstrate that an analytical procedure is suitable for its intended purpose [73]. This application note details the practical application of ICH Q2(R2) principles, focusing on the validation parameters of linearity, precision, and accuracy. The context is a validated Reversed-Phase High-Performance Liquid Chromatography with Ultraviolet detection (RP-HPLC-UV) method for the analysis of key antiretroviral drugs, including molnupiravir, nirmatrelvir, and remdesivir [25] [44]. These parameters are critical for ensuring that the method delivers dependable results for drug potency, purity, and stability testing, ultimately supporting the quality control of pharmaceutical formulations [73] [26].
Core Validation Parameters: Methodologies and Protocols
Linearity
Linearity refers to the ability of an analytical procedure to produce test results that are directly proportional to the concentration of the analyte in a given range [74] [26].
- Experimental Protocol: To evaluate linearity, prepare a minimum of five concentrations of the analyte, covering the intended validation range. For instance, a linearity assessment for nirmatrelvir might involve concentrations from 15 µg/mL to 225 µg/mL [44]. Inject each concentration in triplicate. Plot the average peak area (or height) against the corresponding analyte concentration and perform a linear regression analysis. The resulting plot should yield a straight line, and the correlation coefficient (r) or coefficient of determination (r²) is calculated [74] [75].
- Acceptance Criteria: The correlation coefficient (r) is typically required to be greater than 0.999 for assay methods, and the coefficient of determination (r²) should be ≥ 0.9997 [25] [75]. The y-intercept should be statistically insignificant relative to the target concentration response.
Table 1: Exemplary Linearity Data for Antiviral Drugs by RP-HPLC-UV
| Analyte | Concentration Range (µg/mL) | Correlation Coefficient (r²) | Slve | Y-Intercept |
|---|---|---|---|---|
| Molnupiravir | 2 - 30 [44] | ≥ 0.9997 [25] | -- | -- |
| Nirmatrelvir | 15 - 225 [44] | ≥ 0.9997 [25] | -- | -- |
| Remdesivir | 5 - 75 [44] | ≥ 0.9997 [25] | -- | -- |
| DOTATATE | 0.5 - 3.0 [75] | 0.999 [75] | -- | -- |
Precision
Precision, a measure of method reproducibility, is assessed at three levels: repeatability, intermediate precision, and reproducibility [74] [26]. It is usually expressed as the Relative Standard Deviation (RSD) or Coefficient of Variation (CV%).
- Experimental Protocol for Repeatability: Analyze a minimum of six independent sample preparations at 100% of the test concentration, under the same operating conditions (same analyst, same instrument, same day) [74] [26]. For assay methods, the RSD for the measured content of the six preparations should not exceed a predefined limit, often < 1.1% [25].
- Experimental Protocol for Intermediate Precision: To evaluate the impact of random variations within a laboratory, have a second analyst repeat the precision study on a different day and/or using a different instrument [74] [26]. The results from both analysts are combined, and the RSD is calculated.
- Experimental Protocol for Reproducibility: This is demonstrated when the method is transferred between two different laboratories [74].
Table 2: Precision Acceptance Criteria for HPLC Methods
| Level of Precision | Experimental Design | Acceptance Criteria (RSD) |
|---|---|---|
| System Repeatability | Multiple injections (n≥5) of a single reference solution [26]. | Typically < 2.0% for peak area [26]. |
| Method Repeatability (Analysis) | Six independent sample preparations at 100% test concentration [74] [26]. | < 1.1% for assay of active ingredients [25]. |
| Intermediate Precision | Study replicated with varying analysts, days, or equipment [74]. | Combined RSD from both sets of data meets predefined criteria (e.g., < 2.0%). |
Accuracy
The accuracy of an analytical procedure expresses the closeness of agreement between the value found and the value accepted as a true or conventional reference value [74] [26]. It is typically reported as a percentage of recovery.
- Experimental Protocol: Accuracy is evaluated by analyzing the sample in a minimum of nine determinations over a minimum of three concentration levels (e.g., 80%, 100%, and 120% of the target concentration), covering the specified range [74] [26]. For drug substance assay, this can be done by spiking the analyte into a placebo matrix (for drug products) or by comparing against a reference standard of known purity. The recovery percentage for each level is calculated.
- Acceptance Criteria: Recovery rates should be close to 100%. For assay methods at the 100% level, typical acceptance criteria are 99.59% - 100.08% [25] or, more generally, recoveries within 98-102% [26]. A sliding scale is often applied for impurities, allowing for wider acceptance criteria at lower concentrations.
Table 3: Accuracy Study Design and Exemplary Results
| Accuracy Level | Number of Preparations | Theoretical Concentration | Measured Recovery (%) |
|---|---|---|---|
| Level 1 (80%) | 3 | 80 µg/mL | 99.6 - 100.1 |
| Level 2 (100%) | 3 | 100 µg/mL | 99.59 - 100.08 [25] |
| Level 3 (120%) | 3 | 120 µg/mL | 99.7 - 100.2 |
Experimental Protocol: A Consolidated Workflow
The following workflow diagram outlines the key stages in the validation of an analytical method.
Detailed Experimental Steps for HPLC-UV Method Validation
Solution Preparation:
- Standard Stock Solutions: Accurately weigh and dissolve reference standards of each analyte (e.g., molnupiravir, nirmatrelvir, remdesivir) in an appropriate solvent, typically the mobile phase or a compatible solvent like methanol/water mixture [25] [44].
- Linearity Solutions: Dilute the stock solution to obtain at least five concentrations covering the validation range (e.g., 10-50 µg/mL or other phase-appropriate ranges) [25].
- Accuracy/Precision Solutions: For drug product analysis, prepare placebo samples and spike with known amounts of the analyte at three concentration levels (80%, 100%, 120%). For repeatability, prepare six independent samples at the 100% level.
Chromatographic Conditions (Illustrative Example):
- Column: Hypersil BDS C18 (150 mm x 4.5 mm, 5 µm) [25] or Nova-Pak CN (150 mm x 3.9 mm, 4 µm) [44].
- Mobile Phase: Isocratic or gradient elution. Example: Water:Methanol (30:70 v/v, pH adjusted with 0.1% ortho-phosphoric acid) [25] or a gradient of 50 mM Ammonium Acetate and Methanol [44].
- Flow Rate: 1.0 mL/min [25] [44].
- Detection: UV at 230 nm [25] [44].
- Injection Volume: 20 µL [75].
- Column Temperature: 30°C [44] [75].
System Suitability Test (SST): Prior to validation experiments, perform SST to ensure the HPLC system is performing adequately. This typically involves multiple injections of a standard solution to verify system repeatability (RSD of peak areas < 2.0%), theoretical plate count, and tailing factor [26].
Execution and Data Analysis:
- Inject the linearity, accuracy, and precision samples in a randomized sequence.
- Record retention times and peak areas/heights.
- Perform linear regression on the linearity data.
- Calculate the mean, standard deviation, and RSD for precision data.
- Calculate the percentage recovery for accuracy data.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key materials and reagents required for the development and validation of an RP-HPLC-UV method for antiviral drugs.
Table 4: Essential Research Reagents and Materials
| Item | Specification / Example | Function / Relevance |
|---|---|---|
| HPLC System | System with UV/PDA detector, auto-sampler, and column oven. | Essential for performing the chromatographic separation and detection. |
| Analytical Column | C18 column (e.g., Hypersil BDS C18, 150 x 4.6 mm, 5 µm) [25]. | The stationary phase for reverse-phase separation of analytes. |
| Reference Standards | High-purity Molnupiravir, Nirmatrelvir, Remdesivir (purity >99%) [44]. | Critical for preparing calibration standards and determining accuracy. |
| Mobile Phase Components | HPLC-grade Water, Methanol, Acetonitrile; pH modifiers (e.g., Ortho-phosphoric acid, Trifluoroacetic Acid (TFA)) [25] [75]. | The liquid solvent that moves the analytes through the column. |
| Placebo Formulation | A mock drug product containing all excipients but the Active Pharmaceutical Ingredient (API) [26]. | Used in specificity and accuracy studies to check for interference from non-active components. |
| 2,3-Dichloropropionitrile | 2,3-Dichloropropionitrile, CAS:2601-89-0, MF:C3H3Cl2N, MW:123.97 g/mol | Chemical Reagent |
| 5-Methyl-1,3-benzodioxole | 5-Methyl-1,3-benzodioxole Supplier|CAS 7145-99-5 |
The rigorous validation of linearity, precision, and accuracy, as mandated by ICH Q2(R2) guidelines, is non-negotiable for establishing reliable HPLC-UV methods in pharmaceutical analysis. The protocols and data presented herein provide a clear roadmap for researchers to demonstrate that their analytical methods are fit for purpose. The case study on antiviral drugs like molnupiravir, nirmatrelvir, and remdesivir underscores the practical application of these principles, ensuring the generation of high-quality data that supports drug development, quality control, and regulatory submissions. A method that successfully meets all predefined validation criteria for these parameters provides a solid foundation for the trustworthiness of its analytical results.
Determining LOD, LOQ, Specificity, and Robustness
The validation of analytical methods is a critical prerequisite for generating reliable data in pharmaceutical research, especially for monitoring antiretroviral drugs in biological matrices using HPLC-UV. This document details the experimental protocols and application notes for determining four key validation parameters: Limit of Detection (LOD), Limit of Quantification (LOQ), Specificity, and Robustness. These parameters are evaluated within the context of a broader thesis focusing on the development of a validated HPLC-UV method for the simultaneous analysis of nine antiretroviral drugs (Atazanavir, Dolutegravir, Darunavir, Efavirenz, Etravirine, Lopinavir, Raltegravir, Rilpivirine, and Tipranavir) in human plasma [6]. Establishing these parameters ensures the method is sensitive, specific, and reliable for its intended use in therapeutic drug monitoring and clinical trials.
Core Parameter Definitions and Methodological Approaches
The International Conference on Harmonisation (ICH) Q2(R2) guideline provides the fundamental framework for defining and determining these analytical performance characteristics [76]. A visual summary of the logical relationships and workflow for assessing these parameters is provided below.
1Limit of Detection (LOD)
- Definition: The lowest concentration of an analyte in a sample that can be detected, but not necessarily quantified, under the stated experimental conditions. It is a limit test [76].
- Standard Acceptance Criteria: Typically, a signal-to-noise ratio (S/N) of 3:1 is considered acceptable for detection [76].
2Limit of Quantification (LOQ)
- Definition: The lowest concentration of an analyte in a sample that can be quantitatively determined with acceptable precision and accuracy [76].
- Standard Acceptance Criteria: Typically, a signal-to-noise ratio (S/N) of 10:1 is required. Furthermore, at the LOQ, the method should demonstrate a precision of ±20% and accuracy of 80–120% [77] [76].
3Specificity
- Definition: The ability of the method to measure the analyte accurately and specifically in the presence of other components that may be expected to be present in the sample matrix (e.g., impurities, degradants, or excipients) [76].
- Standard Acceptance Criteria: Specificity is demonstrated by a lack of interference at the retention time of the analyte. For chromatographic methods, this is typically confirmed by a resolution (Rs) of >1.5 between the analyte and the closest eluting potential interferent, and/or by confirming peak purity using techniques like photodiode array (PDA) detection or mass spectrometry (MS) [76].
4Robustness
- Definition: A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters (e.g., mobile phase pH, flow rate, column temperature) and provides an indication of its reliability during normal usage [76].
- Standard Acceptance Criteria: The method is considered robust if the results (e.g., analyte retention time, peak area, resolution) remain within predefined acceptance criteria (e.g., %RSD for system suitability parameters) despite these intentional fluctuations [76].
Experimental Protocols
Protocol for Determining LOD and LOQ
This protocol outlines the determination of LOD and LOQ using the signal-to-noise ratio and standard deviation methods, applicable to the analysis of antiretroviral drugs in plasma [77] [6] [76].
3.1.1 Materials and Equipment
- HPLC-UV system with autosampler and data processing software.
- Analytical column: XBridge C18 (4.6 mm × 150 mm, 3.5 µm) or equivalent [6].
- Blank human plasma (from healthy volunteers).
- Standard solutions of antiretroviral drugs (e.g., Atazanavir, Dolutegravir, etc.) and internal standard (Quinoxaline) [6].
- Centrifuge, vortex mixer, and solid-phase extraction (SPE) apparatus.
3.1.2 Step-by-Step Procedure
- Preparation of Blank and Low-Concentration Samples:
- Process a blank plasma sample (containing no analyte) through the entire sample preparation procedure (solid-phase extraction) to establish the baseline noise [6].
- Prepare and analyze a minimum of 10 independent replicates of the blank sample.
- Prepare and analyze a series of spiked plasma samples with analyte concentrations at the expected LOD/LOQ level (e.g., 20-50 ng/mL for Dolutegravir and Rilpivirine) [6].
Chromatographic Analysis:
- Inject the prepared samples into the HPLC-UV system.
- Use the chromatographic conditions as specified: gradient elution with acetonitrile and 50 mM acetate buffer (pH 4.5); flow rate of 1.0 mL/min; column temperature at 35°C; and UV detection at 260 nm and 305 nm [6].
- Record the chromatograms and measure the signal response for the analyte and the noise from the blank.
Calculation of LOD and LOQ:
- Signal-to-Noise Method: Measure the peak height (H) of the analyte from the low-concentration sample and the peak-to-peak noise (N) from the blank. Calculate the S/N ratio. The concentration giving S/N ≥ 3 is the LOD, and the concentration giving S/N ≥ 10 is the LOQ [76].
- Standard Deviation Method:
- Calculate the standard deviation (σ) of the response from the multiple blank injections.
- Determine the slope (S) of the calibration curve from linearity studies.
- Apply the formulas:
- ( LOD = 3.3 \times \frac{σ}{S} )
- ( LOQ = 10 \times \frac{σ}{S} ) [76].
3.1.3 Acceptance Criteria
- The LOD should demonstrate a signal distinguishable from the baseline noise (S/N ≥ 3).
- The LOQ should demonstrate a signal with S/N ≥ 10, and validation experiments at the LOQ concentration must show an accuracy of 80-120% and precision (RSD) of ≤20% [77] [76].
Protocol for Establishing Specificity
This protocol verifies that the method can unequivocally quantify the analytes of interest in the presence of other components in the plasma matrix [6] [76].
3.2.1 Materials
- Standard solutions of individual antiretroviral drugs.
- Blank human plasma.
- Potential interfering substances (e.g., other co-administered drugs, metabolites).
3.2.2 Step-by-Step Procedure
- Analysis of Blank Matrix: Inject a processed blank plasma sample and check for any interfering peaks at the retention times of the nine antiretroviral drugs and the internal standard.
- Analysis of Spiked Samples: Inject processed plasma samples spiked with the analytes at their respective retention times and verify that the peaks are pure and free from co-elution.
- Forced Degradation Studies (if applicable): Subject the analyte to stress conditions (acid, base, oxidation, heat, light) and analyze the samples. The method should be able to separate the analyte peak from any degradation products formed.
- Peak Purity Assessment: Use a photodiode array (PDA) detector to collect spectra across the analyte peak. The software should indicate peak purity by comparing spectra at different points (apex, up-slope, and down-slope) of the peak [76].
3.2.3 Acceptance Criteria
- There should be no interference (peak area < 20% of the LOQ peak area) from the blank matrix at the retention time of any analyte [76].
- The peak purity index for each analyte should be within the specified threshold, confirming a homogeneous peak.
- Resolution between any two closely eluting peaks (e.g., Efavirenz and Lopinavir, which co-elute under certain conditions) should be greater than 1.5 [6] [76].
Protocol for Evaluating Robustness
This protocol tests the method's resilience to small, deliberate changes in chromatographic conditions [76].
3.3.1 Experimental Design
- A set of system suitability parameters (e.g., retention time, tailing factor, theoretical plates, resolution) is monitored while varying key method parameters one at a time.
- Typical variables to test for an HPLC-UV method include:
3.3.2 Step-by-Step Procedure
- Baseline Analysis: Using the optimized conditions, analyze a system suitability sample (e.g., a middle-level QC sample) and record the critical parameters.
- Variation of Parameters: Alter one parameter (e.g., set flow rate to 0.9 mL/min) while keeping others constant, and inject the same suitability sample.
- Repeat: Repeat the analysis for each varied parameter.
- Data Analysis: Compare the results (retention time, peak area, resolution) obtained under varied conditions against the baseline results.
3.3.3 Acceptance Criteria
- The method is robust if all system suitability criteria (e.g., %RSD of peak area and retention time < 2%, resolution > 1.5 between critical pairs) are met under all varied conditions [76].
Application Notes and Data Presentation
The following table compiles quantitative data for LOD, LOQ, and specificity parameters from a validated method for nine antiretroviral drugs, demonstrating the application of the above protocols [6].
Table 1: Experimental LOD, LOQ, and Specificity Parameters for Antiretroviral Drugs by HPLC-UV
| Analyte | Retention Time (min) | Wavelength (nm) | Calibration Range (ng/mL) | Estimated LOD (ng/mL)* | Estimated LOQ (ng/mL)* | Specificity (Resolution from closest peak) |
|---|---|---|---|---|---|---|
| Dolutegravir (DTG) | 5.4 | 260 | 20 - 8000 | ~6 | ~20 | Resolved from Raltegravir [6] |
| Raltegravir (RGV) | 5.6 | 260 | 40 - 9600 | ~12 | ~40 | Resolved from Dolutegravir [6] |
| Darunavir (DRV) | 9.6 | 260 | 150 - 15000 | ~45 | ~150 | >1.5 from other components [6] |
| Rilpivirine (RPV) | 13.8 | 305 | 20 - 2000 | ~6 | ~20 | >1.5 from other components [6] |
| Atazanavir (ATV) | 15.3 | 260 | 60 - 12000 | ~18 | ~60 | >1.5 from other components [6] |
| Efavirenz (EFV) | 17.1 | 260 | 150 - 15000 | ~45 | ~150 | Co-elutes with Lopinavir; separate calibration needed [6] |
| Etravirine (ETV) | 17.4 | 305 | 50 - 4000 | ~15 | ~50 | >1.5 from other components [6] |
| Lopinavir (LPV) | 17.4 | 260 | 150 - 15000 | ~45 | ~150 | Co-elutes with Efavirenz; separate calibration needed [6] |
| Tipranavir (TPV) | 18.7 | 260 | 500 - 40000 | ~150 | ~500 | >1.5 from other components [6] |
Note: LOD and LOQ values are estimates based on the lowest point of the calibration curve and the signal-to-noise principle. The exact values should be experimentally determined as per protocol 3.1. The method demonstrated specificity for all analytes with no interference from blank plasma, though Efavirenz and Lopinavir co-eluted, necessitating two separate calibration curves (A and B) for complete analysis [6].
Case Study: Managing Co-elution for Specificity
A specific challenge in the simultaneous analysis of these nine drugs was the co-elution of Dolutegravir (DTG) with Raltegravir (RGV), and Efavirenz (EFV) with Lopinavir (LPV) [6]. The strategy to overcome this and maintain specificity was:
- Chromatographic Optimization: Employing a sophisticated gradient elution program to maximize separation where possible.
- Wavelength Selection: Utilizing two detection wavelengths (260 nm and 305 nm) to improve selectivity for certain analytes like Etravirine and Rilpivirine [6].
- Data Processing Strategy: Implementing two separate calibration curves (Curve A and Curve B). Curve A included DTG but not RGV, and EFV but not LPV. Curve B included RGV but not DTG, and LPV but not EFV. This ensured accurate quantification despite the co-elutions [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions and Materials for HPLC-UV Method Validation
| Item | Function / Purpose | Example from Antiretroviral Method |
|---|---|---|
| C18 Reverse-Phase Column | The stationary phase for chromatographic separation of analytes. | XBridge C18 (4.6 mm × 150 mm, 3.5 µm) [6]. |
| Mass Spectrometry (MS) or Photodiode Array (PDA) Detector | MS provides unequivocal peak identification and purity confirmation. PDA assesses peak purity by spectral comparison. | Used for confirming specificity and peak homogeneity [76]. |
| Matrix-Matched Standards | Calibration standards prepared in the same biological matrix as the sample to compensate for matrix effects. | Standards prepared in blank human plasma for accurate calibration [6]. |
| Stable Isotope-Labeled Internal Standards (IS) | Added to samples to correct for losses during sample preparation and variability in instrument response. | Quinoxaline was used as an IS in the antiretroviral study [6]. |
| Solid-Phase Extraction (SPE) Cartridges | For cleaning up complex biological samples and pre-concentrating analytes to improve sensitivity. | A simple SPE procedure was applied to 500 µL aliquots of plasma [6]. |
| Buffers for Mobile Phase | Control the pH of the mobile phase, which critically affects the retention and shape of analyte peaks. | 50 mM acetate buffer at pH 4.5 was used [6]. |
| 2-(4-Ethoxyphenyl)ethanol | 2-(4-Ethoxyphenyl)ethanol|CAS 22545-15-9 | 2-(4-Ethoxyphenyl)ethanol, 98% for research. A pharmaceutical intermediate. Soluble in water. For Research Use Only. Not for human or veterinary use. |
| 2-Butanone, 4-methoxy- | 2-Butanone, 4-methoxy-, CAS:6975-85-5, MF:C5H10O2, MW:102.13 g/mol | Chemical Reagent |
The rigorous determination of LOD, LOQ, specificity, and robustness is fundamental to validating any HPLC-UV method for bioanalysis. The protocols and data presented herein, framed within the context of a complex antiretroviral drug assay, provide a practical framework for researchers. By adhering to these guidelines, scientists can ensure their analytical methods are sufficiently sensitive, free from interference, and reliable enough for critical applications in drug development and therapeutic monitoring, thereby contributing valuable and trustworthy data to pharmaceutical research.
Extraction Recovery and Stability Assessments
In the development of bioanalytical methods for antiretroviral drug analysis, the validation parameters of extraction recovery and stability are critical for ensuring reliable quantification in biological matrices. Extraction recovery assesses the efficiency of the sample preparation process in extracting the analyte from the matrix, while stability evaluations guarantee that the analyte remains unchanged during sample handling, storage, and processing. This application note provides detailed protocols and data for assessing these parameters within the context of a validated HPLC-UV method for antiretroviral drug analysis, supporting research reproducibility and method robustness for scientists and drug development professionals.
Experimental Protocols
Sample Preparation and Extraction Procedure
2.1.1 Solid Phase Extraction (SPE) Protocol for Antiretrovirals in Plasma
This protocol is adapted from a validated method for simultaneous extraction of nine antiretroviral drugs from human plasma [6].
Materials:
- Blank human plasma (from healthy volunteers)
- Antiretroviral drug stock solutions (1 mg/mL in appropriate solvents)
- Internal Standard (IS) solution: Quinoxaline (7.5 mg/mL in methanol)
- Solid phase extraction cartridges (C18 or equivalent)
- HPLC-grade solvents: methanol, acetonitrile, dimethylsulfoxide (DMSO)
- Sodium acetate buffer (50 mM, pH 4.5)
- Microcentrifuge tubes (1.5 mL and 2 mL)
- Volumetric flasks and pipettes
- Vortex mixer and centrifuge
Procedure:
- Aliquot: Pipette 500 µL of human plasma (calibration, quality control, or unknown sample) into a microcentrifuge tube.
- Spike Internal Standard: Add a known volume of the working IS solution (e.g., 10 µL of quinoxaline) to each plasma aliquot [6].
- Condition SPE Cartridge: Condition the SPE cartridge sequentially with 1 mL of methanol and 1 mL of sodium acetate buffer (50 mM, pH 4.5). Do not allow the sorbent to dry.
- Load Sample: Apply the plasma sample (with IS) to the conditioned cartridge.
- Wash: Wash the cartridge with 1 mL of a mixture of sodium acetate buffer and water (e.g., 5:95, v/v) to remove interfering matrix components.
- Elute: Elute the analytes of interest into a clean collection tube using 1 mL of a suitable organic solvent, such as acetonitrile or a mixture of acetonitrile and methanol.
- Evaporate and Reconstitute: Evaporate the eluent to dryness under a gentle stream of nitrogen at 40°C. Reconstitute the dry residue with 200 µL of the HPLC mobile phase initial composition.
- Analyze: Vortex thoroughly and inject an appropriate volume (e.g., 20-50 µL) into the HPLC-UV system.
Extraction Recovery Assessment Protocol
This protocol quantifies the efficiency of the analyte's extraction from the biological matrix.
- Procedure:
- Prepare Samples:
- Set A (Extracted Standards): Prepare quality control (QC) samples at low, medium, and high concentrations (e.g., 90, 900, and 2000 ng/mL for Atazanavir) by spiking blank plasma with the analytes and internal standard. Process these samples through the entire SPE procedure detailed in Section 2.1.1 [6].
- Set B (Unprocessed Standards): Prepare equivalent concentrations of the analytes and internal standard directly in the reconstitution solution (mobile phase), representing 100% recovery. These samples are not subjected to the extraction process.
- HPLC-UV Analysis: Inject both sets of samples (Set A and Set B) into the HPLC-UV system.
- Calculation: Calculate the extraction recovery for each analyte and the IS at each QC level using the formula below. The mean recovery should be consistent, precise, and ideally within 80-120% for bioanalytical methods [6].
- Prepare Samples:
Stability Assessment Protocol
Stability of antiretroviral drugs must be evaluated under conditions mimicking sample handling and storage. The following tests should be performed at a minimum of two concentrations (low and high QC levels) with at least three replicates each [78] [79].
1. Bench-Top Stability:
- Purpose: To assess analyte stability in the matrix at ambient temperature for the expected duration of sample preparation.
- Procedure: Expose QC samples to room temperature (e.g., 25°C) for a predefined period (e.g., 24 hours). Analyze against freshly prepared calibration standards [79].
- Acceptance Criteria: The mean concentration should be within ±15% of the nominal concentration.
2. Processed Sample Stability (Autosampler Stability):
- Purpose: To ensure analyte stability in the prepared solution while in the HPLC autosampler.
- Procedure: After processing and reconstitution, store QC samples in the autosampler (e.g., at 10°C) for the maximum anticipated run time (e.g., 24 hours). Analyze and compare with freshly prepared standards [79].
- Acceptance Criteria: The mean concentration should be within ±15% of the nominal concentration.
3. Freeze-Thaw Stability:
- Purpose: To evaluate stability after multiple cycles of freezing and thawing.
- Procedure: Subject QC samples to at least three complete freeze-thaw cycles (e.g., -20°C or -80°C to room temperature). Analyze after the final cycle and compare with stability standards stored at the designated long-term temperature.
- Acceptance Criteria: The mean concentration should be within ±15% of the nominal concentration.
4. Long-Term Stability:
- Purpose: To determine the storage stability of samples in the freezer.
- Procedure: Store QC samples at the intended long-term storage temperature (e.g., -20°C or -80°C) for a period equal to or exceeding the expected storage time of study samples (e.g., 30 days or more). Analyze against freshly spiked calibration standards.
- Acceptance Criteria: The mean concentration should be within ±15% of the nominal concentration.
Data Presentation
The table below summarizes extraction recovery data for various antiretroviral drugs obtained from a validated HPLC-UV method, demonstrating the efficiency of the SPE procedure [6].
Table 1: Extraction Recovery of Antiretroviral Drugs from Human Plasma via SPE
| Analyte | Low QC Concentration (ng/mL) | Recovery at Low QC (%) | Medium QC Concentration (ng/mL) | Recovery at Medium QC (%) | High QC Concentration (ng/mL) | Recovery at High QC (%) |
|---|---|---|---|---|---|---|
| Atazanavir (ATV) | 90 | 85-95 | 900 | 88-92 | 2000 | 90-95 |
| Dolutegravir (DTG) | 50 | 82-88 | 300 | 85-90 | 2000 | 88-92 |
| Darunavir (DRV) | 600 | 84-92 | 1800 | 86-91 | 8000 | 89-94 |
| Efavirenz (EFV) | 600 | 86-94 | 1800 | 88-93 | 8000 | 91-96 |
| Etravirine (ETV) | 200 | 80-86 | 1600 | 83-88 | 3000 | 85-90 |
| Lopinavir (LPV) | 600 | 87-95 | 1800 | 89-94 | 8000 | 92-97 |
| Raltegravir (RGV) | 80 | 81-87 | 600 | 84-89 | 6000 | 86-91 |
| Rilpivirine (RPV) | 50 | 83-89 | 300 | 85-90 | 1000 | 87-92 |
| Tipranavir (TPV) | 2000 | 88-96 | 16000 | 90-95 | 30000 | 92-98 |
| Internal Standard | - | - | - | - | - | 85-110 |
The following table collates stability data for selected antiretrovirals under various stress conditions, based on validated methods [6] [79].
Table 2: Stability of Antiretroviral Drugs Under Various Conditions (% of Nominal Concentration)
| Analyte | Bench-Top (25°C, 24h) | Autosampler (10°C, 24h) | Freeze-Thaw (3 Cycles) | Long-Term (-20°C) |
|---|---|---|---|---|
| Dolutegravir (DTG) | 95-98 | 96-99 | 93-97 | 94-98 |
| Rilpivirine (RPV) | 94-97 | 95-98 | 92-96 | 93-97 |
| Darunavir (DRV) | 95-99 | 96-100 | 94-98 | 95-99 |
| Etravirine (ETV) | 93-97 | 94-98 | 91-95 | 92-96 |
| Raltegravir (RAL) | 94-98 | 95-99 | 93-97 | 94-98 |
| Maraviroc (MVC) | 95-98 | 96-100 | 94-98 | 95-99 |
Note: Data presented as percentage of nominal concentration. All values are within the acceptable range of 85-115%.
Visualizations
Workflow for Extraction and Stability Assessment
The following diagram illustrates the comprehensive experimental workflow for assessing extraction recovery and stability of antiretroviral drugs in a biological matrix.
Stability Testing Pathways
This diagram outlines the logical relationships and decision pathways involved in the comprehensive stability testing of pharmaceutical compounds.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for HPLC-UV Analysis of Antiretrovirals
| Item | Function/Benefit | Example from Context |
|---|---|---|
| C18 Reverse-Phase Column | Standard stationary phase for separating non-polar to moderately polar analytes; provides robust retention of antiretroviral compounds. | XBridge C18 (4.6 mm × 150 mm, 3.5 µm) [6]; Hypersil BDS C18 [67]; Waters Symmetry C18 [78]. |
| Internal Standards (Stable-Labeled) | Corrects for variability in extraction efficiency and instrument response; improves data accuracy and precision. | Quinoxaline [6]; Deuterated analogs (e.g., Dolutegravir-d5, Raltegravir-d4) [80] [79]. |
| Solid Phase Extraction (SPE) Cartridges | Purifies and concentrates samples by retaining analytes while removing proteins and interfering matrix components. | C18-based SPE cartridges for plasma sample clean-up [6] [13]. |
| HPLC-Grade Solvents & Buffers | Ensure minimal UV background noise and prevent system damage; buffered mobile phases control pH for reproducible retention times. | Acetonitrile/Methanol; Sodium Acetate Buffer (50 mM, pH 4.5) [6]; Ammonium Formate Buffer (10 mM, pH=4) [78]. |
| Photodiode Array (PDA) Detector | Confirms peak purity and identity by collecting full UV spectra; allows method optimization at multiple wavelengths. | Detection at 260 nm for most ARVs; 305 nm for Etravirine and Rilpivirine [6]. |
| Methyl 3-chloro-4-hydroxyphenylacetate | Methyl 3-chloro-4-hydroxyphenylacetate, CAS:57017-95-5, MF:C9H9ClO3, MW:200.62 g/mol | Chemical Reagent |
| 2-Chloro-5-nitronicotinonitrile | 2-Chloro-5-nitronicotinonitrile, CAS:31309-08-7, MF:C6H2ClN3O2, MW:183.55 g/mol | Chemical Reagent |
The quantitative analysis of active pharmaceutical ingredients (APIs), particularly in complex formulations such as antiretroviral drugs, demands robust, precise, and validated analytical methods. High-performance liquid chromatography with ultraviolet detection (HPLC-UV) and ultraviolet-visible spectrophotometry (UV-Vis) represent two foundational techniques employed for this purpose in pharmaceutical research and quality control laboratories. The selection between these methodologies is critical, as it influences the accuracy, specificity, and regulatory acceptance of the analytical data generated, especially within the context of developing a validated method for antiretroviral drug analysis [18].
This application note provides a critical comparison of HPLC-UV and UV-Vis spectrophotometry, delineating their respective principles, capabilities, and limitations. Framed within the scope of antiretroviral drug analysis, it provides detailed experimental protocols and a systematic framework for method selection to support researchers and drug development professionals in making informed decisions that align with their analytical objectives and regulatory requirements.
Principle of Operation and Key Differences
Fundamental Principles
UV-Vis Spectrophotometry is an analytical technique that measures the amount of ultraviolet or visible light absorbed by a sample at a specific wavelength. The fundamental relationship between absorbance and concentration is governed by the Beer-Lambert law (A = ε.c.l), where A is the absorbance, ε is the molar absorptivity, c is the concentration, and l is the path length [81] [82]. The instrument, a spectrophotometer, typically comprises a light source, a wavelength selector (such as a monochromator or filter), a sample holder, and a detector. Measurements are performed against a reference or blank sample to determine the true absorbance of the analytes [82].
In contrast, HPLC-UV is a separation-based technique. It involves the distribution of analytes between a stationary phase (column packing material) and a mobile phase (solvent system). Components of a mixture are separated based on their differential interaction with these phases as they are pumped through the column. Following separation, the individual components pass through a UV detector, which measures their absorbance at a set wavelength [81]. The core strength of HPLC-UV lies in this two-step process: physical separation followed by detection.
The fundamental difference between these techniques dictates their application domains. UV-Vis provides a composite absorbance measurement of the entire sample, while HPLC-UV separates the mixture into individual components before quantification [81] [83].
Specificity and Resolution of Complex Mixtures: HPLC-UV offers high specificity. Each peak in a chromatogram corresponds to a different compound, confirmed by its retention time, and the technique can effectively separate drugs from impurities, degradation products, and excipients [81]. UV-Vis, however, has low specificity. It cannot distinguish between different molecules that absorb light at the same wavelength, making it susceptible to interference from excipients or impurities with similar chromophores [81] [84]. This was demonstrated in a study on Levofloxacin, where UV-Vis was found to be inaccurate for measuring drug concentration released from a composite scaffold due to impurity interference, whereas HPLC provided reliable quantification [84].
Sensitivity: HPLC-UV is generally more sensitive, with detection limits in the ng–µg/mL range using a UV detector, which can be extended to pg–ng/mL with mass spectrometric detection [81]. UV-Vis spectrophotometry is moderately sensitive, typically operating at the µg/mL level [81].
Regulatory Acceptance: HPLC is the standard method in pharmacopeias for assays, impurity profiling, and dissolution testing and is widely accepted for regulatory submissions [81] [85]. UV-Vis is rarely accepted as the sole method for complex formulations, except in simple cases where the absence of interference is conclusively demonstrated [81].
Table 1: Comprehensive Comparison of HPLC-UV and UV-Vis Spectrophotometry
| Aspect | UV-Vis Spectrophotometry | HPLC-UV |
|---|---|---|
| Principle | Measures UV-Vis light absorption by a sample [81] | Separates compounds via liquid chromatography before UV detection [81] |
| Specificity | Low; susceptible to interference [81] | High; separates analytes from impurities [81] |
| Sensitivity | Moderate (µg/mL level) [81] | High (UV: ng–µg/mL; MS: pg–ng/mL) [81] |
| Analysis of Mixtures | Poor for complex mixtures; best for single-component solutions [81] | Excellent; can handle multicomponent formulations [81] [85] |
| Sample Preparation | Typically minimal [83] | Often required (e.g., filtration, extraction) [54] [83] |
| Analysis Speed | Fast (a few minutes) [81] [83] | Longer (10–60 minutes per run) [81] |
| Cost | Inexpensive instrument and operation [81] [83] | High capital and operational costs [81] [83] |
| Regulatory Acceptance | Limited for complex formulations [81] | Gold standard; required for pharmacopeial methods [81] [85] |
| Primary Applications | Routine API assay, dissolution testing (if no interference), quick screening [81] [83] | Drug assay, impurity profiling, stability studies, bioanalytical studies [81] [85] |
Experimental Protocols
Protocol for Q-Absorption Ratio Method in UV-Vis Spectrophotometry
The Q-Absorption Ratio method is a UV-spectrophotometric technique used for the simultaneous estimation of two components in a mixture without prior separation [86].
3.1.1 Research Reagent Solutions
Table 2: Key Reagents and Materials for UV-Vis Analysis
| Reagent/Material | Function |
|---|---|
| Standard API(s) | Primary reference standard for calibration and quantification. |
| HPLC-Grade Methanol | Solvent for dissolving standards and samples. |
| Volumetric Flasks | For precise preparation and dilution of standard and sample solutions. |
| Quartz Cuvettes | Sample holder; quartz is transparent to UV light [82]. |
3.1.2 Method Steps
- Standard Solution Preparation: Accurately weigh and dissolve pure standards of the two analytes (e.g., Cefixime and Moxifloxacin) in a suitable solvent to prepare stock solutions. Dilute these to obtain a series of standard solutions of known concentrations [86].
- Wavelength Selection: Scan the standard solutions using a UV-Vis spectrophotometer to determine the absorbance spectra. Identify two wavelengths: one being the λmax of the first analyte (λ1) and an other being the λmax of the second analyte (λ2). A third wavelength (iso-absorptive point, λ3) where both analytes have the same molar absorptivity is also identified [86].
- Calibration: Measure the absorbance of all standard solutions at all three wavelengths (λ1, λ2, and λ3). Calculate the Q-values (QM = A2/A1) for the standard mixtures. The concentration of each component is determined using derived equations that relate the absorbance ratio to the concentration ratio [86].
- Sample Analysis: Process the sample formulation to extract the APIs into solution. Dilute the sample solution appropriately and measure its absorbance at λ1, λ2, and λ3. Use the calibration data and Q-absorption ratio equations to calculate the concentration of each drug in the sample [86].
Protocol for RP-HPLC Method for Antiretroviral Drug Analysis
This protocol outlines the development and validation of a stability-indicating RP-HPLC method for the simultaneous quantification of two antiretroviral drugs, such as Lamivudine (3TC) and Tenofovir (TDF), in a fixed-dose combination tablet [18].
3.2.1 Research Reagent Solutions
Table 3: Key Reagents and Materials for HPLC-UV Analysis
| Reagent/Material | Function |
|---|---|
| C18 Column | The stationary phase for reversed-phase separation; most widely used for ARVs [18]. |
| HPLC-Grade Water | The aqueous component of the mobile phase. |
| HPLC-Grade Acetonitrile/Methanol | Organic modifiers for the mobile phase to control retention and selectivity. |
| Buffer Salts (e.g., KHâ‚‚POâ‚„, Kâ‚‚HPOâ‚„) | Used to prepare mobile phase buffers to control pH and improve peak shape [18]. |
| Ortho-Phosphoric Acid | For pH adjustment of the mobile phase, typically to acidic conditions (pH 2-5.5) for ARV analysis [18]. |
| Syringe Filters (Nylon, 0.45 µm or 0.22 µm) | For clarification of the final sample solution to protect the HPLC column from particulates [54]. |
3.2.2 Method Steps
- Chromatographic Conditions:
- Column: Sepax BR-C18 or equivalent (250 mm x 4.6 mm, 5 µm) [84].
- Mobile Phase: A mixture of phosphate buffer and an organic solvent (e.g., Acetonitrile or Methanol). A common starting point is a ratio of 75:25 (v/v) buffer:acetonitrile. The pH is often adjusted to be acidic (e.g., pH 3.0-5.0) using ortho-phosphoric acid to suppress ionization of ionizable analytes and enhance peak shape [18].
- Flow Rate: 1.0 mL/min [84].
- Detection Wavelength: 260-280 nm (to be optimized based on the UV maxima of the specific ARVs) [18].
- Column Temperature: 40 °C [84].
- Injection Volume: 20 µL [84].
Mobile Phase Preparation: Prepare the aqueous buffer solution as per the method, adjust the pH accurately, and mix with the organic solvent as per the determined ratio. Filter the final mobile phase through a 0.45 µm membrane filter and degas by sonication.
Standard Solution Preparation: Accurately weigh and transfer pure standards of the ARVs into a volumetric flask. Dissolve and dilute with the mobile phase or a compatible solvent to obtain a stock solution. Further dilute to prepare working standard solutions covering the required concentration range (e.g., 5–25 µg/mL for each drug) [86].
Sample Solution Preparation: Weigh and powder not less than 20 tablets. Transfer an accurately weighed amount of the powder, equivalent to one tablet's drug content, into a volumetric flask. Add diluent, sonicate for 15-20 minutes to extract the drugs, and dilute to volume. Filter a portion of the solution through a 0.45 µm syringe filter before injection [86].
System Suitability Testing: Prior to sample analysis, inject the standard solution to ensure the system is suitable. Key parameters include retention time reproducibility (%RSD < 2%), theoretical plate count (>2000), tailing factor (<2.0), and resolution between the two primary peaks (>2.0) [86] [18].
Calibration and Quantification: Inject the series of working standard solutions to construct a calibration curve (peak area vs. concentration). The method should demonstrate a correlation coefficient (R²) > 0.999. Inject the sample solutions and quantify the drug content by comparing the peak areas to the calibration curve [86].
Visualization of Method Selection and Development
The following diagrams provide a logical workflow for selecting between these analytical techniques and outline the core steps in HPLC method development.
Diagram 1: Analytical Method Selection Workflow. This decision tree guides the choice between UV-Vis and HPLC-UV based on sample complexity and analytical requirements.
Diagram 2: Key Stages of HPLC Method Development. The four essential steps for developing a robust and reproducible HPLC method, from initial screening to formal validation [54].
The choice between HPLC-UV and UV-Vis spectrophotometry is not a matter of one technique being superior to the other, but rather of selecting the right tool for the specific analytical challenge. UV-Vis spectrophotometry offers a rapid, simple, and cost-effective solution for the quantitative analysis of single-component samples where interference is not a concern. However, for the analysis of complex mixtures such as fixed-dose antiretroviral drugs, where specificity, sensitivity, and the ability to resolve APIs from impurities and degradation products are paramount, HPLC-UV is the unequivocal technique of choice [81] [84] [18].
The rigorous validation protocols and widespread regulatory acceptance of HPLC-UV further cement its status as the gold standard for pharmaceutical analysis in drug development and quality control. The experimental protocols and decision framework provided herein are designed to assist researchers in the development and application of these critical analytical methods.
When to Choose HPLC-UV Over Advanced Techniques Like LC-MS/MS
In the era of advanced analytical technologies, high-performance liquid chromatography with ultraviolet detection (HPLC-UV) maintains a critical position in pharmaceutical analysis, particularly for therapeutic drug monitoring (TDM) of antiretroviral agents. While liquid chromatography-tandem mass spectrometry (LC-MS/MS) offers superior sensitivity and specificity, HPLC-UV provides a cost-effective, robust, and technically accessible alternative that is particularly well-suited to resource-limited settings and routine clinical monitoring [6] [87]. The development of validated HPLC-UV methods for antiretroviral drug analysis represents a strategic approach that balances analytical performance with practical implementation constraints.
The persistence of HPLC-UV in specialized research and clinical environments stems from its demonstrated reliability for quantifying drugs at therapeutic concentrations, relatively straightforward method development, and significantly lower operational costs [51]. This application note examines specific scenarios where HPLC-UV emerges as the preferred analytical technique, supported by experimental data and detailed protocols from antiretroviral drug analysis research.
Comparative Technical Specifications: HPLC-UV vs. LC-MS/MS
Table 1: Technical and operational comparison between HPLC-UV and LC-MS/MS for antiretroviral drug analysis
| Parameter | HPLC-UV | LC-MS/MS |
|---|---|---|
| Capital Equipment Cost | 3-5 times lower [51] | Significantly higher |
| Operational Complexity | Moderate; requires HPLC expertise | High; requires specialized MS expertise |
| Sensitivity | Suitable for therapeutic concentrations (ng/mL range) [6] | Superior (pg/mL range) [87] |
| Sample Throughput | Moderate to high (25-minute run times) [6] | High (5.5-minute run times) [5] |
| Method Development | Relatively straightforward | Complex due to ionization optimization |
| Matrix Effects | Minimal with proper sample preparation [87] | Significant; requires stable isotope IS |
| Maintenance Requirements | Routine column and lamp replacement | Complex vacuum system and source maintenance |
Key Application Scenarios for HPLC-UV Implementation
Resource-Limited Settings and Sustainable Analytical Methods
In resource-constrained environments, HPLC-UV provides a sustainable analytical platform for therapeutic drug monitoring without compromising data quality. The development of HPLC-UV methods for nevirapine quantification demonstrates how this technology can be effectively implemented with considerably lower operational costs while still meeting stringent bioanalytical validation requirements [51]. These methods maintain performance through strategic optimization of extraction techniques and mobile phase composition rather than relying on advanced detection technology.
The sustainability advantage of HPLC-UV extends beyond initial equipment acquisition to encompass reduced consumable costs and technical training requirements. Unlike LC-MS/MS, which requires expensive stable isotope-labeled internal standards to compensate for matrix effects, HPLC-UV methods can utilize more readily available compounds as internal standards [51]. This significantly reduces the recurring costs associated with routine analysis, making therapeutic drug monitoring programs more feasible in settings with limited budgets.
Routine Therapeutic Drug Monitoring of Antiretrovirals
HPLC-UV platforms have proven highly effective for routine therapeutic drug monitoring of antiretroviral agents, where target analytes are typically present at concentrations well within detection limits. A validated HPLC-UV method for simultaneous quantification of nine antiretroviral drugs demonstrated excellent performance across their respective therapeutic ranges, with coefficients of determination (r²) exceeding 0.99 for all analytes and precision values with relative standard deviations below 15% [6].
Recent clinical validation studies have further confirmed the reliability of HPLC-UV for TDM applications. When patient serum levels of antiepileptic drugs quantified by HPLC-UV were compared with those determined by immunoassay and LC-MS/MS, the results showed close correlation between methods, establishing that well-optimized HPLC-UV methods provide clinically equivalent data for therapeutic decision-making [87]. This demonstrates that for established antiretroviral regimens with known therapeutic ranges, HPLC-UV delivers sufficient analytical performance without the complexity of mass spectrometry.
Analysis of Fluorescent Antiretroviral Compounds
For antiretroviral compounds with native fluorescence properties, HPLC with fluorescence detection provides an alternative detection strategy that offers enhanced sensitivity and selectivity over UV detection alone. A recent method for simultaneous quantification of emtricitabine, daclatasvir, and ledipasvir in human urine employed programmed fluorescence detection with wavelength switching, achieving detection limits in the nanogram per milliliter range without requiring mass spectrometric detection [21].
This approach leverages the intrinsic molecular properties of certain antiretrovirals to achieve sensitivity approaching that of LC-MS/MS for specific applications. The method demonstrated linearity across clinically relevant concentration ranges (500-15,000 ng/mL for emtricitabine, 1-50 ng/mL for daclatasvir, and 10-100 ng/mL for ledipasvir) with accuracy values between 97.9% and 104.17% for all analytes [21]. Such performance is entirely adequate for therapeutic monitoring and pharmacokinetic studies, particularly when analyzing drugs with strong fluorescent characteristics.
Experimental Protocol: HPLC-UV Method for Simultaneous Antiretroviral Analysis
Materials and Reagents
Table 2: Essential research reagents and materials for HPLC-UV analysis of antiretroviral drugs
| Reagent/Material | Specification | Application Purpose |
|---|---|---|
| HPLC System | With UV/DAD detector and column oven | Separation and detection |
| Analytical Column | XBridge C18 (4.6 × 150 mm, 3.5 µm) [6] | Chromatographic separation |
| Mobile Phase A | 50 mM acetate buffer, pH 4.5 [6] | Aqueous component |
| Mobile Phase B | Acetonitrile (HPLC grade) | Organic modifier |
| Solid Phase Extraction | C18 cartridges (e.g., MonoSpin C18) [87] | Sample clean-up |
| Internal Standard | Quinoxaline [6] | Quantification reference |
| Reference Standards | Antiretroviral drugs (≥95% purity) [6] | Calibration and QC |
Chromatographic Conditions and Instrument Configuration
The following protocol adapts and optimizes conditions from published methods for simultaneous analysis of multiple antiretroviral drugs [6]:
Instrument Setup:
- Column: XBridge C18 (4.6 mm × 150 mm, 3.5 µm) or equivalent reversed-phase column
- Mobile Phase: Gradient elution with solvent A (50 mM acetate buffer, pH 4.5) and solvent B (acetonitrile)
- Gradient Program: Initial 40% B for 9 min, increase to 80% B over 7 min, maintain 80% B for 4 min, return to 40% B for re-equilibration
- Flow Rate: 1.0 mL/min
- Column Temperature: 35°C
- Detection: UV at 260 nm for most antiretrovirals; 305 nm for etravirine and rilpivirine
- Injection Volume: 10-50 µL (dependent on sensitivity requirements)
Sample Preparation Protocol (Solid Phase Extraction):
- Pretreatment: Condition SPE cartridge with 500 µL methanol followed by 500 µL water
- Sample Loading: Apply 500 µL plasma sample to conditioned cartridge
- Washing: Remove interfering components with 500 µL water
- Elution: Elute analytes with 150 µL aqueous acetonitrile (50-70% depending on analyte polarity)
- Analysis: Inject eluate directly into HPLC system [87]
Figure 1: HPLC-UV Method Development Workflow for Antiretroviral Drug Analysis
Method Validation Parameters
For regulatory acceptance, HPLC-UV methods must demonstrate adequate performance across key validation parameters:
- Linearity: Calibration curves with coefficient of determination (r²) ≥ 0.99 across therapeutic range [6]
- Precision: Intra-day and inter-day precision with RSD ≤ 15% [6] [51]
- Accuracy: Mean accuracy within ±15% of nominal concentrations [6]
- Specificity: No interference from plasma components or co-medications [51]
- Recovery: Extraction efficiency between 80-120% for all analytes [6]
- Stability: Analyte stability demonstrated under storage and processing conditions
Decision Framework for Method Selection
Figure 2: Analytical Method Selection Decision Tree
The decision to implement HPLC-UV over LC-MS/MS should be guided by specific analytical requirements and operational constraints. HPLC-UV is particularly advantageous when:
- Analytes are present at concentrations > 10 ng/mL in the sample matrix [6]
- Capital and operational budgets are constrained, as HPLC-UV systems cost 3-5 times less than LC-MS/MS platforms [51]
- Technical expertise in mass spectrometry is limited, as HPLC-UV operation requires less specialized training
- Sample throughput requirements are moderate, with analysis times of 20-30 minutes being acceptable
- Matrix components are well-characterized and don't cause significant interference [87]
Conversely, LC-MS/MS remains essential for applications requiring:
- Ultra-high sensitivity (sub-ng/mL concentrations)
- Analysis of complex matrices with significant interference potential
- Very high sample throughput requirements [5]
- Structural characterization or metabolite identification
HPLC-UV methodology remains a vital analytical tool in antiretroviral research and therapeutic drug monitoring, particularly in settings where cost-effectiveness, sustainability, and technical accessibility are paramount considerations. The technique provides sufficient sensitivity and specificity for quantifying most antiretroviral drugs at therapeutic concentrations when appropriately validated [6] [87]. Through strategic method optimization—including selective sample preparation, judicious mobile phase selection, and targeted detection schemes—HPLC-UV delivers reliable analytical data that supports clinical decision-making and pharmaceutical quality control.
The continued development and validation of robust HPLC-UV methods ensures that essential therapeutic drug monitoring remains accessible across diverse healthcare settings, ultimately contributing to improved treatment outcomes for patients receiving antiretroviral therapy worldwide.
Conclusion
HPLC-UV remains a cornerstone technique for the analysis of antiretroviral drugs, successfully balancing analytical performance, accessibility, and cost-effectiveness. Its proven capability for the simultaneous quantification of multiple drugs, including newer agents like dolutegravir and rilpivirine, makes it indispensable for therapeutic drug monitoring, supporting the management of complex drug interactions and polypharmacy in aging HIV populations. The rigorous validation frameworks established ensure data reliability for both clinical and pharmaceutical applications. Future directions should focus on developing even faster, greener chromatographic methods, expanding applications to emerging antiviral agents, and further simplifying sample preparation to enhance throughput. As HIV treatment evolves and the need for accessible monitoring grows, robust HPLC-UV methods will continue to be vital tools for improving patient outcomes and advancing biomedical research.
References
- 1. Antiretroviral Therapy (ART): How It Works & Side Effects [https://my.clevelandclinic.org/health/treatments/antiretroviral-therapy]
- 2. Initiation of antiretroviral therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4066590/]
- 3. HIV Antiretroviral Therapy - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK513308/]
- 4. Antiretroviral Therapy and HIV Drug Resistance [https://www.paho.org/en/topics/antiretroviral-therapy-and-hiv-drug-resistance]
- 5. A High-Performance Liquid Chromatography-Mass ... [https://www.medrxiv.org/content/10.1101/2025.06.08.25329229v1.full-text]
- 6. Development of an HPLC–UV assay method for the ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5762929/]
- 7. Core Concepts - Antiretroviral Medications and Initial Therapy [https://www.hiv.uw.edu/go/antiretroviral-therapy/general-information/core-concept/all]
- 8. A sensitive method for therapeutic drug monitoring in HIV ... [https://www.sciencedirect.com/science/article/abs/pii/S1010603025006707]
- 9. Reversed-phase liquid chromatographic method with ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267008006909]
- 10. Development and validation of reversed-phase HPLC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5432066/]
- 11. Development and validation of analytical method for ... [https://arabjchem.org/development-and-validation-of-analytical-method-for-quantitation-of-emtricitabine-tenofovir-efavirenz-based-on-hplc/]
- 12. Development and validation of RP-HPLC and ultraviolet ... [https://pubmed.ncbi.nlm.nih.gov/16330261/]
- 13. Validation of high-performance liquid chromatography ... [https://www.sciencedirect.com/science/article/pii/S1130634307753813]
- 14. A rapid validated UV-HPLC method for the simultaneous ... [https://pubmed.ncbi.nlm.nih.gov/28361525/]
- 15. A Review of FDA-Approved Anti-HIV-1 Drugs, Anti-Gag ... [https://www.mdpi.com/1422-0067/25/7/3659]
- 16. Determination of HIV drugs in biological matrices: A review [https://www.sciencedirect.com/science/article/abs/pii/S0003267009006849]
- 17. Development and validation of RP-HPLC and ultraviolet ... [https://www.sciencedirect.com/science/article/pii/S1570023205008408]
- 18. Liquid chromatographic determination of dual therapy ... [https://link.springer.com/article/10.1007/s44371-025-00333-6]
- 19. Green micellar liquid chromatography for The ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25007556]
- 20. Comparative Study of UV And HPLC Methods for ... [https://www.ijsrtjournal.com/article/Comparative-Study-of-UV-And-HPLC-Methods-for-Estimation-of-Drug]
- 21. Sensitive RP-HPLC method with fluorimetric detection for ... [https://www.nature.com/articles/s41598-025-07401-y]
- 22. Validation of an HPLC-UV method for the determination of ... [https://pubmed.ncbi.nlm.nih.gov/21330092/]
- 23. Tandem mass spectrometry of small-molecule antiviral drugs [https://pmc.ncbi.nlm.nih.gov/articles/PMC7834215/]
- 24. UPLC-MS/MS method for the simultaneous quantification ... [https://pubmed.ncbi.nlm.nih.gov/31962247/]
- 25. Development and validation of a RP-HPLC method for ... [https://pubmed.ncbi.nlm.nih.gov/40664729/]
- 26. Validation of Stability-Indicating HPLC Methods for ... [https://www.chromatographyonline.com/view/validation-of-stability-indicating-hplc-methods-for-pharmaceuticals-overview-methodologies-and-case-studies]
- 27. Solid-phase extraction combined with dispersive liquid ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708518317424]
- 28. An accurate and precise high performance liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4480778/]
- 29. Validation of liquid/liquid extraction method coupled with ... [https://www.sciencedirect.com/science/article/abs/pii/S1570023206002273]
- 30. Salting-out Liquid-Liquid Extraction (SALLE) [https://www.chromatographyonline.com/view/salting-out-liquid-liquid-extraction-salle]
- 31. Flow analysis-solid phase extraction system and UHPLC-MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11324774/]
- 32. Methods optimization and application: Solid phase ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708523001279]
- 33. Development of an HPLC-UV assay method for the ... [https://pubmed.ncbi.nlm.nih.gov/29404009/]
- 34. Development of an HPLC–UV assay method for the ... [https://www.sciencedirect.com/science/article/pii/S2095177916300557]
- 35. The Hydrophobic-Subtraction Model for Reversed-Phase ... [https://www.chromatographyonline.com/view/hydrophobic-subtraction-model-reversed-phase-liquid-chromatography-reprise]
- 36. Leveraging Strengths of green chromatography in ... [https://www.sciencedirect.com/science/article/abs/pii/S0026265X24017570]
- 37. Adjusted green HPLC determination of nirmatrelvir and ... [https://www.nature.com/articles/s41598-022-26944-y]
- 38. Modern Trends and Best Practices in Mobile-Phase ... [https://www.chromatographyonline.com/view/modern-trends-and-best-practices-mobile-phase-selection-reversed-phase-chromatography-0]
- 39. HPLC Tips & Tricks: Mobile Phase Preparation Part 2 [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/analytical-chemistry/small-molecule-hplc/hplc-tips-tricks-mobile-phase-preparation?srsltid=AfmBOor-tWnEVeqLx99CI12RXui_c6JmnNxj0Fycdyo2w7D9wu2rqLsU]
- 40. Effect of Organic Solvent on Selectivity in LC Separations [https://www.restek.com/articles/effect-of-organic-solvent-on-selectivity-in-lc-separations?srsltid=AfmBOoork3gugOW801o7xHm8RUawjVr9N-C_-tcAm8YHxS3oTLg5ruBP]
- 41. Mobile Phase Buffers in Liquid Chromatography [https://www.chromatographyonline.com/view/mobile-phase-buffers-in-liquid-chromatography-the-buffer-detector-battle]
- 42. Data on validation using accuracy profile of HPLC-UV ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6449764/]
- 43. Evaluation of the clinical and quantitative performance of a ... [https://jphcs.biomedcentral.com/articles/10.1186/s40780-023-00298-7]
- 44. Rapid RP-HPLC-UV determination of molnupiravir ... [https://link.springer.com/article/10.1007/s44371-025-00354-1]
- 45. Applications and retention properties of alternative organic ... [https://www.sciencedirect.com/science/article/pii/S2772391724000227]
- 46. Gradient vs. Isocratic - HPLC Elution Modes [https://lifesciences.danaher.com/us/en/products/chromatography-columns/topics/gradient-vs-isocratic-elution-hplc.html]
- 47. Gradient vs. Isocratic HPLC: Which Method is Best for Your ... [https://www.mastelf.com/gradient-vs-isocratic-hplc-which-method-is-best-for-your-application/]
- 48. Isocratic vs Gradient Elution In HPLC: How to Choose In 9 ... [https://pharmaguru.co/isocratic-vs-gradient-elution-in-hplc/]
- 49. When is Gradient Elution Better than Isocratic Elution? [https://www.biotage.com/blog/when-is-gradient-elution-better-than-isocratic-elution]
- 50. Development and Validation of an HPLC-UV Method for ... [https://www.mdpi.com/1422-0067/25/5/2685]
- 51. Development and validation of a high performance liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6556864/]
- 52. Development and validation of a RP-HPLC method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264094/]
- 53. Development and Validation of a HPLC and an UV ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3263711/]
- 54. HPLC Method Development Steps [https://www.thermofisher.com/us/en/home/industrial/chromatography/chromatography-learning-center/liquid-chromatography-information/hplc-method-development-steps.html]
- 55. A Generic HPLC/UV Platform Method for Cleaning ... [https://www.americanpharmaceuticalreview.com/Featured-Articles/122193-A-Generic-HPLC-UV-Platform-Method-for-Cleaning-Verification/]
- 56. Advanced high-resolution chromatographic strategies for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11576662/]
- 57. Real Solutions to Improve Your HPLC Peak Resolution [https://www.thermofisher.com/blog/analyteguru/real-solutions-to-improve-your-hplc-peak-resolution/]
- 58. Development and Validation of an HPLC-UV Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9230883/]
- 59. Development and Validation of a Simple and Reliable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11205493/]
- 60. The development and validation of a method using high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4039613/]
- 61. Design-assisted HPLC-UV method for therapeutic drug ... [https://www.nature.com/articles/s41598-024-78793-6]
- 62. Comparison of HPLC and UV Spectrophotometric Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8653657/]
- 63. A validated HPLC-UV method and optimization of sample ... [https://pubmed.ncbi.nlm.nih.gov/25963229/]
- 64. Comparison of ultraviolet and refractive index detections in ... [https://www.sciencedirect.com/science/article/abs/pii/S030881462101520X]
- 65. Different UV Signal Responses [http://www.chromforum.org/viewtopic.php?t=121909]
- 66. A quality-by-design optimized LC method for navigating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357339/]
- 67. Development and validation of a RP-HPLC method for ... [https://www.nature.com/articles/s41598-025-09904-0]
- 68. Forced Degradation Studies and Development ... [https://www.mdpi.com/2079-6382/11/7/897]
- 69. Stability-Indicating RP-HPLC Method for the Determination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4500576/]
- 70. Stability Indicating RP-HPLC Method Development and ... [https://pharmacophorejournal.com/article/stability-indicating-rp-hplc-method-development-and-validation-of-related-substances-for-dolutegravi-l6pixy32ghwcbl8]
- 71. Development of LC/LCMS method for estimation ... [https://www.sciencedirect.com/science/article/pii/S1872204024001142]
- 72. Development and validation of a HPLC method for the ... [https://www.sciencedirect.com/science/article/abs/pii/S1570023212006253]
- 73. ICH Q2(R2) Validation of analytical procedures [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 74. Validation of analytical procedures according to the ICH ... [https://efor-group.com/en/validation-of-analytical-procedures-according-to-the-ich-guidelines/]
- 75. Validation of the HPLC Analytical Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10171759/]
- 76. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 77. Practical Analysis of LOD and LOQ with Examples [https://www.chemistryjobinsight.com/2025/03/practical-analysis-lod-loq-method.html]
- 78. Development and Validation of a Stability-Indicating HPLC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8605923/]
- 79. Validation of a UHPLC-MS/MS Method to Quantify Twelve ... [https://www.mdpi.com/1424-8247/14/1/12]
- 80. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10922569/]
- 81. UV Spectrophotometry vs HPLC: Key Differences [https://www.linkedin.com/posts/satish-s-mane_uv-spectrophotometry-vs-hplc-1-principle-activity-7374455512681086976-wOHu]
- 82. UV-Vis Spectroscopy: Principle, Strengths and Limitations ... [https://www.technologynetworks.com/analysis/articles/uv-vis-spectroscopy-principle-strengths-and-limitations-and-applications-349865]
- 83. Comparative Study of UV And HPLC Methods for ... [https://www.ijsrtjournal.com/article/Comparative+Study+of+UV+And+HPLC+Methods+for+Estimation+of+Drug]
- 84. Comparison of high-performance liquid chromatography ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6425260/]
- 85. The Essence of Modern HPLC: Advantages, Limitations ... [https://www.chromatographyonline.com/view/essence-modern-hplc-advantages-limitations-fundamentals-and-opportunities]
- 86. Comparative validation of UV-spectrophotometry and RP ... [https://www.sciencedirect.com/science/article/abs/pii/S0003269724002689]
- 87. Evaluation of the clinical and quantitative performance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10544152/]